Cranial nerves Trigeminal nerve Trigeminal nerve V Trigeminal


- Slides: 71
Cranial nerves
Trigeminal nerve
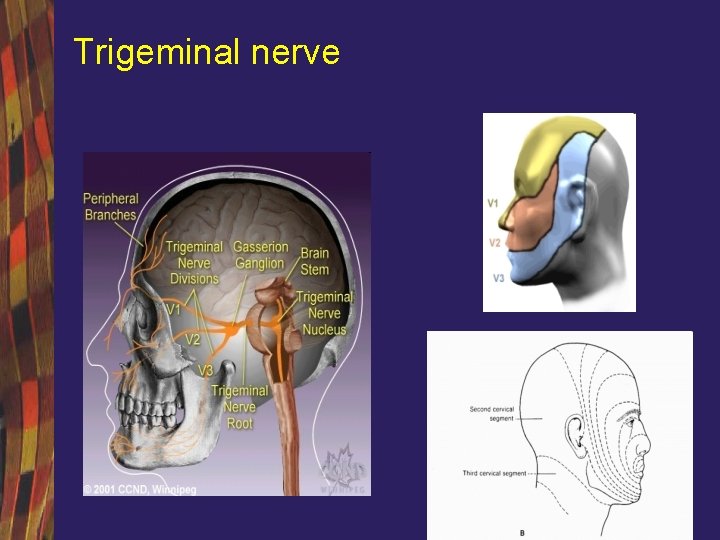
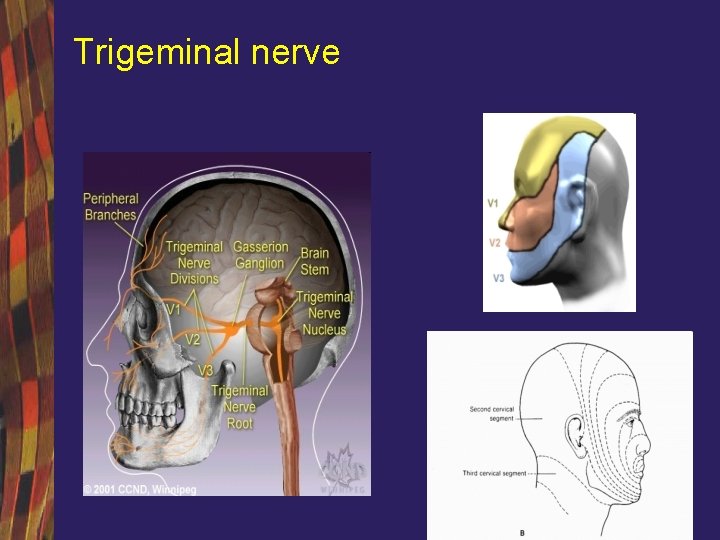
Trigeminal nerve
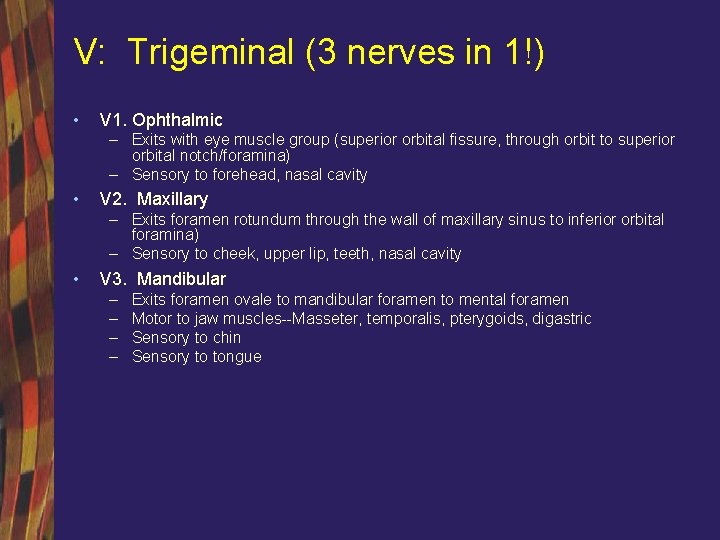
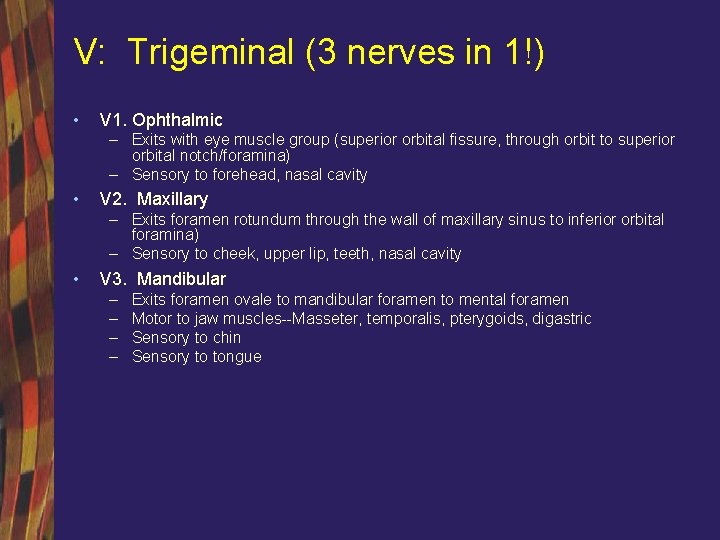
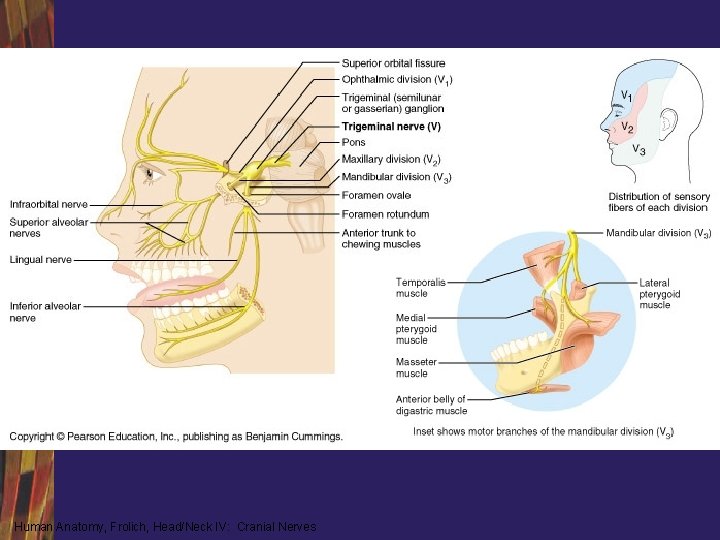
V: Trigeminal (3 nerves in 1!) • V 1. Ophthalmic – Exits with eye muscle group (superior orbital fissure, through orbit to superior orbital notch/foramina) – Sensory to forehead, nasal cavity • V 2. Maxillary – Exits foramen rotundum through the wall of maxillary sinus to inferior orbital foramina) – Sensory to cheek, upper lip, teeth, nasal cavity • V 3. Mandibular – – Exits foramen ovale to mandibular foramen to mental foramen Motor to jaw muscles--Masseter, temporalis, pterygoids, digastric Sensory to chin Sensory to tongue
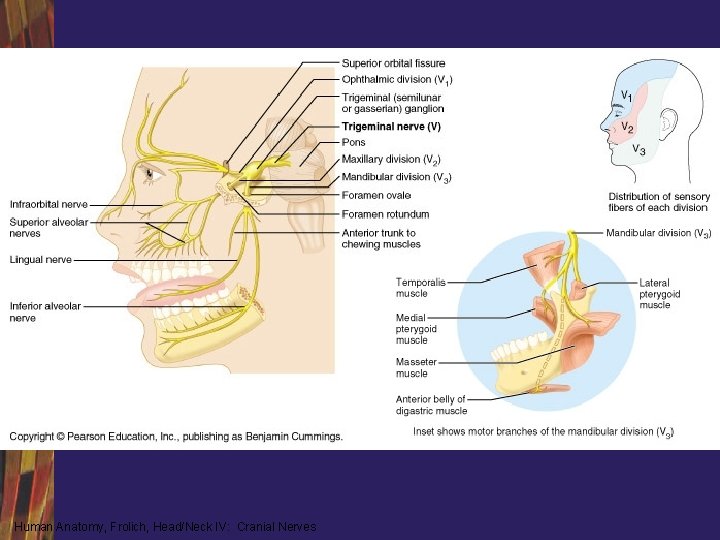
Human Anatomy, Frolich, Head/Neck IV: Cranial Nerves
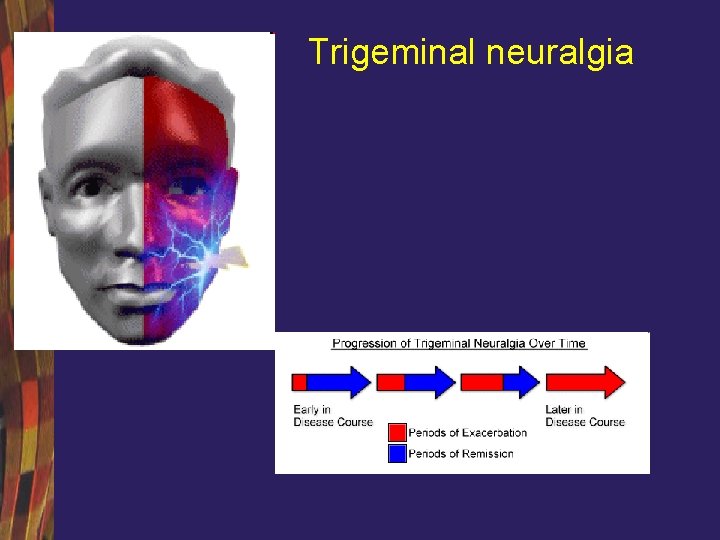
Trigeminal neuralgia
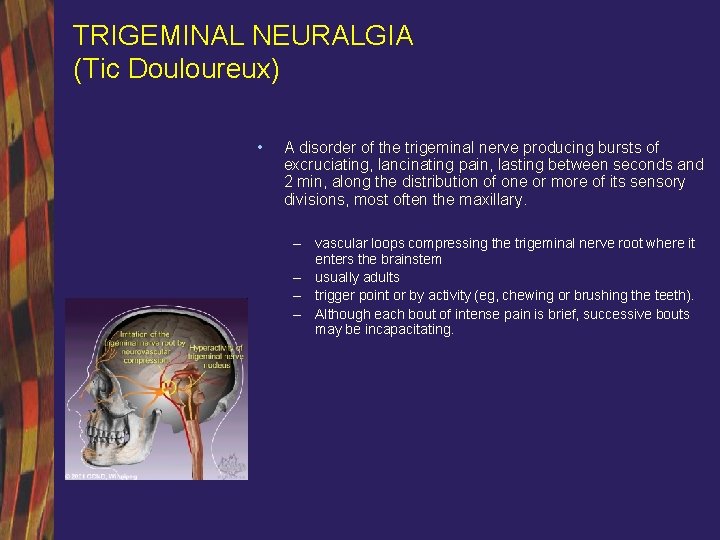
TRIGEMINAL NEURALGIA (Tic Douloureux) • A disorder of the trigeminal nerve producing bursts of excruciating, lancinating pain, lasting between seconds and 2 min, along the distribution of one or more of its sensory divisions, most often the maxillary. – vascular loops compressing the trigeminal nerve root where it enters the brainstem – usually adults – trigger point or by activity (eg, chewing or brushing the teeth). – Although each bout of intense pain is brief, successive bouts may be incapacitating.
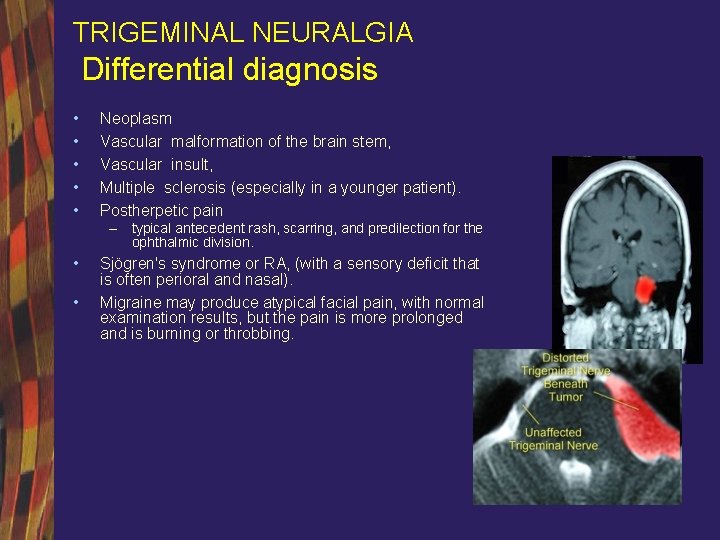
TRIGEMINAL NEURALGIA Differential diagnosis • • • Neoplasm Vascular malformation of the brain stem, Vascular insult, Multiple sclerosis (especially in a younger patient). Postherpetic pain – typical antecedent rash, scarring, and predilection for the ophthalmic division. • • Sjögren's syndrome or RA, (with a sensory deficit that is often perioral and nasal). Migraine may produce atypical facial pain, with normal examination results, but the pain is more prolonged and is burning or throbbing.
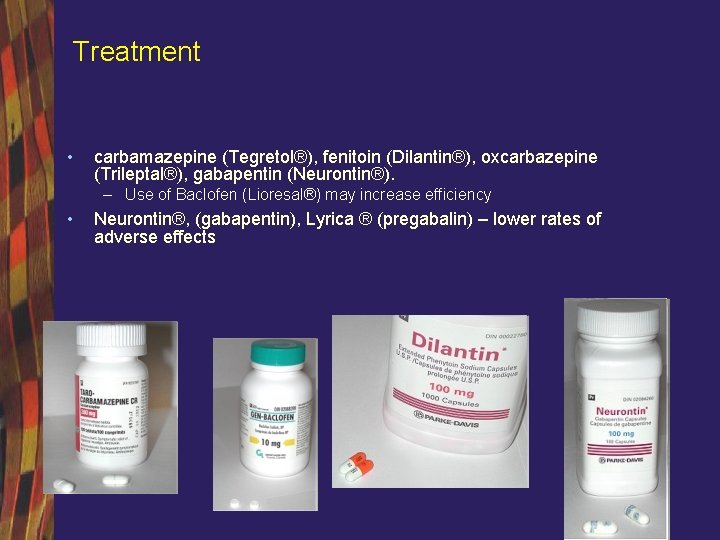
Treatment • carbamazepine (Tegretol®), fenitoin (Dilantin®), oxcarbazepine (Trileptal®), gabapentin (Neurontin®). – Use of Baclofen (Lioresal®) may increase efficiency • Neurontin®, (gabapentin), Lyrica ® (pregabalin) – lower rates of adverse effects
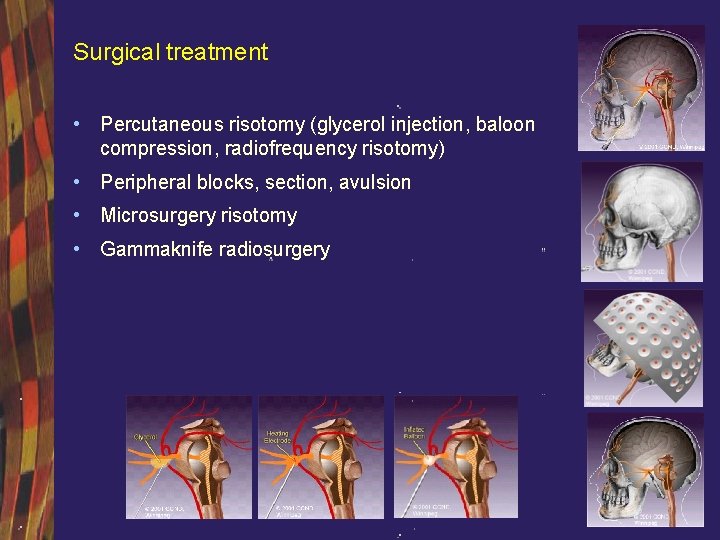
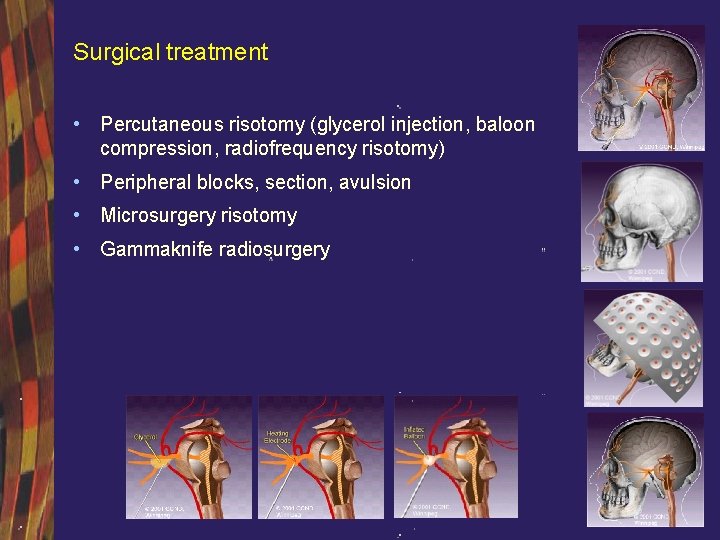
Surgical treatment • Percutaneous risotomy (glycerol injection, baloon compression, radiofrequency risotomy) • Peripheral blocks, section, avulsion • Microsurgery risotomy • Gammaknife radiosurgery
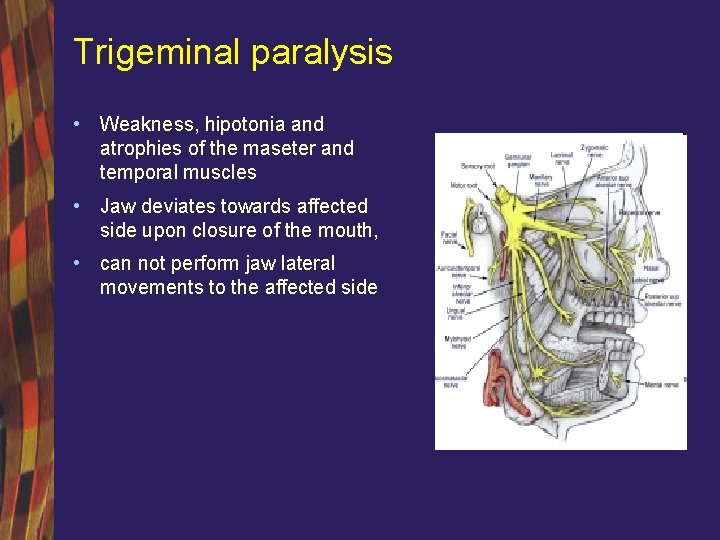
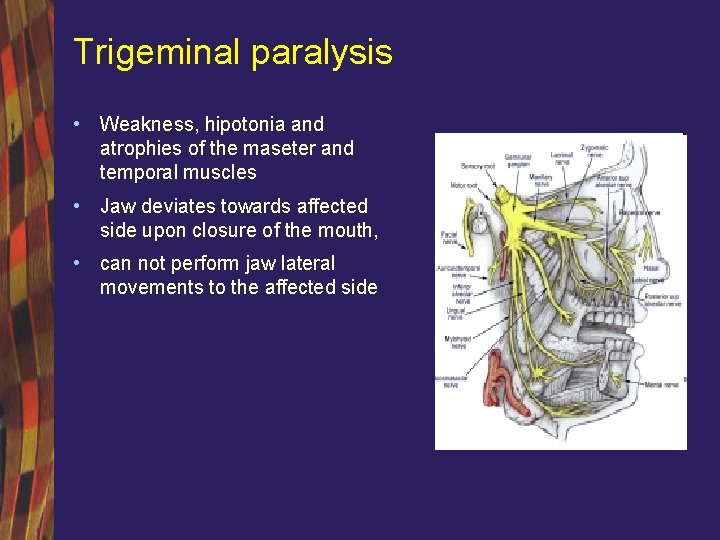
Trigeminal paralysis • Weakness, hipotonia and atrophies of the maseter and temporal muscles • Jaw deviates towards affected side upon closure of the mouth, • can not perform jaw lateral movements to the affected side
Facial nerve
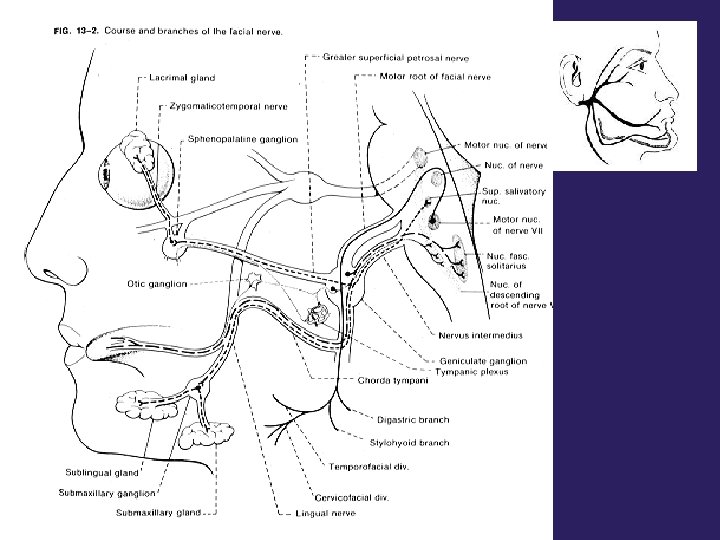
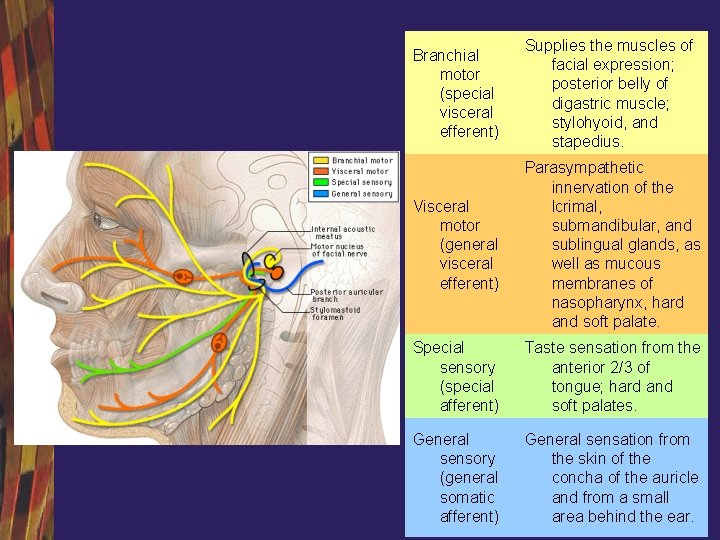
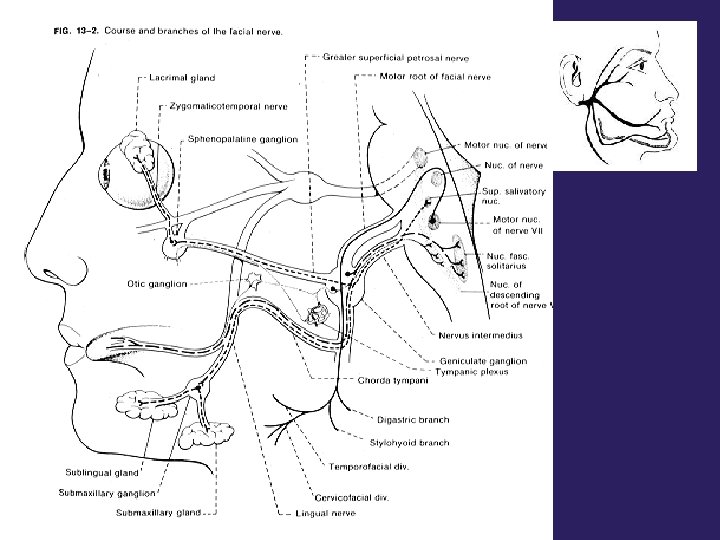
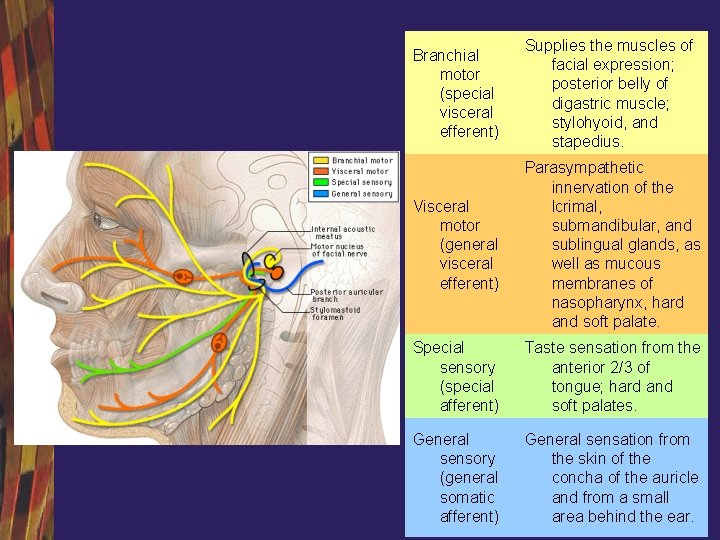
Branchial motor (special visceral efferent) Supplies the muscles of facial expression; posterior belly of digastric muscle; stylohyoid, and stapedius. Visceral motor (general visceral efferent) Parasympathetic innervation of the lcrimal, submandibular, and sublingual glands, as well as mucous membranes of nasopharynx, hard and soft palate. Special sensory (special afferent) Taste sensation from the anterior 2/3 of tongue; hard and soft palates. General sensory (general somatic afferent) General sensation from the skin of the concha of the auricle and from a small area behind the ear.
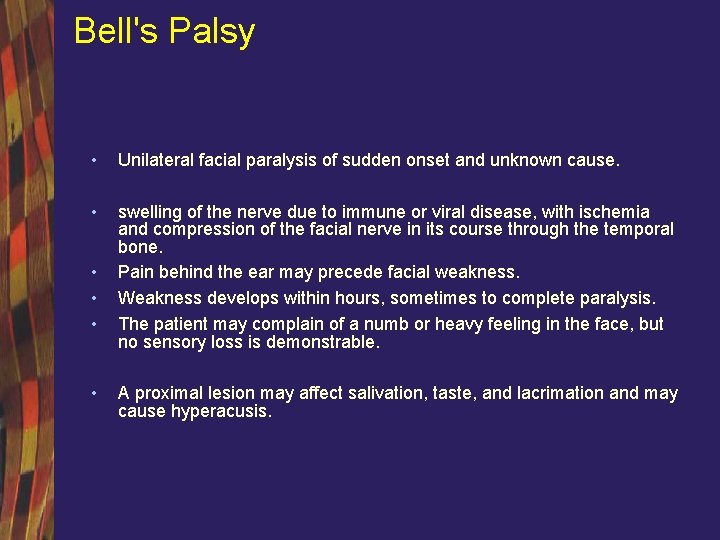
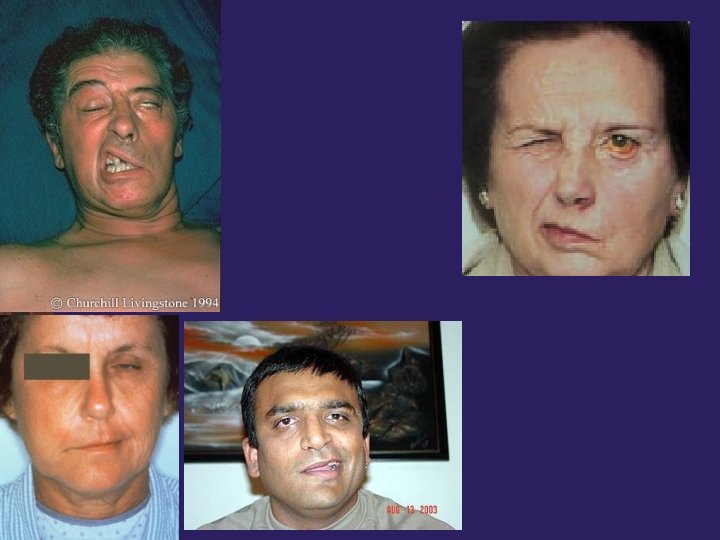
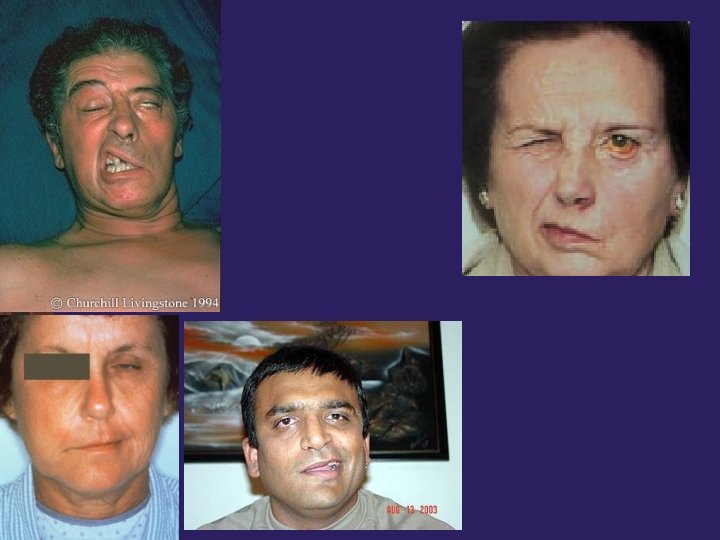
Bell's Palsy • Unilateral facial paralysis of sudden onset and unknown cause. • swelling of the nerve due to immune or viral disease, with ischemia and compression of the facial nerve in its course through the temporal bone. Pain behind the ear may precede facial weakness. Weakness develops within hours, sometimes to complete paralysis. The patient may complain of a numb or heavy feeling in the face, but no sensory loss is demonstrable. • • A proximal lesion may affect salivation, taste, and lacrimation and may cause hyperacusis.
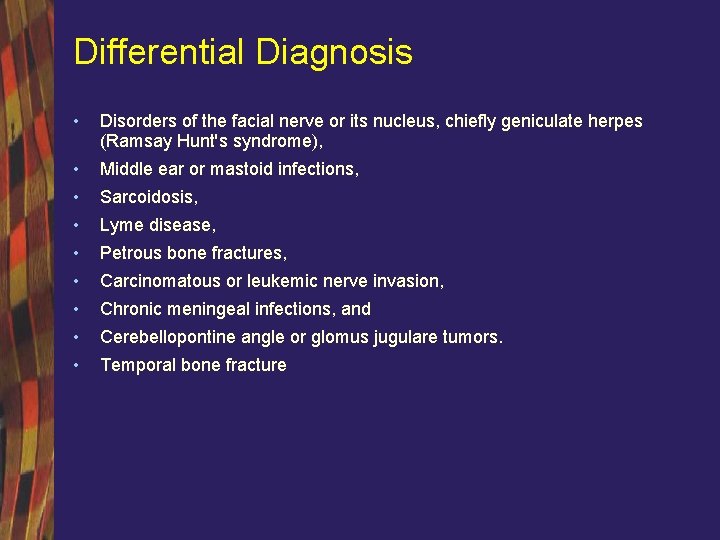
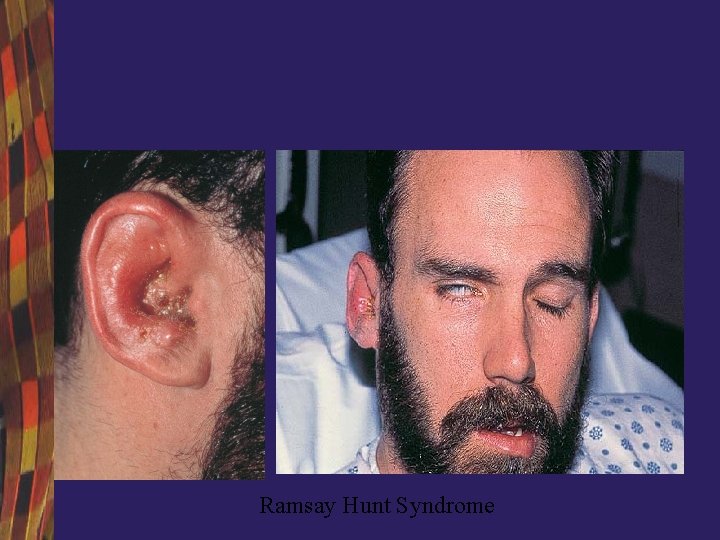
Differential Diagnosis • Disorders of the facial nerve or its nucleus, chiefly geniculate herpes (Ramsay Hunt's syndrome), • Middle ear or mastoid infections, • Sarcoidosis, • Lyme disease, • Petrous bone fractures, • Carcinomatous or leukemic nerve invasion, • Chronic meningeal infections, and • Cerebellopontine angle or glomus jugulare tumors. • Temporal bone fracture

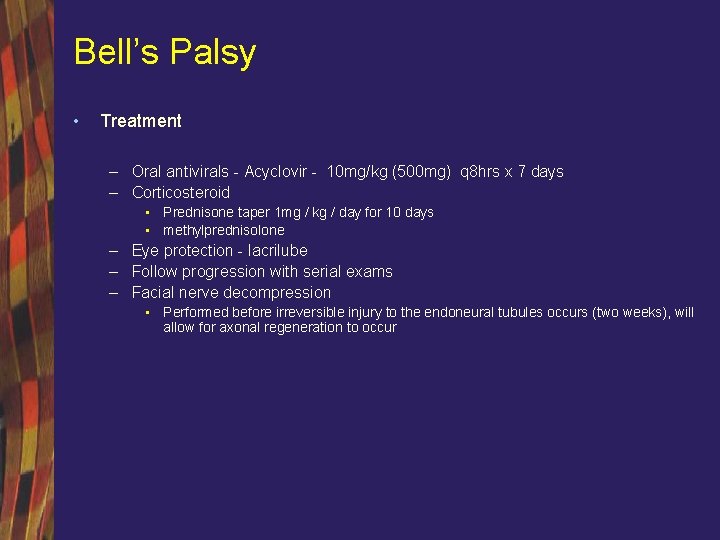
Bell’s Palsy • Treatment – Oral antivirals - Acyclovir - 10 mg/kg (500 mg) q 8 hrs x 7 days – Corticosteroid • Prednisone taper 1 mg / kg / day for 10 days • methylprednisolone – Eye protection - lacrilube – Follow progression with serial exams – Facial nerve decompression • Performed before irreversible injury to the endoneural tubules occurs (two weeks), will allow for axonal regeneration to occur
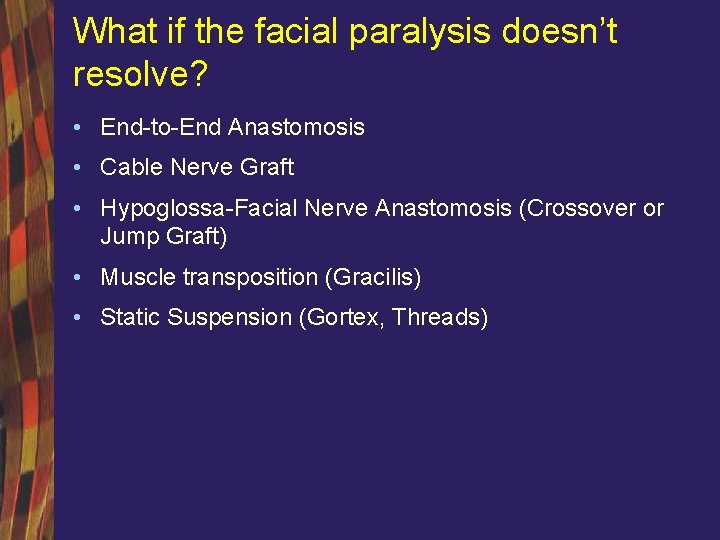
What if the facial paralysis doesn’t resolve? • End-to-End Anastomosis • Cable Nerve Graft • Hypoglossa-Facial Nerve Anastomosis (Crossover or Jump Graft) • Muscle transposition (Gracilis) • Static Suspension (Gortex, Threads)
Complications • Keratitis • Emotional/Social Issues • Synkinesis
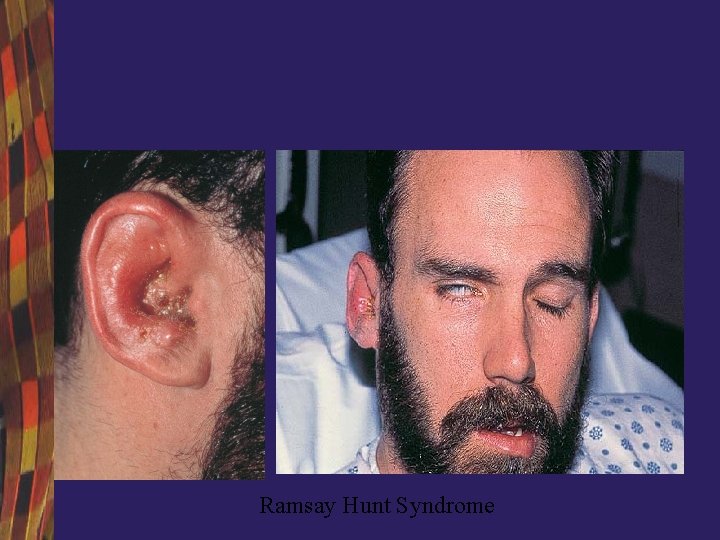
Ramsay Hunt Syndrome
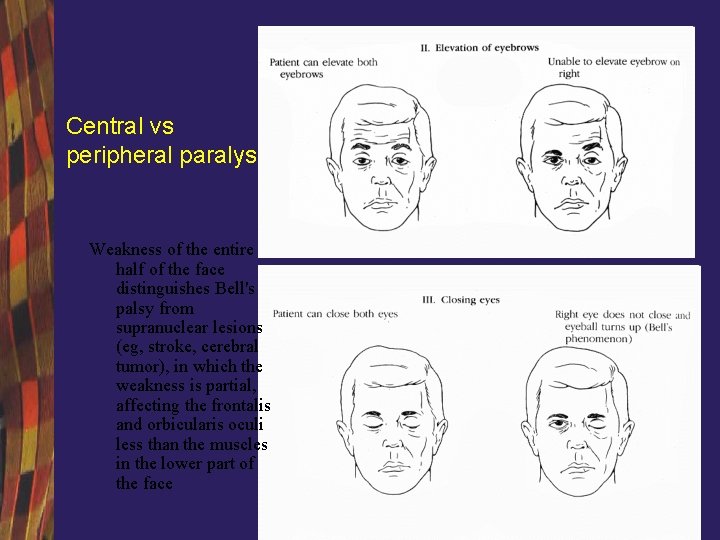
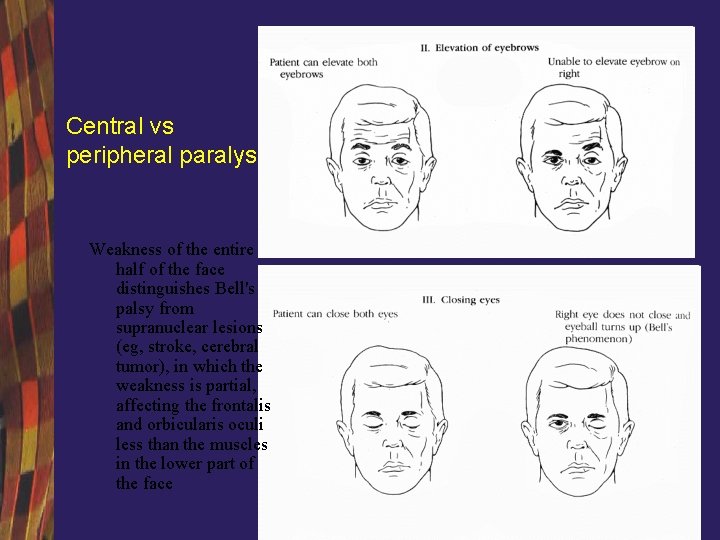
Central vs peripheral paralysis Weakness of the entire half of the face distinguishes Bell's palsy from supranuclear lesions (eg, stroke, cerebral tumor), in which the weakness is partial, affecting the frontalis and orbicularis oculi less than the muscles in the lower part of the face
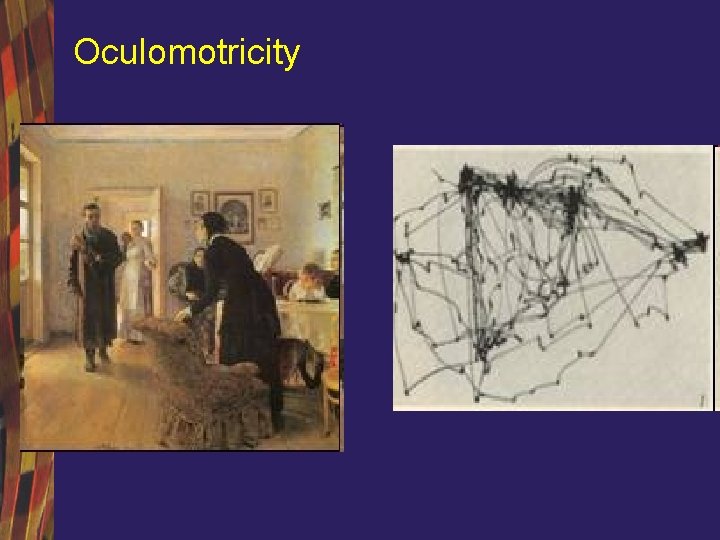
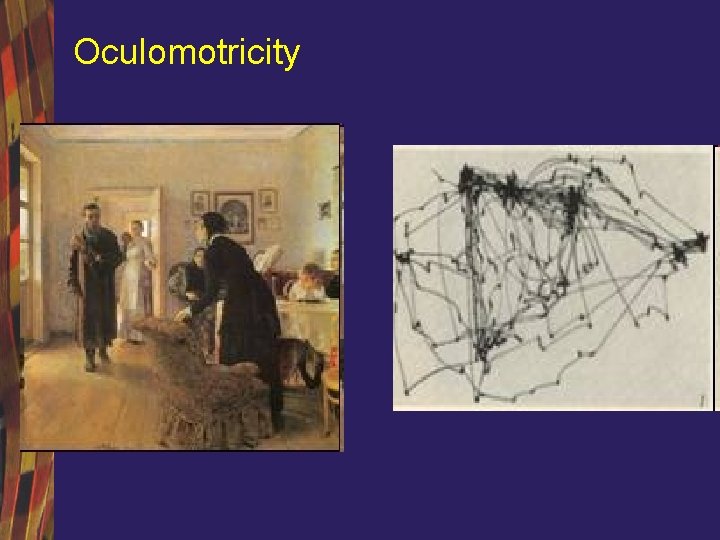
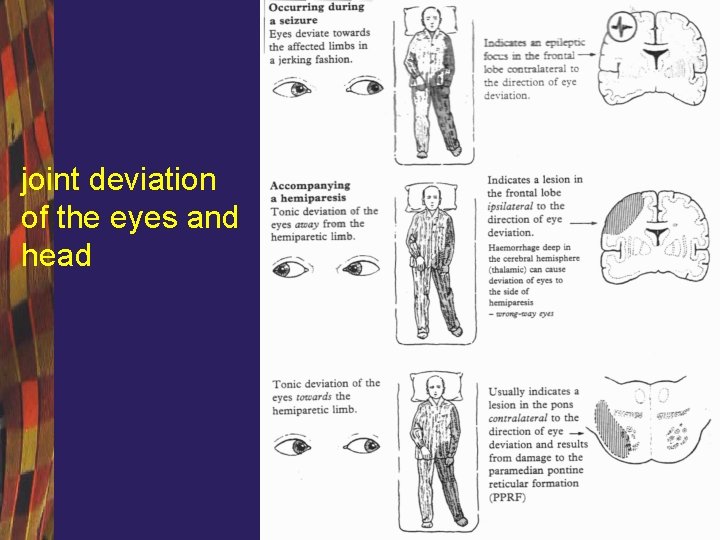
Oculomotricity
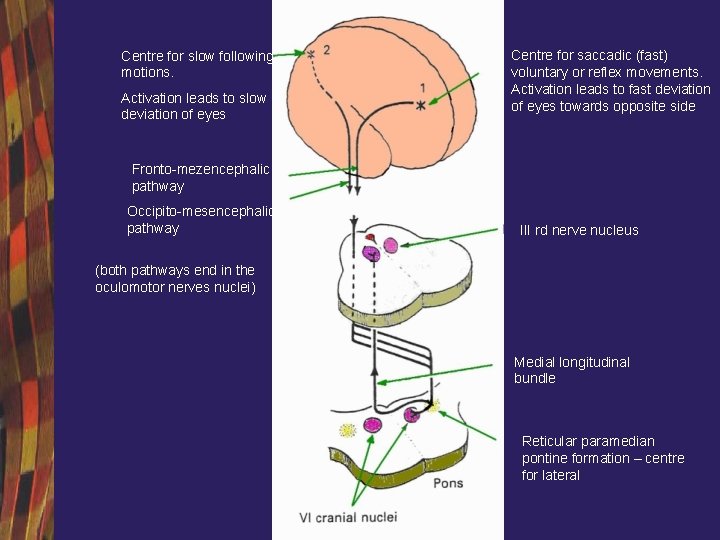
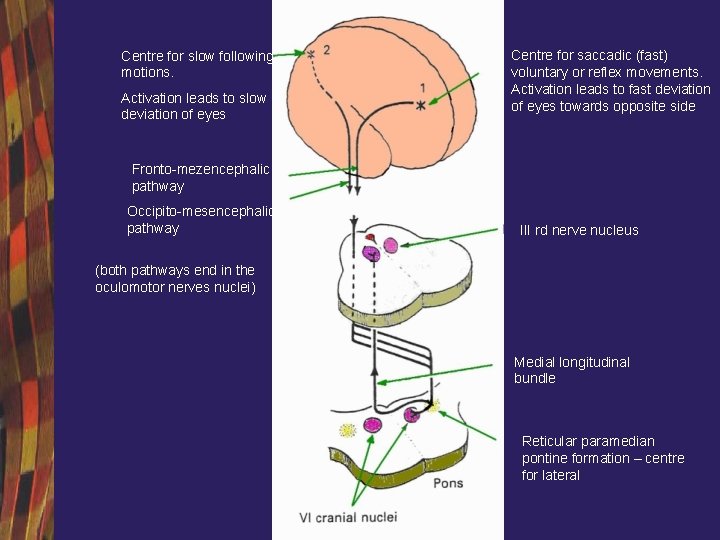
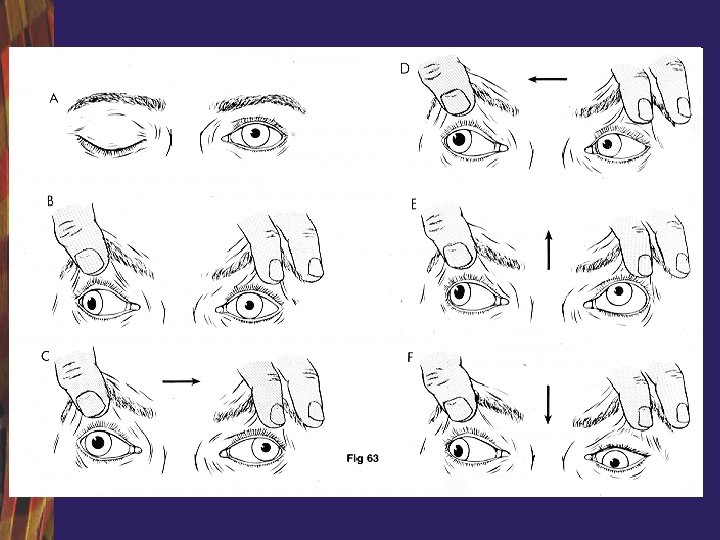
Centre for slow following motions. Activation leads to slow deviation of eyes Centre for saccadic (fast) voluntary or reflex movements. Activation leads to fast deviation of eyes towards opposite side Fronto-mezencephalic pathway Occipito-mesencephalic pathway III rd nerve nucleus (both pathways end in the oculomotor nerves nuclei) Medial longitudinal bundle Reticular paramedian pontine formation – centre for lateral
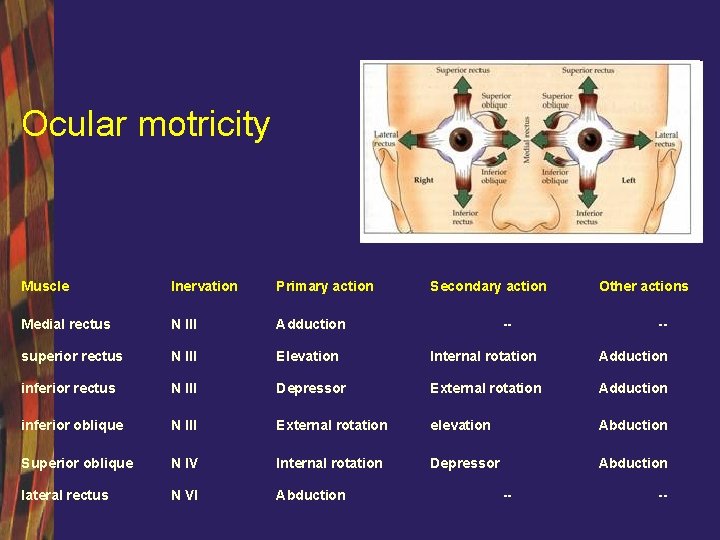
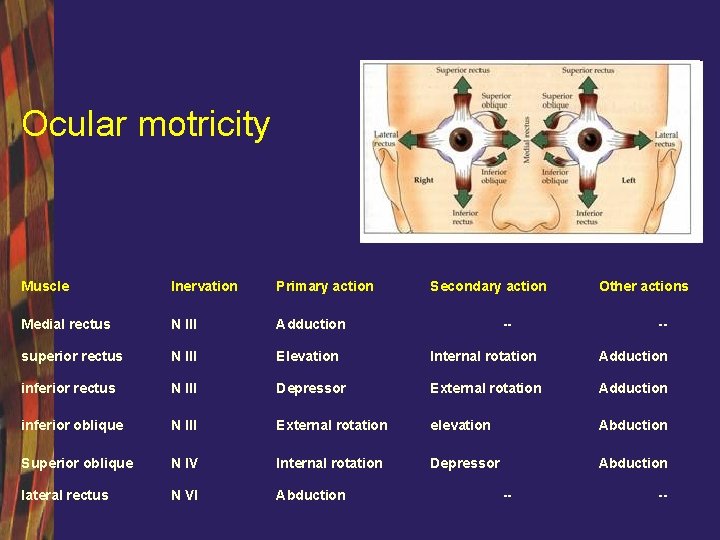
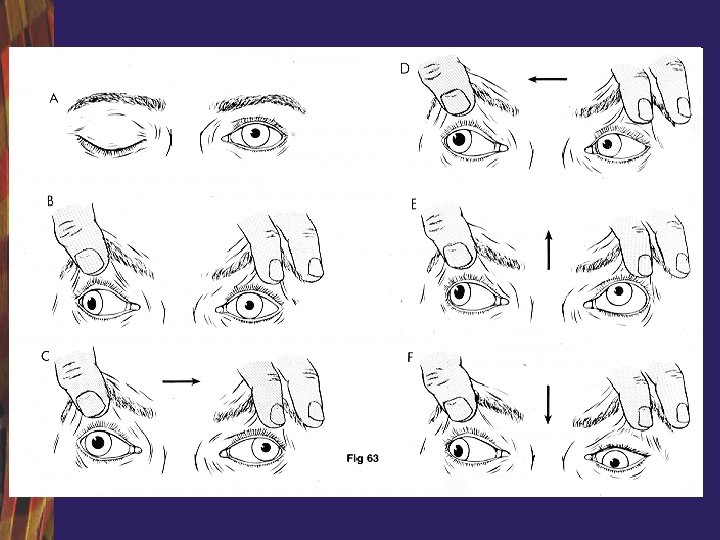
Ocular motricity Muscle Inervation Primary action Secondary action Medial rectus N III Adduction superior rectus N III Elevation Internal rotation Adduction inferior rectus N III Depressor External rotation Adduction inferior oblique N III External rotation elevation Abduction Superior oblique N IV Internal rotation Depressor Abduction lateral rectus N VI Abduction -- -- Other actions -- --
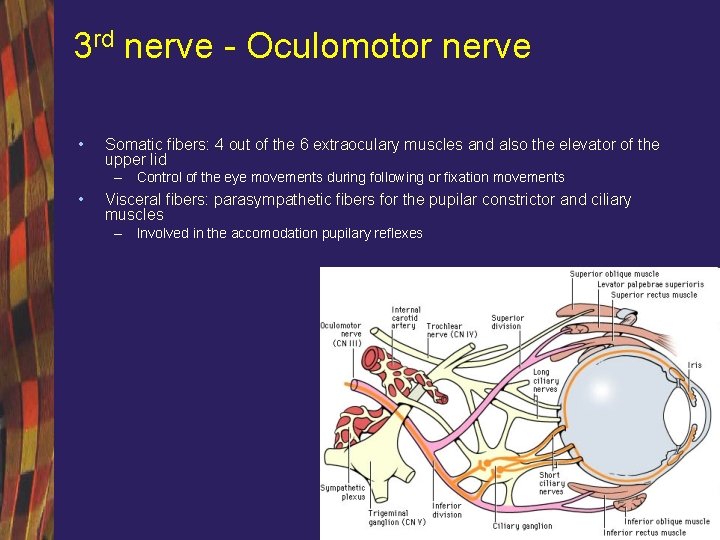
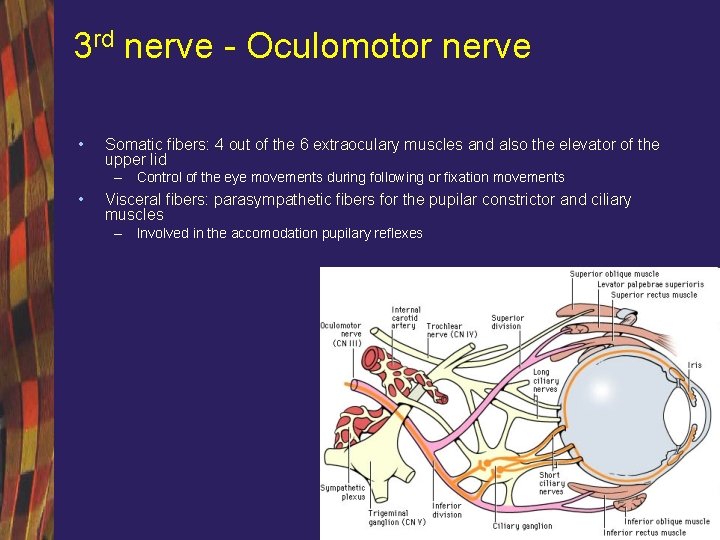
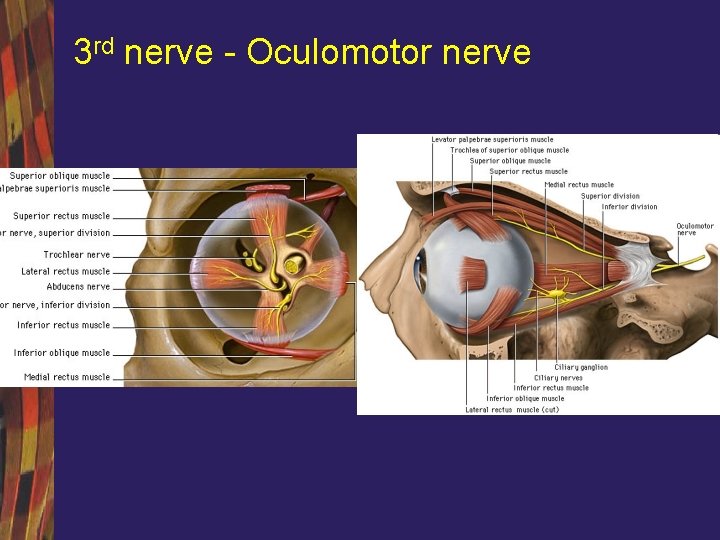
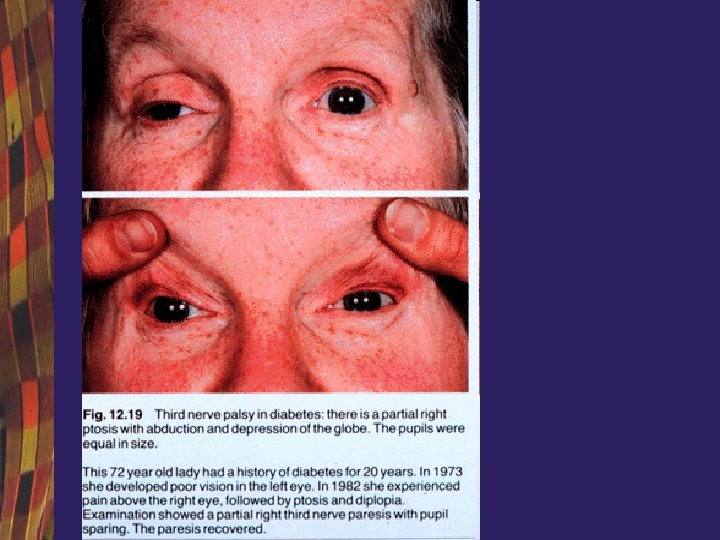
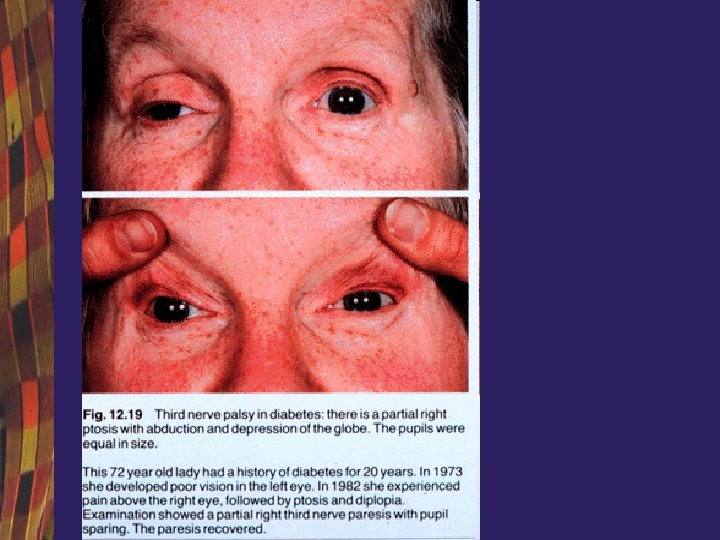
3 rd nerve - Oculomotor nerve • Somatic fibers: 4 out of the 6 extraoculary muscles and also the elevator of the upper lid – Control of the eye movements during following or fixation movements • Visceral fibers: parasympathetic fibers for the pupilar constrictor and ciliary muscles – Involved in the accomodation pupilary reflexes
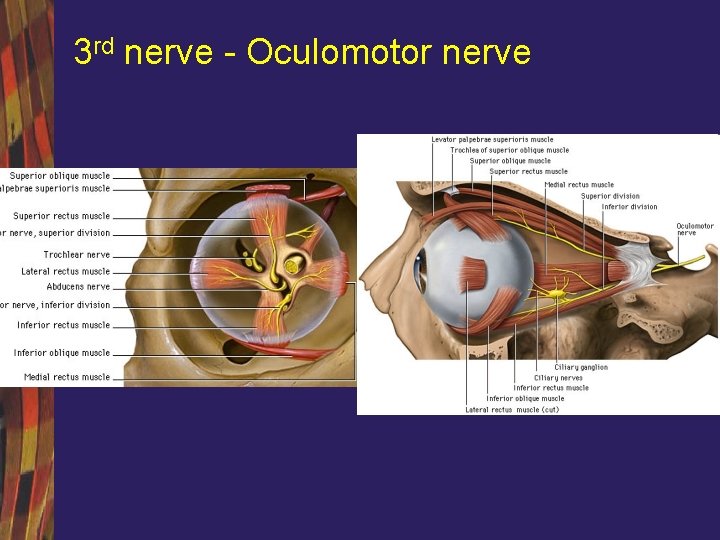
3 rd nerve - Oculomotor nerve
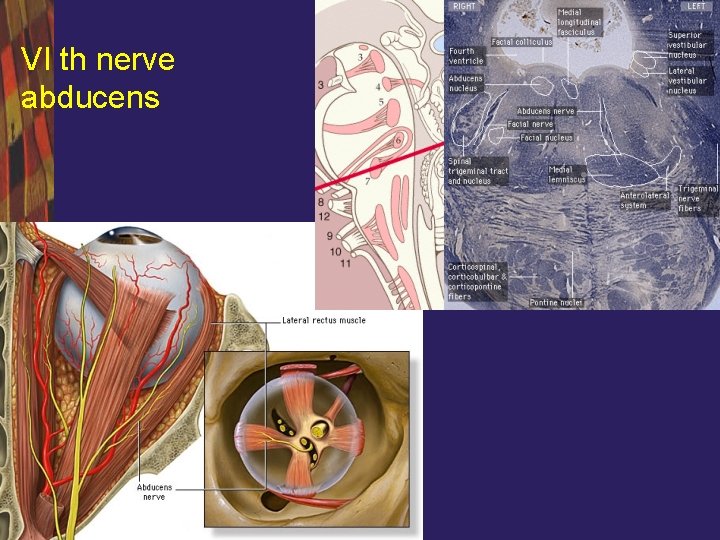
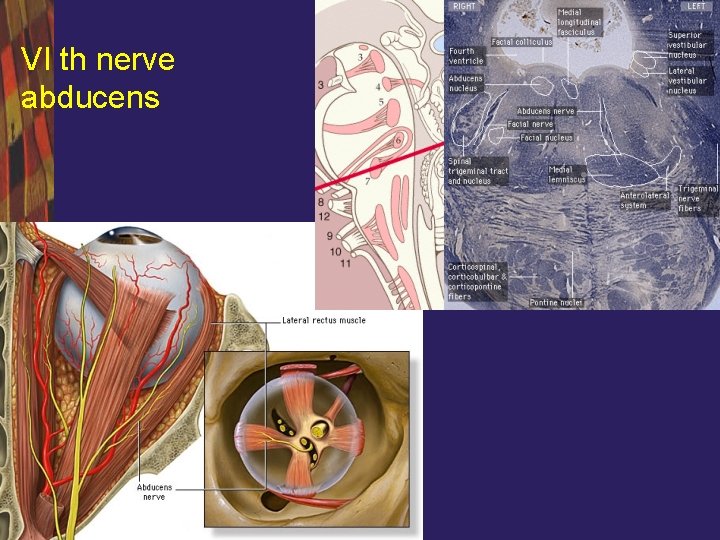
VI th nerve abducens
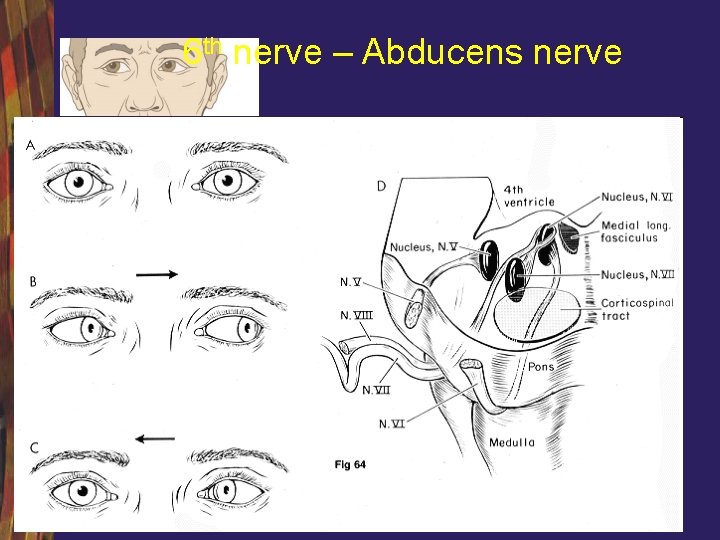
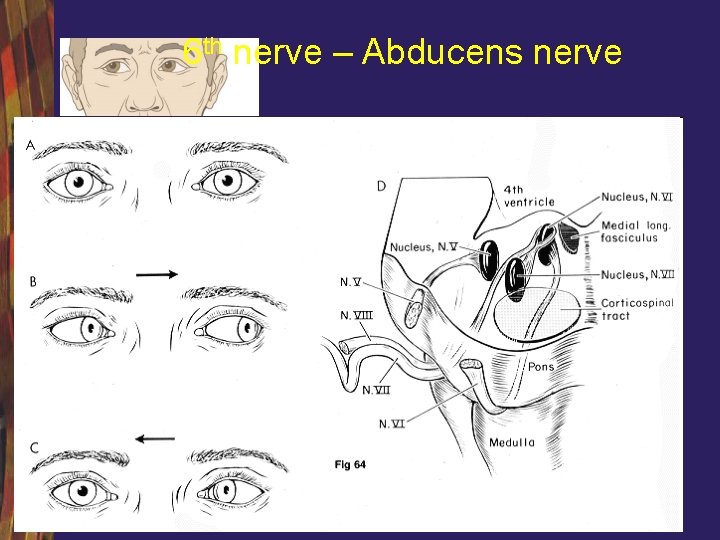
6 th nerve – Abducens nerve
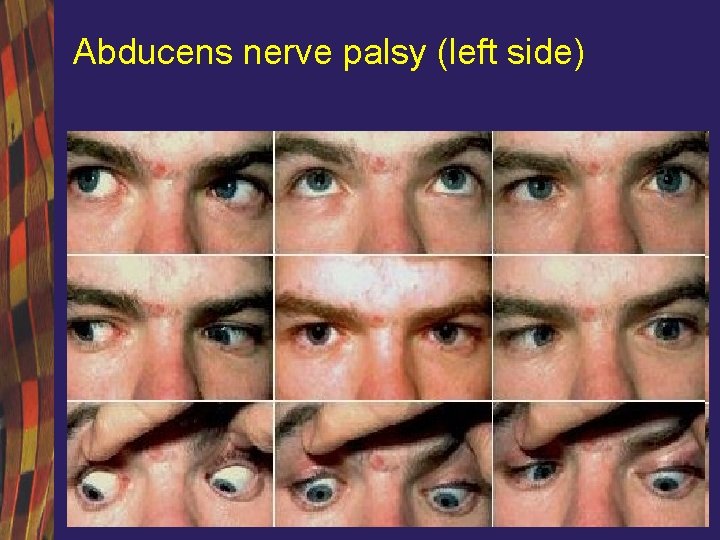
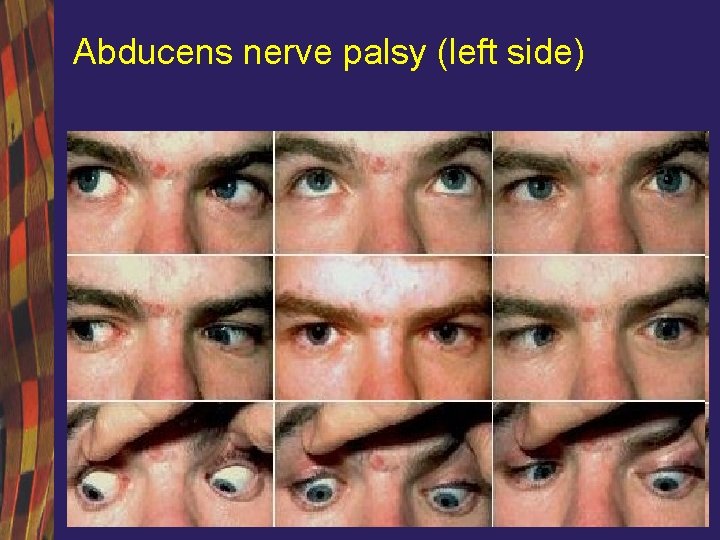
Abducens nerve palsy (left side)
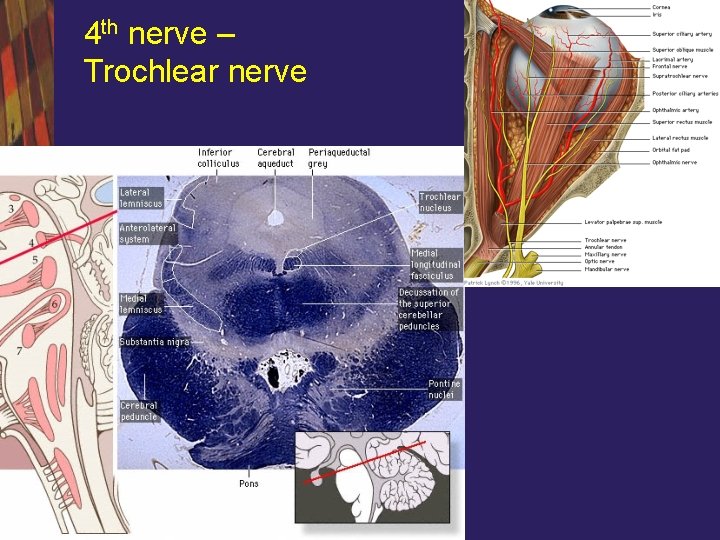
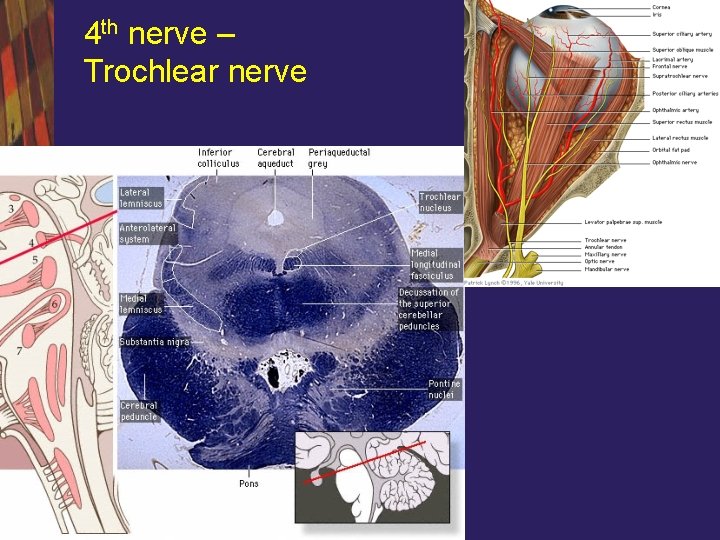
4 th nerve – Trochlear nerve
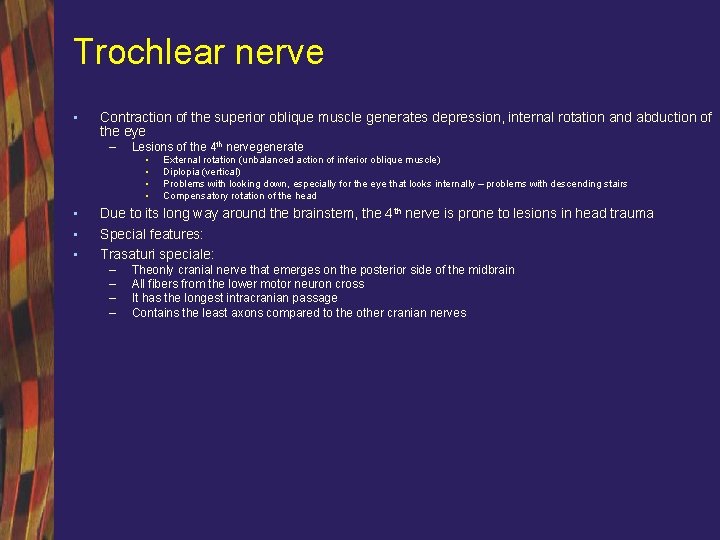
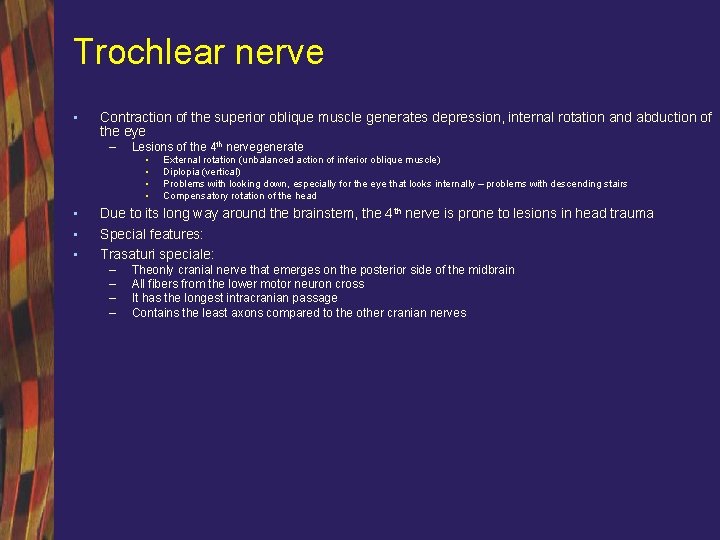
Trochlear nerve • Contraction of the superior oblique muscle generates depression, internal rotation and abduction of the eye – Lesions of the 4 th nervegenerate • • External rotation (unbalanced action of inferior oblique muscle) Diplopia (vertical) Problems with looking down, especially for the eye that looks internally – problems with descending stairs Compensatory rotation of the head Due to its long way around the brainstem, the 4 th nerve is prone to lesions in head trauma Special features: Trasaturi speciale: – – Theonly cranial nerve that emerges on the posterior side of the midbrain All fibers from the lower motor neuron cross It has the longest intracranian passage Contains the least axons compared to the other cranian nerves
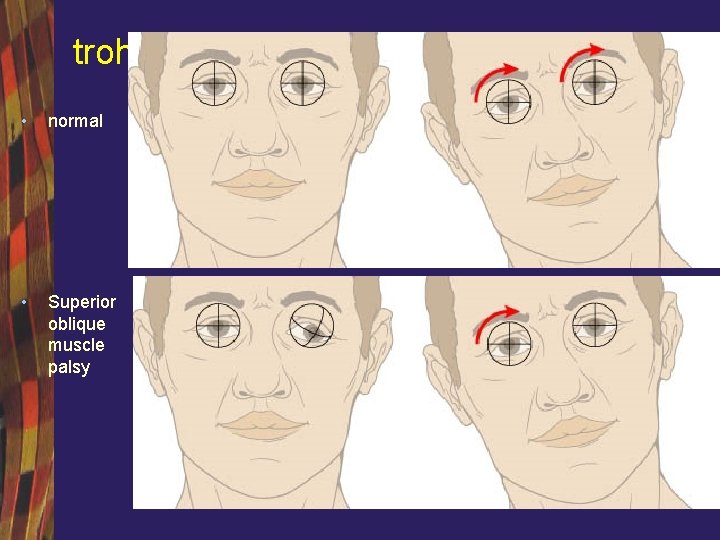
trohlear • normal • Superior oblique muscle palsy
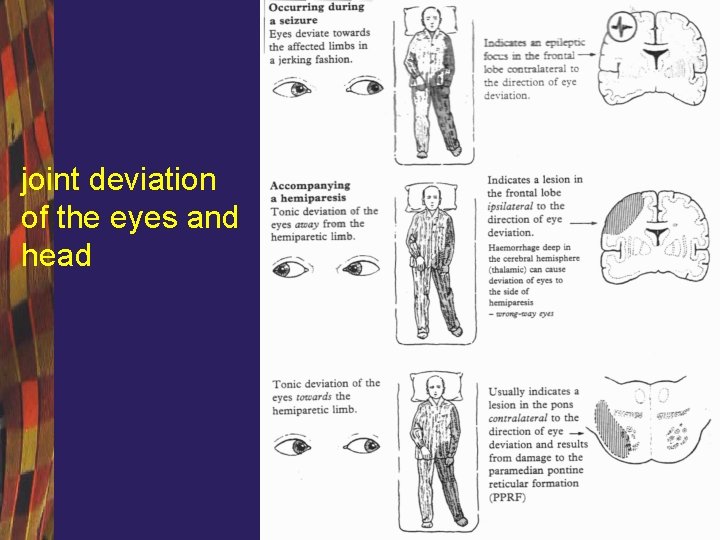
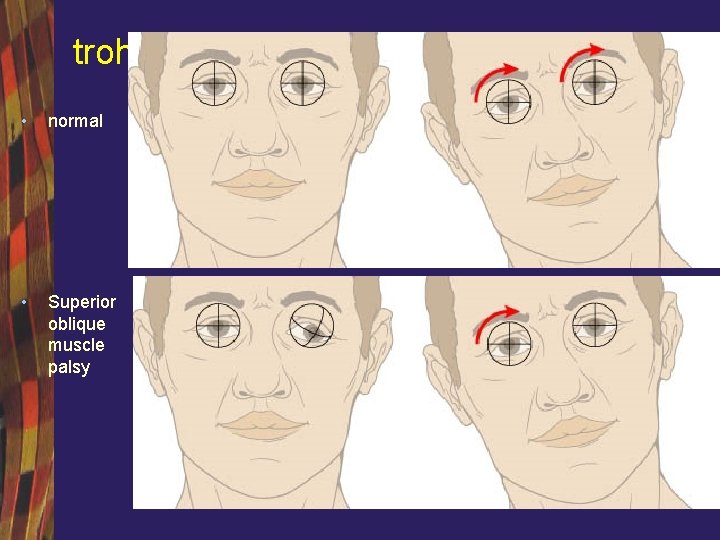
joint deviation of the eyes and head
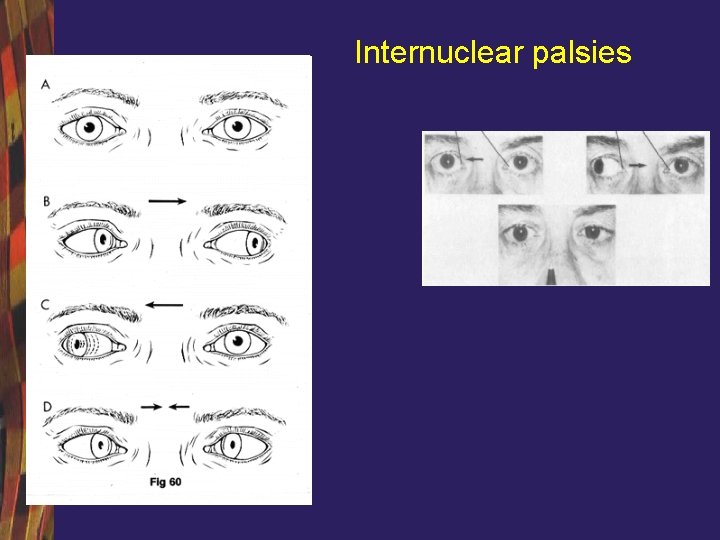
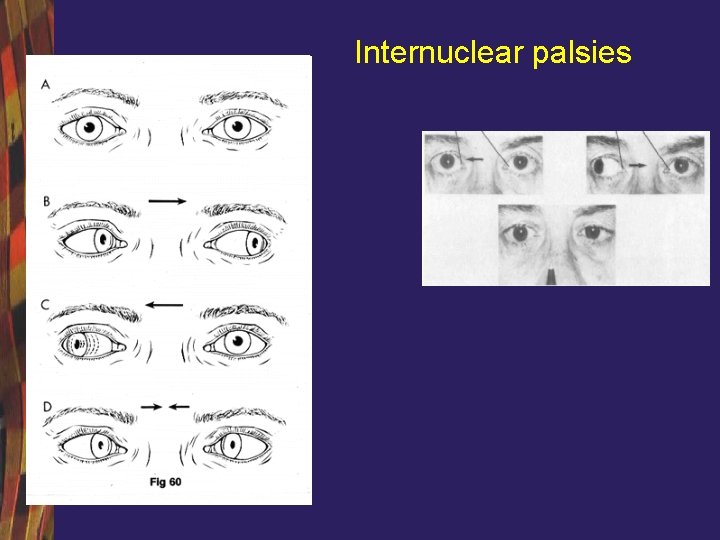
Internuclear palsies
Miasthenia gravis
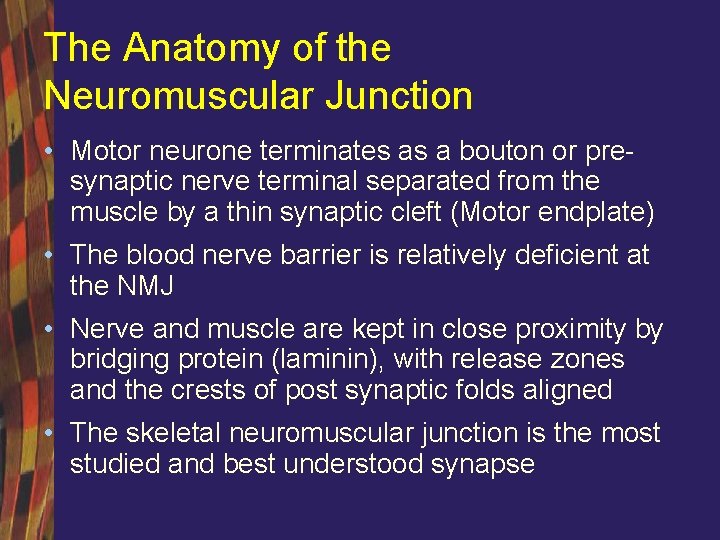
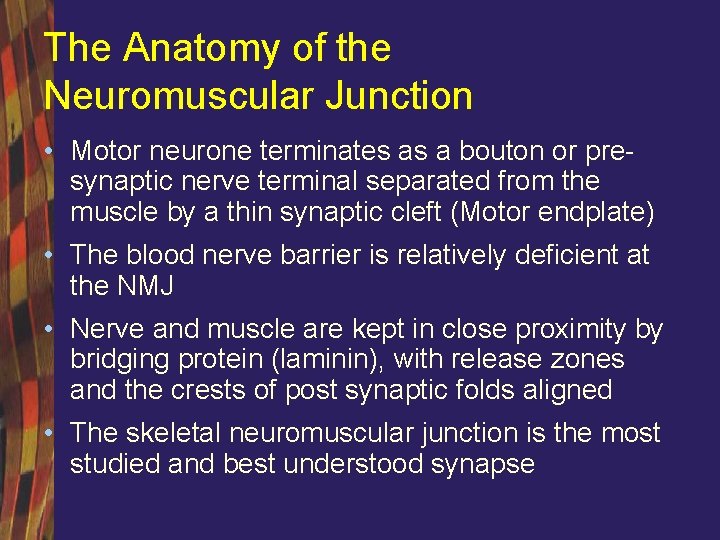
The Anatomy of the Neuromuscular Junction • Motor neurone terminates as a bouton or presynaptic nerve terminal separated from the muscle by a thin synaptic cleft (Motor endplate) • The blood nerve barrier is relatively deficient at the NMJ • Nerve and muscle are kept in close proximity by bridging protein (laminin), with release zones and the crests of post synaptic folds aligned • The skeletal neuromuscular junction is the most studied and best understood synapse
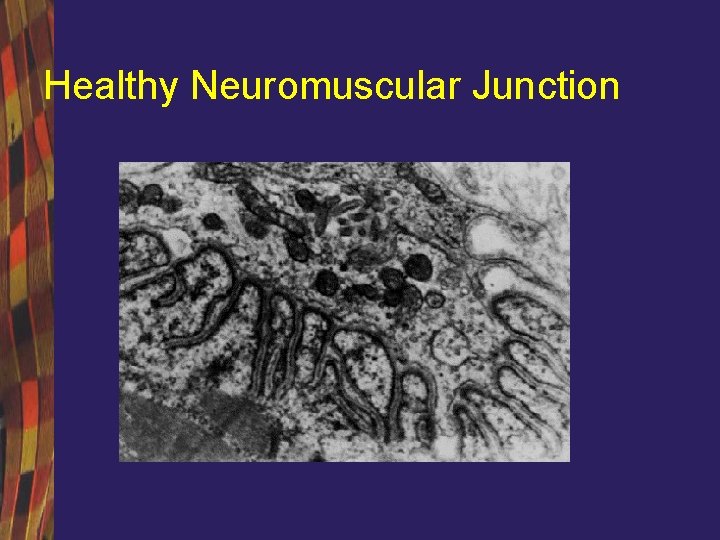
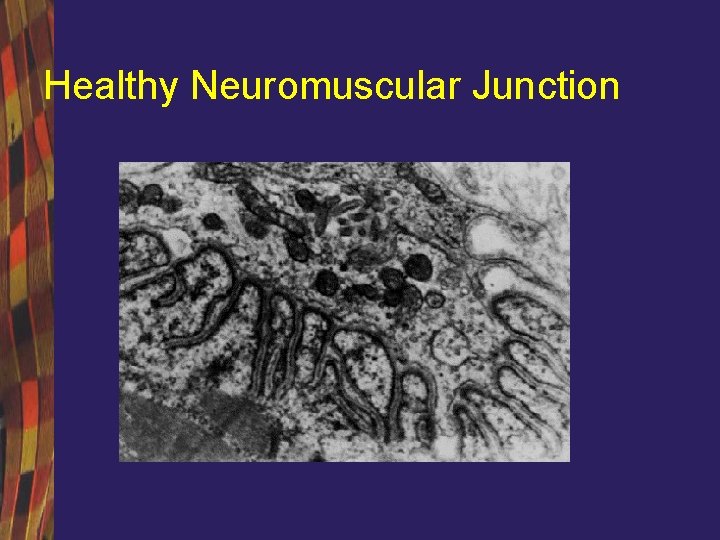
Healthy Neuromuscular Junction
The Physiology of Neuromuscular transmission • Neuronal Action potential invades the presynaptic nerve terminal • Depolarisation triggers opening of VGCCs • Calcium influx triggers quantal release of ACh • ACh binds to post synaptic n. ACh. Rs • Ca and Na ions influx through n. ACh. R triggering muscle membrane depolarisation via VGSCs. CMAP and muscle contraction
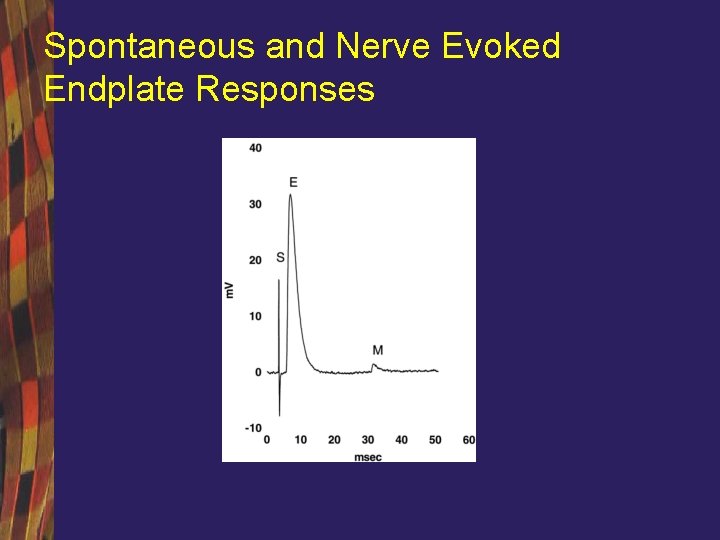
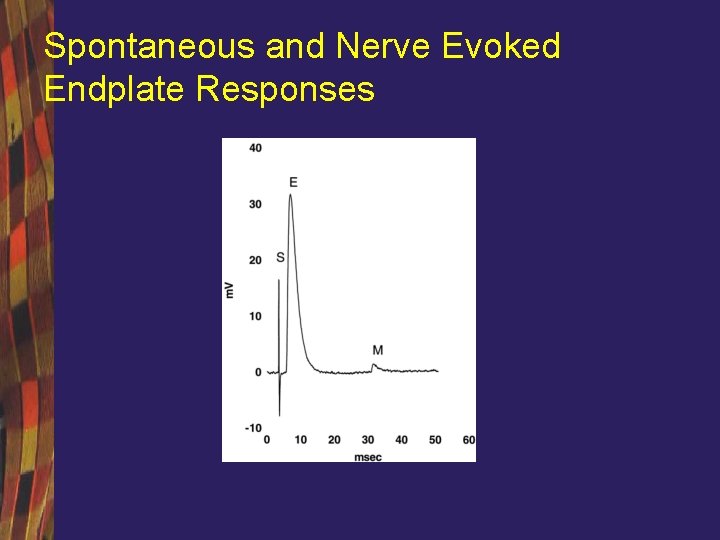
Spontaneous and Nerve Evoked Endplate Responses
Myasthenia Gravis (MG) • MG is the most common disorder of neuromuscular transmission • Incidence 2 -6 per 106 , prevalence 40 per 106 population • MG is an acquired autoimmune disease characterised by the formation of anti- n. ACh. R antibodies • MG is common in young women, and older men • MG is characterized by fluctuating and fatigable weakness • Weakness may be limited to a few muscles, such as the extraocular muscles, bulbar, limb or be generalised in fashion •
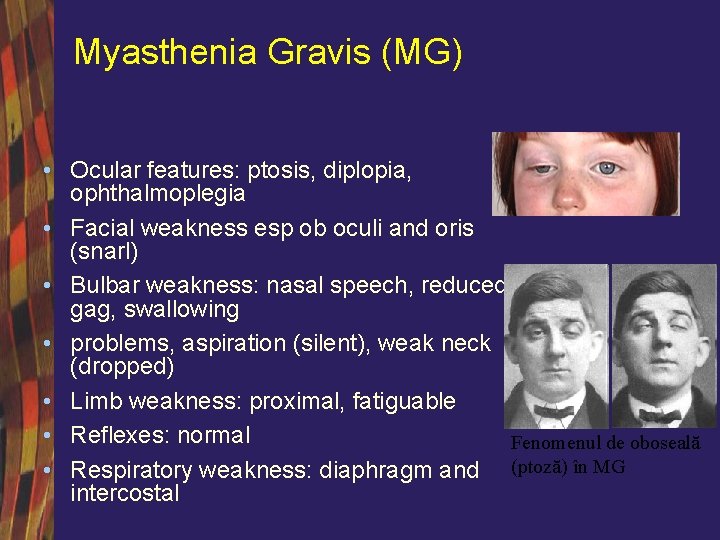
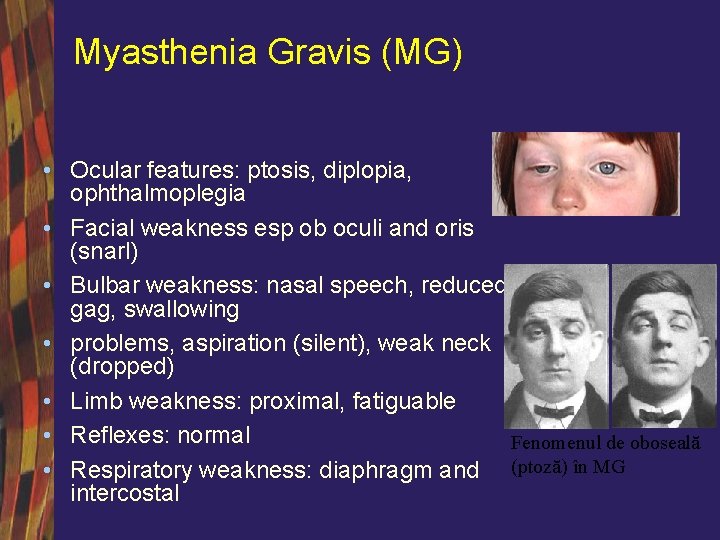
Myasthenia Gravis (MG) • Ocular features: ptosis, diplopia, ophthalmoplegia • Facial weakness esp ob oculi and oris (snarl) • Bulbar weakness: nasal speech, reduced gag, swallowing • problems, aspiration (silent), weak neck (dropped) • Limb weakness: proximal, fatiguable • Reflexes: normal Fenomenul de oboseală • Respiratory weakness: diaphragm and (ptoză) în MG intercostal
Myasthenia Gravis (MG) • MG is a defect of neuromuscular transmission with – reduced efficacy of Acetyl Choline at the post synaptic motor endplate due to pathogenic antibodies which • Block the n. ACh. R, • Down regulate the n. ACh. R • & cause complement dependent destruction of the motor endplate
Myasthenia Gravis (MG) • The immunopathogenesis of MG is unclear but involves • Genetic factors (HLA B 8) • Thymus – Vast majority of young onset cases are autoimmune and associated with thymic hyperplasia – Around 10% of patients with MG, often older patients) have an associated thymic tumour (oft striated muscle Abs) • Seronegative (10% gen, 50% OMG) • Neonatal MG
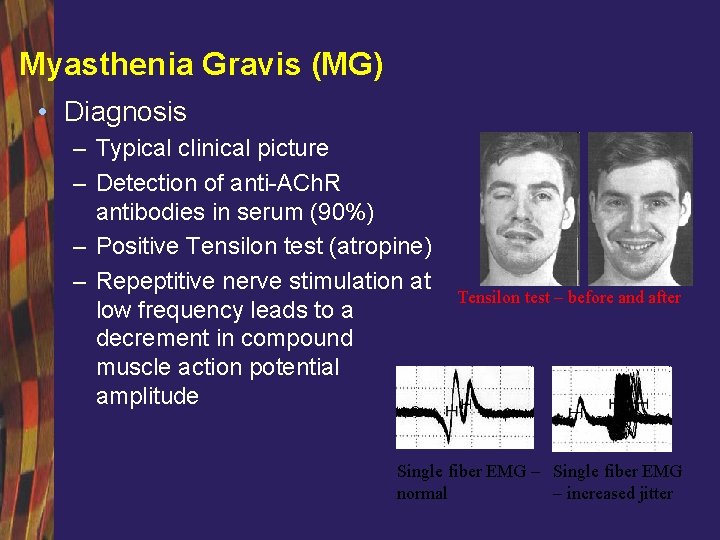
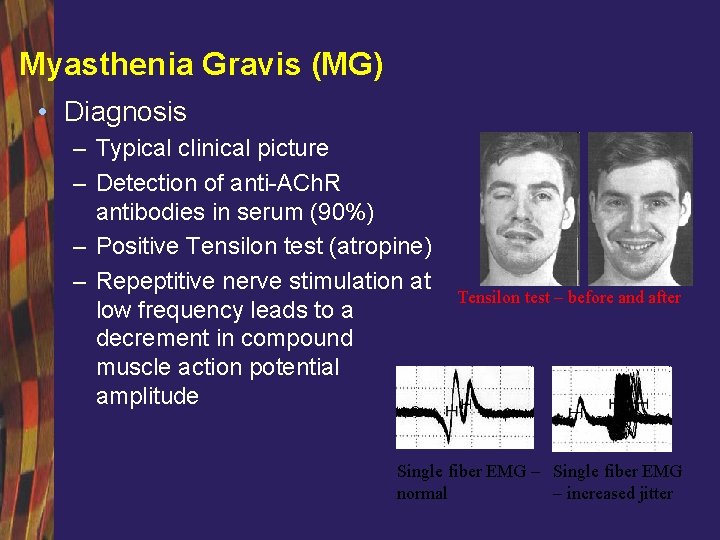
Myasthenia Gravis (MG) • Diagnosis – Typical clinical picture – Detection of anti-ACh. R antibodies in serum (90%) – Positive Tensilon test (atropine) – Repeptitive nerve stimulation at low frequency leads to a decrement in compound muscle action potential amplitude Tensilon test – before and after Single fiber EMG – Single fiber EMG normal – increased jitter
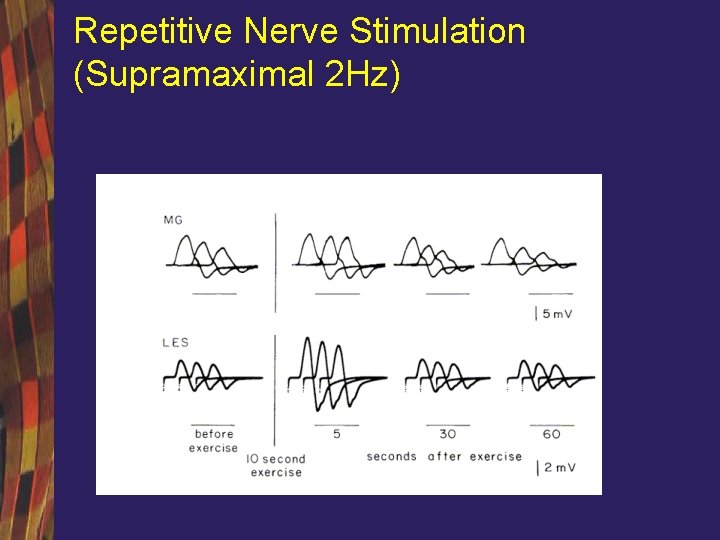
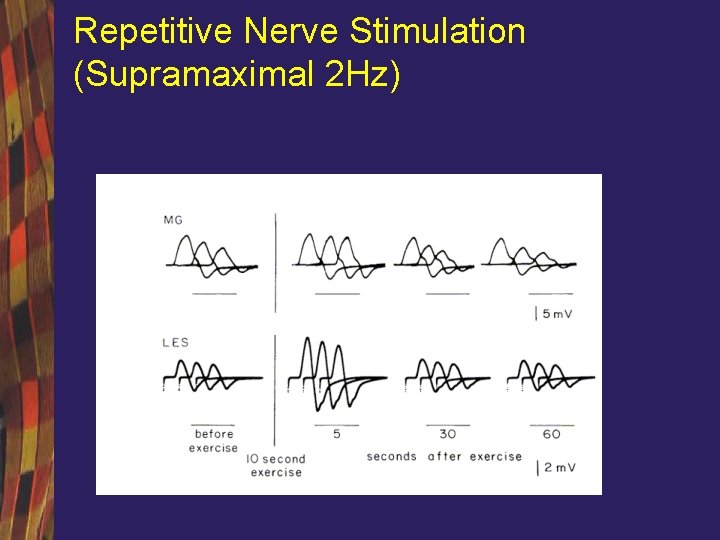
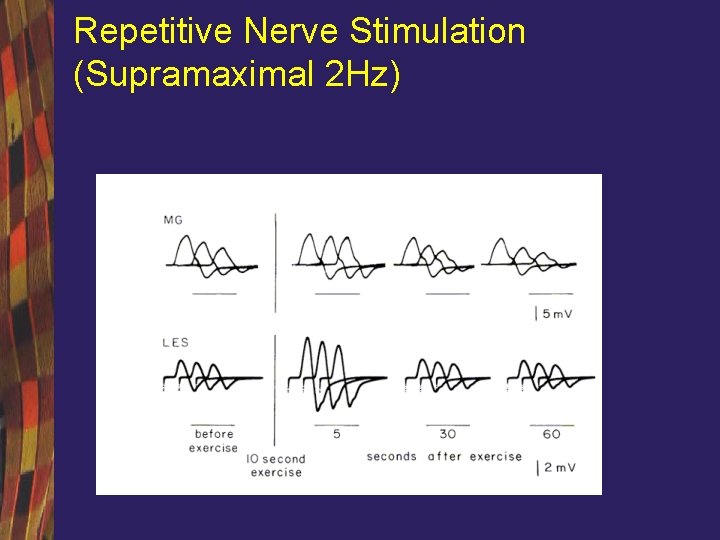
Repetitive Nerve Stimulation (Supramaximal 2 Hz)
Myasthenia Gravis (MG) • Treatment – Symptomatic (pyridostigmine oft with probatheline) – Thymectomy • Hyperplasia (trans-sternal approach), • Thymoma (locally invasive) – Immunotherapy • steroids, and other agents including Azathioprine • plasma exchange, • IVIG
Lambert Eaton Myasthenic syndrome (LEMS) • A defect of neuromuscular transmission with reduced quantal release of Acetyl Choline from the presynaptic nerve terminal • Pathogenic antibodies directed against voltage gated calcium channels (VGCCS) expressed at the NMJ and autonomic ganglia • 2/3 patients with LEMS have cancer, most commonly Small cell lung Ca (express VGCCs)
Lambert Eaton Myasthenic syndrome (LEMS) • Clinical features – – – Dry mouth Fatigable weakness of proximal muscles (like MG) Wasting of proximal muscles (X MG) Depressed reflexes (X MG) Ocular and bulbar weakness rare (X MG)
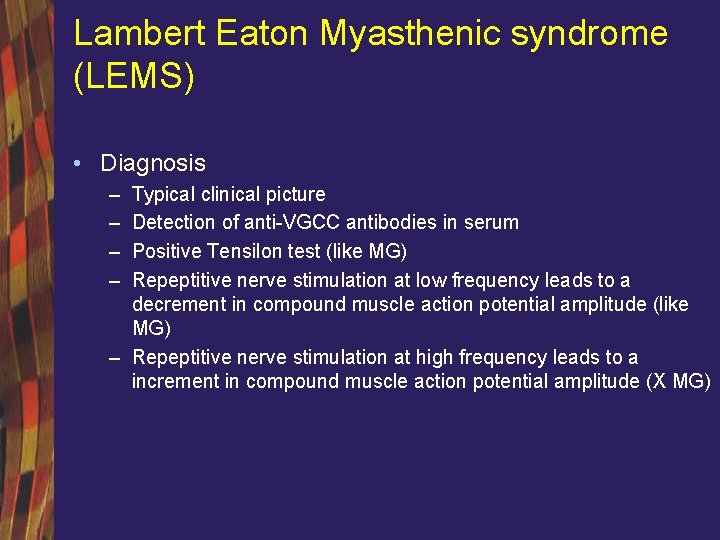
Lambert Eaton Myasthenic syndrome (LEMS) • Diagnosis – – Typical clinical picture Detection of anti-VGCC antibodies in serum Positive Tensilon test (like MG) Repeptitive nerve stimulation at low frequency leads to a decrement in compound muscle action potential amplitude (like MG) – Repeptitive nerve stimulation at high frequency leads to a increment in compound muscle action potential amplitude (X MG)
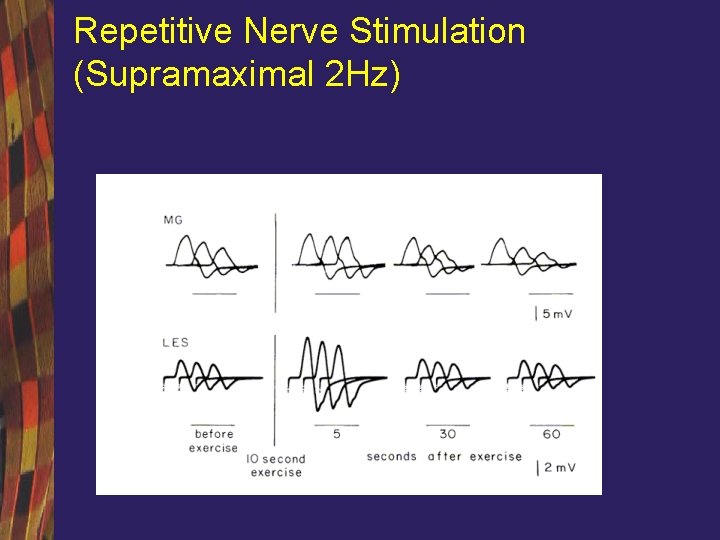
Repetitive Nerve Stimulation (Supramaximal 2 Hz)
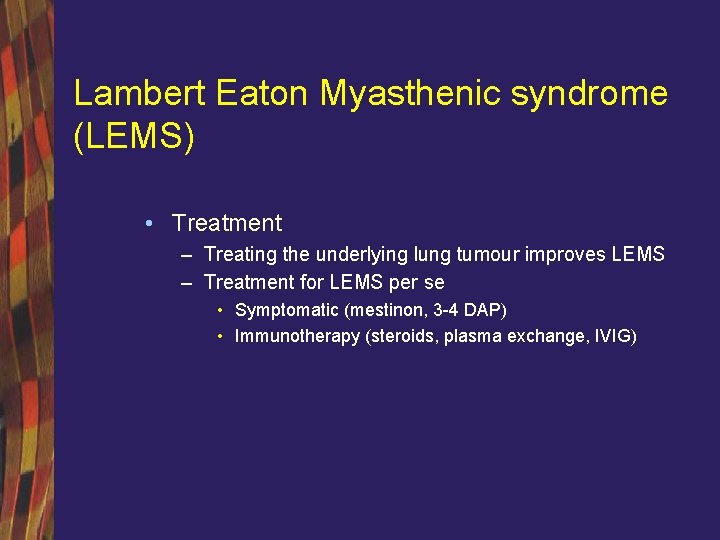
Lambert Eaton Myasthenic syndrome (LEMS) • Treatment – Treating the underlying lung tumour improves LEMS – Treatment for LEMS per se • Symptomatic (mestinon, 3 -4 DAP) • Immunotherapy (steroids, plasma exchange, IVIG)
POLYMYOSITIS DERMATOMYOSITIS
CLASSIFICATION OF POLYMYOSITIS - DERMATOMYOSITIS • Group I: Primary Idiopathic PM • Group II: Primary Idiopathic DM • Group III: DM or PM associated with neoplasia • Group IV: Childhood DM or PM associated with vasculitis • Group V: PM or DM with associated with collagen diseases
POLYMYOSITIS DERMATOMYOSITIS • Onset age: Usually > 20 years • Progression: weeks-months • Possibly preceded by upper tract infection • Other possible trigger factors: – – – Anti hepatitis B vaccination Growth hormone administration Drugs: penicilamine Viral infections: Coxsackie B; Parvovirus; Echovirus HLA • Class II: antigens DQα 1*0501 (88%) • For DM: DMA*0103 si DMB*0102
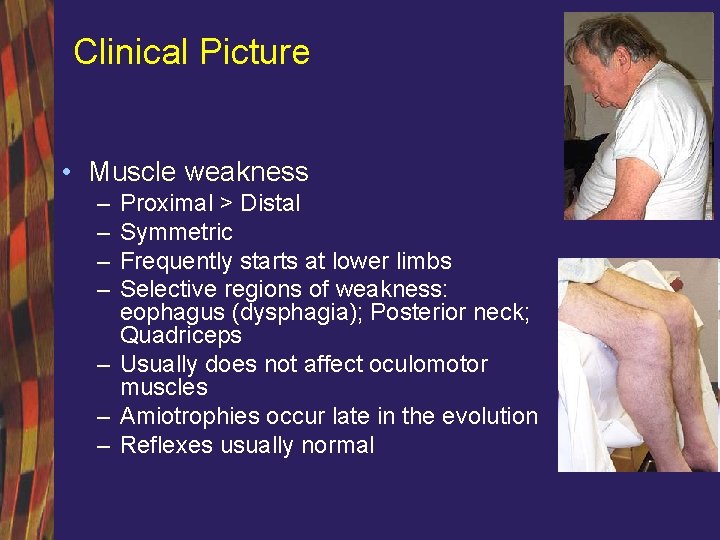
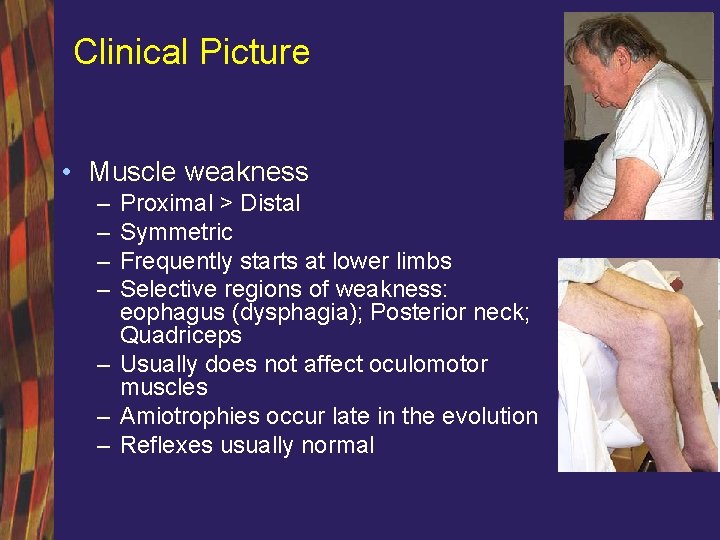
Clinical Picture • Muscle weakness – – Proximal > Distal Symmetric Frequently starts at lower limbs Selective regions of weakness: eophagus (dysphagia); Posterior neck; Quadriceps – Usually does not affect oculomotor muscles – Amiotrophies occur late in the evolution – Reflexes usually normal
Motor deficit • • Proximal: most frequently in PM and DM Distal: inclusion body myositis Lack of simmetry: inclusion body myositis cvadriceps: inclusion body myositis; PM with mitochondrial diseases Extraocular muscles: extraoculary myositis Swallowing : inclusion myositis, granulomatous myositis, scleroderma associated myositis Episodic: episodic miopathy with pipestem capilaries Acute: infectious;
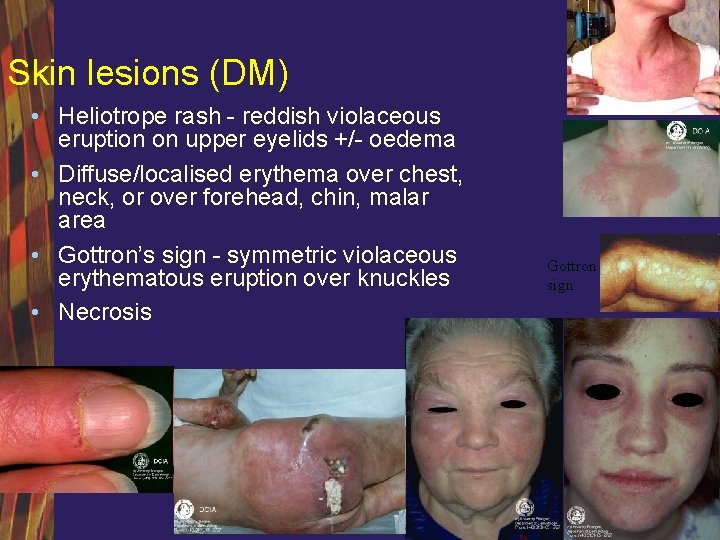
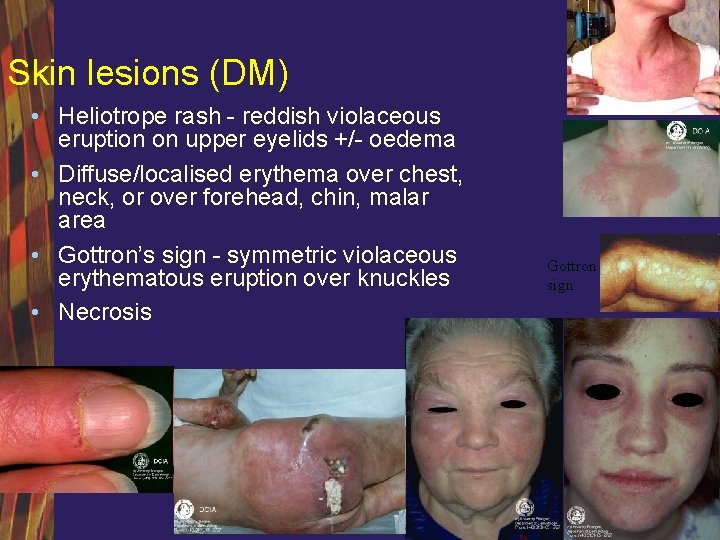
Skin lesions (DM) • Heliotrope rash - reddish violaceous eruption on upper eyelids +/- oedema • Diffuse/localised erythema over chest, neck, or over forehead, chin, malar area • Gottron’s sign - symmetric violaceous erythematous eruption over knuckles • Necrosis Gottron sign

Pain • Pain – 30%; Especially with associated connective tissue disease – Rule out: Polymyalgia; Arthritis; Fasciitis; Rhabdomyolysis • Muscle pain – Associated with contraction, muscle mass compression or spontaneous pain • Joint pain – Arthrites or nondestructive arthralgia – Anti-Jo 1 or Anti. ARNt synthethasys antibody syndromes
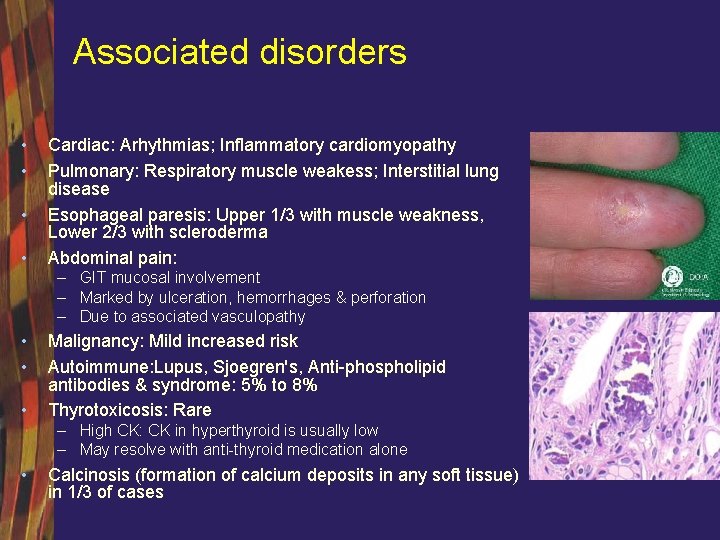
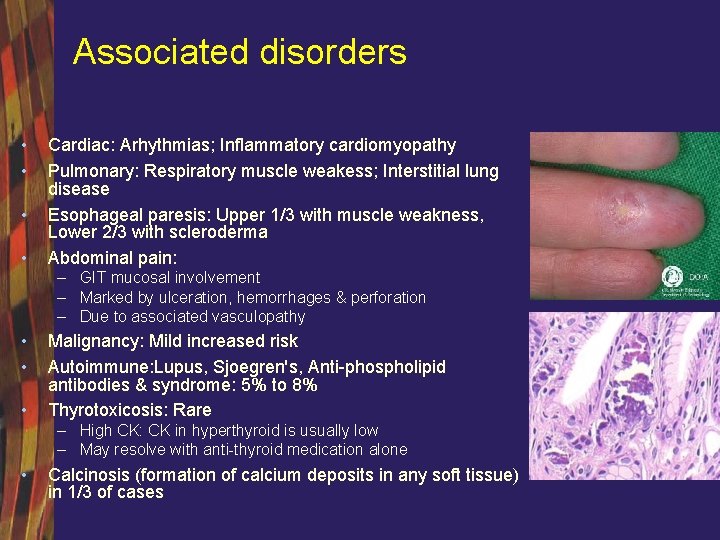
Associated disorders • • Cardiac: Arhythmias; Inflammatory cardiomyopathy Pulmonary: Respiratory muscle weakess; Interstitial lung disease Esophageal paresis: Upper 1/3 with muscle weakness, Lower 2/3 with scleroderma Abdominal pain: – GIT mucosal involvement – Marked by ulceration, hemorrhages & perforation – Due to associated vasculopathy • • • Malignancy: Mild increased risk Autoimmune: Lupus, Sjoegren's, Anti-phospholipid antibodies & syndrome: 5% to 8% Thyrotoxicosis: Rare – High CK: CK in hyperthyroid is usually low – May resolve with anti-thyroid medication alone • Calcinosis (formation of calcium deposits in any soft tissue) in 1/3 of cases
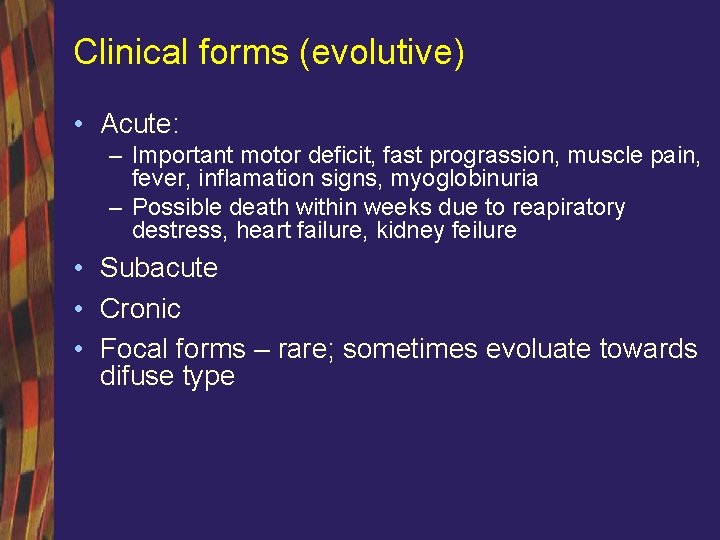
Clinical forms (evolutive) • Acute: – Important motor deficit, fast prograssion, muscle pain, fever, inflamation signs, myoglobinuria – Possible death within weeks due to reapiratory destress, heart failure, kidney feilure • Subacute • Cronic • Focal forms – rare; sometimes evoluate towards difuse type
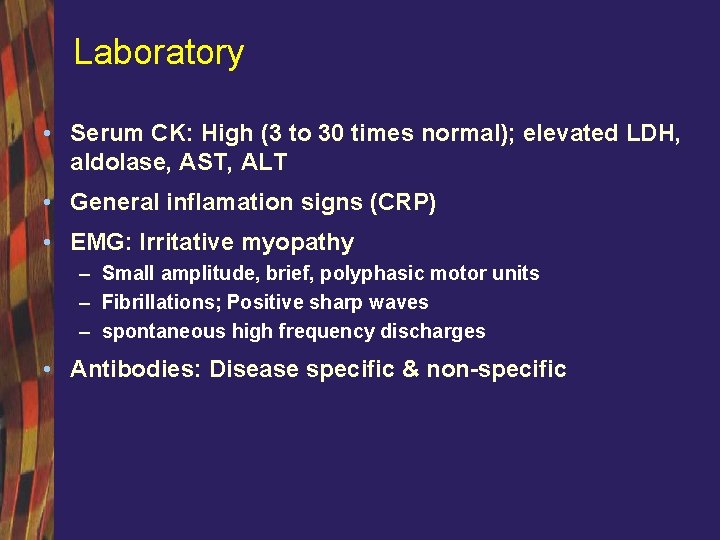
Laboratory • Serum CK: High (3 to 30 times normal); elevated LDH, aldolase, AST, ALT • General inflamation signs (CRP) • EMG: Irritative myopathy – Small amplitude, brief, polyphasic motor units – Fibrillations; Positive sharp waves – spontaneous high frequency discharges • Antibodies: Disease specific & non-specific
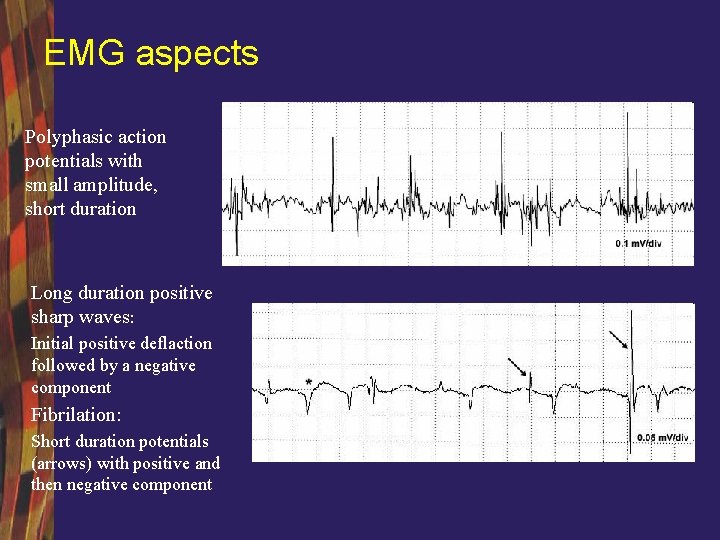
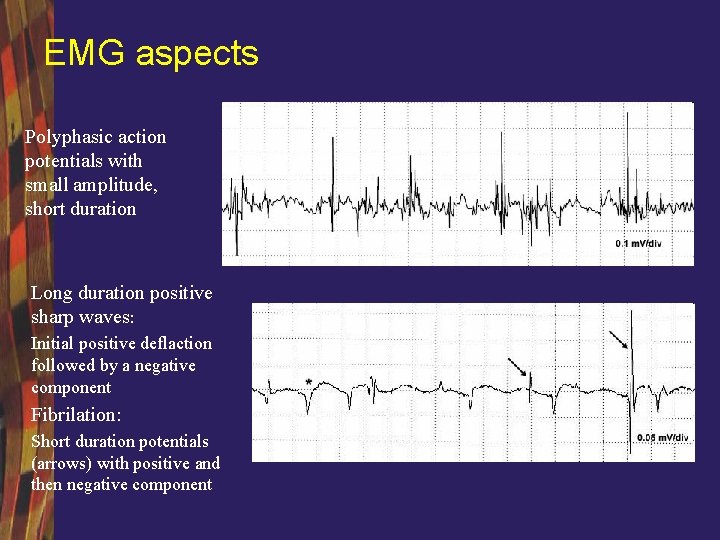
EMG aspects Polyphasic action potentials with small amplitude, short duration Long duration positive sharp waves: Initial positive deflaction followed by a negative component Fibrilation: Short duration potentials (arrows) with positive and then negative component
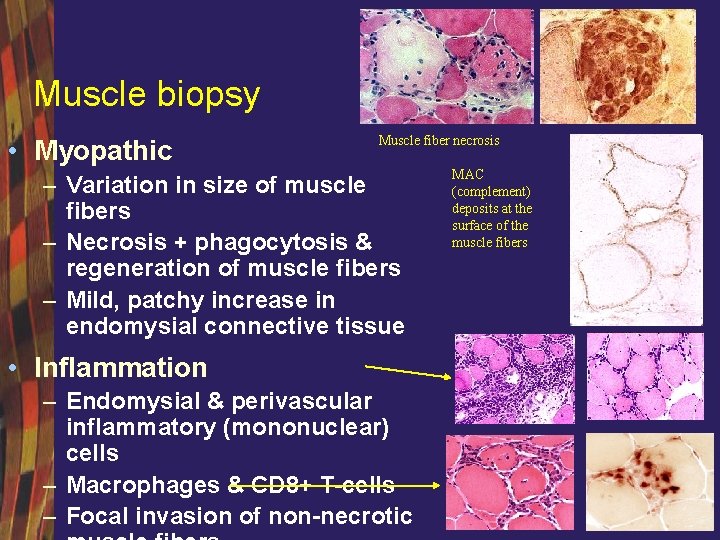
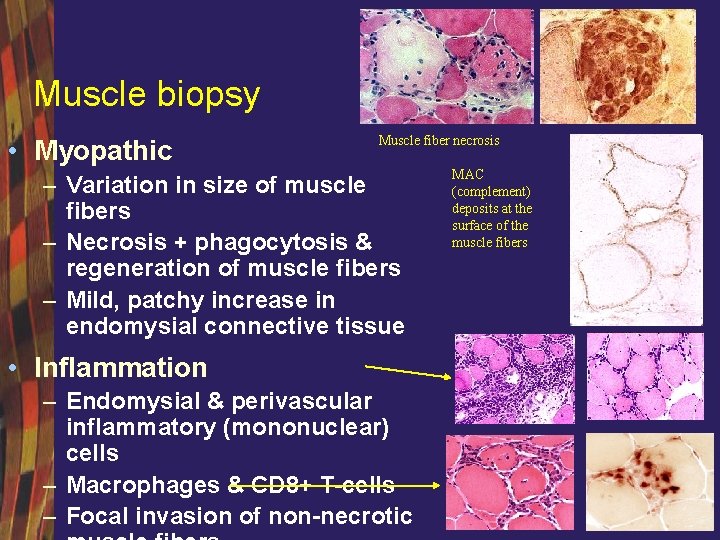
Muscle biopsy • Myopathic Muscle fiber necrosis – Variation in size of muscle fibers – Necrosis + phagocytosis & regeneration of muscle fibers – Mild, patchy increase in endomysial connective tissue • Inflammation – Endomysial & perivascular inflammatory (mononuclear) cells – Macrophages & CD 8+ T-cells – Focal invasion of non-necrotic MAC (complement) deposits at the surface of the muscle fibers
Differential diagnosis • Myasthenia Gravis • Electrolyte disturbances • Metabolic, endocrine or toxic myopathies • Muscular dystrophy • Guillain-Barre Syndrome
Tratament • Corticosteroids – Good response to treatment if: • Clinical picture: proximal or diffuse motor deficit, disease duration <1 year; association with mialgia, cutaneous rash, connective tissue diseases • Lab: very high serum CPK, anti Jo-1 antibodies • Biopsy: perimisial inflammation, perifascicular atrophy, necrosis and regeneration – Poor response to therapy if: • Focal or asymetric motor deficit; acute or very slow form of evolution; family history • Lab: normal or low seric CK • Biopsy: focal invasion of muscle fibers by inflammatory cells; • Prednisone 1 -2 mg/kg/day, tapered after strength improves and CK declines, often after 1 -3 months.
TREATMENT • Cytotoxic agents – introduced if severe disease, relapsing disease, inadequate steroid response or steroid induced cx’s. – AZA or methotrexate used with steroids – Cyclosporin, cyclophosphamide, tacrolimus and anti. TNF are alternatives. • Intravenous immunoglobulin successful – Child DM, esophageal dysfunction – 1 gram/kg/day
Secondary myositis • Malignancy – lung cancer, gastric, prostate, mamary, ovary – Surgical intervention does not always lead to a favourable evolution • Drug induced: D-penicilamine; Procainamide, Hidralazine (Lupus ± miozitis); Interferon-α; Fenitoin (inflamatory myopaty with fever, rash, limphadenopaty and eosinophyilia); – Possibly related with myositis: Peniciline; Ypeca; Sulfonamide; Levodopa; Cimetidine; Leuprolide; Propilthiouracil; Carbimazole • Graft versus host reaction