Cranial Nerves I Cranial Nerves 12 pairs two
- Slides: 64
Cranial Nerves I
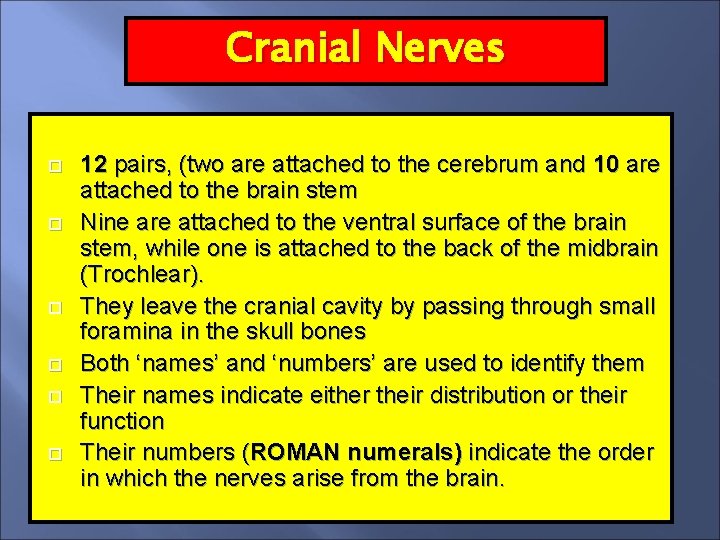
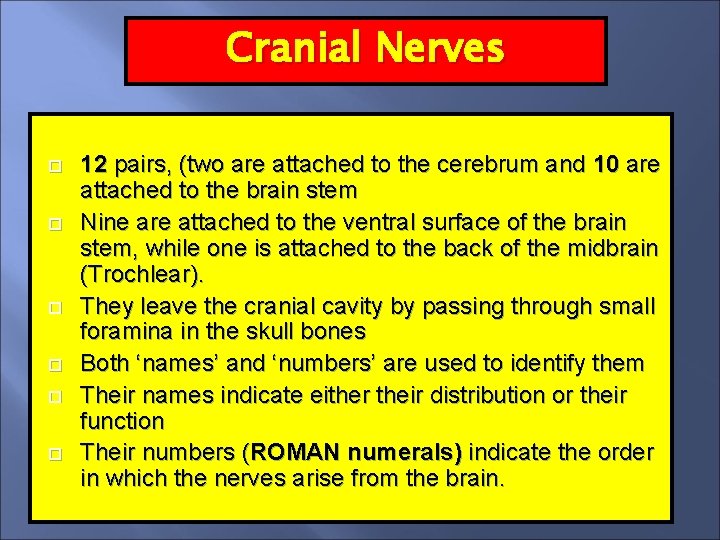
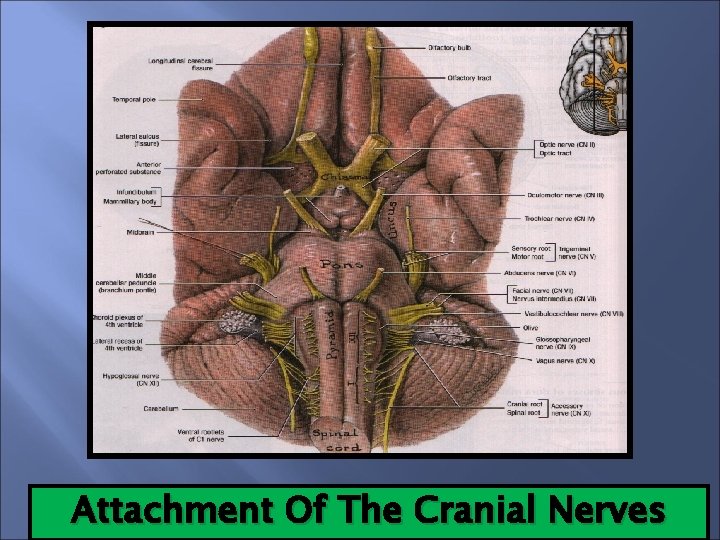
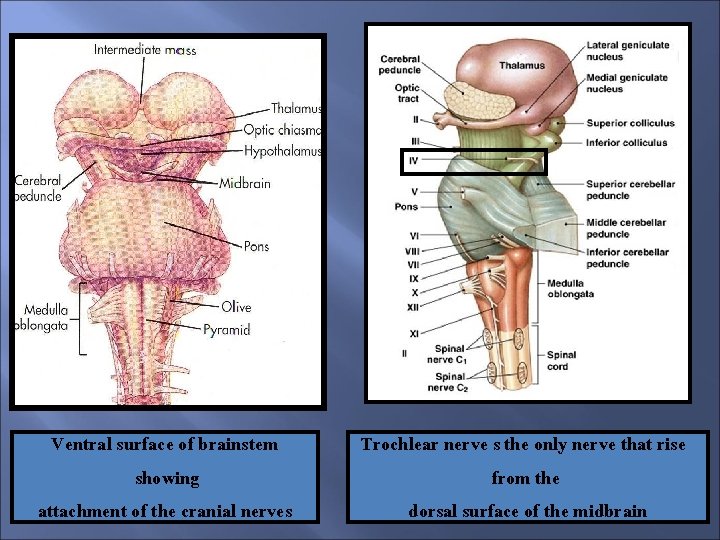
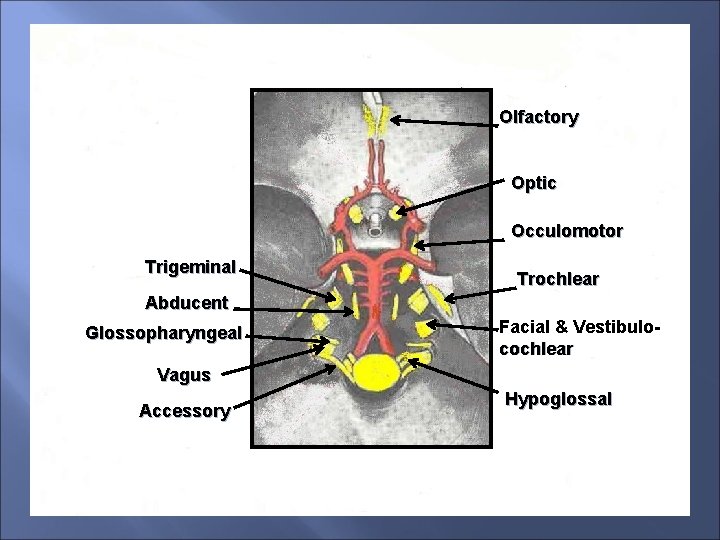
Cranial Nerves 12 pairs, (two are attached to the cerebrum and 10 are attached to the brain stem Nine are attached to the ventral surface of the brain stem, while one is attached to the back of the midbrain (Trochlear). They leave the cranial cavity by passing through small foramina in the skull bones Both ‘names’ and ‘numbers’ are used to identify them Their names indicate either their distribution or their function Their numbers (ROMAN numerals) indicate the order in which the nerves arise from the brain.
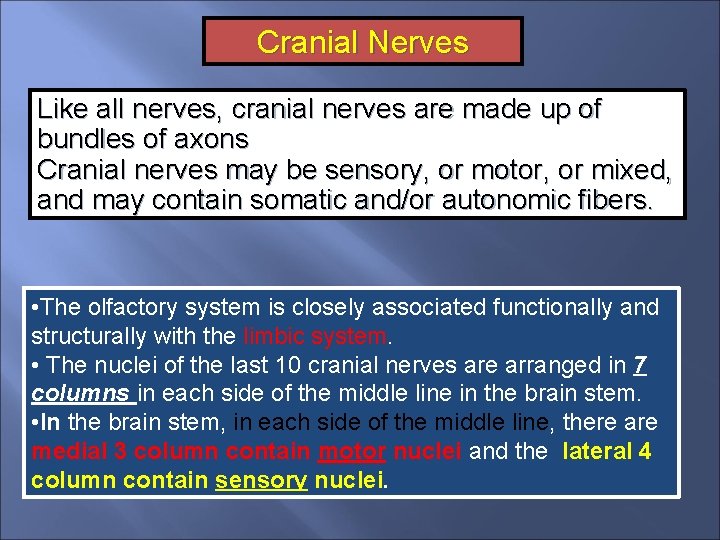
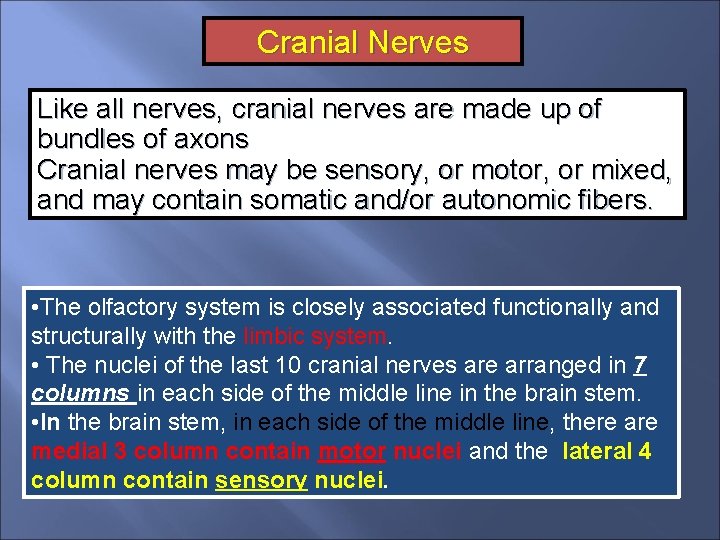
Cranial Nerves Like all nerves, cranial nerves are made up of bundles of axons Cranial nerves may be sensory, or motor, or mixed, and may contain somatic and/or autonomic fibers. • The olfactory system is closely associated functionally and structurally with the limbic system. • The nuclei of the last 10 cranial nerves are arranged in 7 columns in each side of the middle line in the brain stem. • In the brain stem, in each side of the middle line, there are medial 3 column contain motor nuclei and the lateral 4 column contain sensory nuclei.
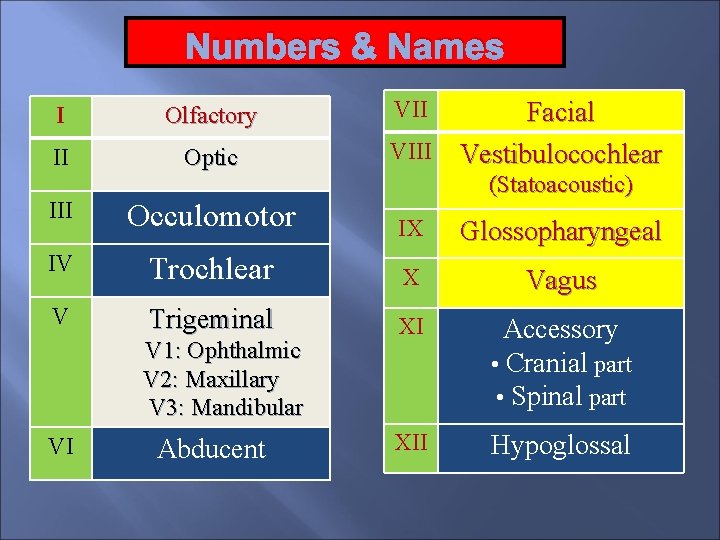
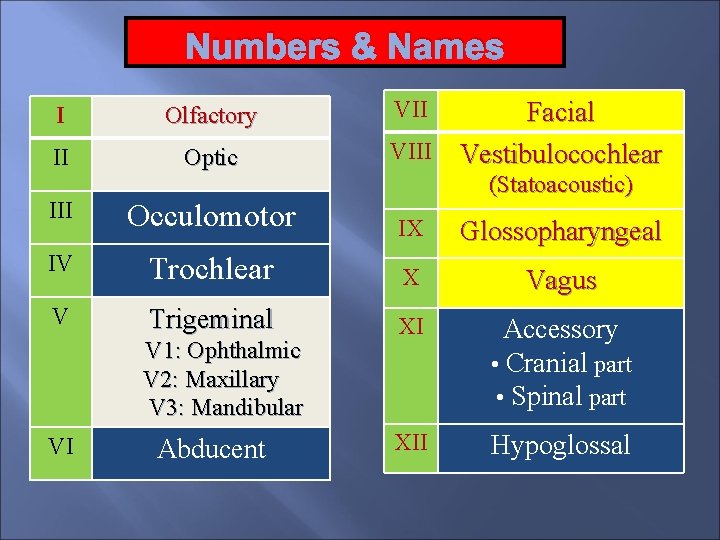
Numbers & Names I Olfactory II Optic VII Facial VIII Vestibulocochlear (Statoacoustic) III Occulomotor IX Glossopharyngeal IV Trochlear X Vagus V Trigeminal XI Accessory • Cranial part • Spinal part XII Hypoglossal V 1: Ophthalmic V 2: Maxillary V 3: Mandibular VI Abducent
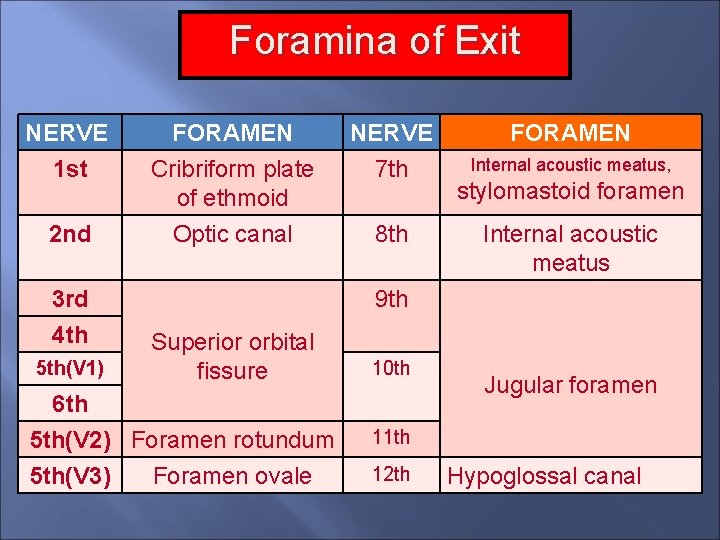
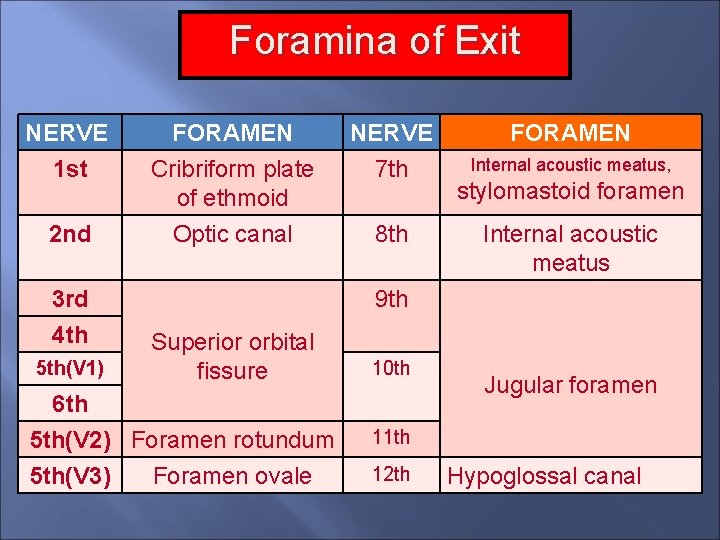
Foramina of Exit NERVE 1 st FORAMEN Cribriform plate of ethmoid NERVE 7 th 2 nd Optic canal 8 th 3 rd 4 th 5 th(V 1) FORAMEN Internal acoustic meatus, stylomastoid foramen Internal acoustic meatus 9 th Superior orbital fissure 10 th 6 th 5 th(V 2) Foramen rotundum 11 th 5 th(V 3) 12 th Foramen ovale Jugular foramen Hypoglossal canal
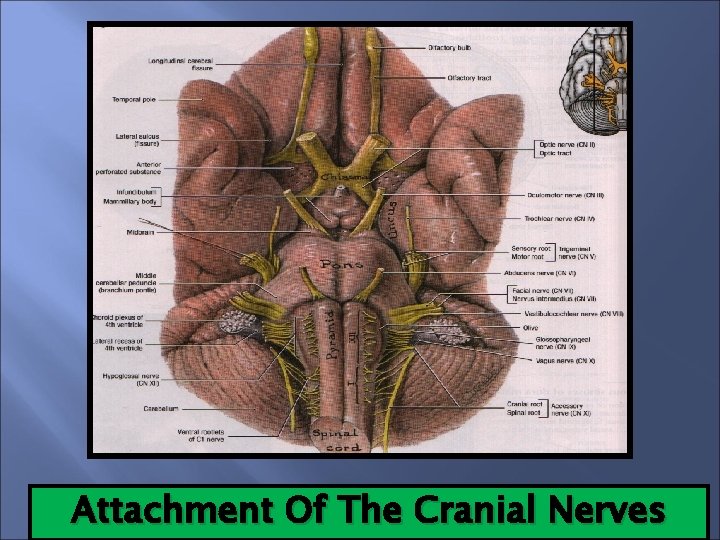
Attachment Of The Cranial Nerves
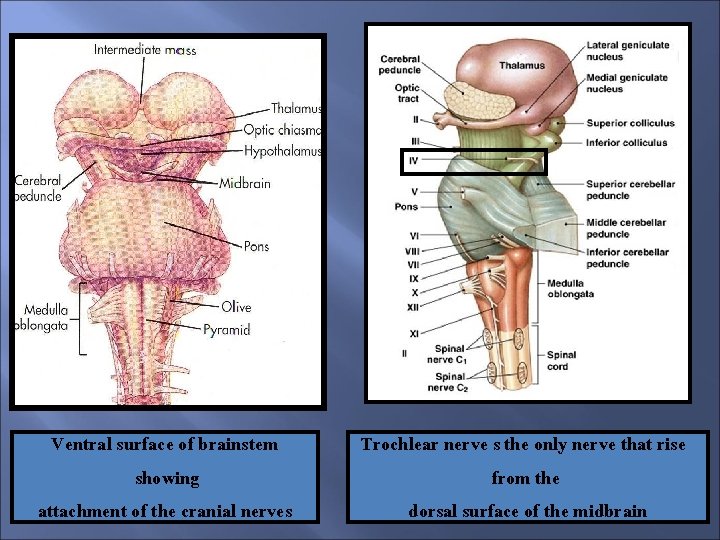
Ventral surface of brainstem showing attachment of the cranial nerves Trochlear nerve s the only nerve that rise from the dorsal surface of the midbrain
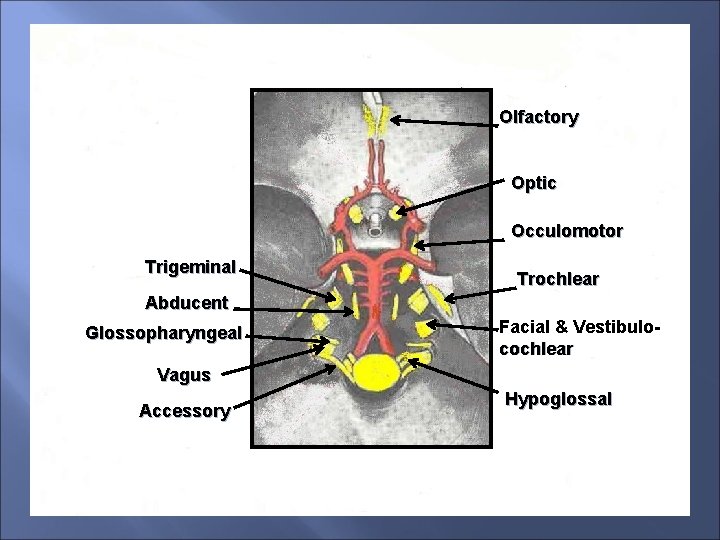
Olfactory Optic Occulomotor Trigeminal Trochlear Abducent Glossopharyngeal Facial & Vestibulocochlear Vagus Accessory Hypoglossal
Functional Components of The Spinal Nerves General Somatic Afferent (GSA): Carries information from skin, muscles, ligament and joints General Somatic Efferent (GSE): Activate skeletal muscles General Visceral Afferent (GVA): Carries sensory information from visceral organs General Visceral Efferent (GVE): Activate visceral (smooth) muscles and glands All the spinal nerves carry all the four components
Spinal Nerves Functional Components General somatic afferent (GSA) General somatic efferent (GSE) General visceral afferent (GVA) General visceral efferent (GVE) NB. All the spinal nerves carry all the four components
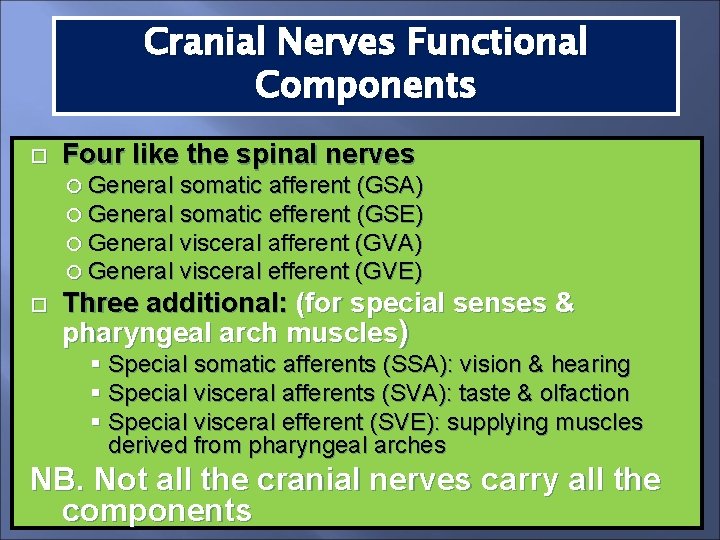
Functional Components of The Cranial Nerves Four like the spinal nerves (GSA, GSE, GVA, GVE) Three additional: 1 -Special Somatic Afferents (SSA): Mediate special sensations of vision and hearing & equilibrium (2&8) 2 -Special Visceral Afferents (SVA): Mediate visceral sensation of taste & olfaction 3 - Special Visceral Efferent (SVE): Activate muscles of face, palate, mouth, pharynx and larynx (derivatives of branchial arches) Not all the cranial nerves carry all the components
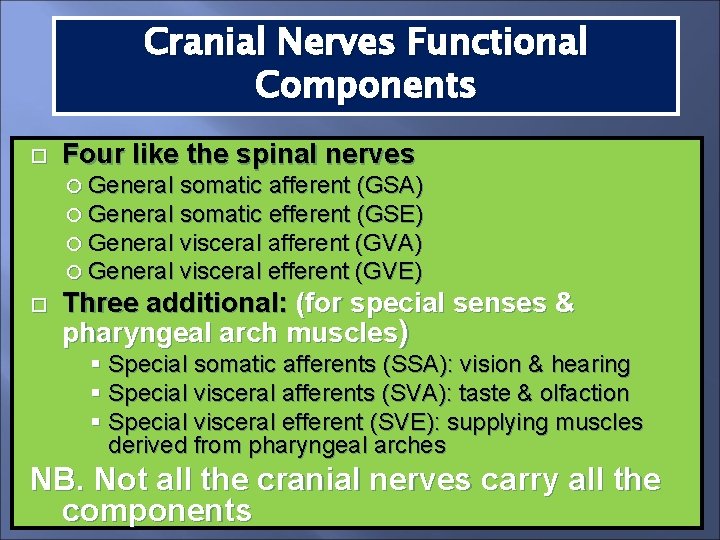
Cranial Nerves Functional Components Four like the spinal nerves General somatic afferent (GSA) General somatic efferent (GSE) General visceral afferent (GVA) General visceral efferent (GVE) Three additional: (for special senses & pharyngeal arch muscles) § Special somatic afferents (SSA): vision & hearing § Special visceral afferents (SVA): taste & olfaction § Special visceral efferent (SVE): supplying muscles derived from pharyngeal arches NB. Not all the cranial nerves carry all the components
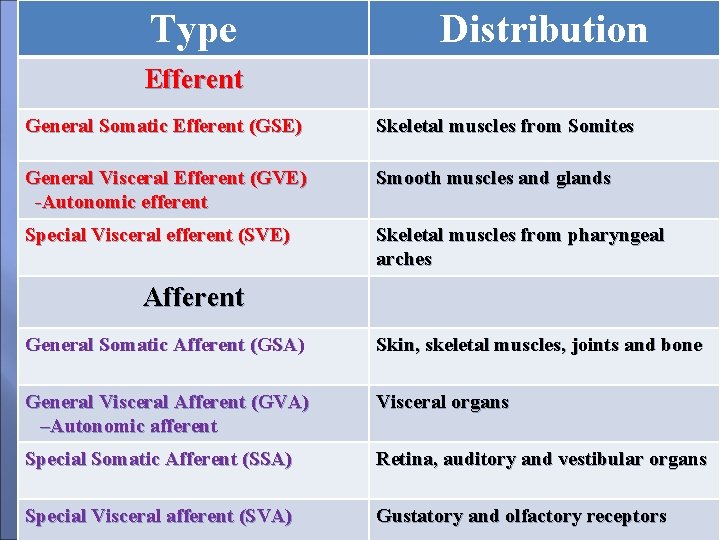
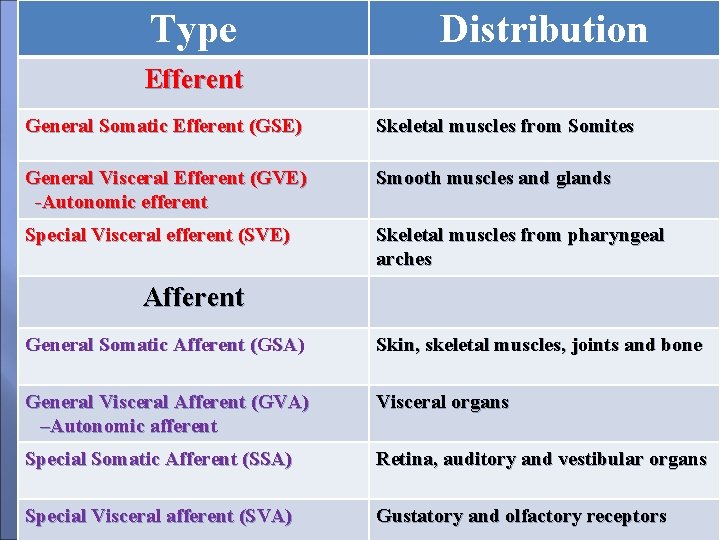
Type Distribution Efferent General Somatic Efferent (GSE) Skeletal muscles from Somites General Visceral Efferent (GVE) -Autonomic efferent Smooth muscles and glands Special Visceral efferent (SVE) Skeletal muscles from pharyngeal arches Afferent General Somatic Afferent (GSA) Skin, skeletal muscles, joints and bone General Visceral Afferent (GVA) –Autonomic afferent Visceral organs Special Somatic Afferent (SSA) Retina, auditory and vestibular organs Special Visceral afferent (SVA) Gustatory and olfactory receptors
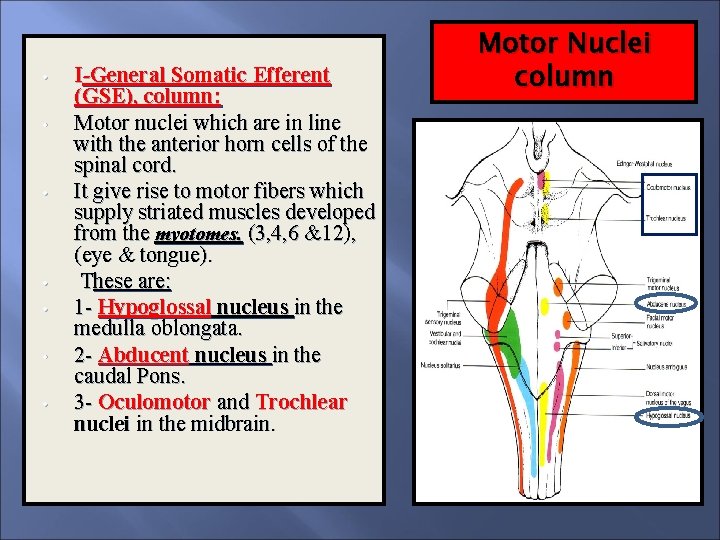
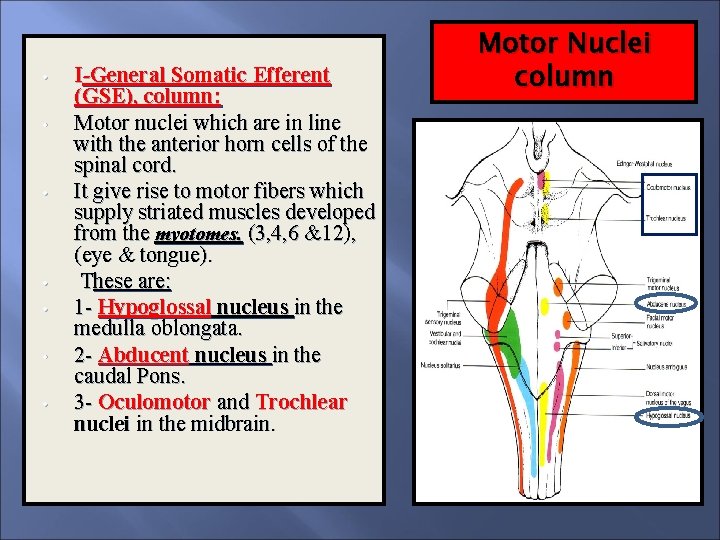
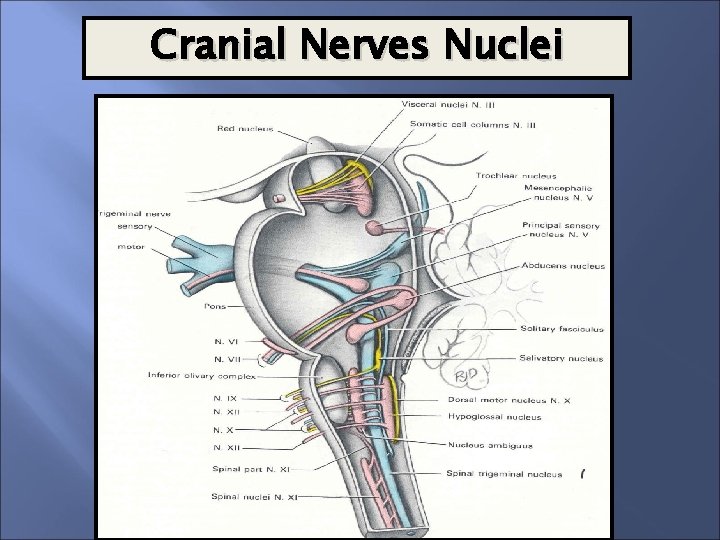
• • I-General Somatic Efferent (GSE), column: Motor nuclei which are in line with the anterior horn cells of the spinal cord. It give rise to motor fibers which supply striated muscles developed from the myotomes. (3, 4, 6 &12), (eye & tongue). These are: 1 - Hypoglossal nucleus in the medulla oblongata. 2 - Abducent nucleus in the caudal Pons. 3 - Oculomotor and Trochlear nuclei in the midbrain. Motor Nuclei column
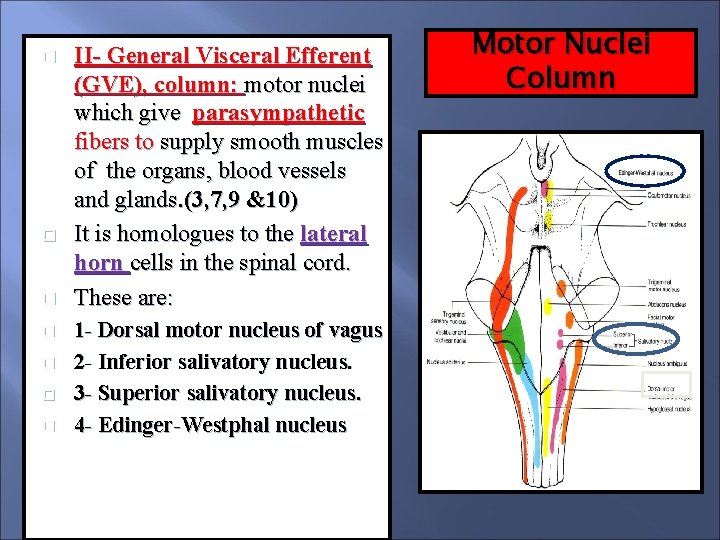
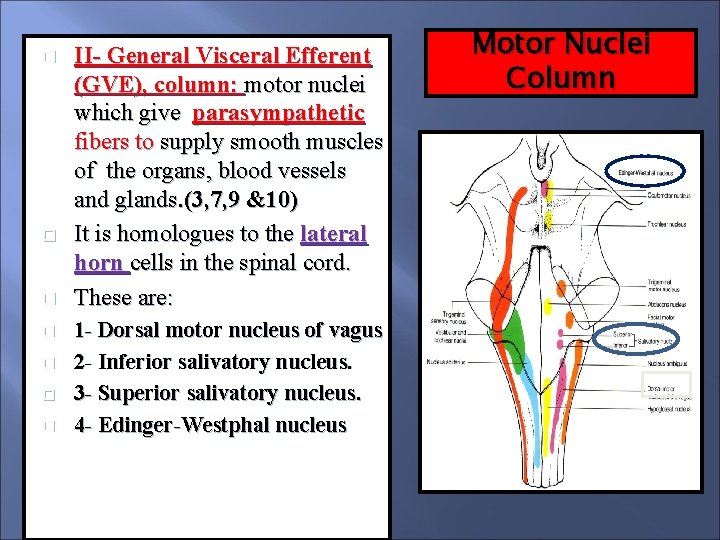
II- General Visceral Efferent (GVE), column: motor nuclei which give parasympathetic fibers to supply smooth muscles of the organs, blood vessels and glands. (3, 7, 9 &10) It is homologues to the lateral horn cells in the spinal cord. These are: 1 - Dorsal motor nucleus of vagus 2 - Inferior salivatory nucleus. 3 - Superior salivatory nucleus. 4 - Edinger-Westphal nucleus Motor Nuclei Column
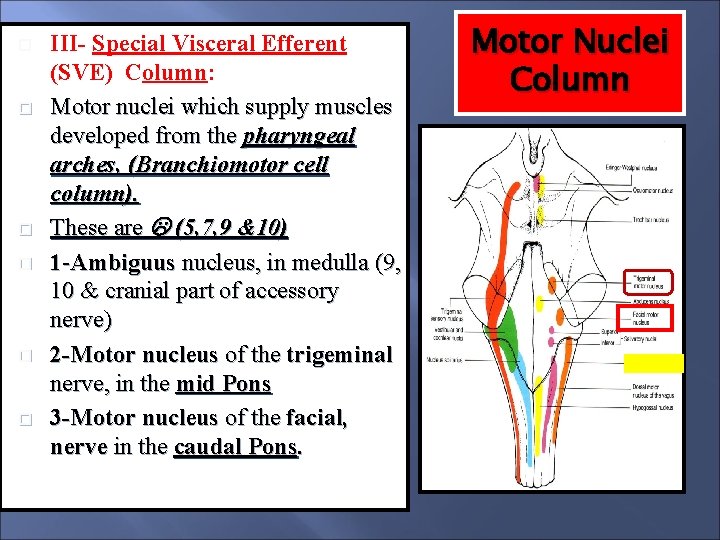
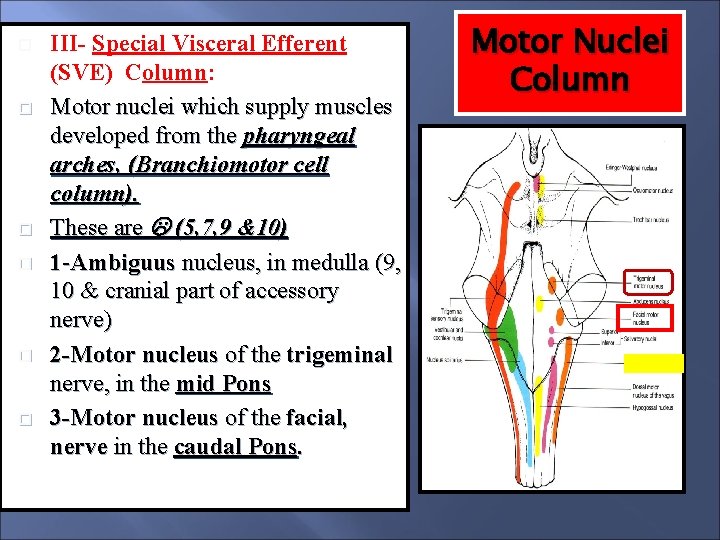
III- Special Visceral Efferent (SVE) Column: Motor nuclei which supply muscles developed from the pharyngeal arches, (Branchiomotor cell column). These are (5, 7, 9 &10) 1 -Ambiguus nucleus, in medulla (9, 10 & cranial part of accessory nerve) 2 -Motor nucleus of the trigeminal nerve, in the mid Pons 3 -Motor nucleus of the facial, nerve in the caudal Pons. Motor Nuclei Column
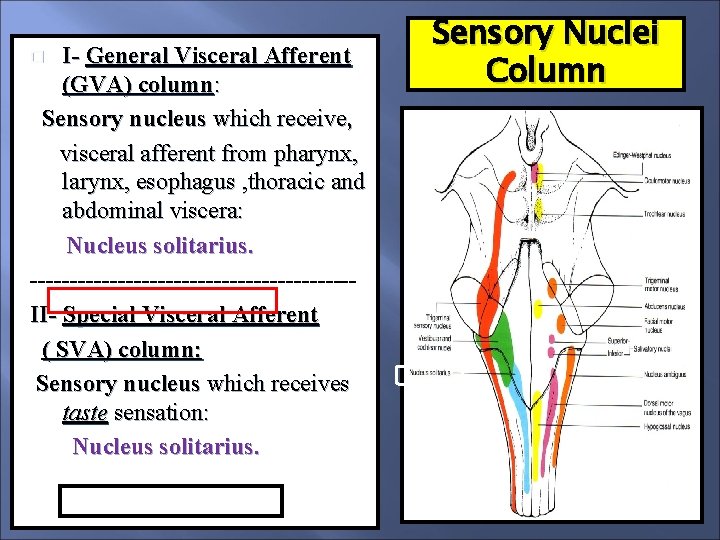
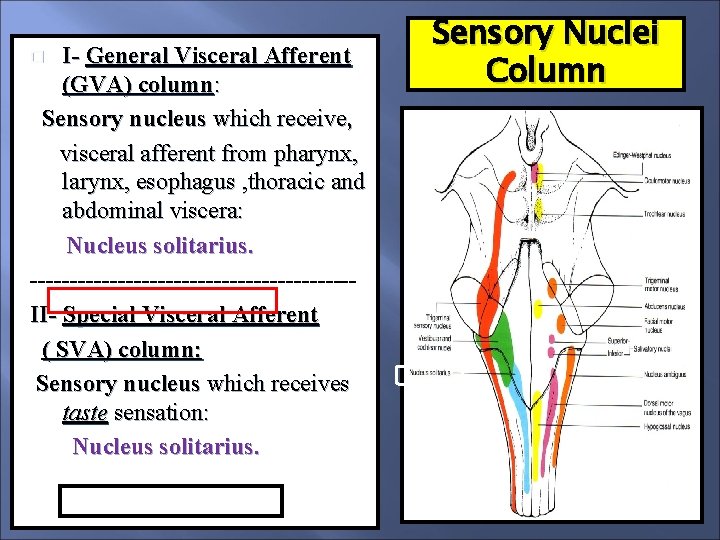
I- General Visceral Afferent (GVA) column: Sensory nucleus which receive, visceral afferent from pharynx, larynx, esophagus , thoracic and abdominal viscera: Nucleus solitarius. --------------------II- Special Visceral Afferent ( SVA) column: Sensory nucleus which receives taste sensation: Nucleus solitarius. Sensory Nuclei Column
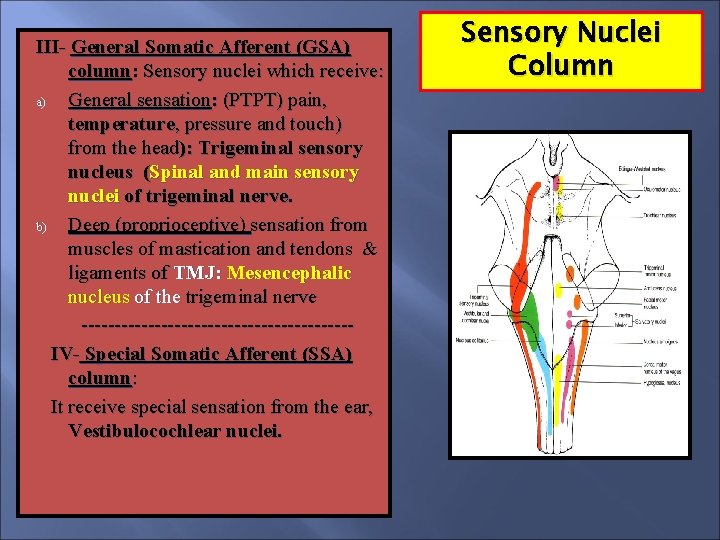
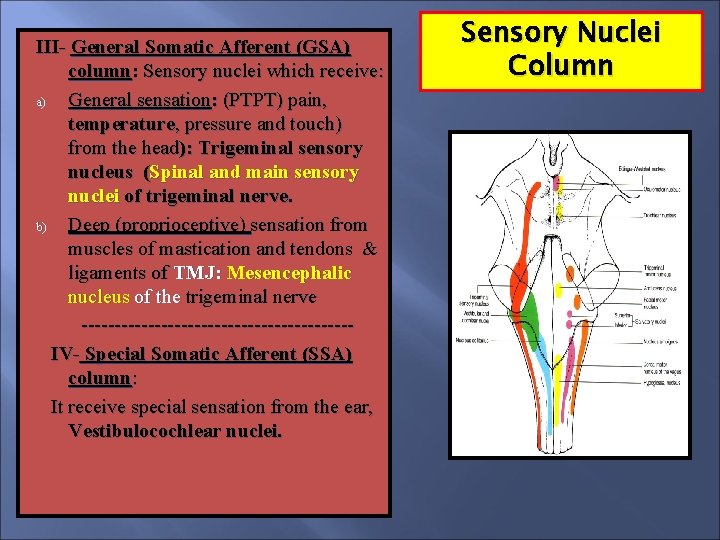
III- General Somatic Afferent (GSA) column: Sensory nuclei which receive: a) General sensation: (PTPT) pain, temperature, pressure and touch) from the head): Trigeminal sensory nucleus (Spinal and main sensory nuclei of trigeminal nerve. b) Deep (proprioceptive) sensation from muscles of mastication and tendons & ligaments of TMJ: Mesencephalic nucleus of the trigeminal nerve --------------------IV- Special Somatic Afferent (SSA) column: It receive special sensation from the ear, Vestibulocochlear nuclei. Sensory Nuclei Column
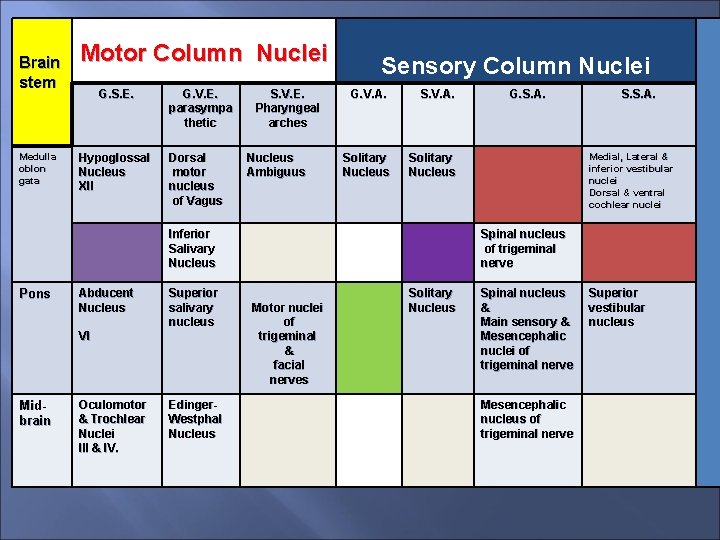
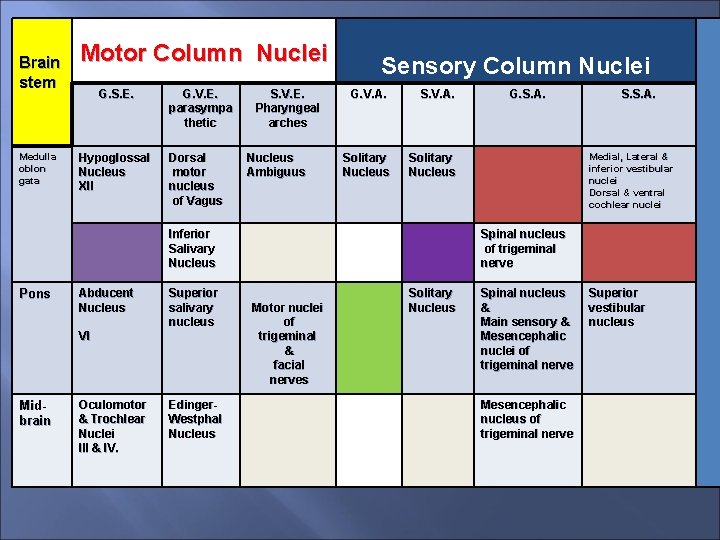
Brain stem Medulla oblon gata Motor Column Nuclei G. S. E. Hypoglossal Nucleus XII G. V. E. parasympa thetic Dorsal motor nucleus of Vagus S. V. E. Pharyngeal arches Nucleus Ambiguus Sensory Column Nuclei G. V. A. Solitary Nucleus Inferior Salivary Nucleus Pons Abducent Nucleus Superior salivary nucleus VI Midbrain Oculomotor & Trochlear Nuclei III & IV. Edinger. Westphal Nucleus G. S. A. S. S. A. Medial, Lateral & inferior vestibular nuclei Dorsal & ventral cochlear nuclei Spinal nucleus of trigeminal nerve Motor nuclei of trigeminal & facial nerves Solitary Nucleus Spinal nucleus & Main sensory & Mesencephalic nuclei of trigeminal nerve Mesencephalic nucleus of trigeminal nerve Superior vestibular nucleus
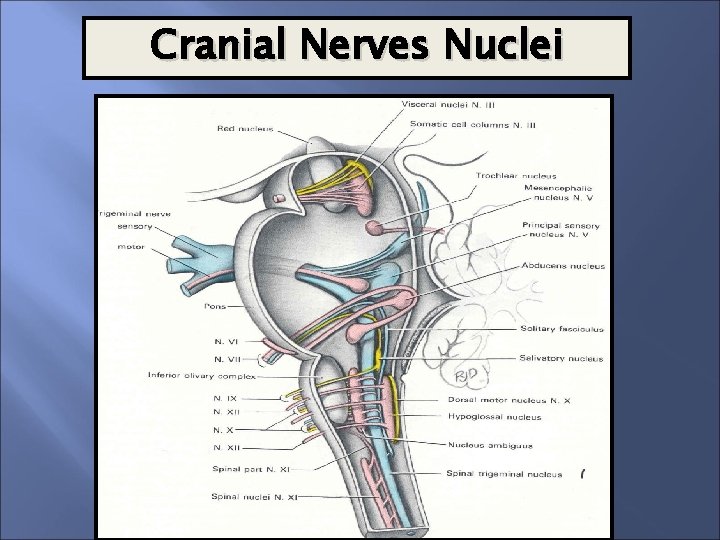
Cranial Nerves Nuclei
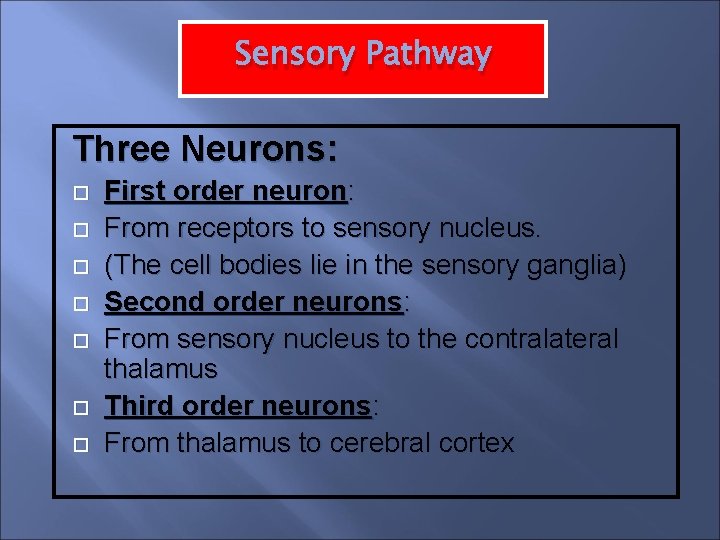
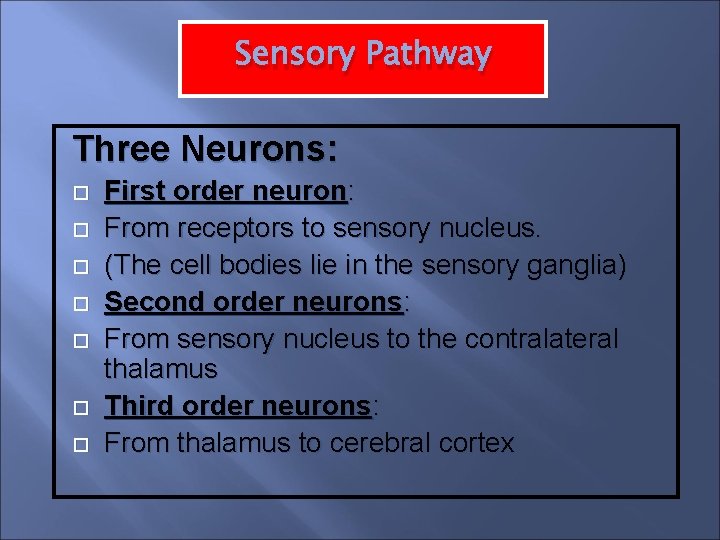
Sensory Pathway Three Neurons: First order neuron: From receptors to sensory nucleus. (The cell bodies lie in the sensory ganglia) Second order neurons: From sensory nucleus to the contralateral thalamus Third order neurons: From thalamus to cerebral cortex
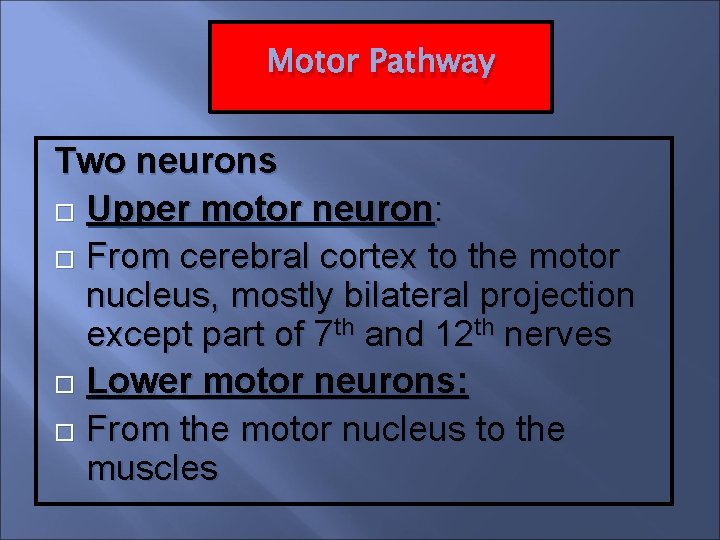
Motor Pathway Two neurons Upper motor neuron: From cerebral cortex to the motor nucleus, mostly bilateral projection except part of 7 th and 12 th nerves Lower motor neurons: From the motor nucleus to the muscles
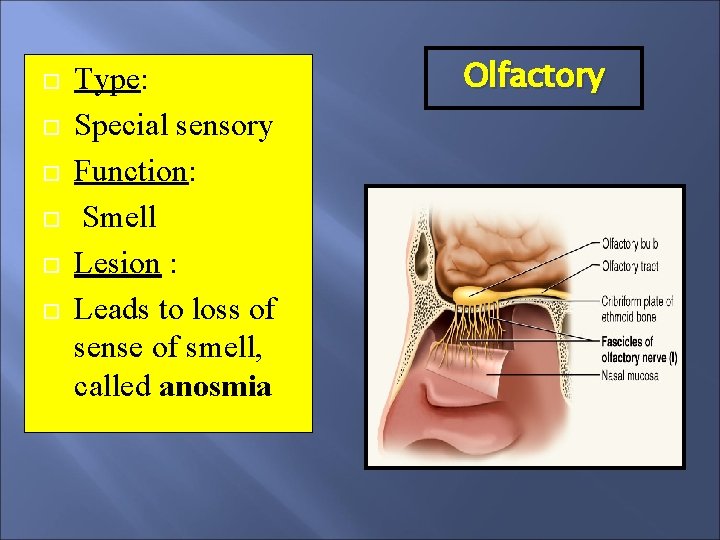
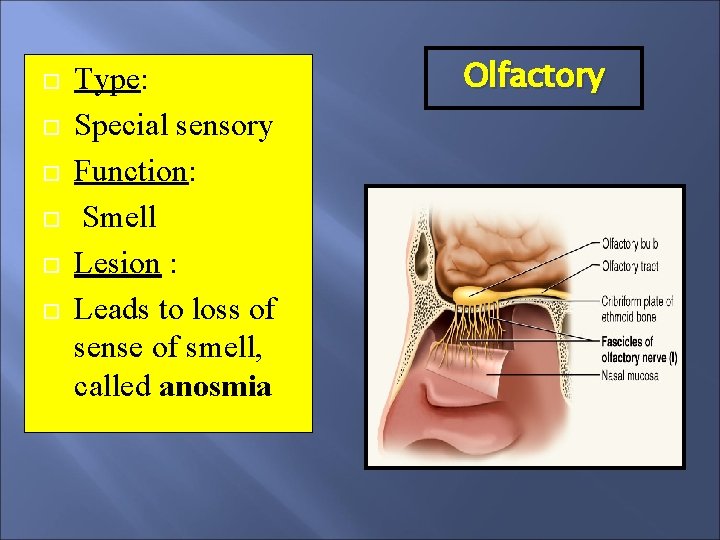
Type: Special sensory Function: Smell Lesion : Leads to loss of sense of smell, called anosmia Olfactory
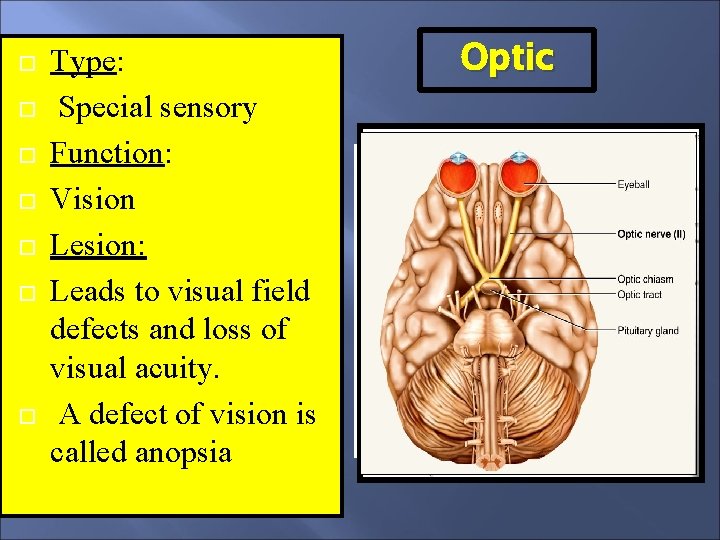
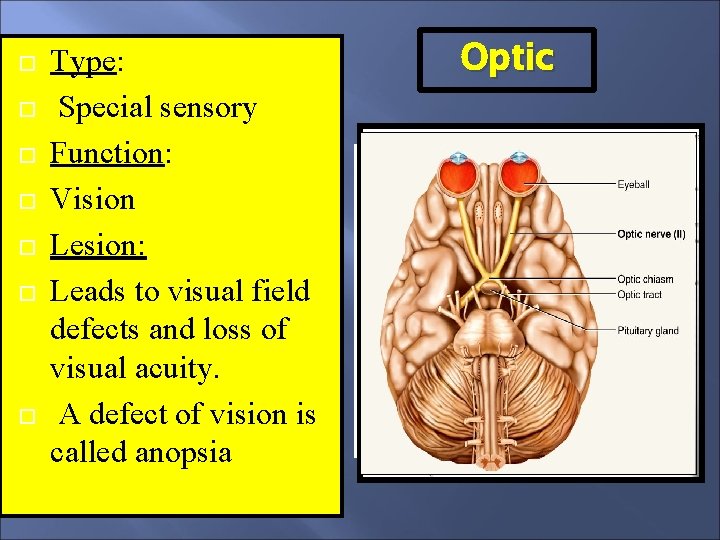
Type: Special sensory Function: Vision Lesion: Leads to visual field defects and loss of visual acuity. A defect of vision is called anopsia Optic
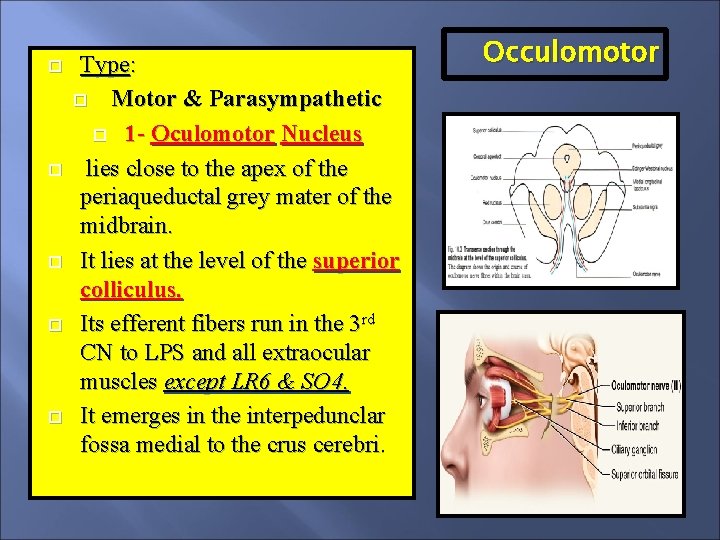
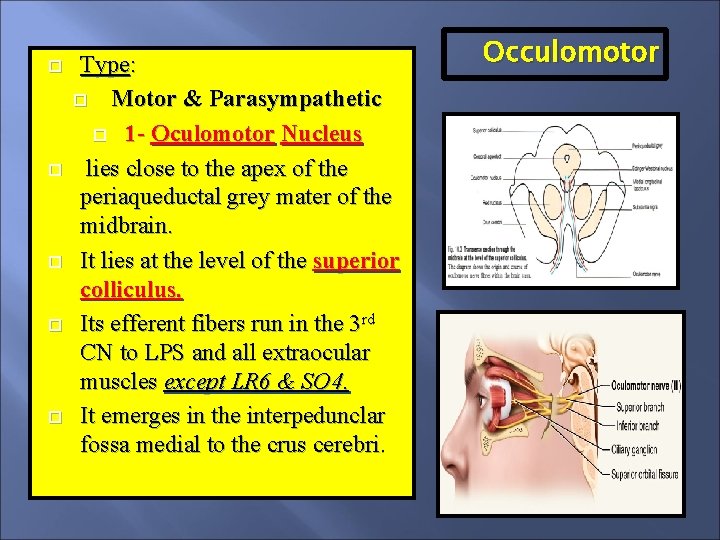
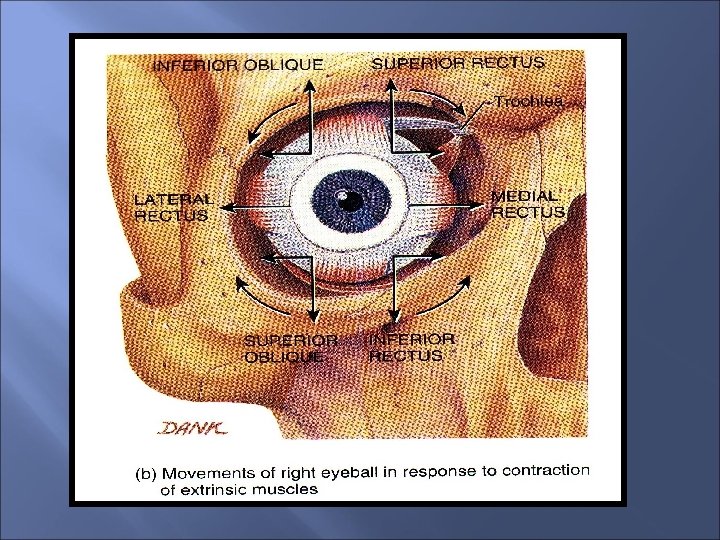
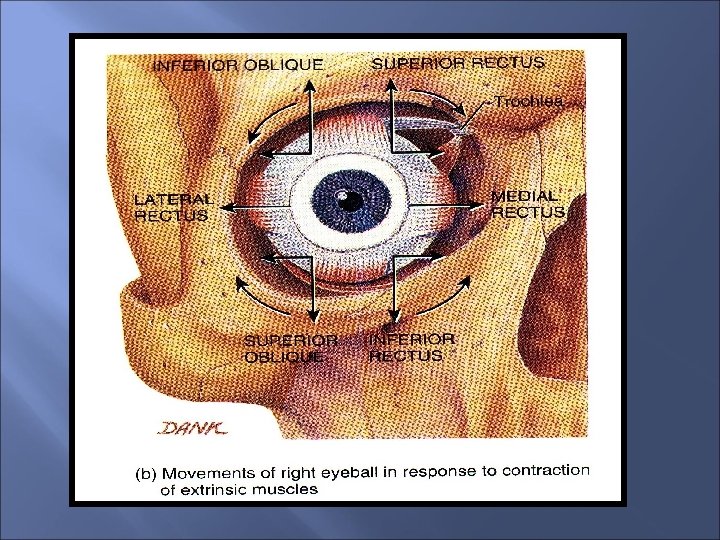
Type: Motor & Parasympathetic 1 - Oculomotor Nucleus lies close to the apex of the periaqueductal grey mater of the midbrain. It lies at the level of the superior colliculus. Its efferent fibers run in the 3 rd CN to LPS and all extraocular muscles except LR 6 & SO 4. It emerges in the interpedunclar fossa medial to the crus cerebri. Occulomotor
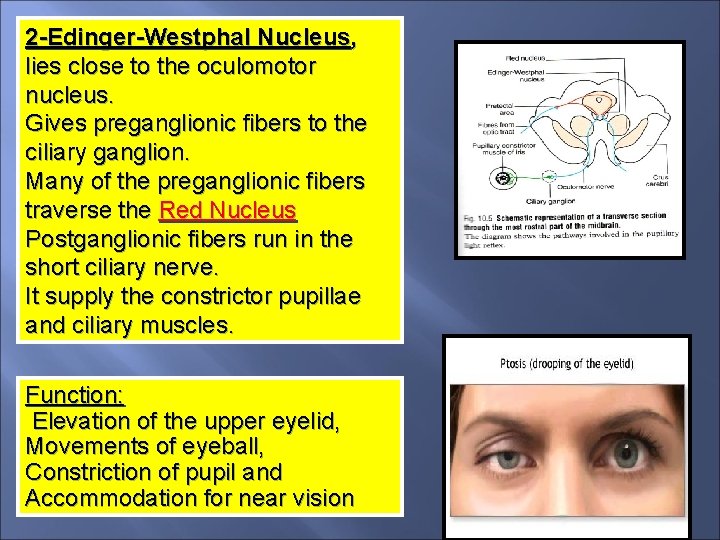
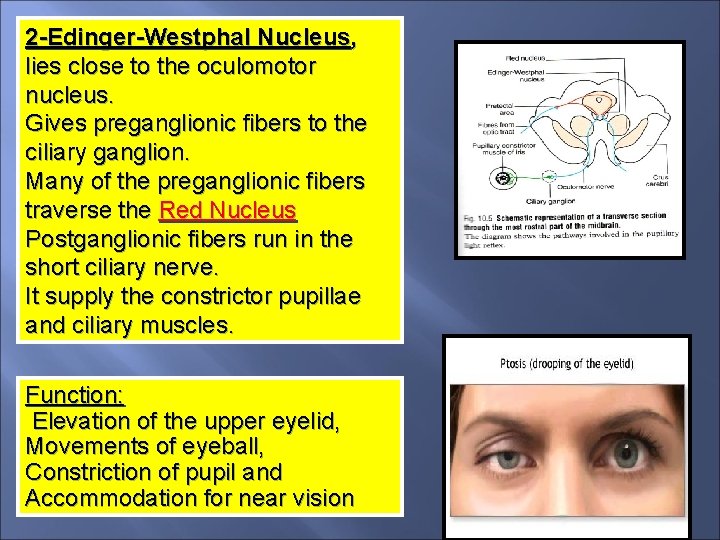
2 -Edinger-Westphal Nucleus, lies close to the oculomotor nucleus. Gives preganglionic fibers to the ciliary ganglion. Many of the preganglionic fibers traverse the Red Nucleus Postganglionic fibers run in the short ciliary nerve. It supply the constrictor pupillae and ciliary muscles. Function: Elevation of the upper eyelid, Movements of eyeball, Constriction of pupil and Accommodation for near vision
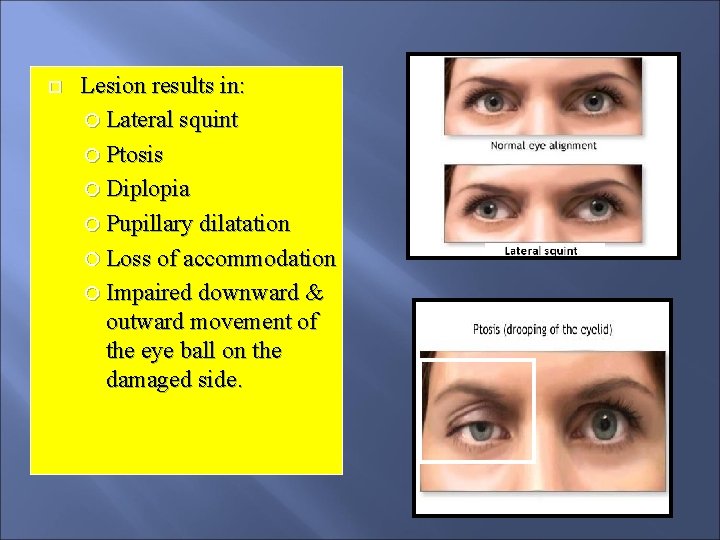
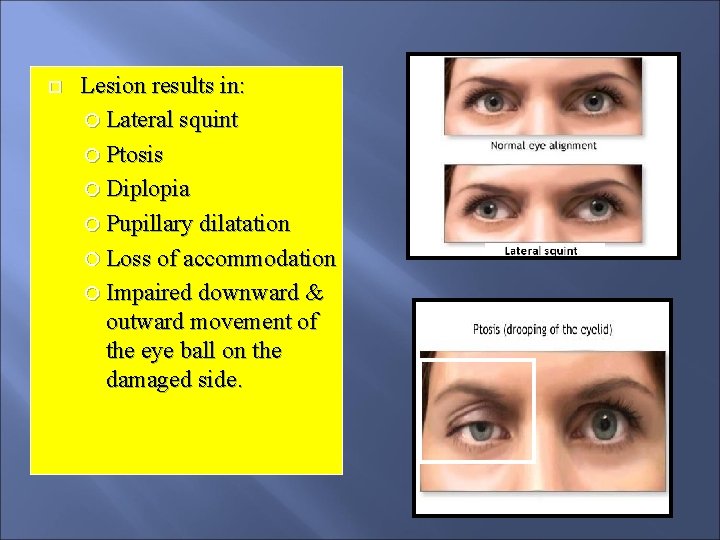
Lesion results in: Lateral squint Ptosis Diplopia Pupillary dilatation Loss of accommodation Impaired downward & outward movement of the eye ball on the damaged side.
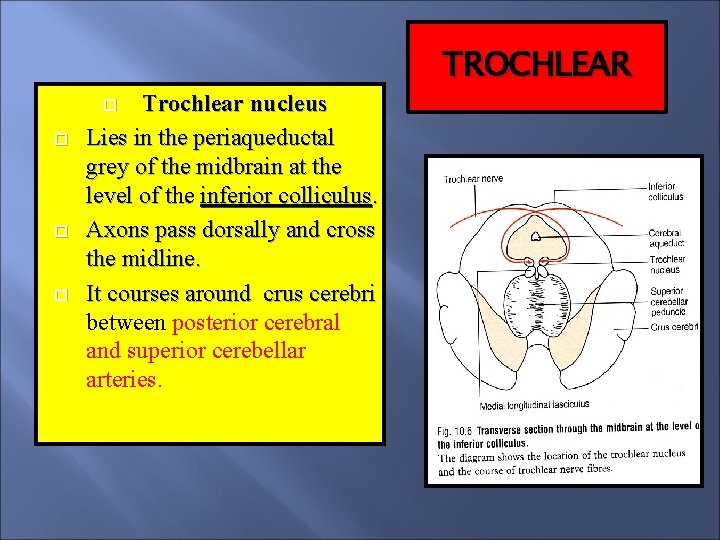
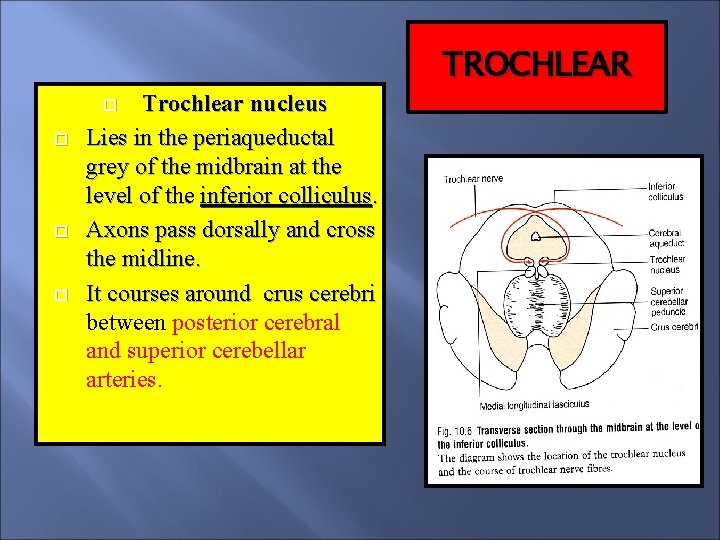
Trochlear nucleus Lies in the periaqueductal grey of the midbrain at the level of the inferior colliculus. Axons pass dorsally and cross the midline. It courses around crus cerebri between posterior cerebral and superior cerebellar arteries. TROCHLEAR
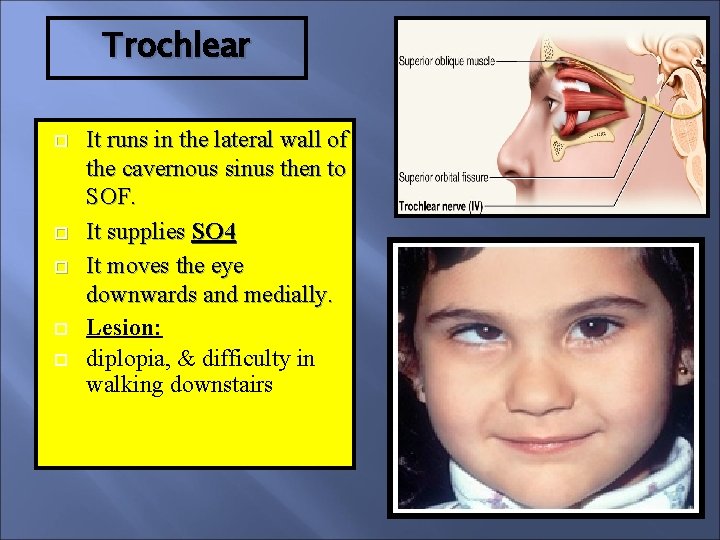
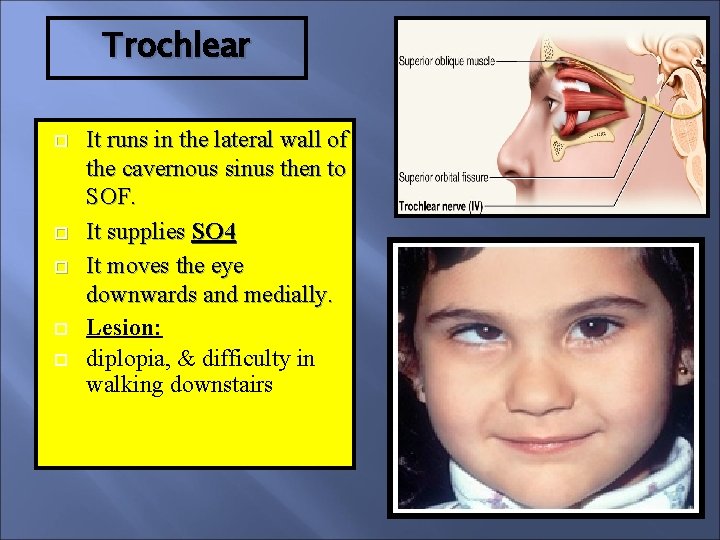
Trochlear It runs in the lateral wall of the cavernous sinus then to SOF. It supplies SO 4 It moves the eye downwards and medially. Lesion: diplopia, & difficulty in walking downstairs
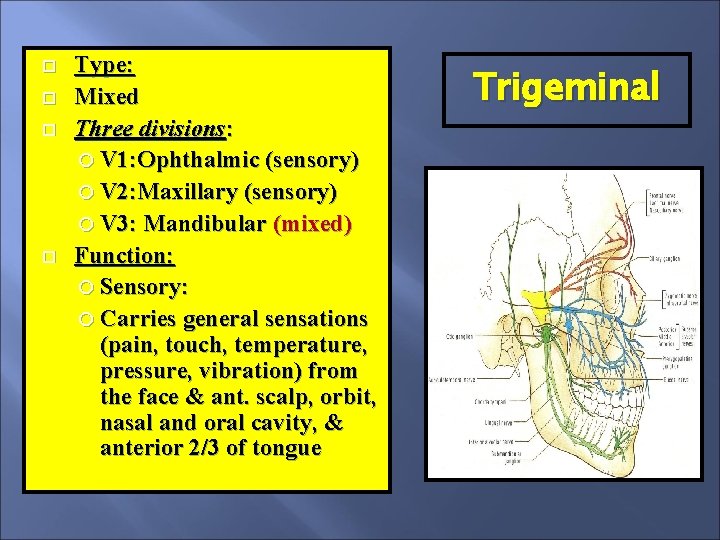
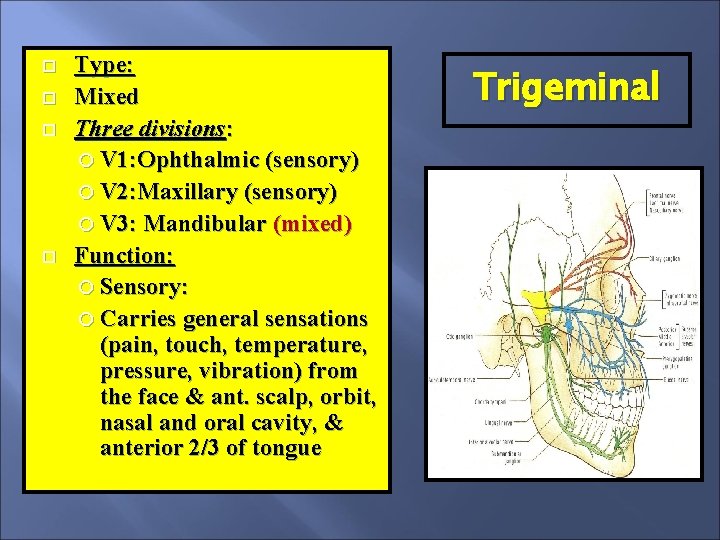
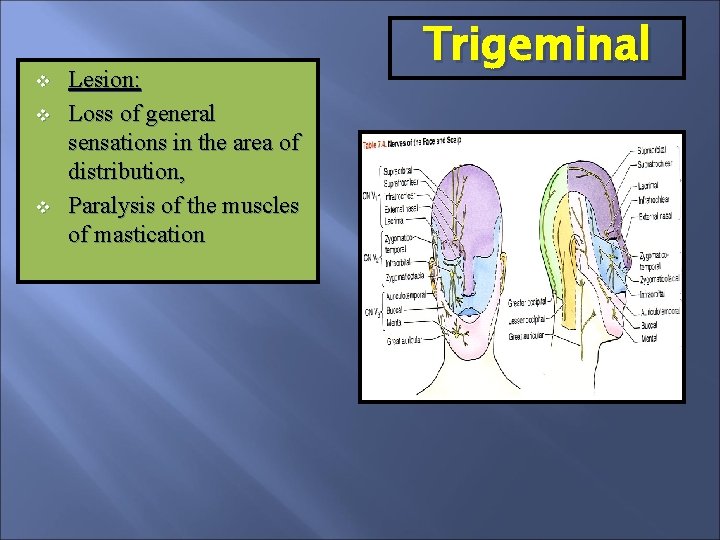
Type: Mixed Three divisions: V 1: Ophthalmic (sensory) V 2: Maxillary (sensory) V 3: Mandibular (mixed) Function: Sensory: Carries general sensations (pain, touch, temperature, pressure, vibration) from the face & ant. scalp, orbit, nasal and oral cavity, & anterior 2/3 of tongue Trigeminal
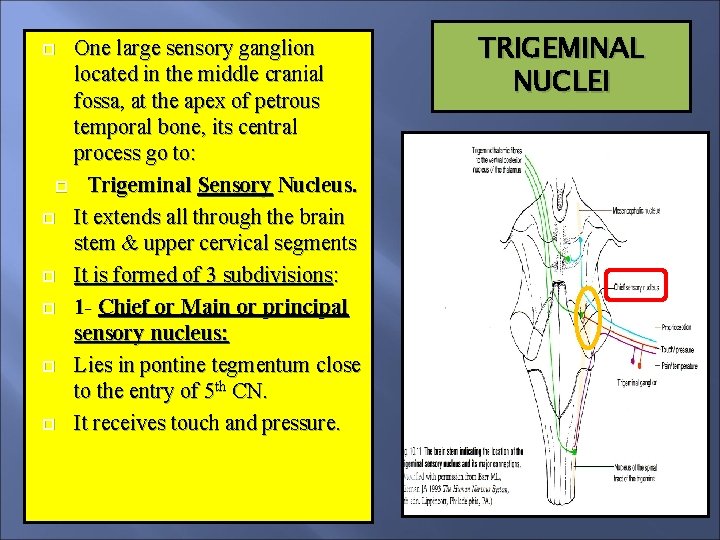
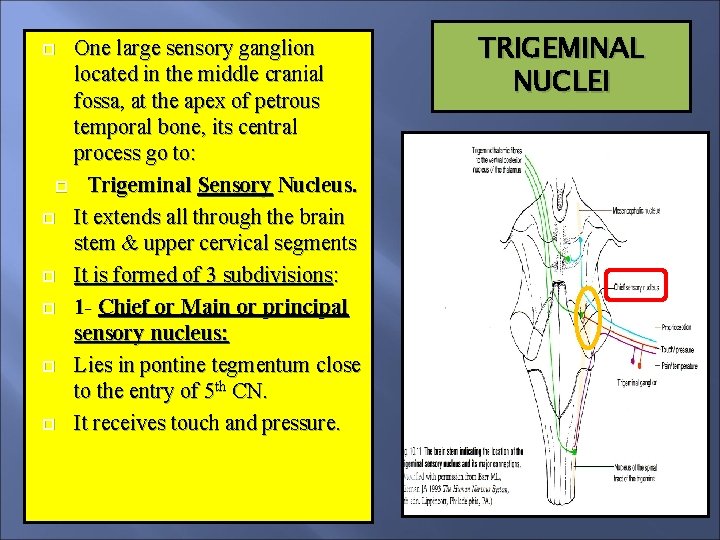
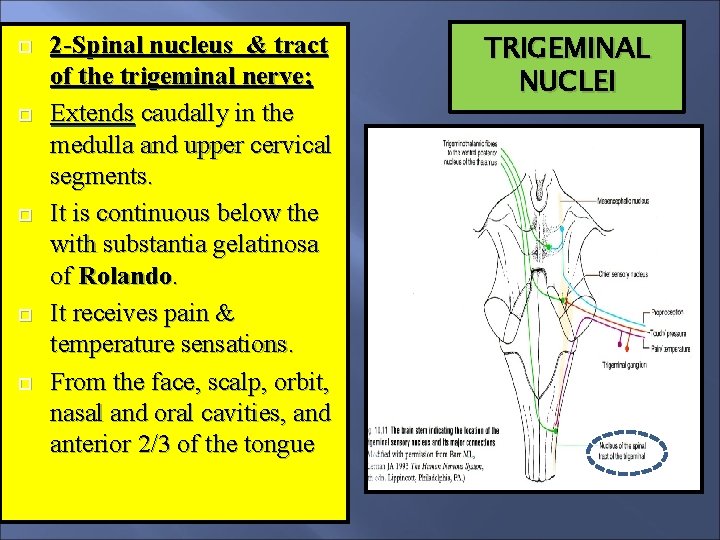
One large sensory ganglion located in the middle cranial fossa, at the apex of petrous temporal bone, its central process go to: Trigeminal Sensory Nucleus. It extends all through the brain stem & upper cervical segments It is formed of 3 subdivisions: 1 - Chief or Main or principal sensory nucleus: Lies in pontine tegmentum close to the entry of 5 th CN. It receives touch and pressure. TRIGEMINAL NUCLEI
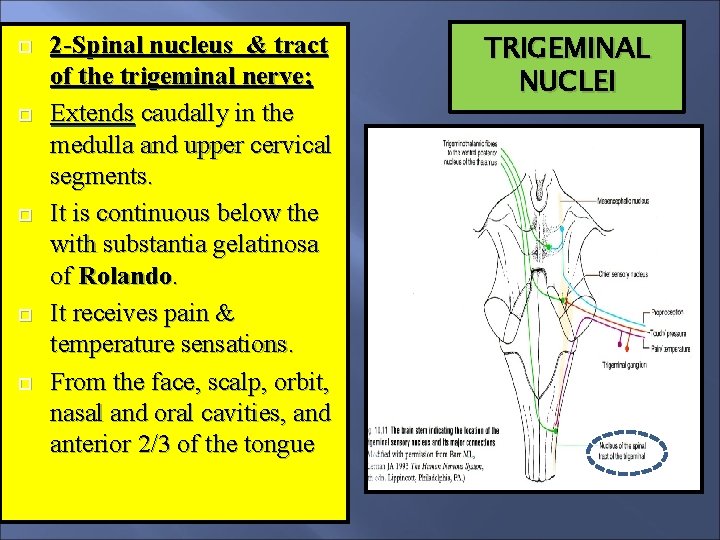
2 -Spinal nucleus & tract of the trigeminal nerve; Extends caudally in the medulla and upper cervical segments. It is continuous below the with substantia gelatinosa of Rolando. It receives pain & temperature sensations. From the face, scalp, orbit, nasal and oral cavities, and anterior 2/3 of the tongue TRIGEMINAL NUCLEI
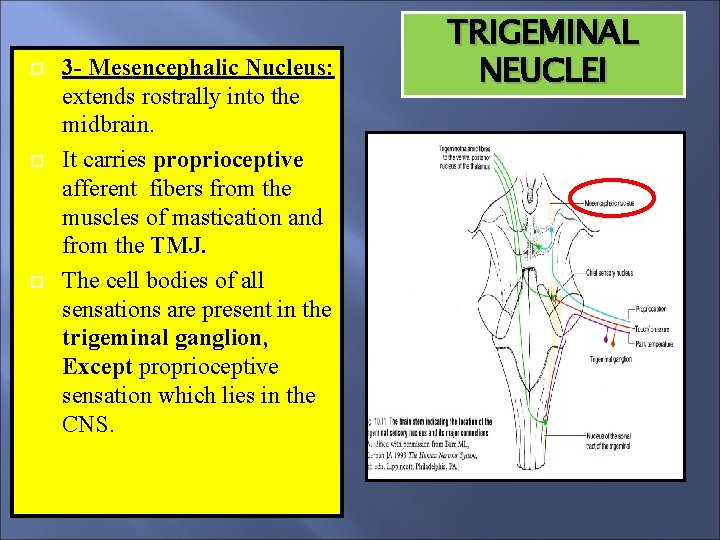
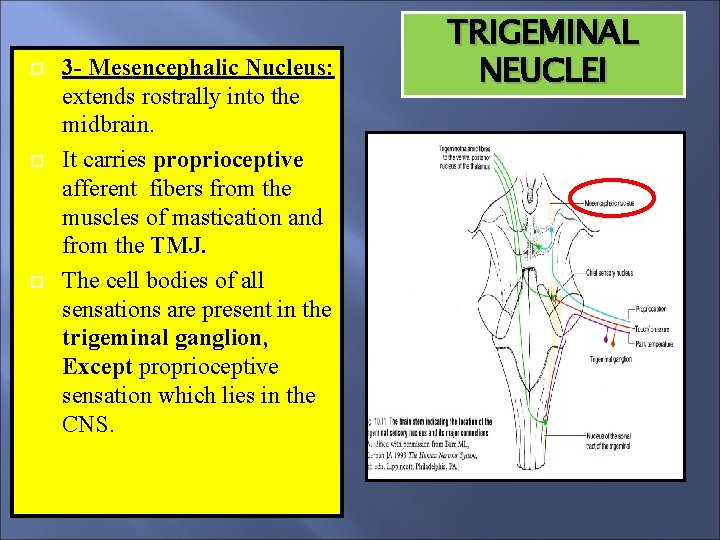
3 - Mesencephalic Nucleus: extends rostrally into the midbrain. It carries proprioceptive afferent fibers from the muscles of mastication and from the TMJ. The cell bodies of all sensations are present in the trigeminal ganglion, Except proprioceptive sensation which lies in the CNS. TRIGEMINAL NEUCLEI
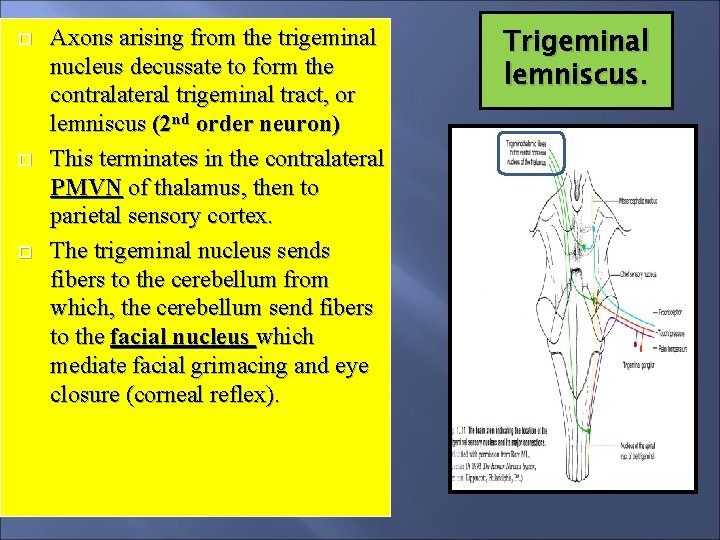
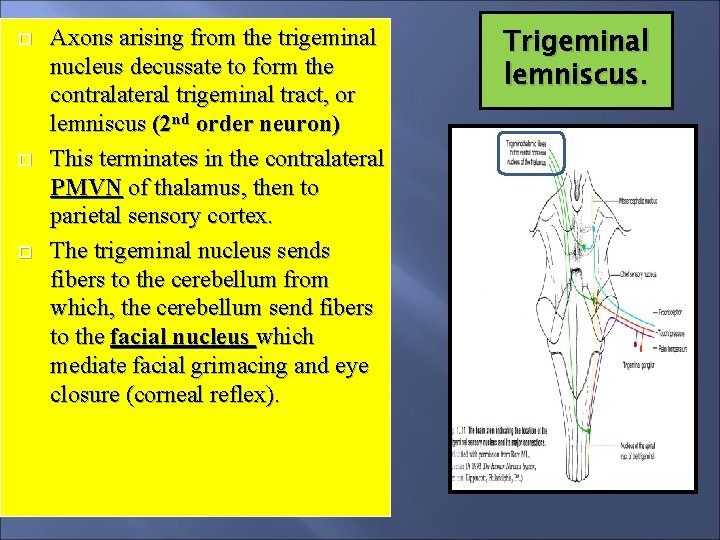
Axons arising from the trigeminal nucleus decussate to form the contralateral trigeminal tract, or lemniscus (2 nd order neuron) This terminates in the contralateral PMVN of thalamus, then to parietal sensory cortex. The trigeminal nucleus sends fibers to the cerebellum from which, the cerebellum send fibers to the facial nucleus which mediate facial grimacing and eye closure (corneal reflex). Trigeminal lemniscus.
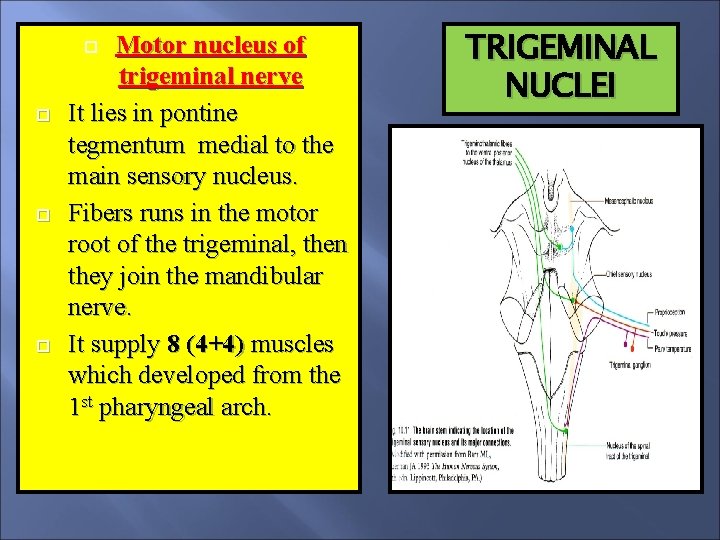
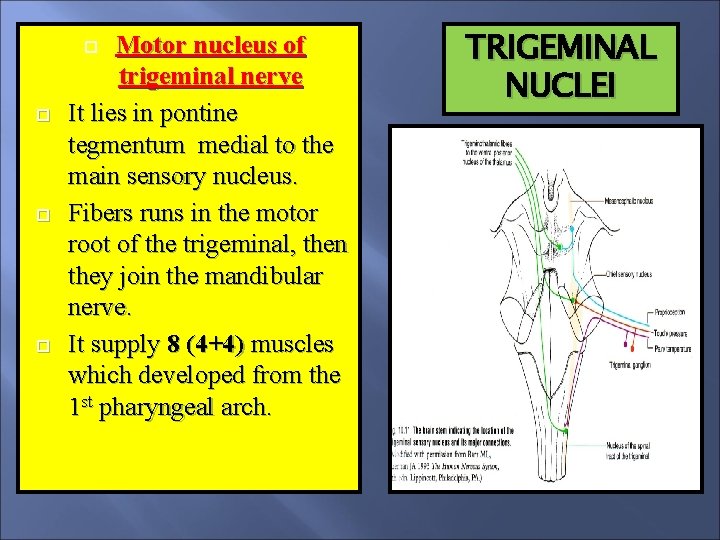
Motor nucleus of trigeminal nerve It lies in pontine tegmentum medial to the main sensory nucleus. Fibers runs in the motor root of the trigeminal, then they join the mandibular nerve. It supply 8 (4+4) muscles which developed from the 1 st pharyngeal arch. TRIGEMINAL NUCLEI
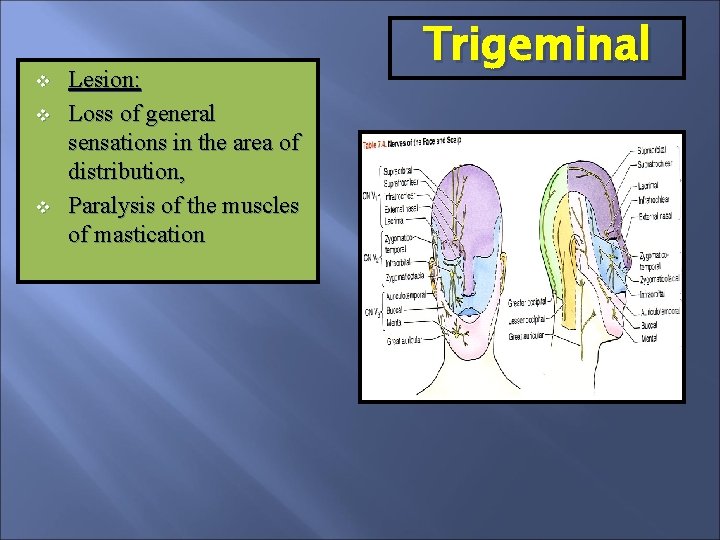
v v v Lesion: Loss of general sensations in the area of distribution, Paralysis of the muscles of mastication Trigeminal
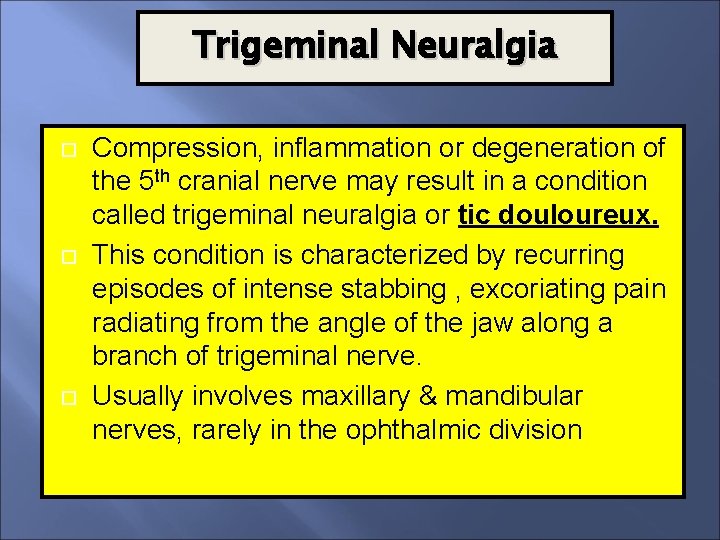
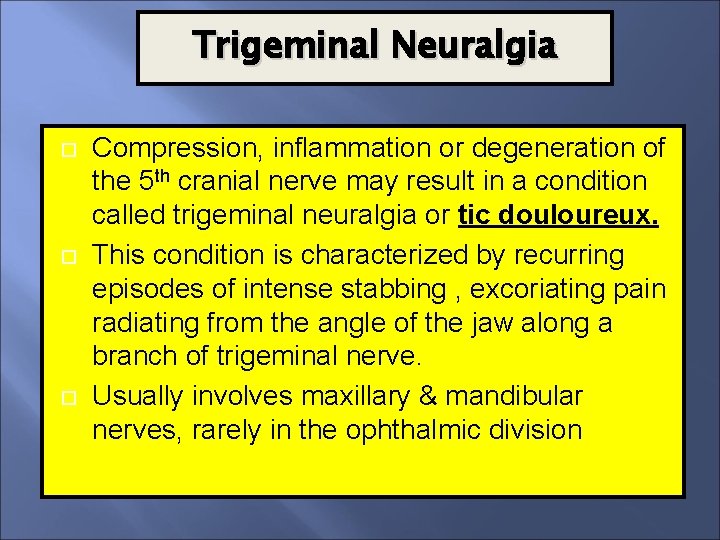
Trigeminal Neuralgia Compression, inflammation or degeneration of the 5 th cranial nerve may result in a condition called trigeminal neuralgia or tic douloureux. This condition is characterized by recurring episodes of intense stabbing , excoriating pain radiating from the angle of the jaw along a branch of trigeminal nerve. Usually involves maxillary & mandibular nerves, rarely in the ophthalmic division
Cranial Nerves II By Prof. Saeed Makarem
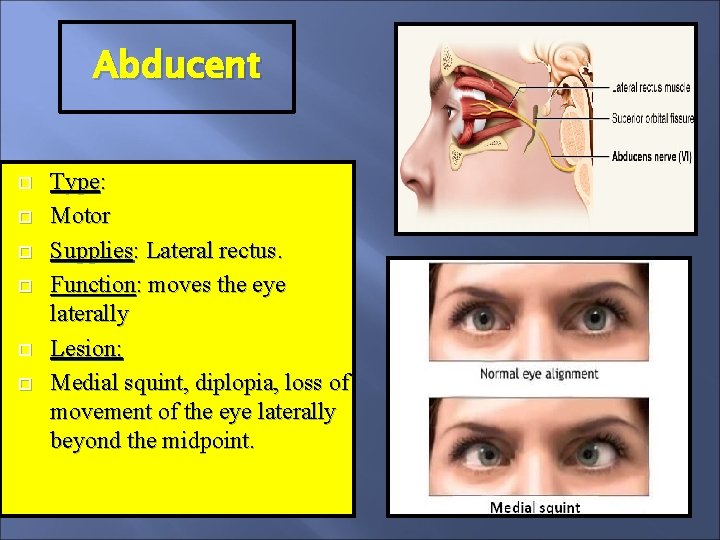
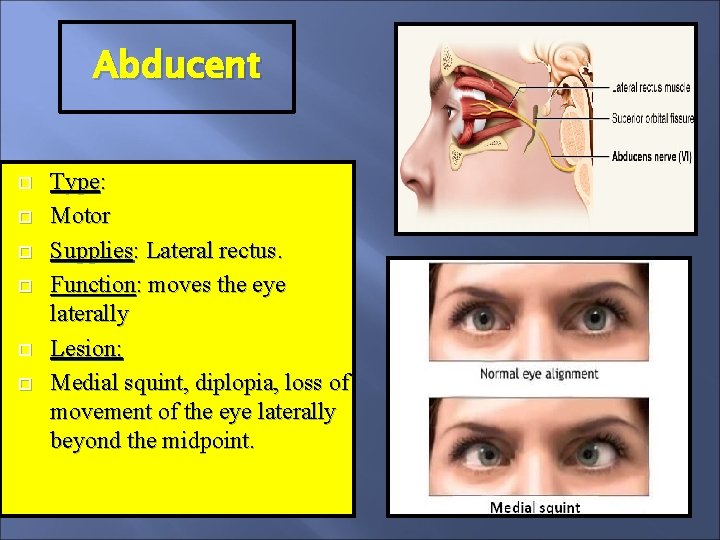
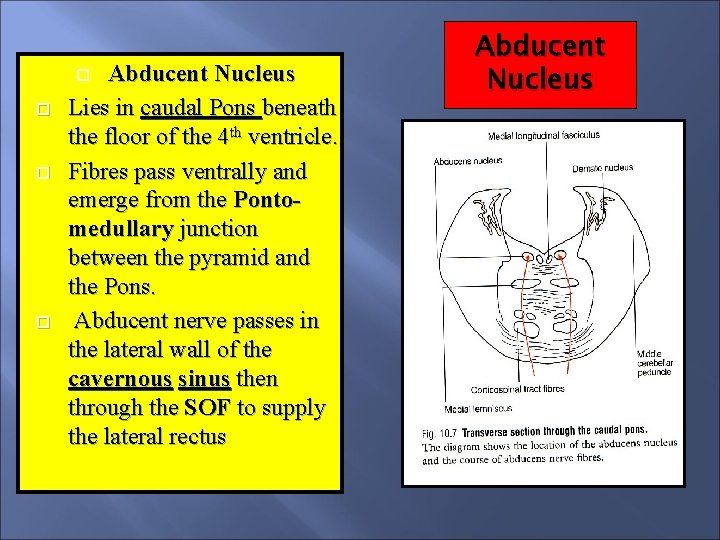
Abducent Type: Motor Supplies: Lateral rectus. Function: moves the eye laterally Lesion: Medial squint, diplopia, loss of movement of the eye laterally beyond the midpoint.
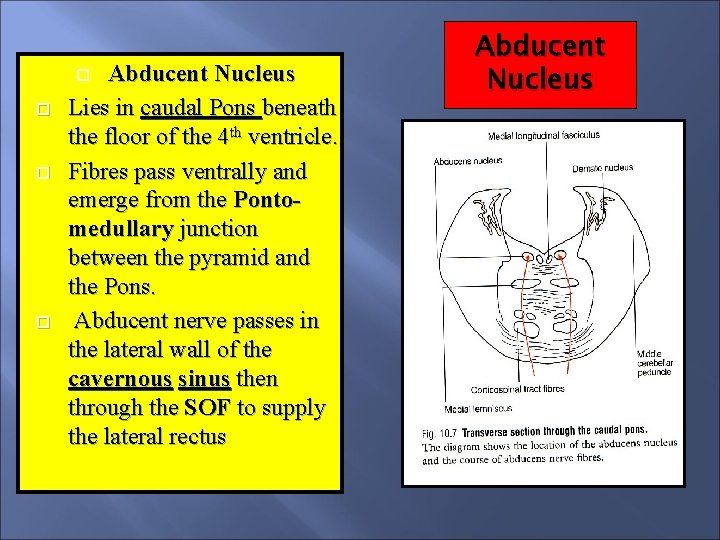
Abducent Nucleus Lies in caudal Pons beneath the floor of the 4 th ventricle. Fibres pass ventrally and emerge from the Pontomedullary junction between the pyramid and the Pons. Abducent nerve passes in the lateral wall of the cavernous sinus then through the SOF to supply the lateral rectus Abducent Nucleus
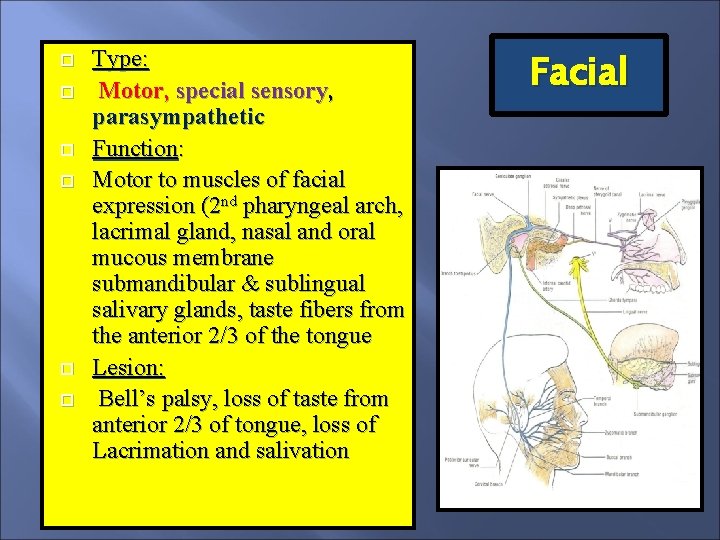
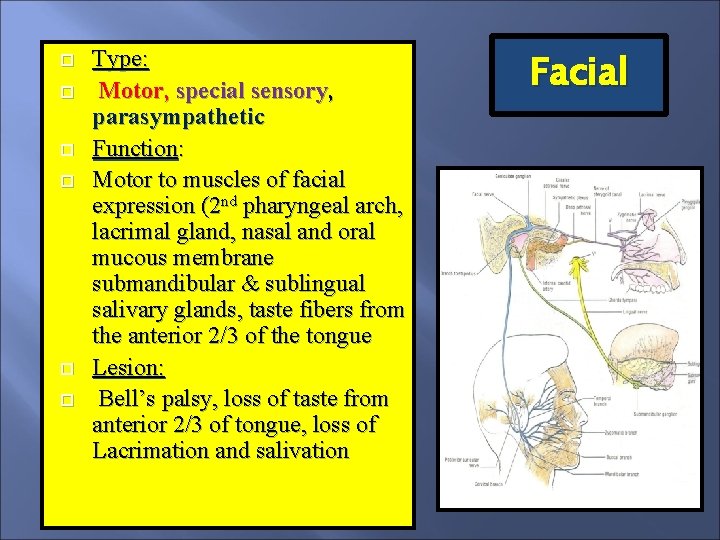
Type: Motor, special sensory, parasympathetic Function: Motor to muscles of facial expression (2 nd pharyngeal arch, lacrimal gland, nasal and oral mucous membrane submandibular & sublingual salivary glands, taste fibers from the anterior 2/3 of the tongue Lesion: Bell’s palsy, loss of taste from anterior 2/3 of tongue, loss of Lacrimation and salivation Facial
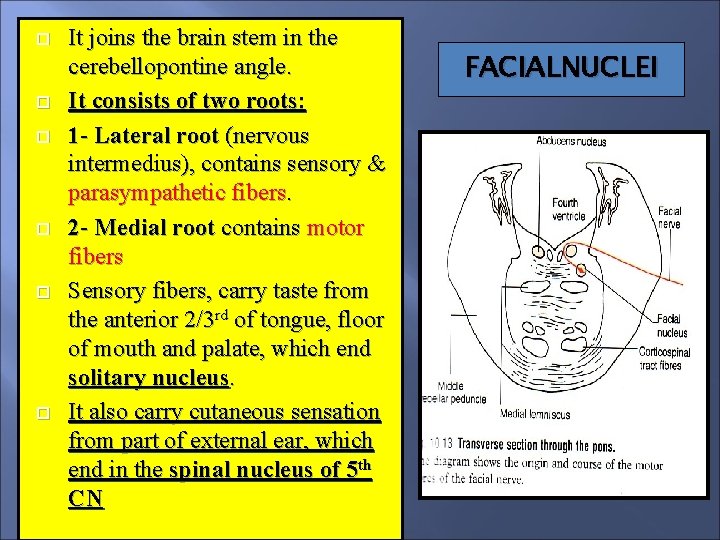
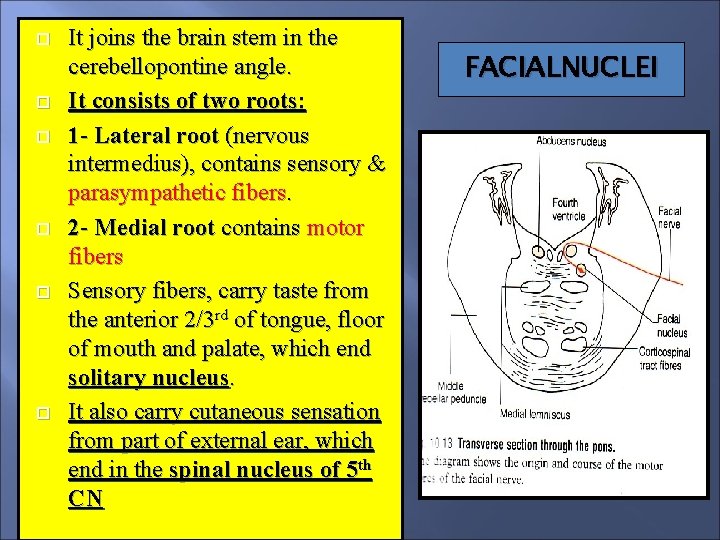
It joins the brain stem in the cerebellopontine angle. It consists of two roots: 1 - Lateral root (nervous intermedius), contains sensory & parasympathetic fibers. 2 - Medial root contains motor fibers Sensory fibers, carry taste from the anterior 2/3 rd of tongue, floor of mouth and palate, which end solitary nucleus. It also carry cutaneous sensation from part of external ear, which end in the spinal nucleus of 5 th CN FACIALNUCLEI
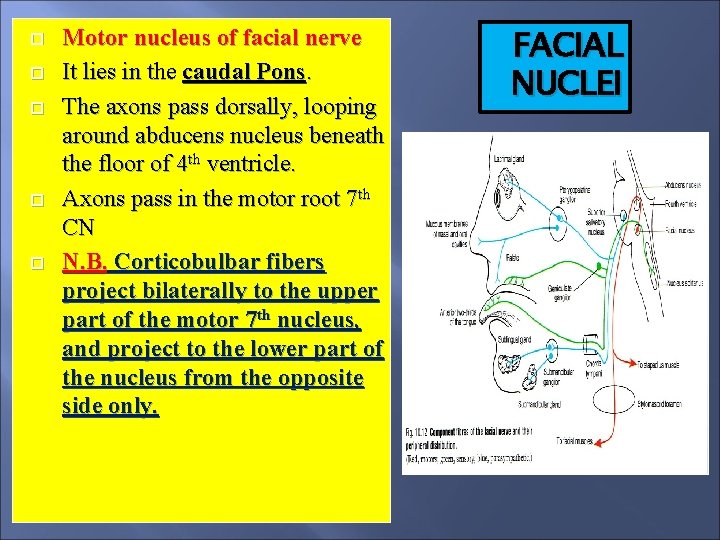
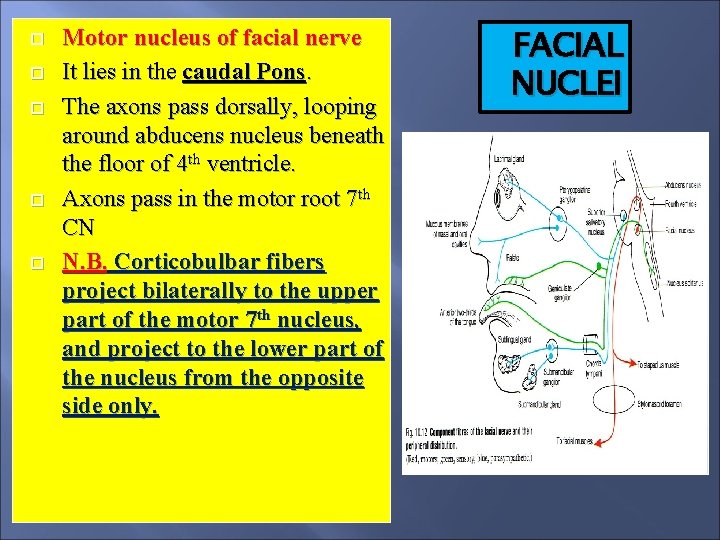
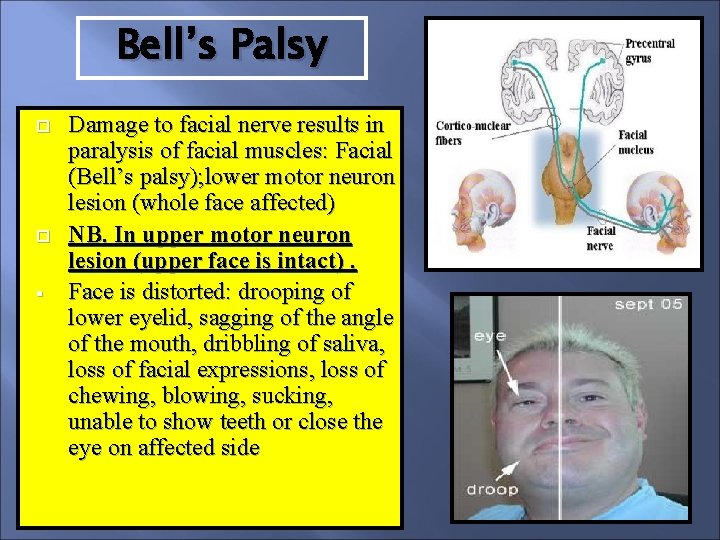
Motor nucleus of facial nerve It lies in the caudal Pons. The axons pass dorsally, looping around abducens nucleus beneath the floor of 4 th ventricle. Axons pass in the motor root 7 th CN N. B. Corticobulbar fibers project bilaterally to the upper part of the motor 7 th nucleus, and project to the lower part of the nucleus from the opposite side only. FACIAL NUCLEI
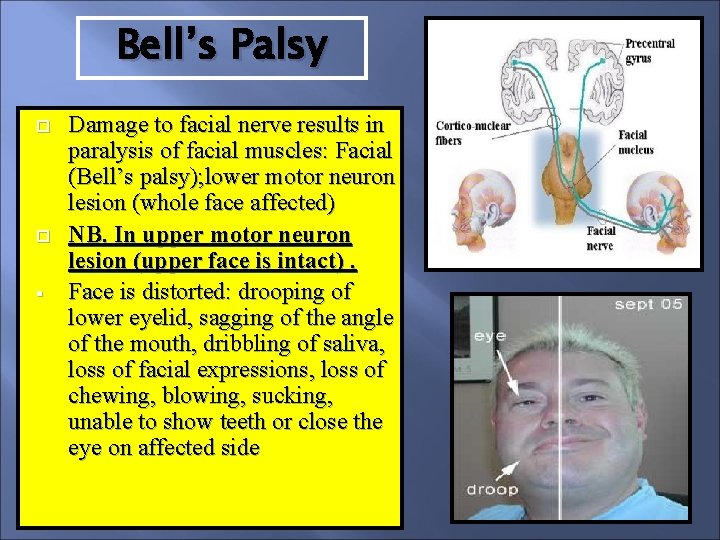
Bell’s Palsy § Damage to facial nerve results in paralysis of facial muscles: Facial (Bell’s palsy); lower motor neuron lesion (whole face affected) NB. In upper motor neuron lesion (upper face is intact). Face is distorted: drooping of lower eyelid, sagging of the angle of the mouth, dribbling of saliva, loss of facial expressions, loss of chewing, blowing, sucking, unable to show teeth or close the eye on affected side
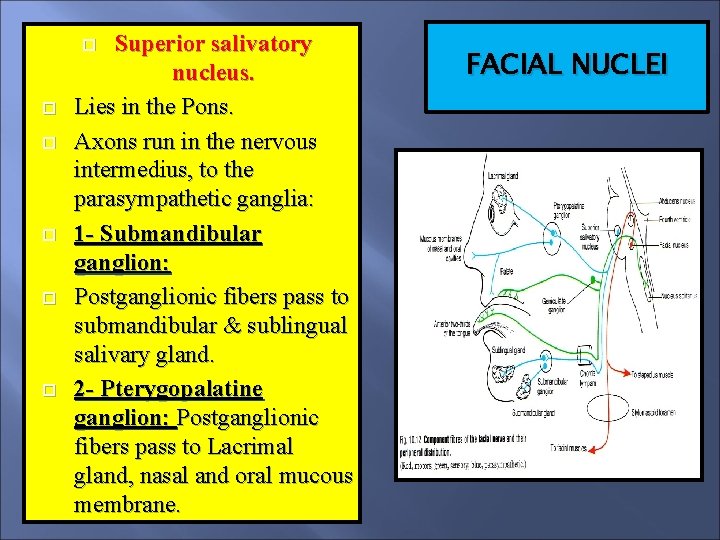
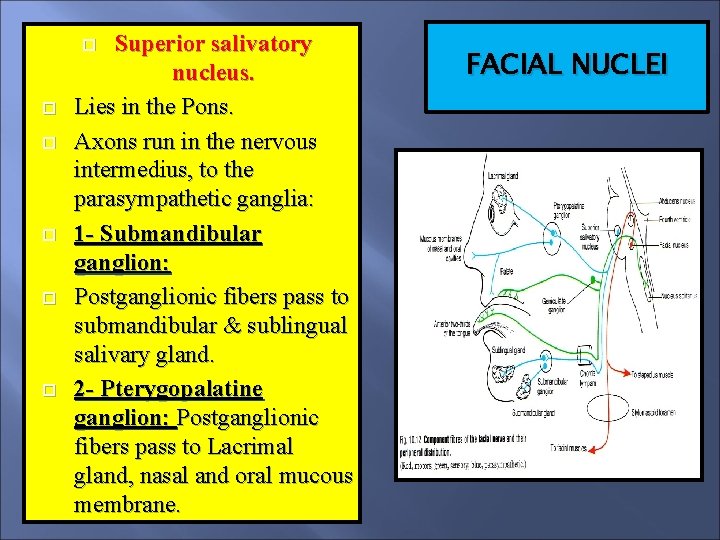
Superior salivatory nucleus. Lies in the Pons. Axons run in the nervous intermedius, to the parasympathetic ganglia: 1 - Submandibular ganglion: Postganglionic fibers pass to submandibular & sublingual salivary gland. 2 - Pterygopalatine ganglion: Postganglionic fibers pass to Lacrimal gland, nasal and oral mucous membrane. FACIAL NUCLEI
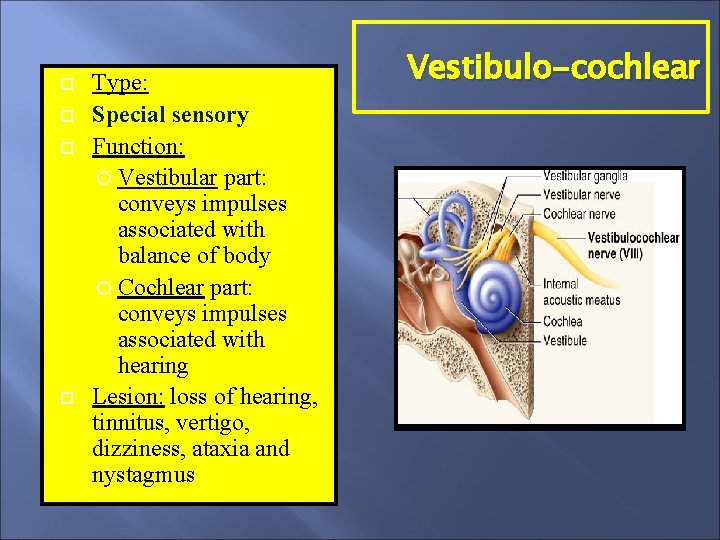
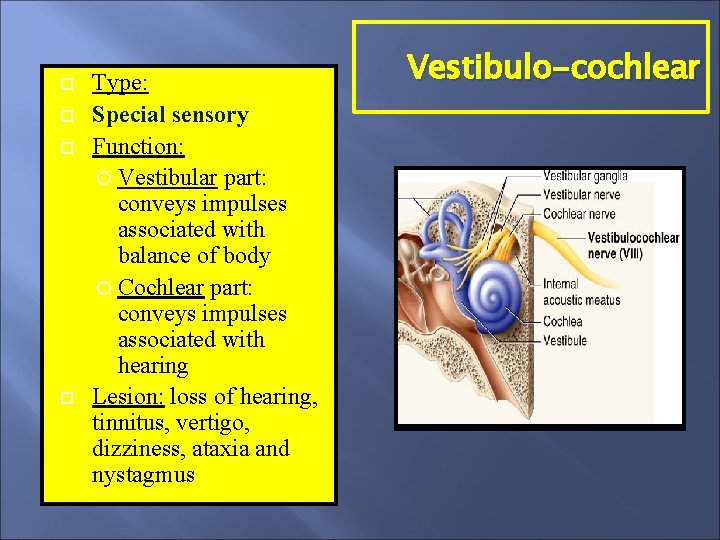
Type: Special sensory Function: Vestibular part: conveys impulses associated with balance of body Cochlear part: conveys impulses associated with hearing Lesion: loss of hearing, tinnitus, vertigo, dizziness, ataxia and nystagmus Vestibulo-cochlear
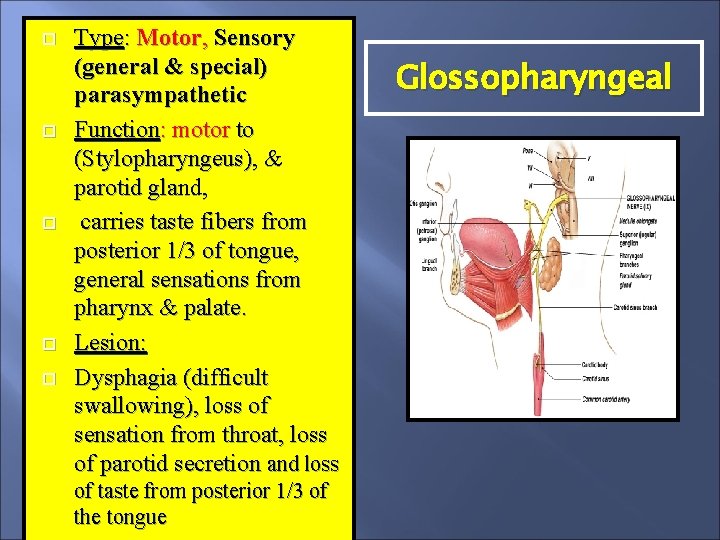
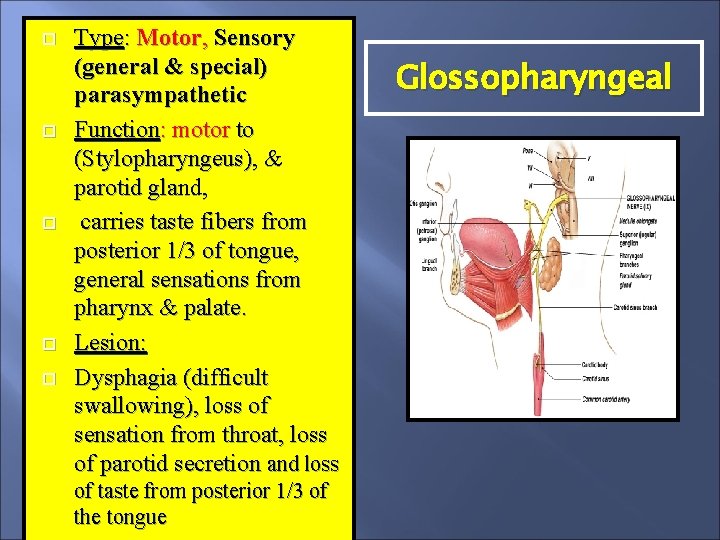
Type: Motor, Sensory (general & special) parasympathetic Function: motor to (Stylopharyngeus), & parotid gland, carries taste fibers from posterior 1/3 of tongue, general sensations from pharynx & palate. Lesion: Dysphagia (difficult swallowing), loss of sensation from throat, loss of parotid secretion and loss of taste from posterior 1/3 of the tongue Glossopharyngeal
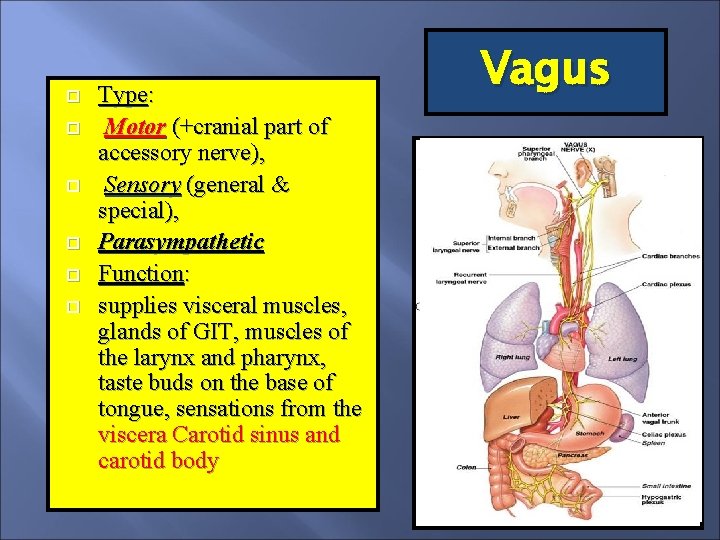
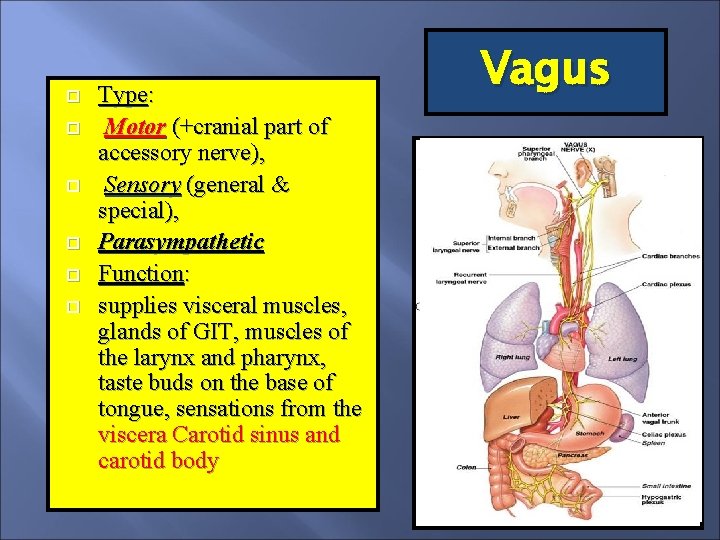
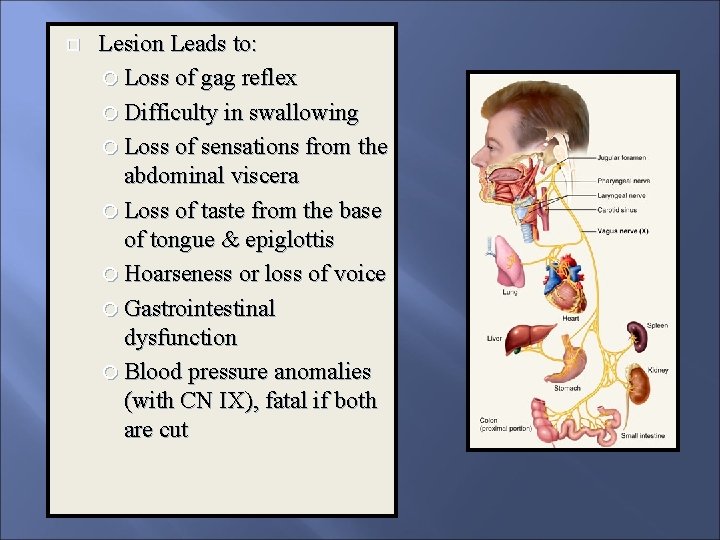
Type: Motor (+cranial part of accessory nerve), Sensory (general & special), Parasympathetic Function: supplies visceral muscles, glands of GIT, muscles of the larynx and pharynx, taste buds on the base of tongue, sensations from the viscera Carotid sinus and carotid body Vagus
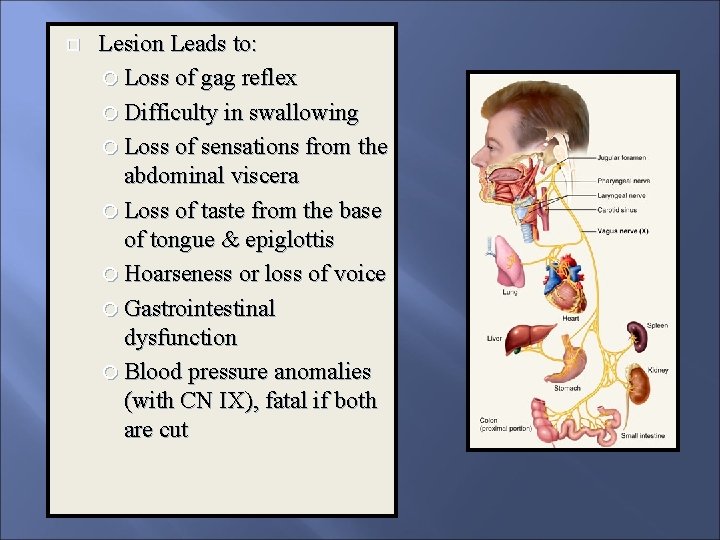
Lesion Leads to: Loss of gag reflex Difficulty in swallowing Loss of sensations from the abdominal viscera Loss of taste from the base of tongue & epiglottis Hoarseness or loss of voice Gastrointestinal dysfunction Blood pressure anomalies (with CN IX), fatal if both are cut
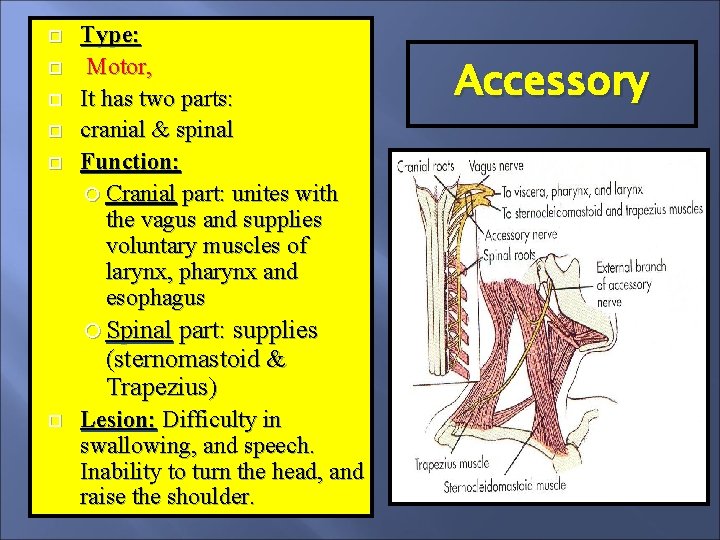
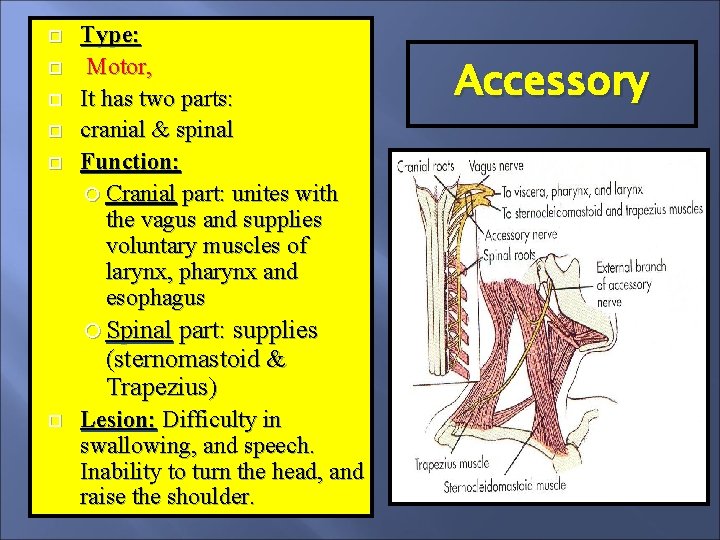
Type: Motor, It has two parts: cranial & spinal Function: Cranial part: unites with the vagus and supplies voluntary muscles of larynx, pharynx and esophagus Spinal part: supplies (sternomastoid & Trapezius) Lesion: Difficulty in swallowing, and speech. Inability to turn the head, and raise the shoulder. Accessory
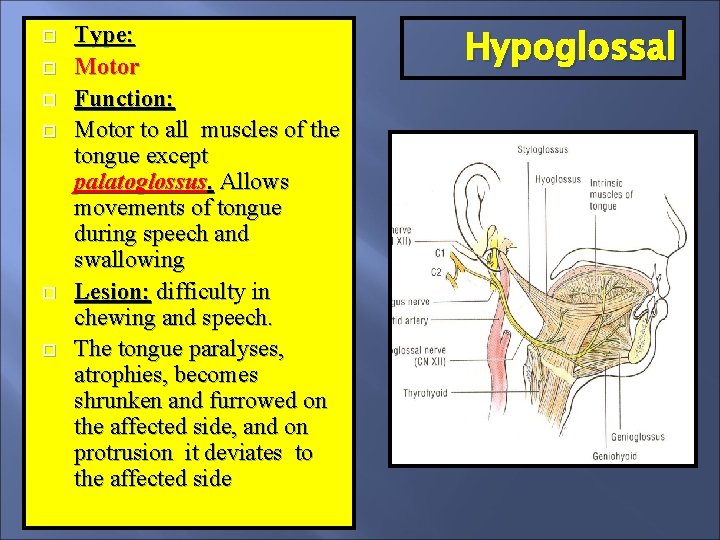
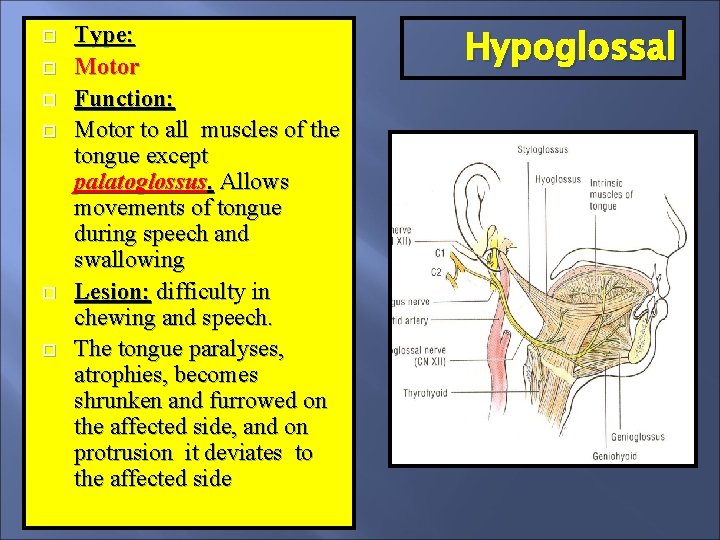
Type: Motor Function: Motor to all muscles of the tongue except palatoglossus. Allows movements of tongue during speech and swallowing Lesion: difficulty in chewing and speech. The tongue paralyses, atrophies, becomes shrunken and furrowed on the affected side, and on protrusion it deviates to the affected side Hypoglossal
Lesion of Cranial Nerves Causes: Severe head injuries, skull bone fractures or penetrating wounds Brain lesions Compression due to raised intracranial pressure (due to any space occupying lesion e. g. tumor, hematoma, or CSF obstruction ) Cavernous sinus thrombosis
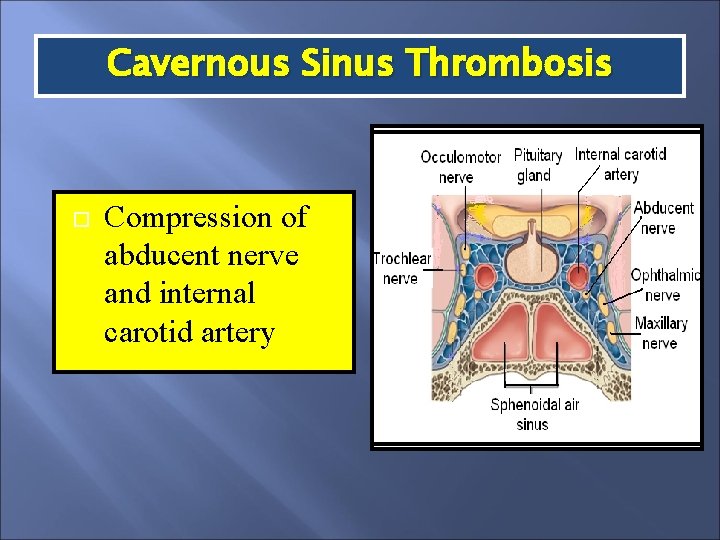
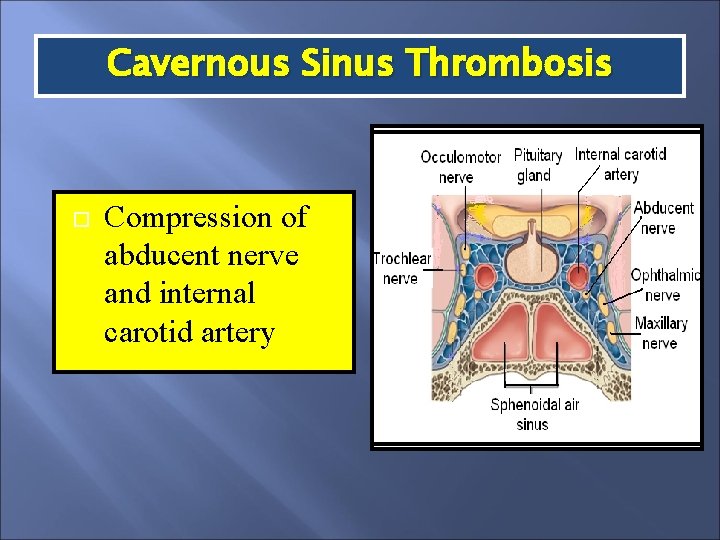
Cavernous Sinus Thrombosis Compression of abducent nerve and internal carotid artery
Clinical tests for Cranial Nerves The integrity of nerves is assessed by examining the: The sensations in the area of distribution Action of muscles Integrity of reflexes Secretory activity of glands
Reflexes Related to Cranial Nerves Pupillary (light) CN 2, 3 Accommodation CN 2, 3 Corneal (Blinking) CN 5, 7 Lacrimation 5, 7 (stimulus may be visual or even thought or emotions) Salivation CN 1, 2, 5, 7, 9 (stimulus may be olfactory, visual, taste, or even thought of food) Sneezing CN 1, 5, 9, 10, 11, phrenic, intercostals Vomiting CN 1, 5, 7, 9 (stimulus may be olfactory, visual, taste, or even thought)
Reflexes Related to Cranial Nerves Yawning CN 5, 7, phrenic, intercostal Swallowing CN 5, 7, 9, 10, 11, 12 Jaw jerk CN 5 Stapedial CN 8, 7 Cough CN 9, 10, 11, phrenic, intercostals Gag CN 9, 10 Carotid sinus reflex CN 9, 10
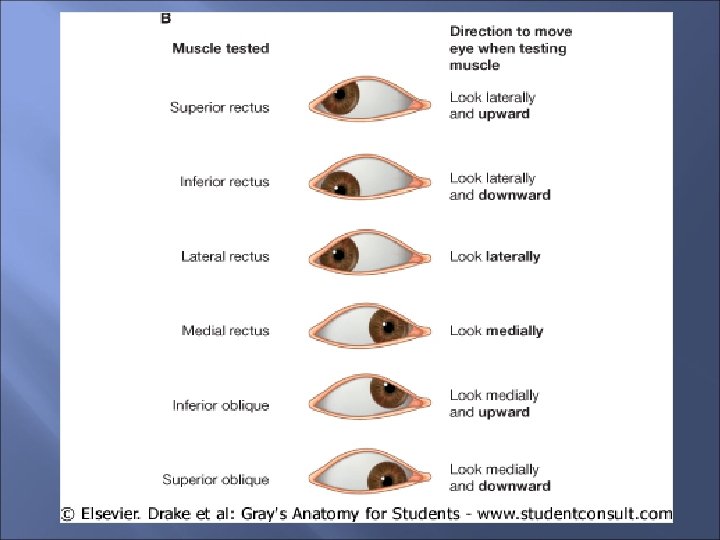
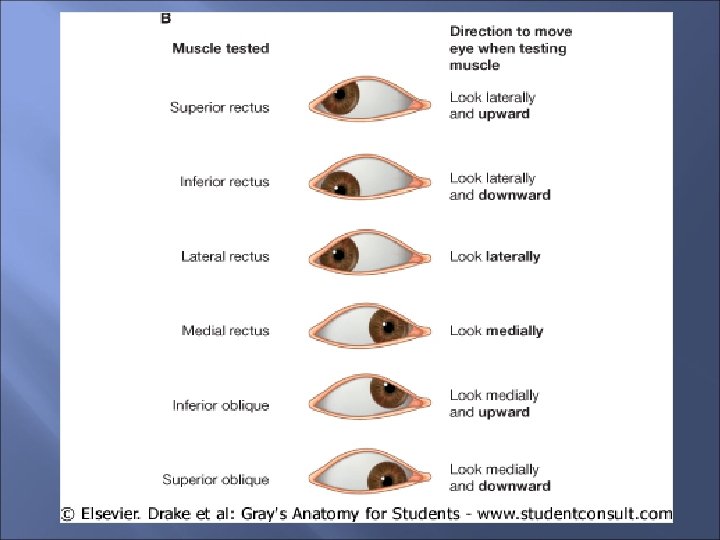
Clinical Tests for Cranial Nerves Olfactory nerve: Ask the patient to identify items with very specific odors, (e. g. . coffee, alcohol, perfume), placed under the nose. Each nostril is tested separately Optic nerve: Ask the patient to read an eye chart. Peripheral vision is tested by detecting object or movement from corners of the eyes Occulomotor nerve: Note the ability to move each eye upward, downward and inward by asking the person to follow a target moved by the examiner. Also examine the constriction of pupil & accommodation
Clinical Tests for Cranial Nerves Trochlear: Note the ability to move each eye downward and inward Trigeminal nerve: General sensations on face are tested by using a pin and a wisp of cotton. Blink reflex is tested by touching the cornea of the eye with a cotton wisp. Strength and action of muscles of mastication are tested by asking the person to clench the teeth and open the jaw against resistance Abducent nerve: Note the ability to move each eye outward beyond the midline
Clinical Tests for Cranial Nerves Facial nerve: The action of muscles of face is tested by asking the person to smile, to open the mouth, to show the teeth, and to close the eyes tightly. Taste sensations from anterior 2/3 tongue is tested using substances that are sweet, sour, salty and bitter Vestibulocochlear nerve: Hearing is tested with a tuning fork. Balance is tested by asking the person to walk on a straight line.
Clinical Tests for Cranial Nerves Glossopharyngeal & Vagus nerves: (cranial part of Accessory nerve) : The person is asked to swallow. The person is asked to say ‘ah-h-h’ to check the movements of palate and uvula. The ‘gag reflex’ is tested by touching the back of the throat by the tongue depressor. The person is asked to speak to check the voice for hoarsness.
Clinical Tests for Cranial Nerves Spinal part of Accessory nerve: The person is asked to turn the head and to shrug the shoulders against resistance provided by the examiner Hypoglossal nerve: The person is asked to stick out the tongue, to observe the deviation to one side or the other