Cranial Nerve Disorders THIRD CRANIAL NERVE PALSIES Partial


- Slides: 30
Cranial Nerve Disorders
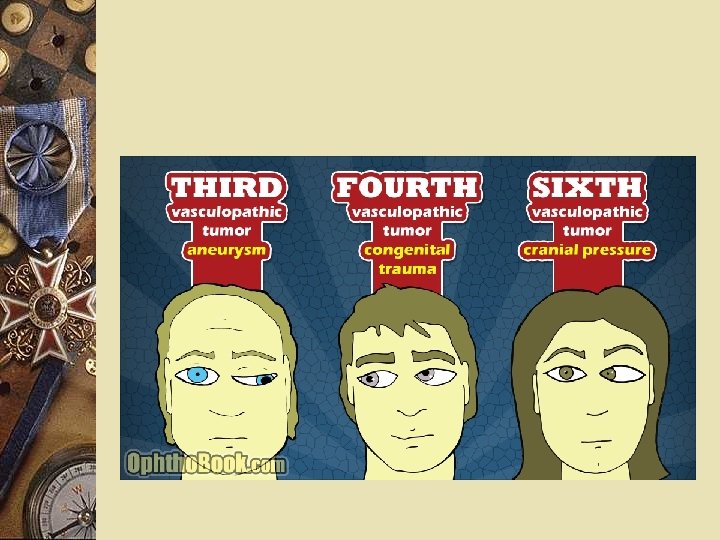
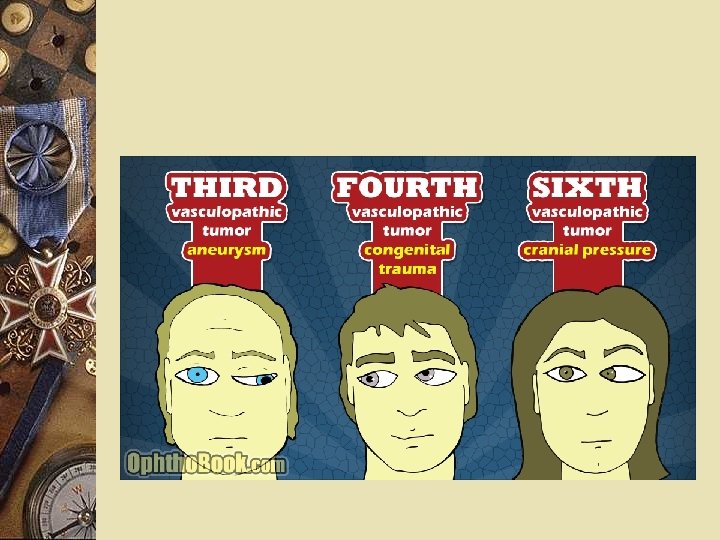
THIRD CRANIAL NERVE PALSIES Partial to complete weakness of the muscles innervated by the 3 rd (oculomotor) nerve When the patient attempts to turn the eye inward, it moves slowly only to the midline. Upward and downward gaze is compromised in the affected eye. When downward gaze is attempted, the superior oblique muscle causes the eye to rotate inward.
Investigation w Third cranial nerve palsies are most indicative of serious disease when associated with severe headache or altered consciousness. w A thorough neurologic examination with CT or MRI is performed. w Lumbar puncture is reserved for suspected subarachnoid hemorrhage when CT does not show blood. w Cerebral angiography must be performed if aneurysm causing subarachnoid hemorrhage is strongly suspected or when the pupil is clearly affected and no head trauma serious enough to fracture the skull has occurred.
FOURTH CRANIAL NERVE PALSIES w Weakness of the muscle innervated by the 4 th (trochlear) nerve (superior oblique muscle). w These palsies are often difficult to detect because they affect vertical eye position predominantly when the eye is turned inward. w The patient sees double images, one above and slightly to the side of the other. However, by tilting the head to the side opposite the palsied muscle, the patient may achieve full or almost full ocular motility without double vision.
SIXTH CRANIAL NERVE PALSIES w Weakness of the muscles innervated by the 6 th (abducens) nerve. w The eye is turned inward; it moves outward sluggishly, reaching the midline at most. w Idiopathic cases are common, although many occur in elderly or diabetic patients in whom small vessel disease may be suspected. In idiopathic cases, no other cranial nerves are involved, and improvement should occur within 2 mo.
TRIGEMINAL NEURALGIA (Tic Douloureux) w A disorder of the trigeminal nerve producing bouts of excruciating, lancinating pain, lasting between seconds and 2 min, along the distribution of one or more of its sensory divisions, most often the maxillary.
FACIAL NERVE DISORDERS w Unilateral facial weakness is a common neurologic sign.
Bell's Palsy w Unilateral facial paralysis of sudden onset and unknown cause. w The mechanism presumably involves swelling of the nerve due to immune or viral disease, with ischemia and compression of the facial nerve in the narrow confines of its course through the temporal bone. w Pain behind the ear may precede facial weakness. Weakness develops within hours, sometimes to complete paralysis. The affected side becomes flat and expressionless, but patients may complain instead about the seemingly twisted intact side. In severe cases, the palpebral fissure widens, and the eye does not close. The patient may complain of a numb or heavy feeling in the face, but no sensory loss is demonstrable. A proximal lesion may affect salivation, taste, and lacrimation and may cause hyperacusis.
GLOSSOPHARYNGEAL NEURALGIA w A rare syndrome characterized by recurrent attacks of severe pain in the posterior pharynx, tonsils, back of the tongue, and middle ear. w The cause is unknown, and no pathologic change can be found (except rarely, when due to a tumor in the cerebellopontine angle or the neck). Men are more commonly affected, usually after age 40. w As in trigeminal neuralgia, intermittent attacks of brief, severe, excruciating pain occur paroxysmally, either spontaneously or precipitated by movement (eg, chewing, swallowing, talking, sneezing). The pain, lasting seconds to a few minutes, usually begins in the tonsillar region or at the base of the tongue and may radiate to the ipsilateral ear. The pain is strictly unilateral. In 1 to 2% of patients, increased vagus nerve activity causes cardiac sinus arrest with syncope. Attacks may be separated by long intervals.
Neuromuscular Disorders
Parkinson’s w Progressive neurodegenerative disease of basal ganglia w Affects 500, 000 in U. S. and 4 million worldwide w Characterized by: – Resting tremors- unilaterally initially – Rigidity – Bradykinesia
Pathophysiology w Lose 9 -13% of dopamine-producing neurons/decade of life w Dopamine has inhibitory effect on excitatory cholinergic neurons (cerebellum) w Dopamine necessary for smooth, coordinated movements
Pathophysiology w Degeneration of substantia nigra and dopamine leads to hyperactivity of cholinergic neurons w Loss of controlled movements
Types of PD w Parkinson’s disease w Parkinsonism – – Post-encephalitic syndrome Side effects of antipsychotic drugs Toxic reaction to a chemical agent Outcome of severe carbon monoxide poisoning
Etiology w Multifactorial w Genetics – mutations on chromosome 6 linked to Lewy body pathology and accumulation of toxic proteins in neurons – Abnormality of gene that protects cells from oxidative stress – Environmental factors – chemicals, toxins/poisons, viruses pesticides and herbicides; oxidative stress
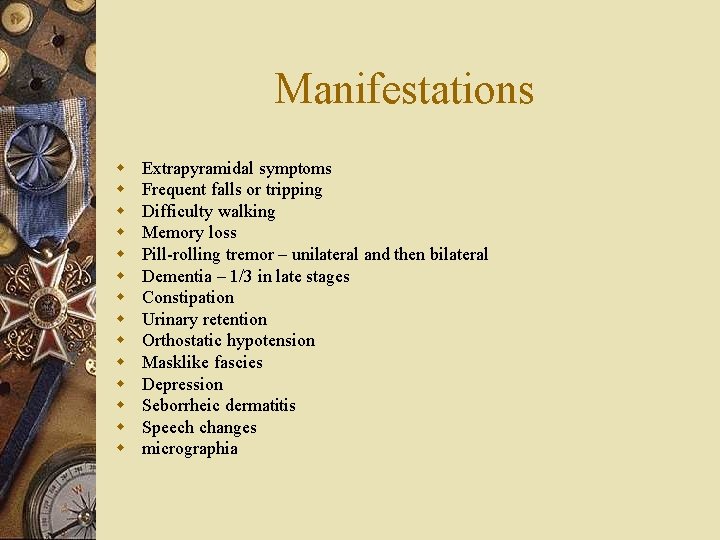
Manifestations w w w w Extrapyramidal symptoms Frequent falls or tripping Difficulty walking Memory loss Pill-rolling tremor – unilateral and then bilateral Dementia – 1/3 in late stages Constipation Urinary retention Orthostatic hypotension Masklike fascies Depression Seborrheic dermatitis Speech changes micrographia
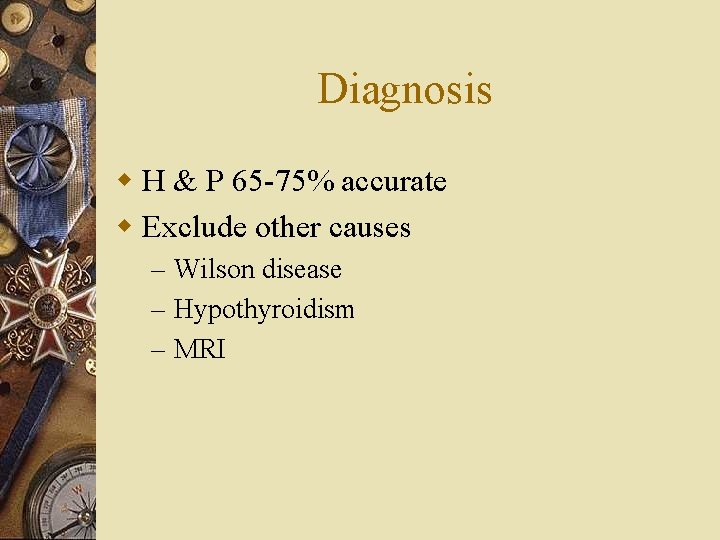
Diagnosis w H & P 65 -75% accurate w Exclude other causes – Wilson disease – Hypothyroidism – MRI

Treatment w Pharmacological – Dopaminergic – Anticholinergic – Augmenting release of dopamine w Surgery w Deep Brain Stimulation w Transplantation
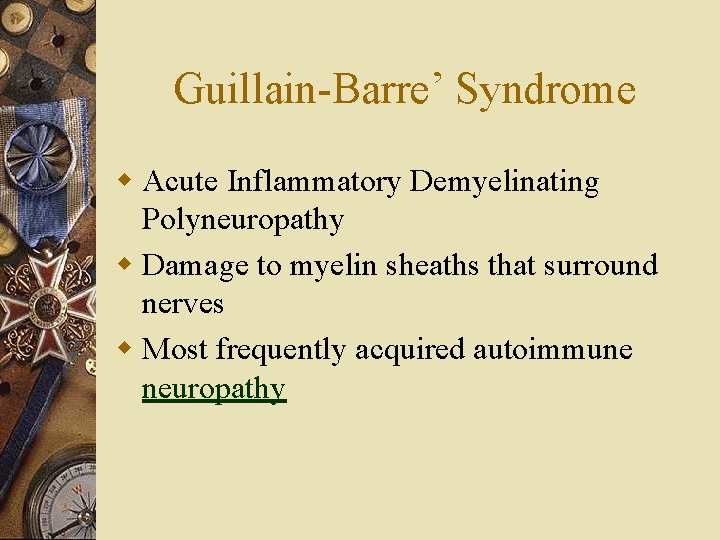
Guillain-Barre’ Syndrome w Acute Inflammatory Demyelinating Polyneuropathy w Damage to myelin sheaths that surround nerves w Most frequently acquired autoimmune neuropathy
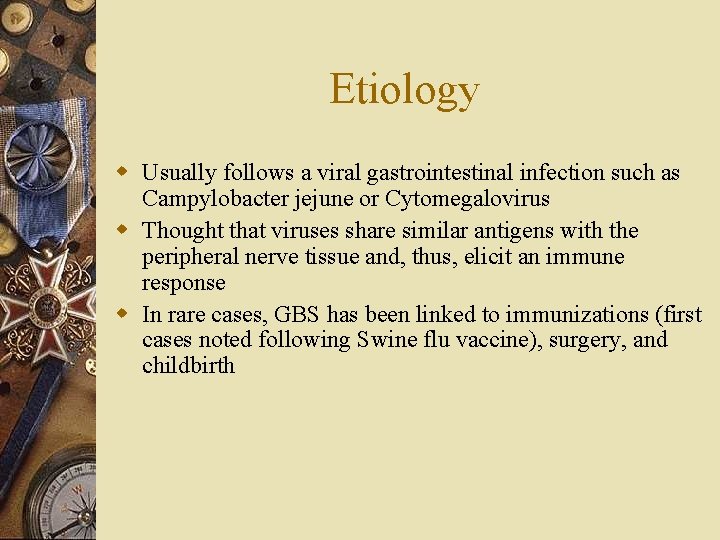
Etiology w Usually follows a viral gastrointestinal infection such as Campylobacter jejune or Cytomegalovirus w Thought that viruses share similar antigens with the peripheral nerve tissue and, thus, elicit an immune response w In rare cases, GBS has been linked to immunizations (first cases noted following Swine flu vaccine), surgery, and childbirth
Signs and Symptoms w Rapid onset of: – Weakness – typically beginning with legs and ascending – Parasthesia – Reflex loss – Breathing may be affected in severe cases (20% require ventilator assistance) – Heart in rare cases
Diagnosis w. H&P w Lumbar puncture – elevated proteins w EMG – excitability of peripheral nerves w Rate of progression varies from patient to patient
Treatment w 80 -90% have spontaneous recovery w Corticosteroids w Immunoglobulin (IVIg) w Plasmaphoresis
Residual effects w 70% full recovery w 20% able to walk, but not run (1 year following onset) w 8% unable to walk unaided (1 year following onset) w 2% bedridden and ventilator dependent (1 year following onset) w May also have some degree of pain, fatigue, and emotional effects
Multiple Sclerosis w Disorder of neurotransmission resulting from demyelination and destruction of axons of motor, sensory, and autonomic nerves w Multifactorial w Autoimmune component – – – Activation of cytotoxic T-cells Macrophages attack myelin Lesions or plaques occur Interruption of nerve transmission Loss or decrease in functioning
Types of MS w Relapsing- remitting w Relapsing-progressive w Chronic progressive
Manifestations w w w w Ataxia Impaired sensation Weakness Numbness Poor coordination Tremors Bowel or bladder problems Spasticity or muscle stiffness Slurred speech Nystagmus Memory problems Visual disturbance paralysis
Diagnosis w History w MRI w Evoked Potential test w In difficult to diagnose patients, LP or MRI scan

Treatment w Beta Interferons ( relapsing-remitting) w Cytotoxic drugs (chronic-progressive) w Steroids (relapsing-progressive) w Symptomatic drugs – Baclofen – Valium