CQM CCDA FHIR Quality Measure Interoperability Solutions www

CQM CCDA FHIR Quality Measure & Interoperability Solutions www. Dynamic. Health. IT. com HL 7®

Clinical Quality Measures: What You Need To Know
Clinical Quality Measures: What You Need to Know Presented by: Jeffery Robbins Raychelle Fernandez President Vice President
Clinical Quality Measures Clinical quality measures (CQMs) are tools that help measure and track the quality of health care services provided by: Eligible Professionals (EPs) Eligible Hospitals Critical Access Hospitals (CAHs)
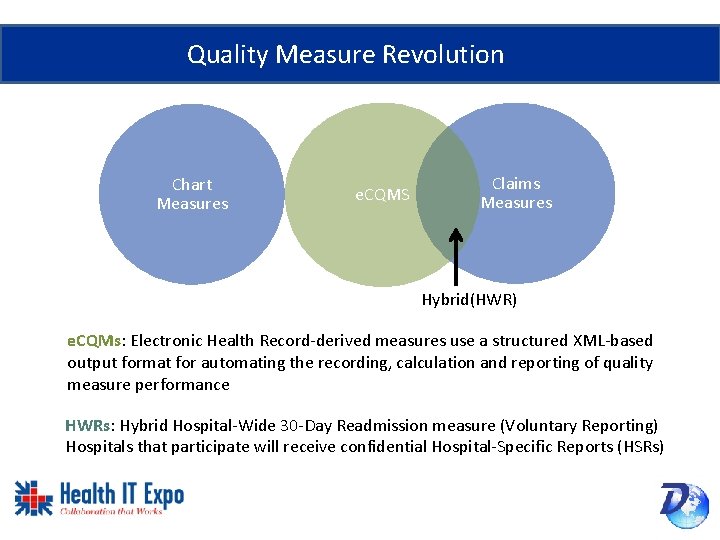
Quality Measure Revolution Chart Measures e. CQMS Claims Measures Hybrid(HWR) e. CQMs: Electronic Health Record-derived measures use a structured XML-based output format for automating the recording, calculation and reporting of quality measure performance HWRs: Hybrid Hospital-Wide 30 -Day Readmission measure (Voluntary Reporting) Hospitals that participate will receive confidential Hospital-Specific Reports (HSRs)
Electronic Clinical Quality Measures (e. CQMs) • e. CQMs used data from ONC Certified EHRs and/or IT systems to measure quality of care • Using e. CQMs is preferable to other reporting methods • For hospitals, required number of e. CQMs now outnumber chart abstracted measures • Required for hospitals since January 2018
Electronic Clinical Quality Measures (e. CQMs) • Data from electronic health records (EHRs) measure quality of healthcare provided • Discrete data elements • No manual intervention to generate output
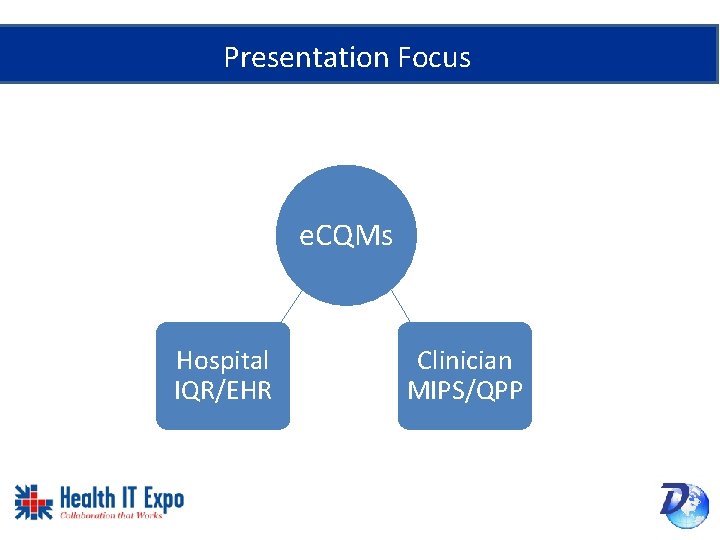
Presentation Focus e. CQMs Hospital IQR/EHR Clinician MIPS/QPP
Audience Poll • Which side are you on? EH EP • What’s your knowledge/experience level? – Beginner – Intermediate – Expert
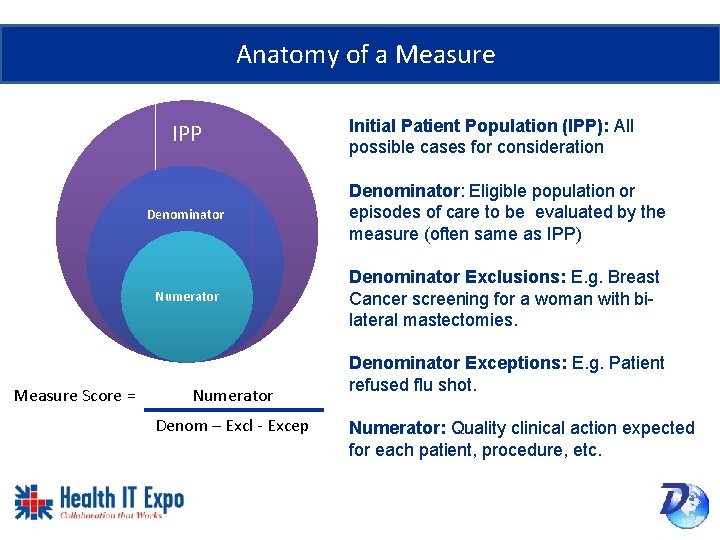
Anatomy of a Measure IPP Measure Score = Initial Patient Population (IPP): All possible cases for consideration Denominator: Eligible population or episodes of care to be evaluated by the measure (often same as IPP) Numerator Denominator Exclusions: E. g. Breast Cancer screening for a woman with bilateral mastectomies. Numerator Denom – Excl - Excep Denominator Exceptions: E. g. Patient refused flu shot. Numerator: Quality clinical action expected for each patient, procedure, etc.
2017 Submission Most popular measures submitted to Joint Commission: 1. e. VTE-1: VTE Prophylaxis (CMS 108) 1. e. VTE-2: ICU VTE Prophylaxis (CMS 190) 2. e. VTE-3: VTE Patients with Anticoagulation Overlap Therapy (CMS 73) Source:
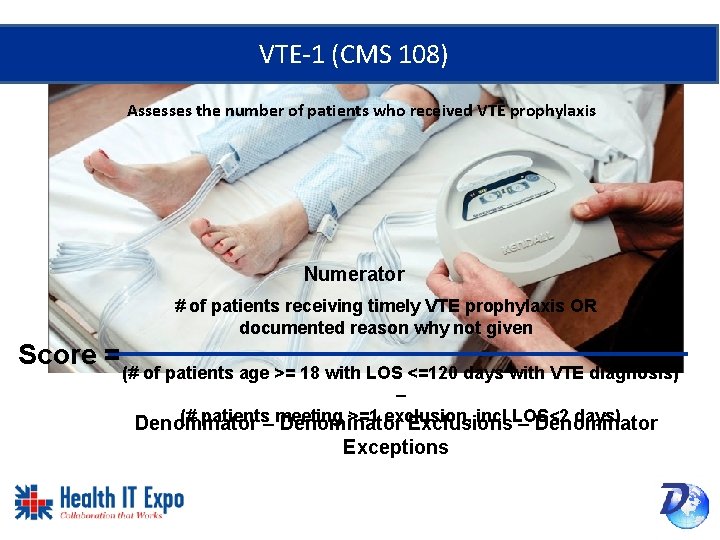
VTE-1 (CMS 108) Assesses the number of patients who received VTE prophylaxis Numerator # of patients receiving timely VTE prophylaxis OR documented reason why not given Score = (# of patients age >= 18 with LOS <=120 days with VTE diagnosis) – (# patients–meeting >=1 exclusion, incl LOS<2 days) Denominator Exclusions – Denominator Exceptions
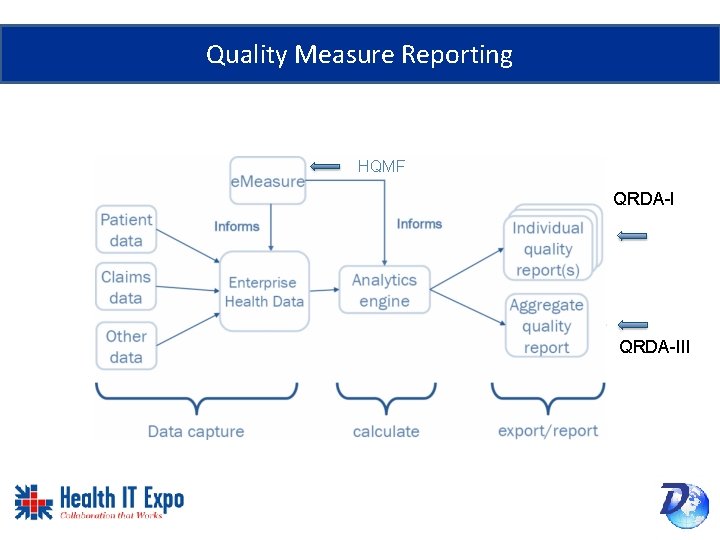
Quality Measure Reporting HQMF QRDA-III
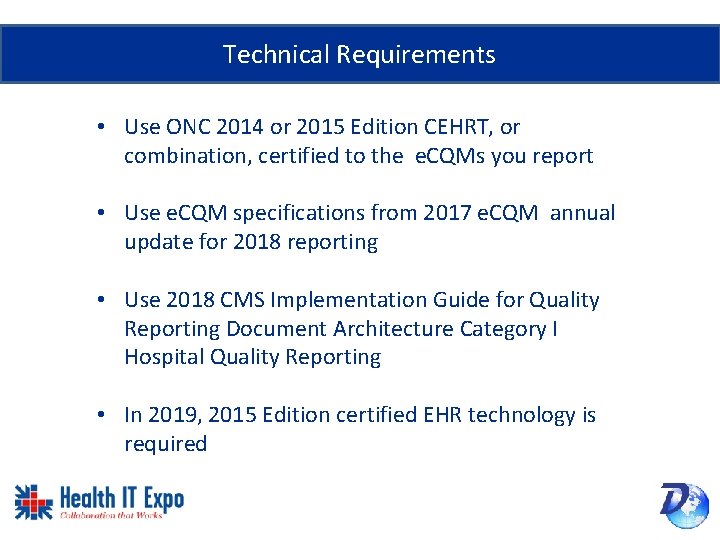
Technical Requirements • Use ONC 2014 or 2015 Edition CEHRT, or combination, certified to the e. CQMs you report • Use e. CQM specifications from 2017 e. CQM annual update for 2018 reporting • Use 2018 CMS Implementation Guide for Quality Reporting Document Architecture Category I Hospital Quality Reporting • In 2019, 2015 Edition certified EHR technology is required

2015 Edition Certified Technology
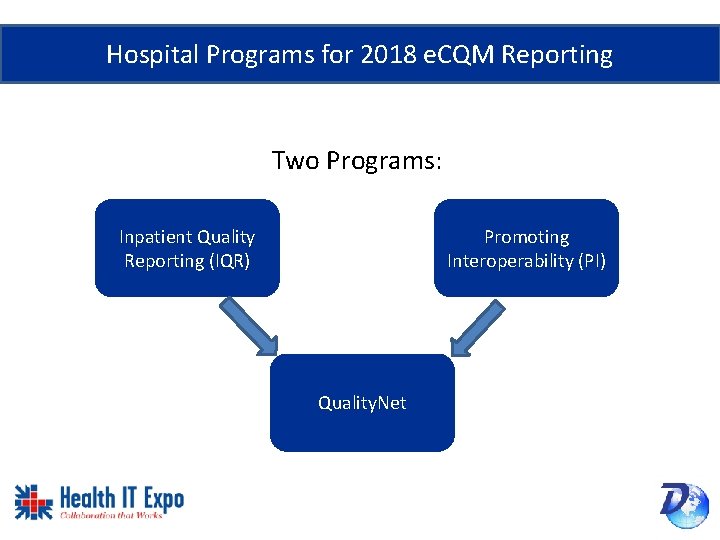
Hospital Programs for 2018 e. CQM Reporting Two Programs: Inpatient Quality Reporting (IQR) Promoting Interoperability (PI) Quality. Net
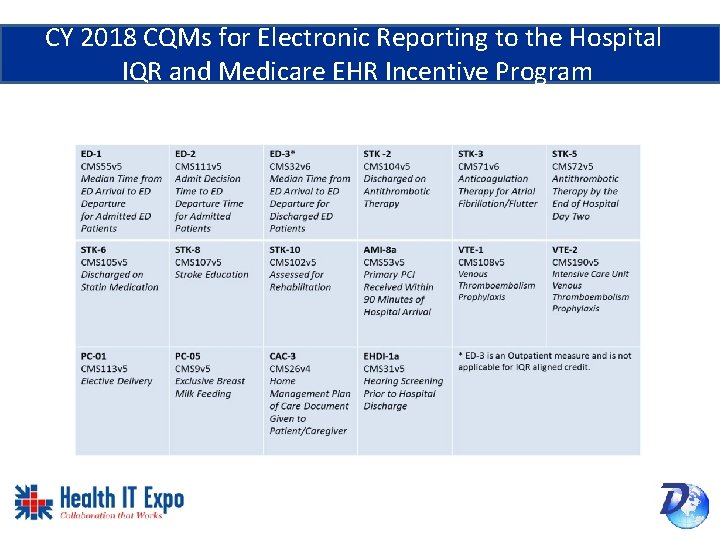
CY 2018 CQMs for Electronic Reporting to the Hospital IQR and Medicare EHR Incentive Program
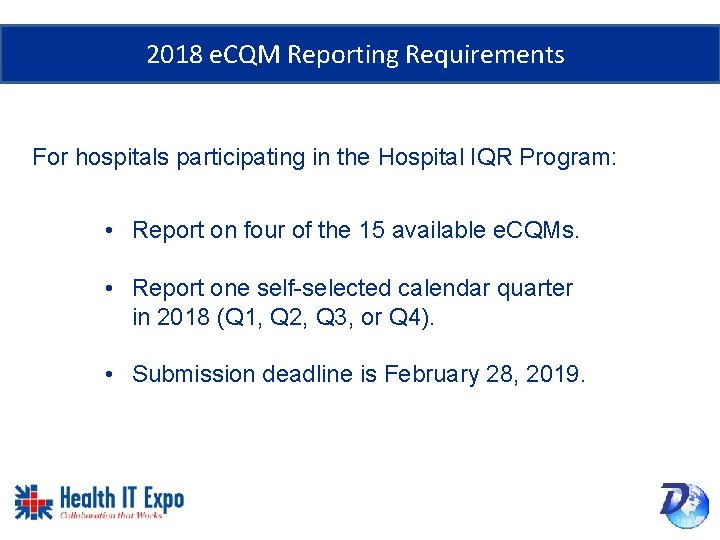
2018 e. CQM Reporting Requirements For hospitals participating in the Hospital IQR Program: • Report on four of the 15 available e. CQMs. • Report one self-selected calendar quarter in 2018 (Q 1, Q 2, Q 3, or Q 4). • Submission deadline is February 28, 2019.
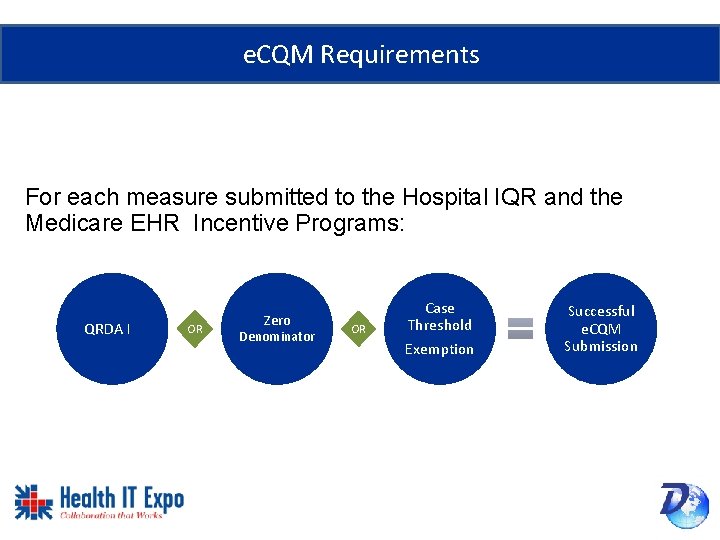
e. CQM Requirements For each measure submitted to the Hospital IQR and the Medicare EHR Incentive Programs: QRDA I OR Zero Denominator OR Case Threshold Exemption Successful e. CQM Submission
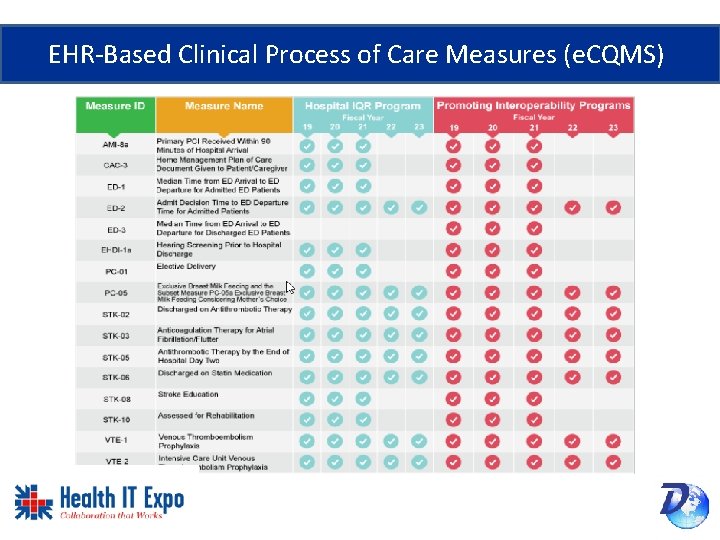
EHR-Based Clinical Process of Care Measures (e. CQMS)
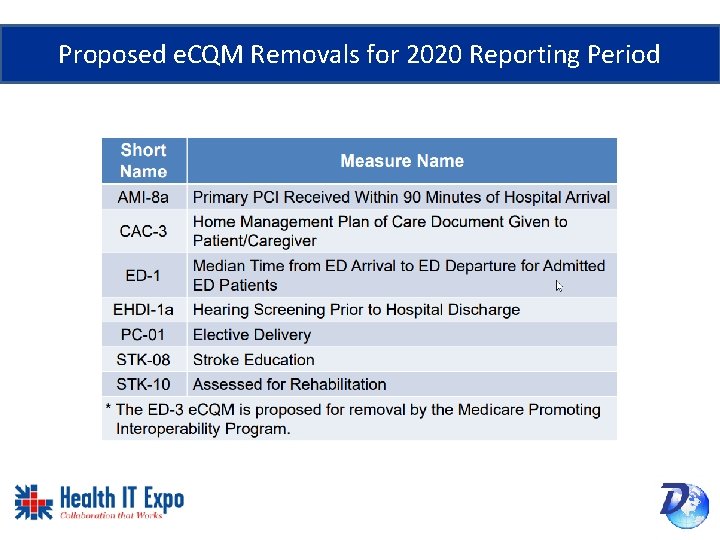
Proposed e. CQM Removals for 2020 Reporting Period
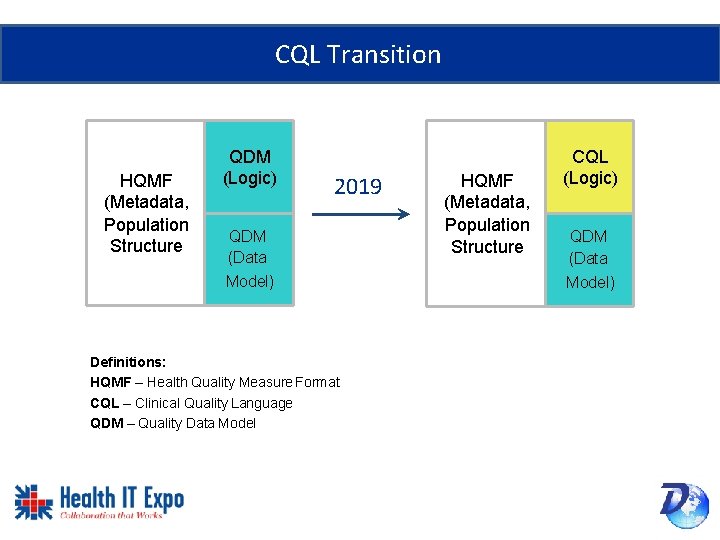
CQL Transition HQMF (Metadata, Population Structure QDM (Logic) 2019 QDM (Data Model) Definitions: HQMF – Health Quality Measure Format CQL – Clinical Quality Language QDM – Quality Data Model HQMF (Metadata, Population Structure CQL (Logic) QDM (Data Model)
Medicare Beneficiary Identifier (MBI) • New 2018 Medicare card no longer displays your social security number • Features Medicare number that is unique to the patient, called a Medicare Beneficiary Identifier (MBI) • The use of the MBI in reporting is an optional data element for 2018 • EMRs should be prepared to capture this identifier
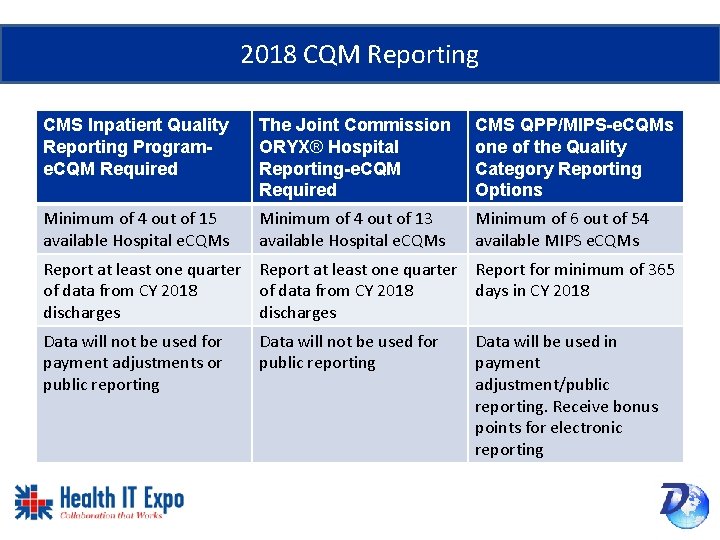
2018 CQM Reporting CMS Inpatient Quality Reporting Programe. CQM Required The Joint Commission ORYX® Hospital Reporting-e. CQM Required CMS QPP/MIPS-e. CQMs one of the Quality Category Reporting Options Minimum of 4 out of 15 available Hospital e. CQMs Minimum of 4 out of 13 available Hospital e. CQMs Minimum of 6 out of 54 available MIPS e. CQMs Report at least one quarter Report for minimum of 365 of data from CY 2018 days in CY 2018 discharges Data will not be used for payment adjustments or public reporting Data will not be used for public reporting Data will be used in payment adjustment/public reporting. Receive bonus points for electronic reporting
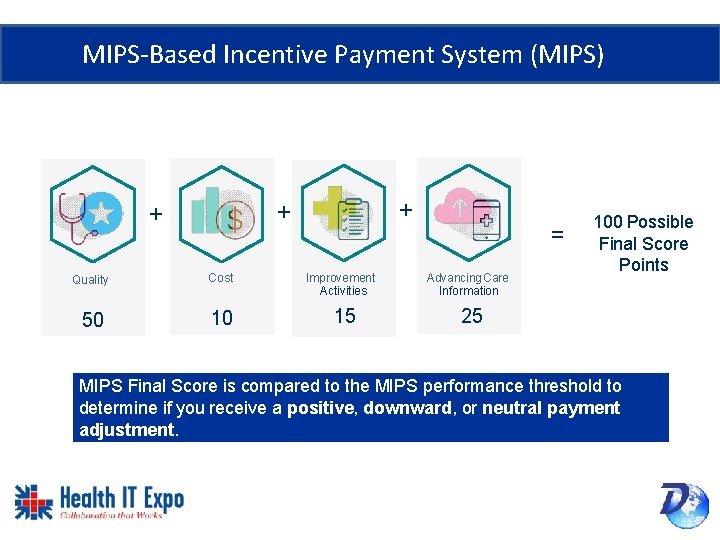
MIPS-Based Incentive Payment System (MIPS) + + + Quality Cost 50 10 Improvement Activities 15 = Advancing Care Information 100 Possible Final Score Points 25 MIPS Final Score is compared to the MIPS performance threshold to determine if you receive a positive, downward, or neutral payment adjustment.
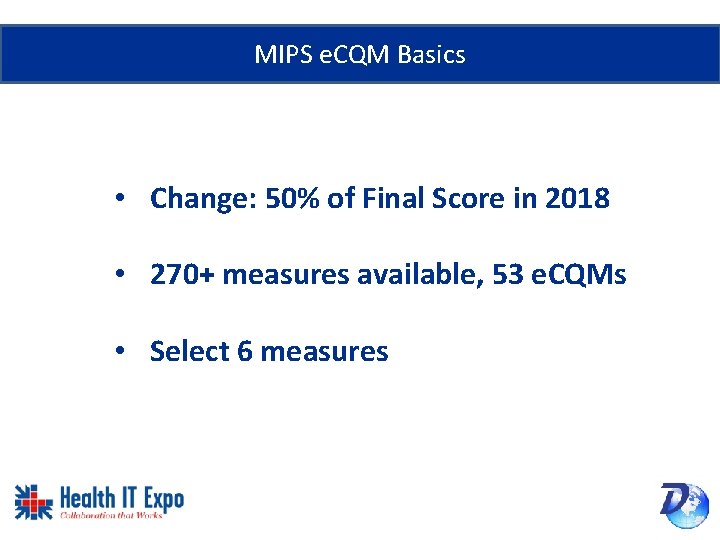
MIPS e. CQM Basics • Change: 50% of Final Score in 2018 • 270+ measures available, 53 e. CQMs • Select 6 measures
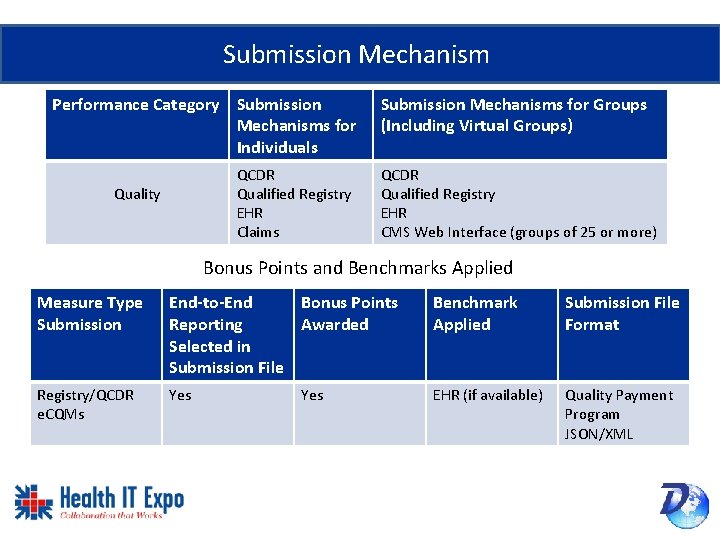
Submission Mechanism Performance Category Submission Mechanisms for Individuals QCDR Qualified Registry EHR Claims Quality Submission Mechanisms for Groups (Including Virtual Groups) QCDR Qualified Registry EHR CMS Web Interface (groups of 25 or more) Bonus Points and Benchmarks Applied Measure Type Submission End-to-End Bonus Points Reporting Awarded Selected in Submission File Benchmark Applied Submission File Format Registry/QCDR e. CQMs Yes EHR (if available) Quality Payment Program JSON/XML Yes
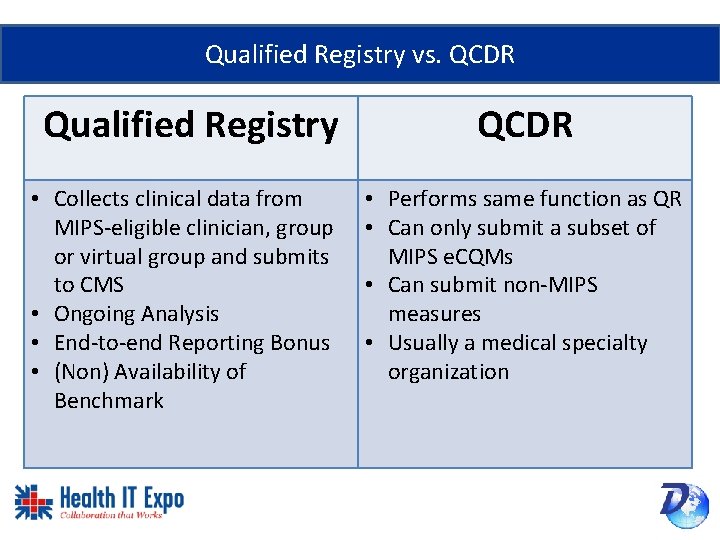
Qualified Registry vs. QCDR Qualified Registry • Collects clinical data from MIPS-eligible clinician, group or virtual group and submits to CMS • Ongoing Analysis • End-to-end Reporting Bonus • (Non) Availability of Benchmark QCDR • Performs same function as QR • Can only submit a subset of MIPS e. CQMs • Can submit non-MIPS measures • Usually a medical specialty organization
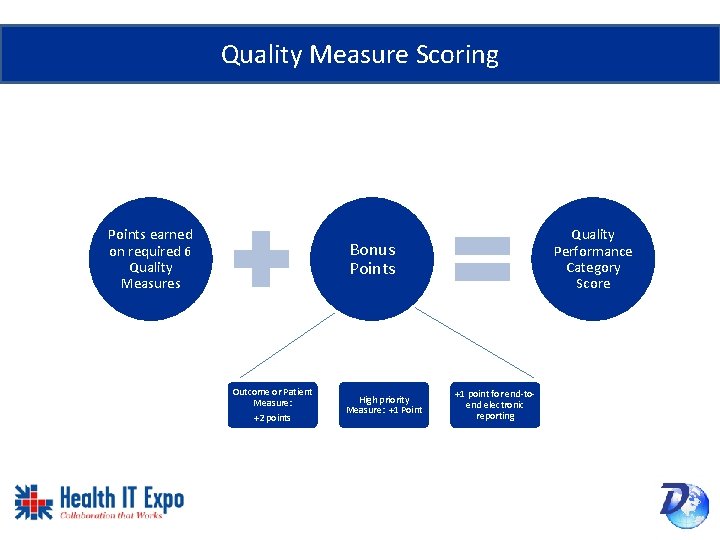
Quality Measure Scoring Points earned on required 6 Quality Measures Quality Performance Category Score Bonus Points Outcome or Patient Measure: +2 points High priority Measure: +1 Point +1 point for end-toend electronic reporting
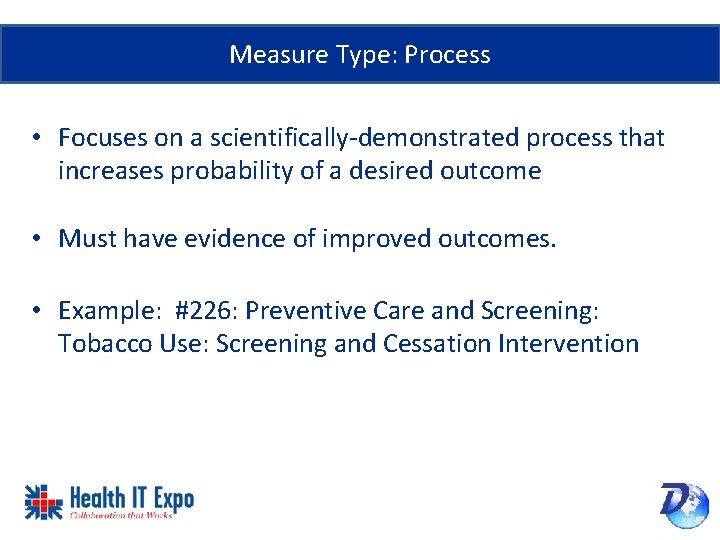
Measure Type: Process • Focuses on a scientifically-demonstrated process that increases probability of a desired outcome • Must have evidence of improved outcomes. • Example: #226: Preventive Care and Screening: Tobacco Use: Screening and Cessation Intervention
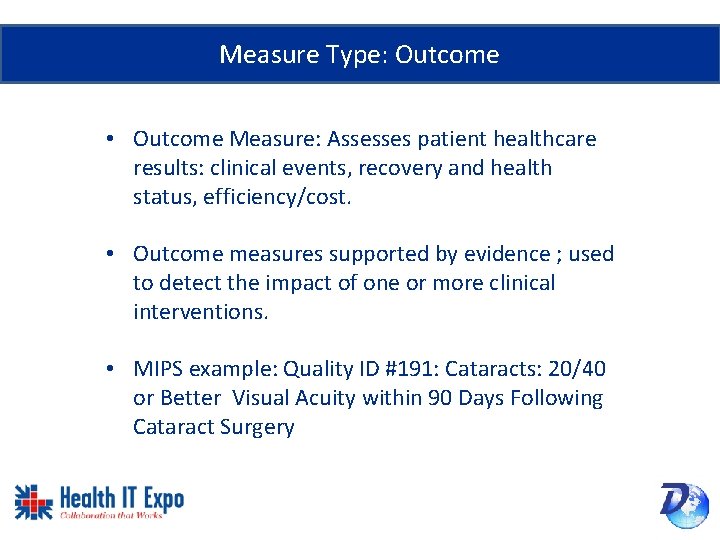
Measure Type: Outcome • Outcome Measure: Assesses patient healthcare results: clinical events, recovery and health status, efficiency/cost. • Outcome measures supported by evidence ; used to detect the impact of one or more clinical interventions. • MIPS example: Quality ID #191: Cataracts: 20/40 or Better Visual Acuity within 90 Days Following Cataract Surgery
Measure Type: High Priority • High-Priority Measure: Addresses national health goal or priority • MIPS quality measure example: Quality ID #238: Use of High-Risk Medications in the Elderly
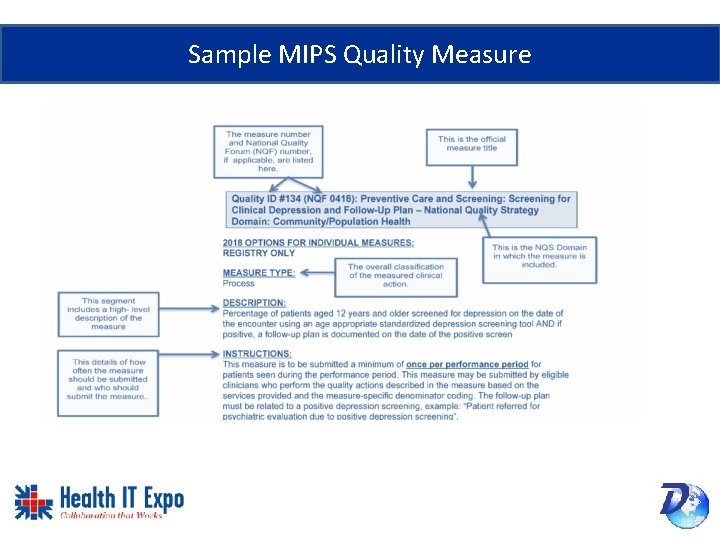
Sample MIPS Quality Measure
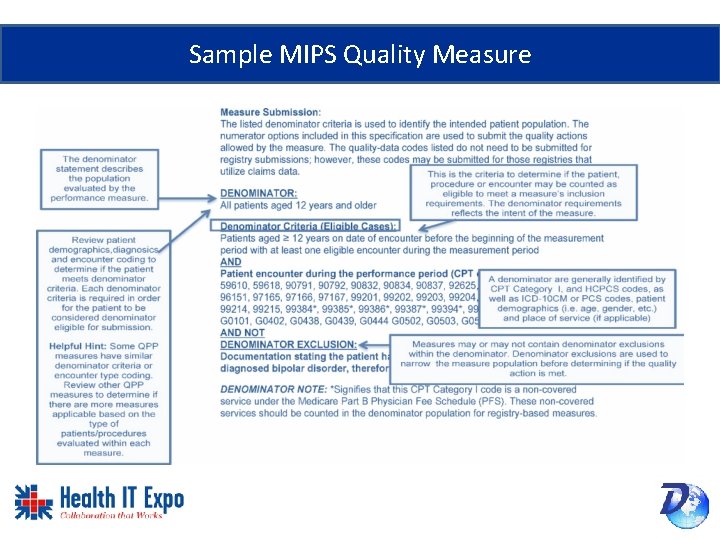
Sample MIPS Quality Measure
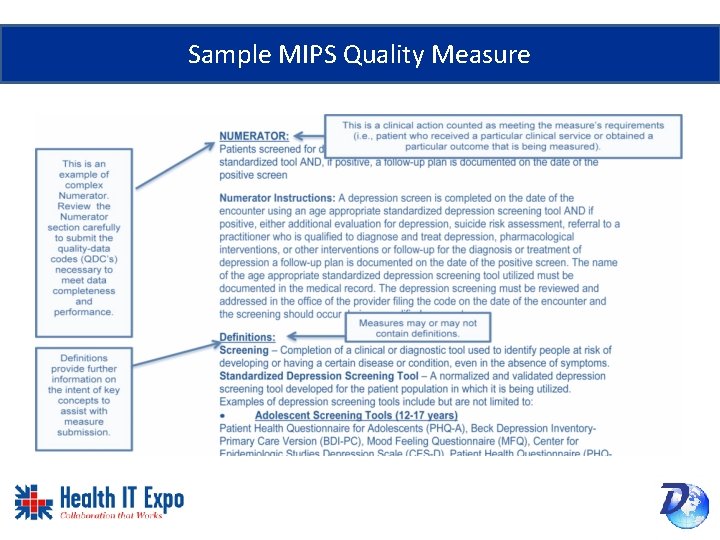
Sample MIPS Quality Measure
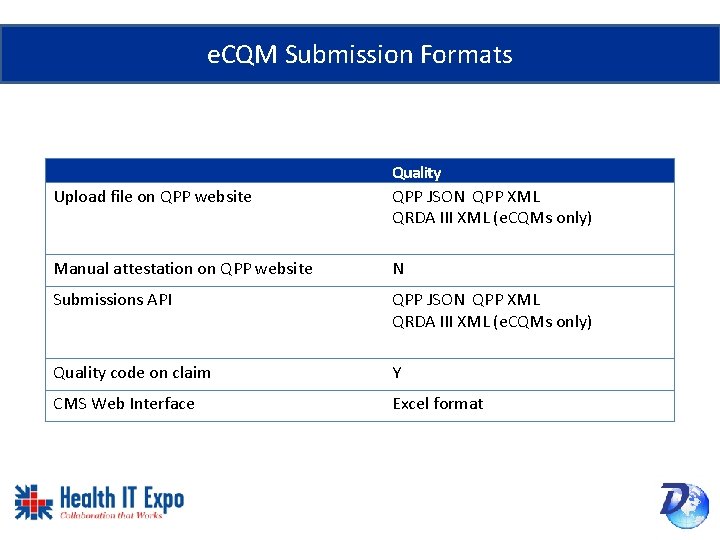
e. CQM Submission Formats Upload file on QPP website Quality QPP JSON QPP XML QRDA III XML (e. CQMs only) Manual attestation on QPP website N Submissions API QPP JSON QPP XML QRDA III XML (e. CQMs only) Quality code on claim Y CMS Web Interface Excel format
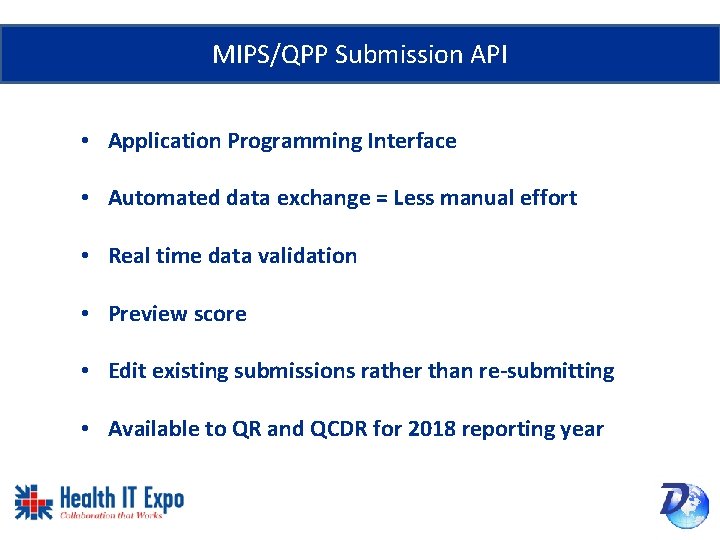
MIPS/QPP Submission API • Application Programming Interface • Automated data exchange = Less manual effort • Real time data validation • Preview score • Edit existing submissions rather than re-submitting • Available to QR and QCDR for 2018 reporting year
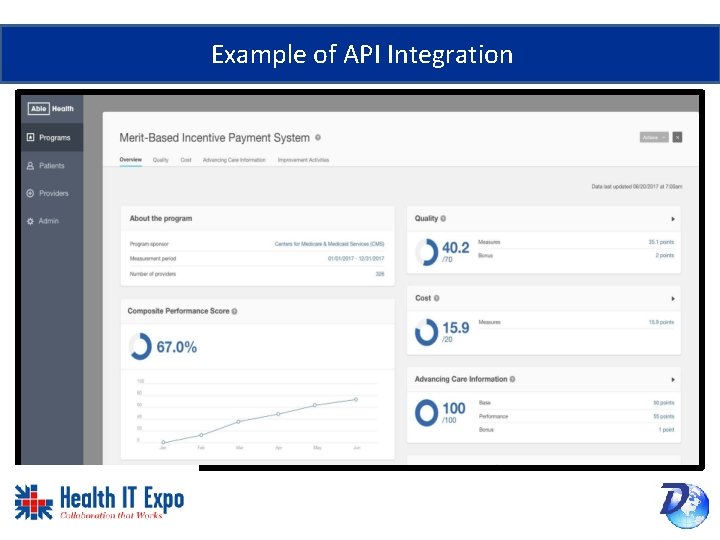
Example of API Integration
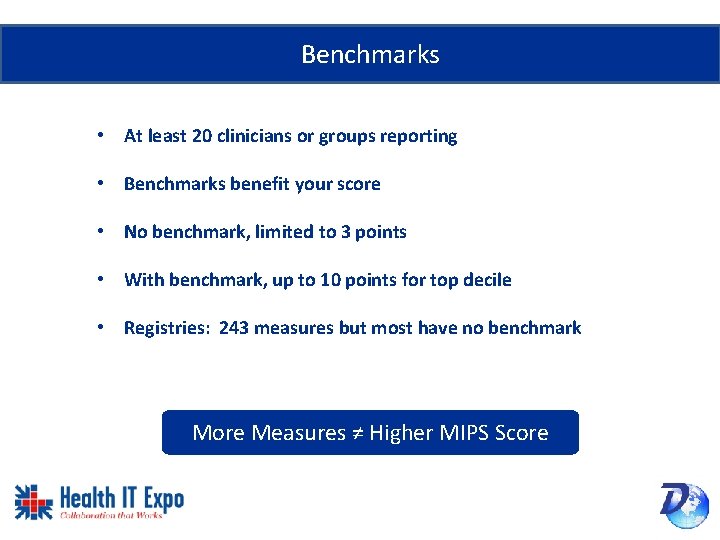
Benchmarks • At least 20 clinicians or groups reporting • Benchmarks benefit your score • No benchmark, limited to 3 points • With benchmark, up to 10 points for top decile • Registries: 243 measures but most have no benchmark More Measures ≠ Higher MIPS Score
Choose Measures Wisely
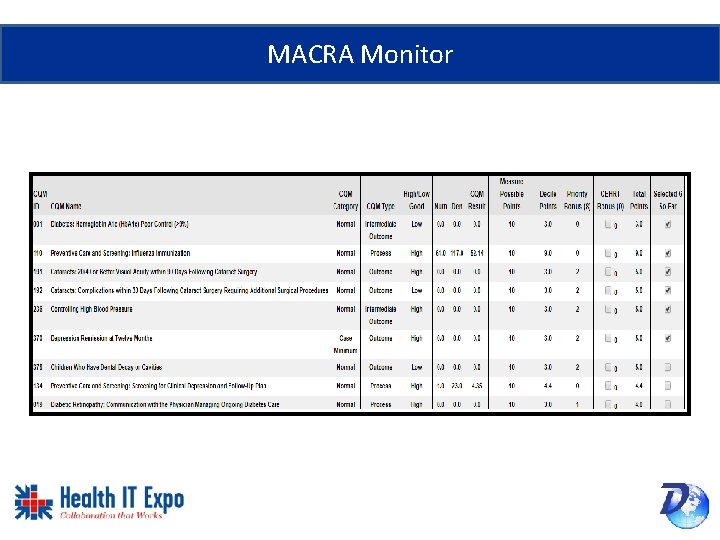
MACRA Monitor
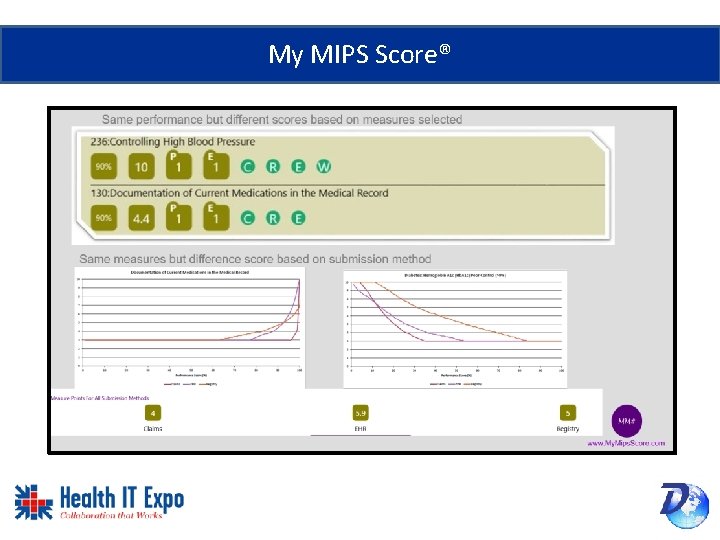
My MIPS Score®
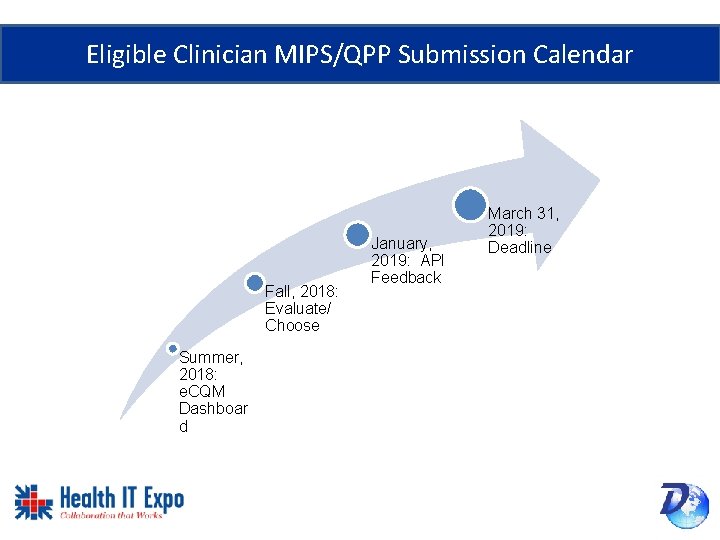
Eligible Clinician MIPS/QPP Submission Calendar Fall, 2018: Evaluate/ Choose Summer, 2018: e. CQM Dashboar d January, 2019: API Feedback March 31, 2019: Deadline
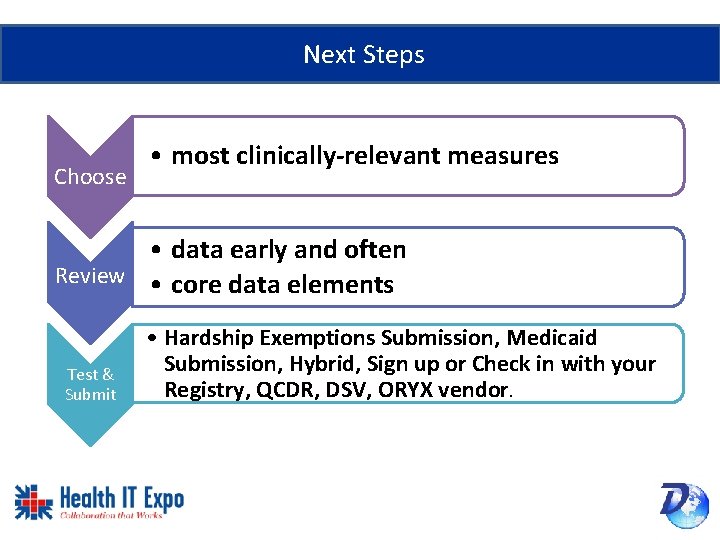
Next Steps Choose • most clinically-relevant measures • data early and often Review • core data elements Test & Submit • Hardship Exemptions Submission, Medicaid Submission, Hybrid, Sign up or Check in with your Registry, QCDR, DSV, ORYX vendor.

Quality Measure & Interoperability Solutions Jeff Robbins jrobbins@dynamichealthit. com @jeffrobbins Raychelle Fernandez raychelle@dynamichealthit. com @raychellefernandez
Resources • DHIT Blog: http: //dynamichealthit. blogspot. com/ • Quality Payment Program Website • https: //qpp. cms. gov/ • Quality Payment Program Resource Library • https: //www. cms. gov/Medicare/Quality-Payment-Program/Resource. Library/Resource-library. html • Quality Payment Program Developer Documentation • https: //qpp. cms. gov/developers • Measure Management System Blueprint • https: //www. cms. gov/Medicare/Quality-Initiatives-Patient-Assessment. Instruments/MMS/Downloads/Blueprint-130. pdf
Resources (cont) • Specs for 2018 submission (hospitals) • Use e. CQM specifications from 2017 e. CQM annual update for 2018 reporting, (see the e. CQI Resource Center website atthttps: //ecqi. healthit. gov/eh • Use 2018 CMS Implementation Guide for Quality Reporting Document Architecture Category I Hospital Quality Reporting, available at https: //ecqi. healthit. gov/qrda. • ONC CHPL (to look up vendor 2015 Edition CEHRT): https: //chpl. healthit. gov/#/search

CQM CCDA FHIR HL 7® Follow us on social media! @Dynamic. Health. IT http: //dynamichealthit. blogspot. com/ @Dynamic. Health. IT www. Dynamic. Health. IT. com
Clinical Quality Measures: Takeaways • e. CQM Submission deadlines: Hospitals February 28, 2019. Clinicians March 31, 2019. • MIPS/QPP: Consider a dashboard with CQM selector/modeling/forecasting. • Avoid topped-out measures and measures slated for elimination. Presented by: Jeffery Robbins & Raychelle Fernandez Dynamic Health IT
- Slides: 49