CPT II Coding for Capturing Quality Measures Gary

- Slides: 33
CPT II Coding for Capturing Quality Measures Gary Lucas, M. Sc. , CPC-I, AHIMA ICD-10 Ambassador Association for Rural & Community Health Professional Coding (ARHPC/ACHPC) Vice President, Education Operations Gary@Rural. Health. Coding. com
Your instructor Gary Lucas, M. Sc. , CPC-I, AHIMA ICD-10 Ambassador ARHPC - Vice President of Education Operations Contact Information Phone: 404 -937 -6633 Email: Gary@Rural. Health. Coding. com Web: http: //www. Rural. Health. Coding. com
Session Objectives Following the presentation, the participants will: 1. Understand the importance of coding CPT II codes to capture quality measures for value based programs 2. Determine the appropriate CPT II codes for a set of quality measures 3. Outline at least three CPT II codes which can be improved in their clinic
DISCLAIMER: CPT® is a registered trademark of the American Medical Association. All rights reserved. Essentially, the AMA owns the CPT code numbers, code definitions, and documentation guidelines from cover-to-cover.
Several other KYPCA presentations help set the foundation for this session • Wednesday - 4: 15 pm – 5: 15 pm – “MACRA: Successfully Navigating the MACRA, MIPS and Quality Payment Program” • Today – 8 am – 9 am – “Improving Performance on Quality Measures: Lessons Learned & Best Practices” • Today – 9: 30 am – 10: 30 am – “Kentucky Medicaid Quality Alignment with MIPS”
Trying to follow all quality measures methods can be a full time job… • MACRA/MIPS/PQRS/HCCs/EIEIOs/BINGOs/etc… – A couple of the above concepts don’t actually exist today – BUT may tomorrow!

Highlights from this Press Release • The Commonwealth is working to with many parties to streamline these “burdensome and often conflicting reporting requirements” • "Every insurer and government program defines quality in their own way. They require different information to be submitted by physicians, which increases administrative burdens and costs, while confusing patients about how the healthcare system defines quality” Source: Accessed on 11/6/2017 at http: //chfs. ky. gov/NR/rdonlyres/9 C 138 A 9 D-689 A 4958 -B 2 B 7 -39 F 56298 C 4 FD/0/nr 092017. pdf
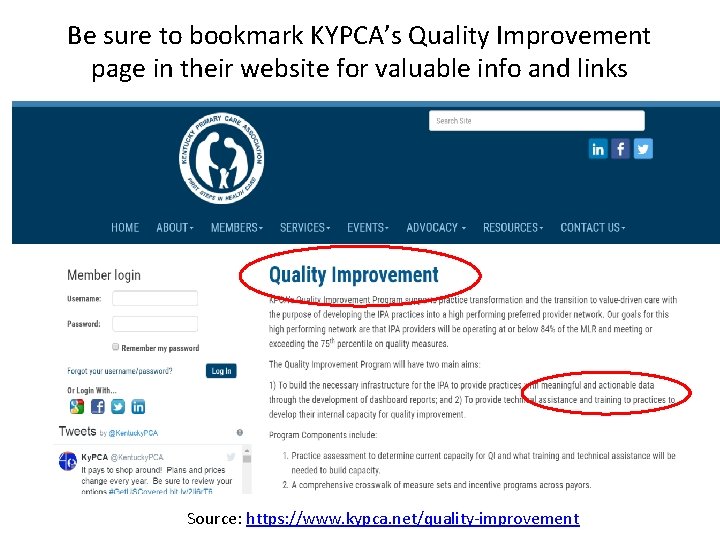
Be sure to bookmark KYPCA’s Quality Improvement page in their website for valuable info and links Source: https: //www. kypca. net/quality-improvement
There are several ways to measure “quality” • Consistent and accurate usage of ICD-10 -CM diagnosis codes allows a clear understanding to patients, your facility, your payers, and public health on the status of your patient’s conditions. – ICD-10 -CM is the “what do the patients have” piece and can be reported via ICD-10 -CM for Hierarchal Condition Coding (HCCs) and determining your Risk Adjustment levels that can raise or lower your managed care payments.
There are several ways to measure “quality” • Our focus in this session will be the “what did we do” piece that will utilize a part of the CPT that is not often used or understood by even the most experienced coder/biller/provider/manager called HCPCS Level 1 Category 2 codes. – Generically these are called “CPT 2” codes that end with the letter “F” - NOT to be confused with HCPCS Level 2 codes that begin with alphabetic letters. – “Dare to dream” – one day EHRs will be able to auto-extract these codes for reporting to carriers who want the information. – Let’s spend some time digging deeply into what the CPT tells us about these “supplemental tracking codes. ”
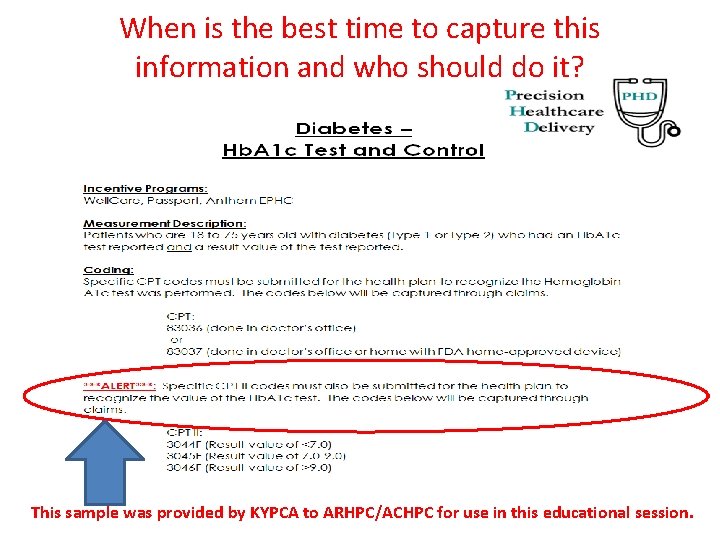
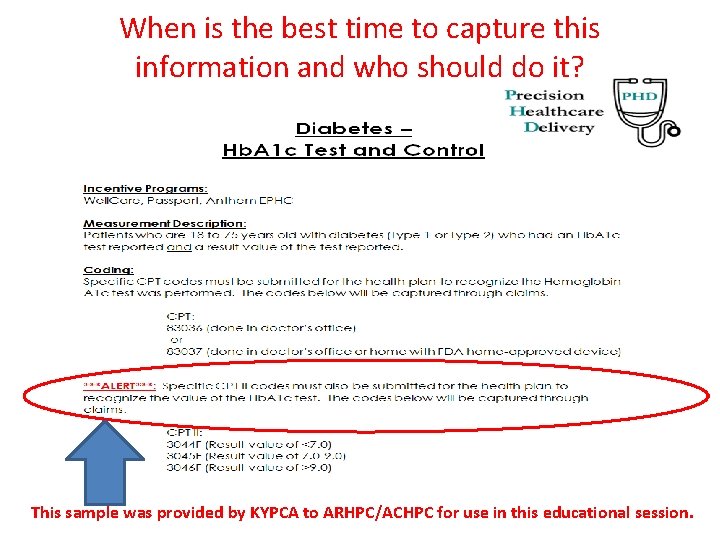
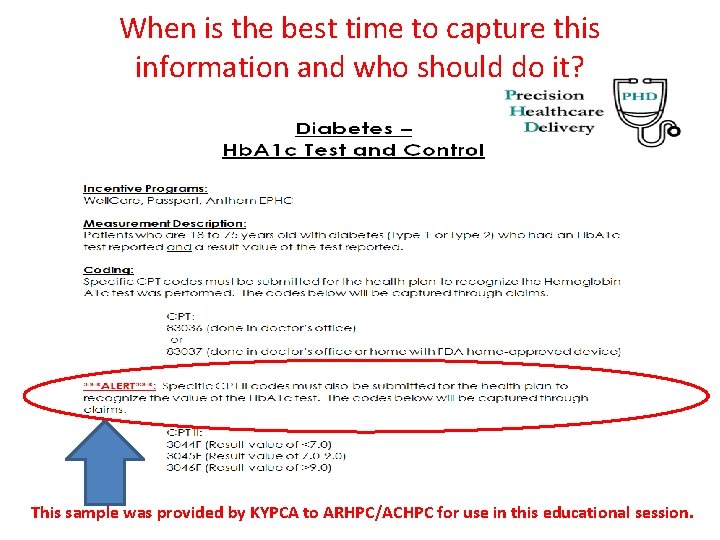
When is the best time to capture this information and who should do it? This sample was provided by KYPCA to ARHPC/ACHPC for use in this educational session.
When do we need to list Category II codes? • It will be highly variable by facility and is primarily based on your participation agreements with Medicare Advantage, Medicaid Managed Care, and commercial plans who may “require” or “encourage” this type of reporting. • In a perfect world, your EHR vendor can design modules that automagically pulls such key data from your completed medical encounter such as BMI being calculated or tobacco-use assessment performed. Good luck! • What they are really trying to determine is a ratio of how many eligible people got “X” of who is considered “eligible”. – 0% through 100% with a targeted amount or minimum threshold to be reached that will impact future payment rates or incentive monies. – This can be done at an individual provider level, for an entire facility, or for an entire network or facility type (ex. FQHCs in a county/state)
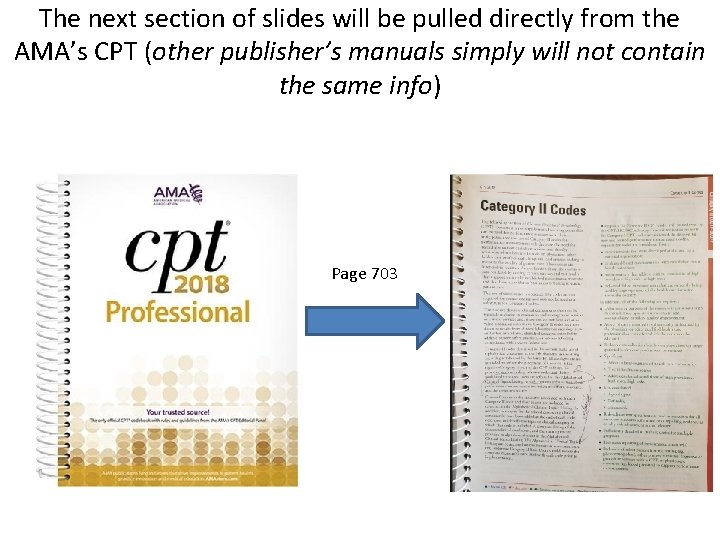
The next section of slides will be pulled directly from the AMA’s CPT (other publisher’s manuals simply will not contain the same info) Page 703
Know the main CPT source material well! • “The following section of Current Procedural Terminology (CPT) contains a set of supplemental tracking codes that can be used for performance measurement” • “It is anticipated that the use of Category II codes for performance measurement will decrease the need for record abstraction and chart review, and thereby minimize administrative burden on physicians…. and entities seeking to measure the quality of patient care. ” • “These codes are intended to facilitate data collection about the quality of care rendered by coding certain services and test results that support nationally established performance measures and that have an evidence base as contributing to quality patient care. ”
Know the main CPT source material well! • “The use of these codes is optional. The codes are not required for correct coding and may not be used as a substitute for Category I codes. ” • “These codes describe clinical components that may be typically included in (E/M) services or clinical services, and therefore, do not have any a relative value associated with them. ” • “Category II codes may also describe results from clinical laboratory or radiology tests and other procedures…or services reflecting compliance with state or federal law. ”
Know the main CPT source material well! • “To promote understanding of these codes and their associate users are referred to the Alphabetical Clinical Topics Listing, which contains information about performance measurement exclusion modifiers, measures, and the measure’s source. ” • “Cross-references to the measures associated with each Category II code and their source are included for reference in the Alphabetical Clinical Topics Listing…. (via) www. ama-assn. org” • “Users should review the complete measure(s) associated with each code prior to implementation” – Get them from the AMA list AND the carrier that requires them!!!
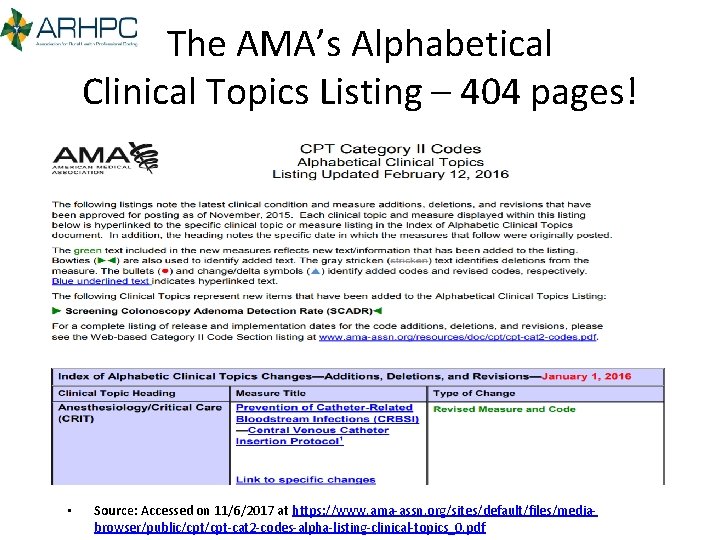
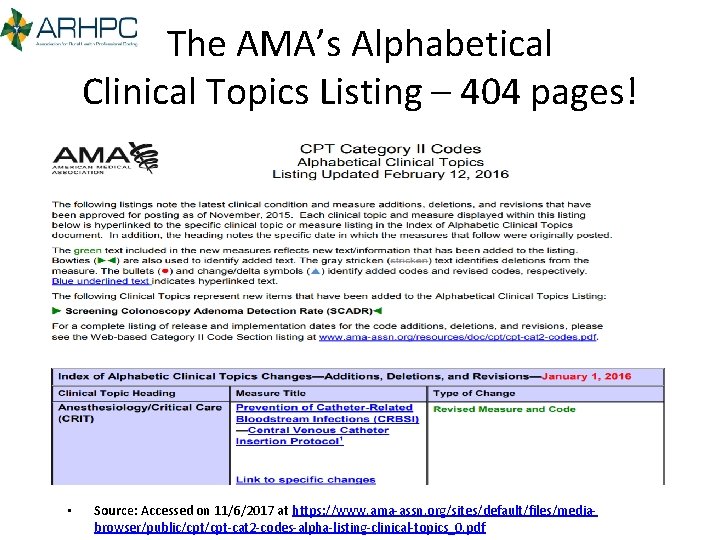
The AMA’s Alphabetical Clinical Topics Listing – 404 pages! • Source: Accessed on 11/6/2017 at https: //www. ama-assn. org/sites/default/files/mediabrowser/public/cpt-cat 2 -codes-alpha-listing-clinical-topics_0. pdf
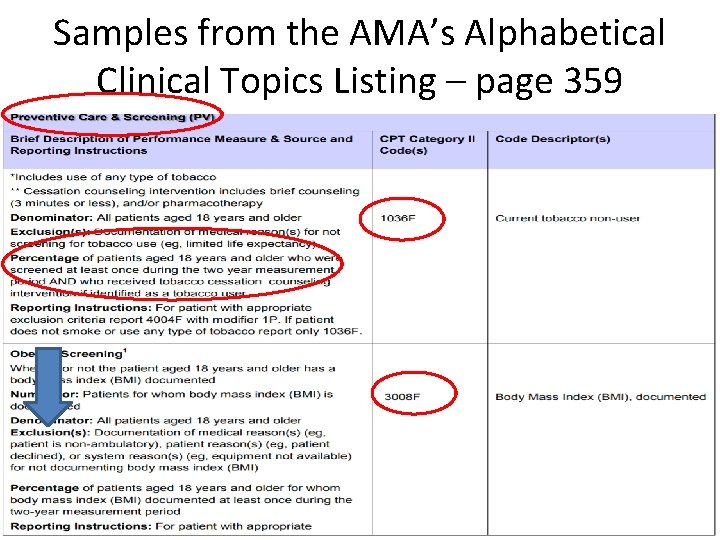
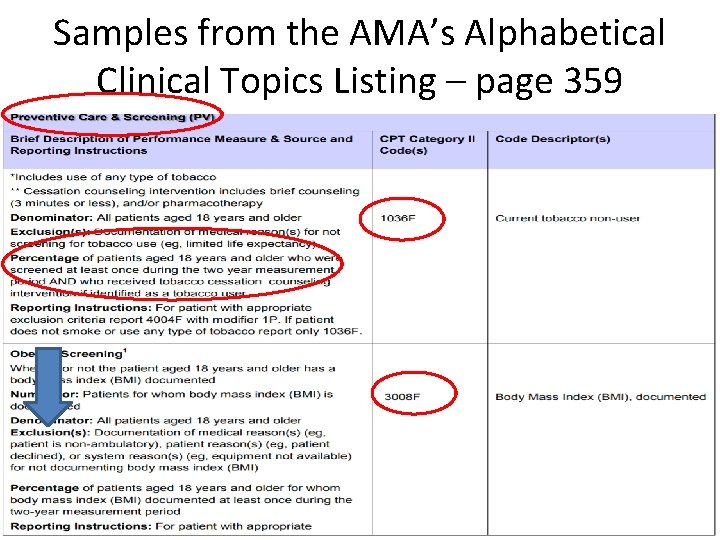
Samples from the AMA’s Alphabetical Clinical Topics Listing – page 359
Medicare’s PQRS Guide has helpful information also! • Source: https: //www. cms. gov/Medicare/Quality-Initiatives-Patient-Assessment. Instruments/PQRS/Downloads/2016 PQRS_Claims_Coding. Rpg. Princ. pdf
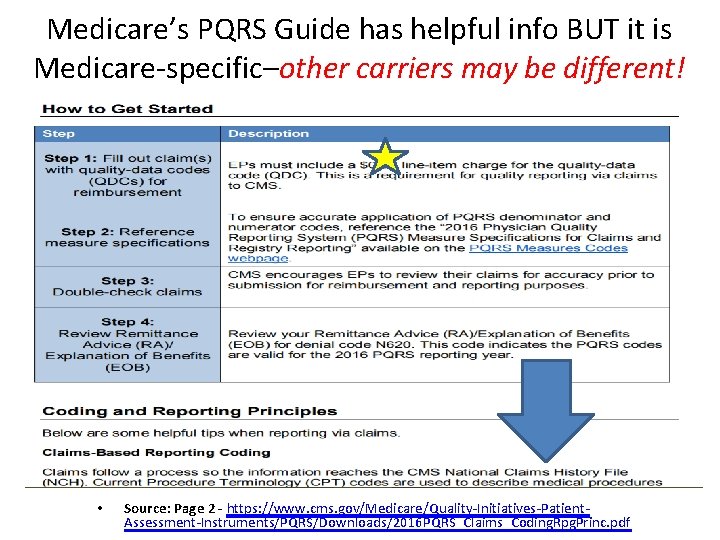
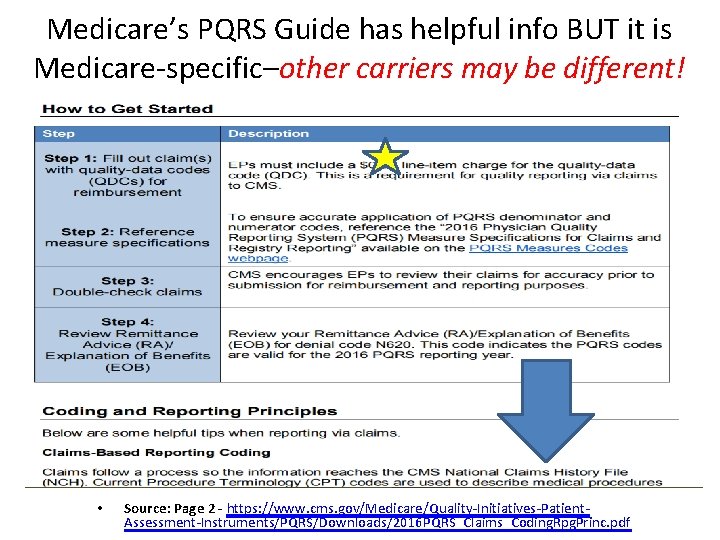
Medicare’s PQRS Guide has helpful info BUT it is Medicare-specific–other carriers may be different! • Source: Page 2 - https: //www. cms. gov/Medicare/Quality-Initiatives-Patient. Assessment-Instruments/PQRS/Downloads/2016 PQRS_Claims_Coding. Rpg. Princ. pdf
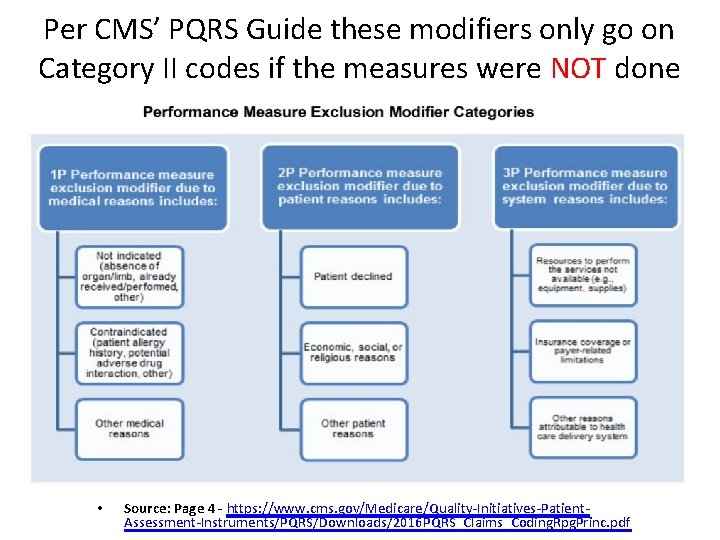
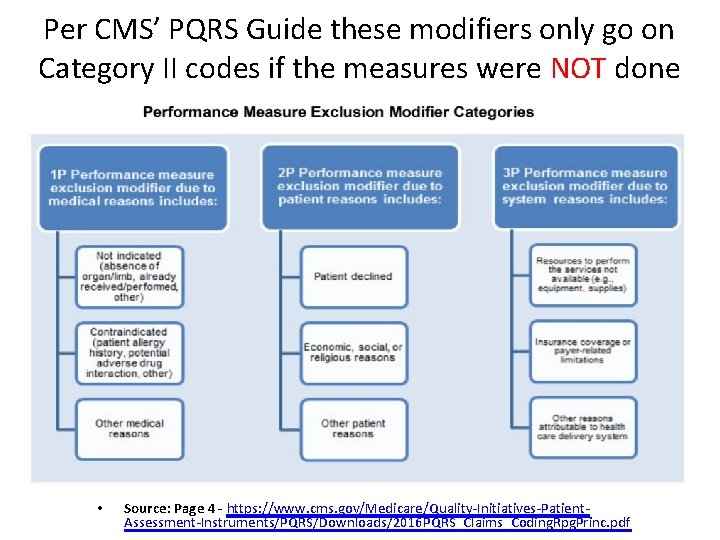
Per CMS’ PQRS Guide these modifiers only go on Category II codes if the measures were NOT done • Source: Page 4 - https: //www. cms. gov/Medicare/Quality-Initiatives-Patient. Assessment-Instruments/PQRS/Downloads/2016 PQRS_Claims_Coding. Rpg. Princ. pdf
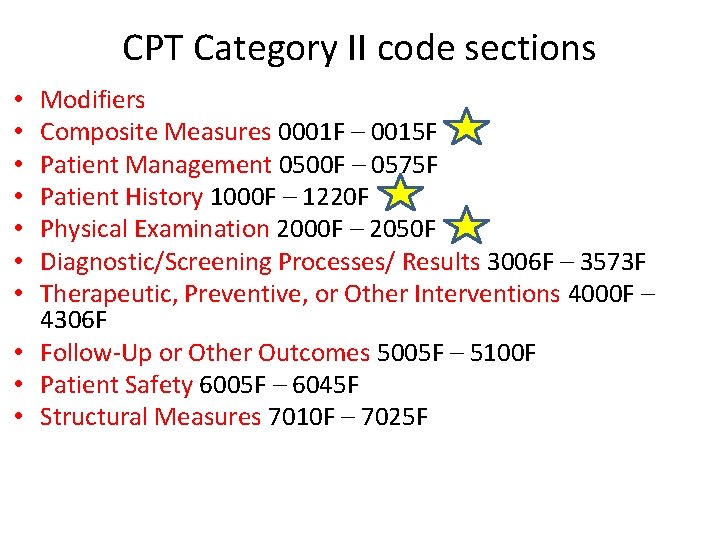
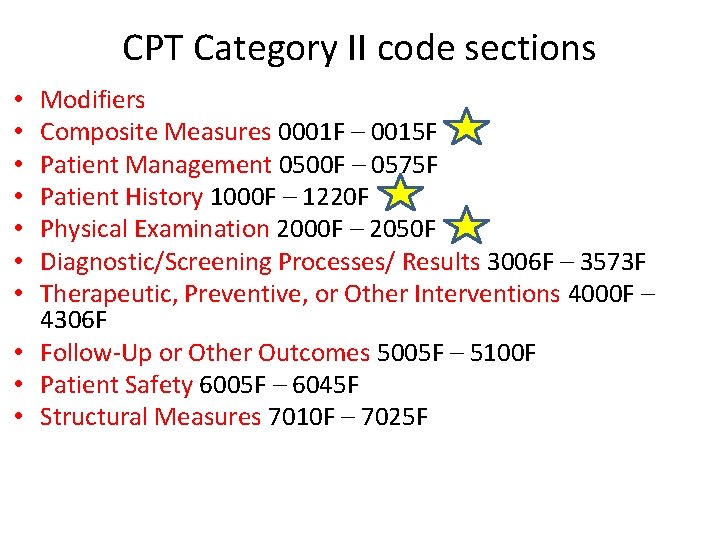
CPT Category II code sections Modifiers Composite Measures 0001 F – 0015 F Patient Management 0500 F – 0575 F Patient History 1000 F – 1220 F Physical Examination 2000 F – 2050 F Diagnostic/Screening Processes/ Results 3006 F – 3573 F Therapeutic, Preventive, or Other Interventions 4000 F – 4306 F • Follow-Up or Other Outcomes 5005 F – 5100 F • Patient Safety 6005 F – 6045 F • Structural Measures 7010 F – 7025 F • •
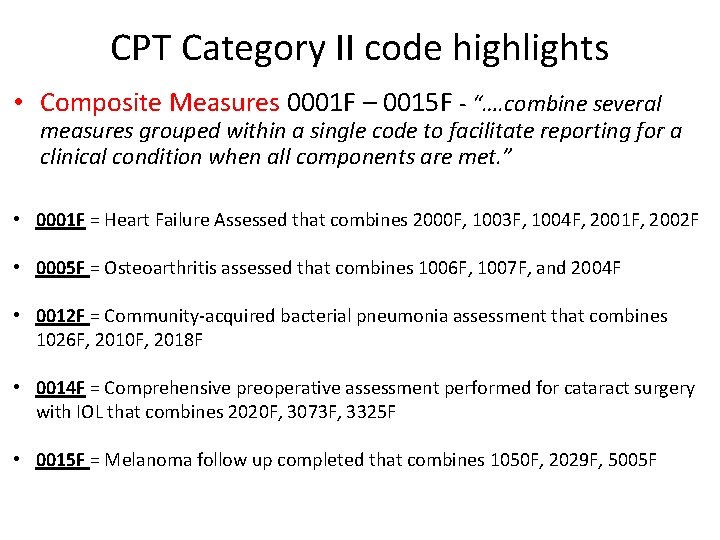
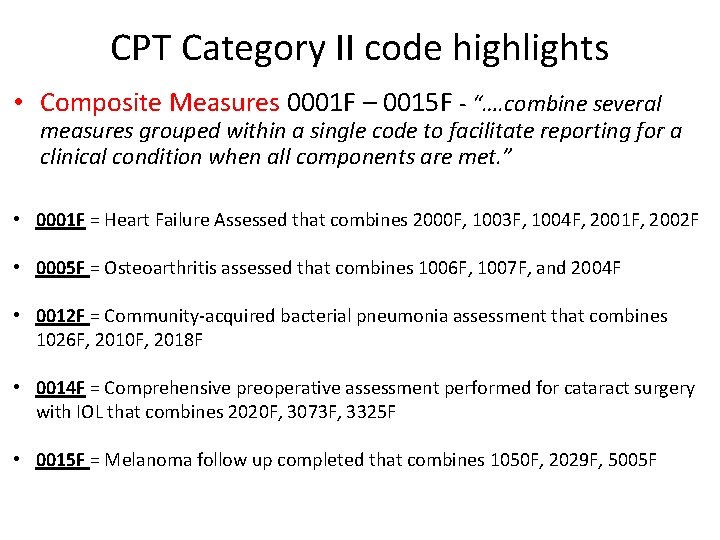
CPT Category II code highlights • Composite Measures 0001 F – 0015 F - “…. combine several measures grouped within a single code to facilitate reporting for a clinical condition when all components are met. ” • 0001 F = Heart Failure Assessed that combines 2000 F, 1003 F, 1004 F, 2001 F, 2002 F • 0005 F = Osteoarthritis assessed that combines 1006 F, 1007 F, and 2004 F • 0012 F = Community-acquired bacterial pneumonia assessment that combines 1026 F, 2010 F, 2018 F • 0014 F = Comprehensive preoperative assessment performed for cataract surgery with IOL that combines 2020 F, 3073 F, 3325 F • 0015 F = Melanoma follow up completed that combines 1050 F, 2029 F, 5005 F
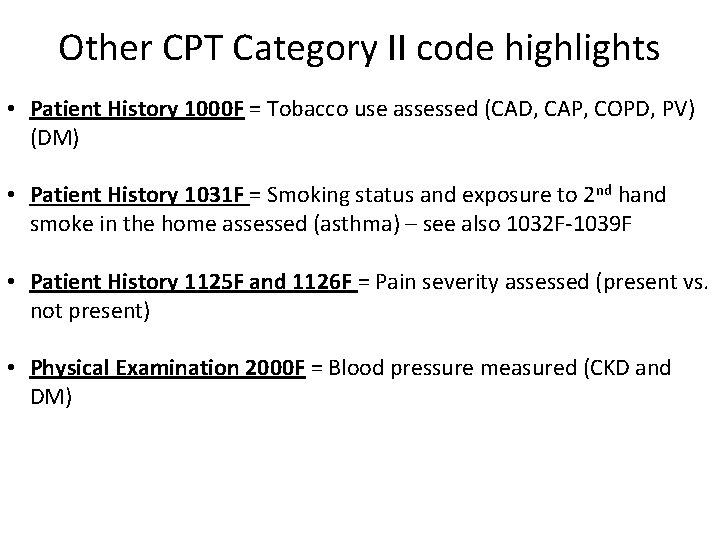
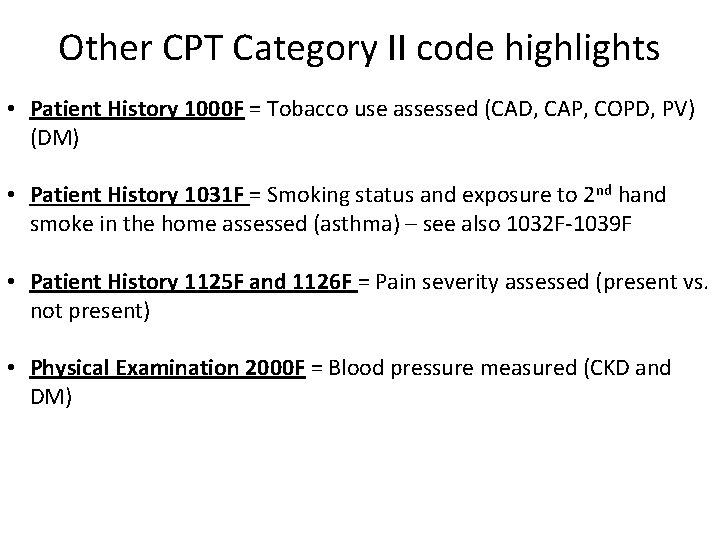
Other CPT Category II code highlights • Patient History 1000 F = Tobacco use assessed (CAD, CAP, COPD, PV) (DM) • Patient History 1031 F = Smoking status and exposure to 2 nd hand smoke in the home assessed (asthma) – see also 1032 F-1039 F • Patient History 1125 F and 1126 F = Pain severity assessed (present vs. not present) • Physical Examination 2000 F = Blood pressure measured (CKD and DM)
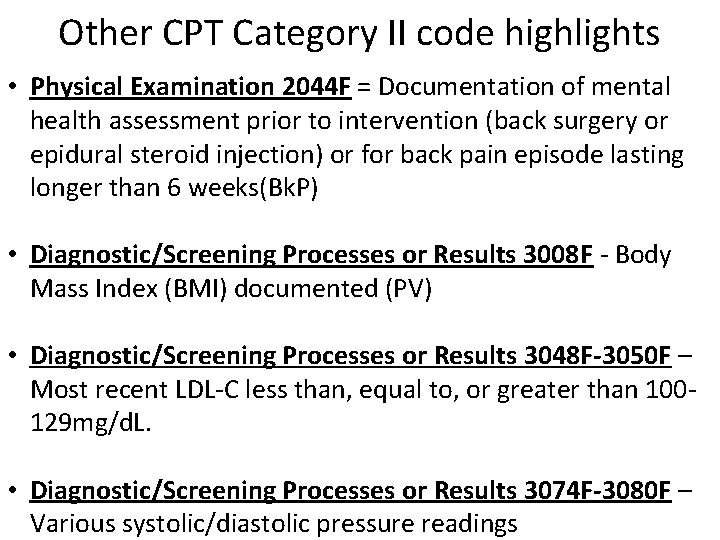
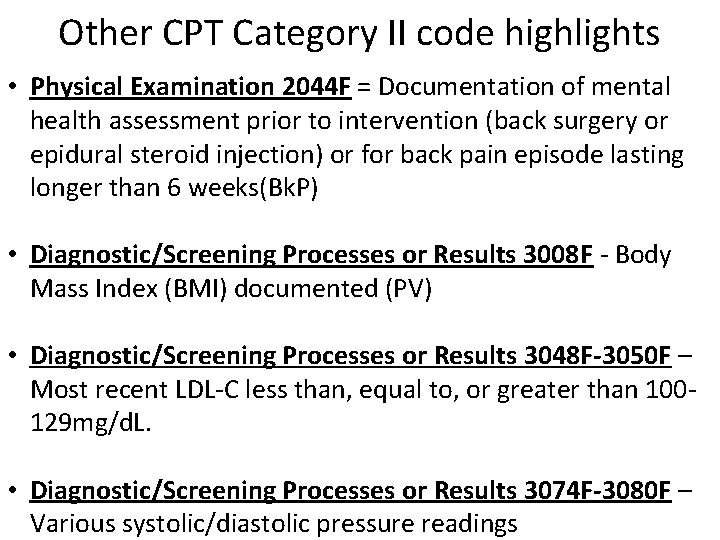
Other CPT Category II code highlights • Physical Examination 2044 F = Documentation of mental health assessment prior to intervention (back surgery or epidural steroid injection) or for back pain episode lasting longer than 6 weeks(Bk. P) • Diagnostic/Screening Processes or Results 3008 F - Body Mass Index (BMI) documented (PV) • Diagnostic/Screening Processes or Results 3048 F-3050 F – Most recent LDL-C less than, equal to, or greater than 100129 mg/d. L. • Diagnostic/Screening Processes or Results 3074 F-3080 F – Various systolic/diastolic pressure readings
Other CPT Category II code highlights • Therapeutic, Preventive, or Other Interventions 4000 F 4001 F, 4004 F = Tobacco use cessation counseling vs. drug therapy • Therapeutic, Preventive, or Other Interventions 4035 F 4040 F – assorted vaccinations administered or recommended • Therapeutic, Preventive, or Other Interventions 4060 F 4065 F – assorted Behavioral Health medication issues • Follow-up or Other Outcomes 5005 F – Patient counseled on self-examination for new or changing moles
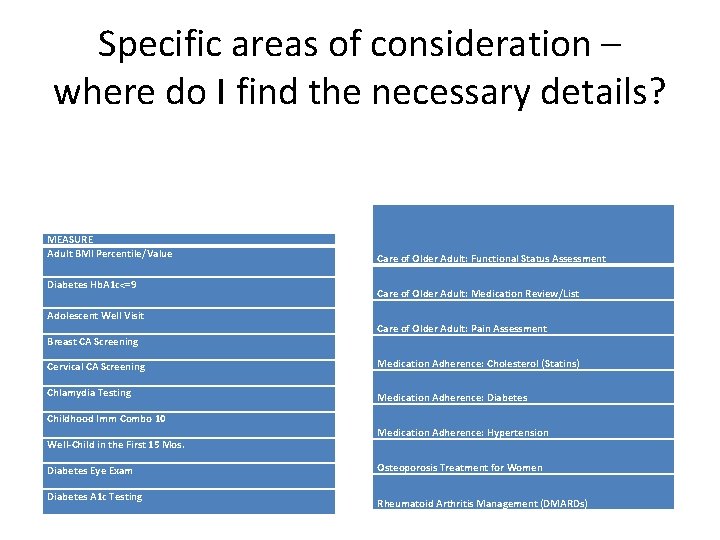
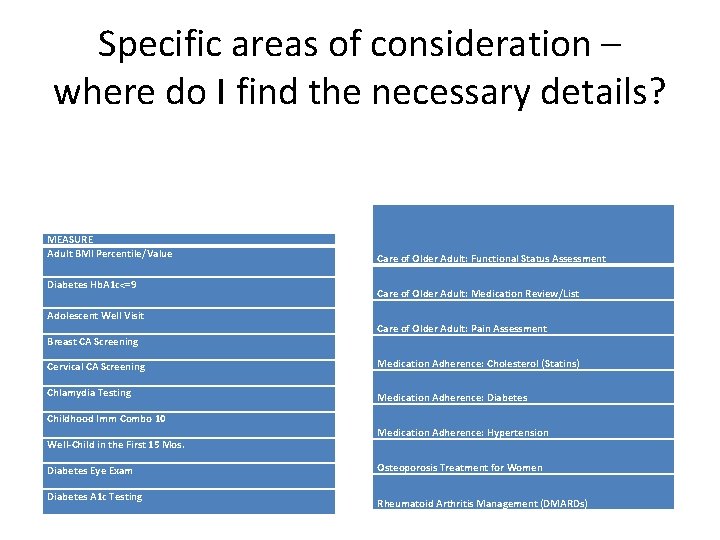
Specific areas of consideration – where do I find the necessary details? MEASURE Adult BMI Percentile/Value Diabetes Hb. A 1 c<=9 Adolescent Well Visit Breast CA Screening Care of Older Adult: Functional Status Assessment Care of Older Adult: Medication Review/List Care of Older Adult: Pain Assessment Cervical CA Screening Medication Adherence: Cholesterol (Statins) Chlamydia Testing Medication Adherence: Diabetes Childhood Imm Combo 10 Well-Child in the First 15 Mos. Diabetes Eye Exam Diabetes A 1 c Testing Medication Adherence: Hypertension Osteoporosis Treatment for Women Rheumatoid Arthritis Management (DMARDs)
Source: https: //www. medicaid. gov/medicaid/quali ty-of-care/downloads/medicaid-and-chipchild-core-set-manual. pdf Source: https: //www. medicaid. gov/medicaid/quality-of-care/downloads/medicaid-andchip-child-core-set-manual. pdf
The AMA’s Alphabetical Clinical Topics Listing – 404 pages! • Source: Accessed on 11/6/2017 at https: //www. ama-assn. org/sites/default/files/mediabrowser/public/cpt-cat 2 -codes-alpha-listing-clinical-topics_0. pdf
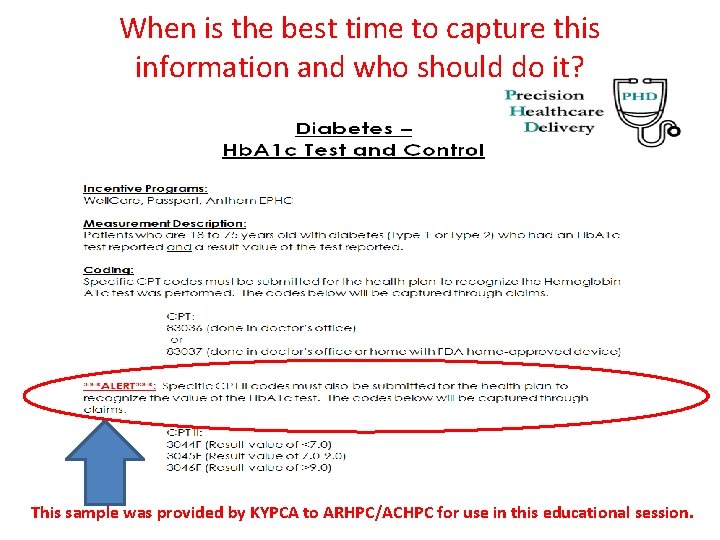
When is the best time to capture this information and who should do it? This sample was provided by KYPCA to ARHPC/ACHPC for use in this educational session.
Items for follow-up • Review the CPT Category II sections and follow the hyperlinks in this presentation to continue the educational process. • Review participation contracts with key payers and professional organizations to identify any required or voluntary measures that you need to be aware of. • Secure documentation from the payer to determine which patients are “eligible” and use Category II modifiers if the measure was not captured.
Items for follow-up • Work closely with your vendors to see what can be automatically captured from discrete EHR data plus investigate any IT issues (i. e. $. 01 charges and CMS 1450/1500 claim form issues) with your clearinghouses who may not be expecting these codes. • Surround yourselves with qualified, welleducated, supported, and (maybe) certified staff who work together to help your facility meet all external requirements on reporting.
Session Objectives Following the presentation, the participants will: 1. Understand the importance of coding CPT II codes to capture quality measures for value based programs 2. Determine the appropriate CPT II codes for a set of quality measures 3. Outline at least three CPT II codes which can be improved in their clinic