COURAGE Nuclear Substudy II Optimal Medical Therapy with
COURAGE Nuclear Substudy II Optimal Medical Therapy with or without PCI to Reduce Ischemic Burden: Results from Clinical Outcomes Utilizing Revascularization & Aggressive Guideline-Driven Drug Evaluation Trial Nuclear Substudy Leslee J. Shaw, Daniel S. Berman, David J. Maron, G. B. John Mancini, Sean W. Hayes, Pamela M. Hartigan, William S. Weintraub, Robert A. O’Rourke, Marcin Dada, John A. Spertus, Bernard R. Chaitman, John Friedman, Piotr Slomka, Gary V. Heller, Guido Germano, Gilbert Gosselin, Peter Berger, William J. Kostuk, Ronald Schwartz, Merill Knudtson, Emir Veledar, Eric R. Bates, Benjamin Mc. Callister, Koon K. Teo, William E. Boden for the COURAGE
Presenter Conflict Disclosure Name: Leslee J. Shaw, Ph. D Within the past 12 months, presenter or spouse/partner have had financial interest/arrangement/ affiliation w/ organization listed below. Company Name: Relationship: BMS Medical Imaging Research grant support Astellas Healthcare Speaker’s Bureau Research grant support; GE Healthcare Research grant support/Speaker’s Bureau
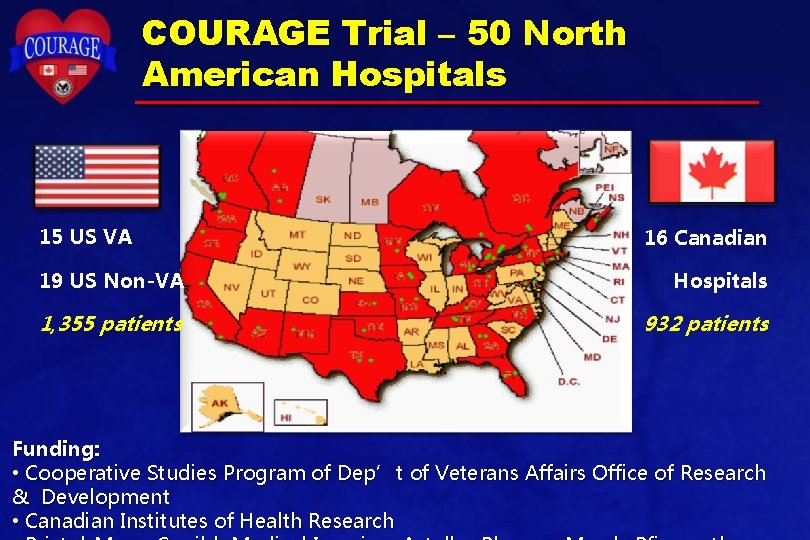
COURAGE Trial – 50 North American Hospitals 15 US VA 16 Canadian 19 US Non-VA Hospitals 1, 355 patients 932 patients Funding: • Cooperative Studies Program of Dep’t of Veterans Affairs Office of Research & Development • Canadian Institutes of Health Research
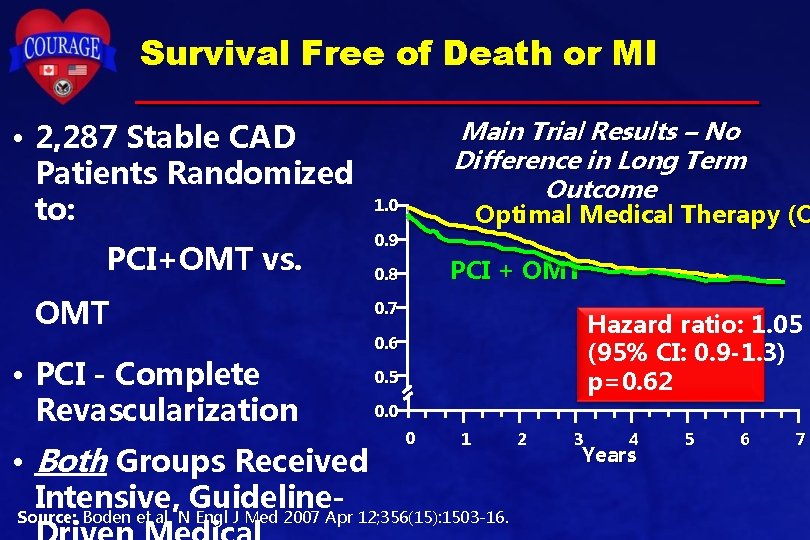
Survival Free of Death or MI • 2, 287 Stable CAD Patients Randomized to: PCI+OMT vs. OMT • PCI - Complete Revascularization • Both Groups Received Intensive, Guideline- Main Trial Results – No Difference in Long Term Outcome 1. 0 Optimal Medical Therapy (O 0. 9 PCI + OMT 0. 8 0. 7 Hazard ratio: 1. 05 (95% CI: 0. 9 -1. 3) p=0. 62 0. 6 0. 5 0. 0 0 1 Source: Boden et al. N Engl J Med 2007 Apr 12; 356(15): 1503 -16. 2 3 4 Years 5 6 7
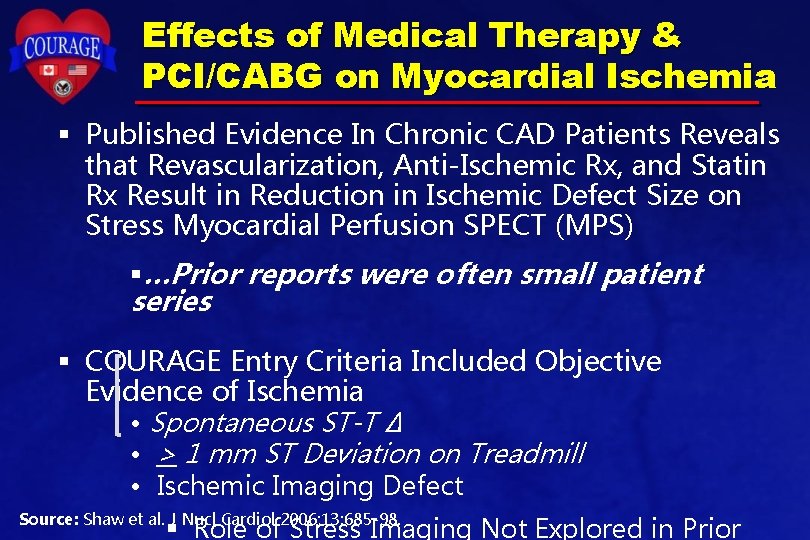
Effects of Medical Therapy & PCI/CABG on Myocardial Ischemia § Published Evidence In Chronic CAD Patients Reveals that Revascularization, Anti-Ischemic Rx, and Statin Rx Result in Reduction in Ischemic Defect Size on Stress Myocardial Perfusion SPECT (MPS) §…Prior reports were often small patient series § COURAGE Entry Criteria Included Objective Evidence of Ischemia • Spontaneous ST-T ∆ • > 1 mm ST Deviation on Treadmill • Ischemic Imaging Defect Source: Shaw et al. J Nucl Cardiol 2006; 13: 685 -98. § Role of Stress Imaging Not Explored in Prior
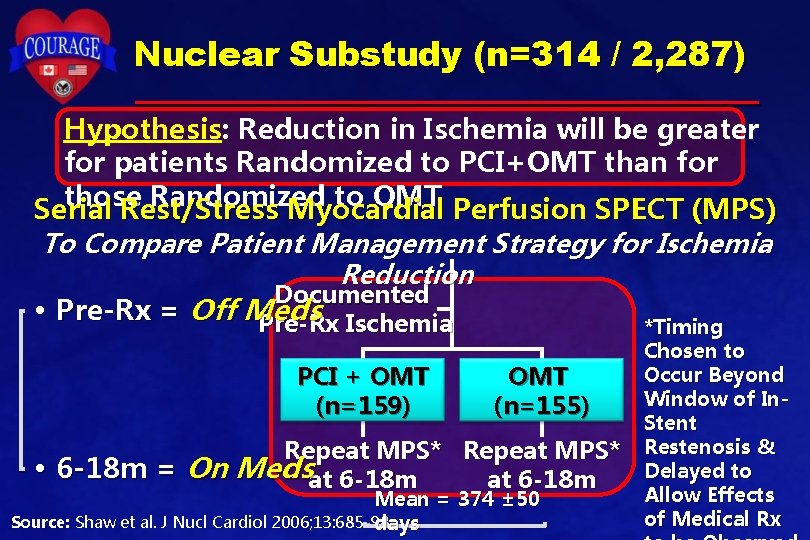
Nuclear Substudy (n=314 / 2, 287) Hypothesis: Reduction in Ischemia will be greater for patients Randomized to PCI+OMT than for those Randomized to OMT Perfusion SPECT (MPS) Serial Rest/Stress Myocardial To Compare Patient Management Strategy for Ischemia Reduction Documented • Pre-Rx = Off Meds Pre-Rx Ischemia *Timing PCI + OMT (n=159) • OMT (n=155) Repeat MPS* 6 -18 m = On Medsat 6 -18 m Mean = 374 ± 50 Source: Shaw et al. J Nucl Cardiol 2006; 13: 685 -98. days *Timing Chosen to Occur Beyond Window of In. Stent Restenosis & Delayed to Allow Effects of Medical Rx
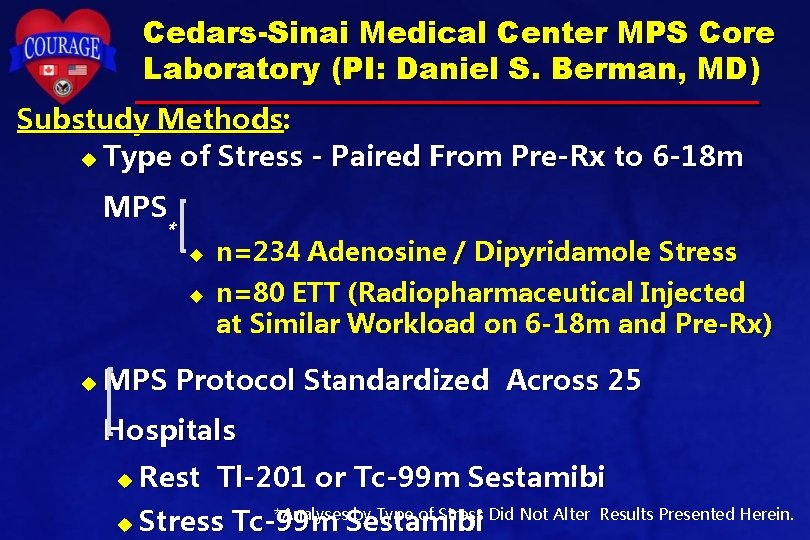
Cedars-Sinai Medical Center MPS Core Laboratory (PI: Daniel S. Berman, MD) Substudy Methods: u Type of Stress - Paired From Pre-Rx to 6 -18 m MPS * u u u n=234 Adenosine / Dipyridamole Stress n=80 ETT (Radiopharmaceutical Injected at Similar Workload on 6 -18 m and Pre-Rx) MPS Protocol Standardized Across 25 Hospitals u Rest Tl-201 or Tc-99 m Sestamibi u *Analyses by Type of Stress Did Not Alter Stress Tc-99 m Sestamibi Results Presented Herein.
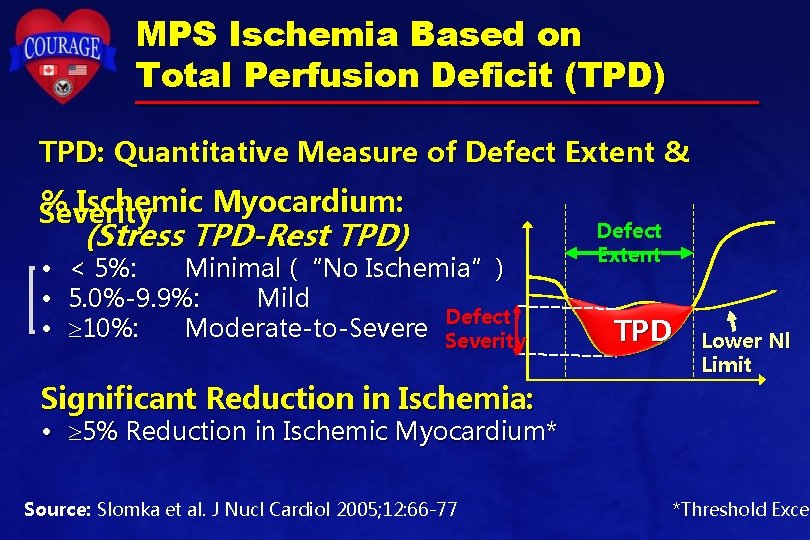
MPS Ischemia Based on Total Perfusion Deficit (TPD) TPD: Quantitative Measure of Defect Extent & % Ischemic Myocardium: Severity • • • (Stress TPD-Rest TPD) < 5%: Minimal (“No Ischemia”) 5. 0%-9. 9%: Mild Defect 10%: Moderate-to-Severe Severity Significant Reduction in Ischemia: Defect Extent TPD Lower Nl Limit • 5% Reduction in Ischemic Myocardium* Source: Slomka et al. J Nucl Cardiol 2005; 12: 66 -77 *Threshold Excee
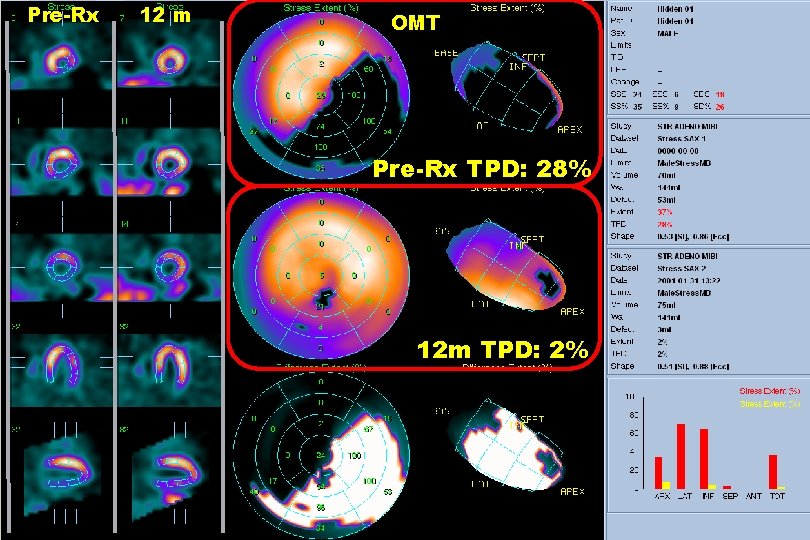
Pre-Rx 12 m OMT Pre-Rx TPD: 28% 12 m TPD: 2%
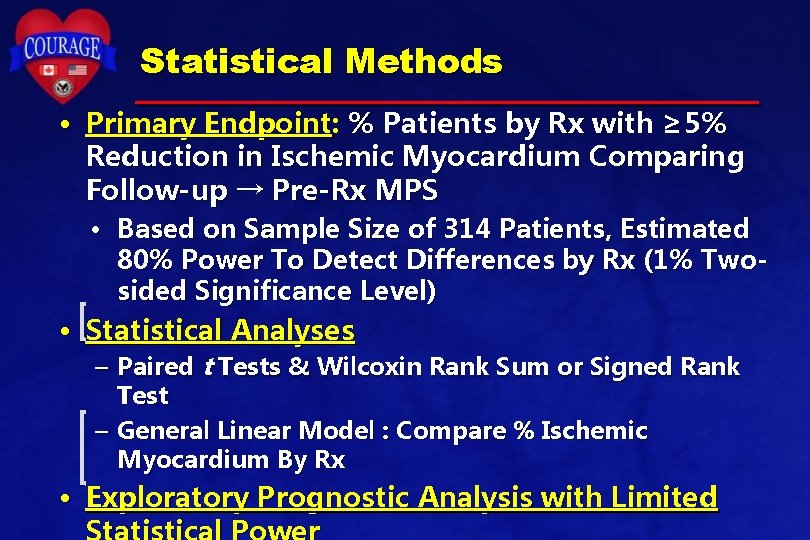
Statistical Methods • Primary Endpoint: % Patients by Rx with ≥ 5% Reduction in Ischemic Myocardium Comparing Follow-up → Pre-Rx MPS • Based on Sample Size of 314 Patients, Estimated 80% Power To Detect Differences by Rx (1% Twosided Significance Level) • Statistical Analyses – Paired t Tests & Wilcoxin Rank Sum or Signed Rank Test – General Linear Model : Compare % Ischemic Myocardium By Rx • Exploratory Prognostic Analysis with Limited
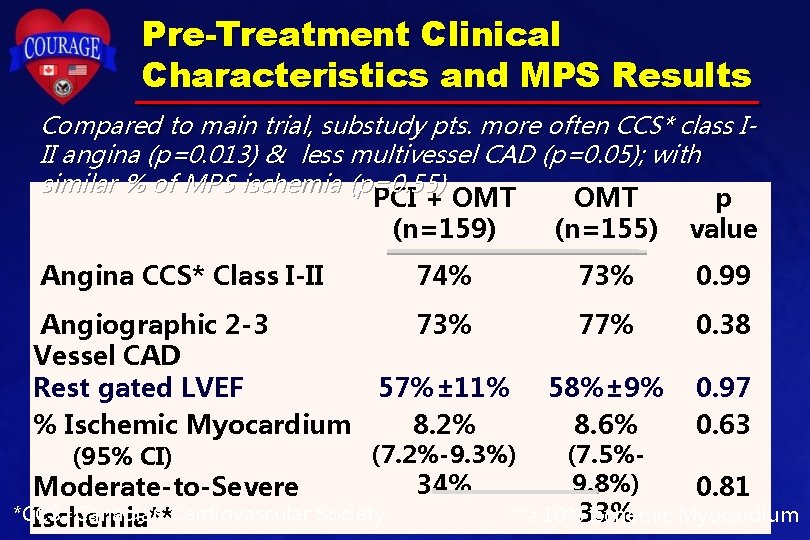
Pre-Treatment Clinical Characteristics and MPS Results Compared to main trial, substudy pts. more often CCS* class III angina (p=0. 013) & less multivessel CAD (p=0. 05); with similar % of MPS ischemia (p=0. 55) PCI + OMT p (n=159) (n=155) value Angina CCS* Class I-II 74% 73% 0. 99 Angiographic 2 -3 Vessel CAD Rest gated LVEF % Ischemic Myocardium 73% 77% 0. 38 57%± 11% 8. 2% 58%± 9% 8. 6% 0. 97 0. 63 (95% CI) (7. 2%-9. 3%) Moderate-to-Severe *CCS=Canadian Ischemia**Cardiovascular Society 34% (7. 5%9. 8%) 0. 81 **≥ 10%33% Ischemic Myocardium
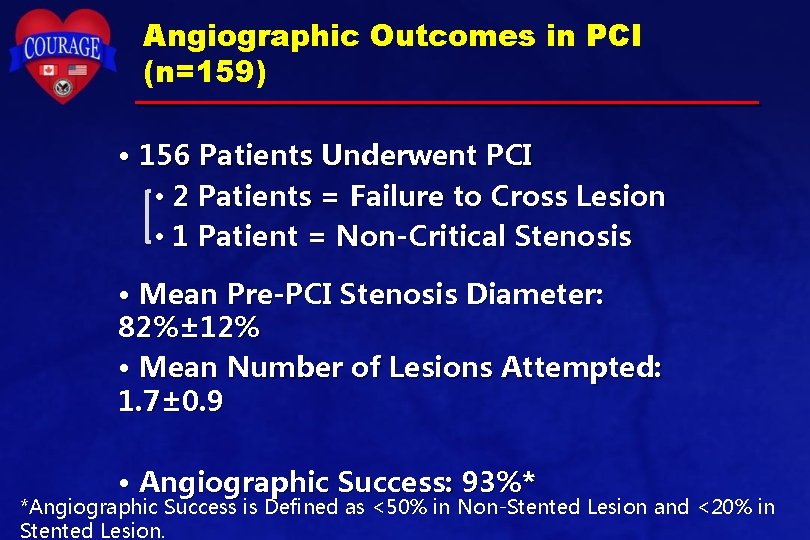
Angiographic Outcomes in PCI (n=159) • 156 Patients Underwent PCI • 2 Patients = Failure to Cross Lesion • 1 Patient = Non-Critical Stenosis • Mean Pre-PCI Stenosis Diameter: 82%± 12% • Mean Number of Lesions Attempted: 1. 7± 0. 9 • Angiographic Success: 93%* *Angiographic Success is Defined as <50% in Non-Stented Lesion and <20% in Stented Lesion.
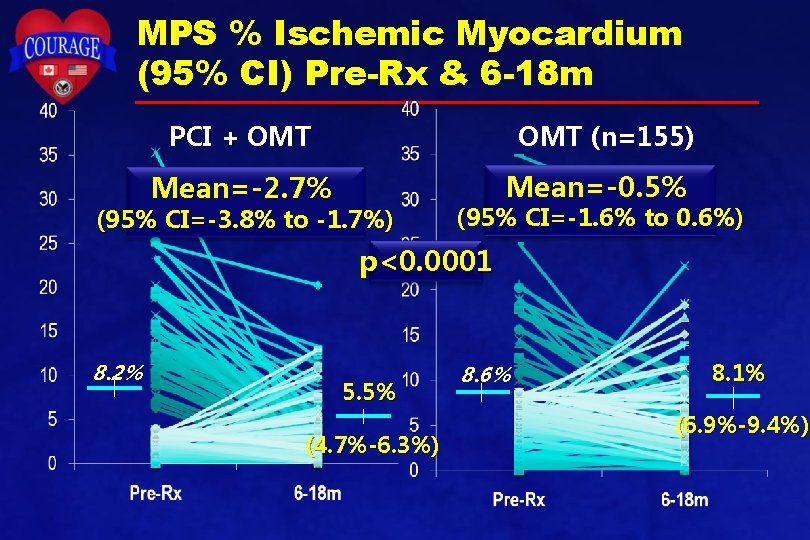
MPS % Ischemic Myocardium (95% CI) Pre-Rx & 6 -18 m OMT (n=155) PCI + OMT Mean=-2. 7% (n=159) (95% CI=-3. 8% to -1. 7%) Mean=-0. 5% (95% CI=-1. 6% to 0. 6%) p<0. 0001 8. 2% 5. 5% (4. 7%-6. 3%) 8. 6% 8. 1% (6. 9%-9. 4%)
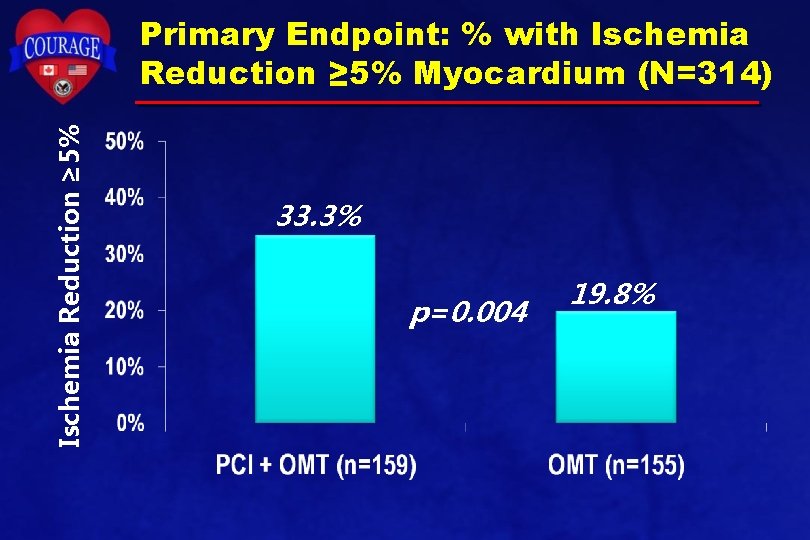
Ischemia Reduction ≥ 5% Primary Endpoint: % with Ischemia Reduction ≥ 5% Myocardium (N=314) 33. 3% p=0. 004 19. 8%
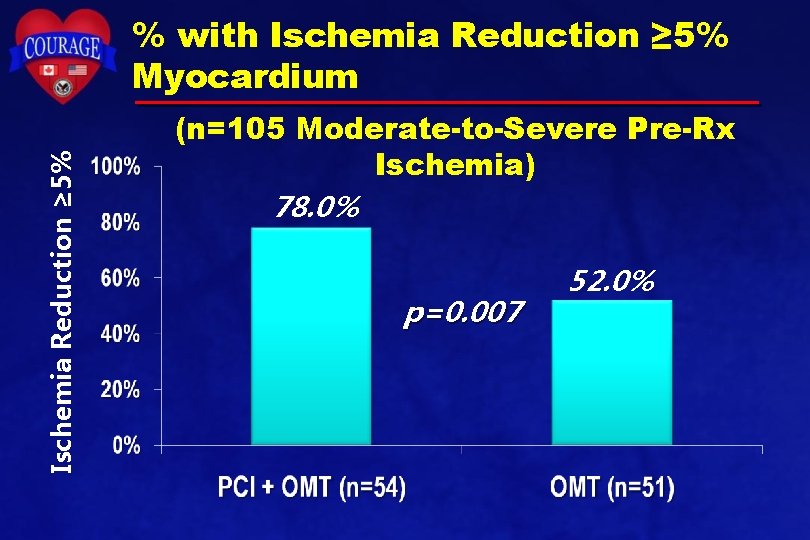
Ischemia Reduction ≥ 5% % with Ischemia Reduction ≥ 5% Myocardium (n=105 Moderate-to-Severe Pre-Rx Ischemia) 78. 0% p=0. 007 52. 0%
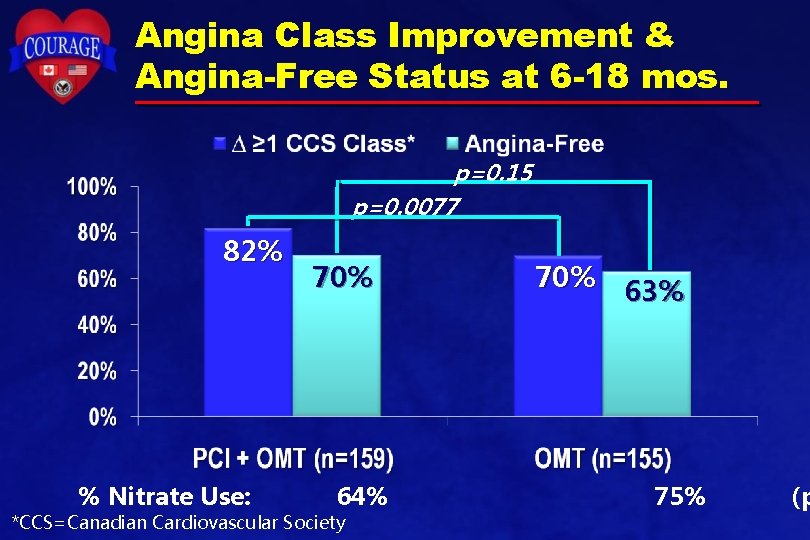
Angina Class Improvement & Angina-Free Status at 6 -18 mos. p=0. 15 p=0. 0077 82% % Nitrate Use: 70% 64% *CCS=Canadian Cardiovascular Society 70% 63% 75% (p
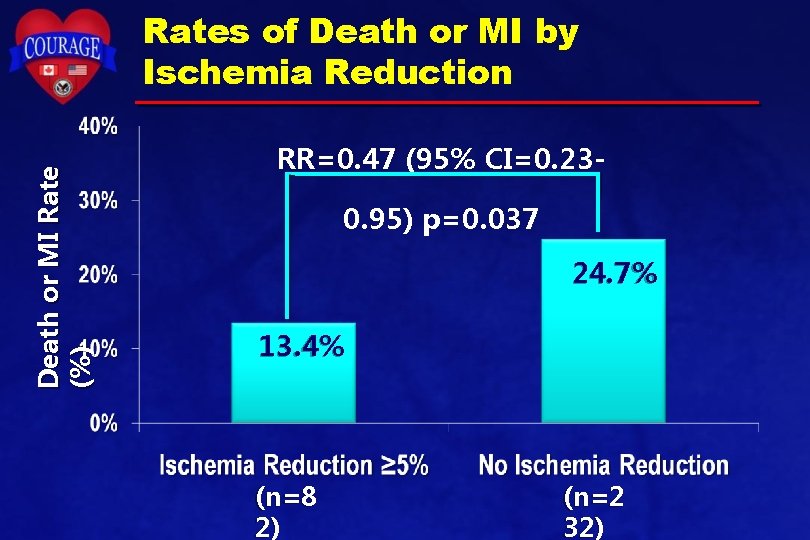
Death or MI Rate (%) Rates of Death or MI by Ischemia Reduction RR=0. 47 (95% CI=0. 230. 95) p=0. 037 24. 7% 13. 4% (n=8 2) (n=2 32)
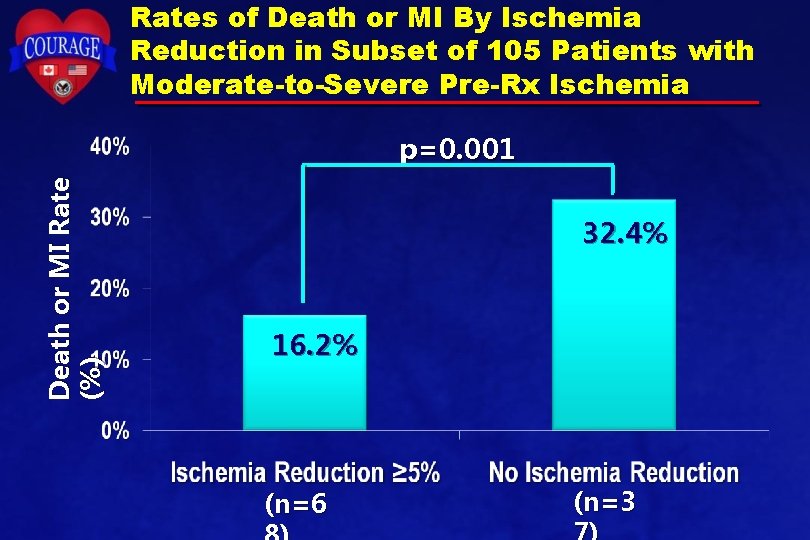
Rates of Death or MI By Ischemia Reduction in Subset of 105 Patients with Moderate-to-Severe Pre-Rx Ischemia Death or MI Rate (%) p=0. 001 32. 4% 16. 2% (n=6 (n=3
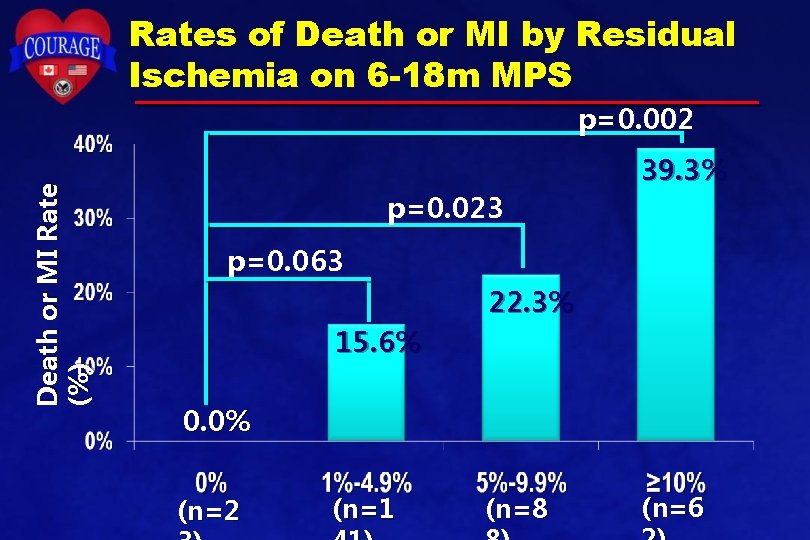
Rates of Death or MI by Residual Ischemia on 6 -18 m MPS Death or MI Rate (%) p=0. 002 39. 3% p=0. 023 p=0. 063 22. 3% 15. 6% 0. 0% (n=2 (n=1 (n=8 (n=6
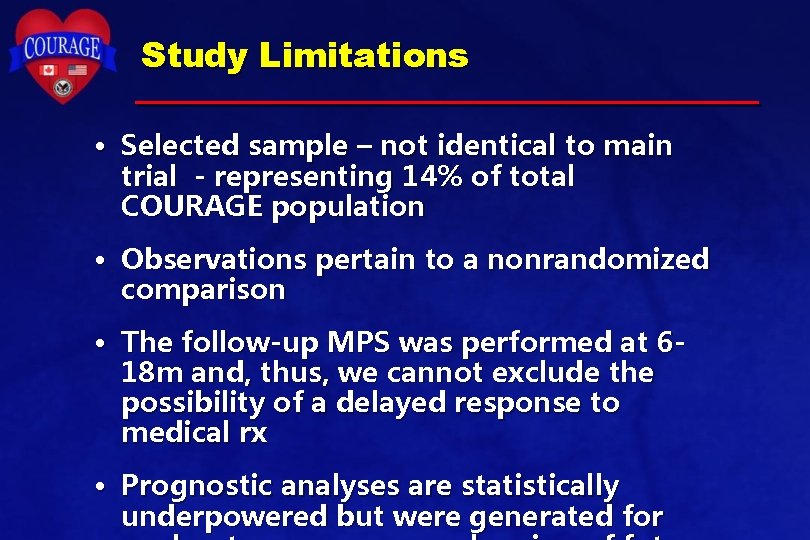
Study Limitations • Selected sample – not identical to main trial - representing 14% of total COURAGE population • Observations pertain to a nonrandomized comparison • The follow-up MPS was performed at 618 m and, thus, we cannot exclude the possibility of a delayed response to medical rx • Prognostic analyses are statistically underpowered but were generated for
Conclusions • PCI added to OMT was more effective in reducing ischemia and improving angina than OMT, particularly in patients with moderate-tosevere pre-rx ischemia • Exploratory outcomes data: – Ischemia reduction ≥ 5% associated with lower risk of death/MI – Residual ischemia ≥ 5% associated with higher risk of death/MI • Randomized trials of management strategies should evaluate quantitative measures of
- Slides: 21