Costeffectiveness of intelligent Liver Function testi LFT for
- Slides: 1
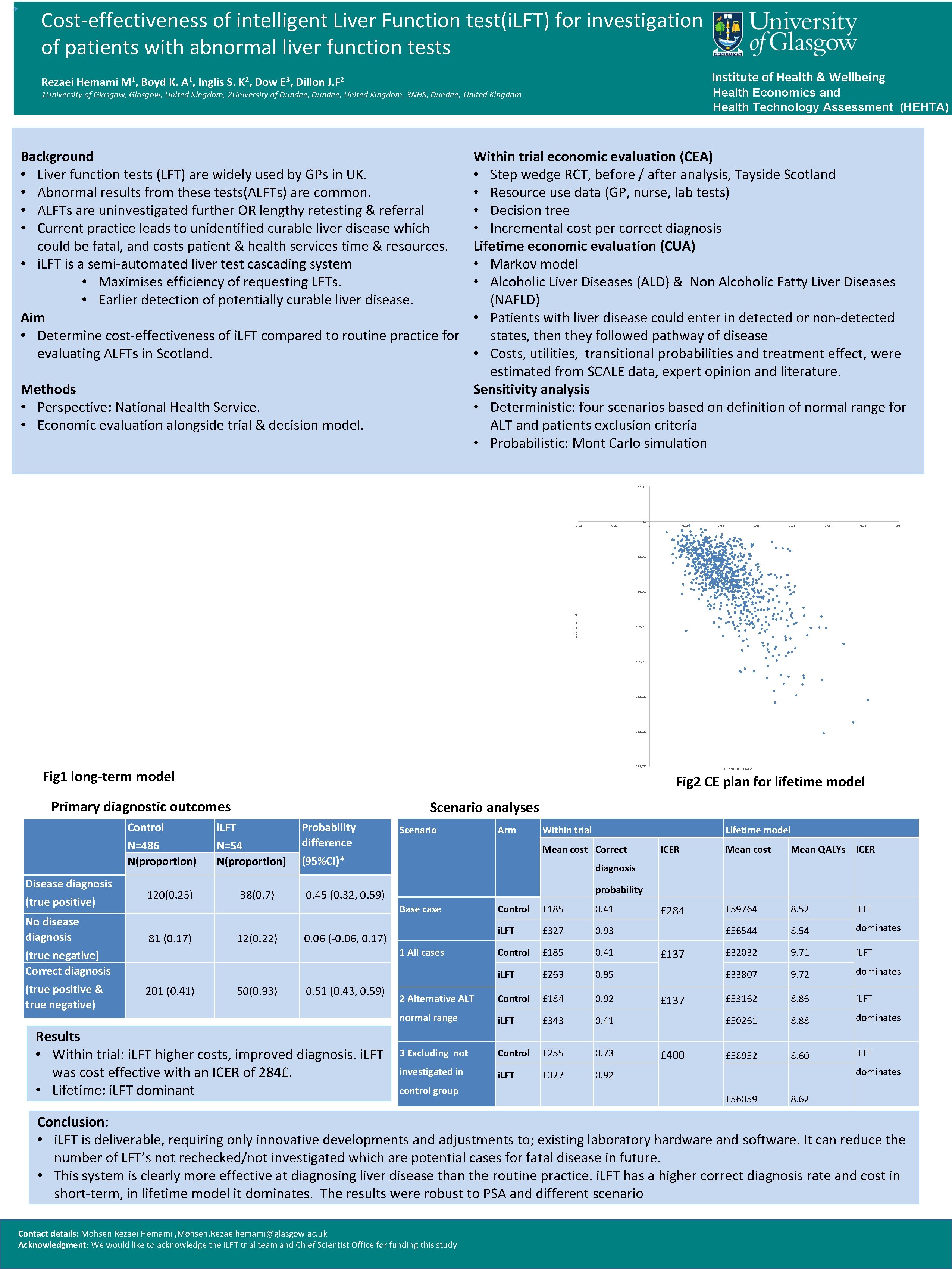
Cost-effectiveness of intelligent Liver Function test(i. LFT) for investigation of patients with abnormal liver function tests Institute of Health & Wellbeing Rezaei Hemami M 1, Boyd K. A 1, Inglis S. K 2, Dow E 3, Dillon J. F 2 Health Economics and Health Technology Assessment (HEHTA) 1 University of Glasgow, United Kingdom, 2 University of Dundee, United Kingdom, 3 NHS, Dundee, United Kingdom Background • Liver function tests (LFT) are widely used by GPs in UK. • Abnormal results from these tests(ALFTs) are common. • ALFTs are uninvestigated further OR lengthy retesting & referral • Current practice leads to unidentified curable liver disease which could be fatal, and costs patient & health services time & resources. • i. LFT is a semi-automated liver test cascading system • Maximises efficiency of requesting LFTs. • Earlier detection of potentially curable liver disease. Aim • Determine cost-effectiveness of i. LFT compared to routine practice for evaluating ALFTs in Scotland. Methods • Perspective: National Health Service. • Economic evaluation alongside trial & decision model. Within trial economic evaluation (CEA) • Step wedge RCT, before / after analysis, Tayside Scotland • Resource use data (GP, nurse, lab tests) • Decision tree • Incremental cost per correct diagnosis Lifetime economic evaluation (CUA) • Markov model • Alcoholic Liver Diseases (ALD) & Non Alcoholic Fatty Liver Diseases (NAFLD) • Patients with liver disease could enter in detected or non-detected states, then they followed pathway of disease • Costs, utilities, transitional probabilities and treatment effect, were estimated from SCALE data, expert opinion and literature. Sensitivity analysis • Deterministic: four scenarios based on definition of normal range for ALT and patients exclusion criteria • Probabilistic: Mont Carlo simulation £ 2, 000 -0. 02 £ 0 -0. 01 0. 02 0. 03 0. 04 0. 05 0. 06 0. 07 -£ 2, 000 Incremental cost -£ 4, 000 -£ 6, 000 -£ 8, 000 -£ 10, 000 -£ 12, 000 -£ 14, 000 Fig 1 long-term model Fig 2 CE plan for lifetime model Primary diagnostic outcomes Disease diagnosis (true positive) No disease diagnosis Scenario analyses Control i. LFT N=486 N(proportion) N=54 N(proportion) 120(0. 25) 38(0. 7) Probability difference 12(0. 22) 50(0. 93) Within trial Mean cost Mean QALYs ICER £ 284 £ 59764 8. 52 i. LFT £ 56544 8. 54 dominates £ 32032 9. 71 i. LFT £ 33807 9. 72 dominates £ 53162 8. 86 i. LFT £ 50261 8. 88 dominates £ 58952 8. 60 i. LFT probability Control £ 185 0. 41 i. LFT £ 327 0. 93 Control £ 185 0. 41 i. LFT £ 263 0. 95 2 Alternative ALT Control £ 184 0. 92 normal range i. LFT £ 343 0. 41 3 Excluding not Control £ 255 0. 73 investigated in i. LFT £ 327 0. 92 0. 06 (-0. 06, 0. 17) Results • Within trial: i. LFT higher costs, improved diagnosis. i. LFT was cost effective with an ICER of 284£. • Lifetime: i. LFT dominant ICER diagnosis 0. 45 (0. 32, 0. 59) 0. 51 (0. 43, 0. 59) Lifetime model Mean cost Correct 1 All cases 201 (0. 41) Arm (95%CI)* (true negative) Correct diagnosis (true positive & true negative) Scenario Base case 81 (0. 17) Incremental QALYs control group £ 137 £ 400 dominates £ 56059 8. 62 Conclusion: • i. LFT is deliverable, requiring only innovative developments and adjustments to; existing laboratory hardware and software. It can reduce the number of LFT’s not rechecked/not investigated which are potential cases for fatal disease in future. • This system is clearly more effective at diagnosing liver disease than the routine practice. i. LFT has a higher correct diagnosis rate and cost in short-term, in lifetime model it dominates. The results were robust to PSA and different scenario Contact details: Mohsen Rezaei Hemami , Mohsen. Rezaeihemami@glasgow. ac. uk Acknowledgment: We would like to acknowledge the i. LFT trial team and Chief Scientist Office for funding this study