Corticosteroid In Dermatology Route n Topical steroid n
- Slides: 26
Corticosteroid In Dermatology
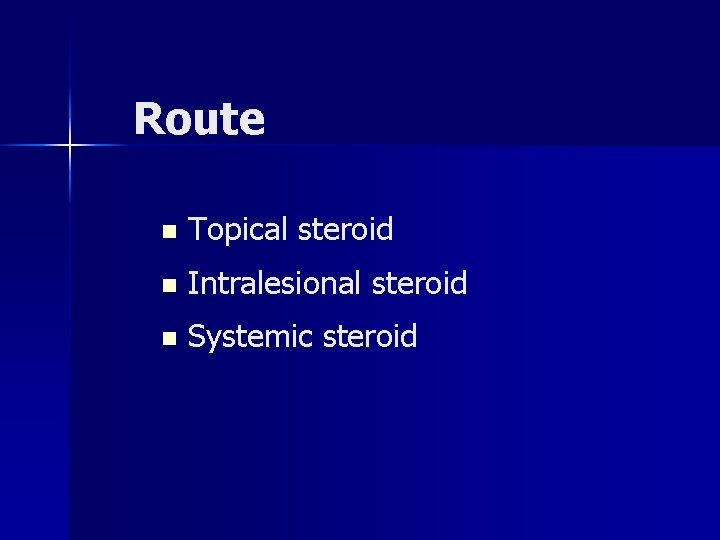
Route n Topical steroid n Intralesional steroid n Systemic steroid
Topical steroid--History n n Began when Sulzberger and Witten reported in 1952 --topically applied hydrocortisone in eczematous dermatitis. The findings soon resulted in investigation toward the development of more potent agents for various inflammatory dermatoses.
Topical steroid--Structure n n All topical steroids have the same basic compound--hydrocortisone (cortisol). Modification of both the ring structure and the side-chains produced dramatic changes in the effectiveness of the steroid.
Mechanism of Action n Anti-inflammation. n Anti-proliferation. n Immunosuppression. n Vasoconstriction.
Factors Affecting Potency (top) n n n n Addition of fluoride or chloride at 6, 9, or 21 position. Addition of double bound at 1, 2 position. Lipophilia of corticosteroid. Drug delivery system--- Vehicle. State of epidermal barrier. Method of application Drug concentration
Percutaneous Absorption (1) n In order for a topical medication to produce its effect, it first must penetrate the epidermal barrier. n One of the greatest influences on the effectiveness of topical steroid.
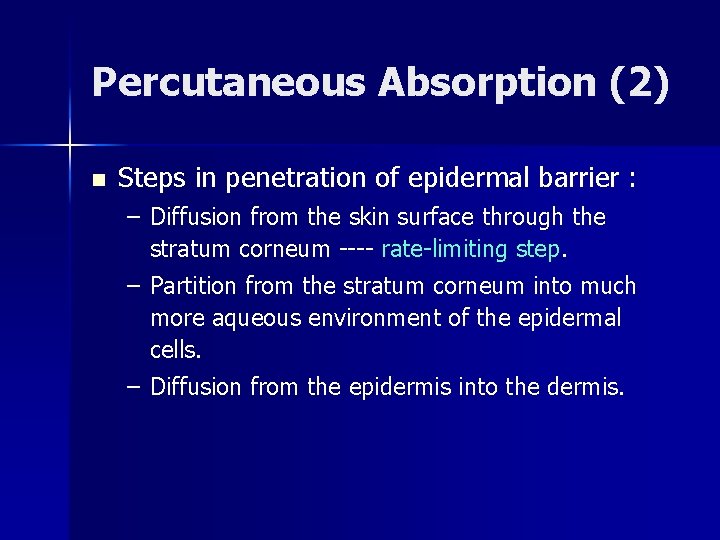
Percutaneous Absorption (2) n Steps in penetration of epidermal barrier : – Diffusion from the skin surface through the stratum corneum ---- rate-limiting step. – Partition from the stratum corneum into much more aqueous environment of the epidermal cells. – Diffusion from the epidermis into the dermis.
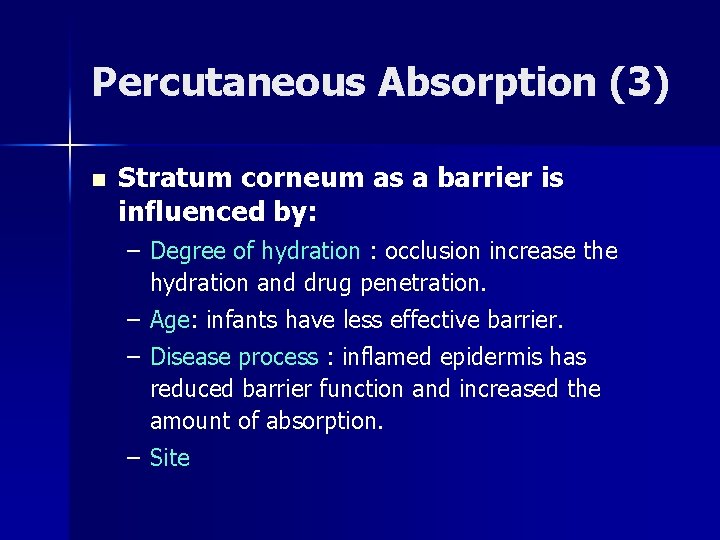
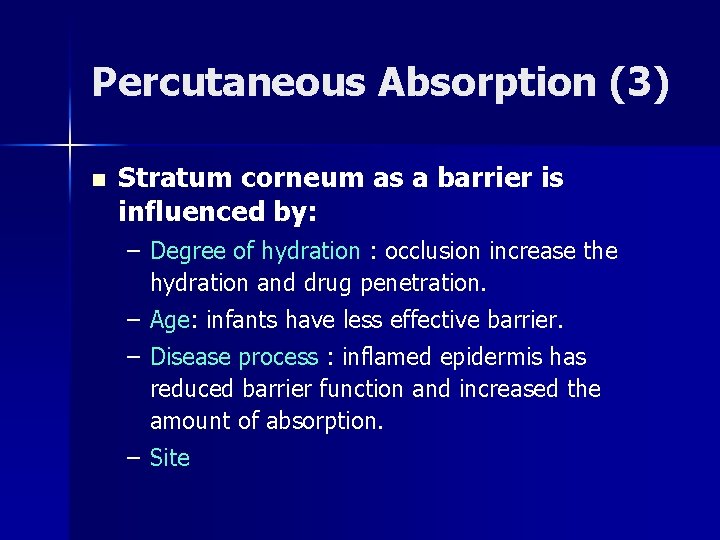
Percutaneous Absorption (3) n Stratum corneum as a barrier is influenced by: – Degree of hydration : occlusion increase the hydration and drug penetration. – Age: infants have less effective barrier. – Disease process : inflamed epidermis has reduced barrier function and increased the amount of absorption. – Site
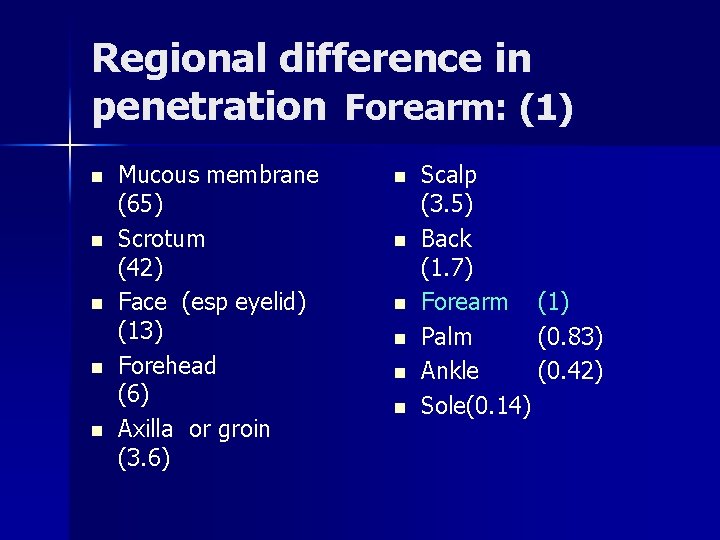
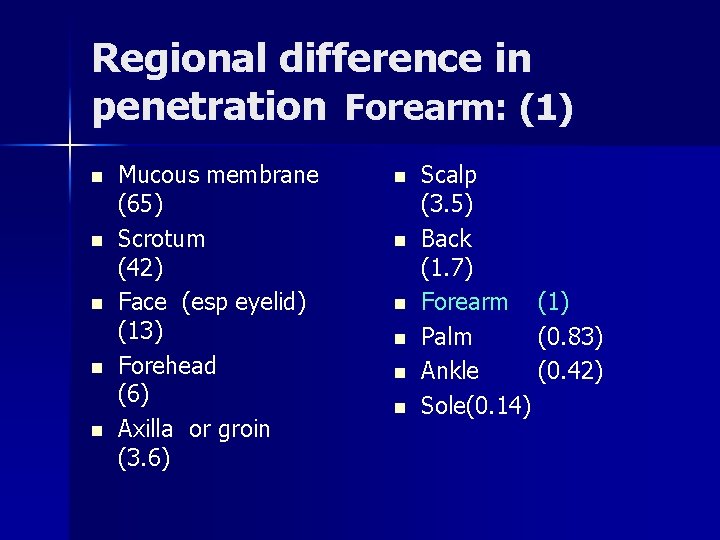
Regional difference in penetration Forearm: (1) n n n Mucous membrane (65) Scrotum (42) Face (esp eyelid) (13) Forehead (6) Axilla or groin (3. 6) n n n Scalp (3. 5) Back (1. 7) Forearm (1) Palm (0. 83) Ankle (0. 42) Sole(0. 14)
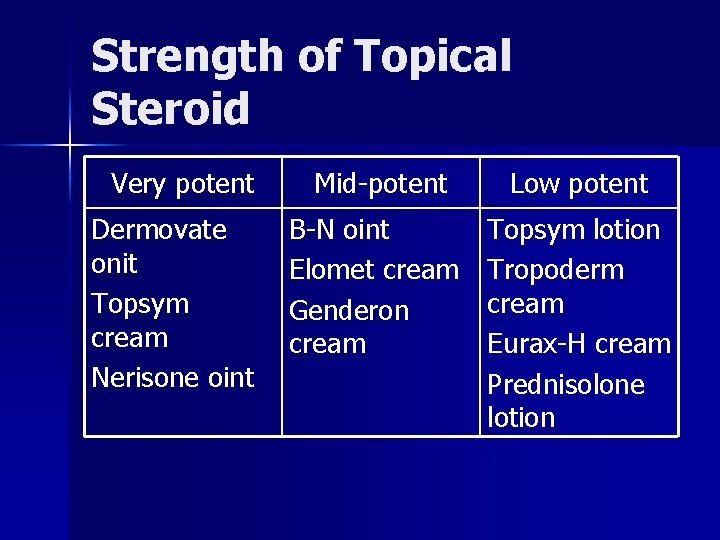
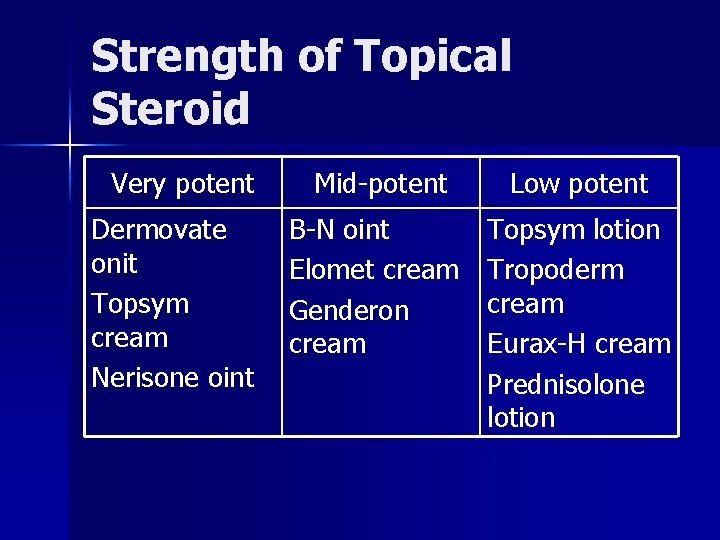
Strength of Topical Steroid Very potent Dermovate onit Topsym cream Nerisone oint Mid-potent Low potent B-N oint Elomet cream Genderon cream Topsym lotion Tropoderm cream Eurax-H cream Prednisolone lotion
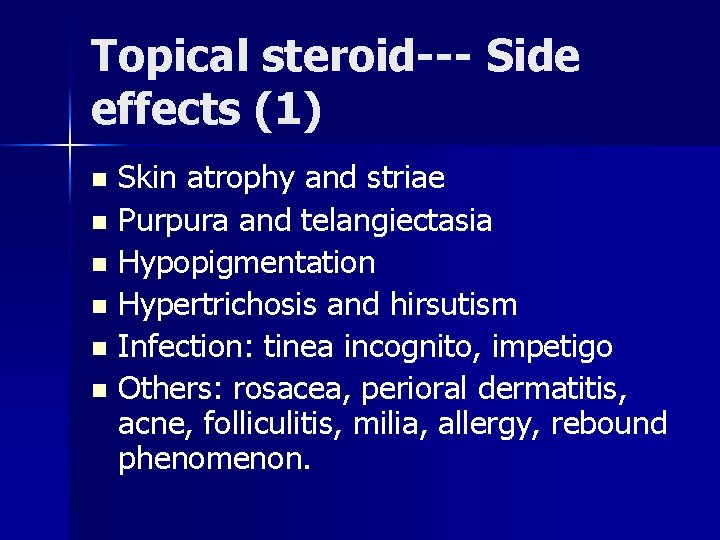
Topical steroid--- Side effects (1) n n n Skin atrophy and striae Purpura and telangiectasia Hypopigmentation Hypertrichosis and hirsutism Infection: tinea incognito, impetigo Others: rosacea, perioral dermatitis, acne, folliculitis, milia, allergy, rebound phenomenon.
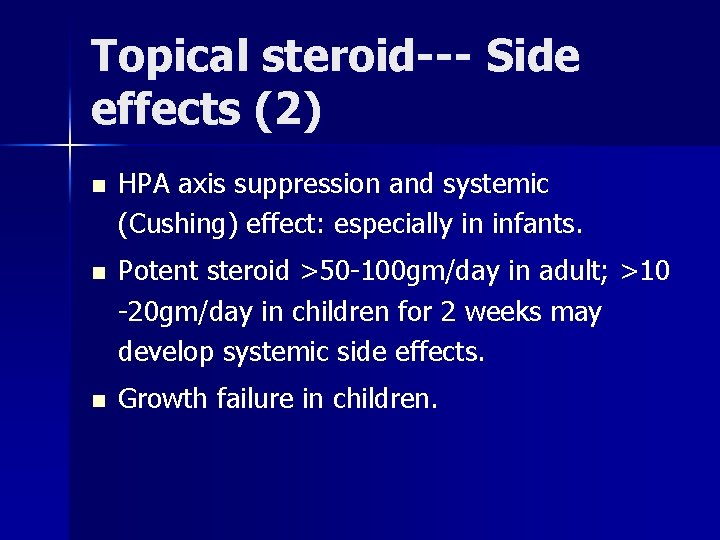
Topical steroid--- Side effects (2) n HPA axis suppression and systemic (Cushing) effect: especially in infants. n Potent steroid >50 -100 gm/day in adult; >10 -20 gm/day in children for 2 weeks may develop systemic side effects. n Growth failure in children.
Intralesional steroids n Indication: keloid, nodular prurigo, lichen simplex chronicus, alopecia …… n Triamcinolone is often used. n Side effects: dermal atrophy, leukoderma. n Blindness was reported following intralesional injection of the eyebrow skin.
Systemic steroid in dermatology n Since skin lesions are accessible, the topical route is preferable than systemic route n because the risk of potentially harmful exposure of internal tissues and organs to the systemic steroid.
Systemic steroid in dermatology -- Indication (1) n Acute, self-limited steroid-sensitive disorders: acute allergic contact dermatitis. . . n Acute anaphylactic reaction: following bee or wasp sting or a drug to which the patient is sensitized.
Systemic steroid in dermatology -- Indication (2) n n Autoimmune connective tissue disease and immunological vascular disorders: SLE, dermatomyositis, polyarteritis nodosa. . . Chronic, disabling immunological bullous diseases: pemphigus, bullous pemphigoid…
Systemic steroid in dermatology -- Indication (3) n Severe drug reaction: erythroderma, Stevens-Johnson syndrome, TEN… n Others: pyoderma gangrenosum, sarcoidosis, severe lichen planus… n Unproven therapeutic value: cutaneous T-cell lymphoma, chronic urticaria. . .
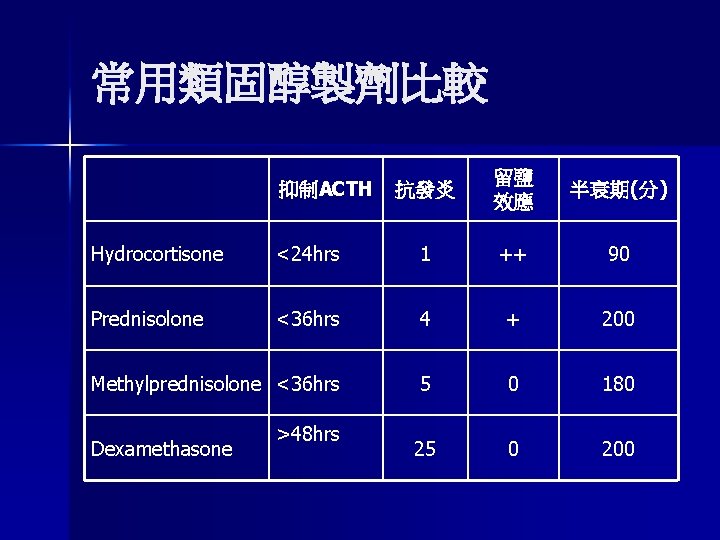
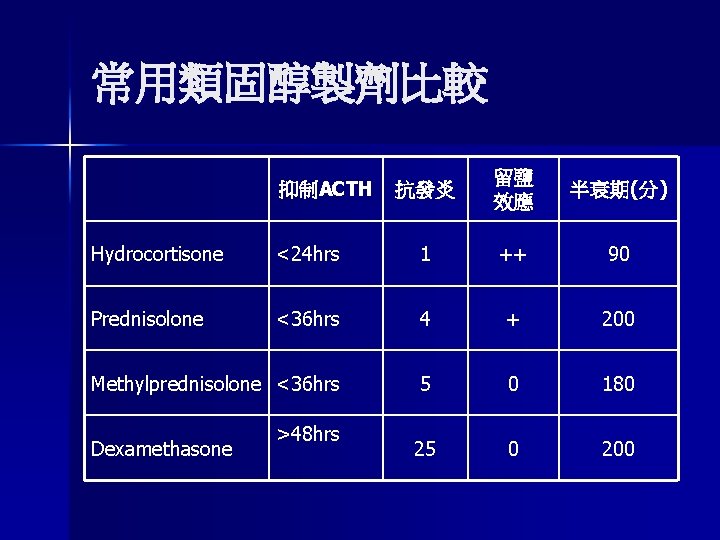
常用類固醇製劑比較 抑制ACTH 抗發炎 留鹽 效應 半衰期(分) Hydrocortisone <24 hrs 1 ++ 90 Prednisolone <36 hrs 4 + 200 Methylprednisolone <36 hrs 5 0 180 25 0 200 Dexamethasone >48 hrs
Mechanism of Action n Anti-inflammation. n Anti-proliferation. n Immunosuppression. n Vasoconstriction.
Route of administration n n Intramuscular : triamcinolone (效力同 prednisolone) , dexamethasone (Dexan). Intravenous : hydrocortisone (Solu-cortef), methylprednisolone (Solu-medrol), dexamethasone (Dexan). Pulse steroid therapy: methylprednisolone pulse, dexan pulse. Oral steroids:
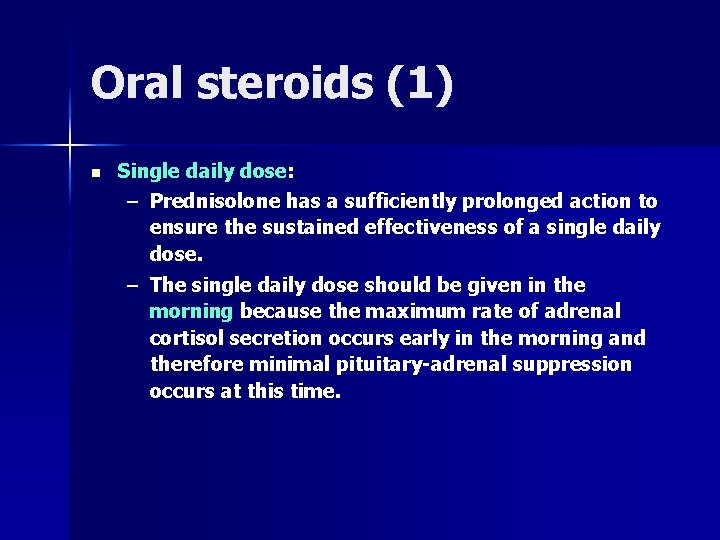
Oral steroids (1) n Single daily dose: – Prednisolone has a sufficiently prolonged action to ensure the sustained effectiveness of a single daily dose. – The single daily dose should be given in the morning because the maximum rate of adrenal cortisol secretion occurs early in the morning and therefore minimal pituitary-adrenal suppression occurs at this time.
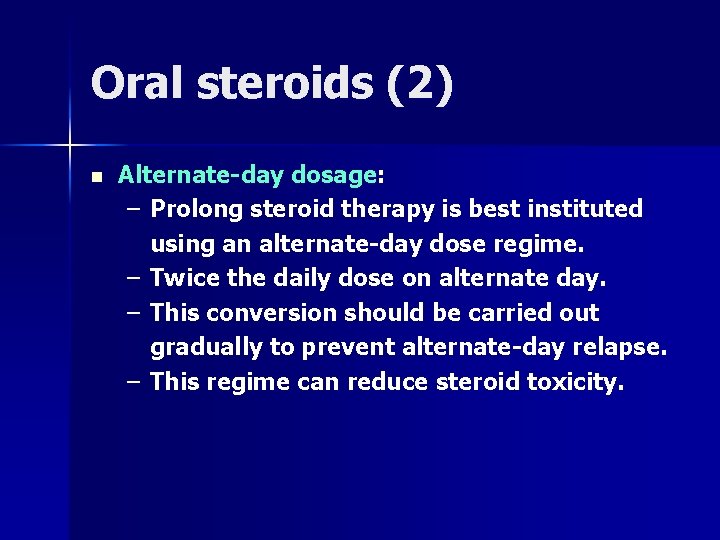
Oral steroids (2) n Alternate-day dosage: – Prolong steroid therapy is best instituted using an alternate-day dose regime. – Twice the daily dose on alternate day. – This conversion should be carried out gradually to prevent alternate-day relapse. – This regime can reduce steroid toxicity.
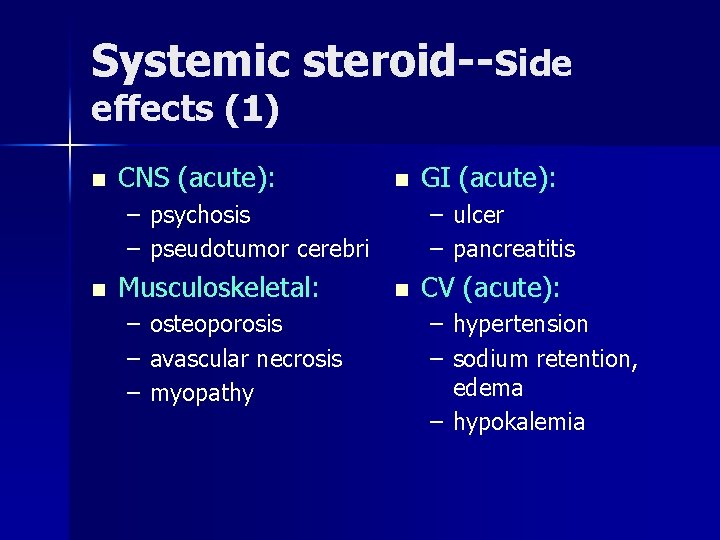
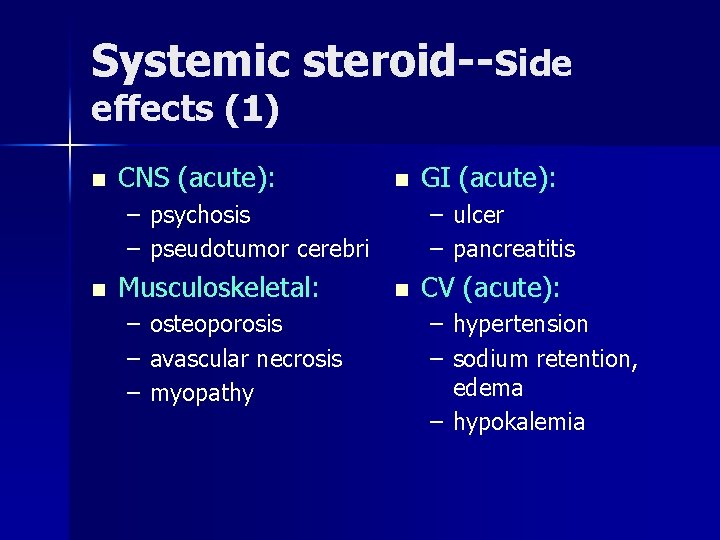
Systemic steroid--Side effects (1) n CNS (acute): n – psychosis – pseudotumor cerebri n Musculoskeletal: – osteoporosis – avascular necrosis – myopathy GI (acute): – ulcer – pancreatitis n CV (acute): – hypertension – sodium retention, edema – hypokalemia
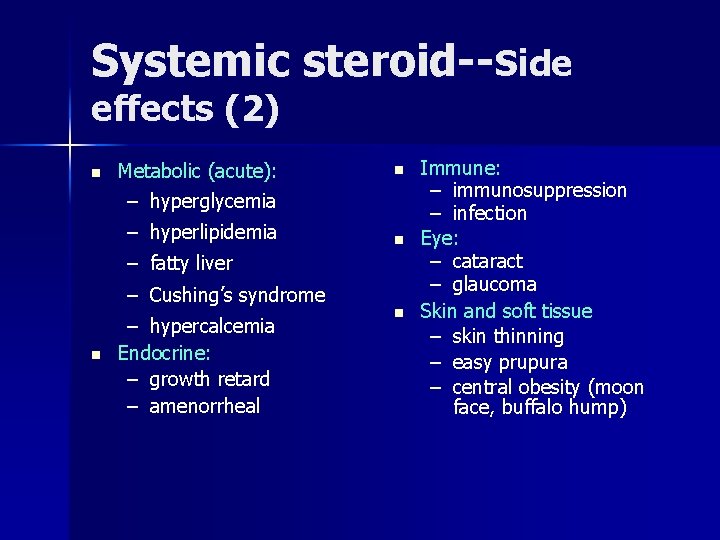
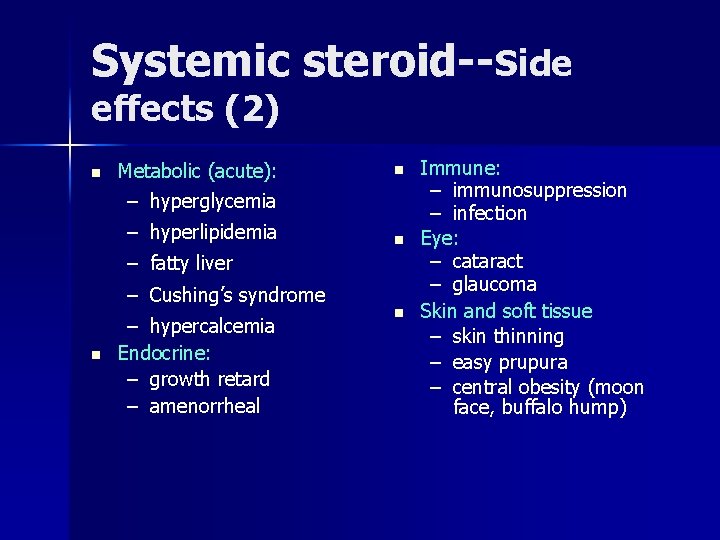
Systemic steroid--Side effects (2) n Metabolic (acute): n – hyperglycemia – hyperlipidemia n – fatty liver – Cushing’s syndrome n – hypercalcemia Endocrine: – growth retard – amenorrheal n Immune: – immunosuppression – infection Eye: – cataract – glaucoma Skin and soft tissue – skin thinning – easy prupura – central obesity (moon face, buffalo hump)