Cor Pulmonale Dr Megangela Christi Amores Definition Cor
- Slides: 13
Cor Pulmonale Dr. Meg-angela Christi Amores
Definition • Cor Pulmonale – pulmonary heart disease – dilation and hypertrophy of the right ventricle (RV) in response to diseases of the pulmonary vasculature and/or lung parenchyma. – excluded congenital heart disease and those diseases in which the right heart fails secondary to dysfunction of the left side of the heart
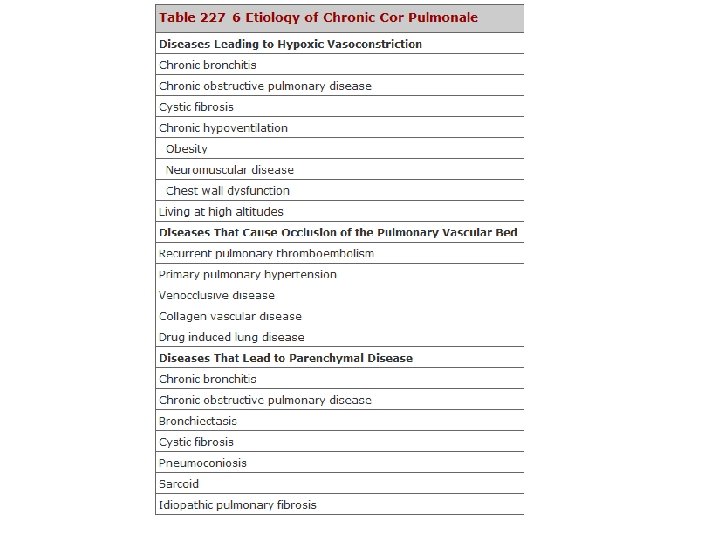
Etiology and Epidemiology • develops in response to acute or chronic changes in the pulmonary vasculature • Changes that are sufficient to cause pulmonary hypertension • Once patients with chronic pulmonary or pulmonary vascular disease develop cor pulmonale, their prognosis worsens
Pathophysiology • pulmonary hypertension that is sufficient to lead to RV dilation, with or without the development of concomitant RV hypertrophy • Right ventricle: thin walled, compliant – Better suited for high volumes than high pressure • Sustained pressure overload (pulm HPN) and increased vascular resistance causes RV to fail
Pathophysiology • Acute Cor Pulmonale – occurs after a sudden and severe stimulus with RV dilatation and failure but no RV hypertrophy • e. g massive pulmonary embolus • Chronic Cor pulmonale – more slowly evolving and slowly progressive pulmonary hypertension that leads to RV dilation and hypertrophy
Factors that determine severity • hypoxia secondary to alterations in gas exchange • Hypercapnia • Acidosis • alterations in RV volume overload that are affected by: • exercise, heart rate, polycythemia, or increased salt and retention because of a fall in cardiac output
Clinical presentation • Symptoms: – Dyspnea, the most common symptom – usually the result of the increased work of breathing secondary to changes in elastic recoil of the lung (fibrosing lung diseases) or altered respiratory mechanics – Orthopnea and paroxysmal nocturnal dyspnea are rarely symptoms of isolated right HF – reflect the increased work of breathing in the supine position that results from compromised excursion of the diaphragm
Clinical presentation • Symptoms: – Tussive or effort-related syncope – because of the inability of the RV to deliver blood adequately to the left side of the heart – Abdominal pain and ascites – Due to right heart failure – Lower extremity edema – secondary to neurohormonal activation, elevated RV filling pressures, or increased levels of carbon dioxide and hypoxia,
Clinical presentation • Signs – tachypnea – elevated jugular venous pressures – hepatomegaly – lower-extremity edema – Cyanosis is a late finding
Diagnosis • ECG – P pulmonale, right axis deviation, and RV hypertrophy • Chest X Ray – enlargement of the main pulmonary artery, hilar vessels, and the descending right pulmonary artery • Spiral CT – acute thromboembolic disease
Diagnosis • 2 D echo – measuring RV thickness and chamber dimensions • Doppler echocardiography – assess pulmonary artery pressures • MRI – assessing RV structure and function, particularly in patients who are difficult to image with 2 -D echocardiography because of severe lung disease
Treatment • Primary goal: target the underlying pulmonary disease • decrease in pulmonary vascular resistance and relieve the pressure overload on the RV • General principles: • decreasing the work of breathing using noninvasive mechanical ventilation, bronchodilation, and steroids • treating any underlying infection – Adequate oxygenation (oxygen saturation 90– 92%) will also decrease pulmonary vascular resistance and reduce the demands on the RV – Diuretics