COPD Review Progressive Syndrome Expiratory airflow obstruction Chronic
COPD Review
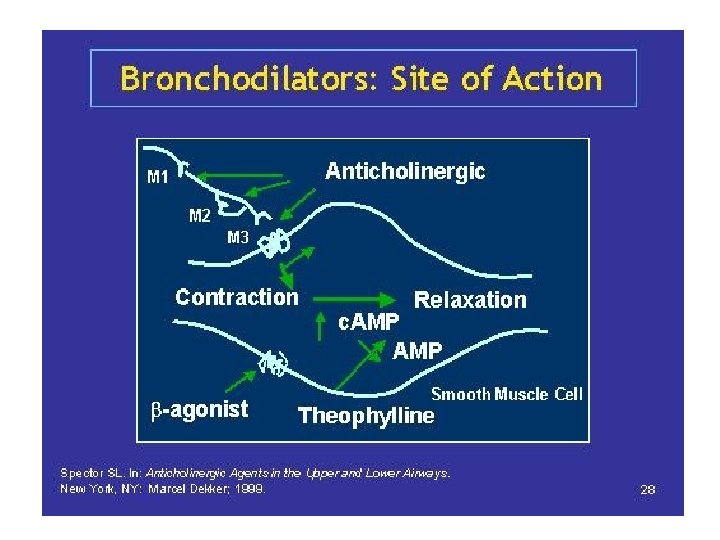
• • Progressive Syndrome Expiratory airflow obstruction Chronic airway and lung parenchyma inflammation
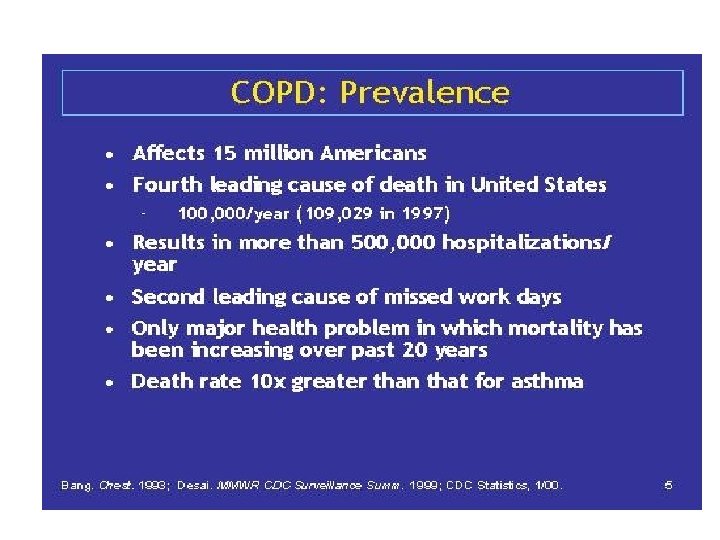
• Preventable, treatable • 24 million adults in US • 4 th leading cause of death in US: – Heart disease – Cancer – Stroke – COPD – Accidents – Diabetes
• GOLD: global initiative for chronic obstructive lung diseasae – Expiratory airflow not fully reversible – Progressive, association with an “abnormal” lung response to noxious gases and particles
• Two major clinical types – Chronic bronchitis: inflammation of small and medium sized airways – Leads to expiratory defect, chronic cough, sputum production and dyspnea
• Emphysema – Inflammation of lung parenchyma – Loss of elastic recoil of lungs – Airflow limitation – Hypoxemia – dyspnea
COPD • Irreversible airflow (as measured by FEV 1 or FEV 1/FVC) caused by: – Increased airway resistance in the conducting airways, or, – Increased lung compliance due to destruction of lung parenchyma/elasticity • Or a combination of both the above
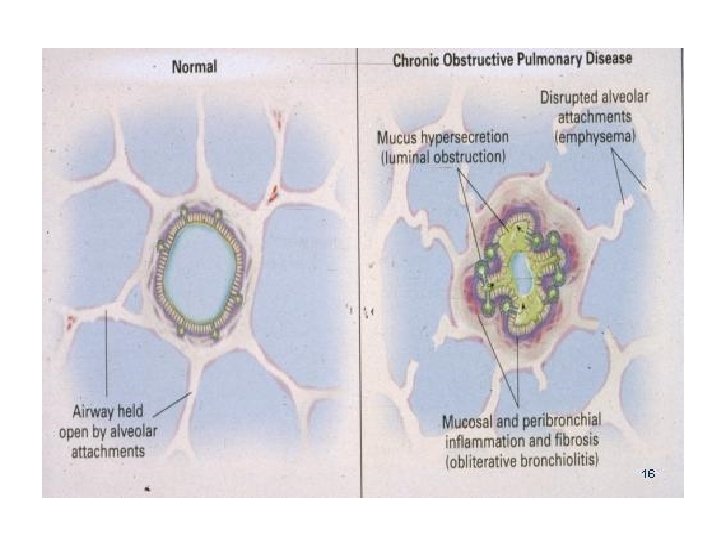
Chronic Bronchitis • Inflammation of the central airways (airways >4 mm diameter and peripheral airways < 2 mm) • Extends to gland ducts and into the mucus producing glands – This produces increase mucus – Defective mucociliary clearance – Disruption (destruction) of epithelial barrier
• Airflow obstruction occurs primarily in the small airways which are <2 mm diameter
Emphysema • Decrease in elastic recoil force needed to drive air out of lung (“paper sack”) • Centrilobular or centriacinar form is associated with cigarette smoking – Major destruction of the acinus at the respiratory bronchiole level
• Panlobular or panacinar form is associated with alpha-1 antitrypsin disease – Destruction of the entire acinus – Occurs as a result of an imbalance of proteolytic enzymes in lung tissue
• In both forms of the disease, the cause of COPD is inflammation, both in the airways and in lung tissue
Inflammation • Smoking, in • Chronic Bronchitis – Neutrophils and macrophages, lymphocytes • Emphysema – Cellular changes in terminal bronchioles – Destruction (protease enzymes) extracellular matrix of aleveoli – Ineffective repair mechanism
COPD vs Asthma • Asthma – Anatomical location of inflammation – With bronchodilators and steroids, lung function returns to normal or near-normal with occasional transient inflammation • COPD – Anatomical (airways and lung parenchyma) – Some degree of irreversible deterioration
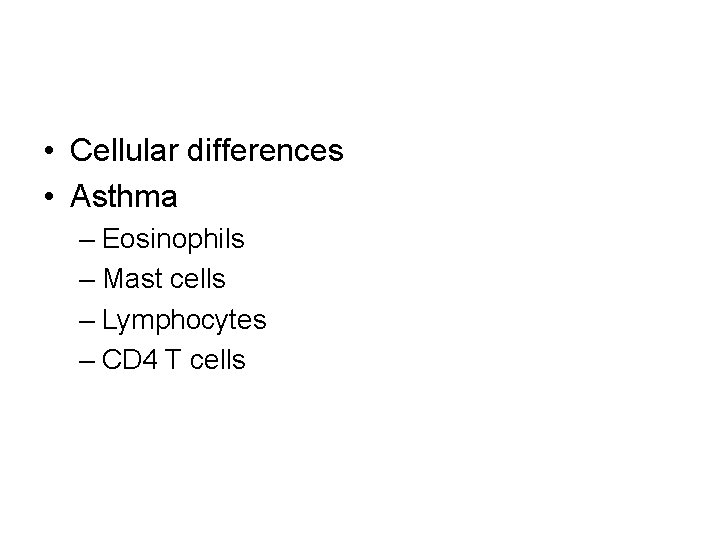
• Cellular differences • Asthma – Eosinophils – Mast cells – Lymphocytes – CD 4 T cells
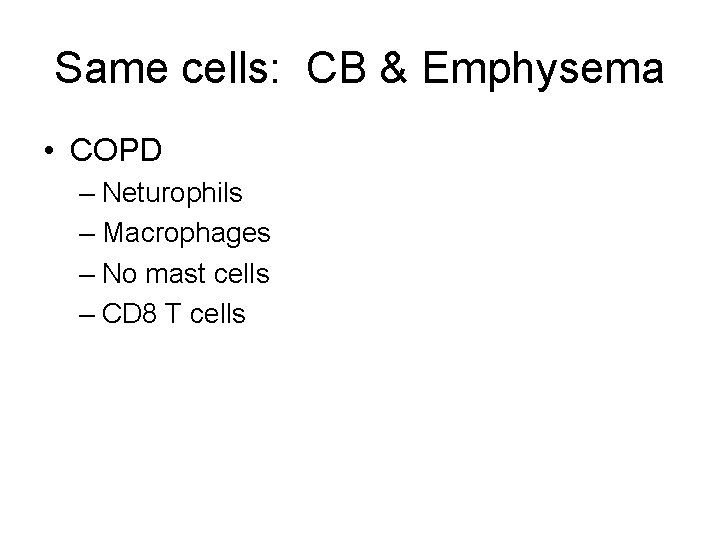
Same cells: CB & Emphysema • COPD – Neturophils – Macrophages – No mast cells – CD 8 T cells
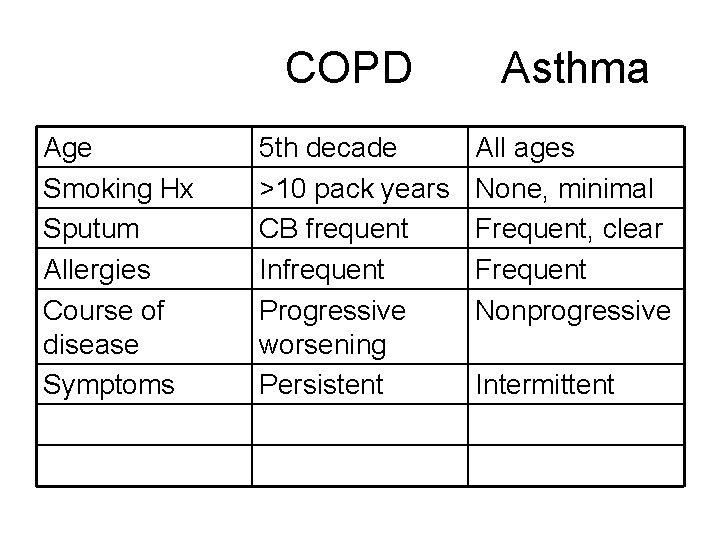
Age Smoking Hx Sputum Allergies Course of disease Symptoms COPD Asthma 5 th decade >10 pack years CB frequent Infrequent Progressive worsening Persistent All ages None, minimal Frequent, clear Frequent Nonprogressive Intermittent
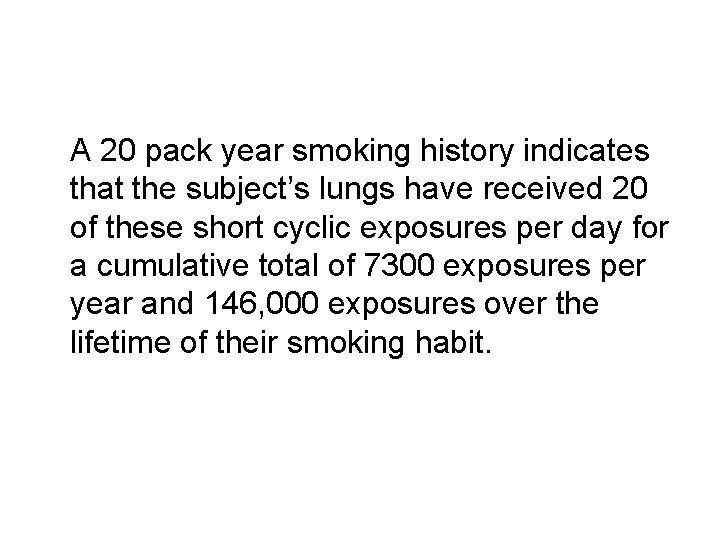
A 20 pack year smoking history indicates that the subject’s lungs have received 20 of these short cyclic exposures per day for a cumulative total of 7300 exposures per year and 146, 000 exposures over the lifetime of their smoking habit.
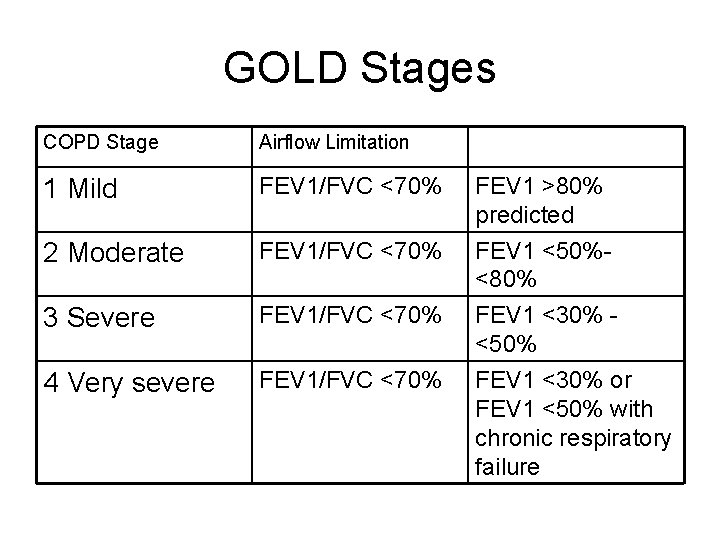
GOLD Stages COPD Stage Airflow Limitation 1 Mild FEV 1/FVC <70% FEV 1 >80% predicted 2 Moderate FEV 1/FVC <70% 3 Severe FEV 1/FVC <70% FEV 1 <50%<80% FEV 1 <30% <50% 4 Very severe FEV 1/FVC <70% FEV 1 <30% or FEV 1 <50% with chronic respiratory failure
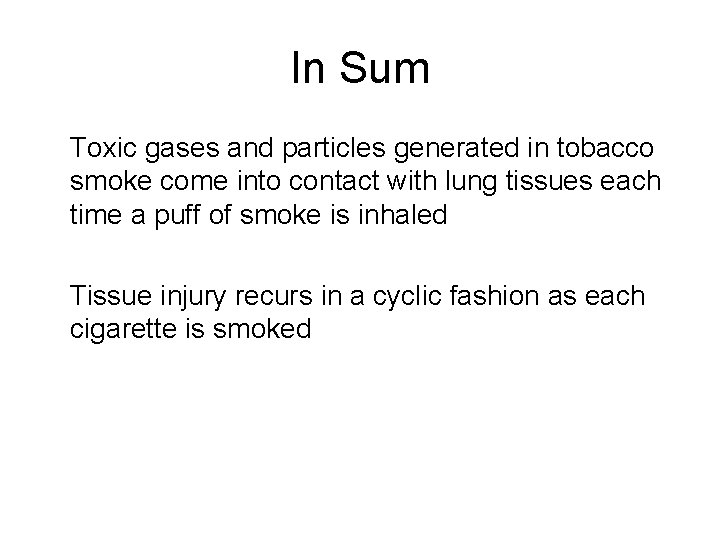
In Sum Toxic gases and particles generated in tobacco smoke come into contact with lung tissues each time a puff of smoke is inhaled Tissue injury recurs in a cyclic fashion as each cigarette is smoked
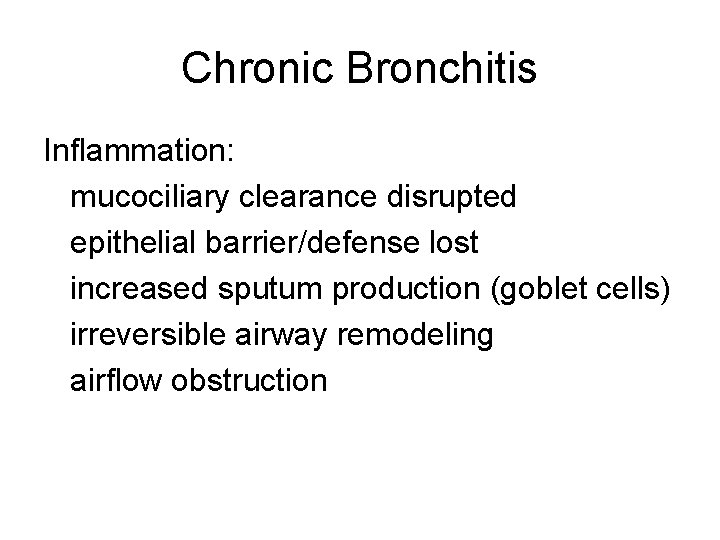
Chronic Bronchitis Inflammation: mucociliary clearance disrupted epithelial barrier/defense lost increased sputum production (goblet cells) irreversible airway remodeling airflow obstruction
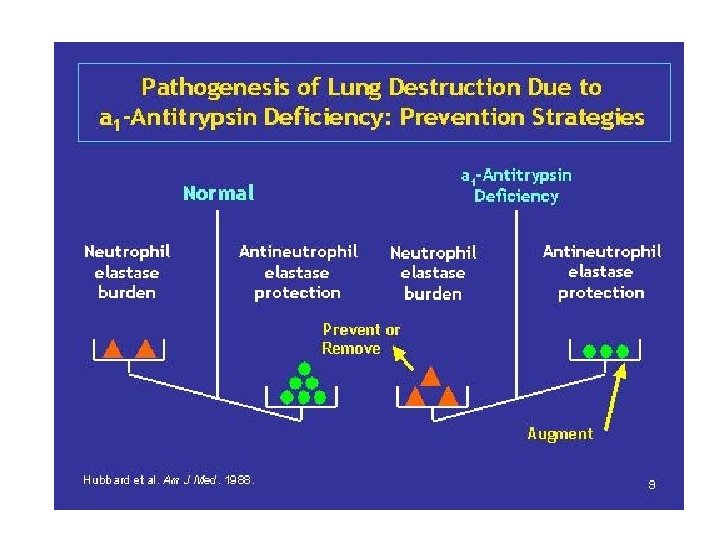
Emphysema In lung tissue, the chronic inhalation also causes inflammation, destroys elastic recoil, disrupts balance of protective, antiprotease enzymes proteinase-antiproteniase theory elastase-antielastase “extracellular matrix”
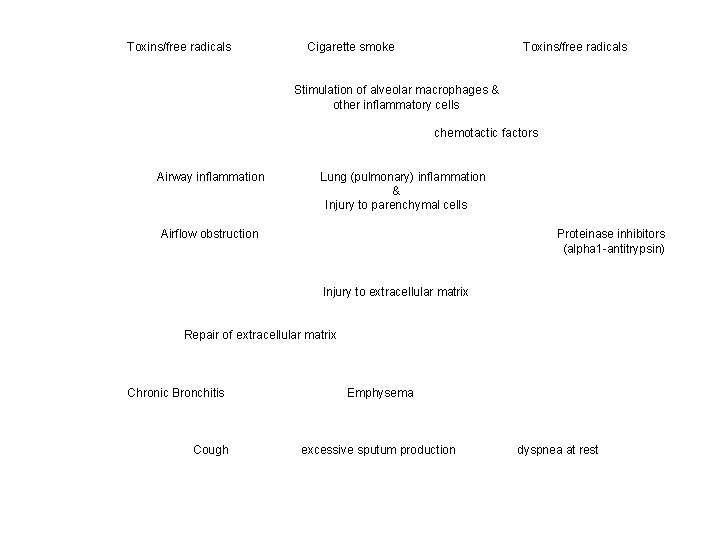
Toxins/free radicals Cigarette smoke Toxins/free radicals Stimulation of alveolar macrophages & other inflammatory cells chemotactic factors Airway inflammation Lung (pulmonary) inflammation & Injury to parenchymal cells Airflow obstruction Proteinase inhibitors (alpha 1 -antitrypsin) Injury to extracellular matrix Repair of extracellular matrix Chronic Bronchitis Cough Emphysema excessive sputum production dyspnea at rest
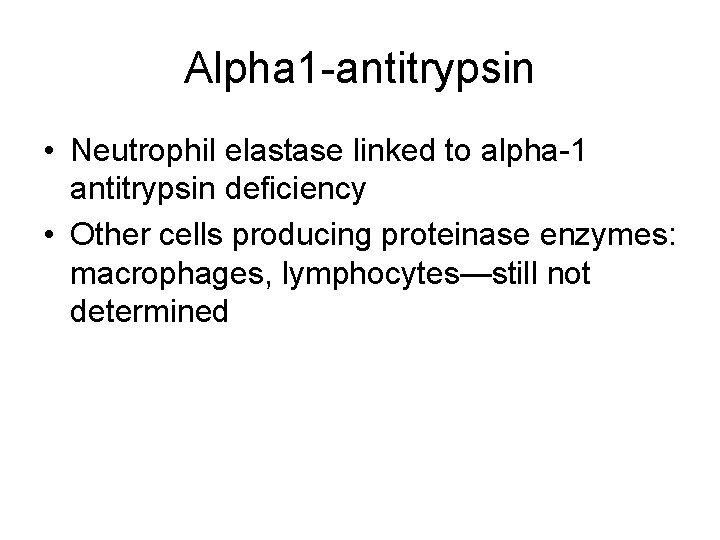
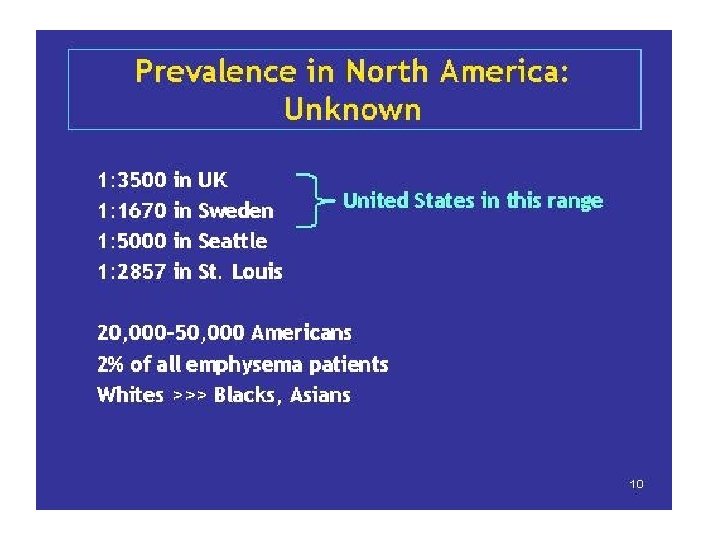
Alpha 1 -antitrypsin • Neutrophil elastase linked to alpha-1 antitrypsin deficiency • Other cells producing proteinase enzymes: macrophages, lymphocytes—still not determined
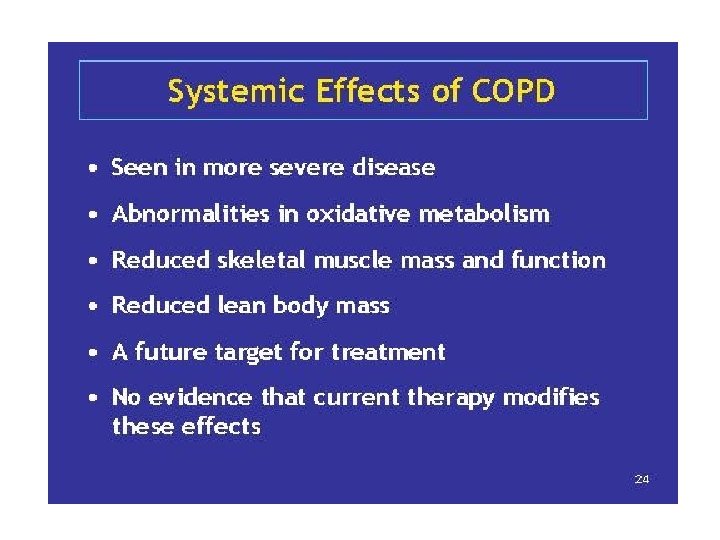
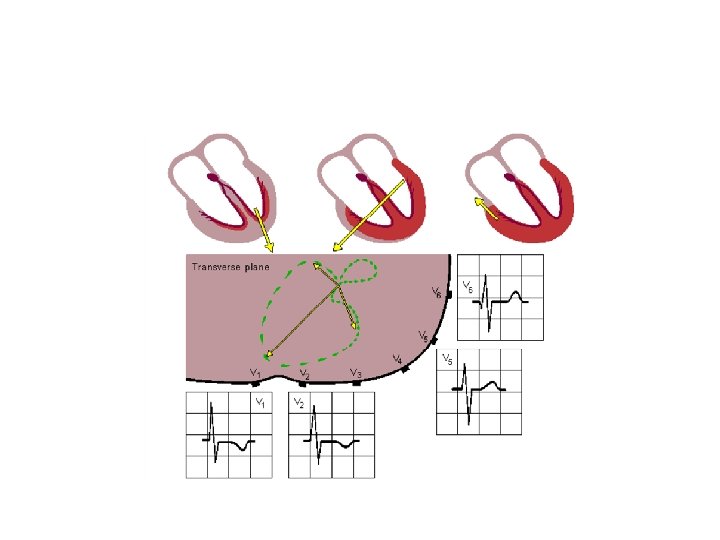
• Decreased airflow resistance (airways) and decreased elastic recoil lead to: • Hyperinflation • V/Q mismatching, which further leads to decreases in Pa 02, increases in Pa. C 02 with decreased ventilation
• In end-stage COPD – Cor pulmonale – Pulmonary vasoconstriction (in presence of chronic low Pa 02) – Increased pulmonary vascular resistance – Increased pressure, leading eventually to right heart enlargement
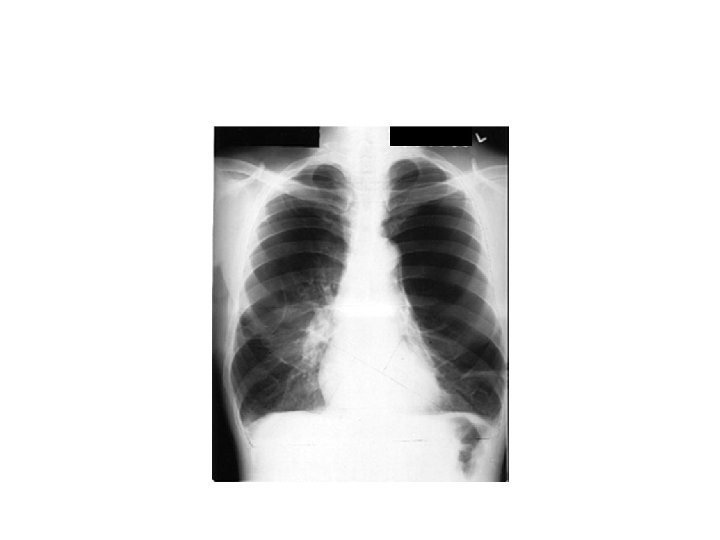
CXR
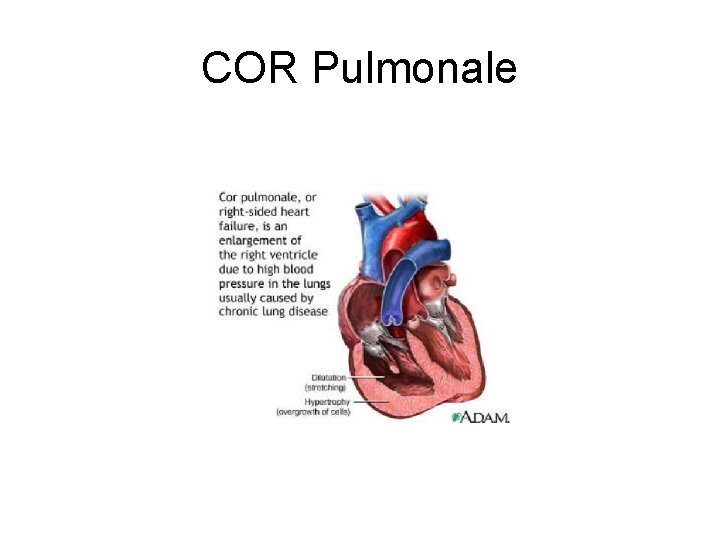
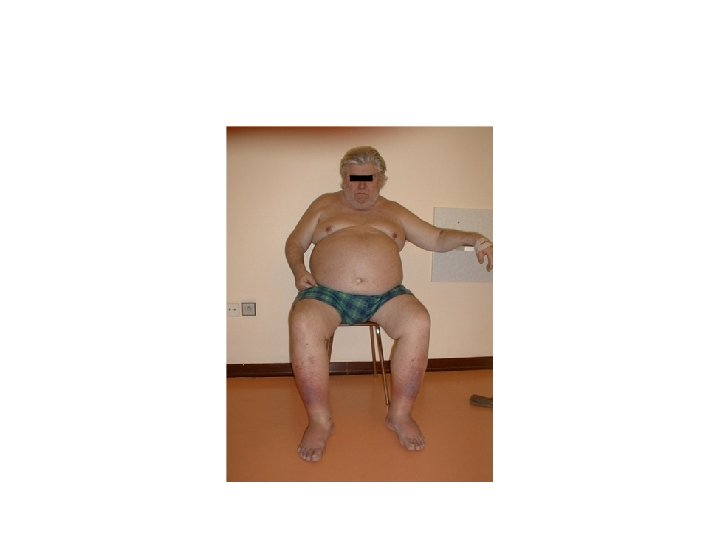
COR Pulmonale
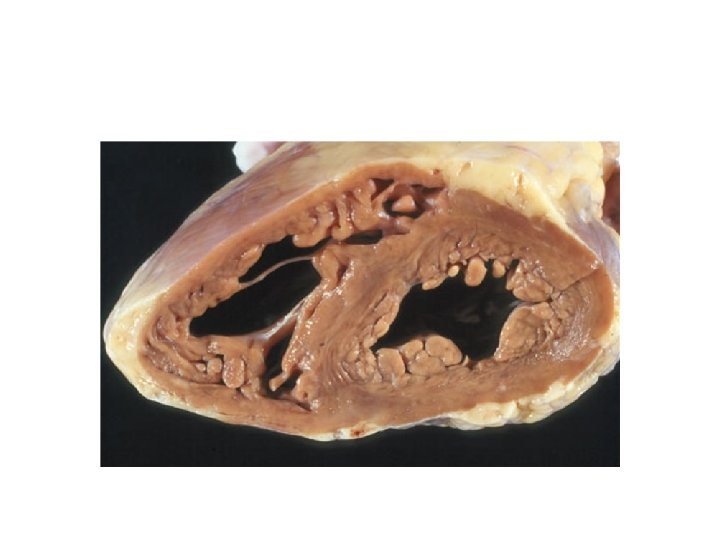
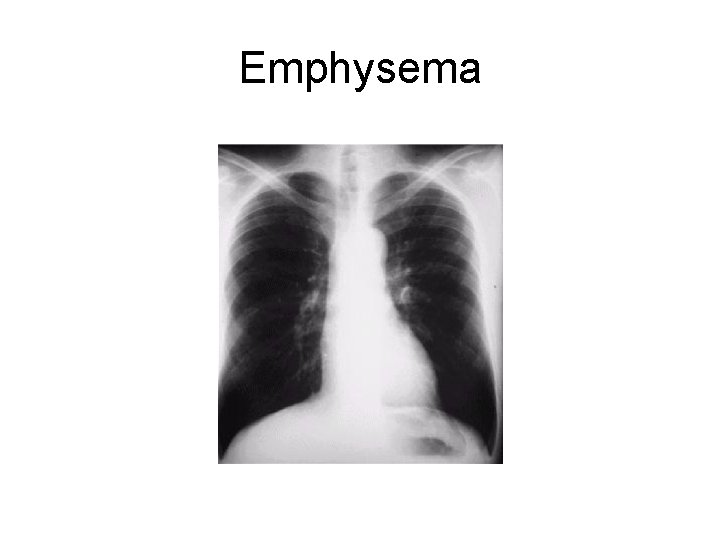
Emphysema
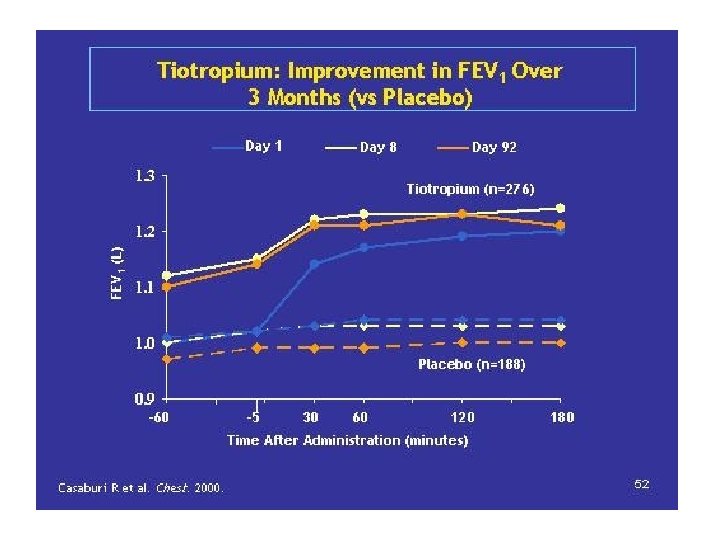
- Slides: 52