COPD Diagnosis Differential Diagnosis 1 Dr Mazen Qusaibaty
COPD: Diagnosis/ Differential Diagnosis 1 Dr Mazen Qusaibaty MD, DIS / Head Pulmonary and Internist Department Ibnalnafisse Hospital Ministry of Syrian health Email: qusaibaty@gmail. com
2 Suggestive of the diagnosis of COPD • The presence of symptoms compatible with chronic COPD ¶Dyspnea at rest or on exertion ¶Cough with or without sputum production ¶Progressive limitation of activity Modrykamien AM, Gudavalli R, Mc. Carthy K, et al. Detection of upper airway obstruction with spirometry results and the flow-volume loop: a comparison of quantitative and visual inspection criteria. Respir Care 2009; 54: 474
3 Suggestive of the diagnosis of COPD • A history of exposure to triggers of COPD ¶Tobacco smoke ¶Occupational dust ¶Indoor biomass smoke Modrykamien AM, Gudavalli R, Mc. Carthy K, et al. Detection of upper airway obstruction with spirometry results and the flow-volume loop: a comparison of quantitative and visual inspection criteria. Respir Care 2009; 54: 474
4 Suggestive of the diagnosis of COPD • A family history of chronic lung disease Modrykamien AM, Gudavalli R, Mc. Carthy K, et al. Detection of upper airway obstruction with spirometry results and the flow-volume loop: a comparison of quantitative and visual inspection criteria. Respir Care 2009; 54: 474
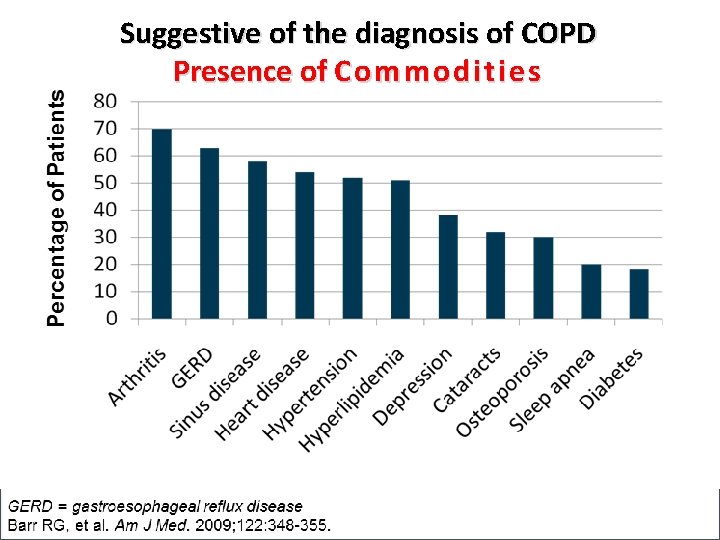
Suggestive of the diagnosis of COPD Presence of Commodities
Confirmation of COPD
7 v Spirometry is essential for the diagnosis of COPD
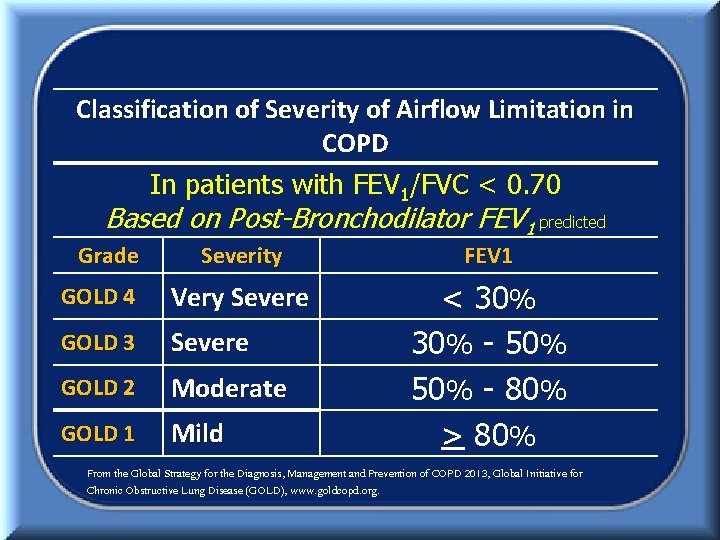
8 Classification of Severity of Airflow Limitation in COPD In patients with FEV 1/FVC < 0. 70 Based on Post-Bronchodilator FEV 1 predicted Grade Severity FEV 1 GOLD 4 Very Severe GOLD 3 Severe GOLD 2 Moderate GOLD 1 Mild < 30% - 50% - 80% > 80% From the Global Strategy for the Diagnosis, Management and Prevention of COPD 2013, Global Initiative for Chronic Obstructive Lung Disease (GOLD), www. goldcopd. org.
9 Confirmation of COPD • Absence of an alternative explanation for the symptoms and airflow limitation
• Consideration the cause because ¶Mitigation of ongoing exposures may reduce disease progression 10
• Consideration the cause because ¶Long-term cigarette smoking ¶Underlying asthma ¶Workplace exposures ¶Indoor use of biomass fuel ¶A prior history of tuberculosis ¶Familial predisposition 11
Differential Diagnosis
Chronic obstructive asthma
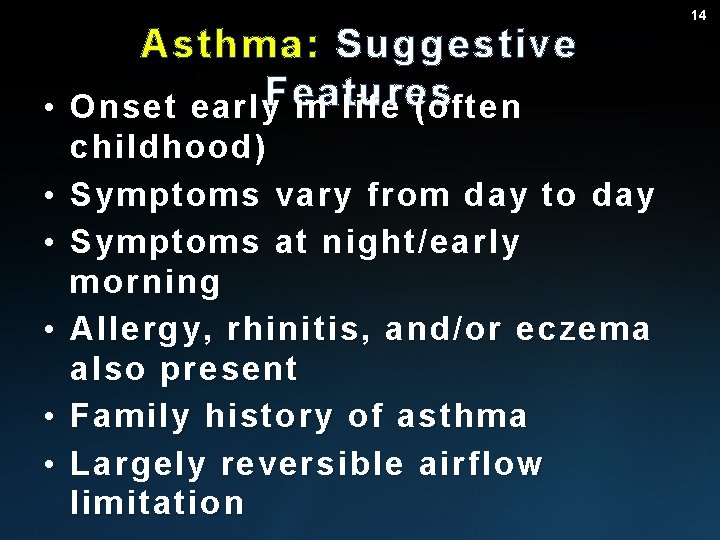
Asthma: Suggestive • Onset early. Features in life (often • • • childhood) Symptoms vary from day to day Symptoms at night/early morning Allergy, rhinitis, and/or eczema also present Family history of asthma Largely reversible airflow limitation 14
Chronic obstructive asthma • In some patients with chronic asthma, a clear distinction from COPD is not possible
Chronic obstructive asthma • A patient, who has had atopic asthma since childhood and smoked cigarettes for 15 years in their twenties and thirties ¶Could present in their fifties with a combination of asthma and COPD
Chronic bronchitis with normal spirometry
18 Chronic bronchitis with normal spirometry • A small portion of cigarette smokers have a chronic productive cough for three months in two successive years ¶But do not have airflow limitation on pulmonary function tests
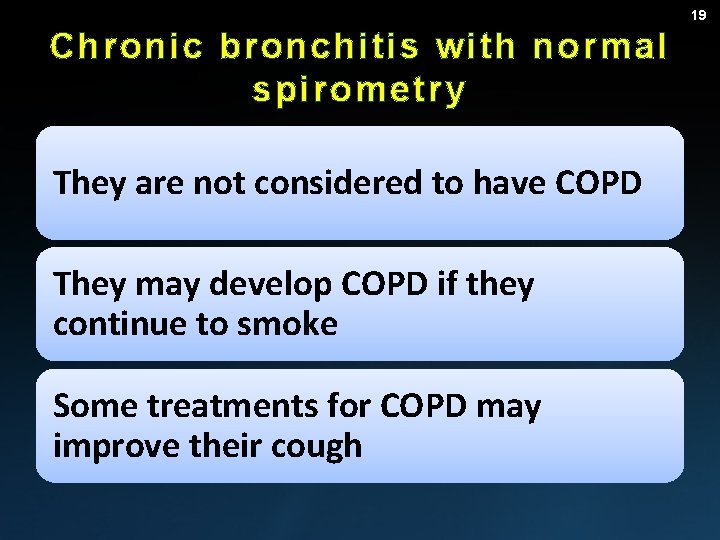
19 Chronic bronchitis with normal spirometry They are not considered to have COPD They may develop COPD if they continue to smoke Some treatments for COPD may improve their cough
Central Airway Stenosis
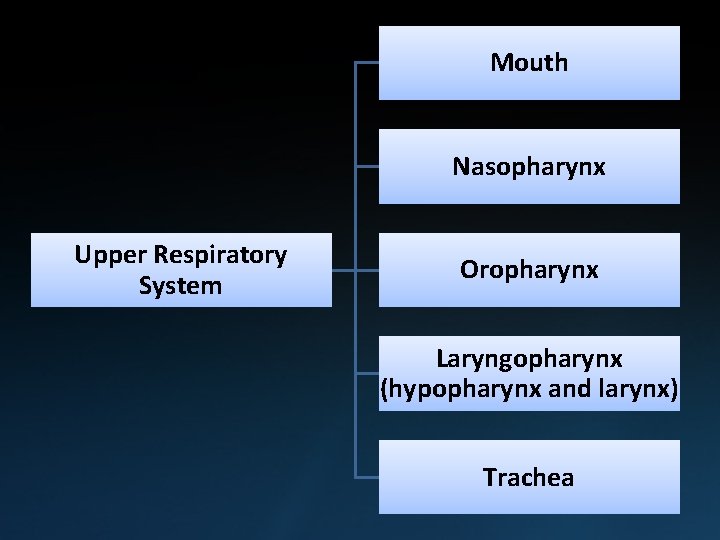
Mouth Nasopharynx Upper Respiratory System Oropharynx Laryngopharynx (hypopharynx and larynx) Trachea
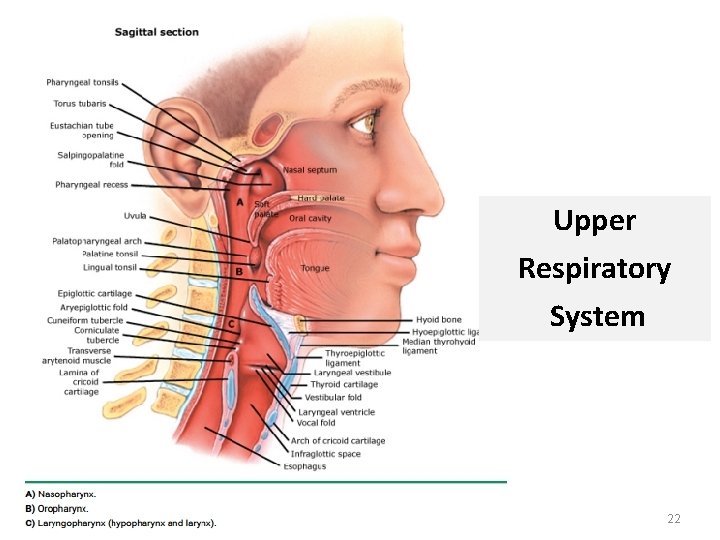
Upper Respiratory System 22
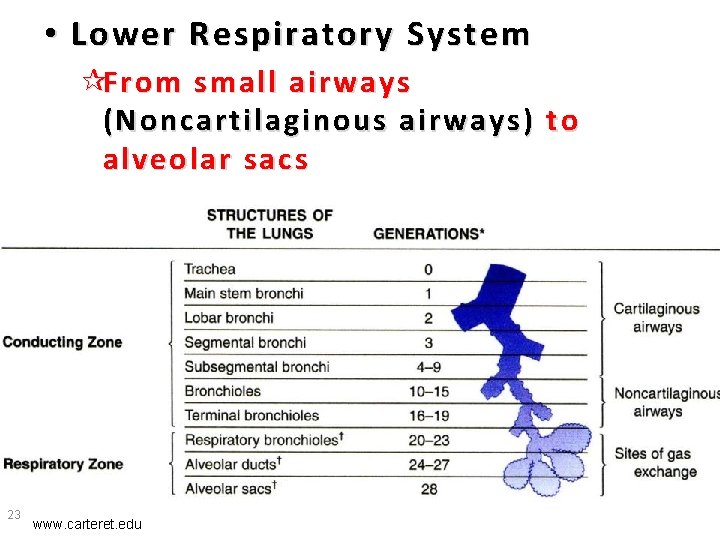
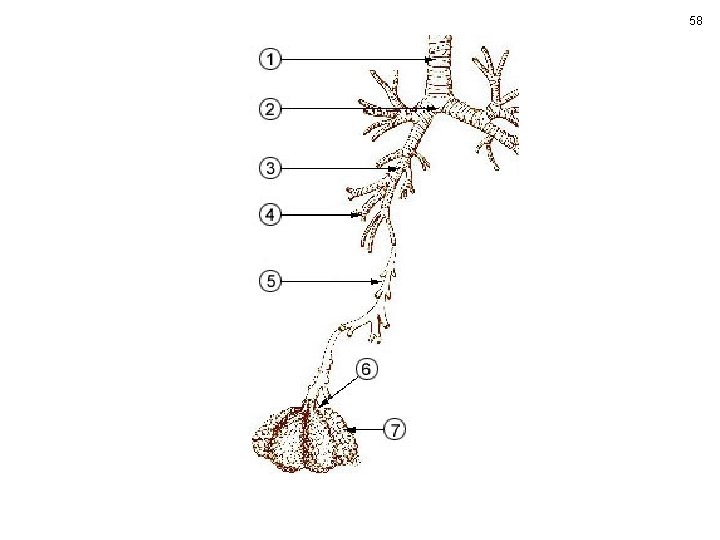
• Lower Respiratory System ¶From small airways (Noncartilaginous airways) to alveolar sacs 23 www. carteret. edu
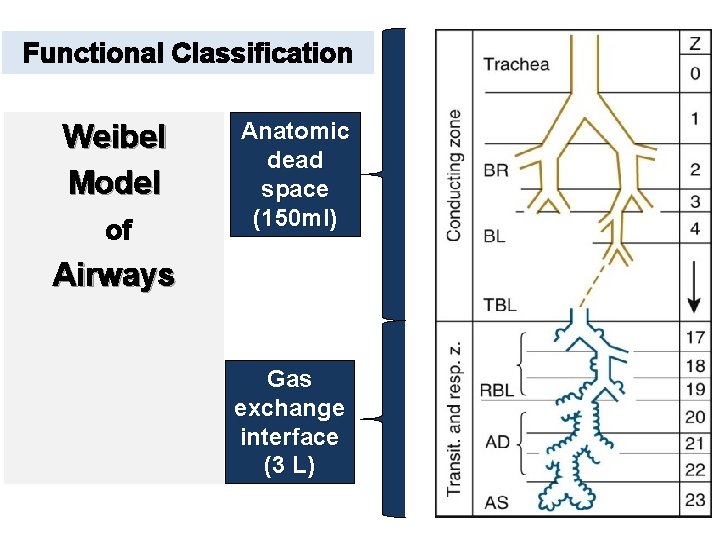
Functional Classification Weibel Model of Anatomic dead space (150 ml) Airways Gas exchange interface (3 L)
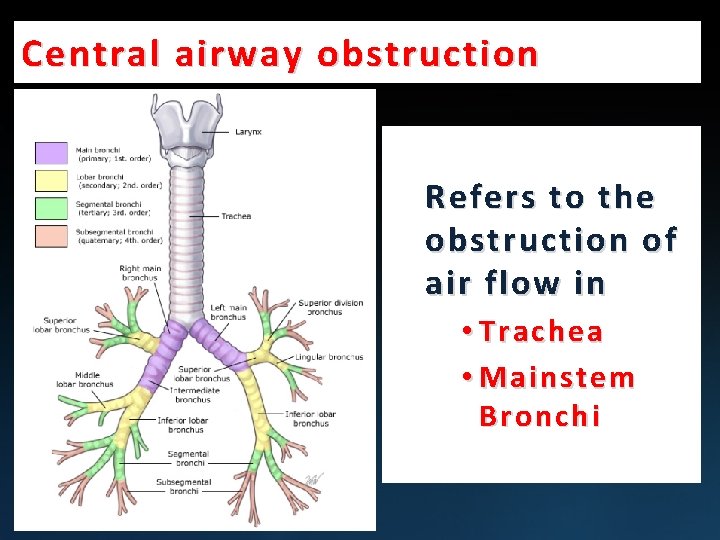
Central airway obstruction Refers to the obstruction of air flow in • Trachea • Mainstem Bronchi
26 Central airway stenosis Numerous Benign and Malignant processes Slowly progressive dyspnea on exertion followed by dyspnea with minimal activity
27 Central airway stenosis • Bronchogenic or metastatic cancer • Lymphadenopathy • Scarring from endotracheal tube
28 Central airway stenosis Suggestive Features • Monophonic wheeze or stridor • Slowly progressive dyspnea on exertion followed by dyspnea with minimal activity
29 Central airway stenosis Suggestive Features • Variable inspiratory or fixed slowing on flow volume loop
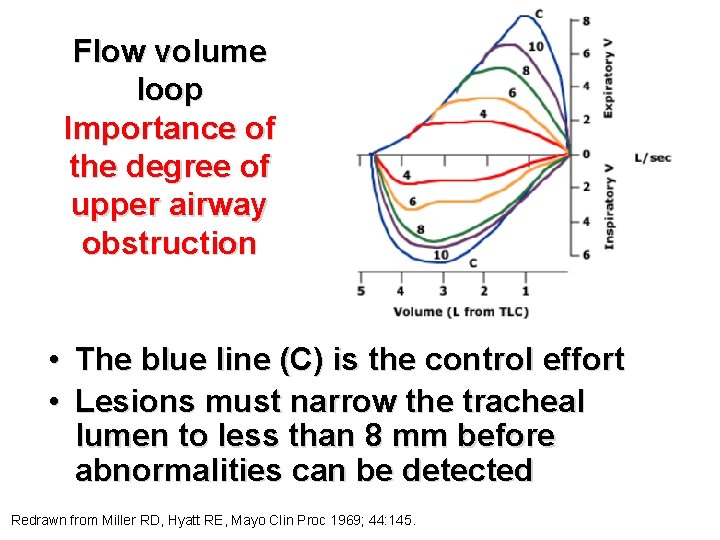
Flow volume loop Importance of the degree of upper airway obstruction • The blue line (C) is the control effort • Lesions must narrow the tracheal lumen to less than 8 mm before abnormalities can be detected Redrawn from Miller RD, Hyatt RE, Mayo Clin Proc 1969; 44: 145.
31 Central airway stenosis • Symptoms are minimally improved by inhaled bronchodilator
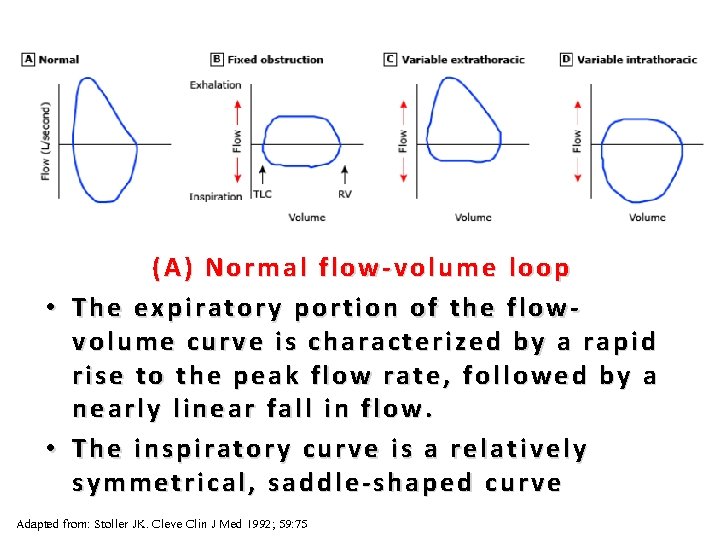
32 (A) Normal flow-volume loop • The expiratory portion of the flowvolume curve is characterized by a rapid rise to the peak flow rate, followed by a nearly linear fall in flow. • The inspiratory curve is a relatively symmetrical, saddle-shaped curve Adapted from: Stoller JK. Cleve Clin J Med 1992; 59: 75
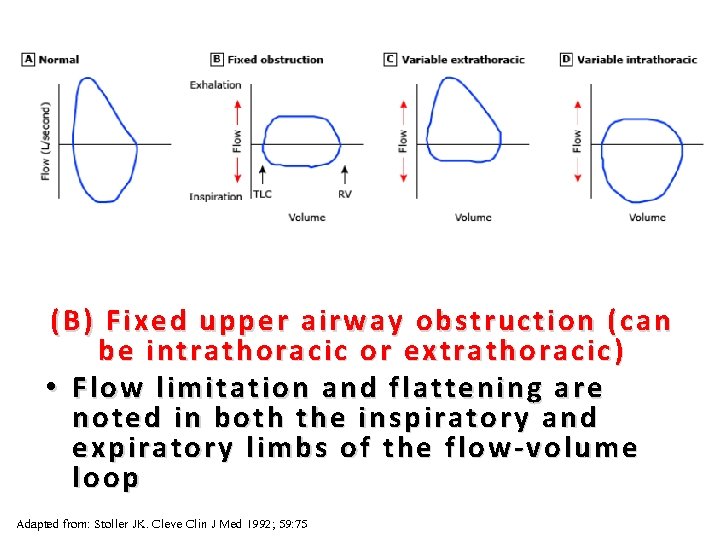
33 (B) Fixed upper airway obstruction (can be intrathoracic or extrathoracic ) • Flow limitation and flattening are noted in both the inspiratory and expiratory limbs of the flow-volume loop Adapted from: Stoller JK. Cleve Clin J Med 1992; 59: 75
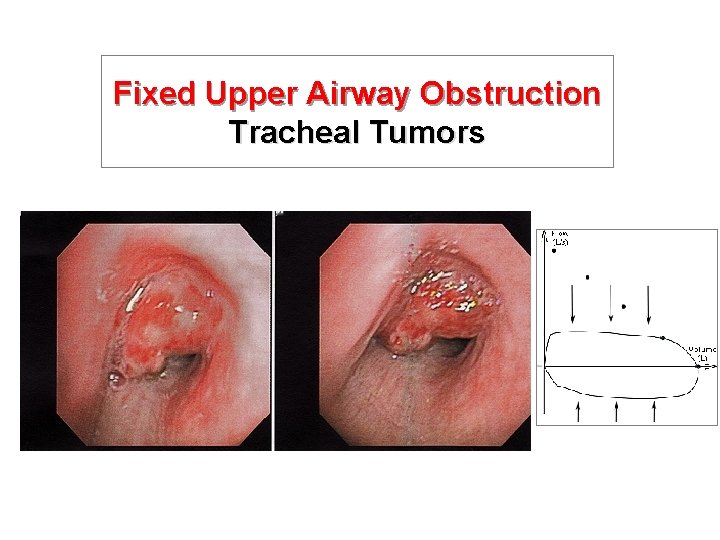
Fixed Upper Airway Obstruction Tracheal Tumors
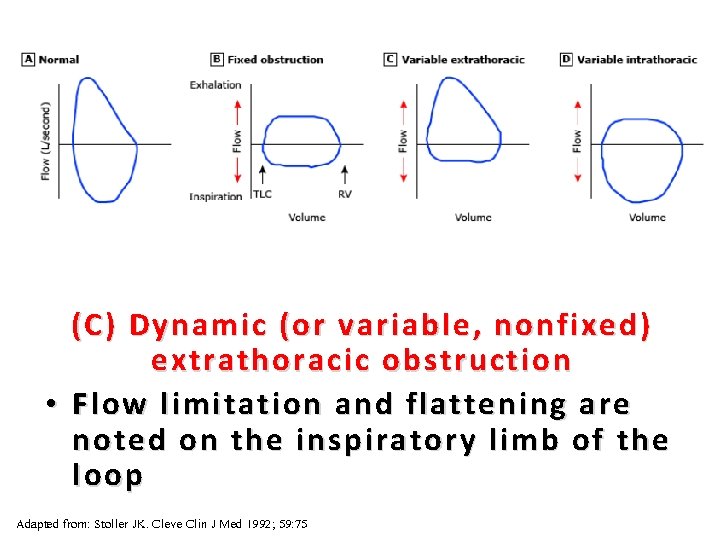
35 (C ) Dynamic (or variable, nonfixed) extrathoracic obstruction • Flow limitation and flattening are noted on the inspiratory limb of the loop Adapted from: Stoller JK. Cleve Clin J Med 1992; 59: 75
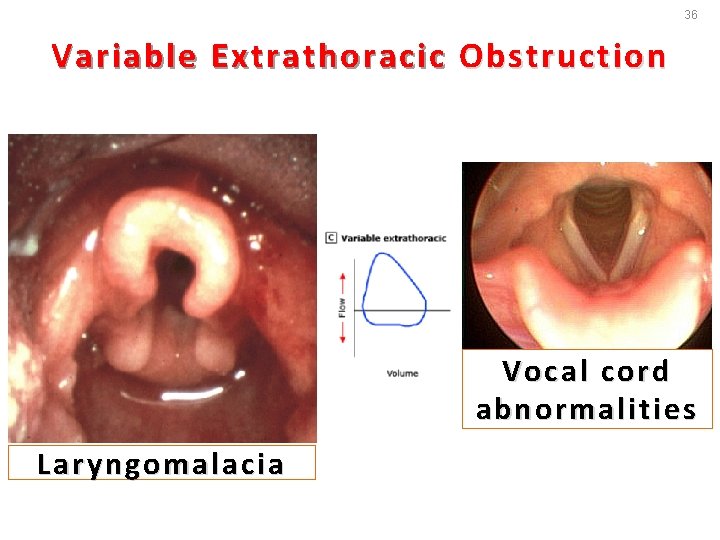
36 Variable Extrathoracic Obstruction Vocal cord abnormalities Laryngomalacia
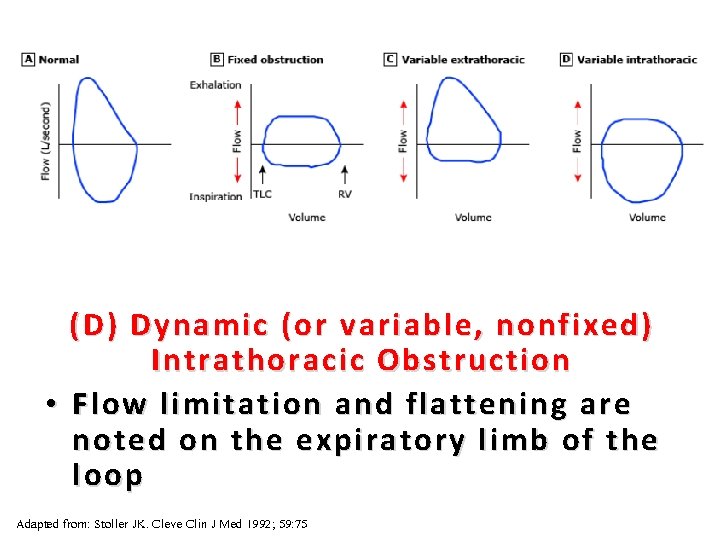
37 (D) Dynamic (or variable, nonfixed) Intrathoracic Obstruction • Flow limitation and flattening are noted on the expiratory limb of the loop Adapted from: Stoller JK. Cleve Clin J Med 1992; 59: 75
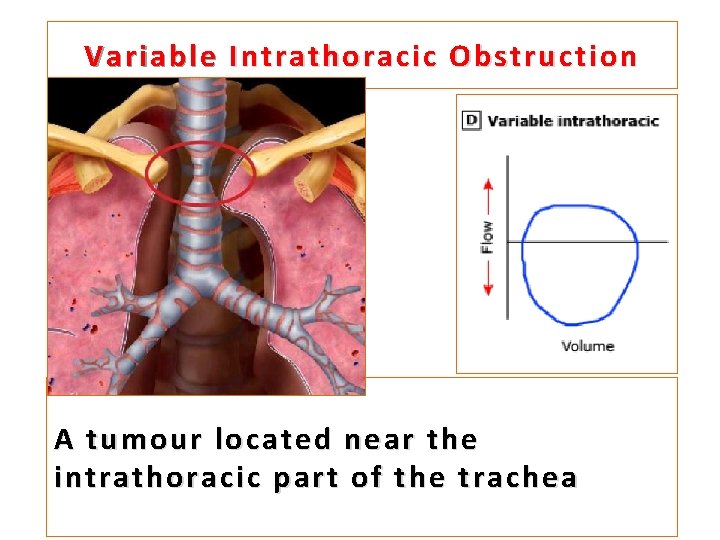
Variable Intrathoracic Obstruction A tumour located near the intrathoracic part of the trachea
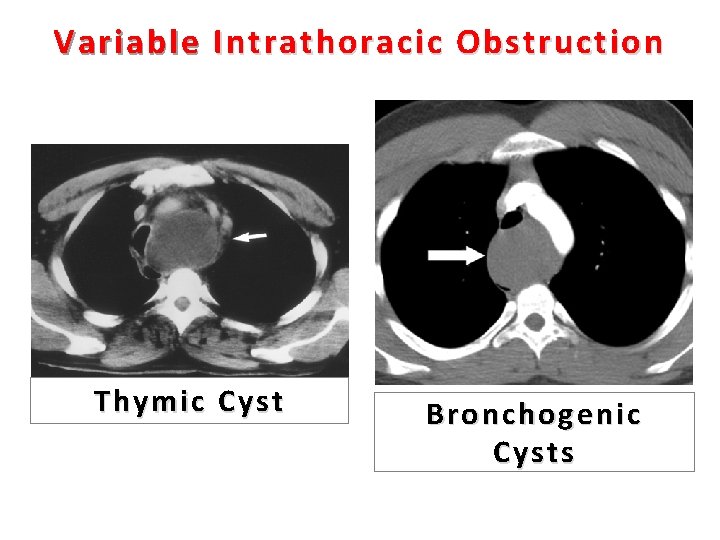
Variable Intrathoracic Obstruction Thymic Cyst Bronchogenic Cysts
40 Central airway stenosis Suggestive Features • Chest radiograph often normal • Airway narrowing on three dimensional reconstruction of HRCT scan
A high resolution CT scan with three-dimensional reconstruction can be helpful
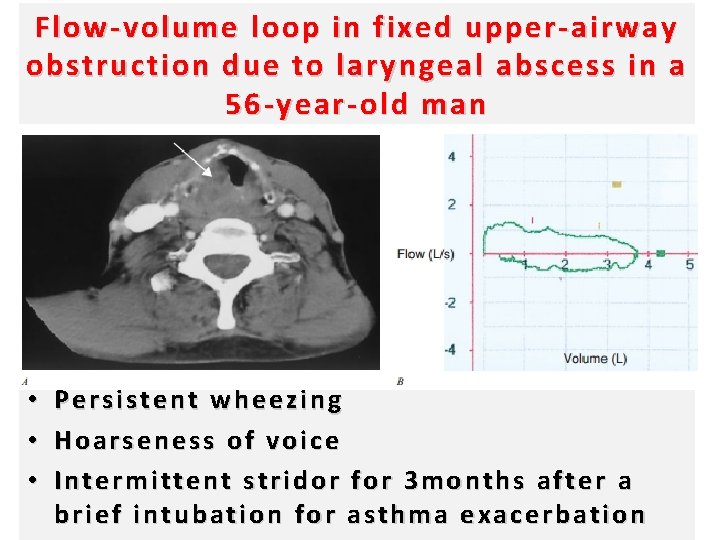
Flow-volume loop in fixed upper-airway obstruction due to laryngeal abscess in a 56 -year-old man • Persistent wheezing • Hoarseness of voice • Intermittent stridor for 3 months after a brief intubation for asthma exacerbation
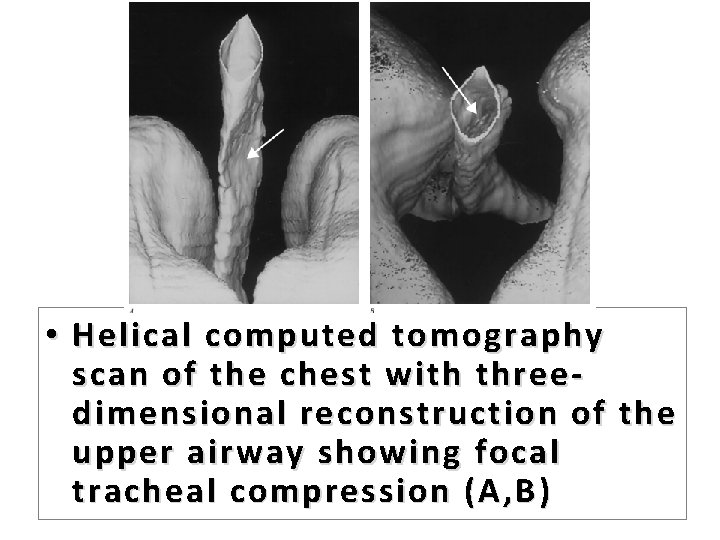
• Helical computed tomography scan of the chest with threedimensional reconstruction of the upper airway showing focal tracheal compression (A, B )
Bronchiectasis 44
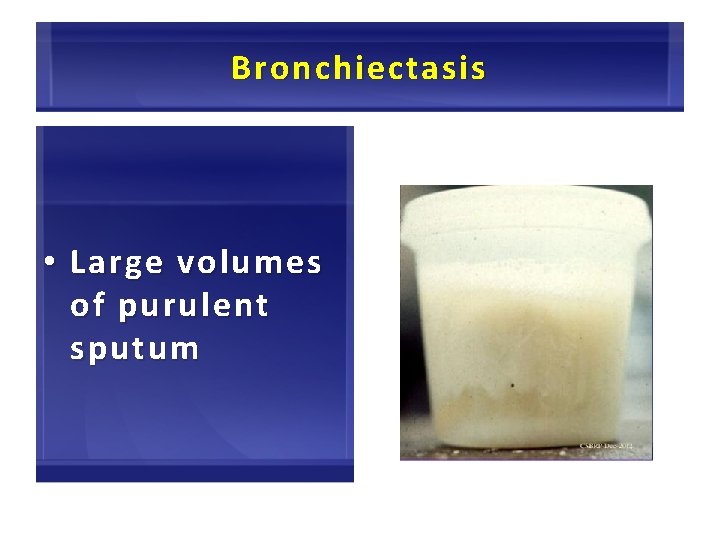
Bronchiectasis • Large volumes of purulent sputum 45
Bronchiectasis • Commonly associated with recurrent or persistent bacterial infection 46
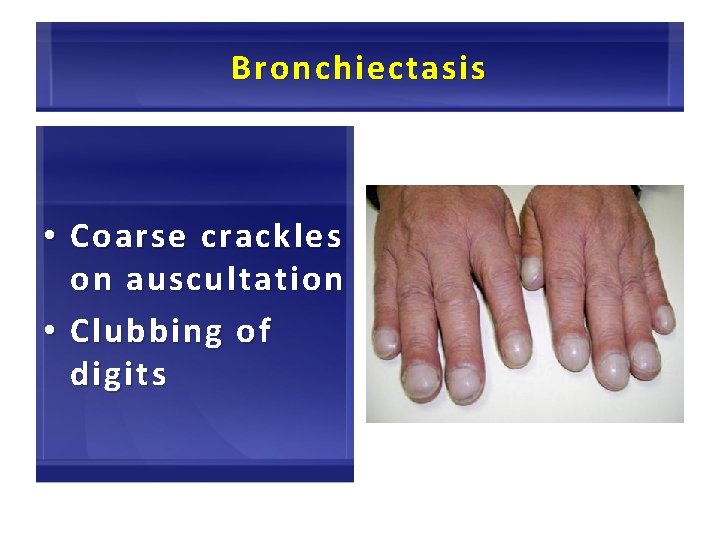
Bronchiectasis • Coarse crackles on auscultation • Clubbing of digits 47
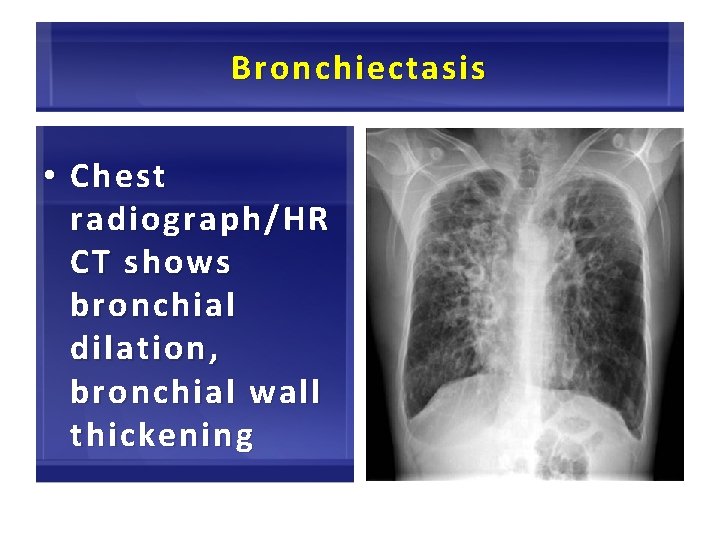
Bronchiectasis • Chest radiograph/HR CT shows bronchial dilation , bronchial wall thickening 48
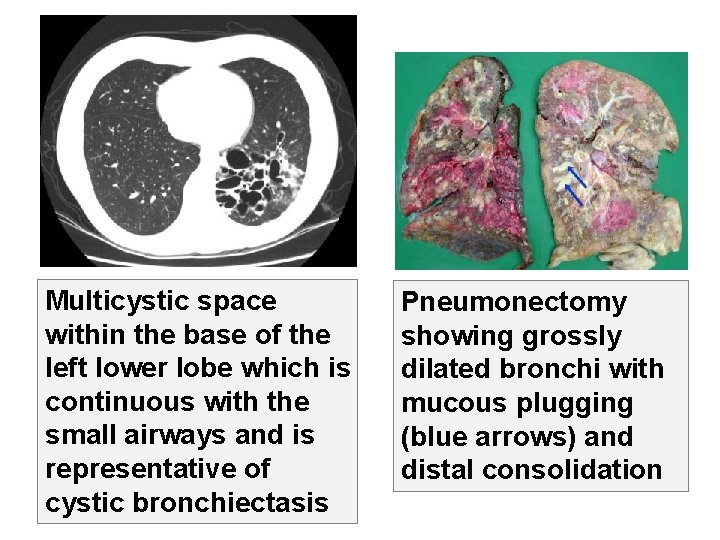
49 Multicystic space within the base of the left lower lobe which is continuous with the small airways and is representative of cystic bronchiectasis Pneumonectomy showing grossly dilated bronchi with mucous plugging (blue arrows) and distal consolidation
Heart Failure 50
Heart Failure • Fine basilar crackles on auscultation 51
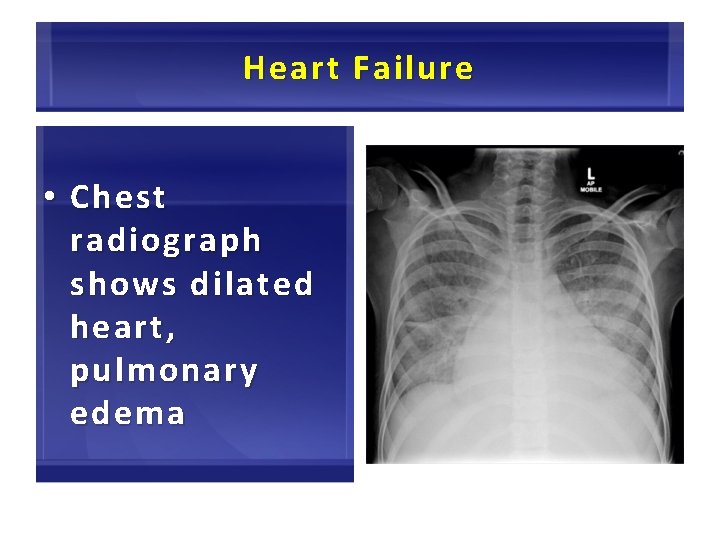
Heart Failure • Chest radiograph shows dilated heart, pulmonary edema 52
Heart Failure • Pulmonary function tests typically indicate: ¶Vo lum e Volume restriction ¶Airflo w Airflow limit l imit ation can sometimes e s ometimes bbe seen s een 53
Tuberculosis 54
55 Tuberculosis • In an area endemic for tuberculosis • The overall prevalence of airflow obstruction was 31 percent among those with a past history of tuberculosis compared with 14 percent among those without
56 Tuberculosis • Tuberculosis is both a risk factor for COPD and a potential comorbidity Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: Revised 2015. Global Initiative for Chronic Obstructive Lung Disease (GOLD). www. goldcopd. org
Constrictive Bronchiolitis 57
58
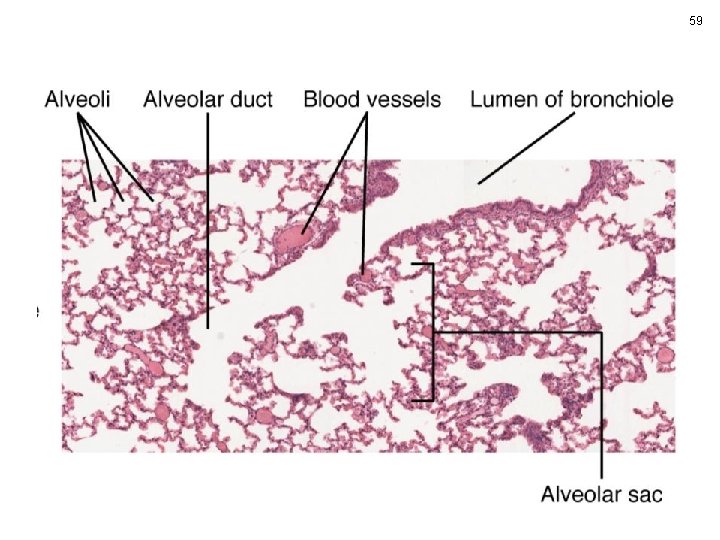
59
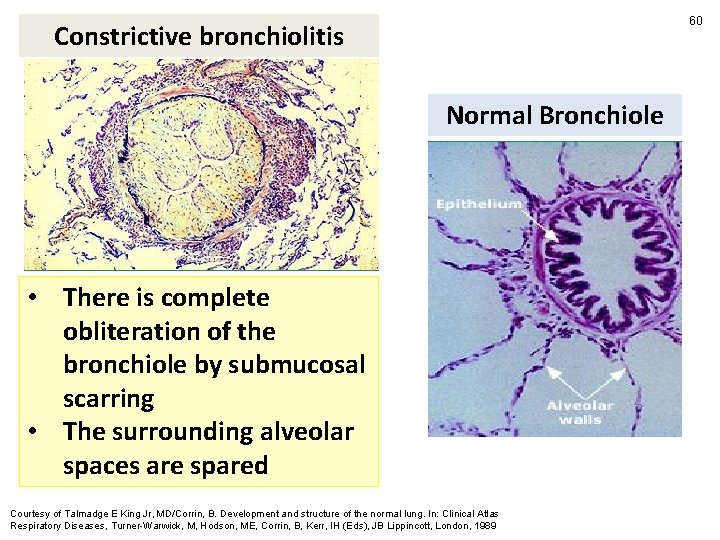
60 Constrictive bronchiolitis Normal Bronchiole • There is complete obliteration of the bronchiole by submucosal scarring • The surrounding alveolar spaces are spared Courtesy of Talmadge E King Jr, MD/Corrin, B. Development and structure of the normal lung. In: Clinical Atlas Respiratory Diseases, Turner-Warwick, M, Hodson, ME, Corrin, B, Kerr, IH (Eds), JB Lippincott, London, 1989
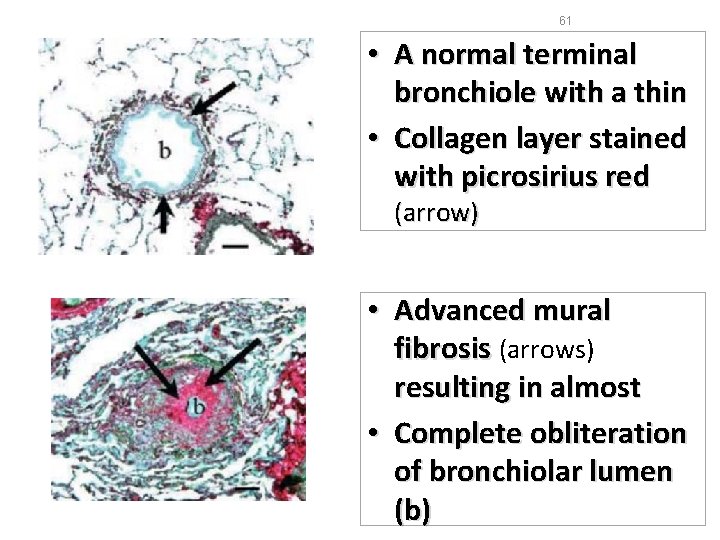
61 • A normal terminal bronchiole with a thin • Collagen layer stained with picrosirius red (arrow) • Advanced mural fibrosis (arrows) resulting in almost • Complete obliteration of bronchiolar lumen (b)
62 Constrictive Bronchiolitis • Onset in younger age, nonsmokers
Conditions associated with the histologic finding of constrictive bronchiolitis 63
64 Inhalation of Dusts • Mineral Dusts ¶Asbestos ¶Silica ¶Iron oxide ¶Aluminum oxide ¶Talc ¶Mica ¶Coal Adapted from Myers JL, Colby TV, Clin Chest Med 1993; 14: 611.
65 Inhalation of Toxins • Toxins ¶NO 2 ¶Sulfur dioxide ¶Ammonia ¶Chlorine ¶Phosgene Adapted from Myers JL, Colby TV, Clin Chest Med 1993; 14: 611.
66 Constrictive Bronchiolitis • Drug reaction • Infection ¶Viral ¶Mycoplasma • Connective tissue disease ¶Especially Rheumatoid Arthritis Adapted from Myers JL, Colby TV, Clin Chest Med 1993; 14: 611.
67 Constrictive Bronchiolitis • Chronic rejection in heartlung, and bone marrow transplant recipients • Hypersensitivity reactions • Ulcerative colitis • Idiopathic Adapted from Myers JL, Colby TV, Clin Chest Med 1993; 14: 611.
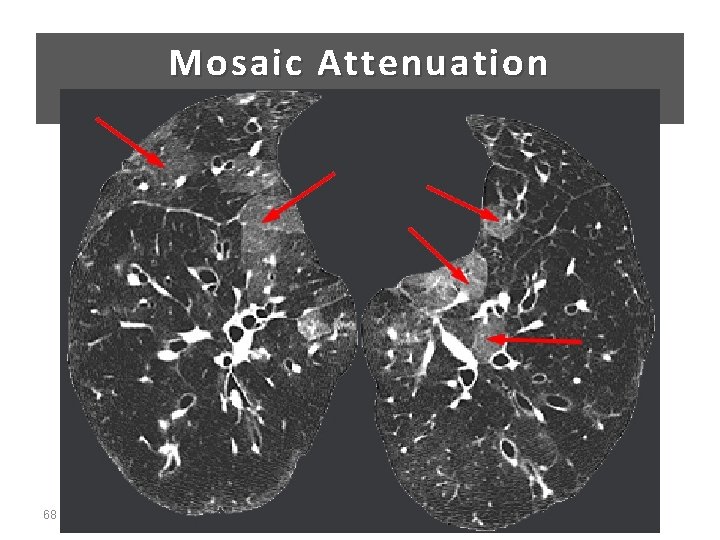
Mosaic Attenuation 68
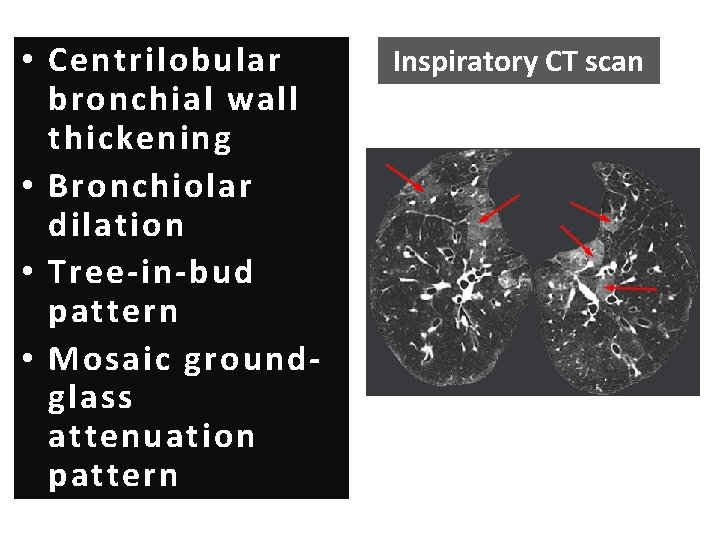
• Centrilobular bronchial wall thickening • Bronchiolar dilation • Tree-in-bud pattern • Mosaic groundglass attenuation pattern Inspiratory CT scan
70 Symptoms Constrictive Bronchiolitis Progressive onset of cough + Dyspnea + Hypoxemia at rest or with exercise Crackles may be present
Pulmonary function tests Obliterative Bronchiolitis • Irreversible airflow limitation 71

Diffuse Panbronchiolitis 72
73 Diffuse Panbronchiolitis • A rare clinicopathologic syndrome characterized by Bronchiolitis + Chronic Sinusitis • Diffuse : 2 Lungs • Pan : Inflammation involves all layers of the respiratory bronchioles Poletti V, Chilosi M, Casoni G, Colby TV. Diffuse panbronchiolitis. Sarcoidosis Vasc Diffuse Lung Dis 2004; 21: 94. Poletti V, Casoni G, Chilosi M, Zompatori M. Diffuse panbronchiolitis. Eur Respir J 2006; 28: 862.
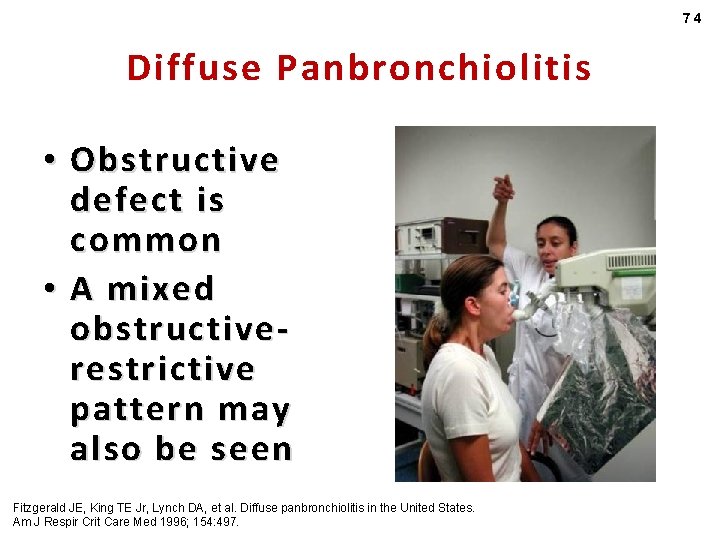
74 Diffuse Panbronchiolitis • Obstructive defect is common • A mixed obstructiverestrictive pattern may also be seen Fitzgerald JE, King TE Jr, Lynch DA, et al. Diffuse panbronchiolitis in the United States. Am J Respir Crit Care Med 1996; 154: 497.
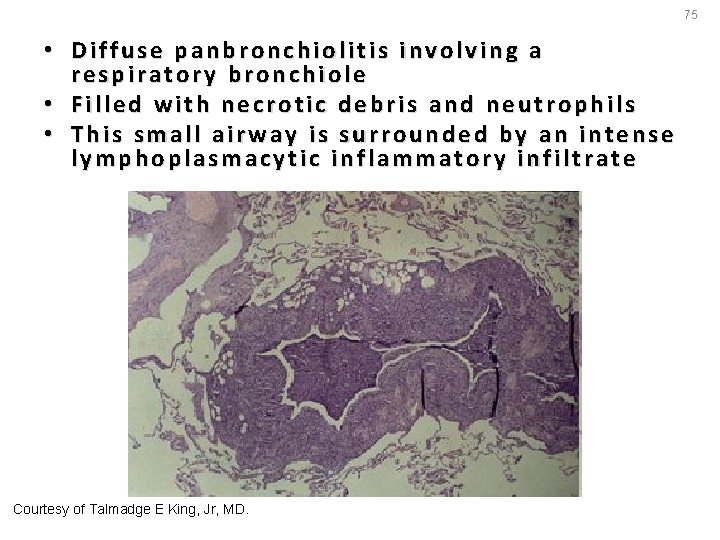
75 • Diffuse panbronchiolitis involving a respiratory bronchiole • Filled with necrotic debris and neutrophils • This small airway is surrounded by an intense lymphoplasmacytic inflammatory infiltrate Courtesy of Talmadge E King, Jr, MD.
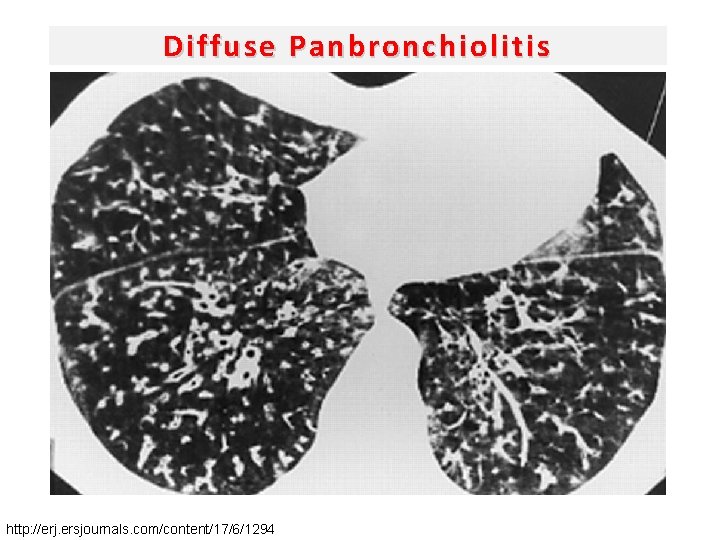
Diffuse Panbronchiolitis http: //erj. ersjournals. com/content/17/6/1294

78 Lymphangioleiomyomatosis • Lymphangioleiomyomatosis (LAM) is seen primarily in young women of childbearing age
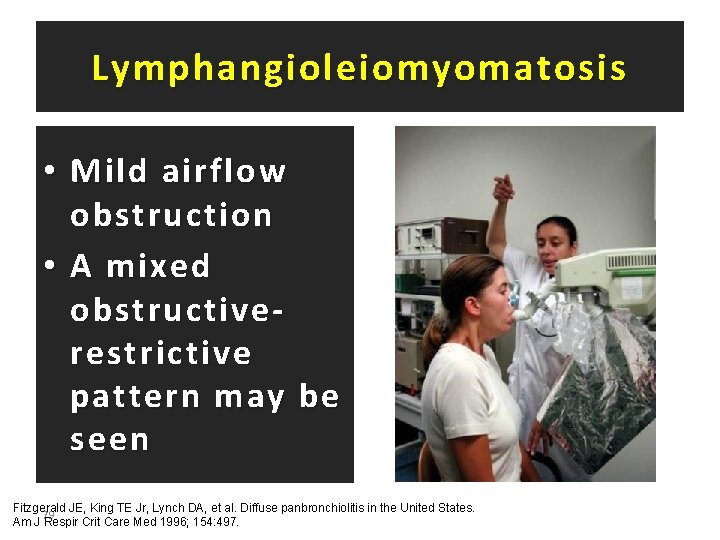
Lymphangioleiomyomatosis • Mild airflow obstruction • A mixed obstructiverestrictive pattern may be seen Fitzgerald JE, King TE Jr, Lynch DA, et al. Diffuse panbronchiolitis in the United States. 79 Am J Respir Crit Care Med 1996; 154: 497.
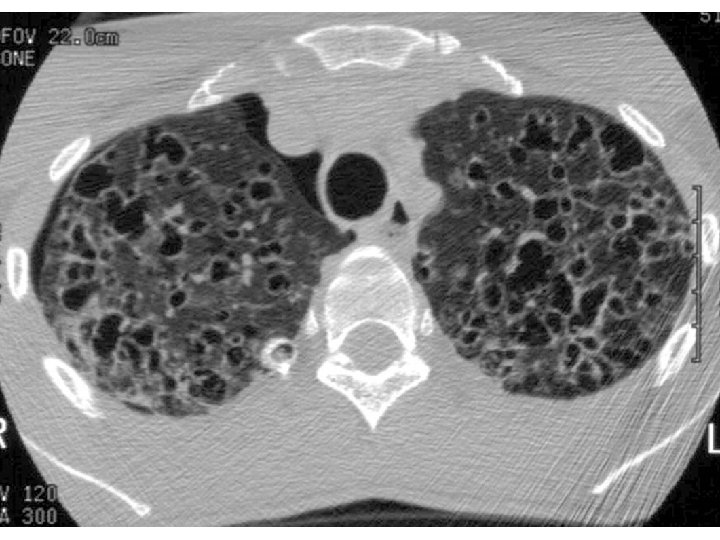
80 CT scans Lymphangioleiomyomatosis • Demonstrate ¶Small , thin-walled cysts that can at times be confused with emphysema
81

- Slides: 82