Conversation mapping tool Ethos These maps and question
- Slides: 5
Conversation mapping tool Ethos These maps and question sheet can be used to give structure to conversations with clients whose health may be deteriorating. They are tools for clients and staff / keyworkers to identify together what is most important to the client and what they hope for the future. The first map can be used as an initial step to identify main priorities in different aspects of the client’s life (physical, relationships, treatment and care etc. ). Any following maps can be used to go into more detail about the area of the client’s life they want to talk about, each time placing the area for discussion in the centre of the map. The question page offers useful prompts to guide conversation in each area. When maps are completed they can be kept as a record for the client and keyworker, and used as a reference in any multi-disciplinary meetings or appointments in the future.
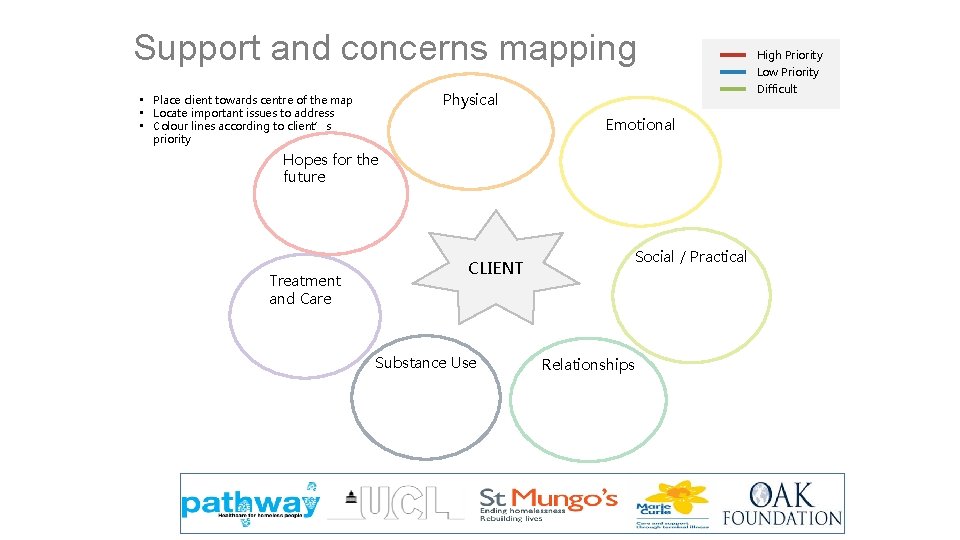
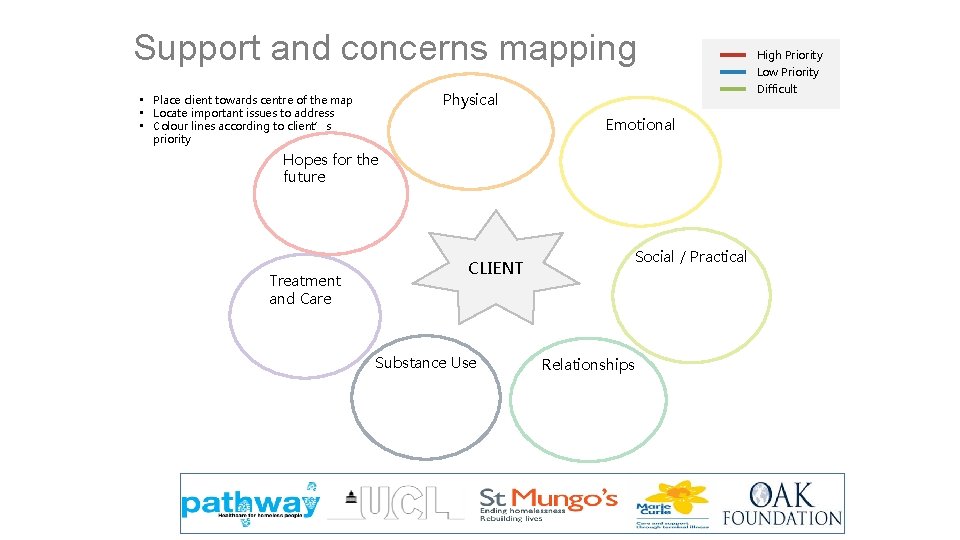
Support and concerns mapping Emotional Hopes for the future Treatment and Care Social / Practical CLIENT Substance Use Low Priority Difficult Physical • Place client towards centre of the map • Locate important issues to address • Colour lines according to client’s priority High Priority Relationships
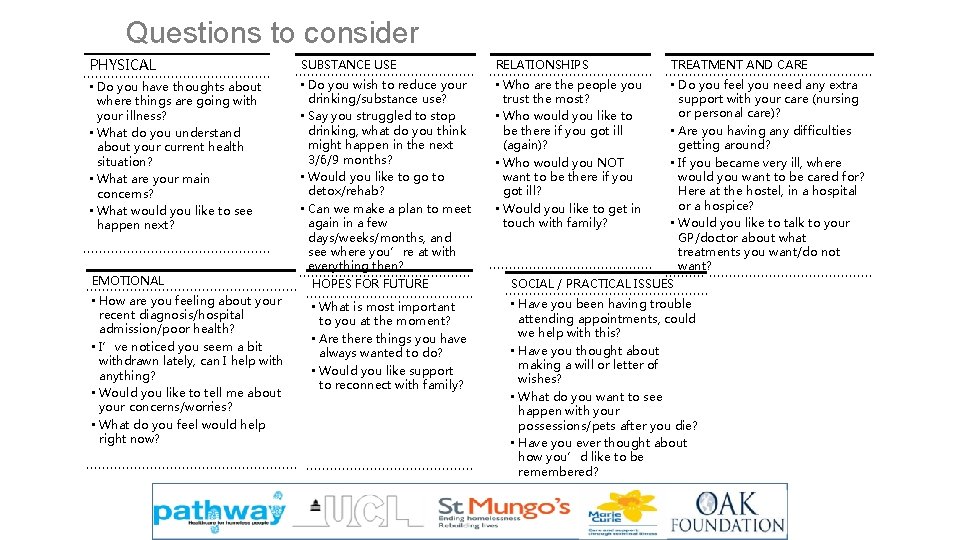
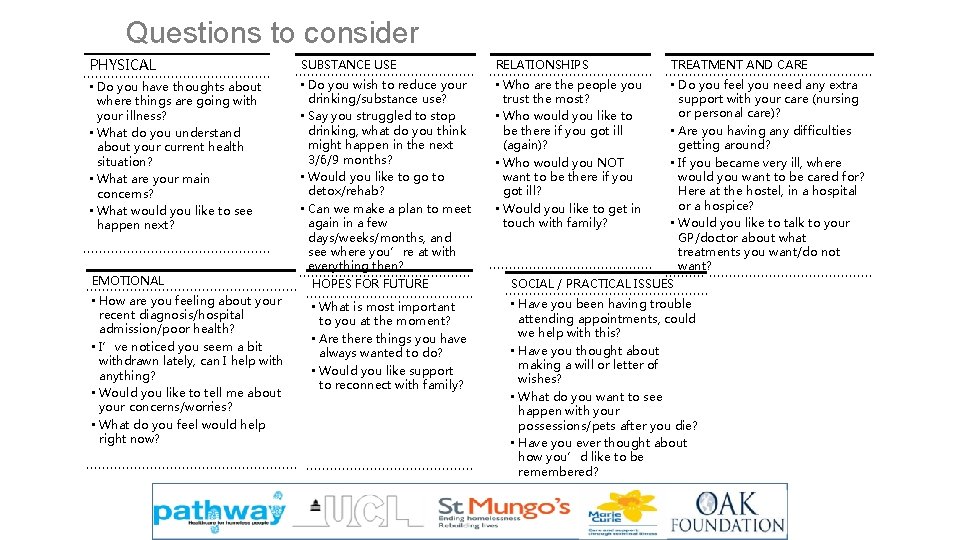
Questions to consider PHYSICAL SUBSTANCE USE RELATIONSHIPS • Do you have thoughts about where things are going with your illness? • What do you understand about your current health situation? • What are your main concerns? • What would you like to see happen next? • Do you wish to reduce your drinking/substance use? • Say you struggled to stop drinking, what do you think might happen in the next 3/6/9 months? • Would you like to go to detox/rehab? • Can we make a plan to meet again in a few days/weeks/months, and see where you’re at with everything then? HOPES FOR FUTURE • Who are the people you trust the most? • Who would you like to be there if you got ill (again)? • Who would you NOT want to be there if you got ill? • Would you like to get in touch with family? EMOTIONAL • How are you feeling about your recent diagnosis/hospital admission/poor health? • I’ve noticed you seem a bit withdrawn lately, can I help with anything? • Would you like to tell me about your concerns/worries? • What do you feel would help right now? • What is most important to you at the moment? • Are there things you have always wanted to do? • Would you like support to reconnect with family? TREATMENT AND CARE • Do you feel you need any extra support with your care (nursing or personal care)? • Are you having any difficulties getting around? • If you became very ill, where would you want to be cared for? Here at the hostel, in a hospital or a hospice? • Would you like to talk to your GP/doctor about what treatments you want/do not want? SOCIAL / PRACTICAL ISSUES • Have you been having trouble attending appointments, could we help with this? • Have you thought about making a will or letter of wishes? • What do you want to see happen with your possessions/pets after you die? • Have you ever thought about how you’d like to be remembered?
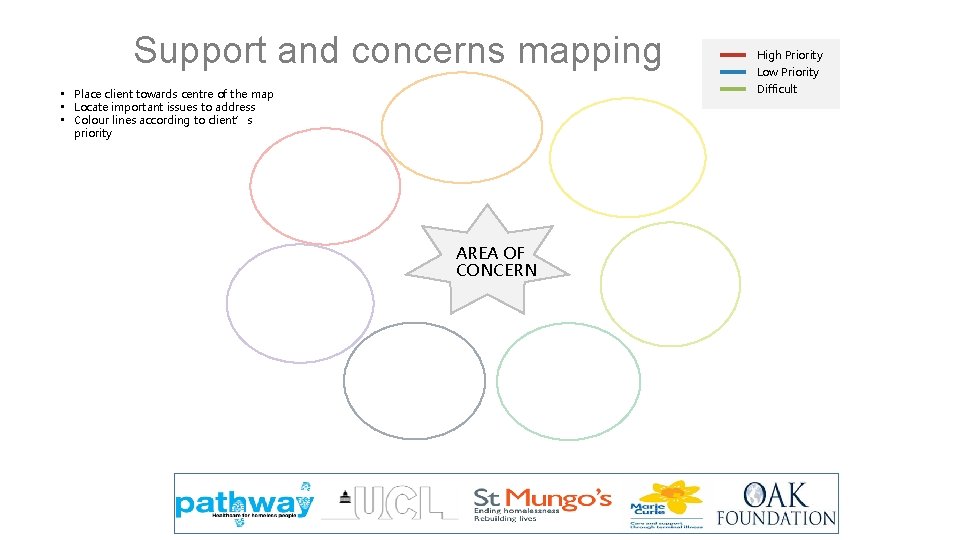
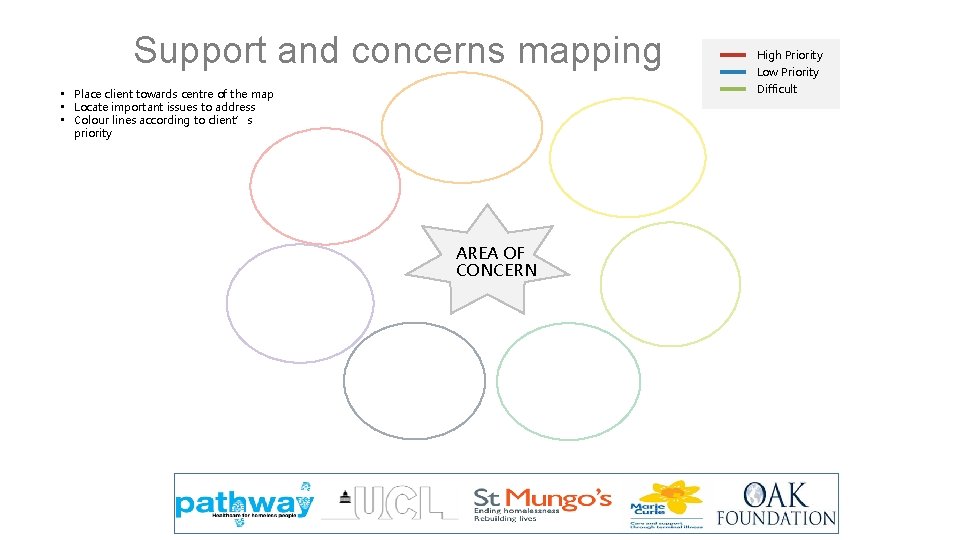
Support and concerns mapping High Priority Low Priority Difficult • Place client towards centre of the map • Locate important issues to address • Colour lines according to client’s priority AREA OF CONCERN
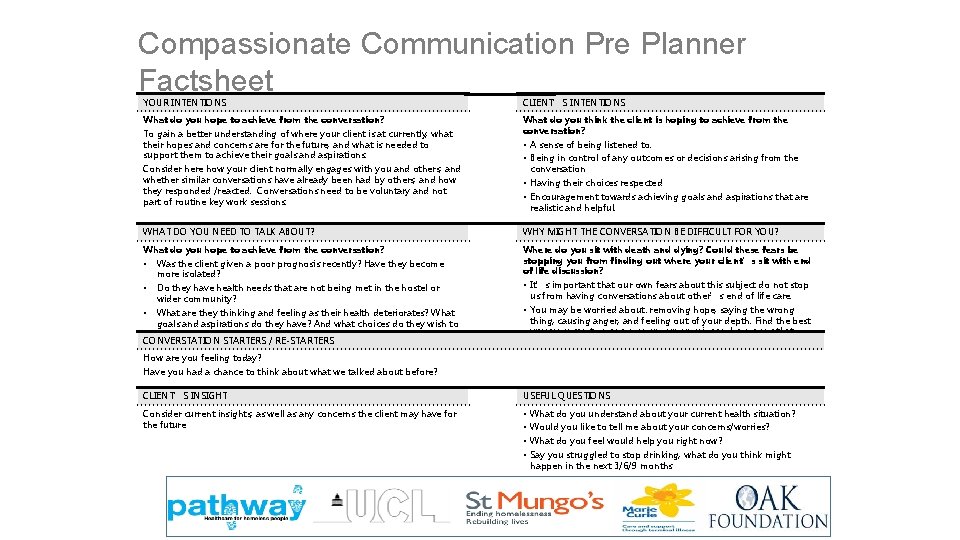
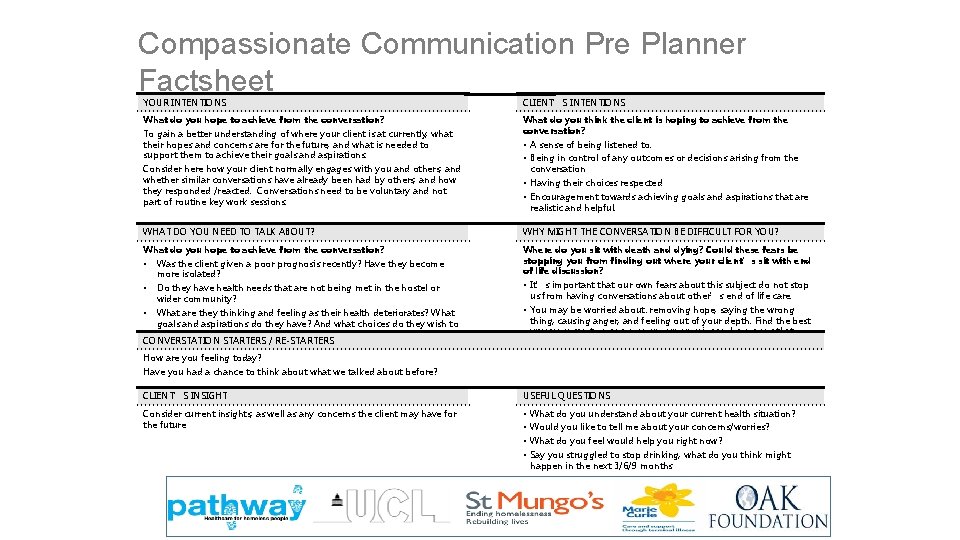
Compassionate Communication Pre Planner Factsheet YOUR INTENTIONS CLIENT’S INTENTIONS What do you hope to achieve from the conversation? What do you think the client is hoping to achieve from the conversation? To gain a better understanding of where your client is at currently, what their hopes and concerns are for the future, and what is needed to support them to achieve their goals and aspirations. Consider here how your client normally engages with you and others, and whether similar conversations have already been had by others, and how they responded /reacted. Conversations need to be voluntary and not part of routine key work sessions. • A sense of being listened to. • Being in control of any outcomes or decisions arising from the conversation • Having their choices respected • Encouragement towards achieving goals and aspirations that are realistic and helpful. WHAT DO YOU NEED TO TALK ABOUT? WHY MIGHT THE CONVERSATION BE DIFFICULT FOR YOU? What do you hope to achieve from the conversation? Where do you sit with death and dying? Could these fears be stopping you from finding out where your client’s sit with end of life discussion? • Was the client given a poor prognosis recently? Have they become more isolated? • Do they have health needs that are not being met in the hostel or wider community? What are they thinking and feeling as their health deteriorates? What goals and aspirations do they have? And what choices do they wish to make CONVERSTATION STARTERS / RE-STARTERS • • It’s important that our own fears about this subject do not stop us from having conversations about other’s end of life care. • You may be worried about: removing hope, saying the wrong thing, causing anger, and feeling out of your depth. Find the best ways you can to manage your own worries and concerns that enables you to engage more fully with theirs. How are you feeling today? Have you had a chance to think about what we talked about before? CLIENT’S INSIGHT USEFUL QUESTIONS Consider current insights, as well as any concerns the client may have for the future • • What do you understand about your current health situation? Would you like to tell me about your concerns/worries? What do you feel would help you right now? Say you struggled to stop drinking, what do you think might happen in the next 3/6/9 months