Controlled hypotension Deliberate hypotension Induced hypotension Hypotensive anesthesia
Controlled hypotension Deliberate hypotension Induced hypotension Hypotensive anesthesia
Definiton Ø Reduction in systolic blood pressure to 80 -90 mm. Hg Ø Decrease in MAP to 50 -65 mm. Hg in normotensive patients Ø Reduction in MAP by one-third of its baseline values
Purpose Ø To reduce intraoperative blood loss Ø To facilitate surgical exposure - faster surgery? Ø To decrease blood transfusion - reduce the chances of transmission of infectious Ds & transfusion reaction
Indication Ø Neurosurgery Ø Orthopedics: THR, spine fusion Ø Ear, nose, throat/oral surgery Ø Gynecologic/urologic: radical pelvic surgery, prostatectomy Ø 기타 : Religious blood refusal, rare blood type, difficult cross matching
Relative contraindication • Cerebrovascular Ds: stroke, Hx of TIA • Spinal cord compression • Cardiovascular Ds: angina, Hx of MI, untreated HT, peripheral vascular Ds
• • • Aortic stenosis Renal or hepatic dysfunction Increased ICP Pregnancy Severe pulmonary Ds Hypovolemia & severe anemia
Reduction in MAP (not CO) primary determinant of intraoperative blood loss Hypotension in operating room 1. Fluid volume status 2. Anesthetic depth
Hypotension from blood loss - vasoconstriction - low cardiac output - low blood flow - great risk for ischemic complication
Hypotension due to vasodilation - high blood flow - preservation of peripheral oxygen delivery
The goal of minimizing surgical hemorrhage by keeping the blood pressure low Best achieved by the use of agents that produce hypotension through vasodilation in the presence of adequate intravascular volume
• The correlation between decrease in arterial blood pressure and blood loss is not linear • Patient position, attention to ventilation influence venous return : important in minimizing blood loss
Effect of hypotension on organ function • Arterial blood pressure reduction by decreasing CO or SVR or both • CO should remain sufficiently high - to provide adequate oxygen & energy substrate - to remove metabolic waste products
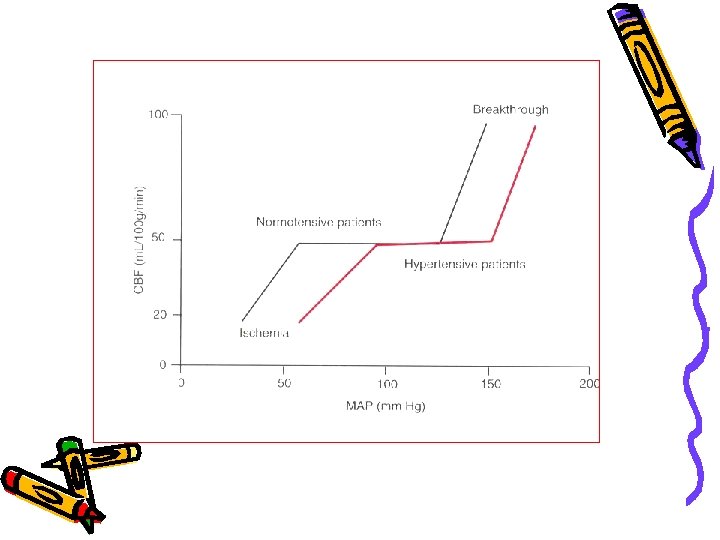
1. Central nervous system • Does not produce permanent changes in cerebral hemodynamics • Autoregulation of CBF is still in force • Safe technique for patients with medically controlled hypertension

• Cerebral perfusion pressure = MAP-ICP In increased ICP pt never undergo CH before the dura is opened unless measurement of ICP is available
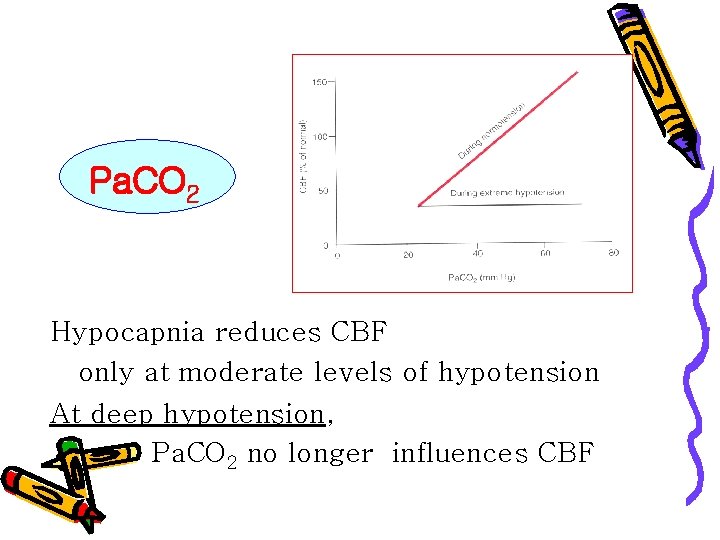
Pa. CO 2 Hypocapnia reduces CBF only at moderate levels of hypotension At deep hypotension, Pa. CO 2 no longer influences CBF
2. Heart • Maintenance of oxygen supply sufficient for the metabolic need of the myocardium is of primary importance • cardiac depression, toxic side effect • reflex tachycardia – increase myocardial metabolites - reduce myocardial perfusion • drugs that reduce metabolic need: protect heart from ischemia
3. Kidney • Well-functioning autoregulatory mechanism • Renal arterioles: - low resting vascular tone - limited ability to dilate further in response to hypotension
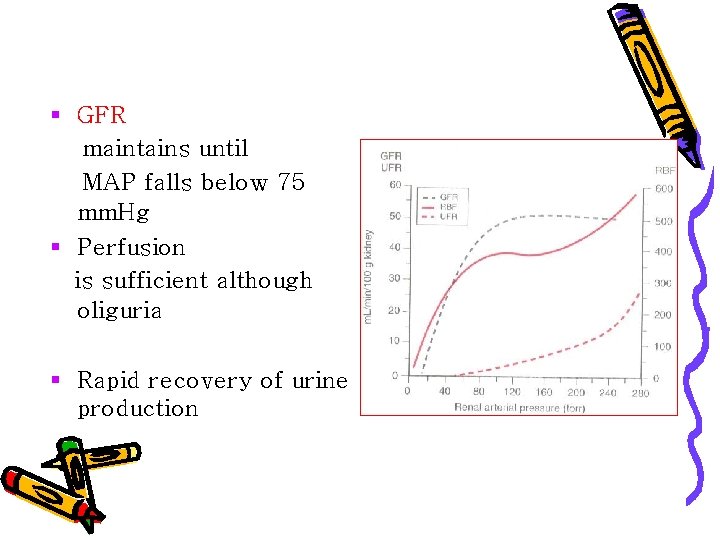
§ GFR maintains until MAP falls below 75 mm. Hg § Perfusion is sufficient although oliguria § Rapid recovery of urine production
4. Eye • Intraocular pressure decreases • Cx: blurring of vision blindness • anterior ischemic optic neuropathy • Posterior ischemic optic neuropathy
Monitoring during Controlled hypotension
1. Arterial blood pressure 2. EKG – myocardial perfusion 3. Capnography – correlation between ETCO 2 and Pa. CO 2 is unreliable but still useful - help avoid hyperventilation during moderate hypotension
4. 5. 6. 7. 8. 9. Pulse oximetry Temperature Urinary out put Central venous pressure Serum electolytes, blood gases, Hct Evoked potential, EEG, * optimized for the type and length of surgery
Method • Physiologic technique • Pharmacologic technique
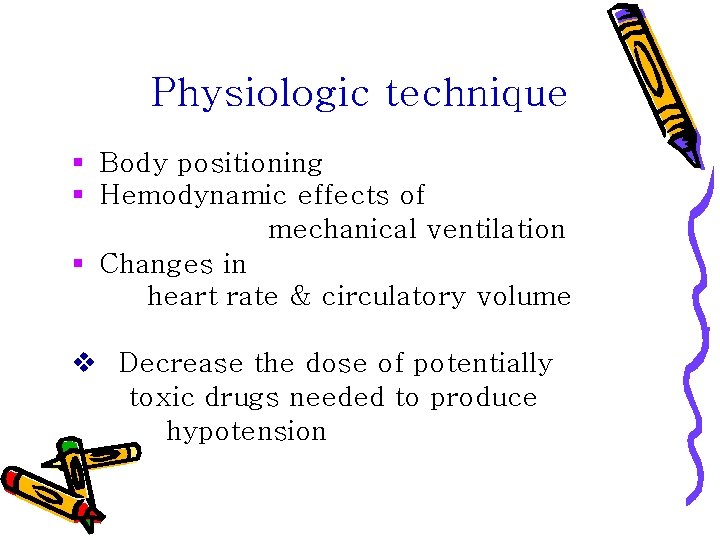
Physiologic technique § Body positioning § Hemodynamic effects of mechanical ventilation § Changes in heart rate & circulatory volume v Decrease the dose of potentially toxic drugs needed to produce hypotension
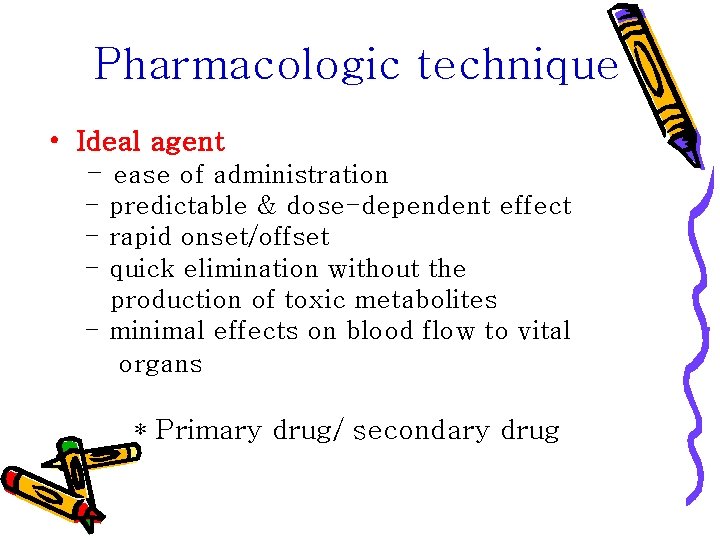
Pharmacologic technique • Ideal agent - ease of administration - predictable & dose-dependent effect - rapid onset/offset - quick elimination without the production of toxic metabolites - minimal effects on blood flow to vital organs * Primary drug/ secondary drug
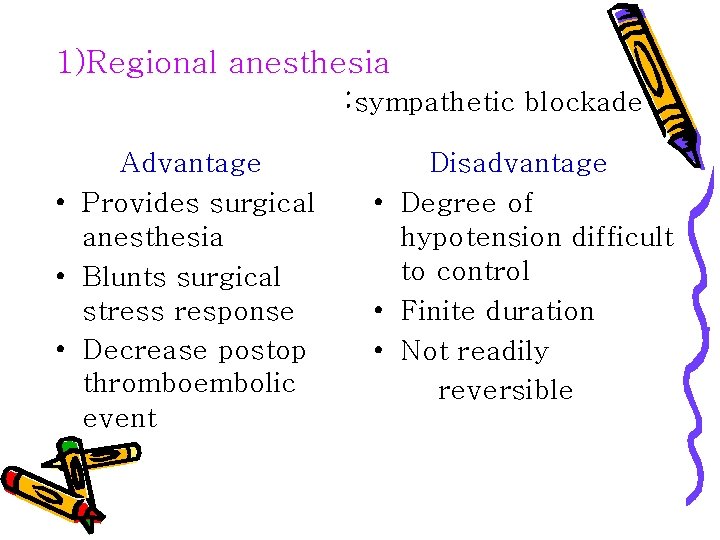
1)Regional anesthesia : sympathetic blockade Advantage • Provides surgical anesthesia • Blunts surgical stress response • Decrease postop thromboembolic event Disadvantage • Degree of hypotension difficult to control • Finite duration • Not readily reversible
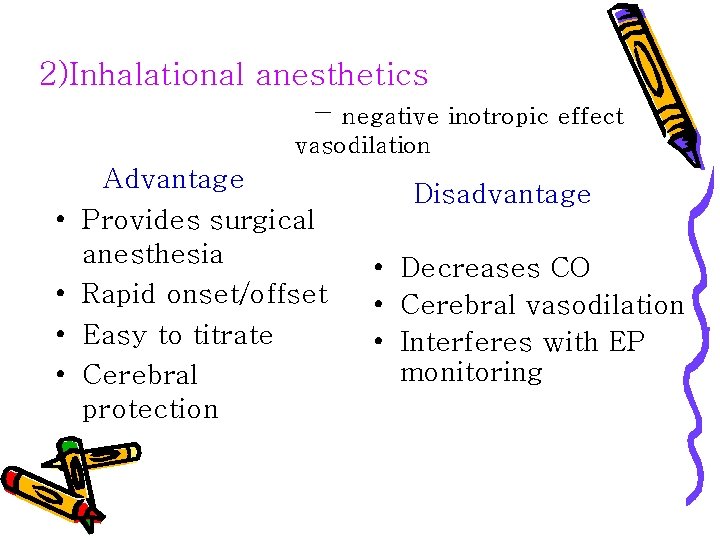
2)Inhalational anesthetics – negative inotropic effect vasodilation • • Advantage Provides surgical anesthesia Rapid onset/offset Easy to titrate Cerebral protection Disadvantage • Decreases CO • Cerebral vasodilation • Interferes with EP monitoring
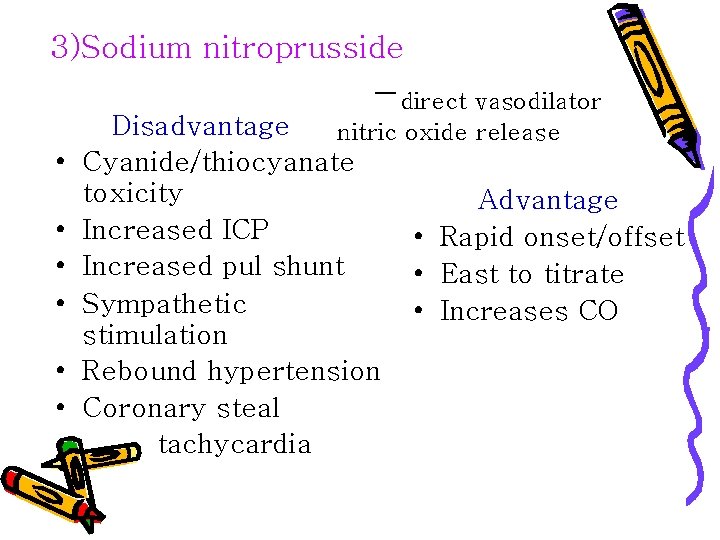
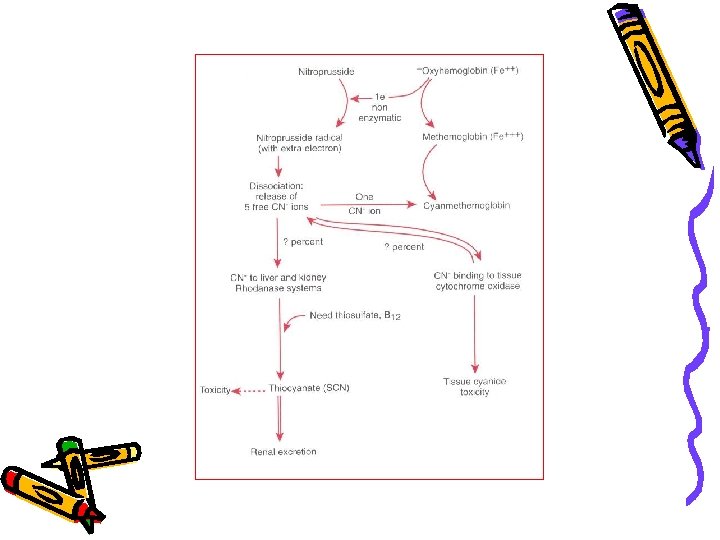
3)Sodium nitroprusside -direct vasodilator • • Disadvantage nitric oxide release Cyanide/thiocyanate toxicity Advantage Increased ICP • Rapid onset/offset Increased pul shunt • East to titrate Sympathetic • Increases CO stimulation Rebound hypertension Coronary steal tachycardia
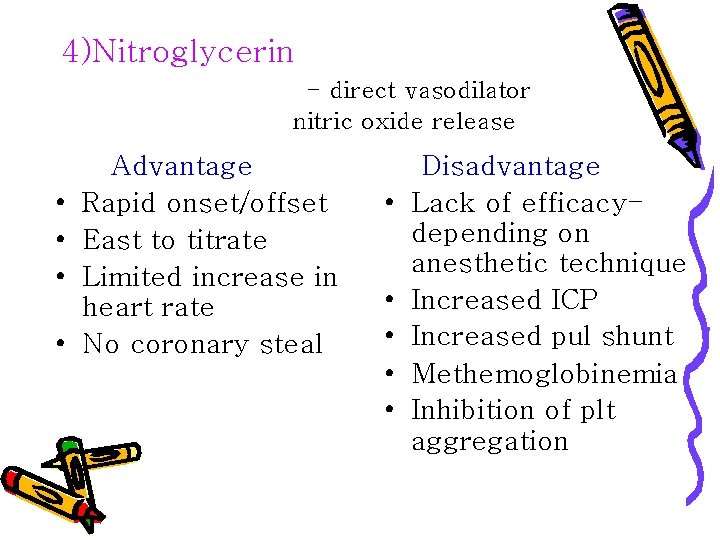
4)Nitroglycerin - direct vasodilator nitric oxide release • • Advantage Rapid onset/offset East to titrate Limited increase in heart rate No coronary steal • • • Disadvantage Lack of efficacydepending on anesthetic technique Increased ICP Increased pul shunt Methemoglobinemia Inhibition of plt aggregation
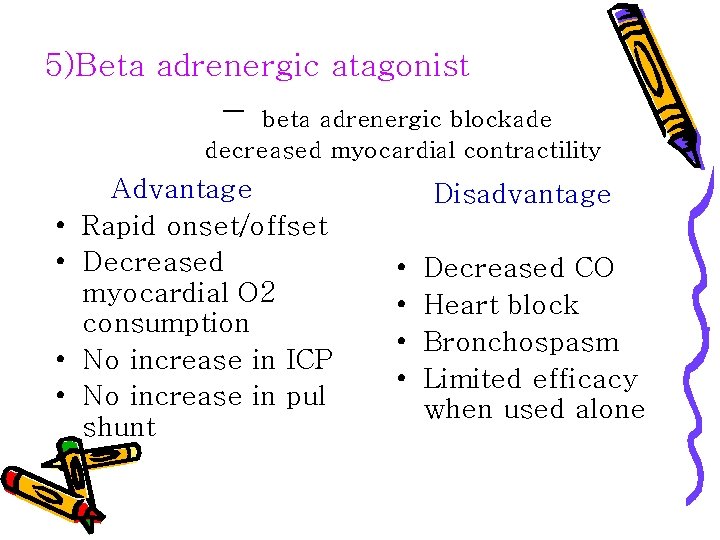
5)Beta adrenergic atagonist - beta adrenergic blockade decreased myocardial contractility • • Advantage Rapid onset/offset Decreased myocardial O 2 consumption No increase in ICP No increase in pul shunt Disadvantage • • Decreased CO Heart block Bronchospasm Limited efficacy when used alone
6)Calcium channel blocker - vasodilation • • • Advantage Rapid onset Limited increase in HR Increase CO No effect on airway reactivity Increased GFR/urine output Disadvantage • Prolonged duration of action • Increased ICP • Increased intrapulmonary shunt
7)Remifentanil § Rapid onset/offset § decrease of CO without peripheral vasodilation § No adverse effects, § No need for additional use of a potent hypotensive or adjunt agents
• Remifentanil and controlled hypotension: comparison with nitroprusside or esmolol during tympanoplasty CAN J ANESTH 2001; 48: 20 -27 • Using remifentanil and sufentanil in functional endoscopic sinus surgery to improve surgical conditions ORL 2005; 67: 83 -86 • Intravenous anesthesia provides optimal surgical conditions during microscopic and endoscopic sinus surgery Laryngoscope 2003; 113: 1369 -1373
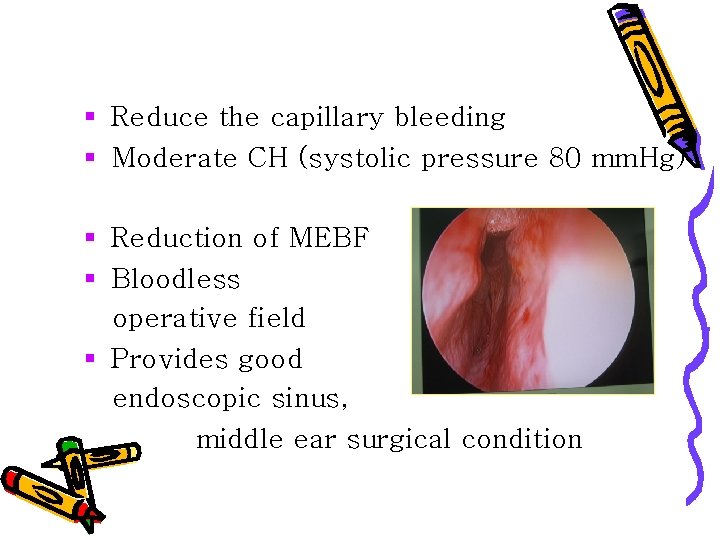
§ Reduce the capillary bleeding § Moderate CH (systolic pressure 80 mm. Hg) § Reduction of MEBF § Bloodless operative field § Provides good endoscopic sinus, middle ear surgical condition
Complication • • • Cardiac arrest Cerebral infarction Myocardial ischemia or infarction Blindness 기타
summary • Many drugs & techniques are successful • Not without risk The intelligent use of CH : has distinct advantages for certain procedures : promote surgical success
- Slides: 39