CONTRAST RADIOGRAPHIC AGENTS AND TECNIQUES Contrast Media Contrast
![Retrograde urethro-cystography. a [a] Normal retrograde urethro-cystogram in a dog. The penile urethra [PU], Retrograde urethro-cystography. a [a] Normal retrograde urethro-cystogram in a dog. The penile urethra [PU],](https://slidetodoc.com/presentation_image_h2/160562d00301e4326c1e67f478a12d2f/image-22.jpg)
- Slides: 27
CONTRAST RADIOGRAPHIC AGENTS AND TECNIQUES
Contrast Media Contrast media are agents used to improve visualization of organs within tissue of similar radiographic contrast. Contast techniques provide detail of organ size, shape, position and internal detail. In some instances assessment of organ function may be permitted
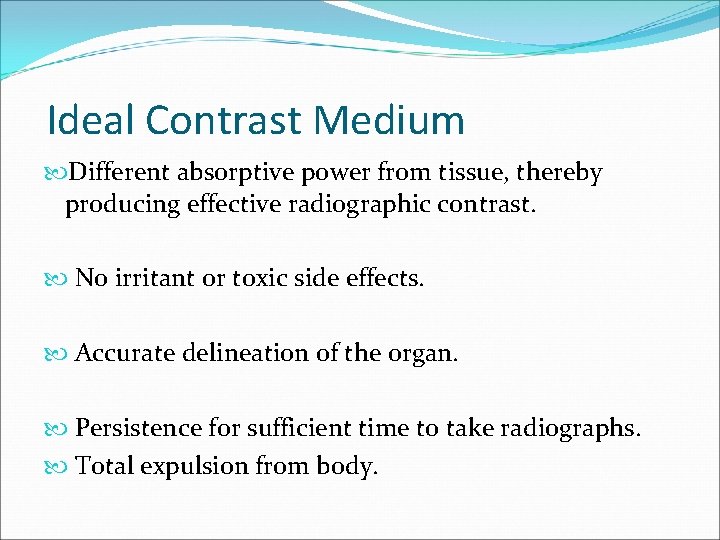
Ideal Contrast Medium Different absorptive power from tissue, thereby producing effective radiographic contrast. No irritant or toxic side effects. Accurate delineation of the organ. Persistence for sufficient time to take radiographs. Total expulsion from body.
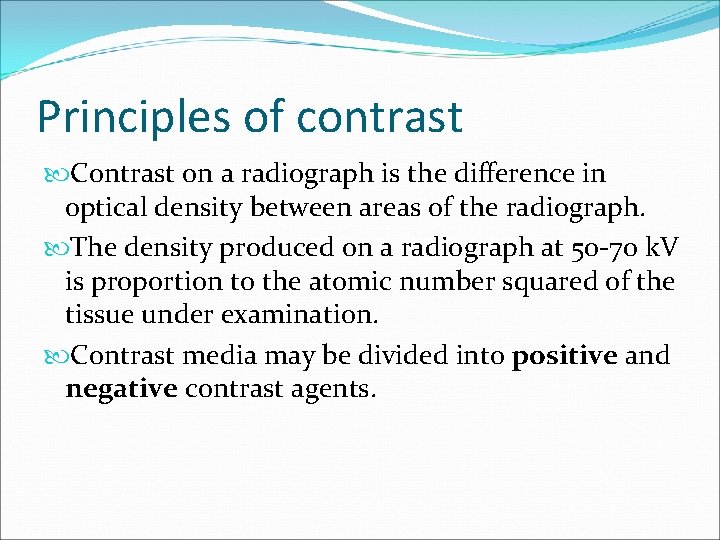
Principles of contrast Contrast on a radiograph is the difference in optical density between areas of the radiograph. The density produced on a radiograph at 50 -70 k. V is proportion to the atomic number squared of the tissue under examination. Contrast media may be divided into positive and negative contrast agents.
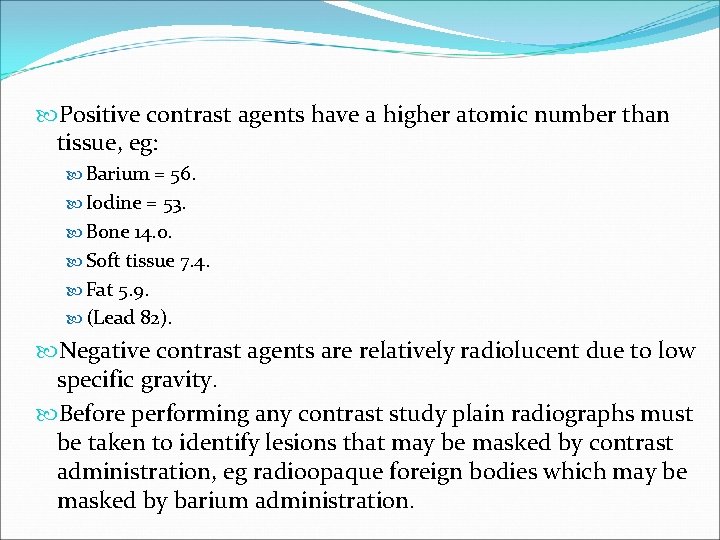
Positive contrast agents have a higher atomic number than tissue, eg: Barium = 56. Iodine = 53. Bone 14. 0. Soft tissue 7. 4. Fat 5. 9. (Lead 82). Negative contrast agents are relatively radiolucent due to low specific gravity. Before performing any contrast study plain radiographs must be taken to identify lesions that may be masked by contrast administration, eg radioopaque foreign bodies which may be masked by barium administration.
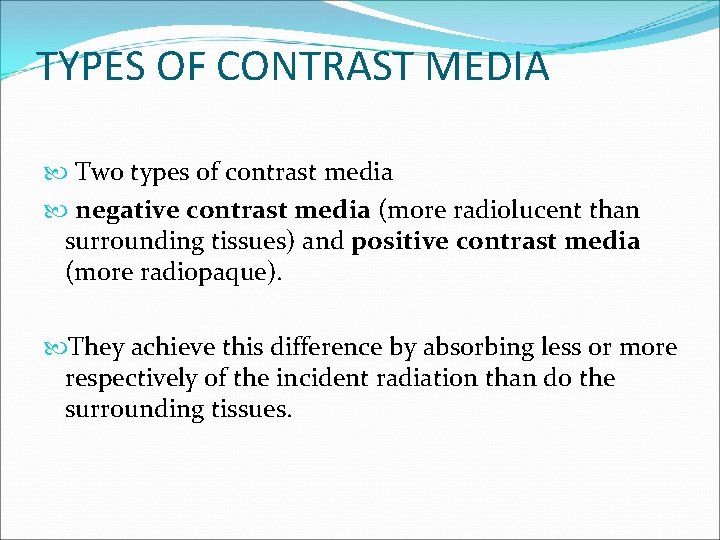
TYPES OF CONTRAST MEDIA Two types of contrast media negative contrast media (more radiolucent than surrounding tissues) and positive contrast media (more radiopaque). They achieve this difference by absorbing less or more respectively of the incident radiation than do the surrounding tissues.
Negative contrast agents Oxygen, air, carbon dioxide and nitrous oxide. Negative contrast agents can be used for: Cystography. Gastrography. Peritonography. Pericardiography. Disadvantages: Do not give as much mucosal detail as positive or double contrast studies. Fatal air embolus has been reported following pneumocystography and urethrography. Carbon dioxide is probably safer due to higher solubility in serum. Oxygen is a fire risk. Advantages: Readily available. Cheap.
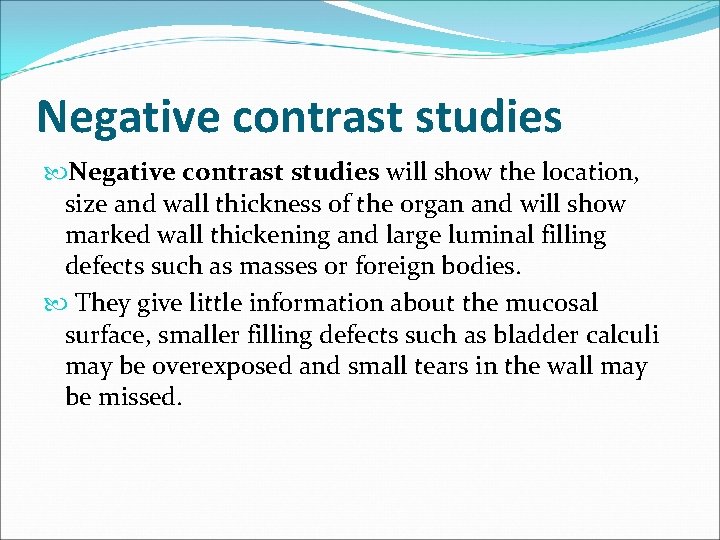
Negative contrast studies will show the location, size and wall thickness of the organ and will show marked wall thickening and large luminal filling defects such as masses or foreign bodies. They give little information about the mucosal surface, smaller filling defects such as bladder calculi may be overexposed and small tears in the wall may be missed.
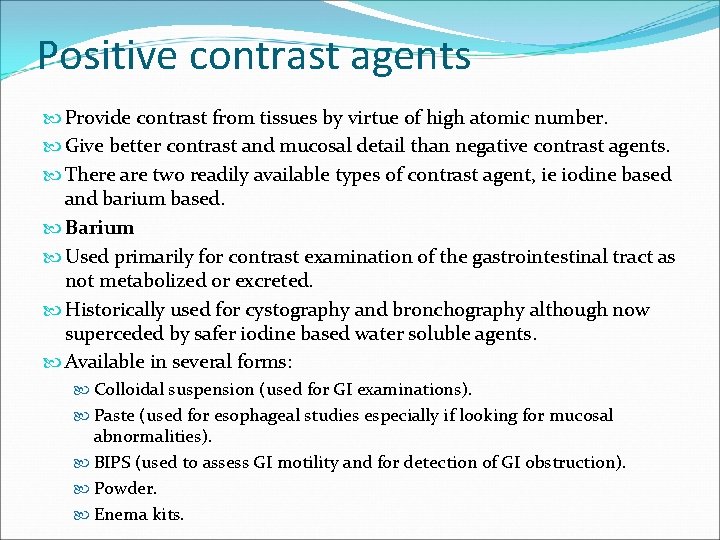
Positive contrast agents Provide contrast from tissues by virtue of high atomic number. Give better contrast and mucosal detail than negative contrast agents. There are two readily available types of contrast agent, ie iodine based and barium based. Barium Used primarily for contrast examination of the gastrointestinal tract as not metabolized or excreted. Historically used for cystography and bronchography although now superceded by safer iodine based water soluble agents. Available in several forms: Colloidal suspension (used for GI examinations). Paste (used for esophageal studies especially if looking for mucosal abnormalities). BIPS (used to assess GI motility and for detection of GI obstruction). Powder. Enema kits.
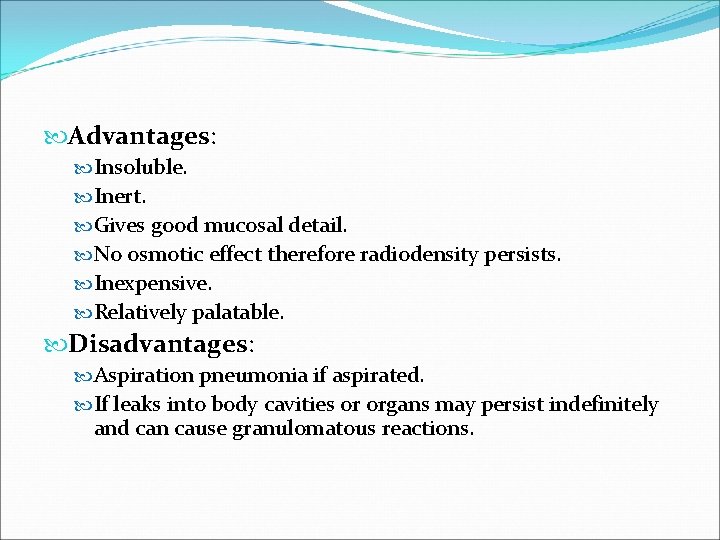
Advantages: Insoluble. Inert. Gives good mucosal detail. No osmotic effect therefore radiodensity persists. Inexpensive. Relatively palatable. Disadvantages: Aspiration pneumonia if aspirated. If leaks into body cavities or organs may persist indefinitely and can cause granulomatous reactions.
Positive contrast studies give little more information than negative contrast studies but are the best way of detecting a small defect in the wall of the organ, as minor contrast leakage is easily seen.
Iodine based preparations Divided into four types: Ionic water soluble. Non-ionic water soluble. Oily agents. Agents excreted in the bile.
Ionic water soluble Uses Imaging of: Cardiovascular system. Urinary system. Joints. Salivary glands. Tear ducts. Fistulas/sinuses. Gastrointestinal tract. Low osmolar ionic water soluble agents safer if poor cardiac or renal function. Dissociate in solution and unsuitable for myelography as ionic charge is neurotoxic. Must use non-ionic water soluble contrast agents for myelography.
High osmotic pressure 5 -7 times body fluids which can cause adverse reactions: Circulatory effects. Palpitations and ECG changes. Nausea/vomiting. Urticaria. Anaphylaxis. Extravascular irritation. Contraindicated if cardiovascular or renal insufficiency. Many of these potential side effects can be avoided by performing studies under general anesthesia. Advantages: Water soluble and intravenous administration possible. Excreted by kidney therefore can be used for urographic studies
Non-ionic water soluble Latest agents are iso-osmolar with plasma. Advantages - a number of advantages over Ionic water soluble compounds: No ionic charge therefore can be used for myelography . Lower osmolarity therefore safer for cardiographic, renal studies and in neonates. Fewer side effects. Disadvantages: More expensive
Oily agents Iodinized oils which do not mix with water. Used for imaging: Lymphatic system. Sinus tracts. Salivary glands. Viscous agents are no longer available but were used in bronchography
Agents excreted in the bile Chylocystopaques can be administered intravenously. Contrast agents with high protein binding capacity, eg meglumine ioglycomate are excreted via the biliary system. Used to image: Gall bladder. Bile ducts. Oral preparations are not suitable for animal use as have variable aborption and excretion patterns.
Double contrast studies use a small amount of positive contrast medium to coat the mucosal surface of a hollow organ such as the bladder, followed by distension with air. This gives much better mucosal detail than a positive or negative study alone, and will also more reliably show small filling defects in the puddle of residual positive contrast medium.
PREPARATION FOR ELECTIVE CONTRAST STUDIES Fast the animal and administer a cleansing enema, to empty the gut and/or prepare for general anaesthesia. Sedate or anaesthetise the patient. Obtain plain (survey) radiographs even if these were performed the previous day-check exposure factors and adequacy of preparation, and use as a baseline image for interpretation of contrast radiographs.
Administer the contrast medium noting the time (with the patient positioned for the first radiograph if it must be taken quickly). Obtain lateral, ventrodorsal/dorsoventral and oblique radiographs at regular time intervals depending on the study, until a confident diagnosis is reached. Mark the time of exposure on each radiograph. When viewing the radiographs, it is often helpful to examine films taken from the same angle together, as consistent abnormalities will be more readily apparent.
Contrast radiographic technique Cystography, , Myelography and Epidurography Contrast cystography Cystography is a radiographic study performed to aid in evaluation of the urinary bladder for extramural, or intraluminal lesions.
![Retrograde urethrocystography a a Normal retrograde urethrocystogram in a dog The penile urethra PU Retrograde urethro-cystography. a [a] Normal retrograde urethro-cystogram in a dog. The penile urethra [PU],](https://slidetodoc.com/presentation_image_h2/160562d00301e4326c1e67f478a12d2f/image-22.jpg)
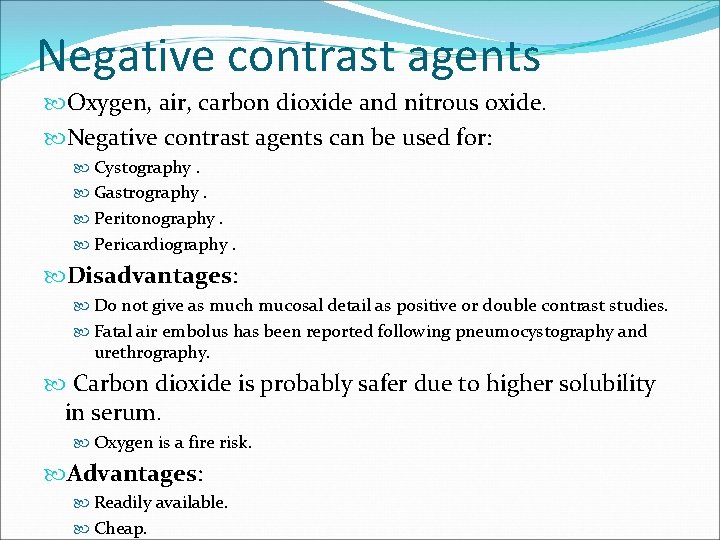
Retrograde urethro-cystography. a [a] Normal retrograde urethro-cystogram in a dog. The penile urethra [PU], membranous urethra [MU], prostatic urethra [Pr U], prostate [Pr] and urinary bladder [UB] are labeled. The catheter tip [arrow] is within the penile urethra. In [b] there is reflux of contrast into the prostatic ducts. [a] [b]
Myelogram xray A myelogram is a specialized form of an xray that helps to determine if there is damage to the spinal cord. To perform a myelogram the animal must be placed under a general anesthetic. Then, a dye is injected into the spinal column. This dye turns up well on radiographs. Then, radiographs are taken of the spine. The dye causes the spinal cord to be outlined. If there is a disc protrusion or bulging we can usually see this on the xray. Often a myelogram cannot be done at a regular practice.
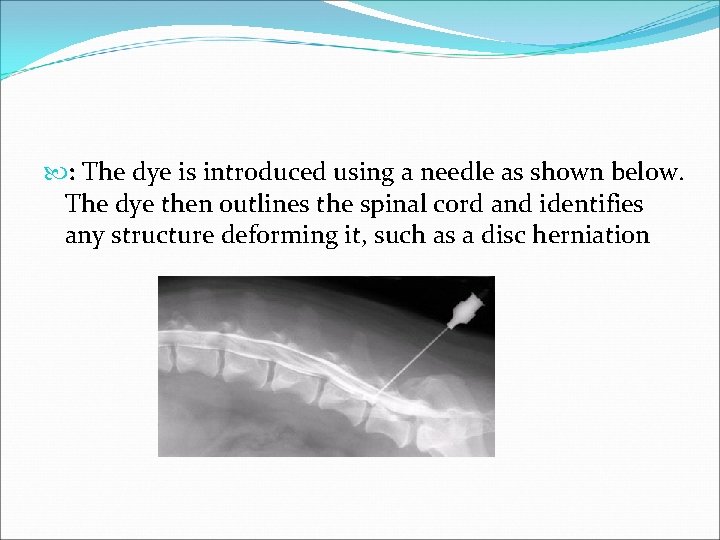
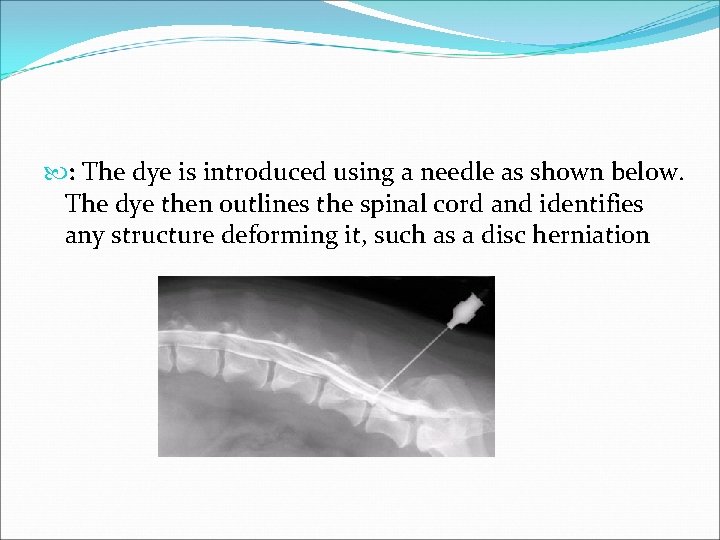
: The dye is introduced using a needle as shown below. The dye then outlines the spinal cord and identifies any structure deforming it, such as a disc herniation
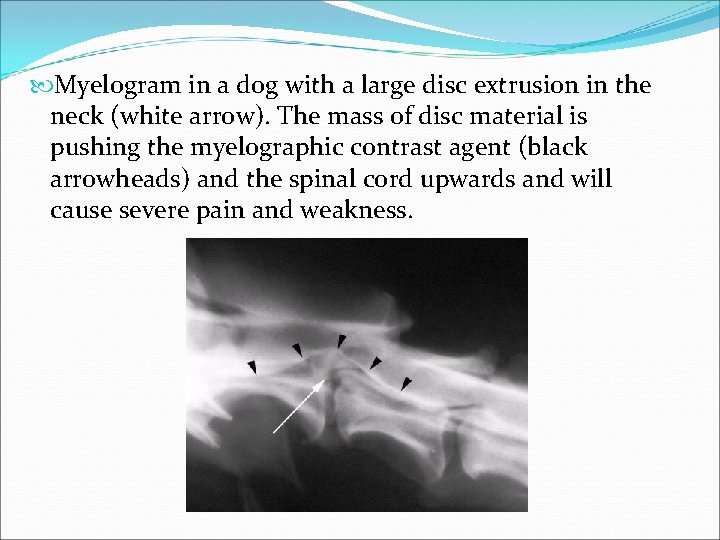
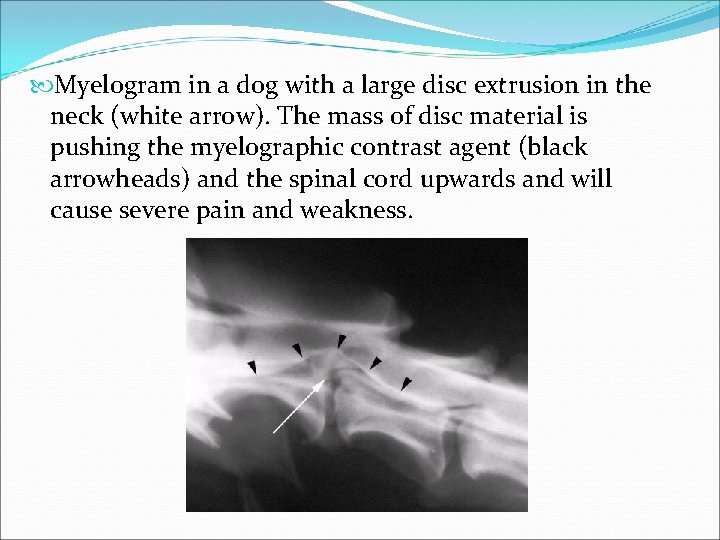
Myelogram in a dog with a large disc extrusion in the neck (white arrow). The mass of disc material is pushing the myelographic contrast agent (black arrowheads) and the spinal cord upwards and will cause severe pain and weakness.
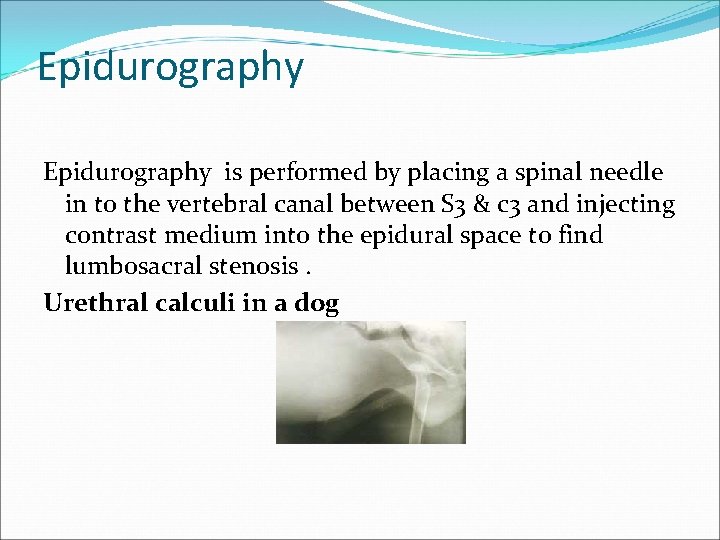
Epidurography is performed by placing a spinal needle in to the vertebral canal between S 3 & c 3 and injecting contrast medium into the epidural space to find lumbosacral stenosis. Urethral calculi in a dog
Reference Text book of veterinary diagnostic radiology(4 th edi) by Donald E. Thrall, DVM, Ph. D 2. Dennis R and Herrtage M E (1989) Low osmolar contrast media - a review. Vet Radiol 30, 2 -12. 3. Barium meal techniques in dogs and cats; Dennis, R. (1992) In Practice 14 237 -248. 4. Contrast media and their use in small animal radiology; Herrtage, M. E. and Dennis, R. (1987) Journal of Small Animal Practice 28 1105 -1114. 1.