CONTRAST MEDIA IN RADIOLOGY SUPPAT ITTIMAKIN MD CONTRAST







- Slides: 60
CONTRAST MEDIA IN RADIOLOGY SUPPAT ITTIMAKIN, MD.
CONTRAST MEDIA • Substance used to enhance the contrast of the structures or fluid within the body in medical imaging • Types of contrast agent - Iodinated contrast agent - MR contrast agent: Gadolinium-based contrast agent - Negative contrast agent air
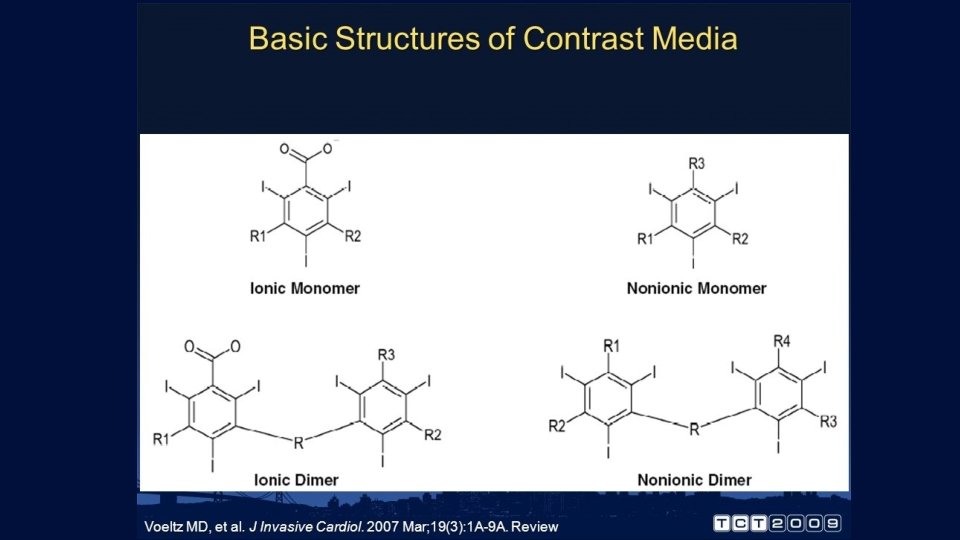
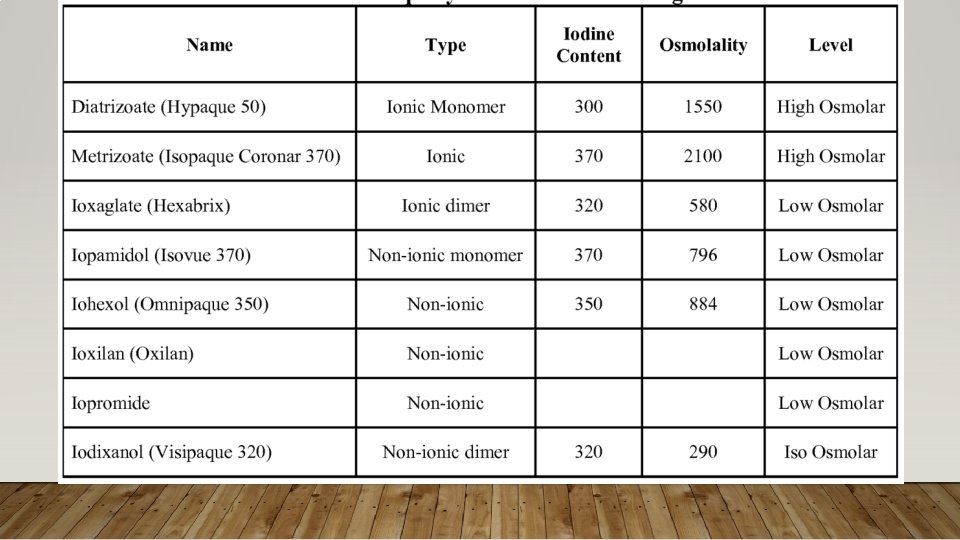
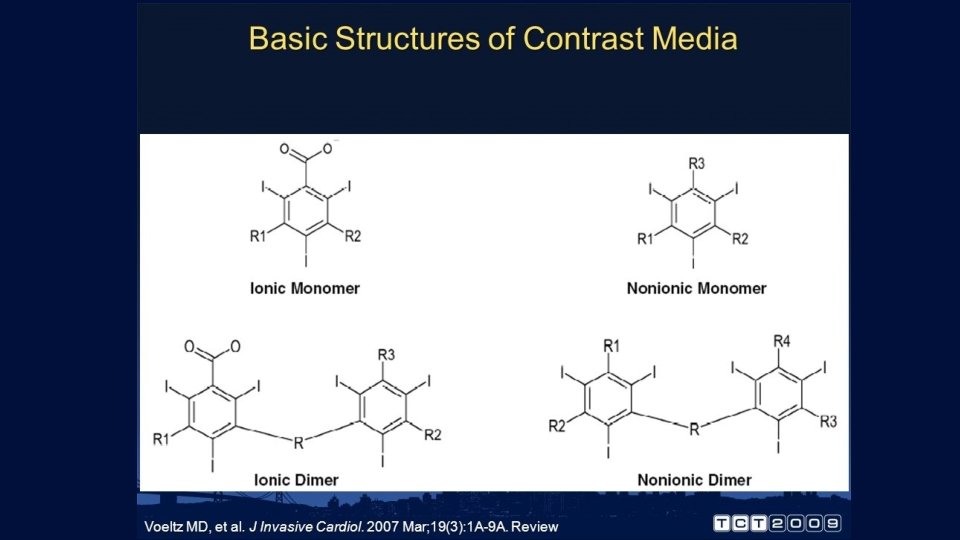
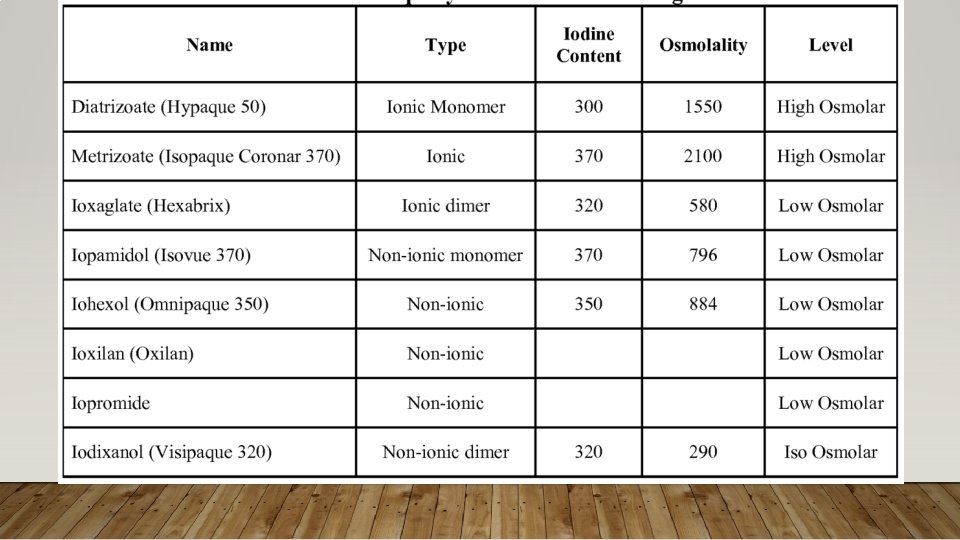
IODINATED CONTRAST MEDIA • Radiopaque contrast agents are often used in radiography and fluoroscopy to help delineate borders between tissues with similar radiodensity • Types of iodinated contrast media - Ionic - Non-ionic
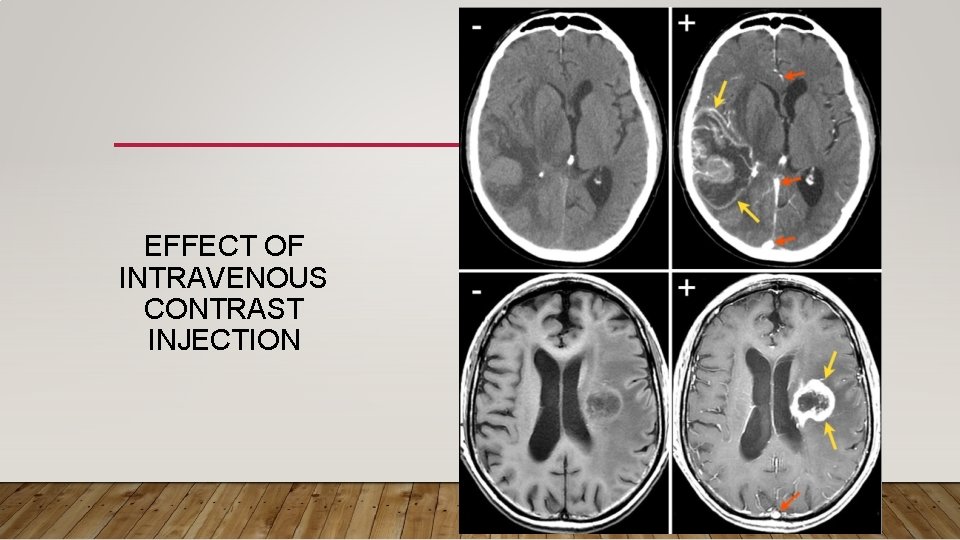
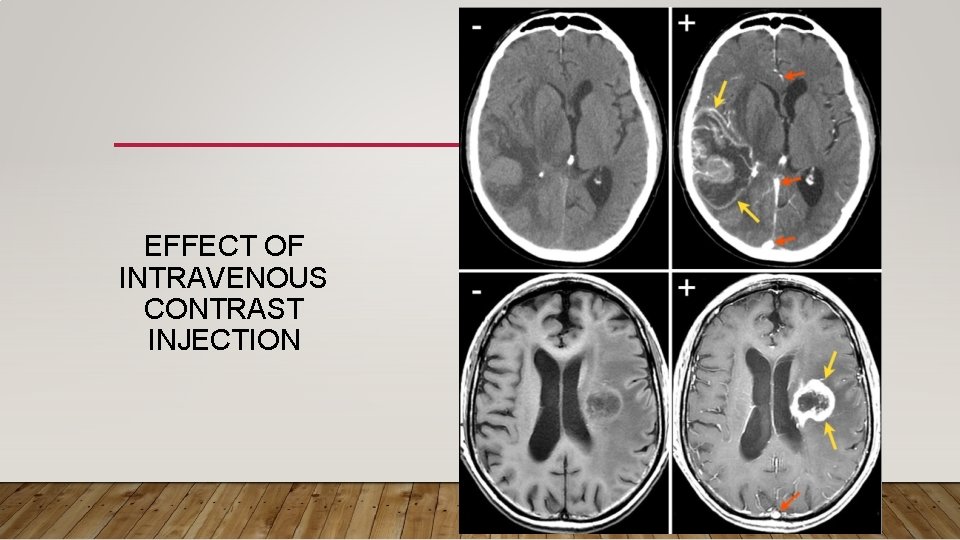
EFFECT OF INTRAVENOUS CONTRAST INJECTION

CONTRAST MEDIA Ionic contrast agents: • Hyperosmolarity to blood • Should not be used for myelography or in injections that may enter the spinal canal (because neurotoxicity is a risk) or the bronchial tree (because pulmonary edema is a risk) • Incidence of irreversible renal failure in some medical condition such as paraproteinemia in multiple myeloma
CONTRAST MEDIA Nonionic contrast agents: • Low-osmolar (but still hyperosmolar relative to blood ; 300 mg I/ml) or isoosmolar (with the same osmolarity as blood) • Now routinely used Fewer adverse effects
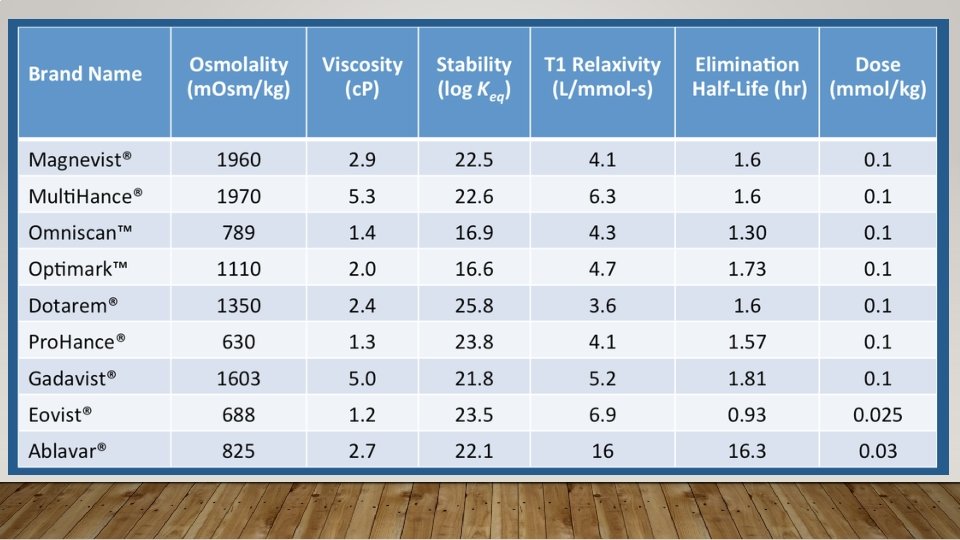
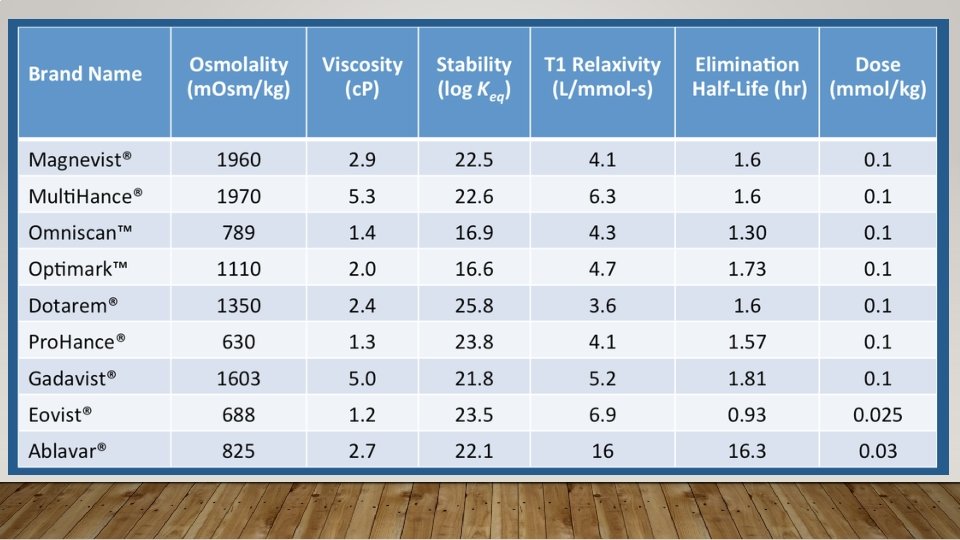
MR CONTRAST AGENT • Extracellular contrast agent • Organ specific agent • Blood pool agent
GADOLINUM-BASED MR CONTRAST • Improve visilbility of the internal body structures in MRI • Shortening of the T 1 relaxing time of the atom • Do not pass blood brain barrier
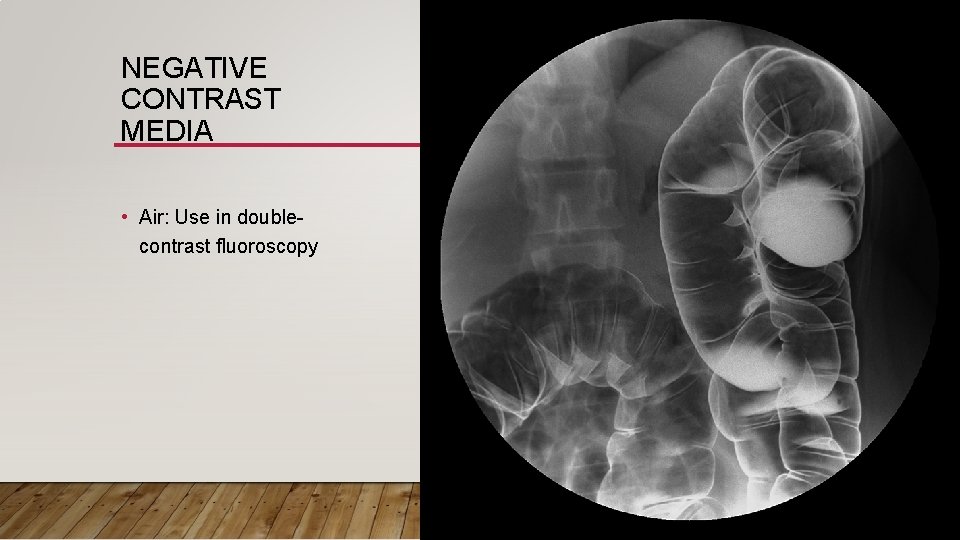
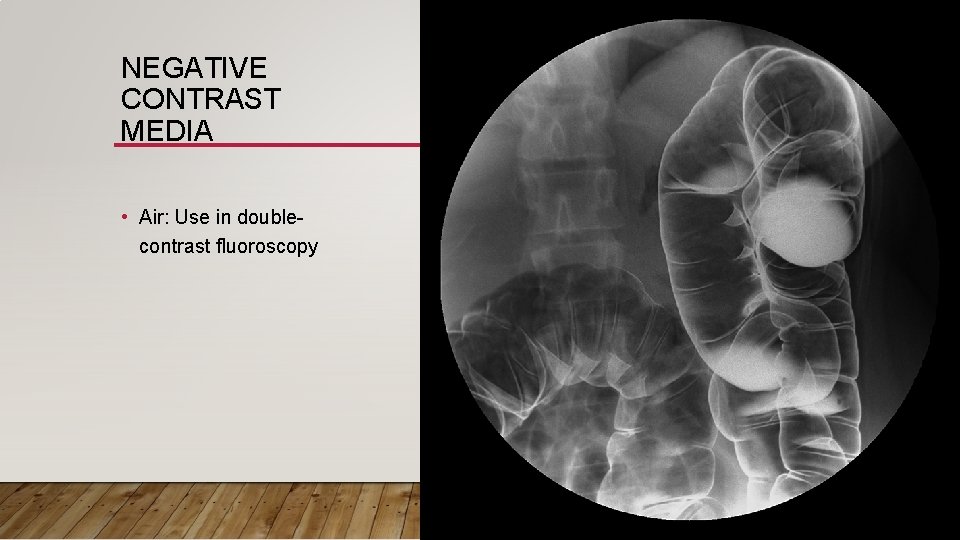
NEGATIVE CONTRAST MEDIA • Air: Use in doublecontrast fluoroscopy

CONTRAST REACTION
GOAL OF CONTRAST USAGE • 1) to assure that the administration of contrast is appropriate for the patient and the indication • 2) to minimize the likelihood of a contrast reaction • 3) to be fully prepared to treat a reaction should one occur
ADVERSE EFFECT OF INTRAVENOUS CONTRAST MEDIA • Allergy • Contrast-induced nephropathy • Nephrogenic systemic fibrosis • Contrast extravasation

ALLERGY
RISK FACTOR FOR INTRAVENOUS CONTRAST REACTION • Allergy • Asthma • Renal insufficiency • Cardiac status • Miscellaneous factors: Age, underlying disease such as hyperthyroidism, paraproteinemia in multiple myeloma, sickle cell anemia, etc.
ALLERGY • Allergic of prior contrast usage increased 5 fold likelihood ratio • Allergic rhinitis ? ? • Seafood allergy ? ? • History of anaphylaxis
ASTHMA • A history of asthma may indicate an increased likelihood of a contrast reaction • Especially active hyperresponsive airway disease
RENAL INSUFFICIENCY • Can causes contrast-induced nephropathy (CIN), nephrogenic systemic fibrosis (NSF) • Metformin usage
CARDIAC DISEASE • Congestive heart disease, severe aortic stenosis, pulmonary hypertension, severe cardiomyopathy • May increased risk of contrast reaction • Attention should be paid to limiting the volume and osmolality of the contrast media.
PREMEDICATION • Approximately 90% of such adverse reactions are associated with direct release of histamine and other mediators from circulating basophils and eosinophils • Pathophysiologic explanations include activation of mast cells and basophils releasing histamine, activation of the contact and complement systems, conversion of L-arginine into nitric oxide, activation of the XII clotting system leading to production of bradykinin, and development of “pseudoantigens”
PREMEDICATION • Dose response studies in humans of the suppression of whole blood histamine and basophil counts by IV methylprednisone show a reduction in circulating basophils and eosinophils by the end of the first postinjection hour • However, reaching statistical significance compared with controls by the end of the second hour, and maximal statistical significance at the end of 4 hours
RECOMMENDED PREMEDICATION REGIMENS Elective Premedication Two frequently used regimens are: First regimen: • Prednisone – 50 mg by mouth at 13 hours, 7 hours, and 1 hour before contrast media injection, plus • Diphenhydramine (Benadryl®) – 50 mg intravenously, intramuscularly, or by mouth 1 hour before contrast medium
RECOMMENDED PREMEDICATION REGIMENS Second regimen: • Methylprednisolone (Medrol®) – 32 mg by mouth 12 hours and 2 hours before contrast media injection • An anti-histamine (as in option 1) can also be added to this regimen injection If the patient is unable to take oral medication, 200 mg of hydrocortisone intravenously may be substituted for oral prednisone
RECOMMENDED PREMEDICATION REGIMENS Emergency Premedication (In Decreasing Order of Desirability) • Methylprednisolone sodium succinate (Solu-Medrol®) 40 mg or hydrocortisone sodium succinate (Solu-Cortef®) 200 mg intravenously every 4 hours (q 4 h) until contrast study required plus diphenhydramine 50 mg IV 1 hour prior to contrast injection
RECOMMENDED PREMEDICATION REGIMENS • Dexamethasone sodium sulfate (Decadron®) 7. 5 mg or betamethasone 6. 0 mg intravenously q 4 h until contrast study must be done in patent with known allergy to methylpred-nisolone, aspirin, or non-steroidal anti-inflammatory drugs, especially if asthmatic. Also diphenhydramine 50 mg IV 1 hour prior to contrast injection. • Note: IV steroids have not been shown to be effective when administered less than 4 to 6 hours prior to contrast injection.
PREMEDICATION Type of contrast agent • Osmolarity: Hyperosmolality is associated with the stimulation of release of histamine from basophils and mast cells • Complexity and molecular size: Increase in the size and complexity of the contrast molecule may potentiate the release of histamine Nonionic monomers also produce lower levels of histamine release from basophils compared with high-osmolality ionic monomers, low-osmolality ionic dimers and iso -osmolality nonionic dimers
ACUTE CONTRAST REACTION • Allergic-liked reaction : from histamine which is released by mast cell and basophil • Physiologic reaction : direct chemotoxicity, osmotoxicity (adverse effects due to hyperosmolality) or molecular binding to certain activators • Frequently dose and concentration dependent • Frequent reaction: vagovagal reaction, feeling of apprehension and accompanying diaphoresis • Rare reaction: Cardiac arrhythmias, depressed myocardial contractility, cardiogenic pulmonary edema, and seizures
DELAYED CONTRAST REACTION • Most commonly cutaneous and may develop from 30 to 60 minutes to up to one week following contrast material exposure • Can occurring between three hours and two days • Symptoms; allergic-liked cutaneous reaction (most common), nausea/vomitting, fever, headache, iodine-related sialoadenopathy, polyarthroplasty
EVALUATION OF THE CONTRAST REACTION Mild reaction • Signs and symptoms are self-limited without evidence of progression. Mild reactions include: • Allergic-like : Limited urticaria / pruritis Limited cutaneous edema Limited “itchy” / “scratchy” throat Nasal congestion/ Sneezing / conjunctivitis / rhinorrhea • Physiologic : Limited nausea / vomiting/ Transient ushing / warmth / chills Headache / dizziness / anxiety / altered taste Mild hypertension/ Vasovagal reaction that resolves spontaneously
EVALUATION OF THE CONTRAST REACTION Moderate • Signs and symptoms are more pronounced and commonly require medical management. Some of these reactions have the potential to become severe if not treated. Moderate reactions include: • Allergic-like • Diffuse urticaria / pruritis, Diffuse erythema, stable vital signs, Facial edema without dyspnea, Throat tightness or hoarseness without dyspnea • Wheezing / bronchospasm, mild or no hypoxia
EVALUATION OF THE CONTRAST REACTION Moderate • Physiologic • Protracted nausea / vomiting Hypertensive urgency Isolated chest pain • Vasovagal reaction that requires and is responsive to treatment
EVALUATION OF THE CONTRAST REACTION Severe • Allergic-like • Diffuse edema, or facial edema with dyspnea Diffuse erythema with hypotension Laryngeal edema with stridor and/or hypoxia, Wheezing / bronchospasm, Significant hypoxia, Anaphylactic shock (hypotension + tachycardia) • Physiologic • Vasovagal reaction resistant to treatment Arrhythmia Convulsions, seizures Hypertensive emergency
TREATMENT OF MILD REACTION • Typically do not require medical treatment • Vital signs should be obtained to detect hypotension that may be clinically silent while the patient is supine • Observed for 20 to 30 minutes, or as long as necessary • Antihistamine IV
TREATMENT OF MODERATE TO SEVERE REACTION • IV fluid • Antihistamine : Benadryl 1 mg/kg IV for moderate urticaria • Epinephrine 0. 1 mg/kg IV or 0. 3 mg IM for profound hypotension, anaphylaxis, bronchospasm • Betaagonist inhalator for mild and moderate bronchospasm
CONTRAST-INDUCED NEPHROPATHY (CIN)
CONTRAST-INDUCED NEPHROPATHY • A sudden deterioration in renal function that is caused by the intravascular administration of iodinated contrast medium • Diagnosis by use percent change in the baseline serum creatinine and absolute elevation from baseline serum creatinine (absolute increase of 0. 5 mg/d. L over a baseline)
DEFINITION OF ACUTE RENAL INJURY The diagnosis of AKI is made according to the AKIN criteria if one of the following occurs within 48 hours after a nephrotoxic event (e. g. , intravascular iodinated contrast medium exposure): • Absolute serum creatinine increase ≥ 0. 3 mg/d. L (>26. 4 μmol/L) • A percentage increase in serum creatinine ≥ 50% (≥ 1. 5 -fold above baseline) • Urine output reduced to ≤ 0. 5 m. L/kg/hour for at least 6 hours.
RENAL FUNCTION • Serum creatinine concentration is the most commonly used measure of renal function • BUT!!! Serum creatinine has limited accuracy for evaluate GFR • Calculated estimated glomerular filtration rate (e. GFR) is more accurate than is serum creatinine at predicting true GFR e. GFR is gaining attention as a potentially better marker of CIN risk
RISK FACTORS • Pre-existing severe renal insufficiency Most important risk factor • - e. GFR < 30 ml/min/1. 73 m 2 significant risk • Underlying disease: DM, Cardiovascular disease, Multiple myeloma, Hypertension • Dehydration • Diuretic use • Advanced age • Multiple iodinated contrast medium doses in a short time interval (<24 hours)
PREVENTION • Avoid usage of the iodinated-contrast agent • Select type of contrast agent : LOCM are less nephrotoxic than HOCM in patients with underlying renal insufficiency. • Volume expansion : Major effective action - 0. 9% saline at 100 m. L/hr, beginning 6 to 12 hours before and continuing 4 to 12 hours after intravenous iodinated contrast administration • N-acetylcysteine : unknown mechanism
RENAL INSUFFICIENCY • Most low-osmolality iodinated contrast media are not protein-bound, have relatively low molecular weights, and are readily cleared by dialysis • Unless an unusually large volume of contrast medium is administered, or there is substantial underlying cardiac dysfunction, there is no need for urgent dialysis after intravascular iodinated contrast medium administration
NEPHROGENIC SYSTEMIC FIBROSIS (NSF)
NEPHROGENIC SYSTEMIC FIBROSIS • Fibrosing disease, primarily involving the skin and subcutaneous tissues • but also involve other organs, such as the lungs, esophagus, heart, and skeletal muscles • Initial symptoms typically include skin thickening and/or pruritis • May develop and progress rapidly, with some affected patients developing contractures and joint immobility • In some patients, the disease may be fatal
ASSOCIATION • Gadolinium-based MR contrast • Acute kidney injury (AKI) • Chronic renal disease Patients with end-stage CKD (CKD 5, e. GFR < 15 m. L / min/1. 73 m 2) and severe CKD (CKD 4, e. GFR 15 to 29 m. L / min/1. 73 m 2) have a 1% to 7% chance of developing NSF after one or more exposures to at least some GBCAs
RECOMMENDATION ACR Committee on Drugs and Contrast Media believes that patients receiving any GBCA should be considered at risk of developing NSF if any of the following conditions applies: • on dialysis (of any form) • severe or end-stage CKD (CKD 4 or 5, e. GFR < 30 m. L / min/1. 73 m 2) without dialysis • e. GFR 30 to 40 m. L / min/1. 73 m 2 without dialysis* • AKI
NSF WITH HEMODIALYSIS • Hemodialysis ? ? ? • Most patients who developed NSF had end-stage kidney disease and were on dialysis at the time of exposure • So, hemodialysis cannot prevent NSF !!!

CONTRAST EXTRAVASATION
CONTRAST EXTRAVASATION • Leakage of the contrast agent from systemic circulation • Incidence 0. 1% - 0. 9% Sign and symptom: • Complain of initial swelling or tightness, and/or stinging or burning pain at the site of extravasation • Edematous, erythematous, and tender nearby the injected site


RISK OF CONTRAST EXTRAVASATION • Patients who cannot communicate adequately • Severely ill or debilitated patients • Patients with abnormal circulation in the limb to be injected : • - Atherosclerotic peripheral vascular disease • - Diabetic vascular disease, Raynaud’s disease, venous thrombosis or insuffciency • - Prior radiation therapy or extensive surgery
RISK OF CONTRAST EXTRAVASATION (CONT. ) • >24 hour of injected site • Multiple venous punture • High injected flow rate ? ? ? • Amount of injected contrast agent ? ? ?
SEQUELAE OF CONTRAST EXTRAVASATION • Acute local inflammatory response (24 -48 hr) due to hyperosmolarity of the contrast media • Hyperosmolar contrast agent can cause more severe reaction than low-osmolar contrast agent • Most extravasations are limited to the immediately adjacent soft tissues (typically the skin and subcutaneous tissues), and usually there is no permanent injury
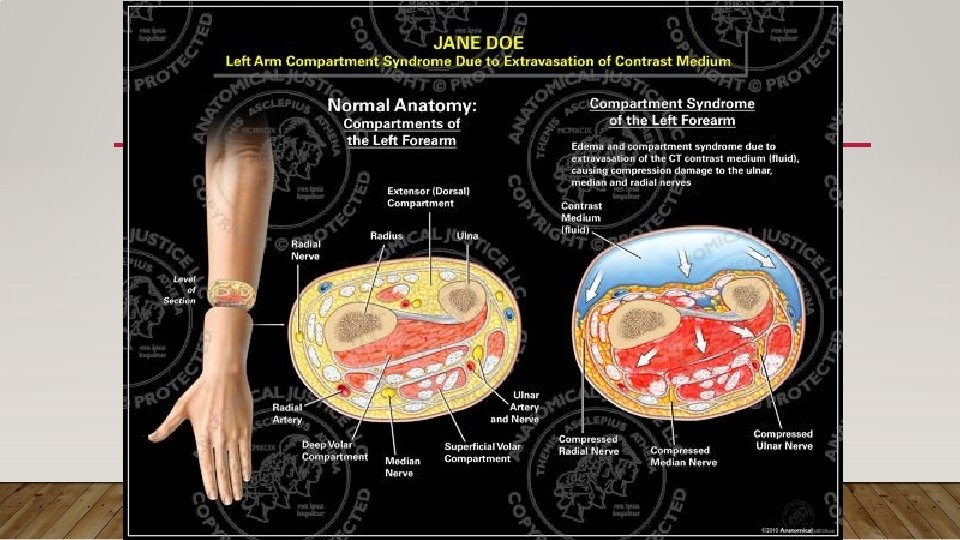
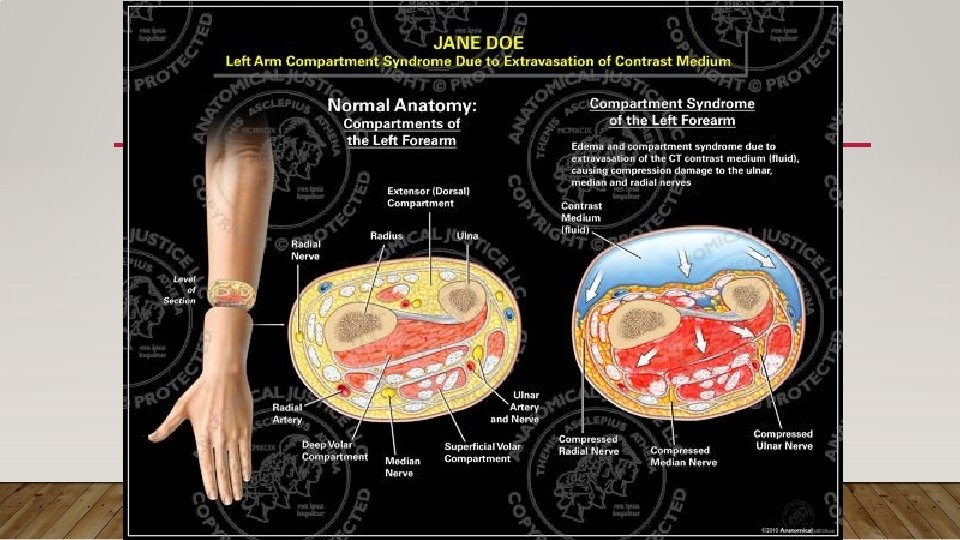
COMPLICATION OF THE CONTRAST EXTRAVASTION • Compartment syndrome occur after large amount of contrast leakage • Skin ulceration • Soft tissue necrosis
TREATMENT OF CONTRAST EXTRAVASATION • Elevation of the affected extremity above the level of the heart decrease capillary hydrostatic pressure and promote resorption of extravasated fluid • Warm or cold compresses ? ? ? • Aspirate the extravasated contrast medium through an inserted needle or angiocatheter ? ? ? • Local injection of other agents such as corticosteroids or hyaluronidase ? ? ? • Surgical consult : progressive swelling or pain, altered tissue perfusion, change in sensation in the affected limb, and skin ulceration or blistering
REFERENCES • Introduction ACR Manual on Contrast Media – Version 10. 1, 2015

THANK YOU FOR YOUR ATTENTION