Contrast Induced Nephropathy Sh Taheri Associate Prof MUI





































- Slides: 61
Contrast Induced Nephropathy Sh. Taheri Associate Prof. MUI
History • �In 1906, Von Lichtenberg and Voelcker used 2% colloidal silver solution, for retrograde pyelography studies. (toxic to kidneys, death). • �In 1920, Osborne and colleagues, 10% “Na. I” for Rx of syphilis, fortuiously found it to be radiopaque , excreted by kidneys. —first pyelogram. • Selectan - Moses Swick • Uroselectan , 1927 – increased solubility and less toxicity. • In 1993, Hippuran was introduced. • Binz and Rath – Neo ipax(Iodoxyl) and diodrast (Diodone) • 1927 – Werner Frossmann – self catheterization, using urinary catheter( antecubital vein), (Na. I) • 1923, Berbrich and hirsch –femoral angiogram • 1924, Brooks – first angiogram (under GA).
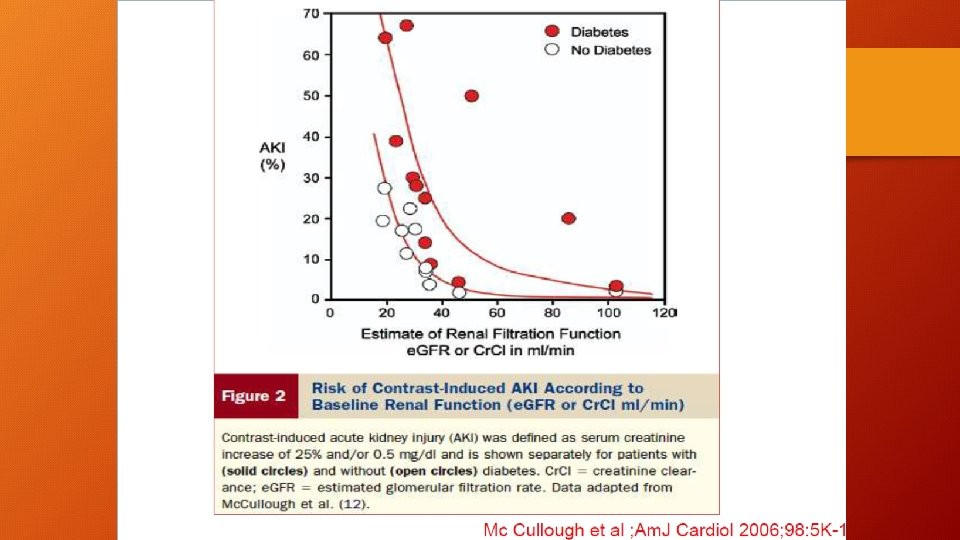
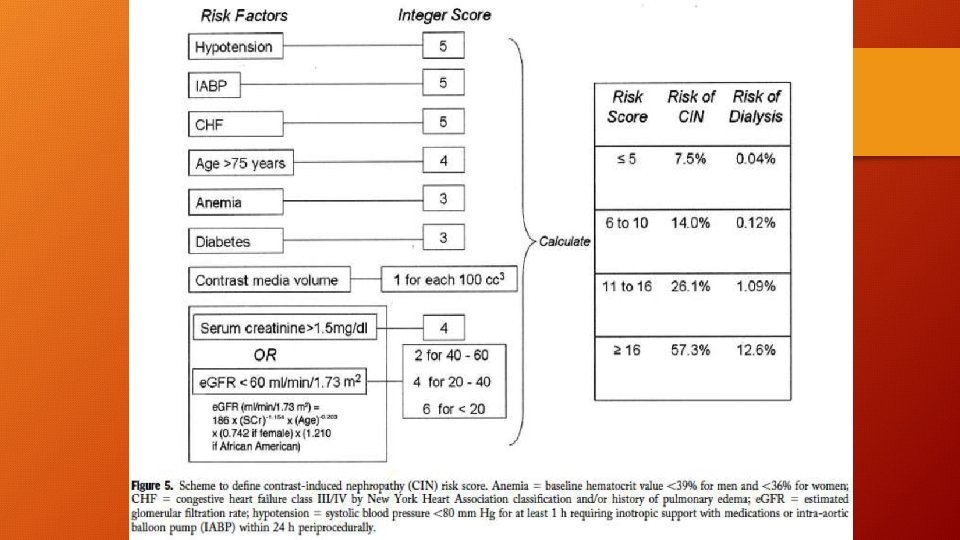
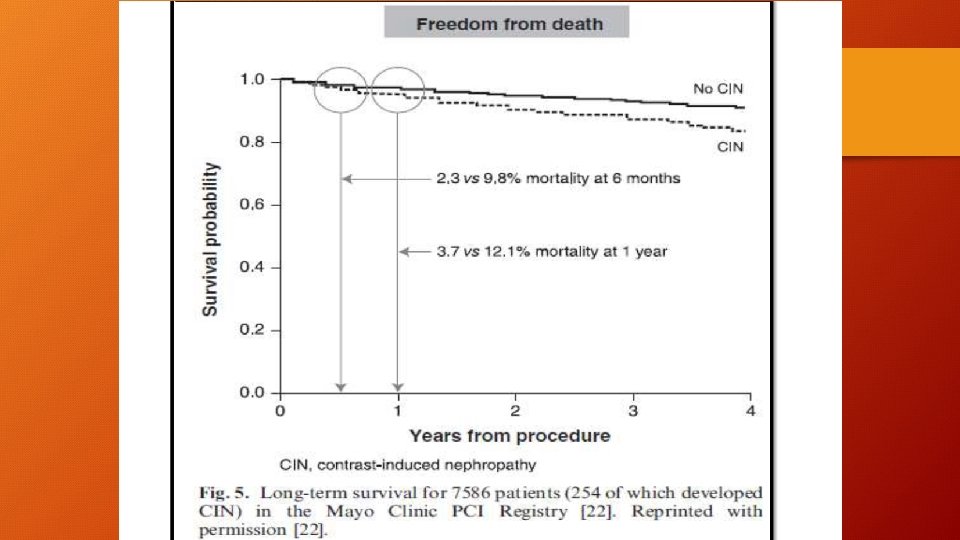
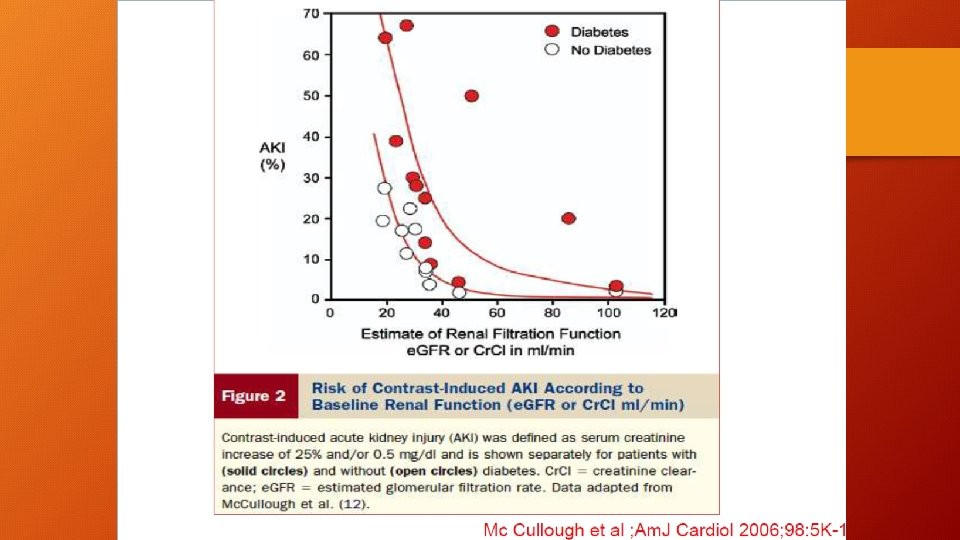
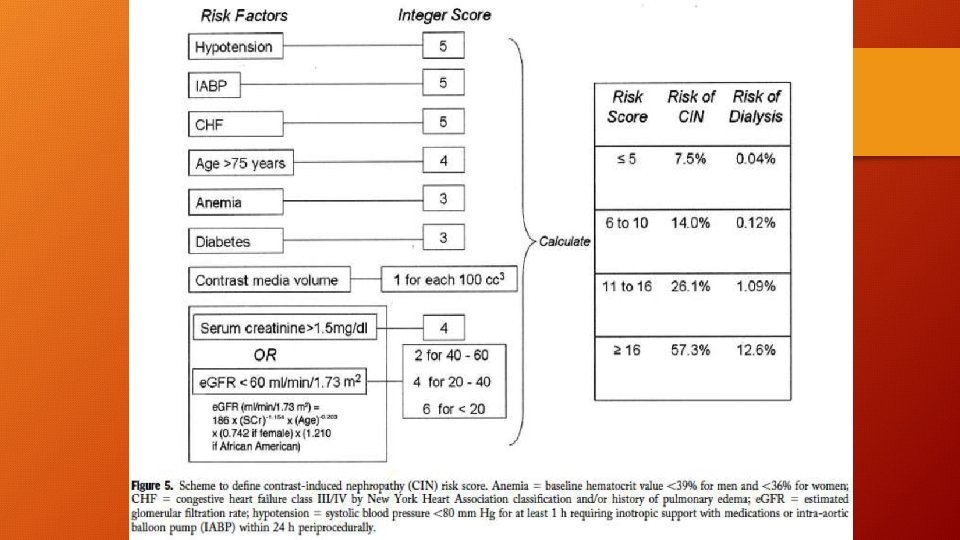
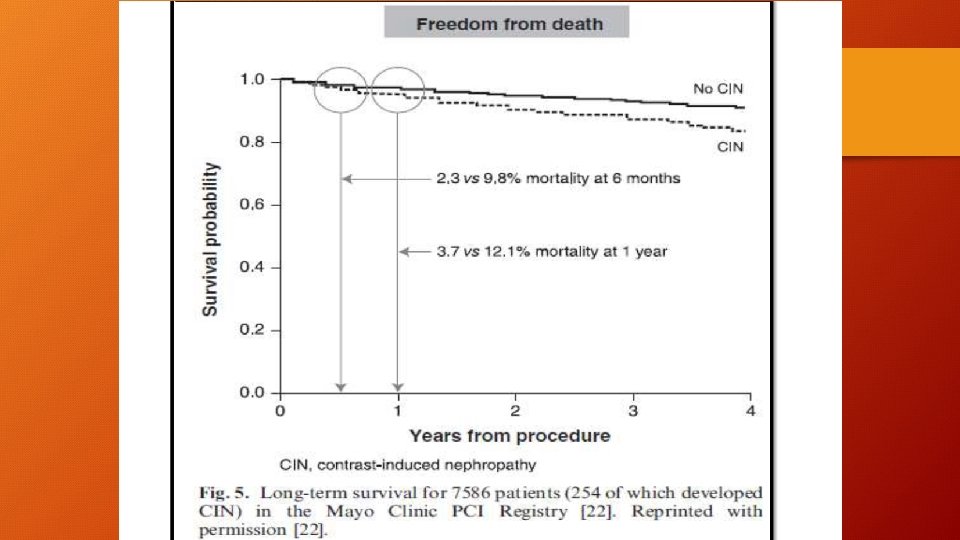
Epidemiology • Incidence in General population <2%. * • Overall incidence is 14. 5% (epidemiological study)^ • Among diabetics, mild –moderate CKD – 9 -40%. # • Severe CKD 50 -90%. • 5% of hospital admissions. ** • Cases of CI-AKI leading to dialysis are rare (0. 5 to 2. 0%). • When it leads to dialysis in hospital mortality of 35. 7%, 18. 8% • - 2 yr survival rate $.
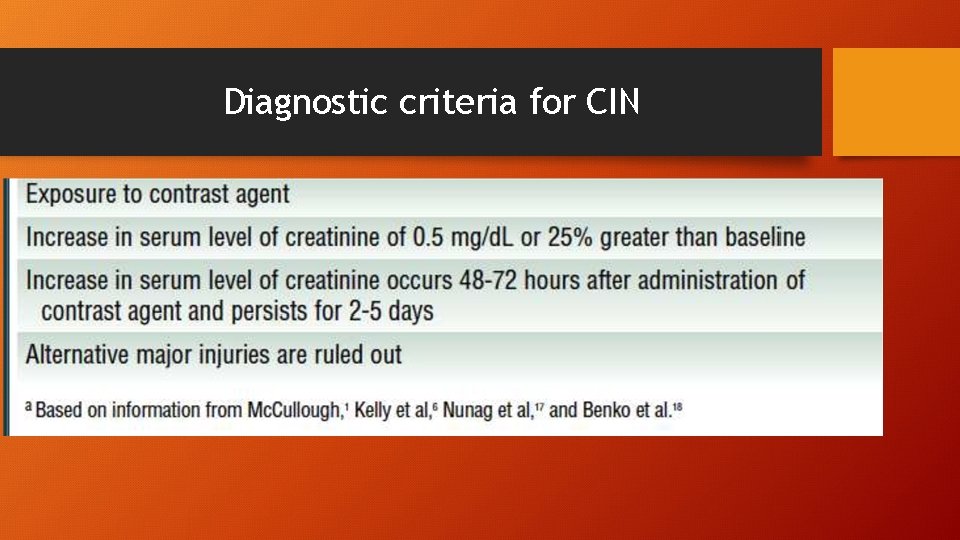
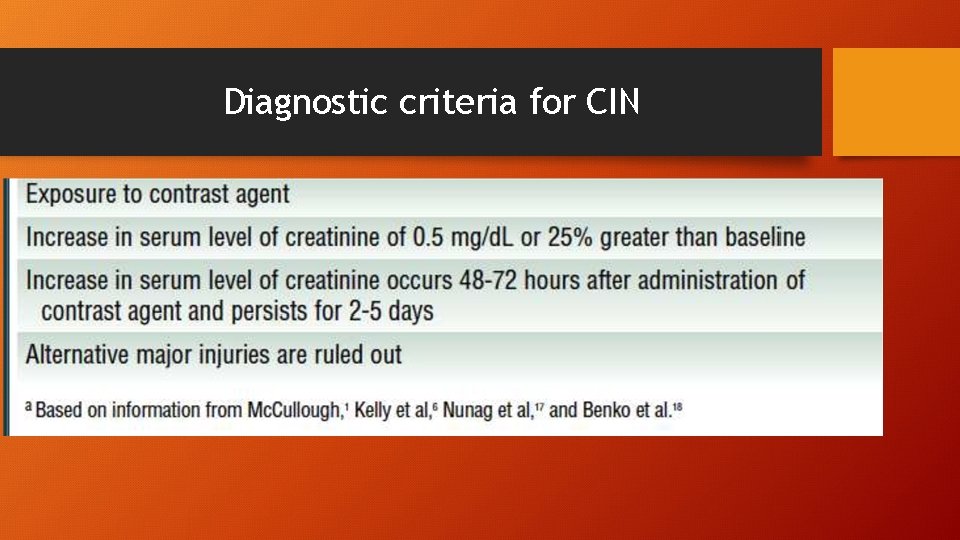
Diagnostic criteria for CIN

KDIGO Definition • CI-AKI is defined by the Kidney Disease Global Outcomes (KDIGO) guidelines as: • “…increase in serum creatinine of 0. 3 mg/d. L or greater within 48 hours of contrast use or • a 50% or greater increase from baseline serum creatinine within 7 days”.
Course • The serum creatinine usually increases within 24 -48 hrs after contrast administration, peaks at 3 to 5 days, and returns to baseline in 1 -3 weeks.


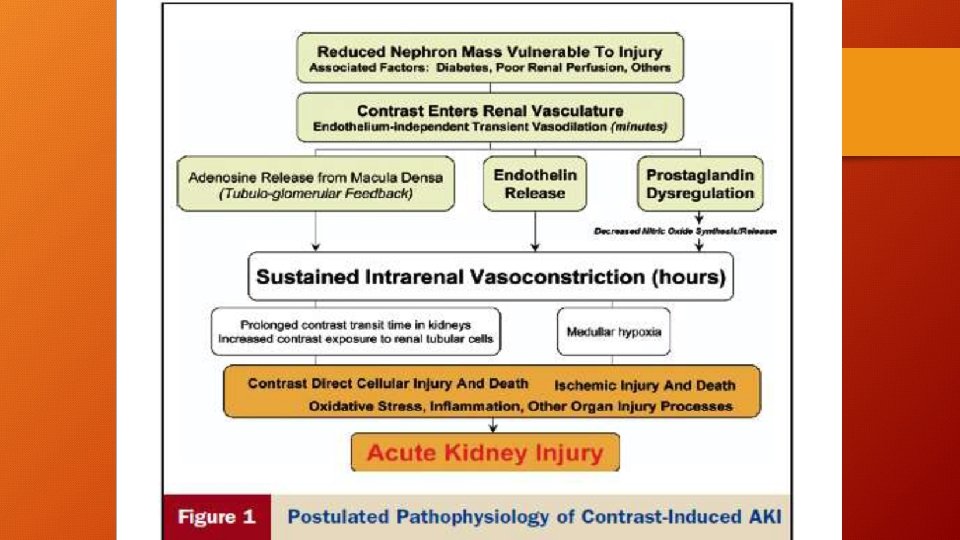
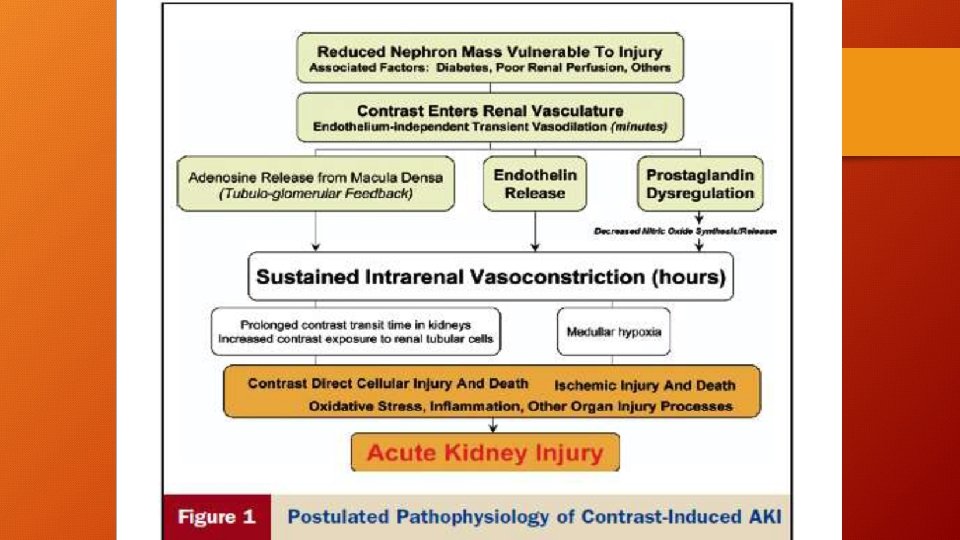
Pathophysiology • • • Combination of toxic and ischemic injury to renal tubular cells. Rheological alterations Activation of tubuloglomerular feedback Vasoconstriction Decreased blood flow Regional Hypoxia Cytotoxic effect on renal epithelial cells Generation of ROS Increased adenosine or endothelin production









CONTRAST MEDIA • Important considerations in choosing a contrast agent • �SOLUBILITY • �OSMOLALITY • �VISCOSITY

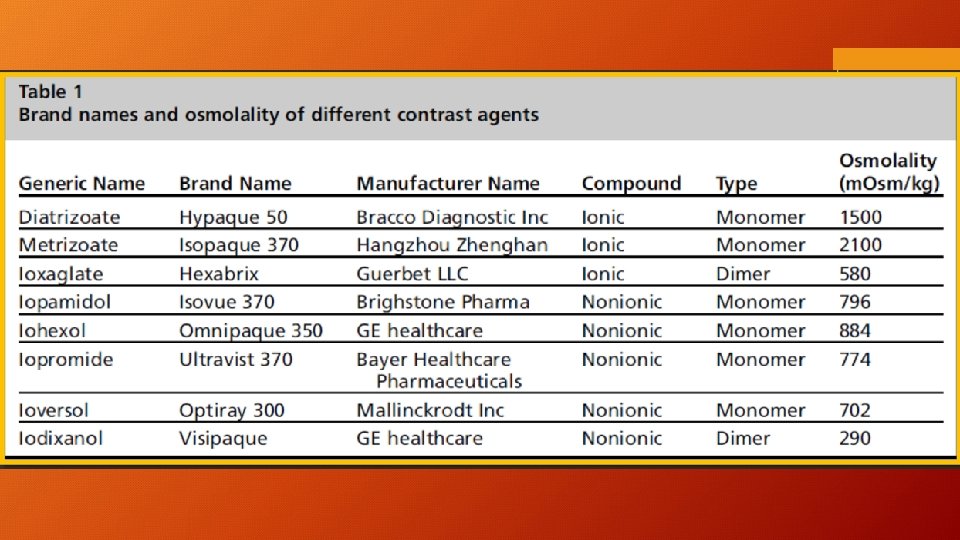
CONTRAST MEDIA • Classified into ionic and nonionic groups based on water solubility. • Ionic agents, water soluble, dissosciate into negative and positive ions, bind with negative and positive poles of water molecules. • Nonionic agents donot dissosciate, but are water soluble, polar OH groups.
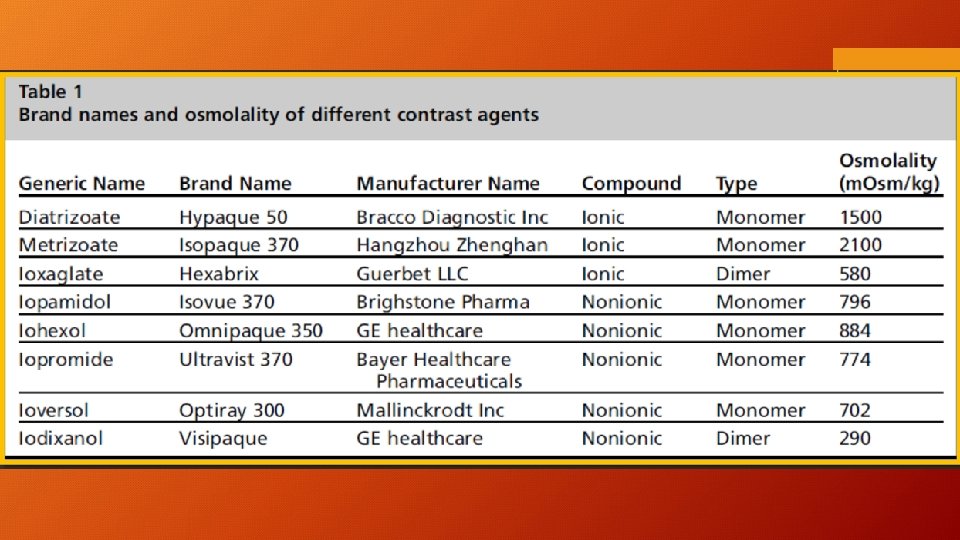
TYPES OF CONTRAST MEDIA • Based on osmolality relative to plasma • HIGH OSMOLAR CONTRAST AGENTS (HOCM) • LOW OSMOLAR CONTRAST AGENTS (LOCM) • ISOOSMOLAR CONTRAST AGENTS (IOCM) • Further classification is by contrast agent ratio No. of iodine atoms/No. of particles in solution. • Most imp. factor impacting attenuation.

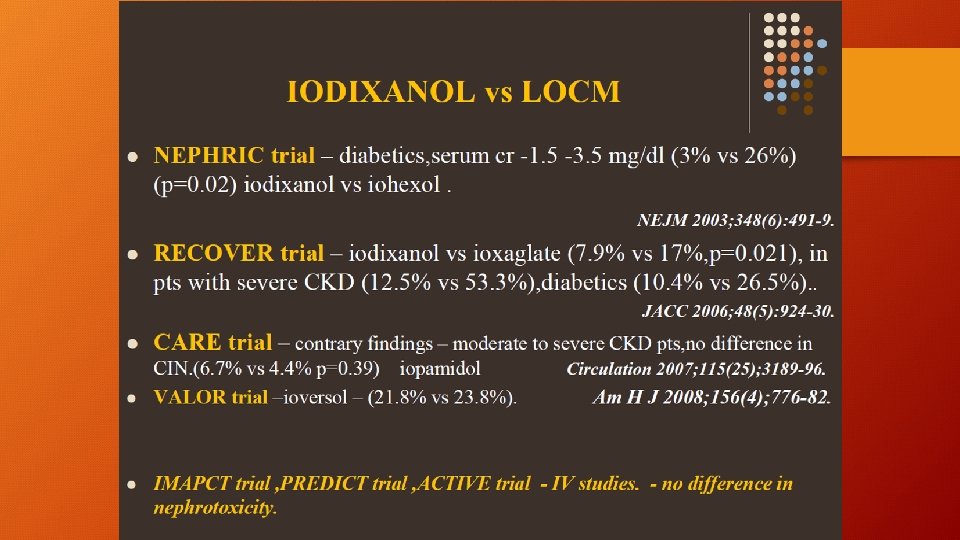
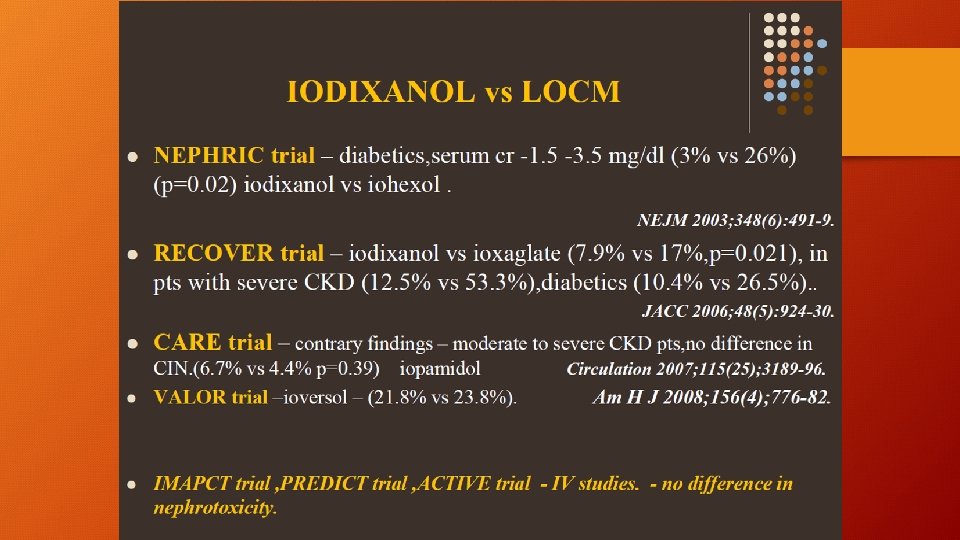
Comparison of different osmolar agents. . which is beneficial ? ? • Iohexol cooperative study; Rudnick et al – IOHEXOL vs DIATRIZOATE, iohexol was less nephrotoxic in patients with CKD ±Diabetes. (7% vs 4% , 27% vs 12%) Kidney Intern 1995; 47(1): 254 -61 • No difference in nephrotoxicity in patients with normal kidney function, with or without diabetes.

PREVENTIVE MEASURES
Four basic concepts 1. hydration and volume expansion 2. choice and quantity of contrast material (IOCM or LOCM) 3. pre, intra, post procedural end organ protection with pharmacotherapy. 4. Post procedural monitoring and expectant care. (24 -48 hrs post procedure s. creatinine), (dialysis need in patients with e. GFR<30 ml/min/1. 73 m 2)
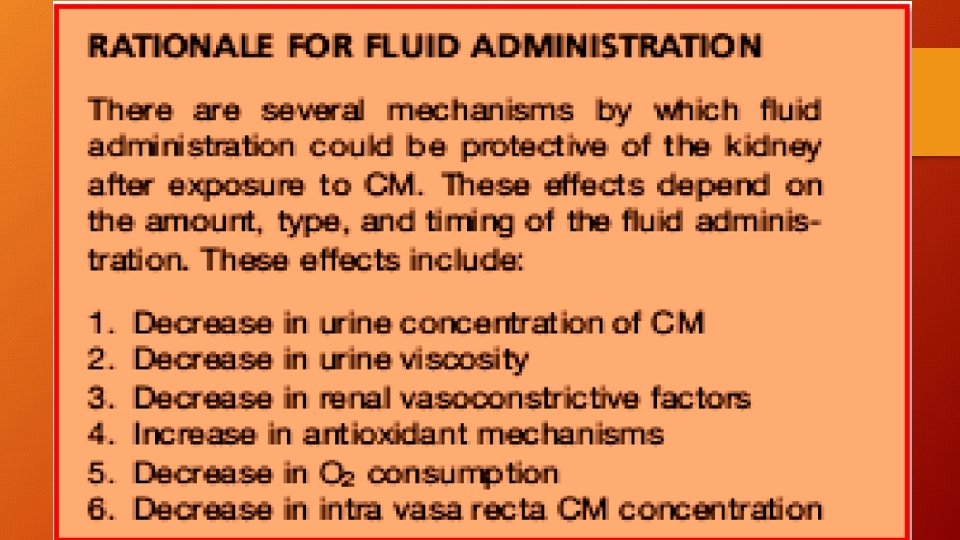
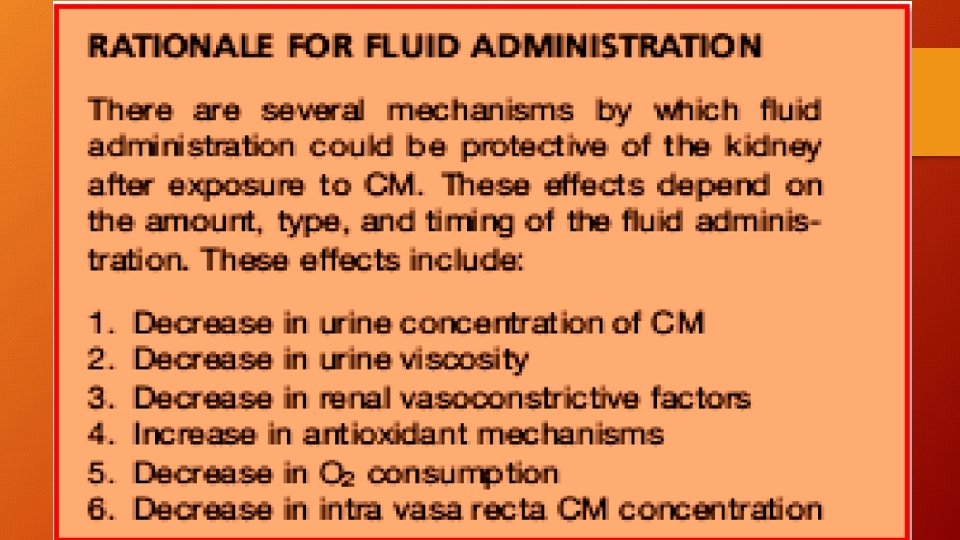
HYDRATION �Simplest and most effective way of protecting renal function. (decreases by 50% chance of CI-AKI) �Effect of contrast agents on kidney is prolonged in dehydration. ( RBF, GFR). � 0. 9% NS by IV infusion at a rate of approx. 1 -1. 5 ml/kg/hr. (adjust accordingly). �At least 300 -500 ml of IV hydration before administration of contrast material. � 6 -12 hr before the procedure and continued for upto 12 -24 hr after the radiographic examination, if diuresis is appropriate. �Urine output 150 ml/hr. (if more – replace the lost fluids)
When before/during/after procedure? • Administration of fluid immediately before or at the time of CM exposure is less efficacious for prevention of CIN. • Sufficient time to increase urine output, decrease vasoconstrictive forces, replete extracellular volume are required for optimal protection. • 6 hrs -12 hrs before procedure, 12 hrs -24 hrs after procedure.

















RECENT TRENDS IN CI-AKI




