CONTRACEPTION Objectives l Describe the advantages disadvantages failure
CONTRACEPTION
Objectives l Describe the advantages, disadvantages, failure rates, and complications associated with the following methods of contraception – – – Sterilization Oral steroid contraception Injectable steroid contraception Implantable steroid contraception Barrier methods Natural family planning
Abstinence l Mechanism: excludes sperm from female reproductive tract l Effectiveness: 0% failure rate l Ideal for adolescents at high risk for pregnancy and STD’s including HIV l Complications: None
Breastfeeding: Lactation Amenorrhea Method (LAM) l Mechanism: Suckling causes increased prolactin, which inhibits estrogen production and ovulation l 2% typical use failure rate in 1 st six mos. l Candidates: – Amenorrheic women < 6 mos post-partum who exclusively breastfeed (90% of nutrition is breast milk) – Women free of blood-borne infections – Women not on drugs that could effect baby Kennedy KI. et al. , Contraceptive Technology. 2004

LAM Complications l Breastfeeding may increase the risk of mastitis l Return of fertility or ovulation may precede menses. l 33 -45% ovulate during 1 st 3 months. l Encourage backup form of contraception

Barrier Methods: Male Condoms
Barrier Methods: Male Condoms l Sheaths of latex, polyurethane, or natural membranes that may or may not have spermicide. l Mechanism: Barrier that prevents sperm and infections from entering vagina. l Effectiveness: 15% typical use failure rate. l Candidates: – – Couples not in mutually monogamous relationships Couples in which one partner has an STD/HIV Couples starting other types of birth control Couples who can’t use hormonal methods Warner DL, et al. Contraceptive Technology. 2004

Barrier Method: Female Condom l Disposable single use polyurethane sheath placed in vagina. l Flexible movable inner ring at closed end used to insert into vagina. l Flexible outer ring to cover part of the introitus. l Mechanism: Prevents passage of sperm and infections into the vagina. l Failure rate is high at 21% with typical use. Hatcher et al. Managing Contraception. 2004
Barrier Method: Female Condom l Candidates the same as for male condoms. l Female condom is reusable only if the partner does not have an STD. l Disadvantages: – Awkward and difficult to place – Most users do not enjoy using female condom (88% of women and 91% of men) – Many couples complain about noise of condom
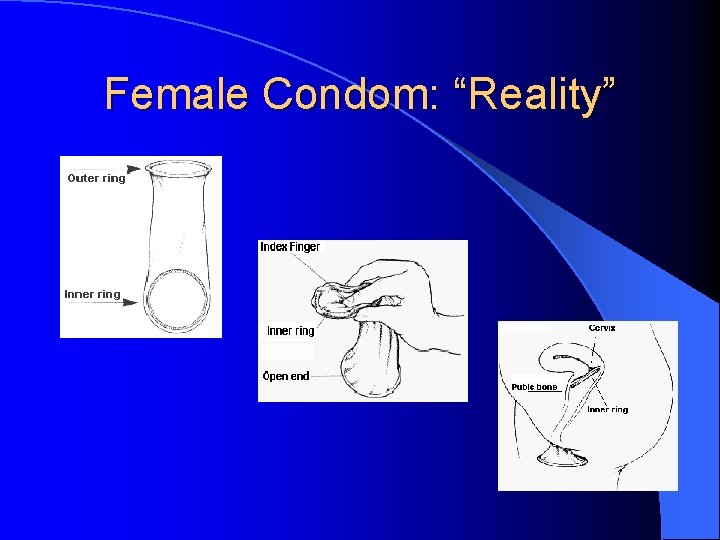
Female Condom: “Reality”
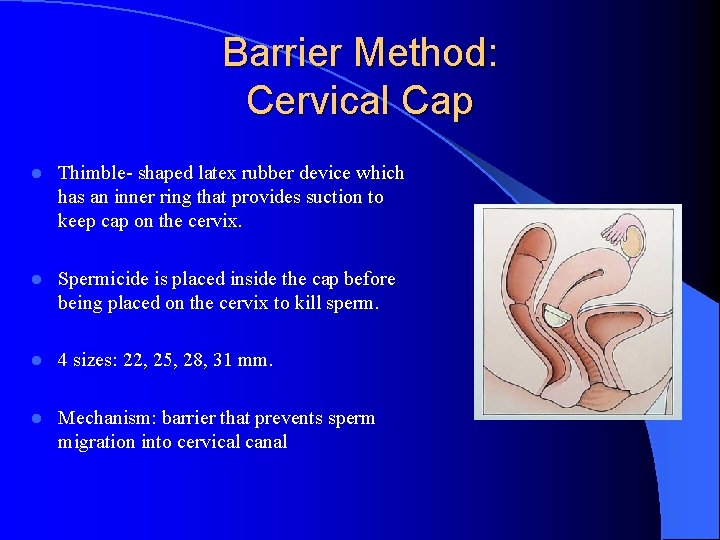
Barrier Method: Cervical Cap l Thimble- shaped latex rubber device which has an inner ring that provides suction to keep cap on the cervix. l Spermicide is placed inside the cap before being placed on the cervix to kill sperm. l 4 sizes: 22, 25, 28, 31 mm. l Mechanism: barrier that prevents sperm migration into cervical canal
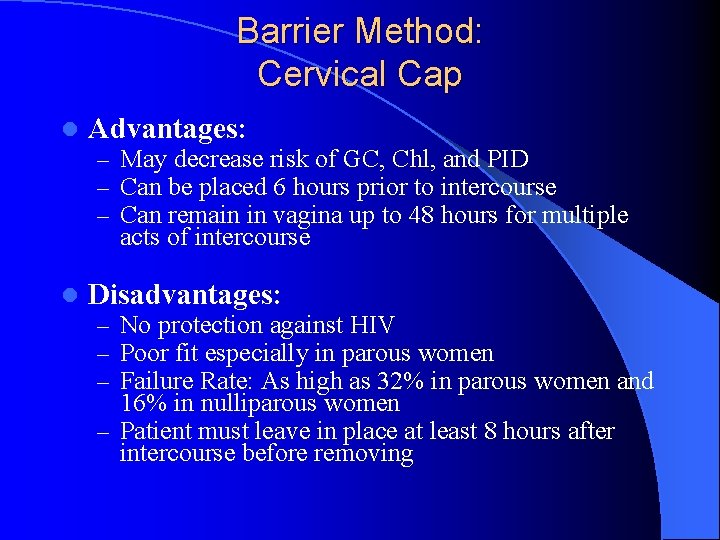
Barrier Method: Cervical Cap l Advantages: – May decrease risk of GC, Chl, and PID – Can be placed 6 hours prior to intercourse – Can remain in vagina up to 48 hours for multiple acts of intercourse l Disadvantages: – No protection against HIV – Poor fit especially in parous women – Failure Rate: As high as 32% in parous women and 16% in nulliparous women – Patient must leave in place at least 8 hours after intercourse before removing
Diaphragm
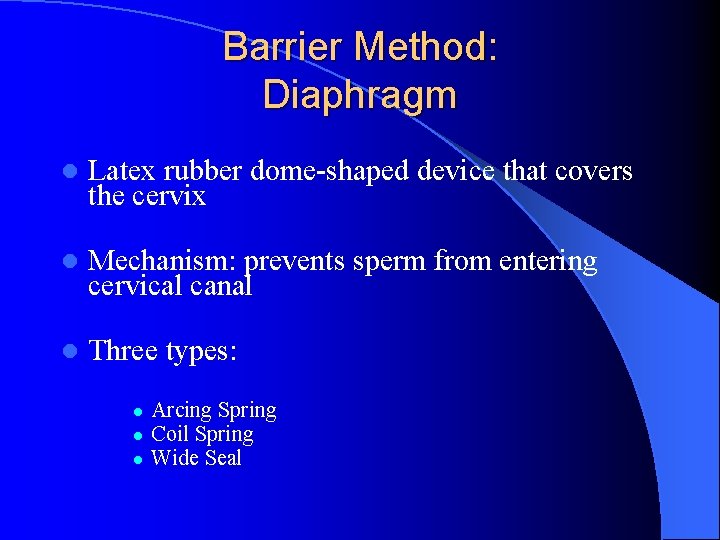
Barrier Method: Diaphragm l Latex rubber dome-shaped device that covers the cervix l Mechanism: prevents sperm from entering cervical canal l Three types: l l l Arcing Spring Coil Spring Wide Seal
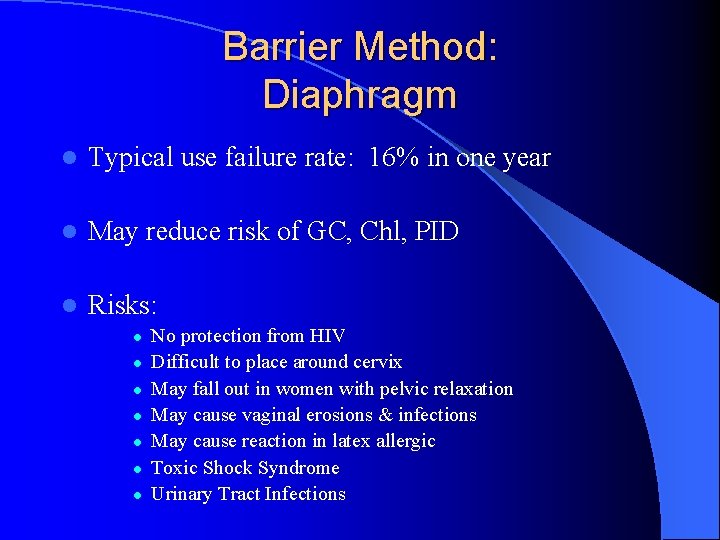
Barrier Method: Diaphragm l Typical use failure rate: 16% in one year l May reduce risk of GC, Chl, PID l Risks: l l l l No protection from HIV Difficult to place around cervix May fall out in women with pelvic relaxation May cause vaginal erosions & infections May cause reaction in latex allergic Toxic Shock Syndrome Urinary Tract Infections
SPERMICIDE l Most common is nonoxynol-9 l Available in creams, films, foams, gels, suppositories, sponges, and tablets l Best when used with barrier methods l 29% typical use failure rate when used alone l Provides no protection against STD’s and HIV

Emergency Contraception (EC) l Any method used after unprotected or inadequately protected sexual intercourse l Three types of EC available in the United States: l l l High dose progestin only ( Plan B) Yuzpe method- 13 different combined oral contraceptives (Preven) Copper IUD ( Paragard) Dickey. Managing Contraceptive Pill Patients, 2002
Emergency Contraception (EC) l Mechanism: Prevents fertilization and implantation. l Counsel patients that this method does not abort a pregnancy that is already implanted l Common in women after an assault or rape l Most women will have a cycle 21 days after completing emergency contraception l If patient does not have a cycle in 21 days, it is important to check a pregnancy test
Emergency Contraception (EC) l High dose progestin-only (Plan B): l l l 1. 5 mg Norgestrel at one time or in divided doses. Divided Dose: 1 st dose within 72 -120 hours of intercourse. 2 nd dose 12 hours later. One dose: Both tablets within 72 -120 hours of intercourse
Emergency Contraception (EC) l Yuzpe Method (Preven) – 100 mcg of ethinyl estradiol and 0. 50 mg of levonorgestrel in each dose. – 1 st dose within 72 hours of intercourse and 2 nd dose 12 hours later
Emergency Contraception (EC) l Copper IUD – Place within 5 days of unprotected coitus. – This is usually given to women who plan to use the IUD for long term birth control. – Interferes with implantation after fertilization.
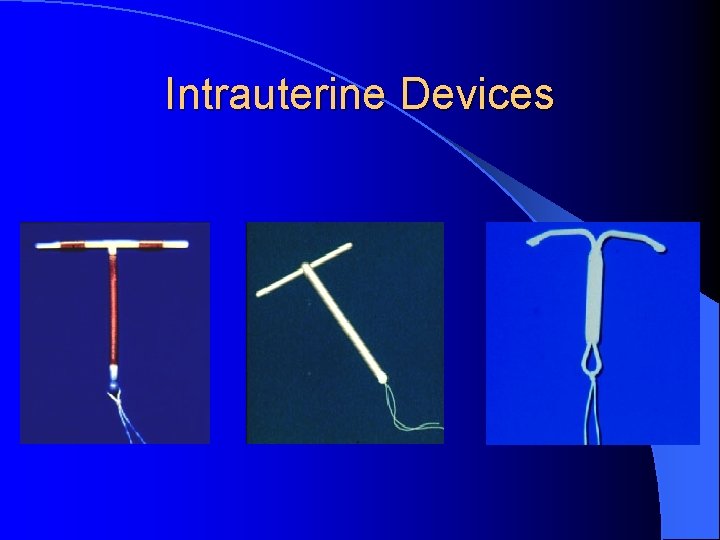
Intrauterine Devices
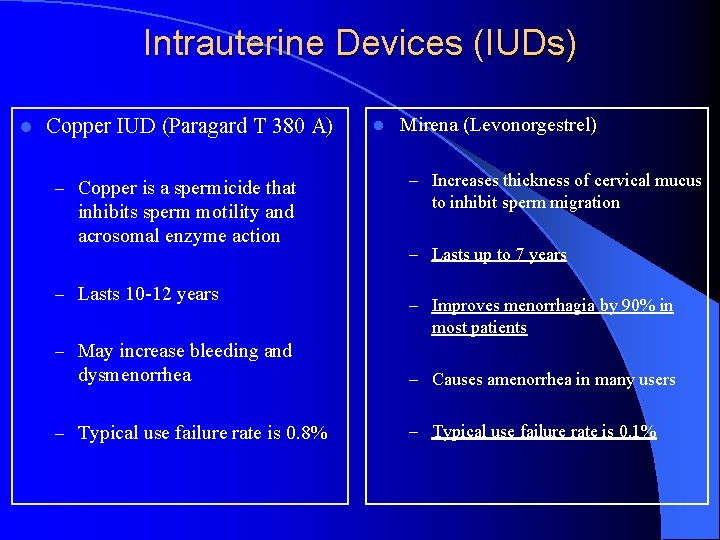
Intrauterine Devices (IUDs) l Copper IUD (Paragard T 380 A) – Copper is a spermicide that inhibits sperm motility and acrosomal enzyme action – Lasts 10 -12 years l Mirena (Levonorgestrel) – Increases thickness of cervical mucus to inhibit sperm migration – Lasts up to 7 years – Improves menorrhagia by 90% in most patients – May increase bleeding and dysmenorrhea – Typical use failure rate is 0. 8% – Causes amenorrhea in many users – Typical use failure rate is 0. 1%
IUD l Good for women in mutually monogamous relationships l Risks: – Increased risk of PID within 1 st 20 days – Uterine perforation – Fainting with insertion – Expulsion – Unexpected pregnancy following poor placement
Combined Oral Contraceptives (Estrogen & Progestin) l Mechanism: – Blocks ovulation – Thickens cervical mucus – Thins the endometrial lining
Combined Oral Contraceptives (Estrogen & Progestin) l Ethinyl estradiol is the most commonly used estrogen in OCP’s l There are multiple forms of progestins l Monophasic: same amount of hormone in each active tablet l Multiphasic: varying amounts of hormone in each active pill l Most OCP’s have 21 active pills and 7 placebo pills
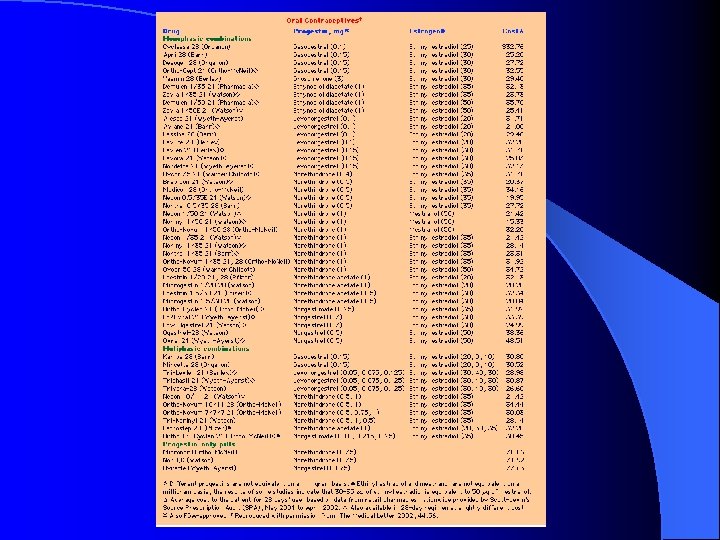

Combined Oral Contraceptives (Estrogen & Progestin) l Alternate Formulations: – Seasonale: 84 consecutive hormonal pills followed by 7 days of placebo – Ovcon-35: chewable pills – Yasmin: Drospirenone which is anti-androgenic and anti-mineralcorticoid

Combined Oral Contraceptives (Estrogen & Progestin) l Non-contraceptive Uses of OCPs – Dysfunctional uterine bleeding – Dysmenorrhea – Mittelschmerz – Endometriosis prophylaxis – Acne and hirsutism – Hormone replacement – Prevention of menstrual porphyria – Functional ovarian cysts
Combined Oral Contraceptives (Estrogen & Progestin) Advantages: – Less endometrial cancer (50% reduction) – Less ovarian cancer (40% reduction) – Less benign breast disease – Fewer ovarian cysts (50% to 80% reduction) – Fewer uterine fibroids (31% reduction) – Fewer ectopic pregnancies – Fewer menstrual problems – – --more regular --less flow --less dysmenorrhea --less anemia Less salpingitis (pelvic inflammatory disease) Less rheumatoid arthritis (60% reduction) Increased bone density Probably less endometriosis
Combined Oral Contraceptives (Estrogen & Progestin) Disadvantages § Spotting especially in 1 st few months § May decrese Libido § Requires daily pill intake § No protection against STD’s and HIV § Possible weight gain § Post-contraception amenorrhea
Combined Oral Contraceptives (Estrogen & Progestin) l Absolute Contraindications: – Thromboembolic disorder (or history thereof) – Cerebrovascular accident (or history thereof) – Coronary artery disease (or history thereof) – Impaired liver function (current) – Hepatic adenoma (or history thereof) – Breast cancer, endometrial cancer, other estrogen-dependant malignancies – Pregnancy – Undiagnosed vaginal bleeding – Tobacco user over age 35
Combined Oral Contraceptives (Estrogen & Progestin) l Relative Contraindications – Migraine headaches, esp. worsening with pill use – Hypertension – Diabetes mellitus – Elective surgery (needs 1 to 3 month discontinuation) – Seizure disorder, anticonvulsant use – Sickle cell disease (SS or sickle C disease (SC) – Gall bladder disease.
Choosing The Right OCP’s l Endometriosis: Choose a pill with a strong progestin to create a pseudo-pregnancy state l Functional Ovarian Cysts: High dose monophasic pill may be more effective l Androgen excess: Choose a pill with high estrogen/progestin ratio to reduce free testosterone and inhibit 5 a reductase activity l Breastfeeding: Progestin -only pill
Transdermal: Ortho Evra l Delivers 20 mcg of ethinyl estradiol and 150 mcg of norelgestromin daily l Takes 3 days to achieve a steady state of hormone in the blood stream l Patch is replaced once per week for 3 consecutive weeks l Worn on abdomen, buttocks, upper outer arm, or upper torso l Do not place on the breast
Transdermal: Ortho Evra l Advantages: – Only has to be replaced once per week – May be taken continuously l Disadvantages: – May slip off- provide pt. with an emergency patch – Patch may be less effective in women who are > 198 pounds

Vaginal Contraceptive Ring: Nuva. Ring l Combined hormonal contraception consisting of a 5. 4 cm diameter flexible ring l 15 mcg ethinyl estradiol and 120 mcg of desogestrel l Mechanism: suppresses ovulation l Typical use failure rate: 8%

Vaginal Contraceptive Ring: Nuva. Ring l Place in vagina and remove after 3 weeks l Allow withdrawal bleeding and replace new ring l Steady low release state l Advantage is patient only has to remember to insert and remove the ring 1 x/ month l May be placed anywhere in the vagina

Depo Provera l 150 mg IM every 3 months l Contraceptive level maintained for 14 weeks l Failure Rate: 3% typical use failure rate l Mechanism: – Thickens cervical mucus – Blocks the LH surge – Initiate treatment during the first week of menses
Depo Provera l Advantages – Long acting l Disadvantages – Irregular bleeding (70% in first year) – Estrogen-free – Breast tenderness – Safe in breast-feeding – Weight gain – Can be used in sickle-cell disease and seizure disorder – Pt. does not have to take daily – Depression – Slow return of menses after stopping use – Increases milk quality in nursing mothers – Decreases HDL cholesterol
Female Sterilization l Interrupts the patency of fallopian tubesthereby preventing fertilization l Failure rate: Depends on method used -ranges from 0. 8 -3. 7% l May be performed through a mini-laparotomy incision , laparoscopically, or transcervically
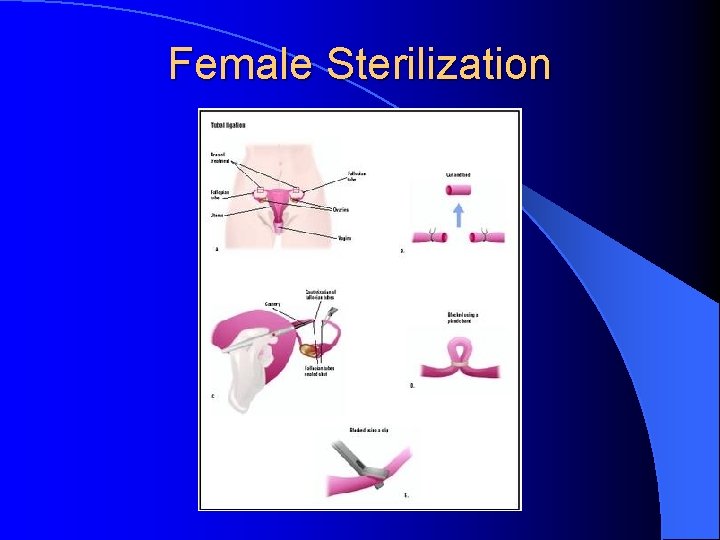
Female Sterilization
Male Sterilization
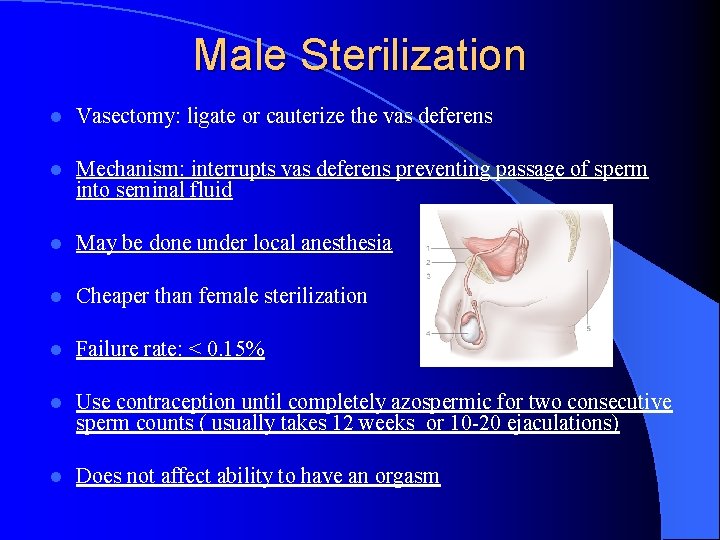
Male Sterilization l Vasectomy: ligate or cauterize the vas deferens l Mechanism: interrupts vas deferens preventing passage of sperm into seminal fluid l May be done under local anesthesia l Cheaper than female sterilization l Failure rate: < 0. 15% l Use contraception until completely azospermic for two consecutive sperm counts ( usually takes 12 weeks or 10 -20 ejaculations) l Does not affect ability to have an orgasm
- Slides: 45