Contraception in Adolescents Karen Soren MD Director Adolescent

- Slides: 35
Contraception in Adolescents Karen Soren, MD Director, Adolescent Medicine Associate Clinical Professor Pediatrics & Public Health Columbia University Medical Center
What are the barriers to teens using contraception? • Developmental issues: – Early adolescence: present oriented, impulsive – Middle adolescence: omnipotent, invincible • Teens are spontaneous • Teens may be ambivalent about pregnancy • Teens have inadequate access to information and confidential care; lack of awareness of NYS rights
The conversation: • AAP recommends postponement of sexual activity, especially for young teens • “But -if you are going to be sexually active, you need protection!” • Condoms are the best method for protection against sexually transmitted • Condoms are an imperfect method for pregnancy –prevention • You need a back-up for your condom…
The contraceptive visit : What do you need to do? • Reassure adolescents of confidentiality • History – PMH- rule out conditions that would not allow safe use of estrogen-containing methods – Sexual history – History of previous contraceptive use – Current medications • Physical (very basic!) – Weight, BP – Gyn exam NOT required
How Methods are Chosen • • • Use by friends or relatives Accessibility Personal knowledge Media Fear of side effects Physician recommendation
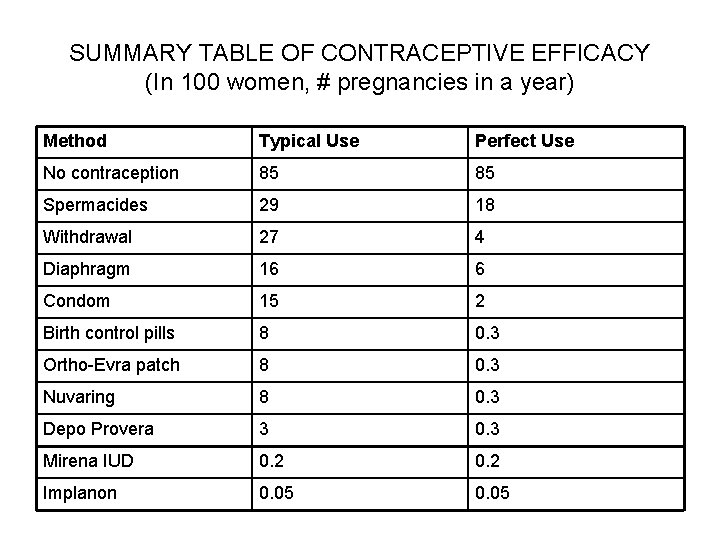
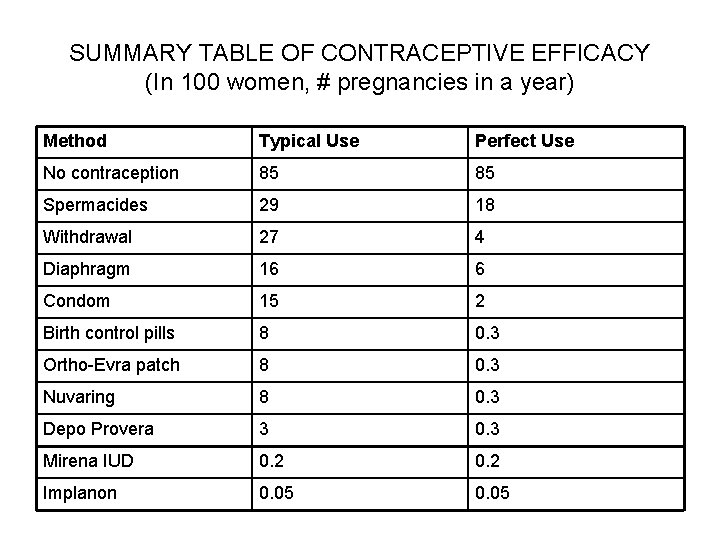
SUMMARY TABLE OF CONTRACEPTIVE EFFICACY (In 100 women, # pregnancies in a year) Method Typical Use Perfect Use No contraception 85 85 Spermacides 29 18 Withdrawal 27 4 Diaphragm 16 6 Condom 15 2 Birth control pills 8 0. 3 Ortho-Evra patch 8 0. 3 Nuvaring 8 0. 3 Depo Provera 3 0. 3 Mirena IUD 0. 2 Implanon 0. 05
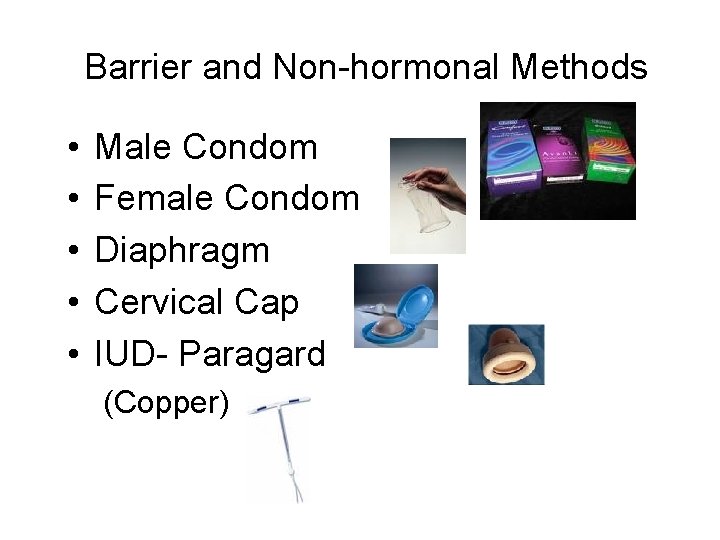
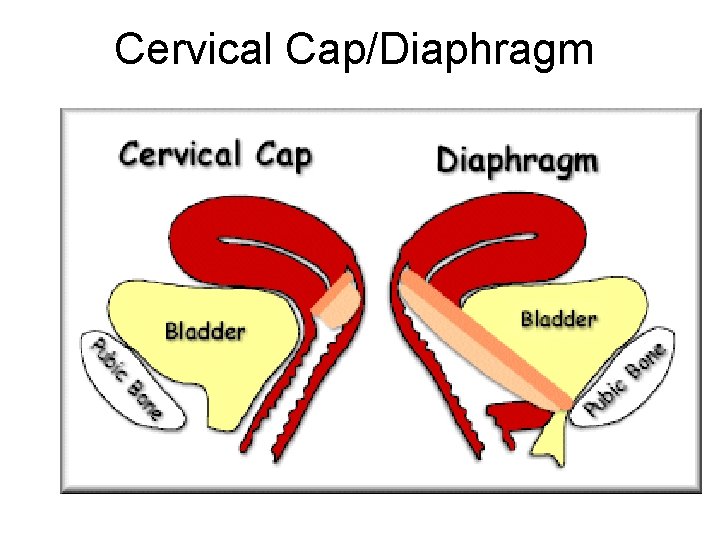
Barrier and Non-hormonal Methods • • • Male Condom Female Condom Diaphragm Cervical Cap IUD- Paragard (Copper)
Male Condom • STI protection • Over the counter • Imperfect method of contraception – 85% effective • Possible latex allergy (my need to use polyurethane condoms) • Many condoms now lubricated but do not contain spermicide - issues with nonoxynol nine – mucosal irritant • Need a back-up method…

Plan B • Large dose of levonorgestral • Best taken as soon as possible after unprotected intercourse • Can take up to 5 days after mess-up (package says 72 hours) • Now Plan B One-Step – single pill • 75 -85% effective in reducing pregnancy if used within 72 hours, less so if used later • No serious side effects • Over the counter now - >17 yo
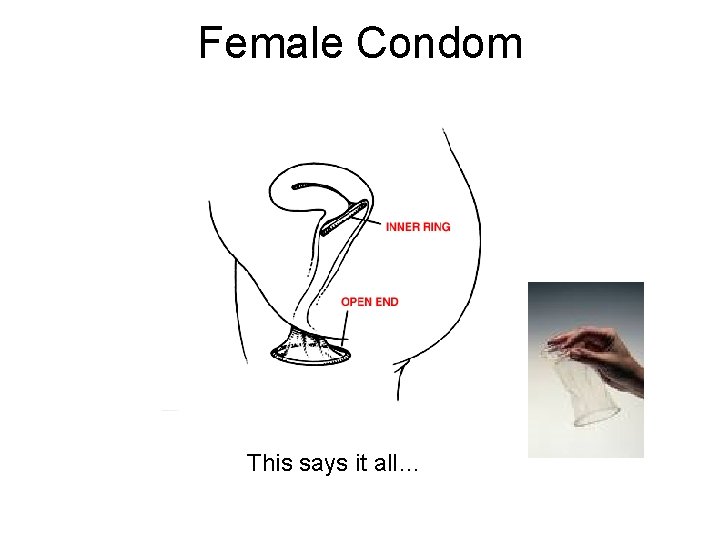
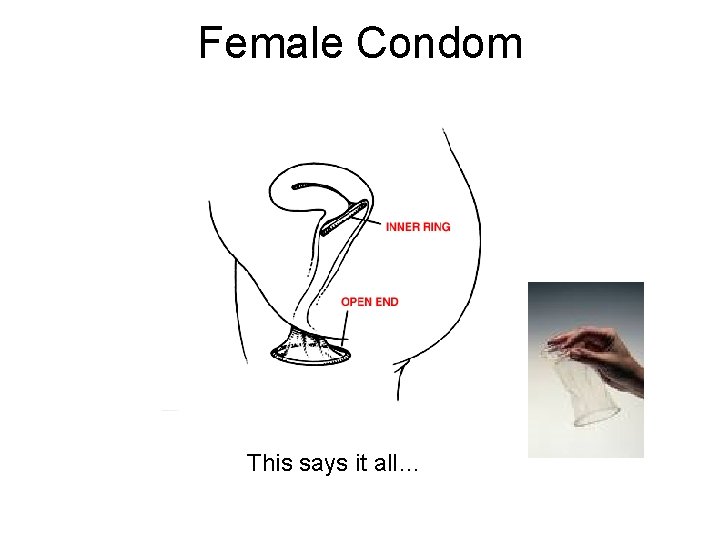
Female Condom This says it all…
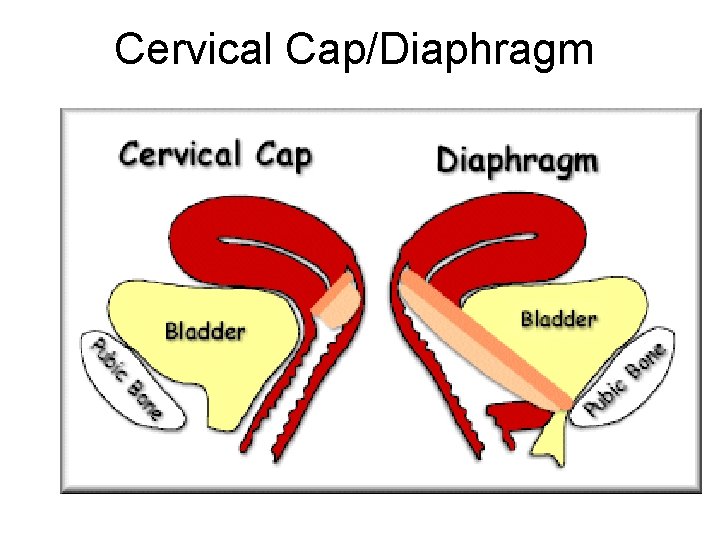
Cervical Cap/Diaphragm
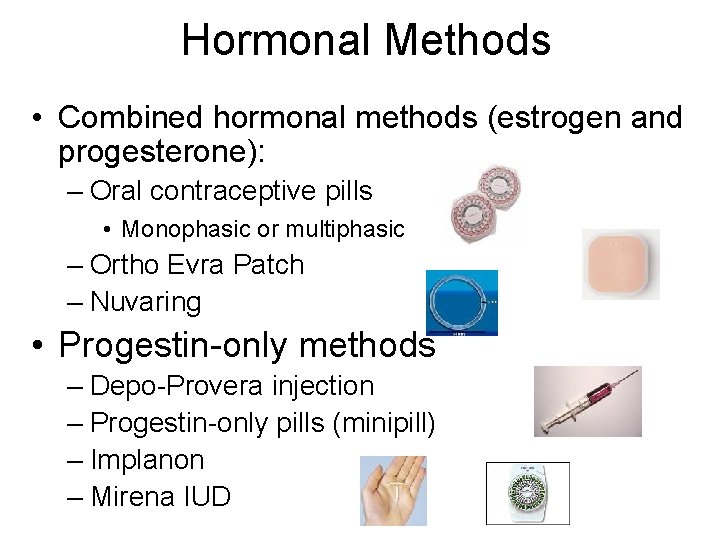
Hormonal Methods • Combined hormonal methods (estrogen and progesterone): – Oral contraceptive pills • Monophasic or multiphasic – Ortho Evra Patch – Nuvaring • Progestin-only methods – Depo-Provera injection – Progestin-only pills (minipill) – Implanon – Mirena IUD
A little about estrogens… • Older pill (1960’s) started with 150 mcg mestranol – eventually decreased to 50 mcg because of side effects • Ethinyl estradiol introduced in 1970’s • Dose varies from 50 mcg to 20 mcg, but most pills now used are between 20 and 30 mcg • Lower dose → less side effects, but more break- through bleeding, and less room for noncompliance
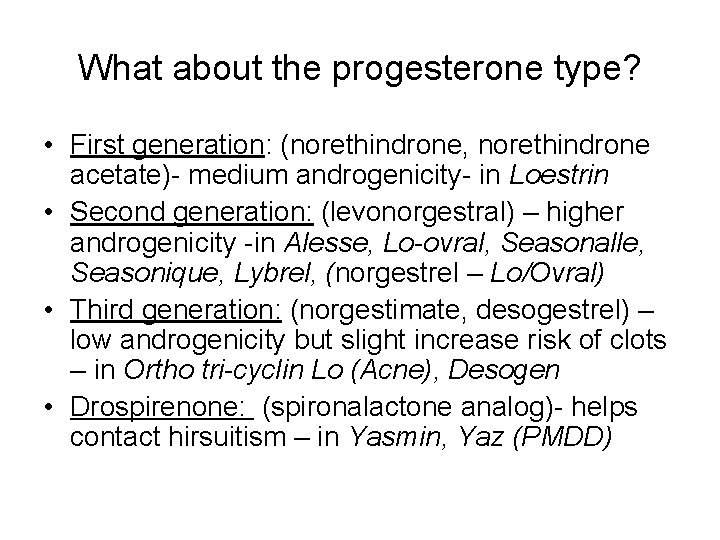
What about the progesterone type? • First generation: (norethindrone, norethindrone acetate)- medium androgenicity- in Loestrin • Second generation: (levonorgestral) – higher androgenicity -in Alesse, Lo-ovral, Seasonalle, Seasonique, Lybrel, (norgestrel – Lo/Ovral) • Third generation: (norgestimate, desogestrel) – low androgenicity but slight increase risk of clots – in Ortho tri-cyclin Lo (Acne), Desogen • Drospirenone: (spironalactone analog)- helps contact hirsuitism – in Yasmin, Yaz (PMDD)
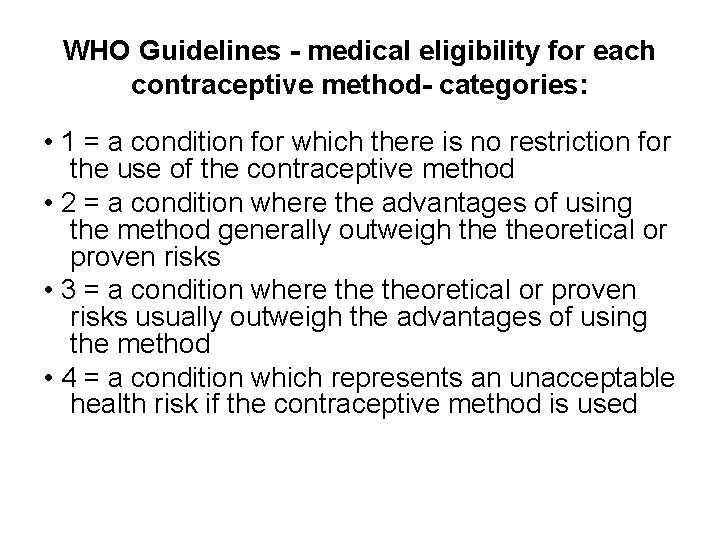
WHO Guidelines - medical eligibility for each contraceptive method- categories: • 1 = a condition for which there is no restriction for the use of the contraceptive method • 2 = a condition where the advantages of using the method generally outweigh theoretical or proven risks • 3 = a condition where theoretical or proven risks usually outweigh the advantages of using the method • 4 = a condition which represents an unacceptable health risk if the contraceptive method is used
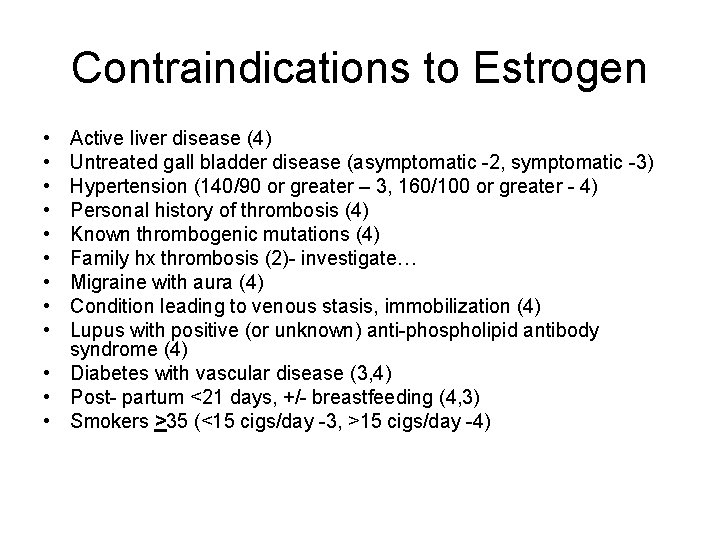
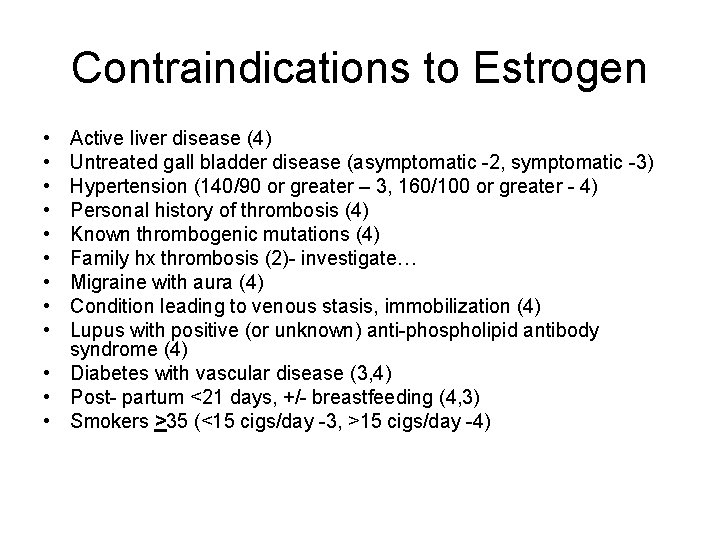
Contraindications to Estrogen • • • Active liver disease (4) Untreated gall bladder disease (asymptomatic -2, symptomatic -3) Hypertension (140/90 or greater – 3, 160/100 or greater - 4) Personal history of thrombosis (4) Known thrombogenic mutations (4) Family hx thrombosis (2)- investigate… Migraine with aura (4) Condition leading to venous stasis, immobilization (4) Lupus with positive (or unknown) anti-phospholipid antibody syndrome (4) • Diabetes with vascular disease (3, 4) • Post- partum <21 days, +/- breastfeeding (4, 3) • Smokers >35 (<15 cigs/day -3, >15 cigs/day -4)
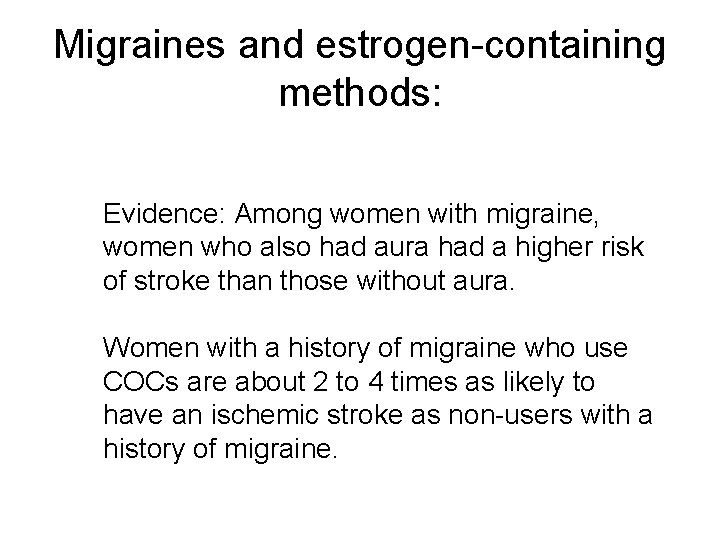
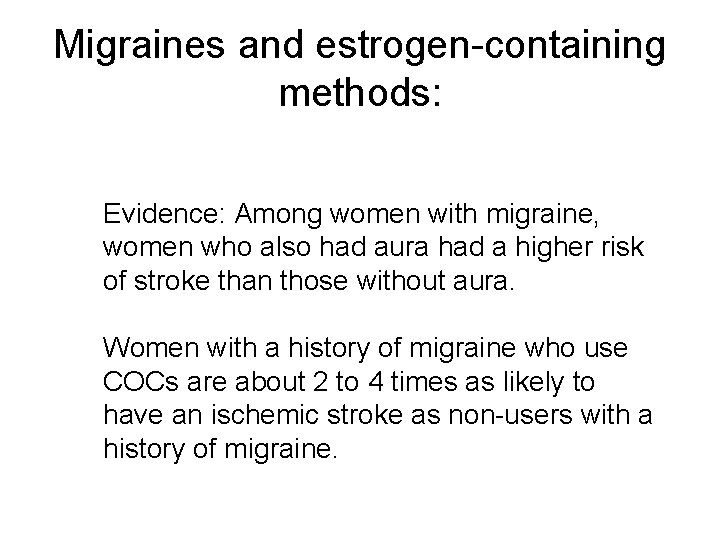
Migraines and estrogen-containing methods: Evidence: Among women with migraine, women who also had aura had a higher risk of stroke than those without aura. Women with a history of migraine who use COCs are about 2 to 4 times as likely to have an ischemic stroke as non-users with a history of migraine.
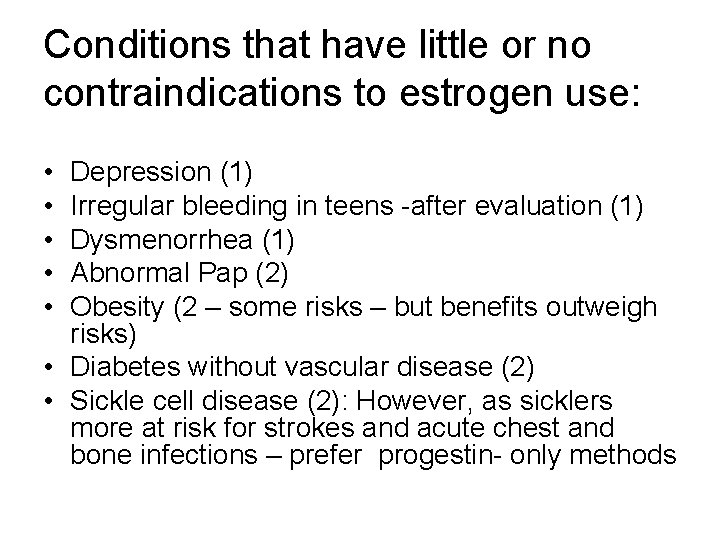
Conditions that have little or no contraindications to estrogen use: • • • Depression (1) Irregular bleeding in teens -after evaluation (1) Dysmenorrhea (1) Abnormal Pap (2) Obesity (2 – some risks – but benefits outweigh risks) • Diabetes without vascular disease (2) • Sickle cell disease (2): However, as sicklers more at risk for strokes and acute chest and bone infections – prefer progestin- only methods
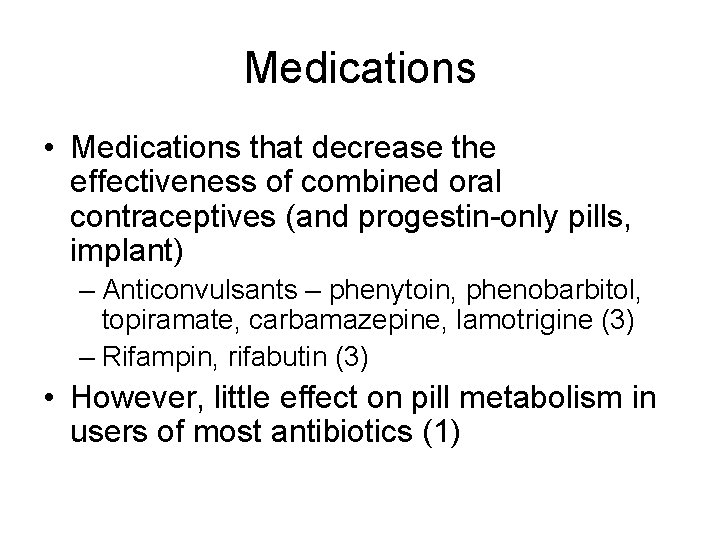
Medications • Medications that decrease the effectiveness of combined oral contraceptives (and progestin-only pills, implant) – Anticonvulsants – phenytoin, phenobarbitol, topiramate, carbamazepine, lamotrigine (3) – Rifampin, rifabutin (3) • However, little effect on pill metabolism in users of most antibiotics (1)
Combined OCP’s • Mechanism of action – Progesterone inhibits LH, thickens cervical mucus, atrophies endometrium – Estrogen inhibits FSH • Other actions of BCPs – Increase SHBG and decrease free testosterone – Inhibit 5 - reductase in skin, decreasing conversion of testosterone to DHT
Combined OCP’s • PROS – – Rapid return to fertility No anticipation Menstrual regularity Decrease dysmenorrhea and anemia – Decrease ectopic pregnancy rate – Decrease PID – Decrease ovarian and endometrial cancer • CONS – – Daily medication Regular supply needed Multiple SEs Multiple contraindications – CLOTS
Combined OCP Side Effects • PROGESTERONE • ESTROGEN – Increases appetite – Nausea – Depression – Fluid retention – Elevated lipids (TG) – Breast tenderness – Increases clotting by decreasing protein C, S, antithrombin III – HTN
How to prescribe OCP’s • Become familiar with a few types of pills • Rule out contraindications to estrogen • Patient can start any day (but some prefer Sundays or first day of period) • Can give up to 6 packs at a time • Bring back after 3 -4 weeks to determine: – If teen started pill and if it is taken correctly – Any side effects
So what pill do I prescribe? • Can start with a low-dose pill (Alesse, Loestrin 1/20) • If teen has acne or PCOS-type stigmata, consider Ortho tri-cyclin Lo • If teen has hirsuitism / PCOS, can use Yaz or Yasmin instead • For dysfunctional uterine bleeding, can use Lo/Ovral – longer half-life of progestin- stabilizes endometrium
Ortho Evra Patch • Norelgestromin 6 mg/ ethinyl estradiol 0. 75 mg in a transdermal delivery system • 1 patch weekly for 3 weeks, then patch -free for 1 week • Traditionally, Sunday or first day of menses start- however, can start anytime • Menses usually 4 days after patch removal
Ortho Evra • • PROS – No need for daily med – Teens like ease of usage CONS – 2 -3% detach – Nausea/ vomiting – Less effective if >90 kg – More complicated if forget to change or falls off – Breast pain, rash – CLOTS: 60% more estrogen than a 35 mcg pill (FDA alert)
Nuva. Ring • Etonogestrel 120 mcg/d + ethinyl estradiol 15 mcg/d • Silastic ring inserted intravaginally for 3 weeks with 1 week off • Less estrogen because more bioavailable • Does not need to be put around cervix, just in vaginal vault adjacent to mucosa
Nuva. Ring • PROS – Less estrogen (15 mcg equivalent) – Protects for a full cycle • CONS – No STI protection – 18% of women, 30% of men feel ring – Most common SE is leukorrhea – Again - clots
Depo-Provera • Medroxyprogesterone acetate – 150 mg IM every 11 -13 weeks (up to 14 weeks) • Progesterone actions – – Suppresses LH and prevents ovulation Thickens cervical mucus Atrophies endometrium Decreases cilia motility in fallopian tubes • 50% amenorrheic at 1 year
Depo-Provera, cont • CONS • PROS – SE can’t be – Highly effective immediately stopped – No anticipation – Delay in return to – Can breast feed fertility – Decrease endometrial – Irregular bleeding and ca, yeast infection, amenorrhea PID, fibroids – Hypo-estrogenic state – Increases seizure OSTEOPOROSIS threshold
Depo-Provera, side effects • • • Headache Mood swings Weight gain Hair Loss Irregular bleeding One third discontinue use after one year as a result of side effects
POPs • Progestin-only pills (Micronor, Nor-QD) • Small dose of progestin – works primarily by increasing viscosity of cervical mucus • Does not reliably inhibit ovulation • Need to be taken carefully and consistently – if more than 3 hours late with pill, will not be effective • Useful for teens with contraindications to estrogen who will not accept Depo or Mirena
Implanon • Contains 68 mg etonogestrel • Single rod implanted subdermally on day 1 -5 of cycle • Last for 3 years. • Works by thickening cervical mucus and also inhibits ovulation • No effects on bones or lipids • Irregular bleeding common side effect
Mirena – progestin containing IUD • • IUD containing levonorgestral Helpful for menorrhagia and dysmenorrhea Effective for 5 years Previously discouraged in teens because teens more at risk for infection- liability concerns • Movement to encourage IUD use in teens currently • Infection probably most related to insertion • Can be inserted in nulliparous young woman- slight risk that will be expelled – teens should check for the string
So- what contraceptive method would you recommend? • 18 year old with no significant medical or family history going off to college • 14 year old coming in after an abortion – does not want her mother to know she is sexually active • Obese 17 year old with acne and irregular periods • 15 year old with heavy bleeding for a month who comes to the emergency room and has a hemoglobin of 8 • Amenorrheic 16 year old with facial hair • 17 year old tampon user who cannot remember to take a pill, and wants to keep her sexual activity from her mother • 15 year old with migraines, and some preceding blurry vision • 18 year old with lupus who is non-compliant with her medications