Continuous Veno Venous Haemofiltration CVVH Handy Hints for

- Slides: 29
Continuous Veno- Venous Haemofiltration (CVVH) Handy Hints for Registrars
Indications for CVVH Ø Children in ARF, tumourlysis syndrome, in born errors of metabolism Ø Main one on PICU is pre renal failure Ø When conservative management is no longer effective Ø Children with haemodynamic instability Ø Severe electrolyte imbalance, hypervolaemia, symptomatic metabolic abnormalities
CVVH Ø A procedure whereby solutes are removed by convective transfer and the large ultra filtered volume is replaced by a balanced electrolyte solution
Why CVVH Ø The use of pumps has the advantage of predictably allowing fluid to be removed Ø Continuous treatment allows constant adjustment of therapy Ø Well tolerated by patients with haemodynamic instability Ø Allows nutrition to be optimised (enteral or TPN)
The Basics Ø Access • Vascath Ø Blood Ø Commencing CVVH Ø Housekeeping • Blood tests • Ordering blood • Prescription chart Ø Trouble Shooting
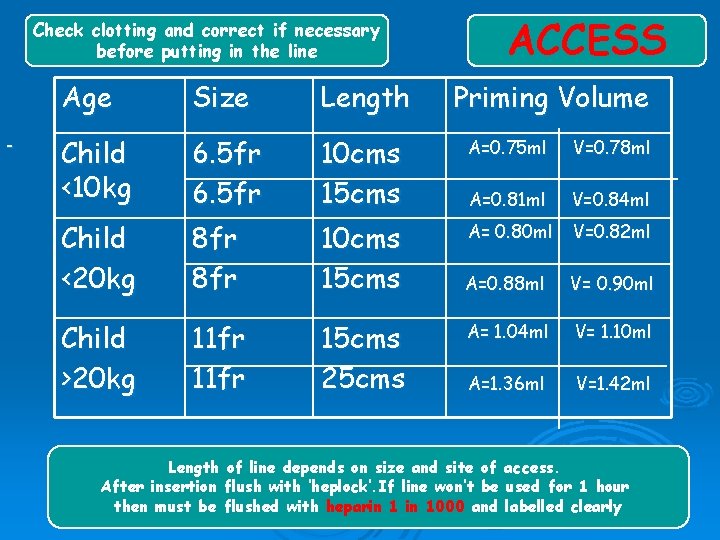
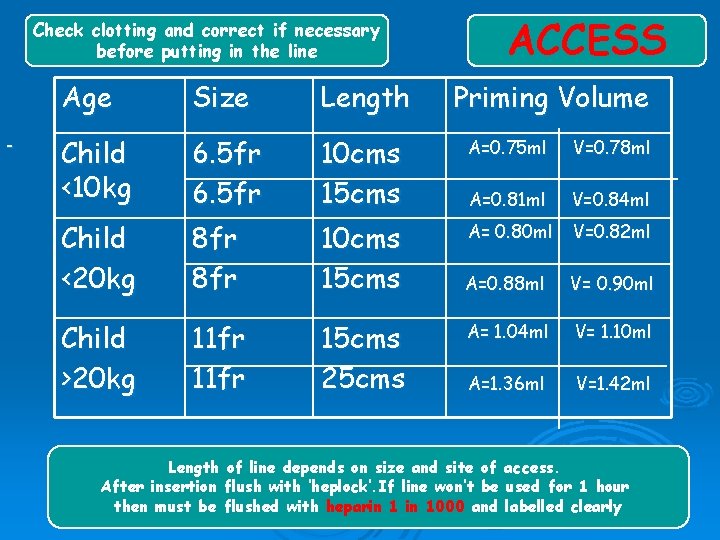
Check clotting and correct if necessary before putting in the line ACCESS Age Size Length Priming Volume Child <10 kg 6. 5 fr 10 cms 15 cms A=0. 75 ml V=0. 78 ml A=0. 81 ml V=0. 84 ml Child <20 kg 8 fr 10 cms 15 cms A= 0. 80 ml V=0. 82 ml A=0. 88 ml V= 0. 90 ml Child >20 kg 11 fr 15 cms 25 cms A= 1. 04 ml V= 1. 10 ml A=1. 36 ml V=1. 42 ml Length of line depends on size and site of access. After insertion flush with ‘heplock’. If line won’t be used for 1 hour then must be flushed with heparin 1000 and labelled clearly
Access Ø Ø Ø Vascath is line used at GOSH Insertion as for any other central line. Be aware of the priming volume. Treat as for any other central line Close observation of the site is essential. X ray to confirm placement of vascath: Sub-clavian Neck lines Neonates no neck line without discussion with consultant
Prior to going on Check routine bloods have been sent to have a baseline Ø Make sure a cross match has been sent especially if child <10 kgs Ø You should request an ADULT unit of blood – pedi pack is not enough volume Ø Blood should available in blood bank Ø X ray to confirm placement of vascath Ø • Sub-clavian • Neck lines • Neonates no neck line without discussion with consultant

The Aquarius Platinum by Edwards Life Sciences
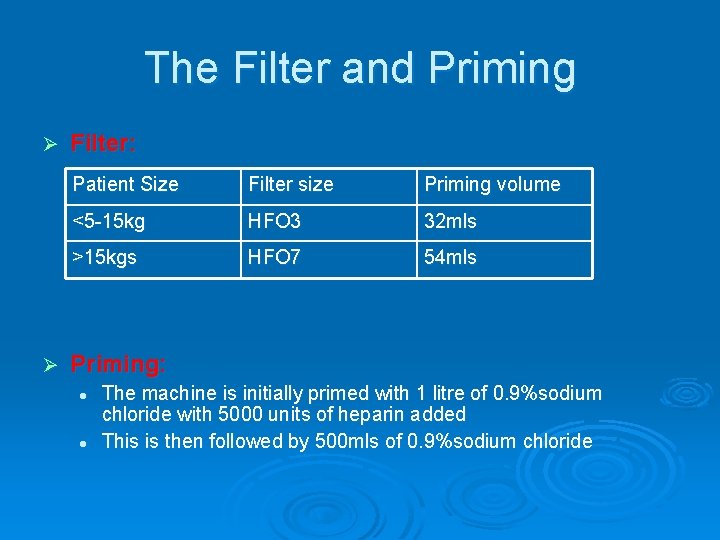
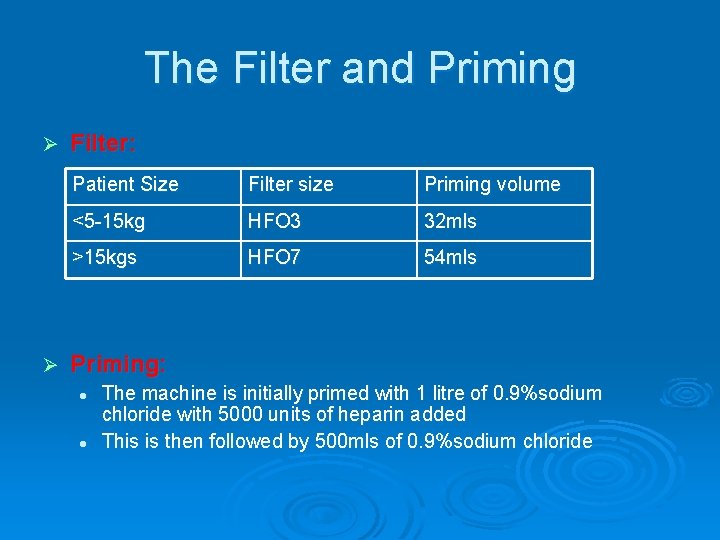
The Filter and Priming Ø Ø Filter: Patient Size Filter size Priming volume <5 -15 kg HFO 3 32 mls >15 kgs HFO 7 54 mls Priming: l l The machine is initially primed with 1 litre of 0. 9%sodium chloride with 5000 units of heparin added This is then followed by 500 mls of 0. 9%sodium chloride
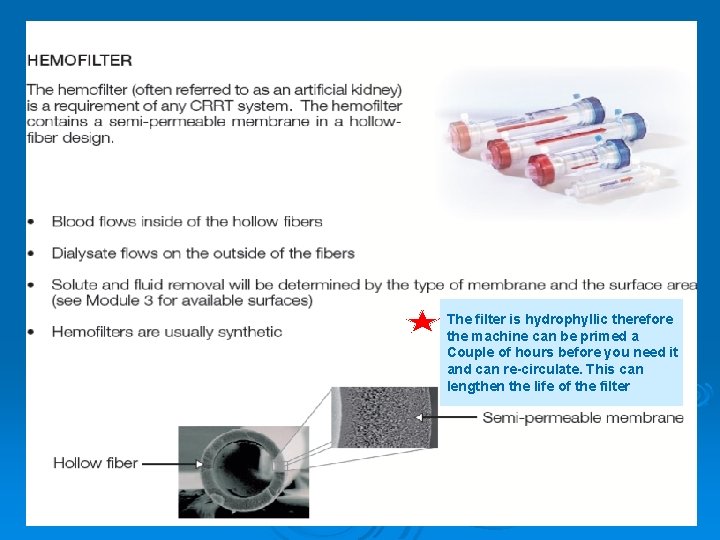
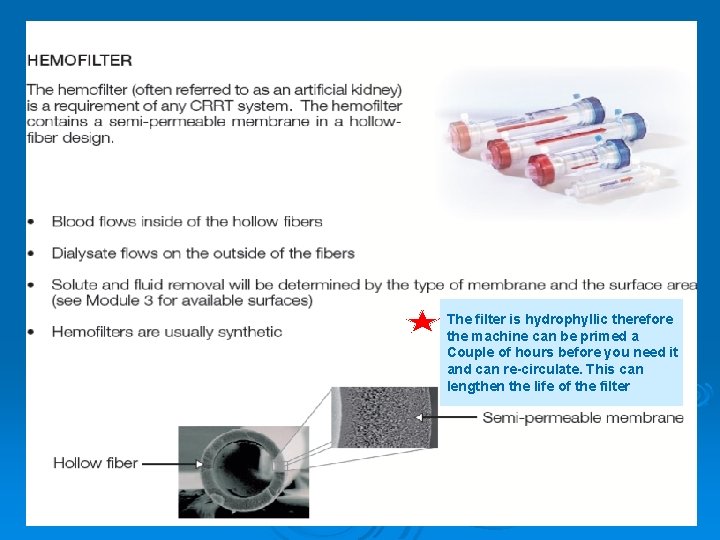
The filter is hydrophyllic therefore the machine can be primed a Couple of hours before you need it and can re-circulate. This can lengthen the life of the filter
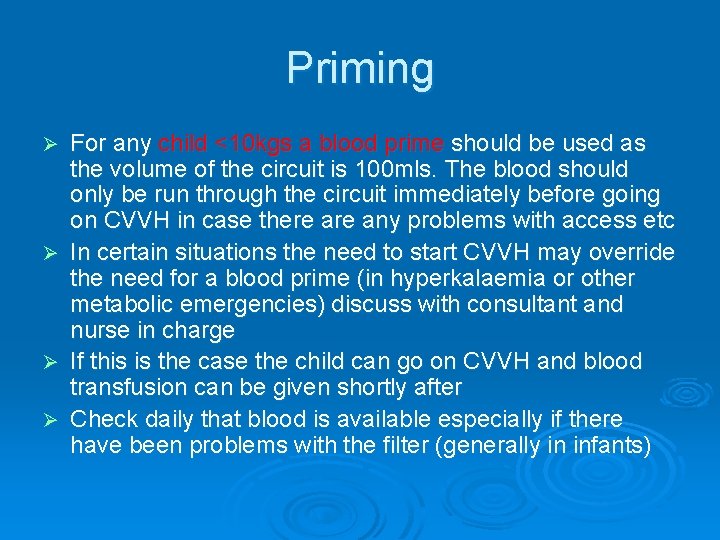
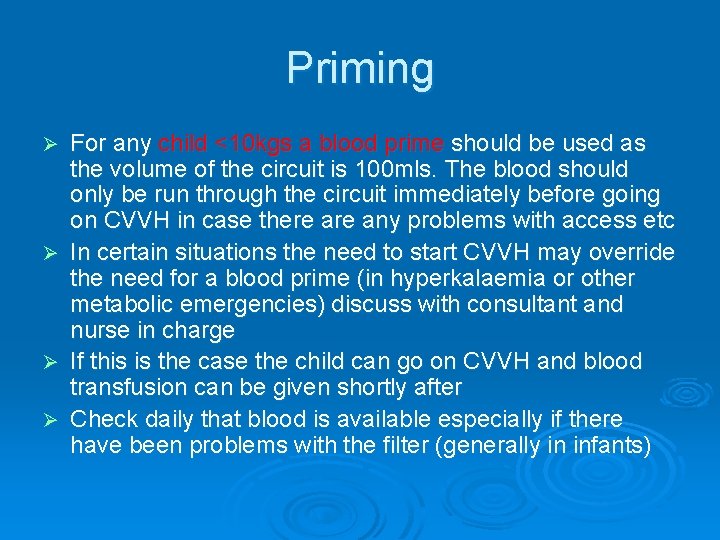
Priming For any child <10 kgs a blood prime should be used as the volume of the circuit is 100 mls. The blood should only be run through the circuit immediately before going on CVVH in case there any problems with access etc Ø In certain situations the need to start CVVH may override the need for a blood prime (in hyperkalaemia or other metabolic emergencies) discuss with consultant and nurse in charge Ø If this is the case the child can go on CVVH and blood transfusion can be given shortly after Ø Check daily that blood is available especially if there have been problems with the filter (generally in infants) Ø
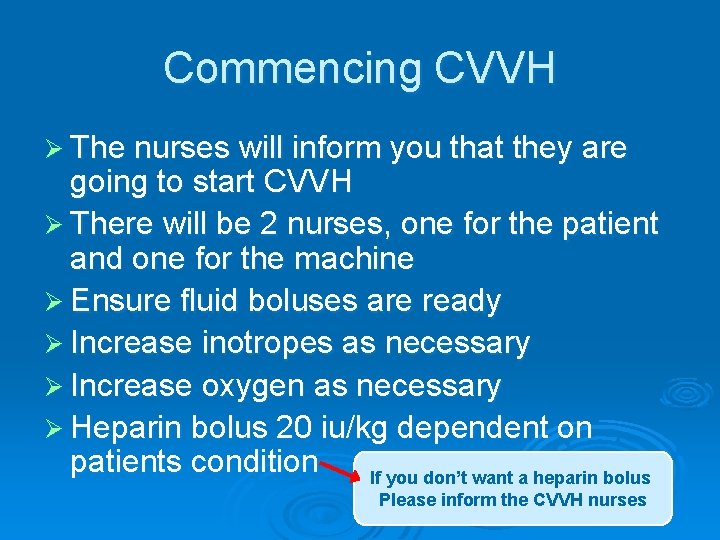
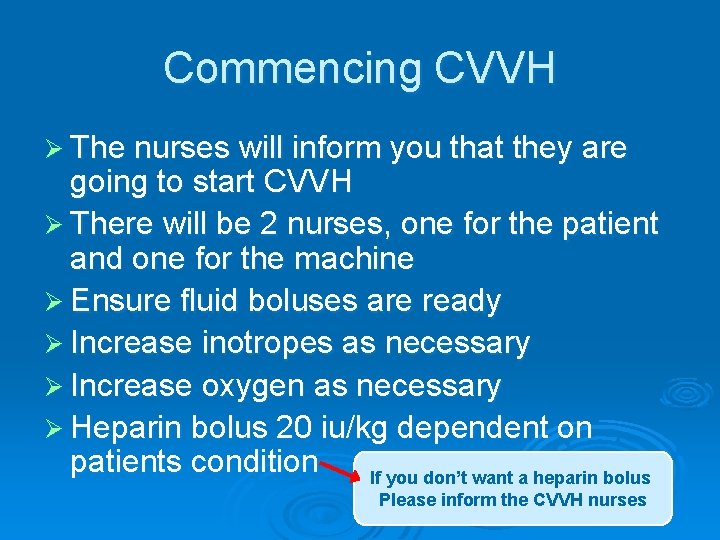
Commencing CVVH Ø The nurses will inform you that they are going to start CVVH Ø There will be 2 nurses, one for the patient and one for the machine Ø Ensure fluid boluses are ready Ø Increase inotropes as necessary Ø Increase oxygen as necessary Ø Heparin bolus 20 iu/kg dependent on patients condition If you don’t want a heparin bolus Please inform the CVVH nurses
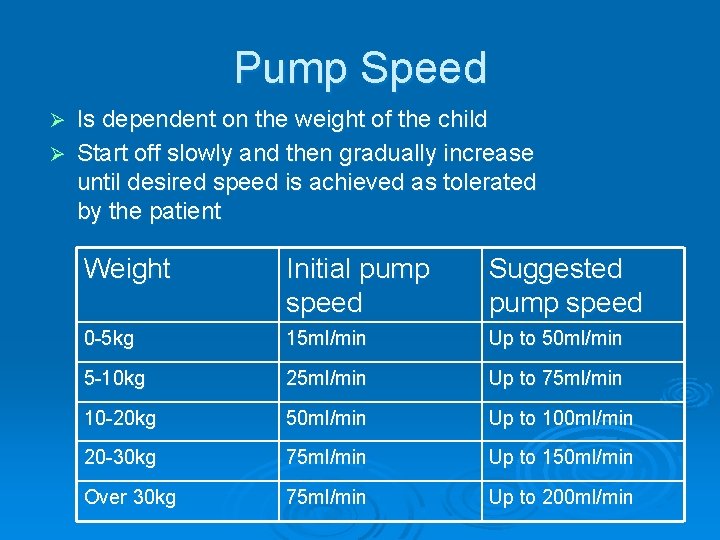
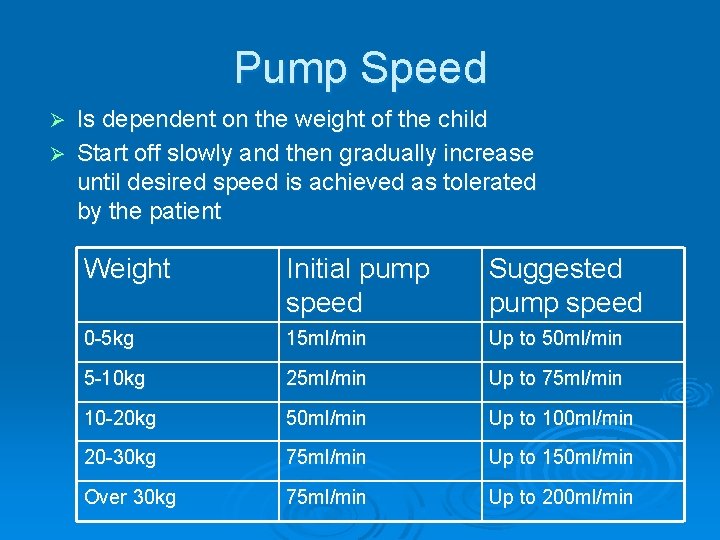
Pump Speed Is dependent on the weight of the child Ø Start off slowly and then gradually increase until desired speed is achieved as tolerated by the patient Ø Weight Initial pump speed Suggested pump speed 0 -5 kg 15 ml/min Up to 50 ml/min 5 -10 kg 25 ml/min Up to 75 ml/min 10 -20 kg 50 ml/min Up to 100 ml/min 20 -30 kg 75 ml/min Up to 150 ml/min Over 30 kg 75 ml/min Up to 200 ml/min
Ø Once satisfied the patient is tolerating the pump speed then the turnover and fluid loss programmes can be set and started
Pre-dilution or Filtration Fraction Ø Turnover is set usually between 5 -15% but in certain circumstances up to 30% can be used safely (tumourlysis syndrome, metabolic problems) Ø Represents the percentage of ultra filtration fluid that is removed from the blood passing through the filter every hour
Substitution /Replacement Fluid Primary function to remove solutes via convection Ø Is pre-filter, to lengthen the life of the circuit Ø One type used at GOSH. Can have extra potassium added if needed to a maximum of 5 mmols per litre l Accusol • For all patients • Suitable for patients with severe metabolic acidosis • For patients in liver failure • Bicarbonate based solution • Comes in plain bags and bags with added potassium Ø l Pre mixed: 2 mmols & 4 mmols per litre
Fluid Loss The programme is set on an hourly basis Ø The nurse will have calculated all the fluids (including, infusions IV antibiotics, and feeds or TPN going into the child) over a 24 hour period. Ø This is divided by 24 to get the hourly total Ø Decide with the consultant what fluid balance they would like to achieve in 24 hour period. (Andy Petros - 3 litres negative by the morning!) Ø Use of inotropes to maintain blood pressure in order to remove fluid – again discuss with consultant Ø
Fluid loss… Child has 360 mls of infusions, drugs and feed going in in 24 hours. Therefore every hour 15 mls is going in to the patient. For an even balance the machine would be set to take off 15 mls per hour Ø If we want the child negative 10 mls per hour then the machine would be set to take off 25 mls per hour Ø Other things to think about, if you are giving FFP, blood, etc to correct numbers then remember, that fluid can be taken off as it’s going in to prevent a positive fluid balance Ø
Setting the programme Ø Every cycle should be set for 4 hours • To allow for re calculation of fluids (if having FFP or other blood transfusions) • To prevent errors
Heparin Ø The circuit is heparinsed to prolong the life of the filter Ø Is delivered pre-filter Ø ACT’s are measured post filter Ø Aim to keep them 180 -200 unless patient is bleeding then 160 -180 Ø Or sometimes don’t use at all
Daily Housekeeping Check if the child needs any blood cross matching and ordering Ø Check the CVVH prescription chart Ø Check fluid balance Ø Check U&E’s Ø Check phosphate levels (Has an affinity to the filter) and commence infusion if necessary. Also if the filter is old and less effective the phosphate level could increase Ø Maximise the patient’s nutrition whether TPN or enteral Ø Did you know that the venous (return line) can be used for administration of TPN or other infusions if access is a problem
Check with Rachelle
Trouble shooting Ø Access • if the vascath is positional or one or both of the lumens are difficult to aspirate then it might need re-positioning Ø U&E’s not clearing as well • Check how old the filter is, if it has been going for a few days it may need to be electively changed • Could the filtration fraction be increased Ø Clotting • If the child is coagulapathic then heparin does not have to be used, although this could shorten the life of the filter • Have to balance between the risk of bleeding and the risk of loosing the filter. Especially in very small infants (<5 kgs as the pump speed is so slow)
roberc 1@gosh. nhs. uk
References Dykes M, Ameerally P (2002) Anatomy. 2 nd edition. Ø Guyton AC, Hall JE (2006) Textbook of Medical Physiology. 11 th edition. Ø Hazinski MF (1992) Nursing Care of the Critically Ill Child. 2 nd edition Ø http: //en. wikipedia. org/wiki/tumor_lysis_syndrom e Ø http: //www. purchon. com/biology/osmosis. htm Ø
3. 5 kg baby with metabolic condition ammonia at dangerously high level. • • What would the pump speed be? Would you do a blood prime? What would the filtration fraction be? What would you set the fluid loss, even negative, or positive?
20 kg child. Mo. F on multiple inotropes. ARDS 3 L +ve. Fluids 50 mls hour Ø What would the pump speed be Ø What filtration fraction would you set Ø How would you calculate the fluid loss
30 kg child. Tumourlysis Syndrome. Hb 7. 5. K+ 6. 3 Fluids 50 mls hour. Ø What would the pump speed be Ø What filtration fraction would you set? Ø Would you do a blood prime? Ø Would you set the child on an even, positive, or negative fluid balance?