Continuous renal replacement therapy R 4 CRRT Either

- Slides: 24

Continuous renal replacement therapy 신장내과 R 4 위지완
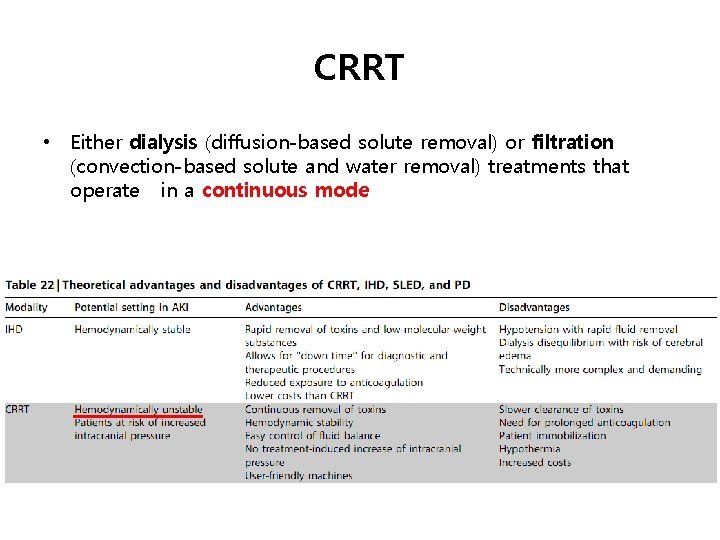
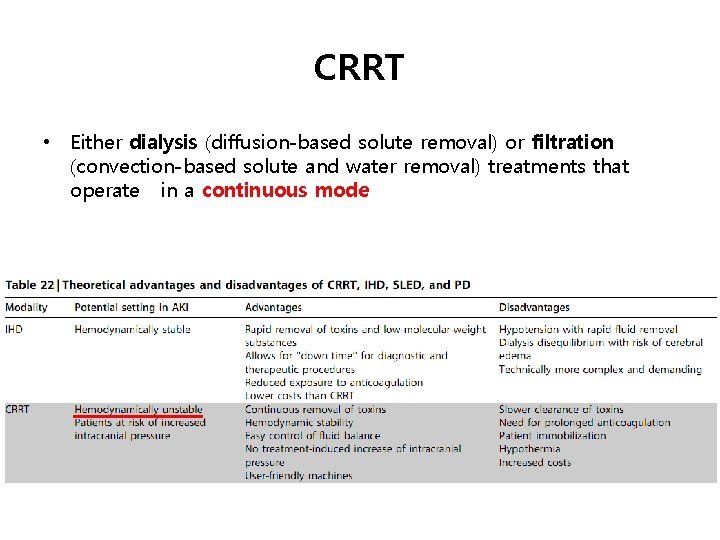
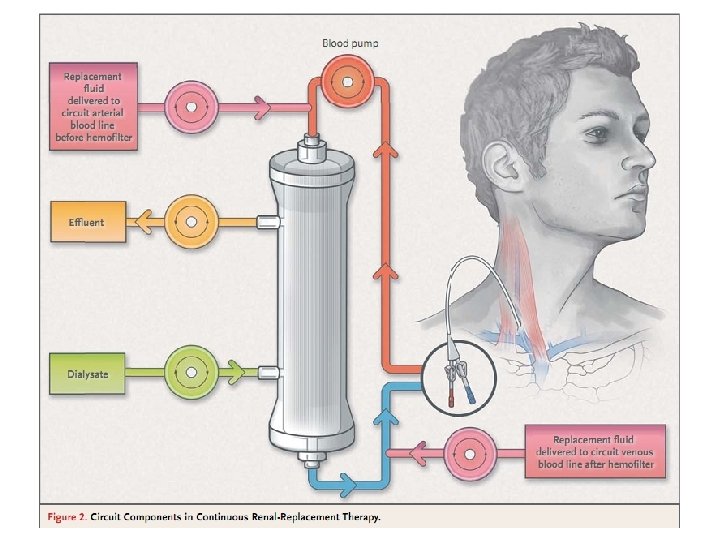
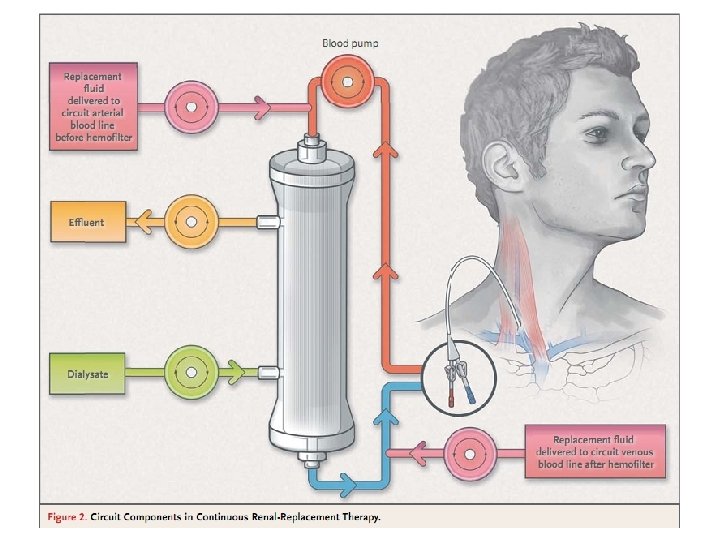
CRRT • Either dialysis (diffusion-based solute removal) or filtration (convection-based solute and water removal) treatments that operate in a continuous mode
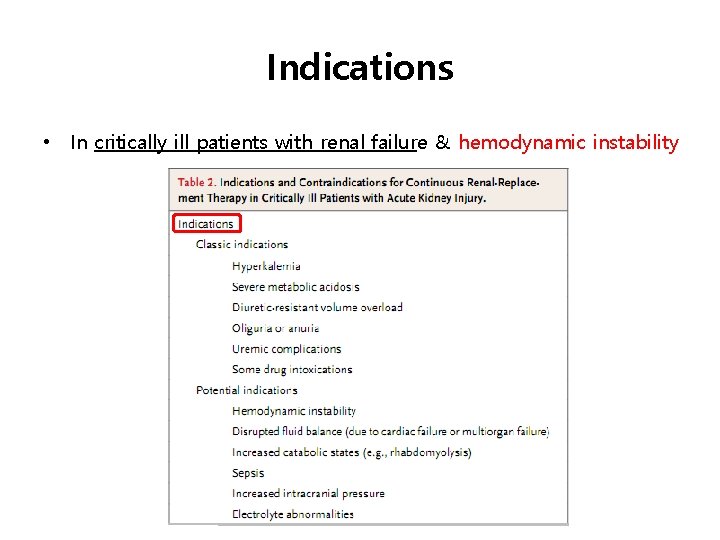
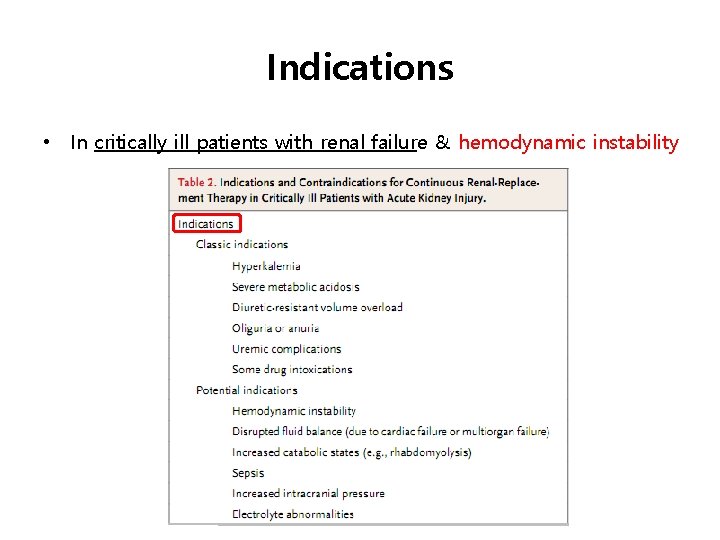
Indications • In critically ill patients with renal failure & hemodynamic instability
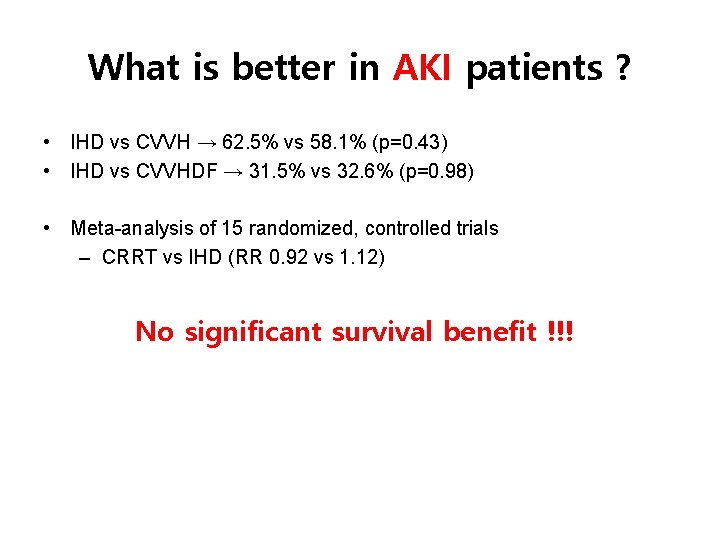
What is better in AKI patients ? • IHD vs CVVH → 62. 5% vs 58. 1% (p=0. 43) • IHD vs CVVHDF → 31. 5% vs 32. 6% (p=0. 98) • Meta-analysis of 15 randomized, controlled trials – CRRT vs IHD (RR 0. 92 vs 1. 12) No significant survival benefit !!!
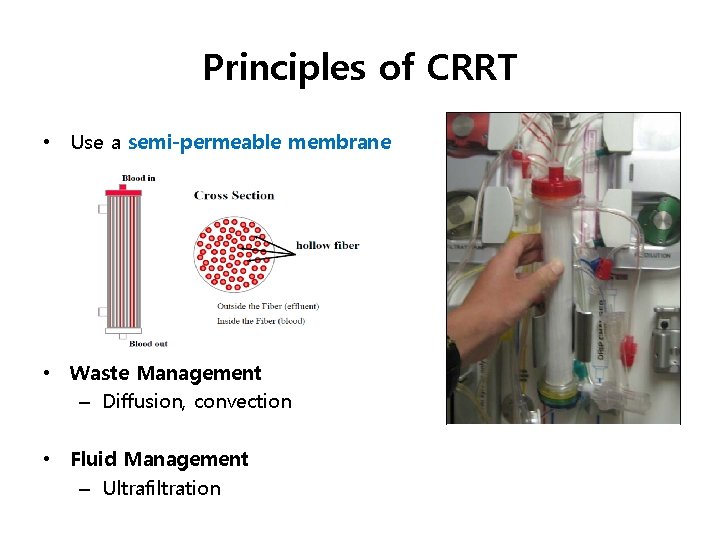
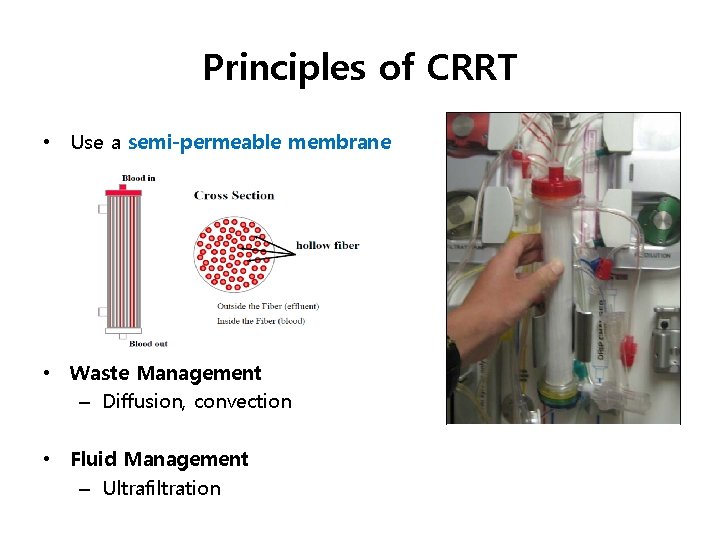
Principles of CRRT • Use a semi-permeable membrane • Waste Management – Diffusion, convection • Fluid Management – Ultrafiltration
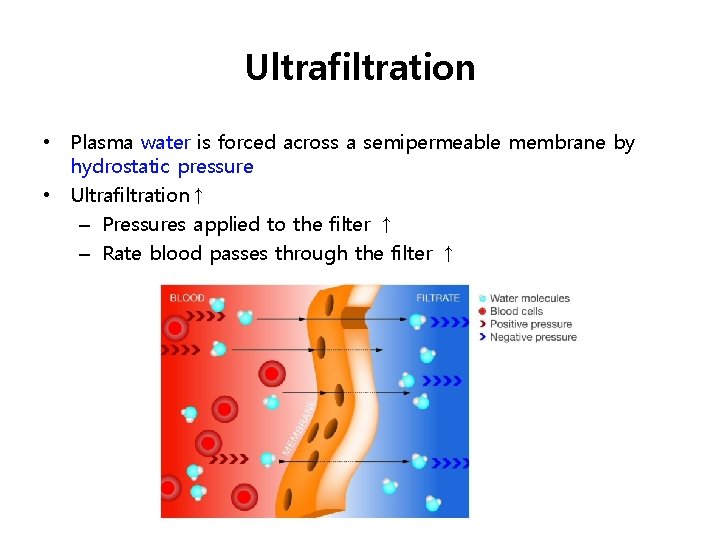
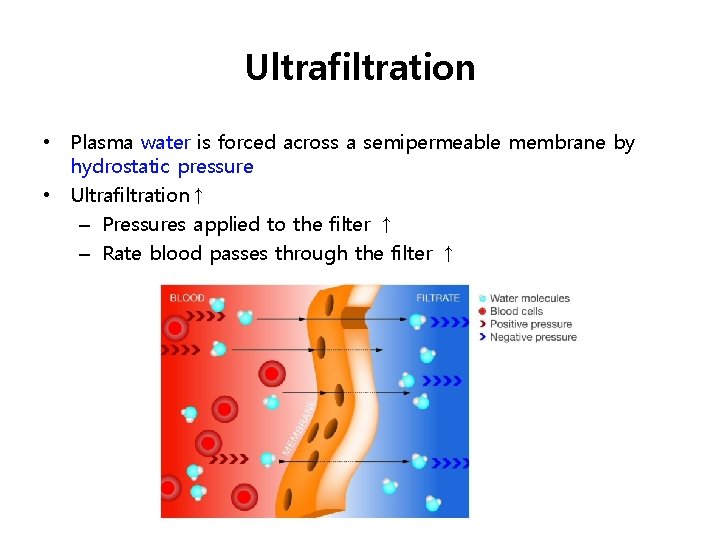
Ultrafiltration • Plasma water is forced across a semipermeable membrane by hydrostatic pressure • Ultrafiltration↑ – Pressures applied to the filter ↑ – Rate blood passes through the filter ↑
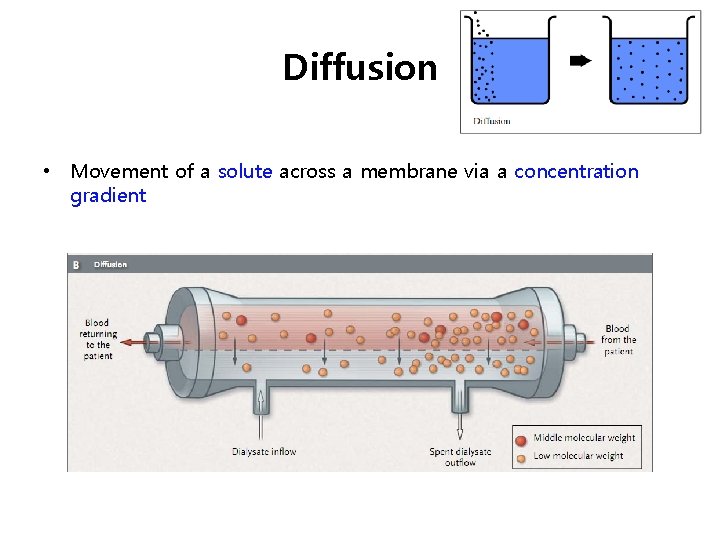
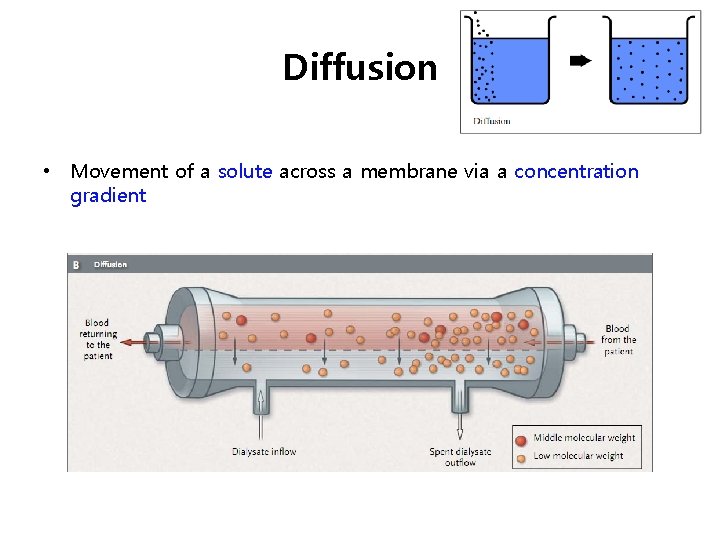
Diffusion • Movement of a solute across a membrane via a concentration gradient
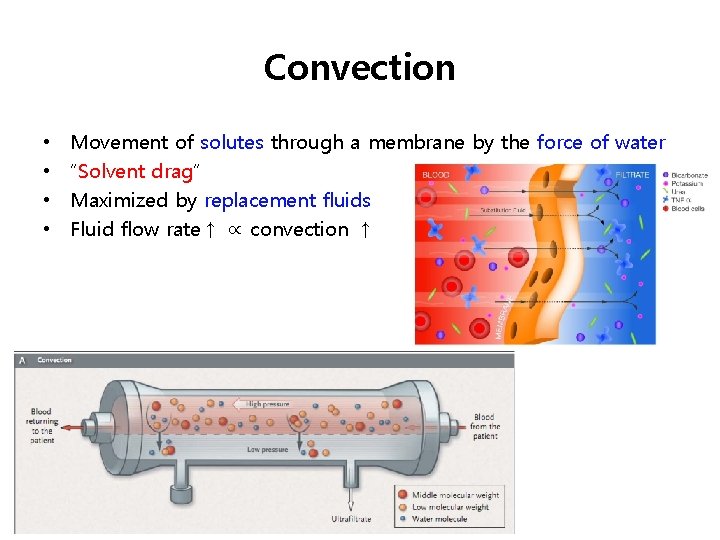
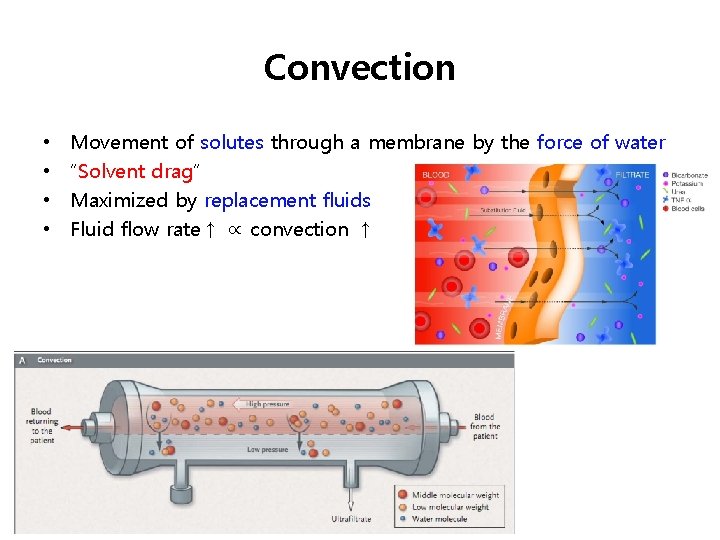
Convection • • Movement of solutes through a membrane by the force of water “Solvent drag” Maximized by replacement fluids Fluid flow rate↑ ∝ convection ↑
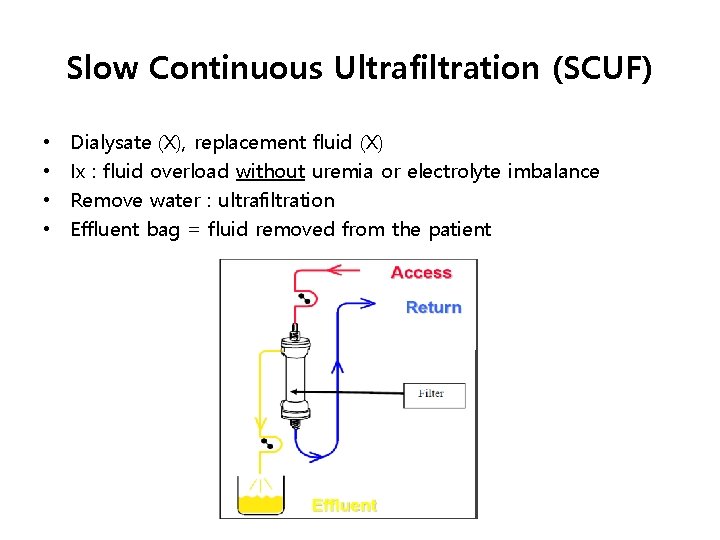
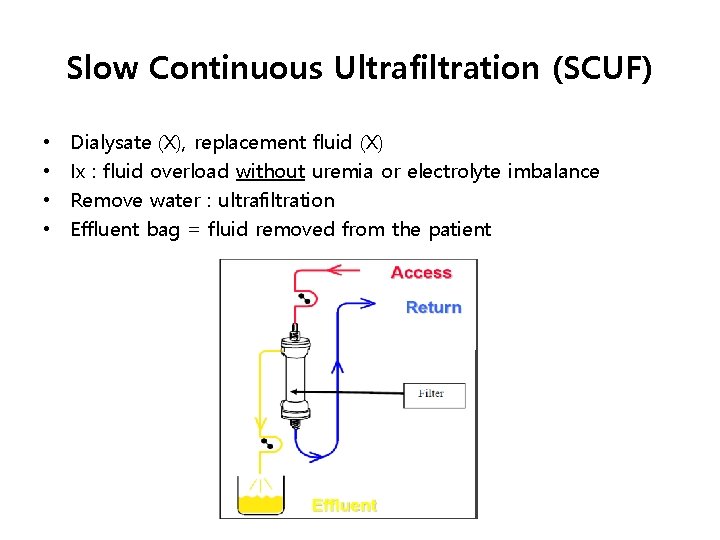
Slow Continuous Ultrafiltration (SCUF) • • Dialysate (X), replacement fluid (X) Ix : fluid overload without uremia or electrolyte imbalance Remove water : ultrafiltration Effluent bag = fluid removed from the patient
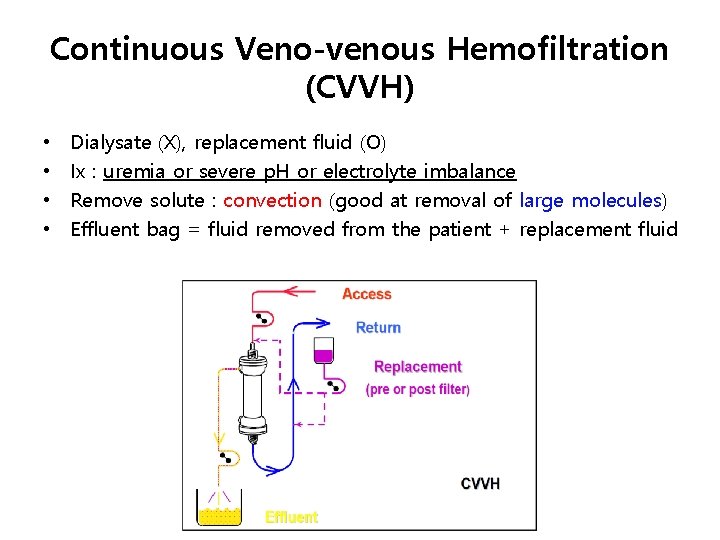
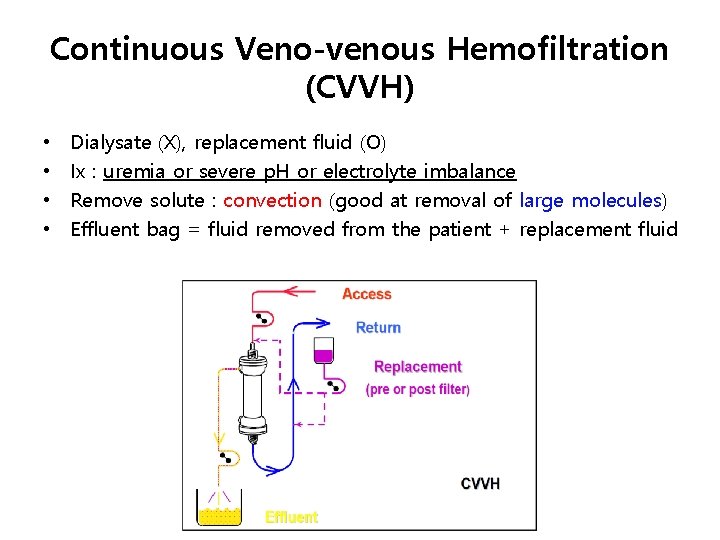
Continuous Veno-venous Hemofiltration (CVVH) • • Dialysate (X), replacement fluid (O) Ix : uremia or severe p. H or electrolyte imbalance Remove solute : convection (good at removal of large molecules) Effluent bag = fluid removed from the patient + replacement fluid
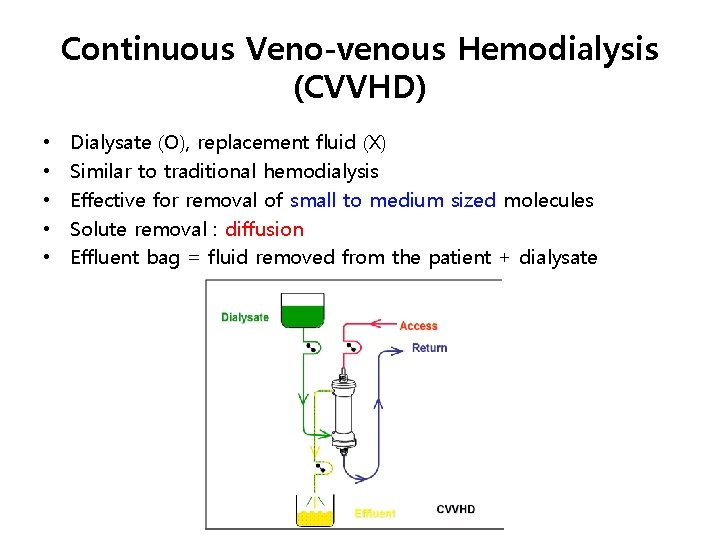
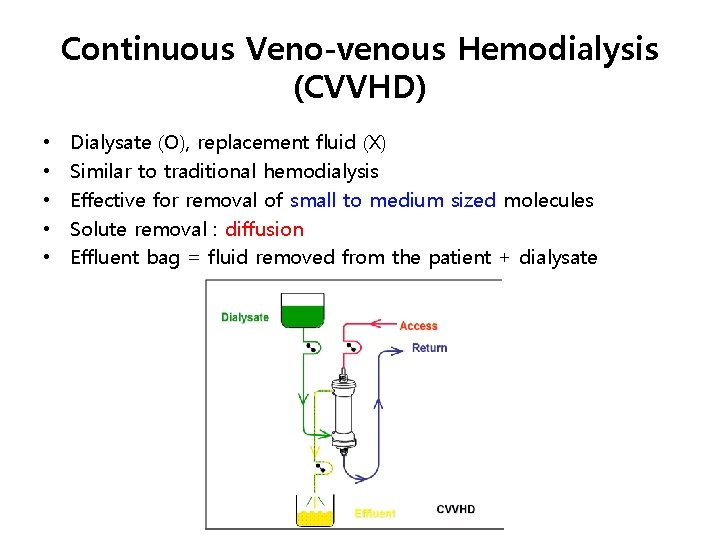
Continuous Veno-venous Hemodialysis (CVVHD) • • • Dialysate (O), replacement fluid (X) Similar to traditional hemodialysis Effective for removal of small to medium sized molecules Solute removal : diffusion Effluent bag = fluid removed from the patient + dialysate
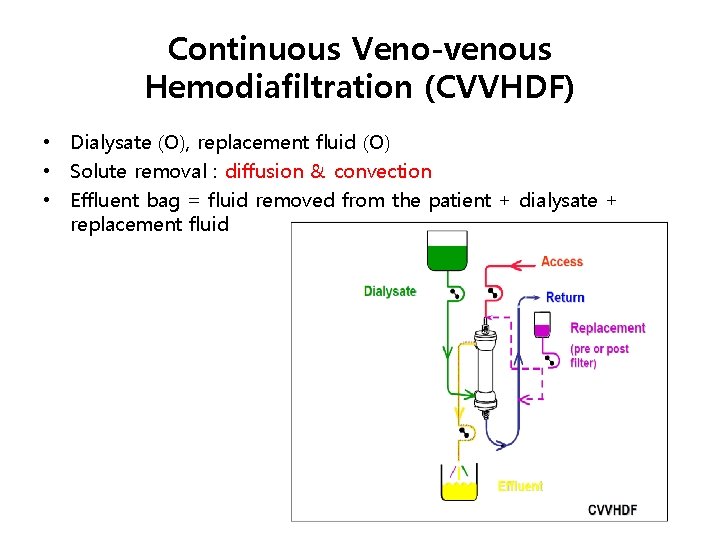
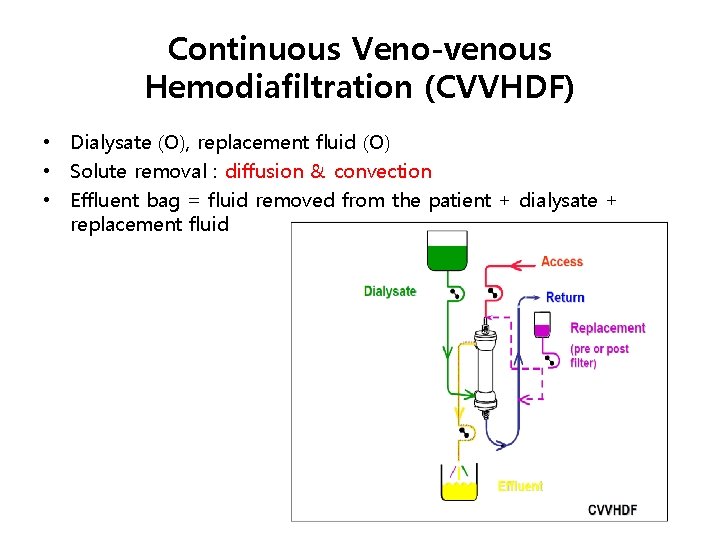
Continuous Veno-venous Hemodiafiltration (CVVHDF) • Dialysate (O), replacement fluid (O) • Solute removal : diffusion & convection • Effluent bag = fluid removed from the patient + dialysate + replacement fluid
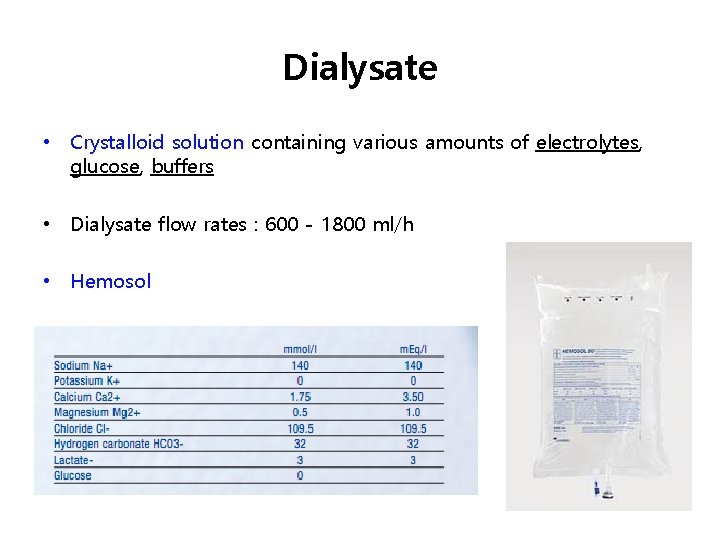
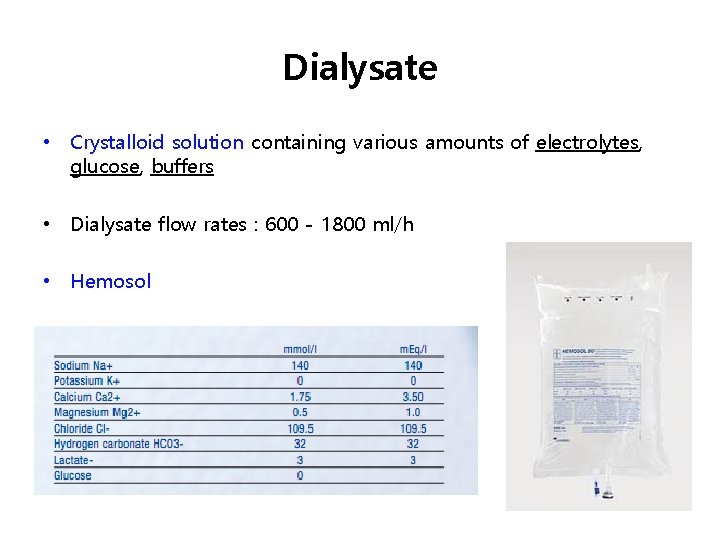
Dialysate • Crystalloid solution containing various amounts of electrolytes, glucose, buffers • Dialysate flow rates : 600 - 1800 ml/h • Hemosol
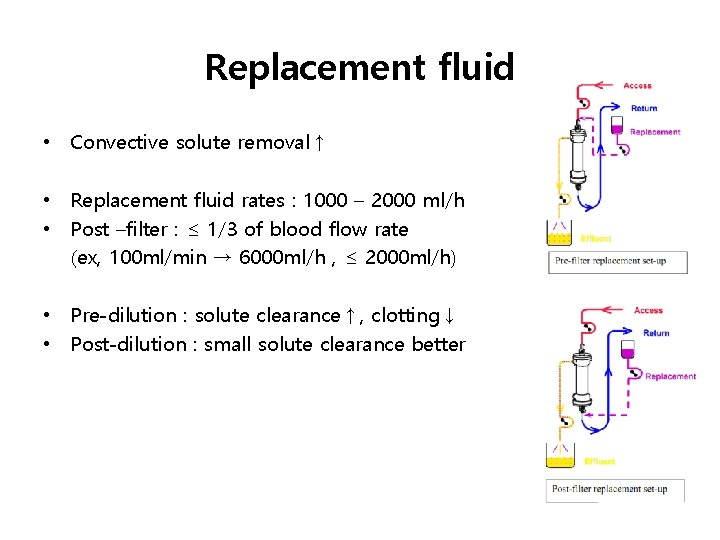
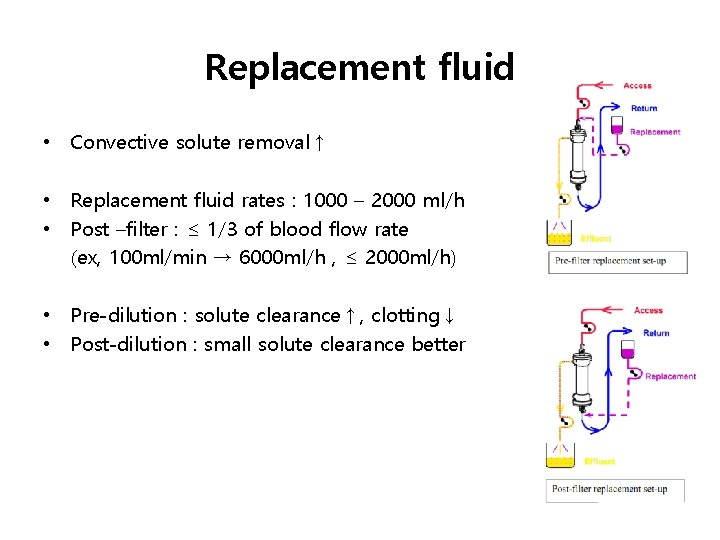
Replacement fluid • Convective solute removal↑ • Replacement fluid rates : 1000 – 2000 ml/h • Post –filter : ≤ 1/3 of blood flow rate (ex, 100 ml/min → 6000 ml/h , ≤ 2000 ml/h) • Pre-dilution : solute clearance↑, clotting↓ • Post-dilution : small solute clearance better
Blood flow rate • Common before : 100 - 150 ml/min • Now : 200 - 250 ml/min to reduce the risk of thrombosis
Effluent • Fluid that drains out of the hemofilter • Plasma water + removed solutes + dialysate + replacement fluid • Recommend effluent volume : 20– 25 ml/kg/h in AKI • Generally necessary to prescribe : 25– 30 ml/kg/h
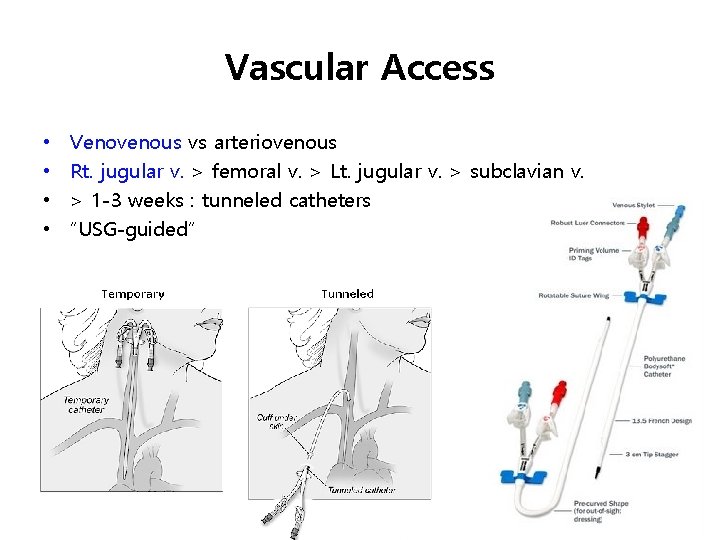
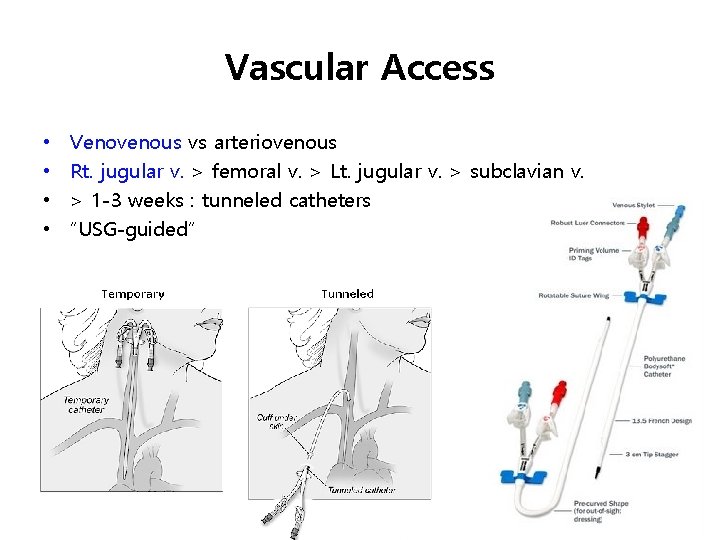
Vascular Access • • Venovenous vs arteriovenous Rt. jugular v. > femoral v. > Lt. jugular v. > subclavian v. > 1 -3 weeks : tunneled catheters “USG-guided”
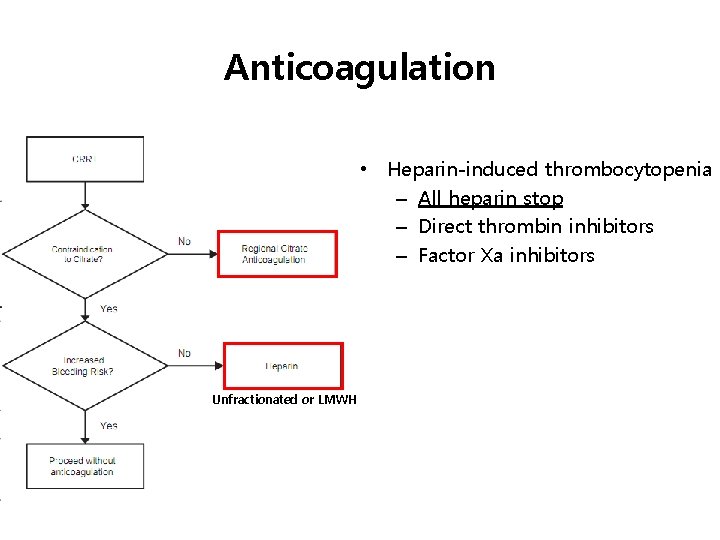
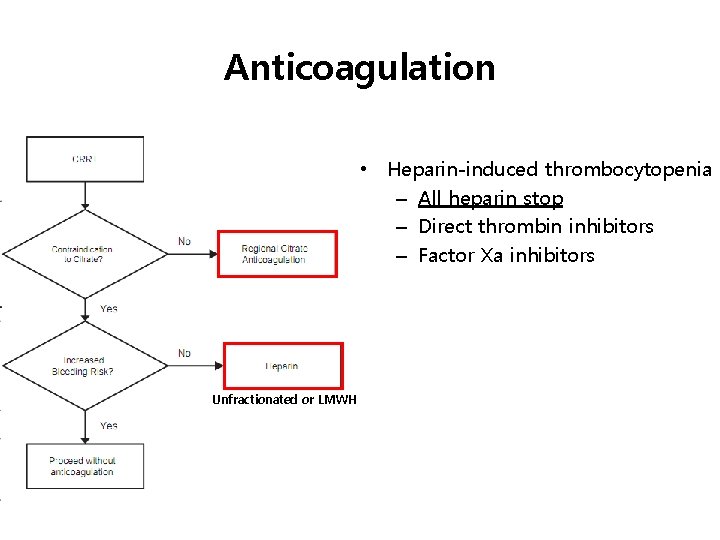
Anticoagulation • Heparin-induced thrombocytopenia – All heparin stop – Direct thrombin inhibitors – Factor Xa inhibitors Unfractionated or LMWH
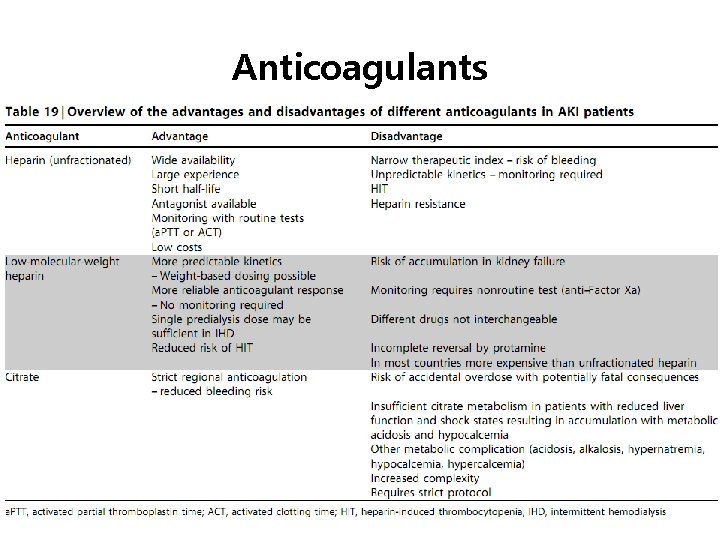
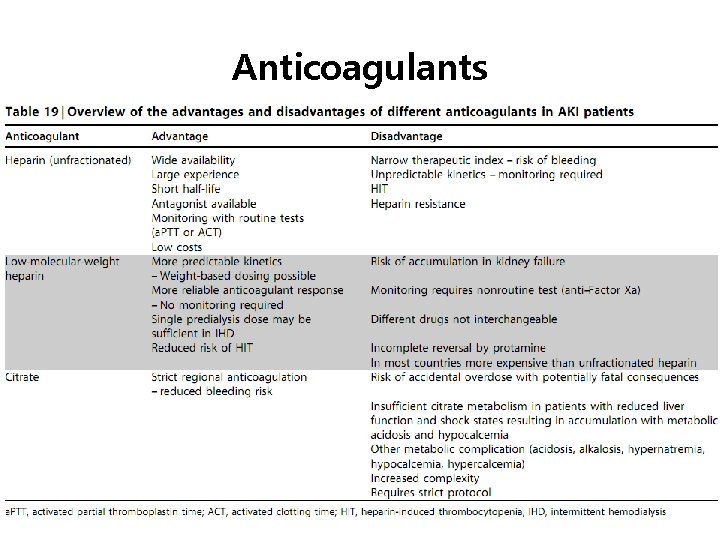
Anticoagulants
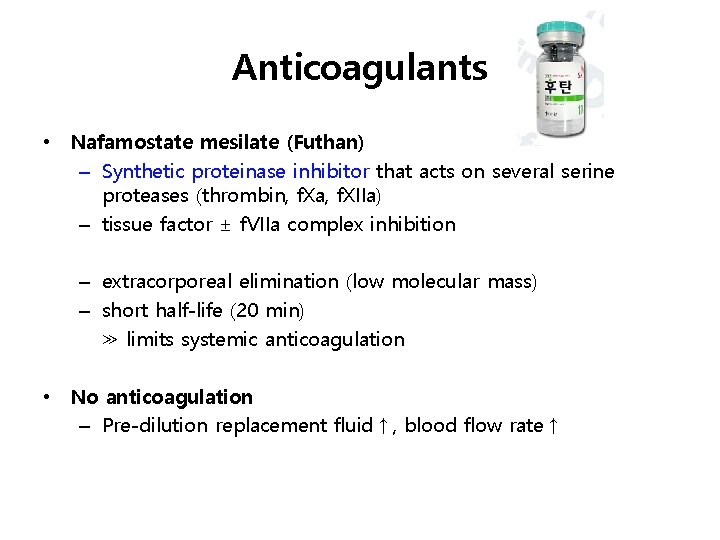
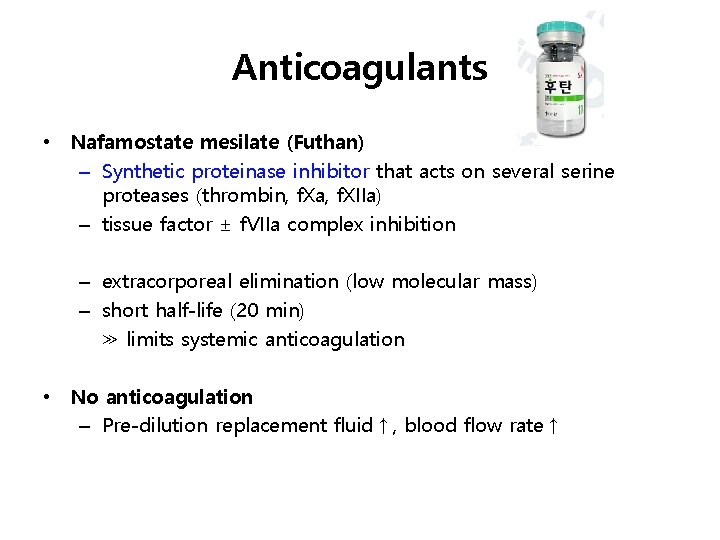
Anticoagulants • Nafamostate mesilate (Futhan) – Synthetic proteinase inhibitor that acts on several serine proteases (thrombin, f. Xa, f. XIIa) – tissue factor ± f. VIIa complex inhibition – extracorporeal elimination (low molecular mass) – short half-life (20 min) ≫ limits systemic anticoagulation • No anticoagulation – Pre-dilution replacement fluid↑, blood flow rate↑
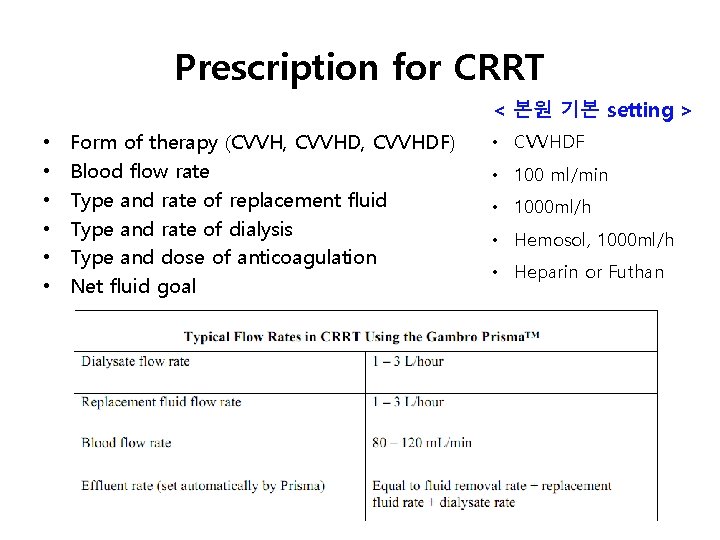
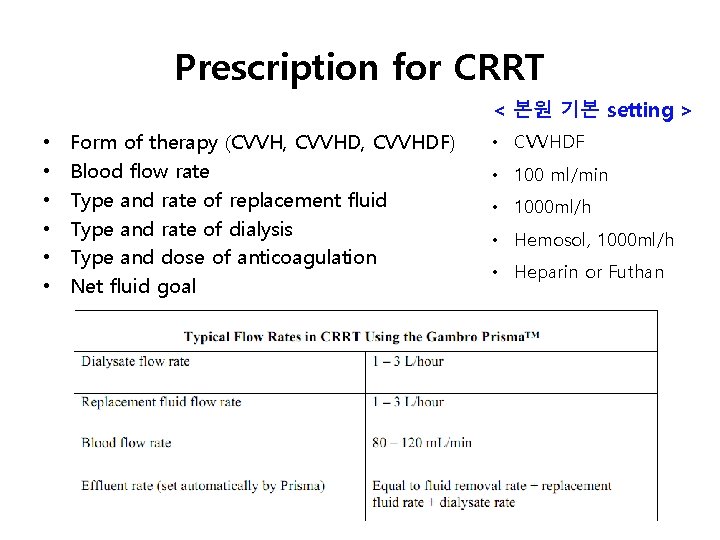
Prescription for CRRT < 본원 기본 setting > • • • Form of therapy (CVVH, CVVHDF) Blood flow rate Type and rate of replacement fluid Type and rate of dialysis Type and dose of anticoagulation Net fluid goal • CVVHDF • 100 ml/min • 1000 ml/h • Hemosol, 1000 ml/h • Heparin or Futhan
Summary of guidelines • Ix : life-threatening changes in fluid, electrolyte, acid-base balance • Vascular access : Rt. jugular > femoral > Lt. jugular > subclavian • Effluent flow rate 20 -25 ml/kg/hr in AKI (actually higher) • Anticoagulation : citrate > heparin
Complication • Vascular access – infection, vascular injury, arterial puncture, hematoma, hemothorax, pneumothorax, arteriovenous fistula, aneurysm, thrombus formation • During therapy – hypotension, arrhythmias, fluid & electrolyte disturbances, nutrient losses, hypothermia, bleeding, hypokalemia, hypophosphatemia, potential underdosing of drugs