Continuous Renal Replacement Therapy Annual Refresher Course in
![Pdialysat = P blood Cd <<< Csang Progressive equilibrium of the [plasma] and [dial] Pdialysat = P blood Cd <<< Csang Progressive equilibrium of the [plasma] and [dial]](https://slidetodoc.com/presentation_image_h/1790d55472cfc31fba0e12a72711520a/image-9.jpg)
![Pdialysat = P blood Cd << Csang Progressive equilibrium of the [plasma] and [dial] Pdialysat = P blood Cd << Csang Progressive equilibrium of the [plasma] and [dial]](https://slidetodoc.com/presentation_image_h/1790d55472cfc31fba0e12a72711520a/image-10.jpg)
![Pdialysat = P blood Cd < Csang Progressive equilibrium of the [plasma] and [dial] Pdialysat = P blood Cd < Csang Progressive equilibrium of the [plasma] and [dial]](https://slidetodoc.com/presentation_image_h/1790d55472cfc31fba0e12a72711520a/image-11.jpg)








- Slides: 51
Continuous Renal Replacement Therapy Annual Refresher Course in CRITICAL CARE Mc. Gill Course Director: Peter Goldberg, MD Didier Payen CC Division & Dept of Anesthesiology 13/4/2000
Content • • • Physical principles Definitions Techniques Clinical issues Supportive therapy or active therapy? – Sepsis an example – Why? – How? – For what goal?
PHYSICAL PRINCIPLES & DEFINITIONS
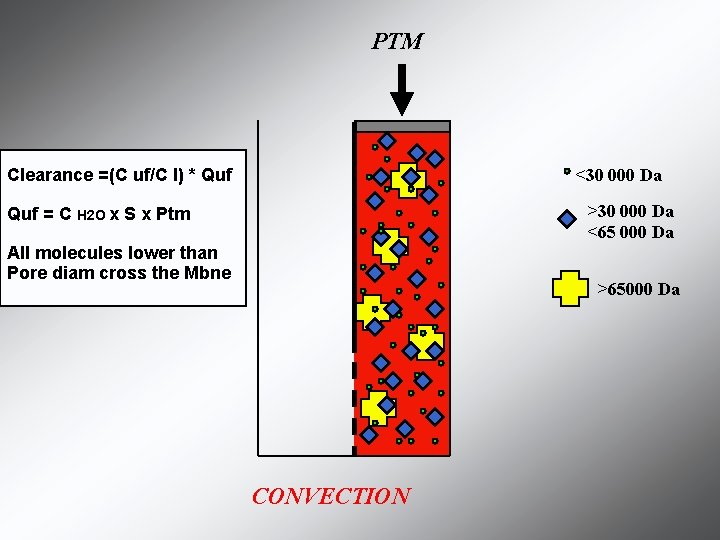
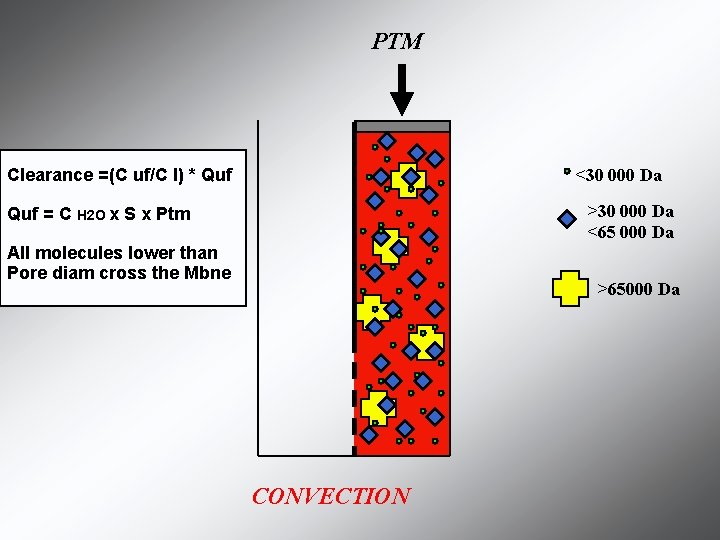
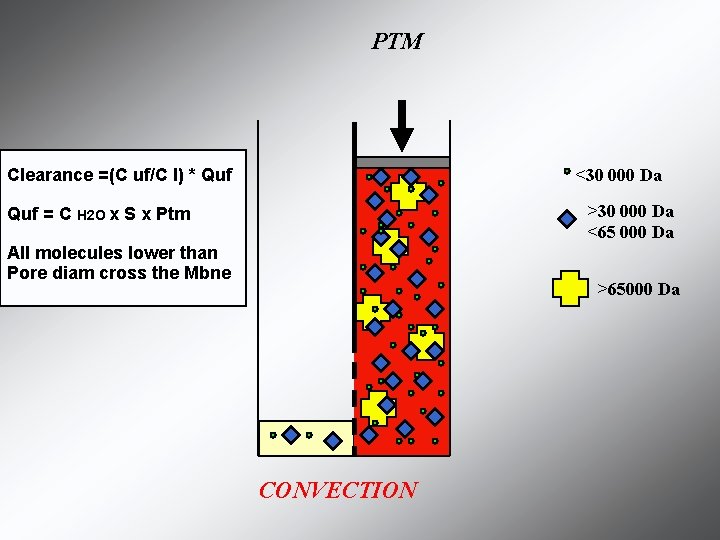
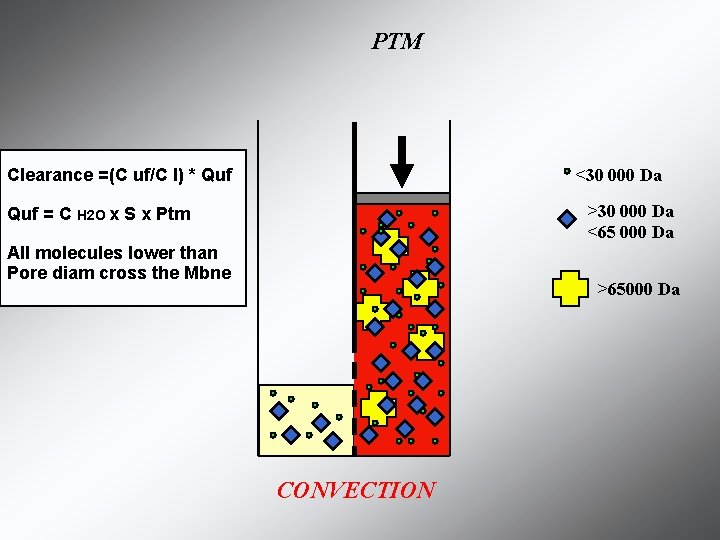
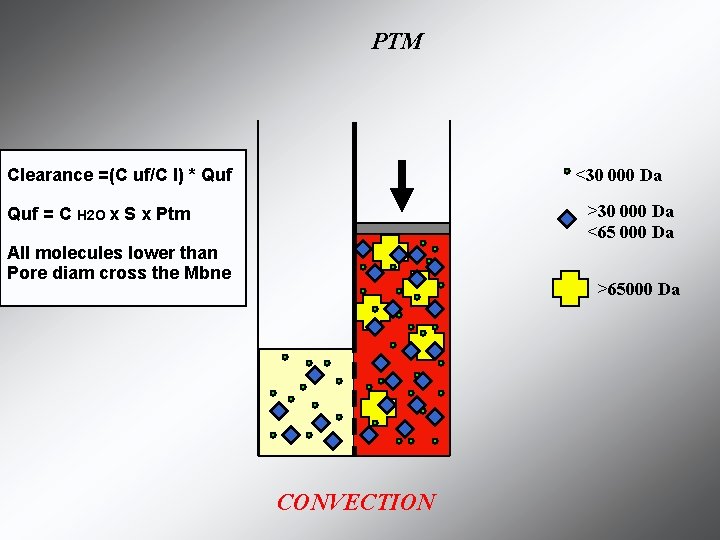
PTM <30 000 Da Clearance =(C uf/C I) * Quf >30 000 Da <65 000 Da Quf = C H 2 O x S x Ptm All molecules lower than Pore diam cross the Mbne >65000 Da CONVECTION
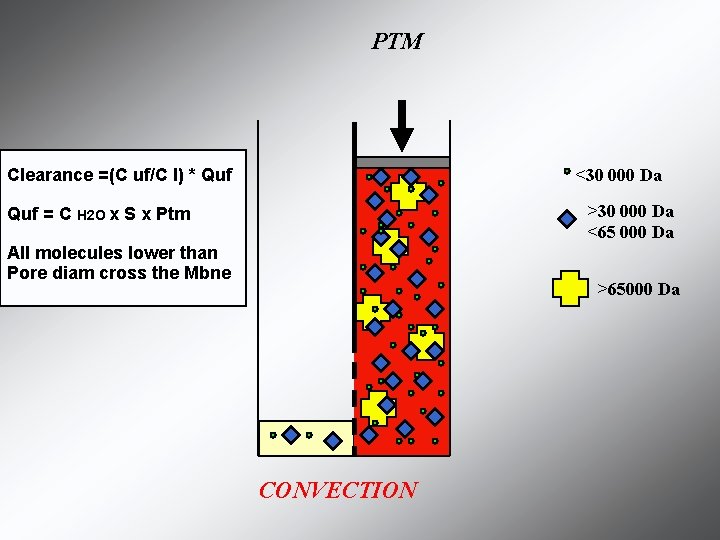
PTM <30 000 Da Clearance =(C uf/C I) * Quf >30 000 Da <65 000 Da Quf = C H 2 O x S x Ptm All molecules lower than Pore diam cross the Mbne >65000 Da CONVECTION
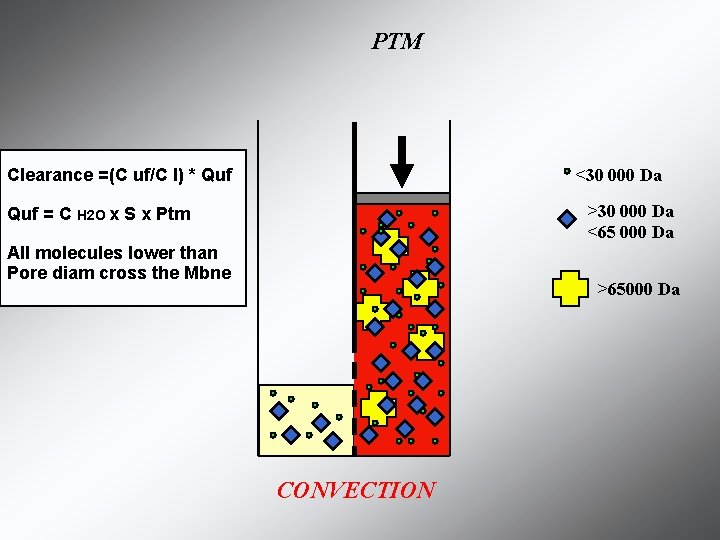
PTM <30 000 Da Clearance =(C uf/C I) * Quf >30 000 Da <65 000 Da Quf = C H 2 O x S x Ptm All molecules lower than Pore diam cross the Mbne >65000 Da CONVECTION
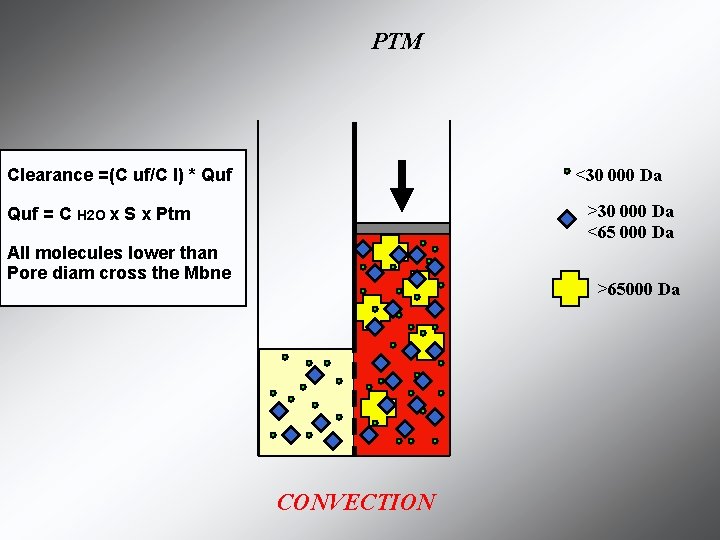
PTM <30 000 Da Clearance =(C uf/C I) * Quf >30 000 Da <65 000 Da Quf = C H 2 O x S x Ptm All molecules lower than Pore diam cross the Mbne >65000 Da CONVECTION
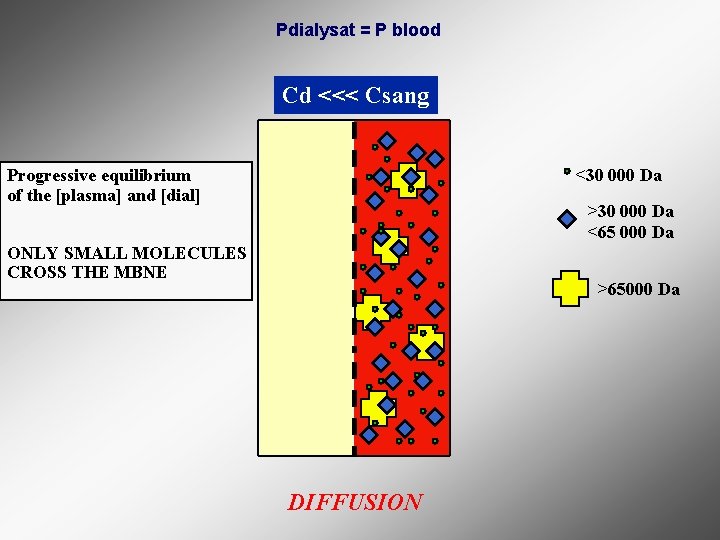
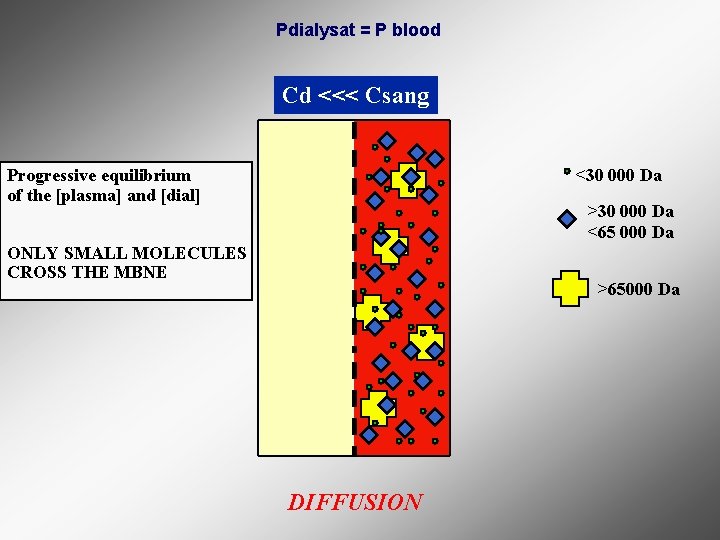
Pdialysat = P blood Cd <<< Csang <30 000 Da Progressive equilibrium of the [plasma] and [dial] >30 000 Da <65 000 Da ONLY SMALL MOLECULES CROSS THE MBNE >65000 Da DIFFUSION
![Pdialysat P blood Cd Csang Progressive equilibrium of the plasma and dial Pdialysat = P blood Cd <<< Csang Progressive equilibrium of the [plasma] and [dial]](https://slidetodoc.com/presentation_image_h/1790d55472cfc31fba0e12a72711520a/image-9.jpg)
Pdialysat = P blood Cd <<< Csang Progressive equilibrium of the [plasma] and [dial] <30 000 Da >30 000 Da <65 000 Da ONLY SMALL MOLECULES CROSS THE MBNE >65000 Da DIFFUSION
![Pdialysat P blood Cd Csang Progressive equilibrium of the plasma and dial Pdialysat = P blood Cd << Csang Progressive equilibrium of the [plasma] and [dial]](https://slidetodoc.com/presentation_image_h/1790d55472cfc31fba0e12a72711520a/image-10.jpg)
Pdialysat = P blood Cd << Csang Progressive equilibrium of the [plasma] and [dial] <30 000 Da >30 000 Da <65 000 Da ONLY SMALL MOLECULES CROSS THE MBNE >65000 Da DIFFUSION
![Pdialysat P blood Cd Csang Progressive equilibrium of the plasma and dial Pdialysat = P blood Cd < Csang Progressive equilibrium of the [plasma] and [dial]](https://slidetodoc.com/presentation_image_h/1790d55472cfc31fba0e12a72711520a/image-11.jpg)
Pdialysat = P blood Cd < Csang Progressive equilibrium of the [plasma] and [dial] <30 000 Da >30 000 Da <65 000 Da ONLY SMALL MOLECULES CROSS THE MBNE >65000 Da DIFFUSION
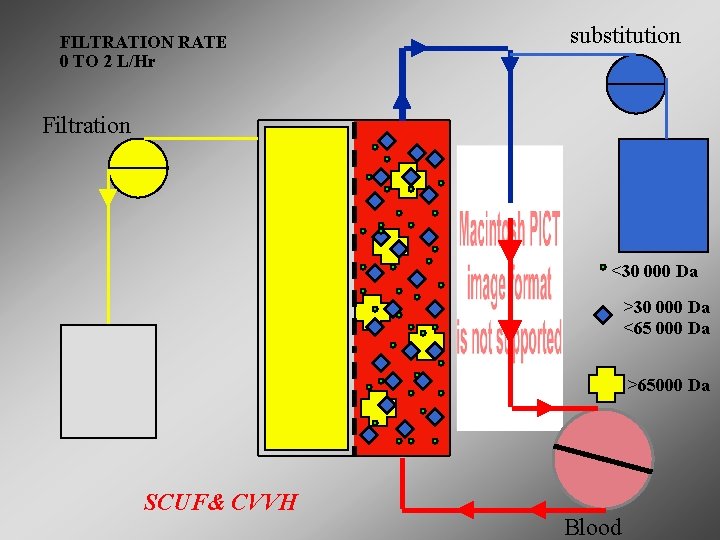
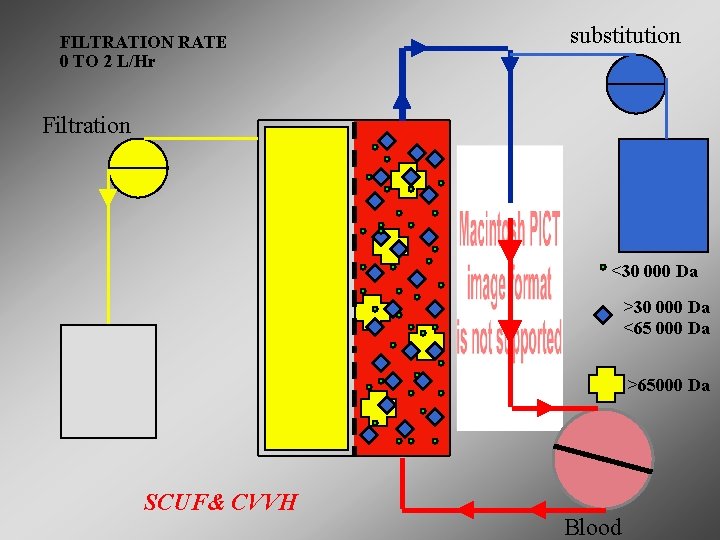
FILTRATION RATE 0 TO 2 L/Hr substitution Filtration <30 000 Da >30 000 Da <65 000 Da >65000 Da SCUF& CVVH Blood
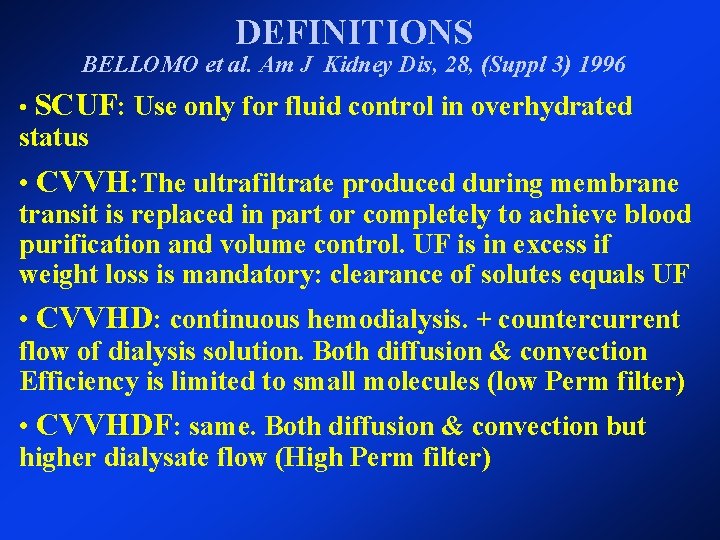
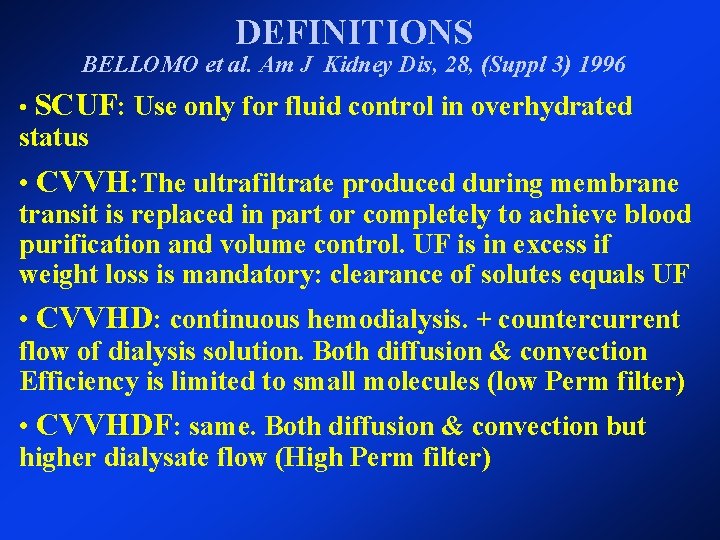
DEFINITIONS BELLOMO et al. Am J Kidney Dis, 28, (Suppl 3) 1996 • SCUF: Use only for fluid control in overhydrated status • CVVH: The ultrafiltrate produced during membrane transit is replaced in part or completely to achieve blood purification and volume control. UF is in excess if weight loss is mandatory: clearance of solutes equals UF • CVVHD: continuous hemodialysis. + countercurrent flow of dialysis solution. Both diffusion & convection Efficiency is limited to small molecules (low Perm filter) • CVVHDF: same. Both diffusion & convection but higher dialysate flow (High Perm filter)

Therapy options Access Return SCUF Slow Continuous Ultrafiltration P R I S M A S Effluent Maximum Pt. Fluid removal rate = 2000 ml/h
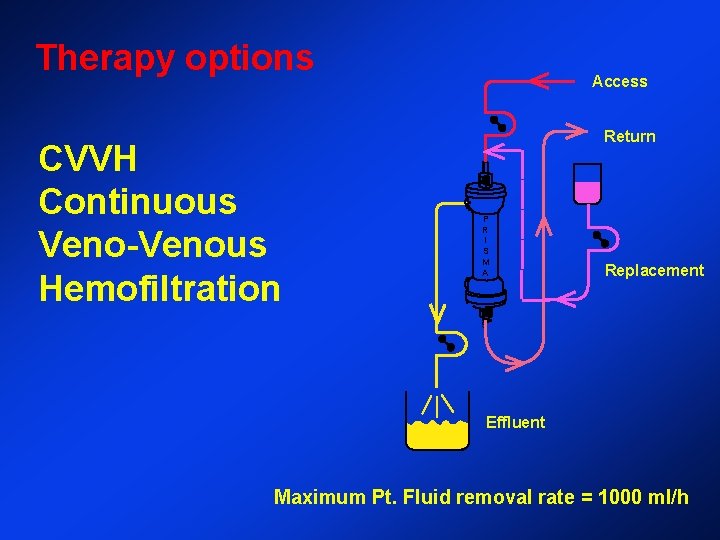
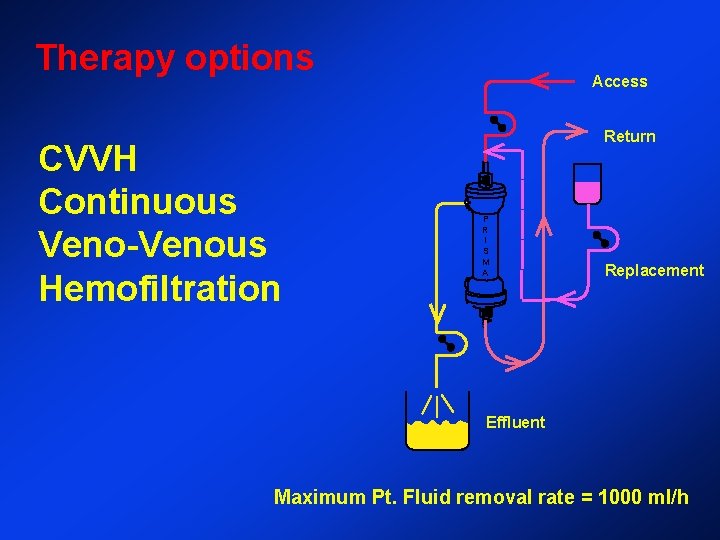
Therapy options CVVH Continuous Veno-Venous Hemofiltration Access Return P R I S M A Replacement S Effluent Maximum Pt. Fluid removal rate = 1000 ml/h

Therapy Options Access Dialysate CVVHD Continuous Veno-Venous Hemodialysis Return P R I S M A S Effluent Maximum Pt. fluid removal rate = 1000 ml/h
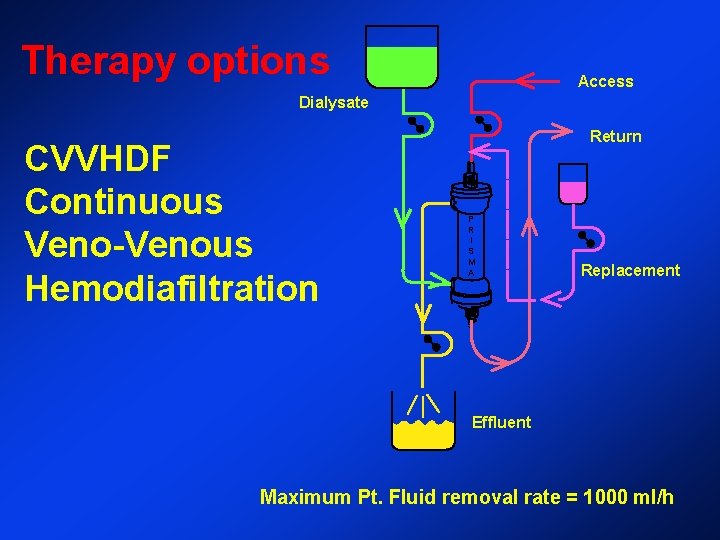
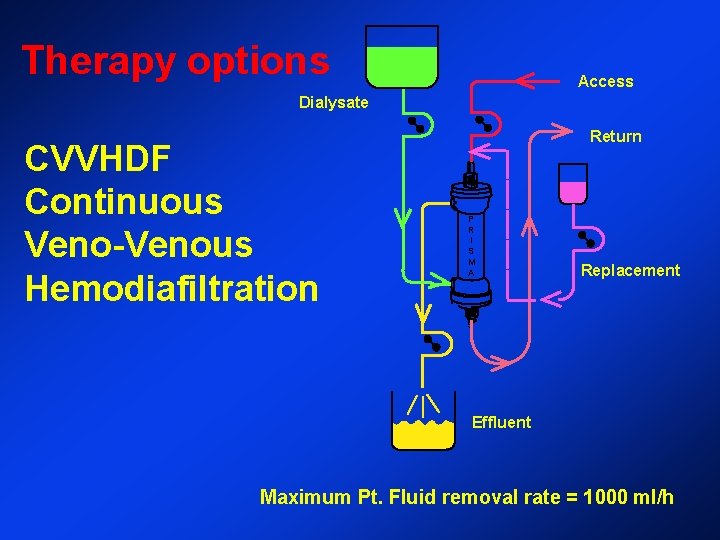
Therapy options Access Dialysate CVVHDF Continuous Veno-Venous Hemodiafiltration Return P R I S M A Replacement S Effluent Maximum Pt. Fluid removal rate = 1000 ml/h
EFFICIENCY

CLINICAL ISSUES
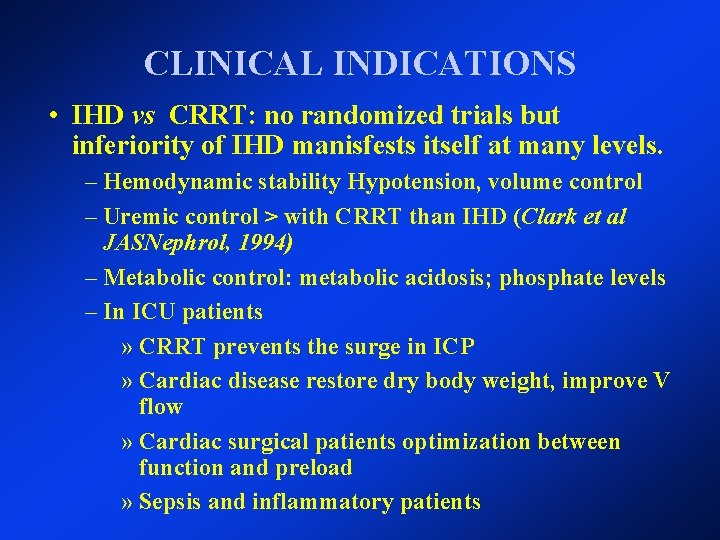
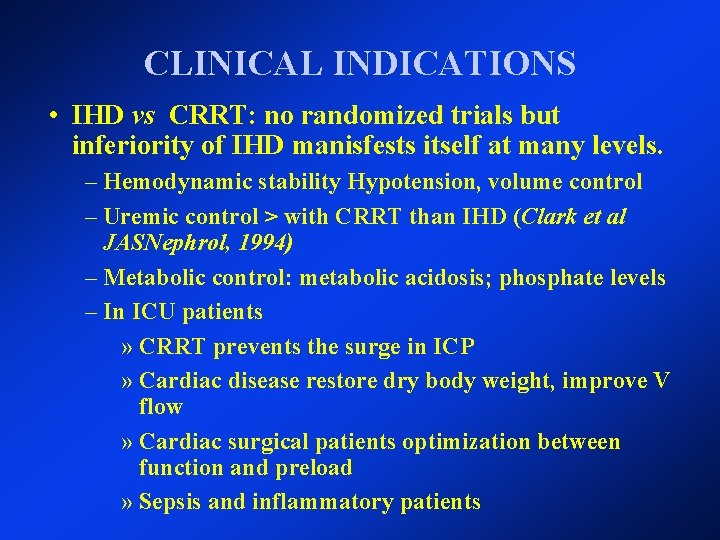
CLINICAL INDICATIONS • IHD vs CRRT: no randomized trials but inferiority of IHD manisfests itself at many levels. – Hemodynamic stability Hypotension, volume control – Uremic control > with CRRT than IHD (Clark et al JASNephrol, 1994) – Metabolic control: metabolic acidosis; phosphate levels – In ICU patients » CRRT prevents the surge in ICP » Cardiac disease restore dry body weight, improve V flow » Cardiac surgical patients optimization between function and preload » Sepsis and inflammatory patients
CRRT AND INFLAMMATION Sepsis an example
HYPOTHESIS FOR MODS PREVENTION • Control of tissue edema • EDTX adsorption • Immunomodulation
CAVH after Staph Aureus in swine (Lee PA et al; Crit Care Med 1993; 21: 914 -924) • Goals: 1) CAVH impact on morbidity and mortality 2) If UF contains mediators • Design: prospective, randomized, controlled (n=65) • Staph aureus (8 x 10 9 CFU) over 1 hr • Part 1: Group 1: 5. 5% plasma filtration fraction Group 2: 16. 6% " " " Group 3: 33. 4% Control clean UF • Part 2: UFiltrate concentrate from each group infused into healthy pigs
CAVH after Staph Aureus in swine (Lee PA et al; Crit Care Med 1993; 21: 914 -924) Measurements and results: • In G 1, 2, 3, the survival rate increased in relation to FF in comparison with control • UF concentrate injection led to animal death similarly to Staph aureus in control group. • Conclusion: CAVH-improved survival rate might be related to mediators removal

EDTX & HEMOFILTRATION : In vivo experimental studies (1) • Stein et al, Intens. Care Med. , 1991 – pig model, LPS injection – membrane : polysulfone, zero balanced HF – decrease in PVR, EVLW ==> other mechanisms than water balance
EDTX & HEMOFILTRATION : In vivo experimental studies (2) • Gomez et al, Anesthesiology, 1990 – dog model, alive E coli ; in vitro study – cuprophane membrane – CHF reversed myocardial depression – septic sera depressed ex vivo myocardial contraction, an effect which is prevented by CHF ==> removal of cardio-depressive substances
EDTX & HEMOFILTRATION : In vivo experimental studies Grootendorst et al, J. Crit. Care, 1993 - Endotoxin shock in pigs - Polysulfone membrane - Ultrafiltrate contains filtrable factors that increase Pap and depress cardiac performance in healthy animals Mateo et al, Am. Resp. J. Crit. Care Med. , 1993, 1994 - Rabbit endotoxinic shock model - AN 69 adapted circuit; Hemo-adsorption only; pre-EDTX injection - No resuscitation; Ao BF, Pas, HR, - EDTX clearance; TNF�; ex vivo vascular reactivity.
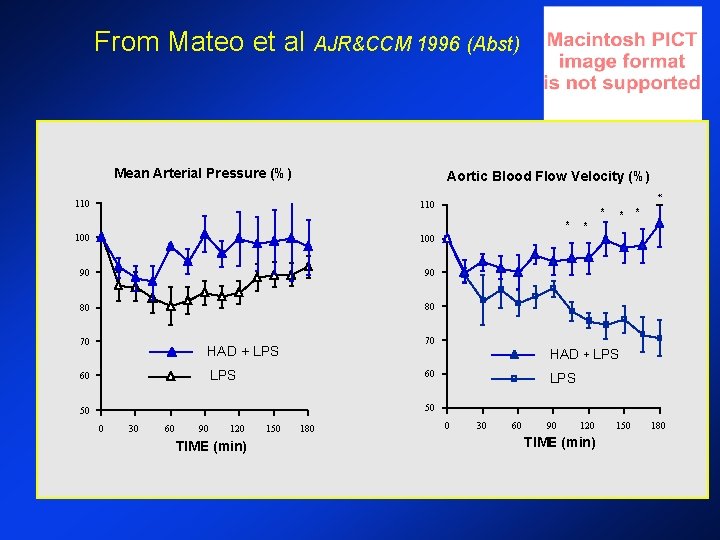
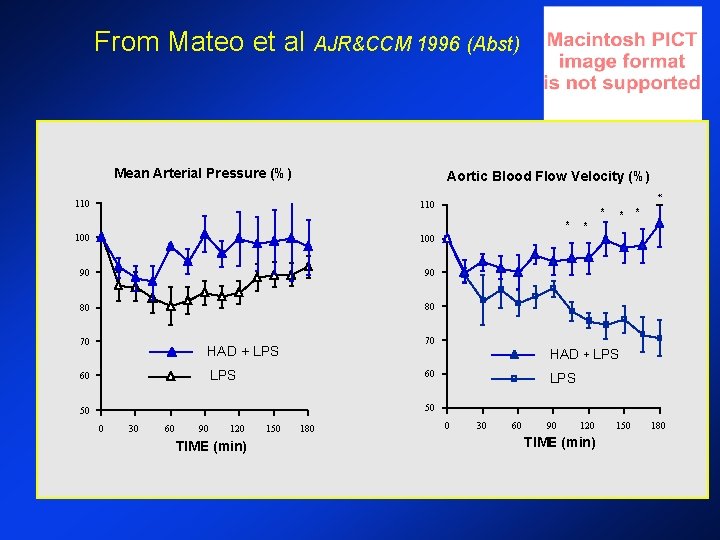
From Mateo et al AJR&CCM 1996 (Abst) Mean Arterial Pressure (%) * Aortic Blood Flow Velocity (%) 110 * 100 90 90 80 80 70 70 HAD + LPS * * HAD + LPS 60 * * 60 LPS 50 50 0 30 60 90 120 TIME (min) 150 180
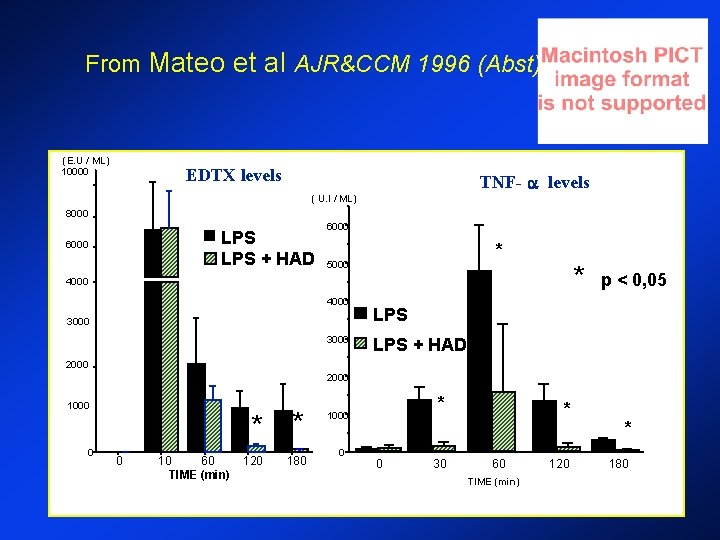
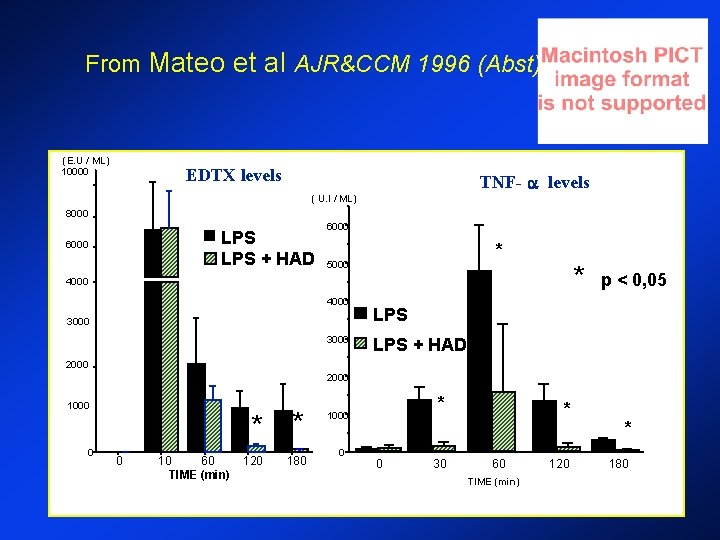
From Mateo et al AJR&CCM 1996 (Abst) (E. U / ML) 10000 EDTX levels TNF- levels ( U. I / ML) 8000 LPS + HAD 6000 * 5000 * 4000 3000 p < 0, 05 LPS + HAD 2000 1000 0 0 10 60 TIME (min) * * 120 180 * 1000 0 0 30 * 60 TIME (min) 120 * 180
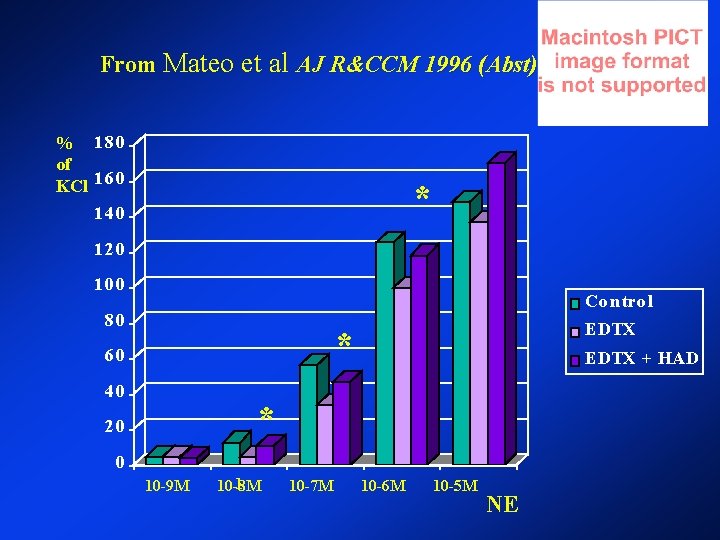
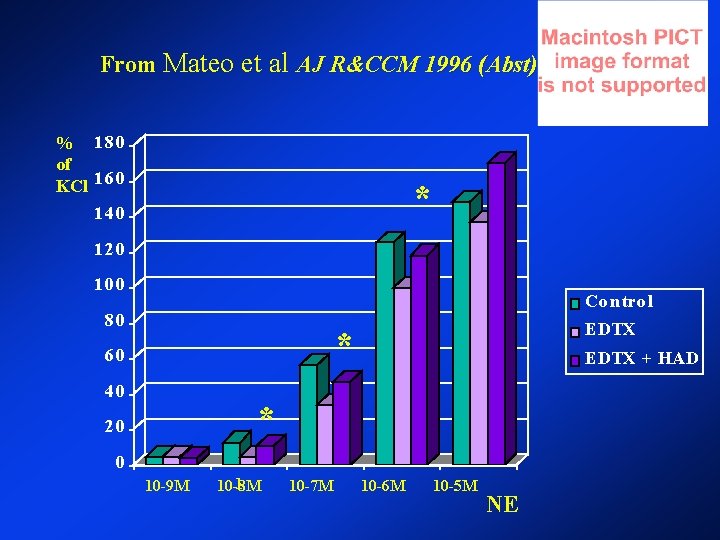
From Mateo et al AJ R&CCM 1996 (Abst) % 180 of KCl 160 * 140 120 100 Co n tro l 80 EDTX * 60 40 EDTX + HAD * 20 0 10 -9 M 1 10 -8 M 10 -7 M 10 -6 M 10 -5 M NE
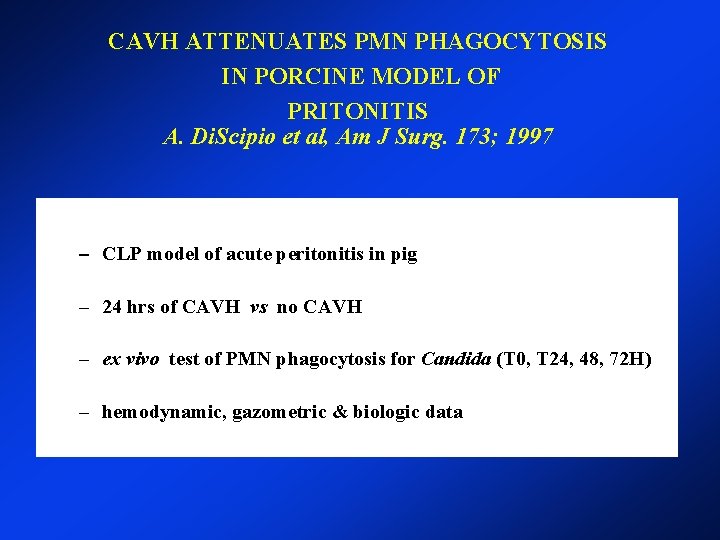
CAVH ATTENUATES PMN PHAGOCYTOSIS IN PORCINE MODEL OF PRITONITIS A. Di. Scipio et al, Am J Surg. 173; 1997 – CLP model of acute peritonitis in pig – 24 hrs of CAVH vs no CAVH – ex vivo test of PMN phagocytosis for Candida (T 0, T 24, 48, 72 H) – hemodynamic, gazometric & biologic data
CAVH ATTENUATES PMN PHAGOCYTOSIS IN PORCINE MODEL OF PERITONITIS (A. Di. Scipio et al, Am J Surg. 173; 1997) • RESULTS – No difference in hemodynamic & gasometric parameters between CAVH & control – CAVH decreases intensity of PMN phagocytosis (opsonisation) and PMN hyperactivity until the early phase of sepsis
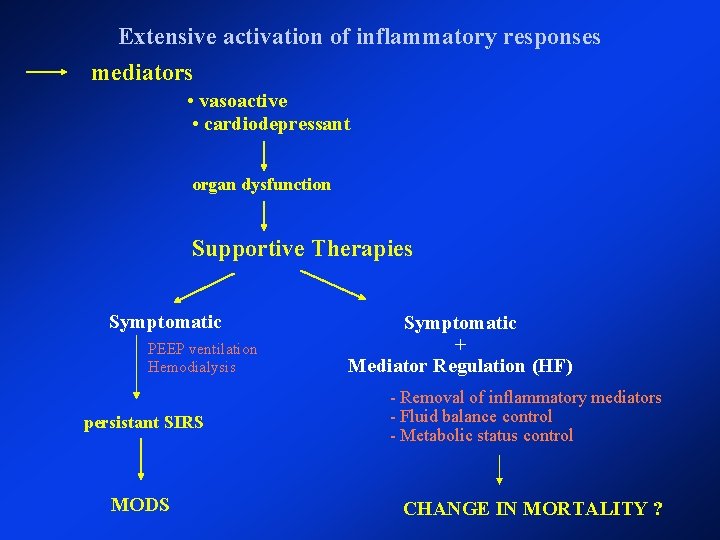
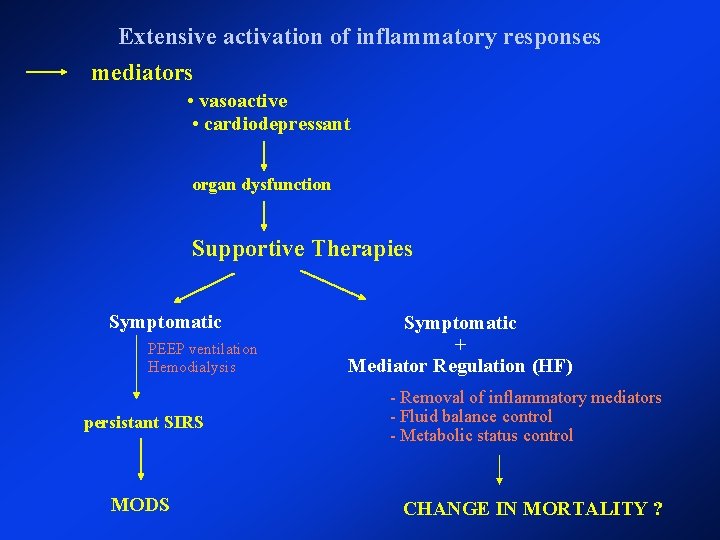
Extensive activation of inflammatory responses mediators • vasoactive • cardiodepressant organ dysfunction Supportive Therapies Symptomatic PEEP ventilation Hemodialysis persistant SIRS MODS Symptomatic + Mediator Regulation (HF) - Removal of inflammatory mediators - Fluid balance control - Metabolic status control CHANGE IN MORTALITY ?
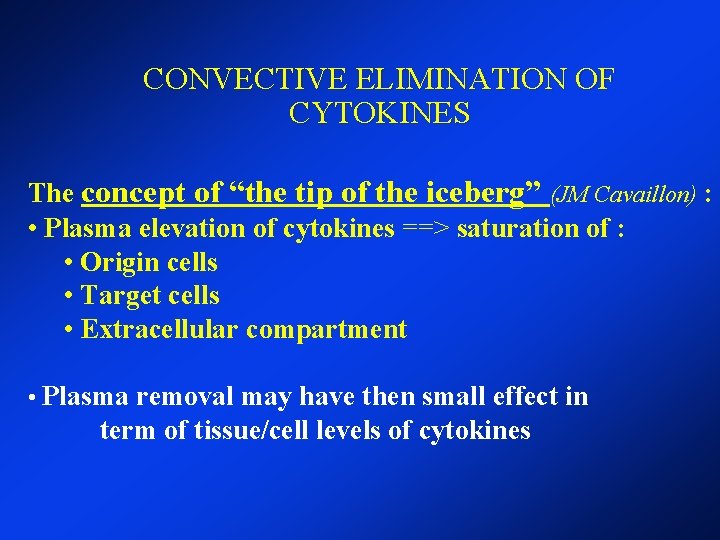
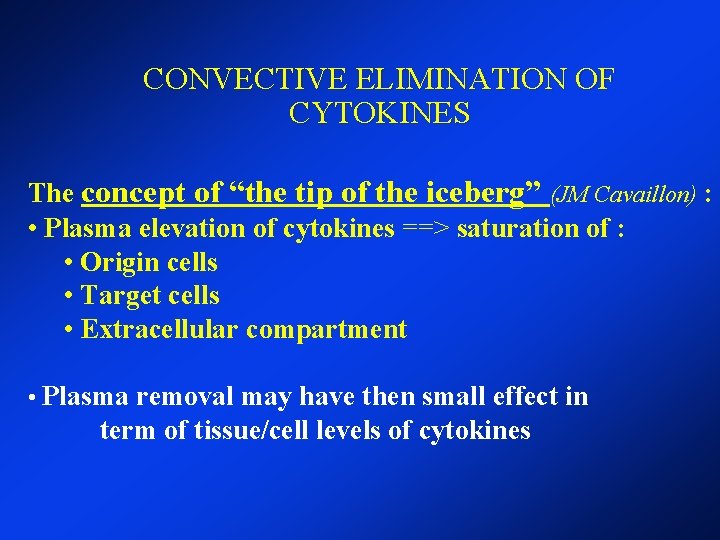
CONVECTIVE ELIMINATION OF CYTOKINES The concept of “the tip of the iceberg” (JM Cavaillon) : • Plasma elevation of cytokines ==> saturation of : • Origin cells • Target cells • Extracellular compartment • Plasma removal may have then small effect in term of tissue/cell levels of cytokines
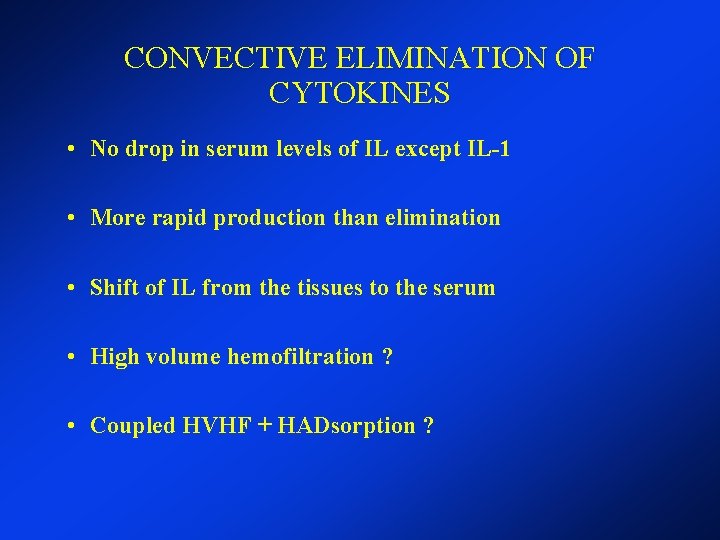
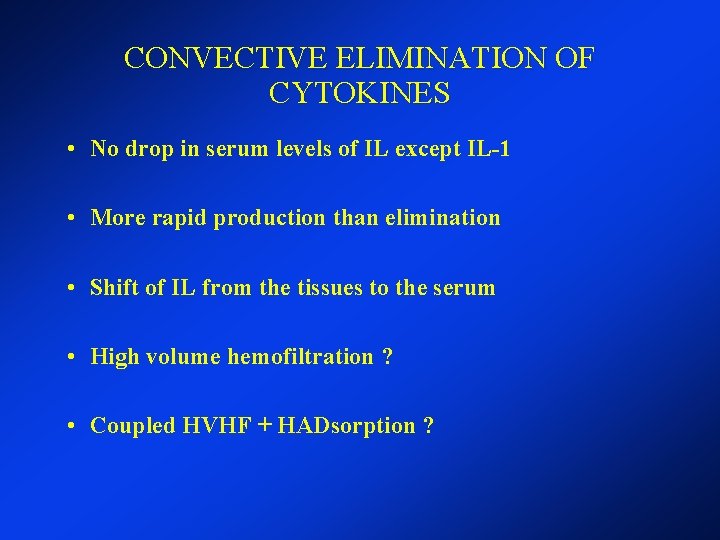
CONVECTIVE ELIMINATION OF CYTOKINES • No drop in serum levels of IL except IL-1 • More rapid production than elimination • Shift of IL from the tissues to the serum • High volume hemofiltration ? • Coupled HVHF + HADsorption ?
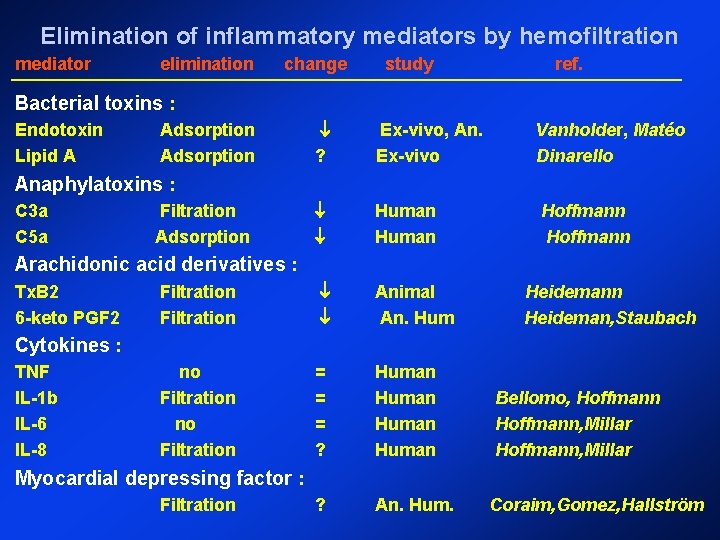
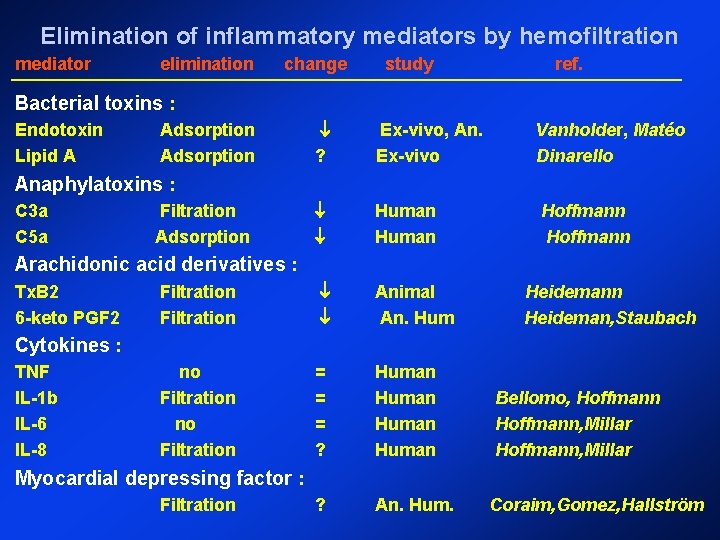
Elimination of inflammatory mediators by hemofiltration mediator elimination change study ref. Bacterial toxins : Endotoxin Lipid A ? Ex-vivo, An. Ex-vivo Human Filtration Animal An. Hum no Filtration = = = ? Human ? An. Hum. Adsorption Vanholder, Matéo Dinarello Anaphylatoxins : C 3 a C 5 a Filtration Adsorption Hoffmann Arachidonic acid derivatives : Tx. B 2 6 -keto PGF 2 Heidemann Heideman, Staubach Cytokines : TNF IL-1 b IL-6 IL-8 Bellomo, Hoffmann, Millar Myocardial depressing factor : Filtration Coraim, Gomez, Hallström
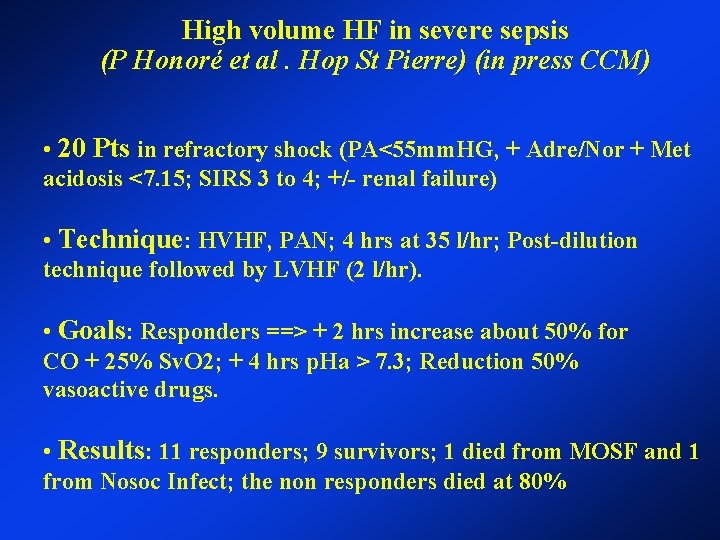
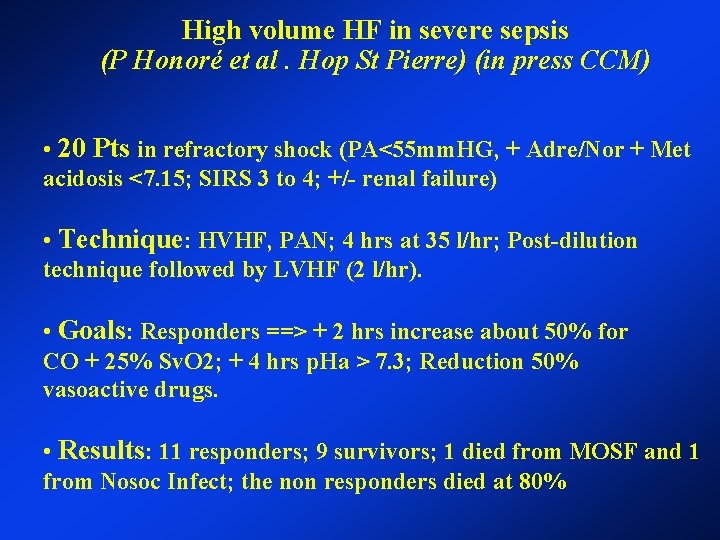
High volume HF in severe sepsis (P Honoré et al. Hop St Pierre) (in press CCM) • 20 Pts in refractory shock (PA<55 mm. HG, + Adre/Nor + Met acidosis <7. 15; SIRS 3 to 4; +/- renal failure) • Technique: HVHF, PAN; 4 hrs at 35 l/hr; Post-dilution technique followed by LVHF (2 l/hr). • Goals: Responders ==> + 2 hrs increase about 50% for CO + 25% Sv. O 2; + 4 hrs p. Ha > 7. 3; Reduction 50% vasoactive drugs. • Results: 11 responders; 9 survivors; 1 died from MOSF and 1 from Nosoc Infect; the non responders died at 80%
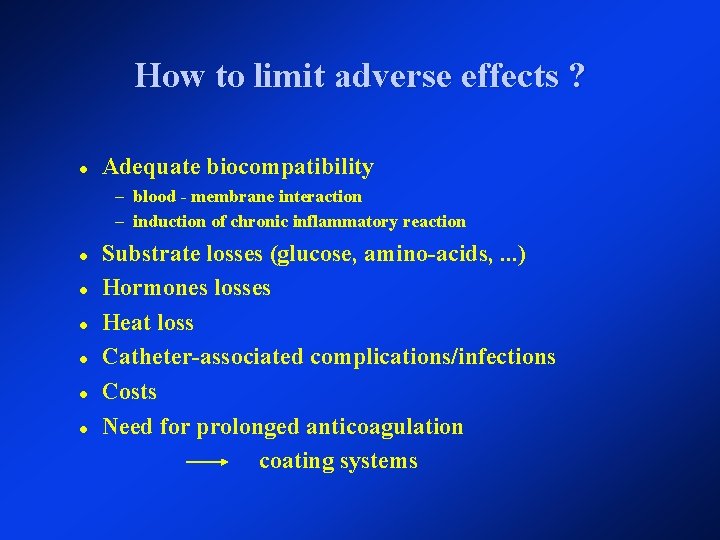
How to limit adverse effects ? Adequate biocompatibility – blood - membrane interaction – induction of chronic inflammatory reaction Substrate losses (glucose, amino-acids, . . . ) Hormones losses Heat loss Catheter-associated complications/infections Costs Need for prolonged anticoagulation coating systems
CONTROL STUDIES • • Substances involved ? Mechanisms of the inflammatory reaction ? Before or after renal failure appearance? End-points : mortality ? Organ failure ? Cost/benefit ? design? ? ?
PERSPECTIVES Materials • Enhanced adsorption • Definitions of cut-offs for specific molecules • Selective or non-selective removal • Anticoagulation coating systems

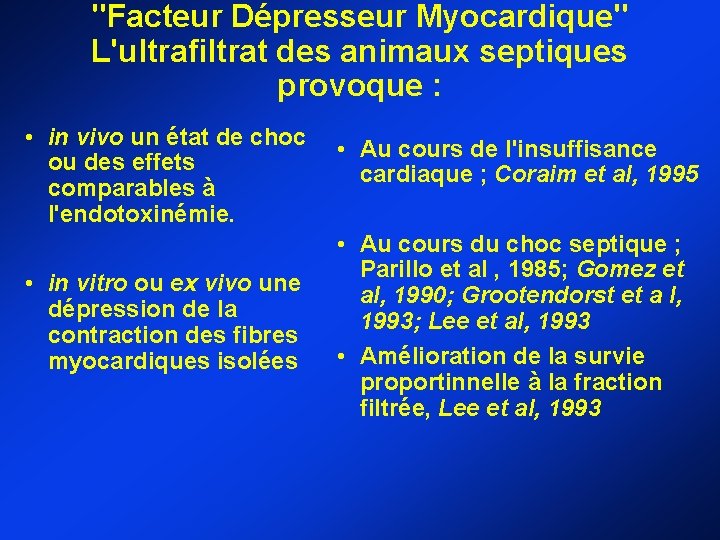
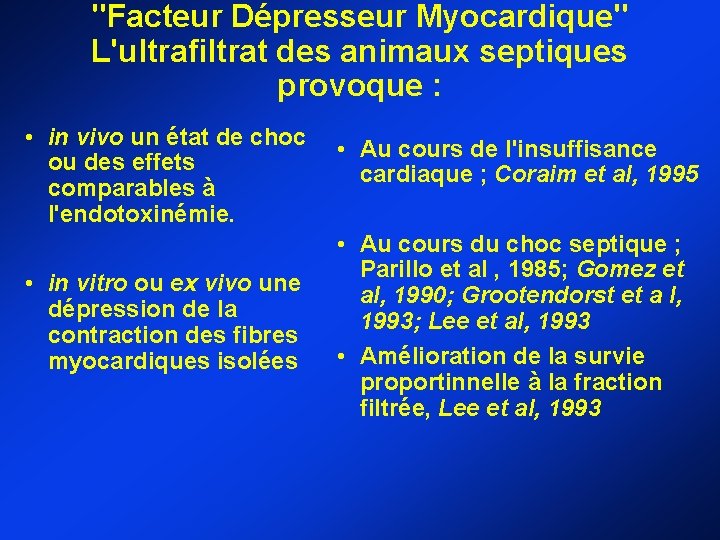
"Facteur Dépresseur Myocardique" L'ultrafiltrat des animaux septiques provoque : • in vivo un état de choc ou des effets comparables à l'endotoxinémie. • in vitro ou ex vivo une dépression de la contraction des fibres myocardiques isolées • Au cours de l'insuffisance cardiaque ; Coraim et al, 1995 • Au cours du choc septique ; Parillo et al , 1985; Gomez et al, 1990; Grootendorst et a l, 1993; Lee et al, 1993 • Amélioration de la survie proportinnelle à la fraction filtrée, Lee et al, 1993

Initial insult (bacterial, viral, traumatic, thermal) Local pro-inflammatory response Systemic spillover of pro-inflammatory mediators Local anti-inflammatory response from Bone Systemic spillover of anti-inflammatory mediators Systemic reaction SIRS (pro-inflammatory) CRRT? ? CARS (anti-inflammatory) MARS (mixed) C H A O Cardiovascular compromise (shock) SIRS predominates Homeostasis CARS and SIRS balanced Apoptosis (cell death) Death with minimal inflammation Organ dysfunction SIRS predominates S Suppression of the immune system CARS predominates
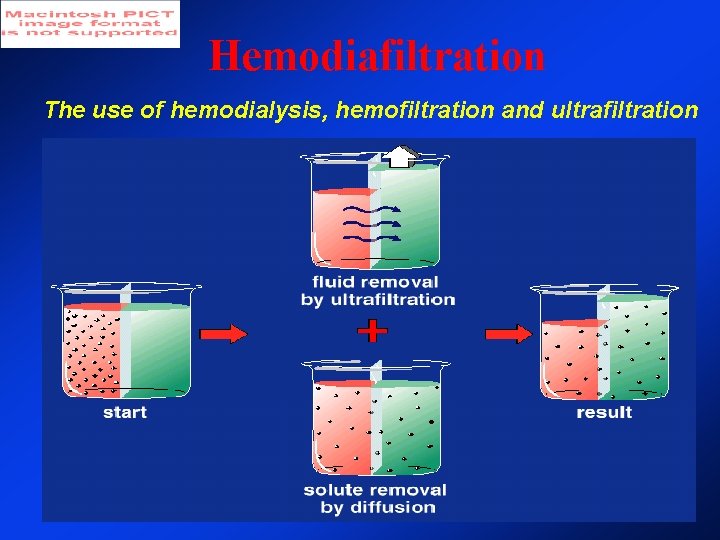
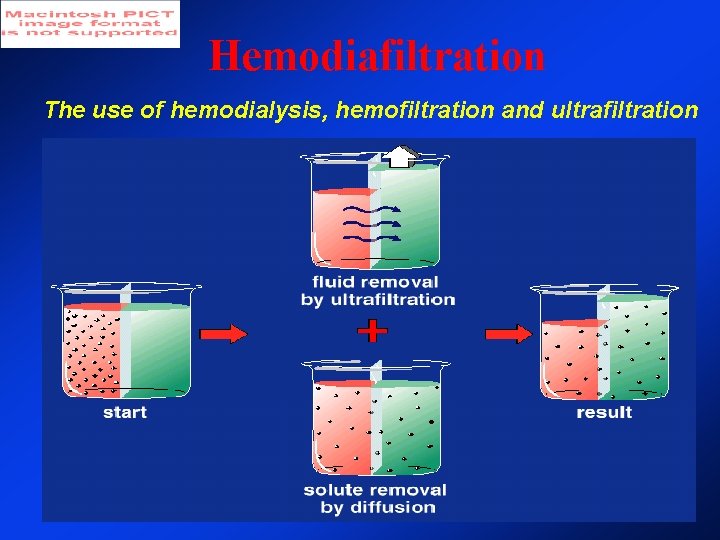
Hemodiafiltration The use of hemodialysis, hemofiltration and ultrafiltration
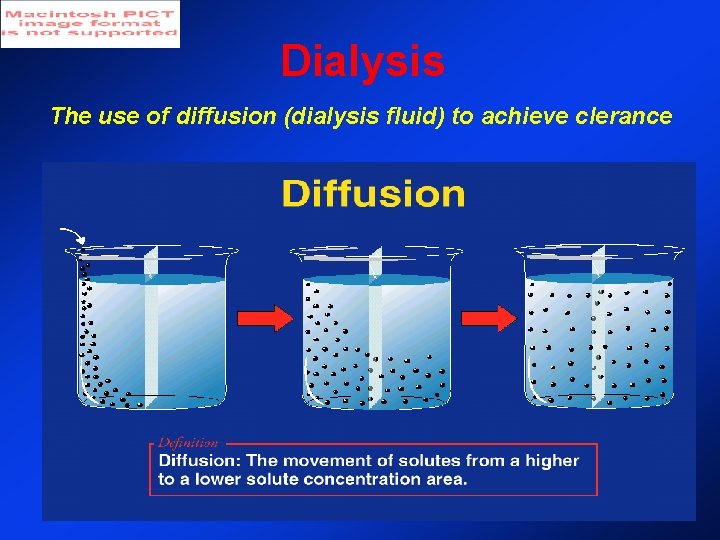
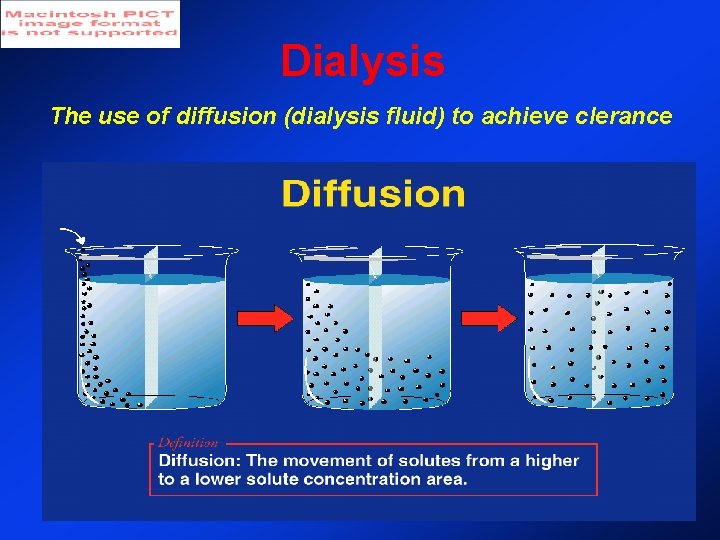
Dialysis The use of diffusion (dialysis fluid) to achieve clerance
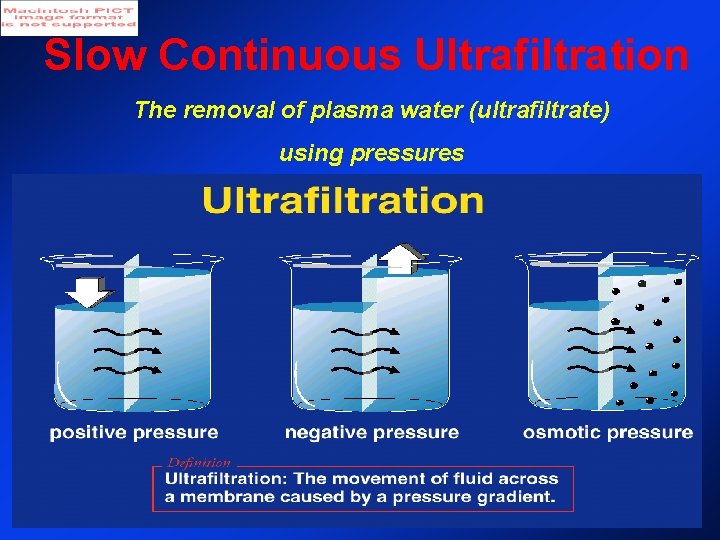
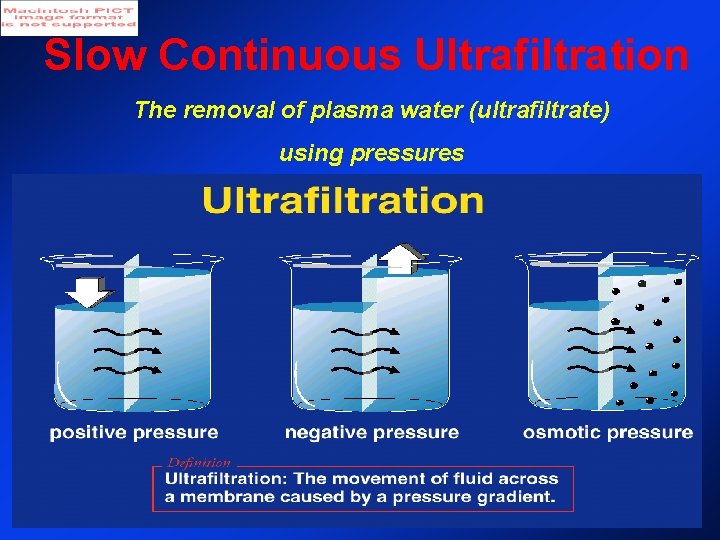
Slow Continuous Ultrafiltration The removal of plasma water (ultrafiltrate) using pressures
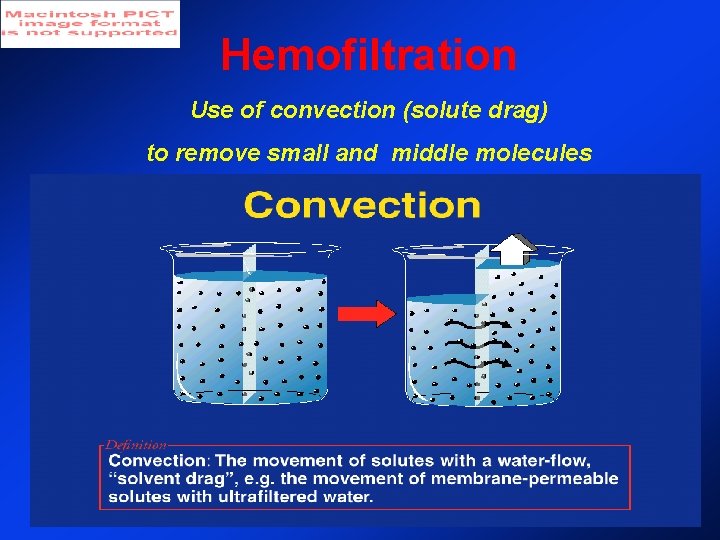
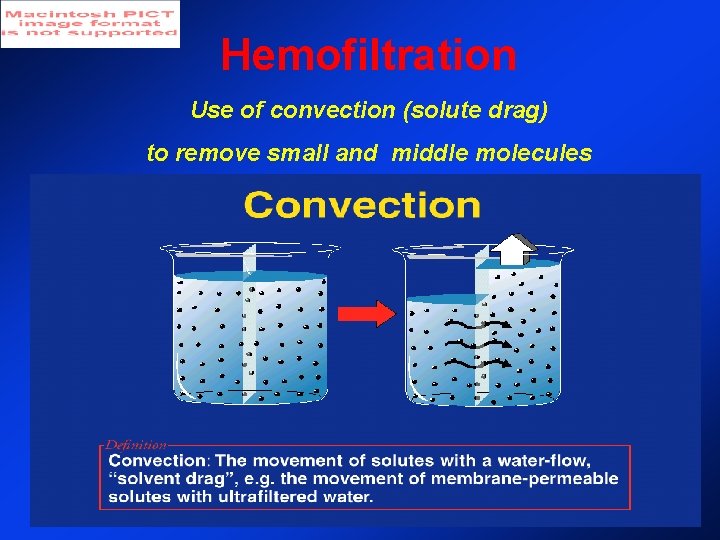
Hemofiltration Use of convection (solute drag) to remove small and middle molecules