Continuous Positive Airway Pressure For EMT Providers State
- Slides: 44
Continuous Positive Airway Pressure For EMT Providers State Education & Training Committee December 2012
Goal n The student will be able to correctly utilize service specific CPAP devices in a respiratory compromised patient n [img]http: //hammondems. com/images/d_1976. jpg
Objectives n At the completion of this training, the BLS provider will: Describe respiratory anatomy and physiology n Verbalize understanding of respiratory disorders / illnesses n Appreciate the benefits and limitations of CPAP in alleviating patient symptoms n List indication and contraindications for use. n
Anatomy and Physiology of Respiration
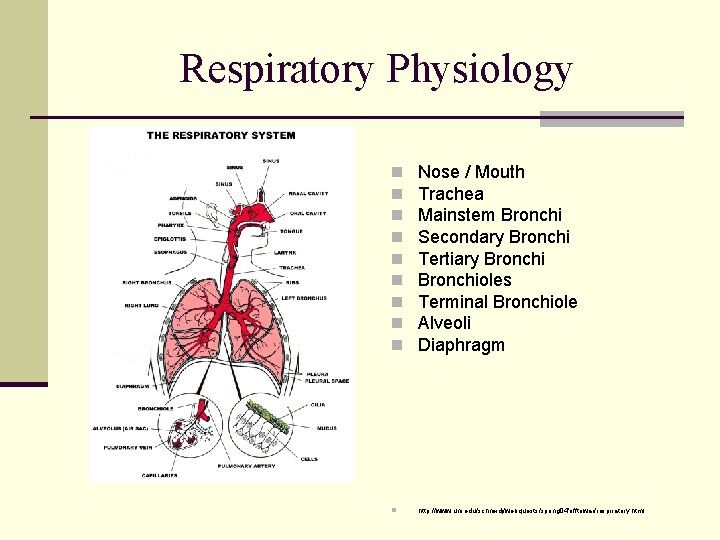
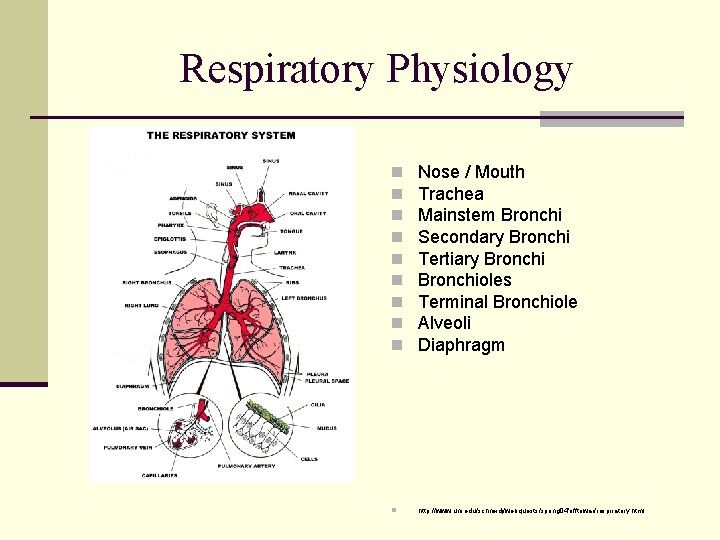
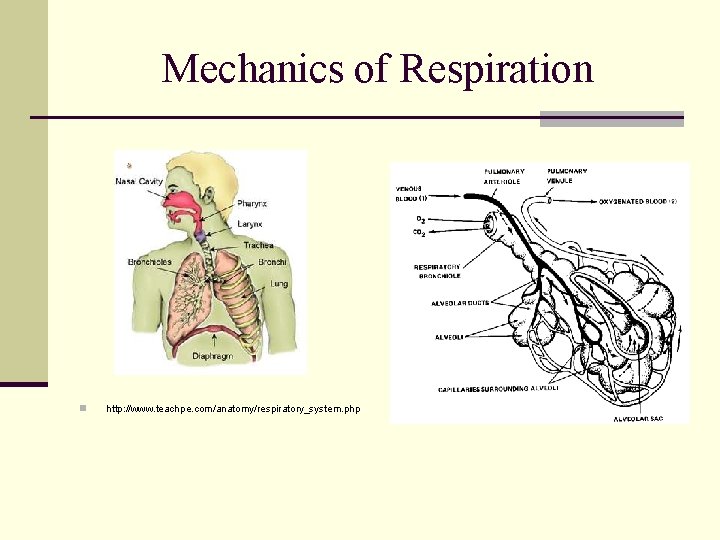
Respiratory Physiology n n n n n Nose / Mouth Trachea Mainstem Bronchi Secondary Bronchi Tertiary Bronchioles Terminal Bronchiole Alveoli Diaphragm n http: //www. uni. edu/schneidj/webquests/spring 04/offtowar/respiratory. html
Negative Pressure n Respiration driven by process of negative intrathoracic pressures n Negative pressure n n Initiates inhalation and acquisition of O 2 Assists to increase intrathoracic blood flow n Hemodynamic Effects n Equalization of pressures n initiates exhalation and elimination of CO 2
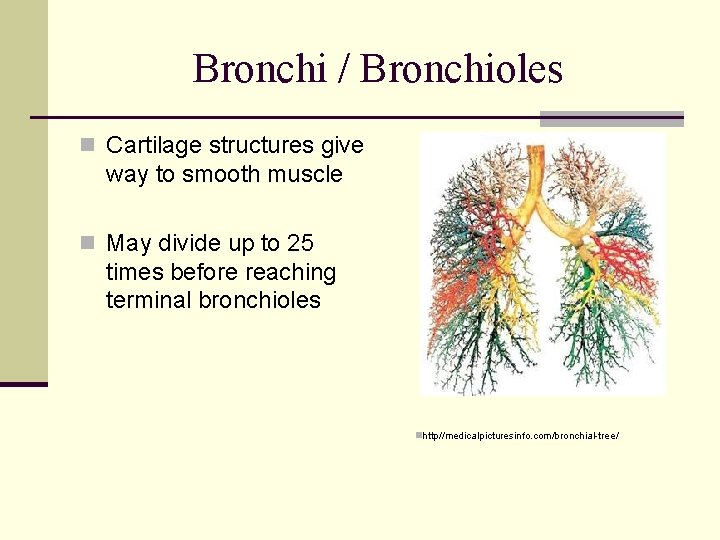
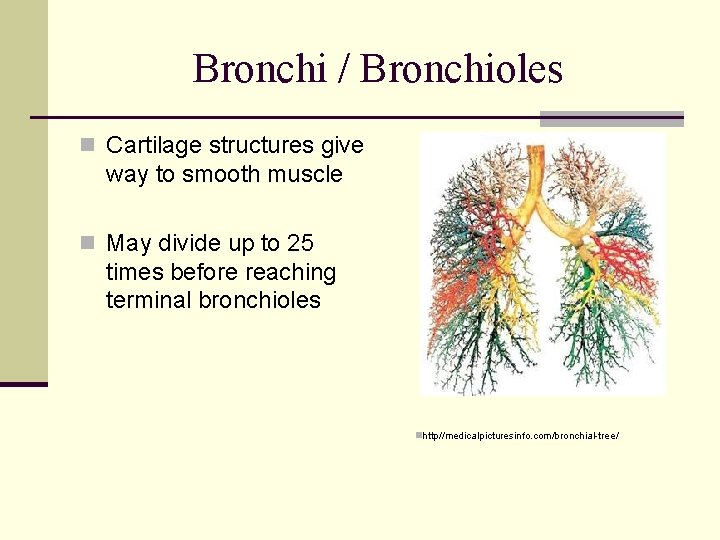
Bronchi / Bronchioles n Cartilage structures give way to smooth muscle n May divide up to 25 times before reaching terminal bronchioles nhttp//medicalpicturesinfo. com/bronchial-tree/
Alveoli n Expand contract with breathing n Contact with pulmonary capillary beds for gas exchange n Inside surface coated with surfactant Prevents aveoli from sticking together n Keeps alveoli open n n Atelectasis
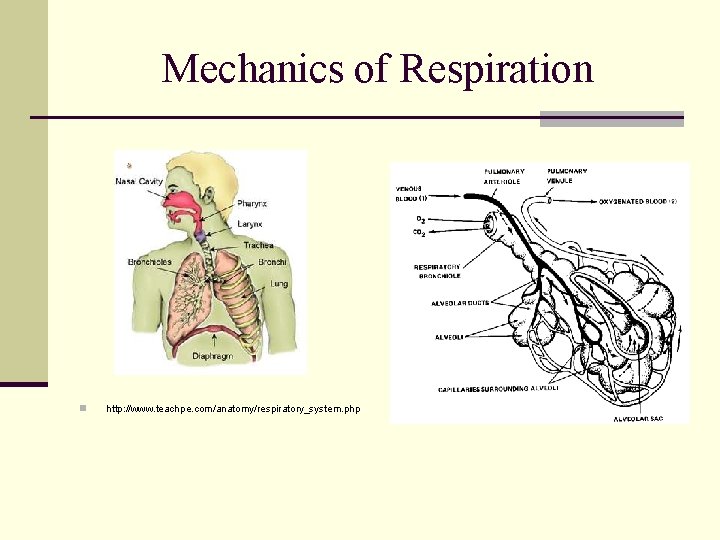
Mechanics of Respiration n http: //www. teachpe. com/anatomy/respiratory_system. php
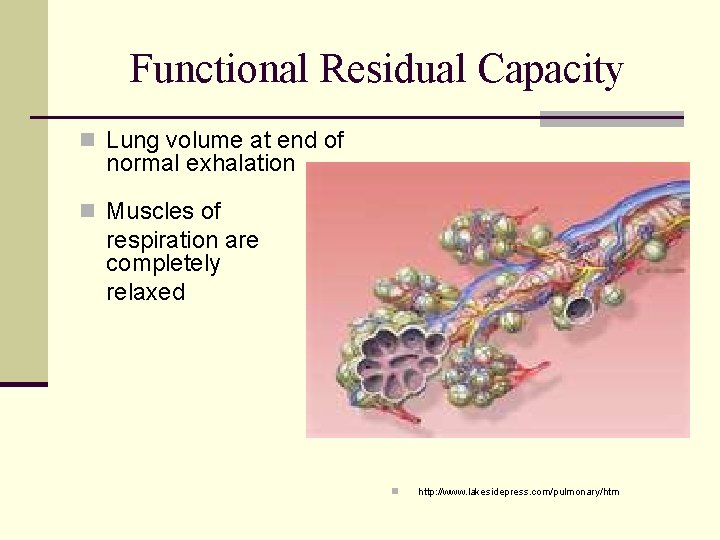
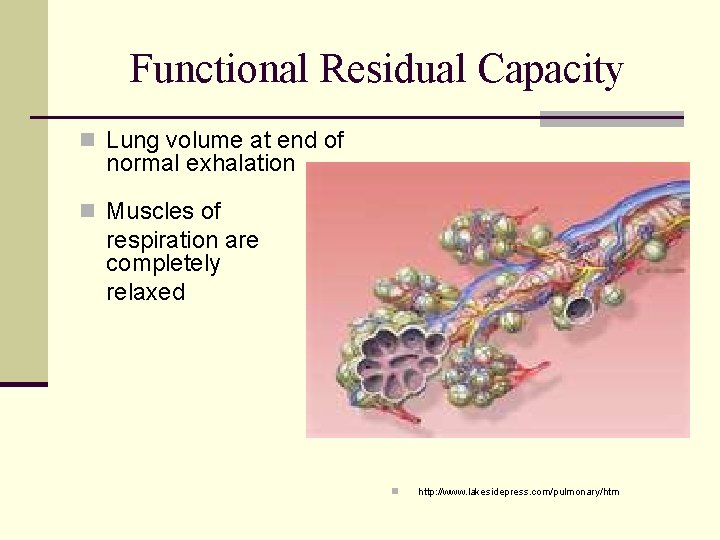
Functional Residual Capacity n Lung volume at end of normal exhalation n Muscles of respiration are completely relaxed n http: //www. lakesidepress. com/pulmonary/htm
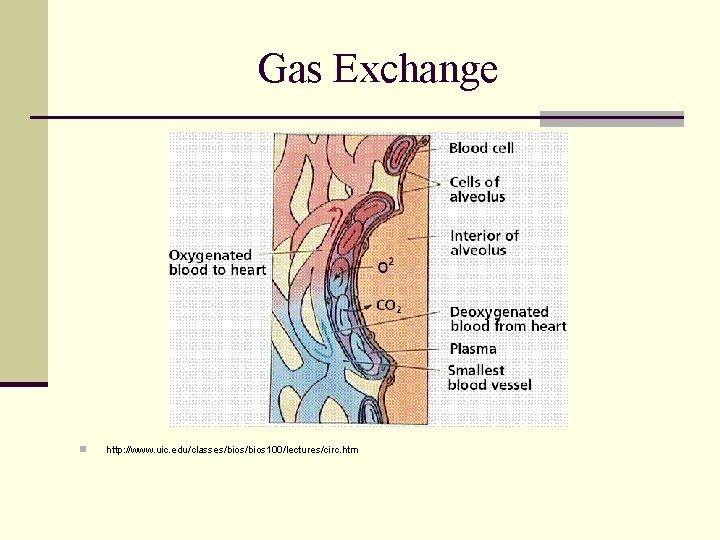
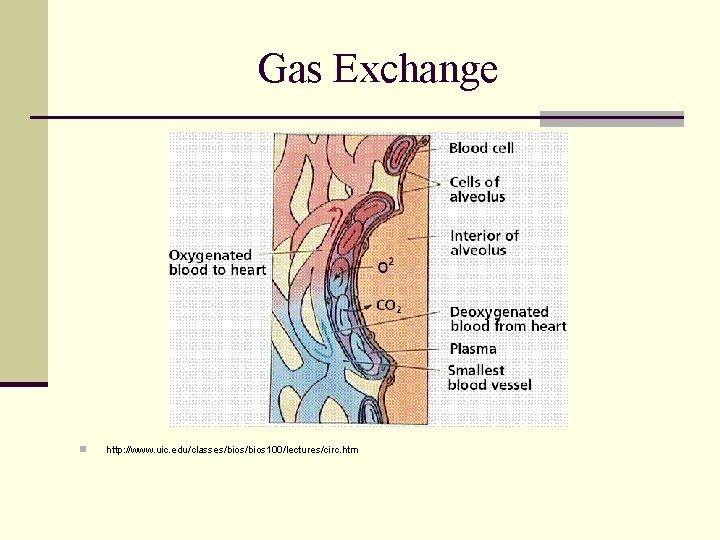
Gas Exchange n http: //www. uic. edu/classes/bios 100/lectures/circ. htm
Oxygenation n Process of getting oxygen to end organs and tissues Inhaled through lungs n Picked up from alveoli on RBCs n Off-loaded in exchange for CO 2 n n Measured by pulse oximetry (Sp. O 2)
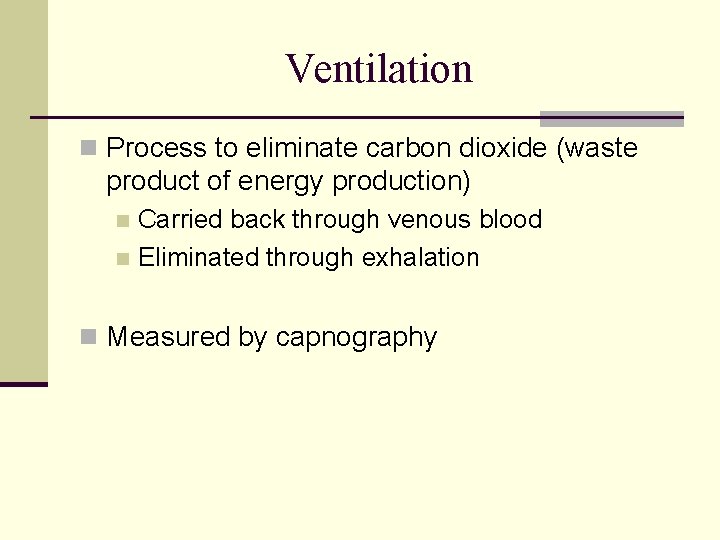
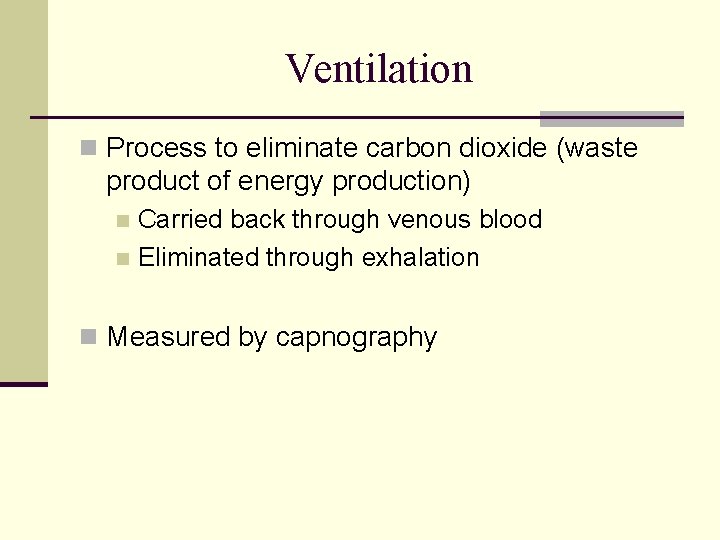
Ventilation n Process to eliminate carbon dioxide (waste product of energy production) Carried back through venous blood n Eliminated through exhalation n n Measured by capnography
Capnography n The capnogram wave form begins before exhalation and ends with inspiration. Exhalation comes before inhalation n http: //www. lusotech. com. br/catalogo/continuous-waveform-capnography
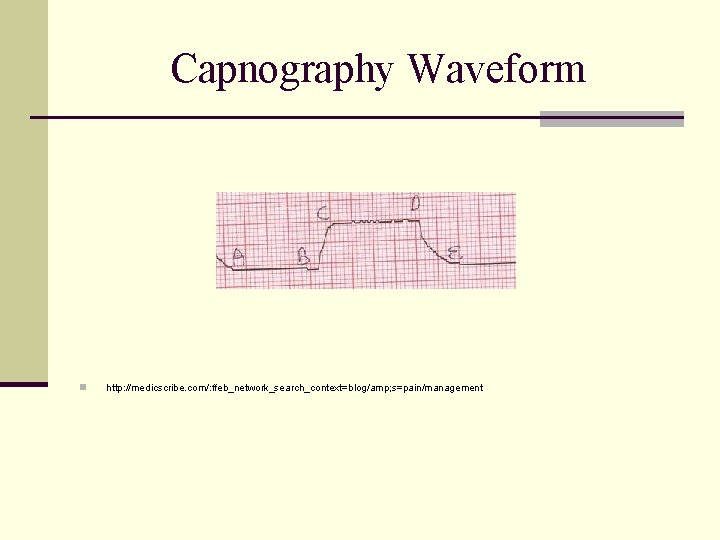
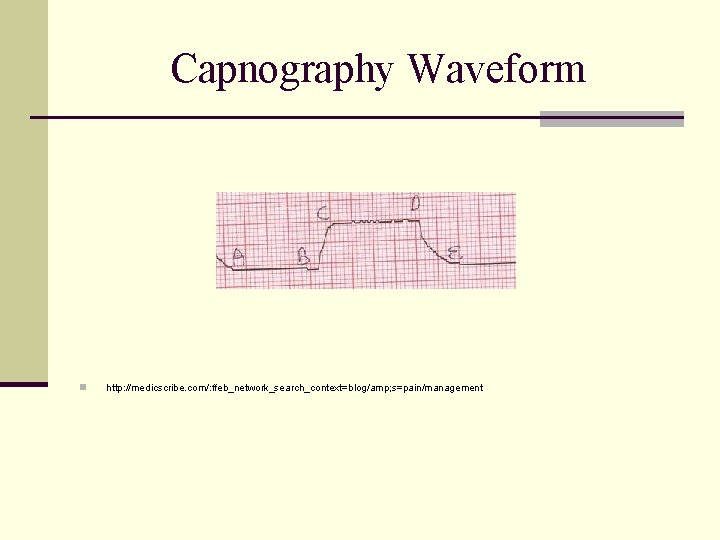
Capnography Waveform n http: //medicscribe. com/: ffeb_network_search_context=blog/amp; s=pain/management
Respiratory Disorders
Respiratory Disorders A combination of many disease processes responsible for emergencies related to ventilation, diffusion and perfusion.
Respiratory Distress n Subjective indication of some degree of difficulty breathing n Causes n n n Upper or lower airway obstruction Inadequate ventilation Impaired respiratory muscle function Impaired nervous system Trauma Bronchitis, pneumonia, cancer
Respiratory Failure n Clinical state of inadequate oxygenation, ventilation or both. n Often end-stage of respiratory distress n Signs: n n n n Tachypnea (early) Bradypnea or apnea (late) Increased, decreased, or no respiratory effort Tachycardia (early) Bradycardia (late) Cyanosis Altered Mental Status
Mechanism of Heart Failure n Frequently a chronic, yet manageable condition n Left ventricle fails to work as effective pump n Blood volume backs up into pulmonary circulation n Most often caused by: n n Volume overload Pressure overload Loss of myocardial tissue Impaired contractility
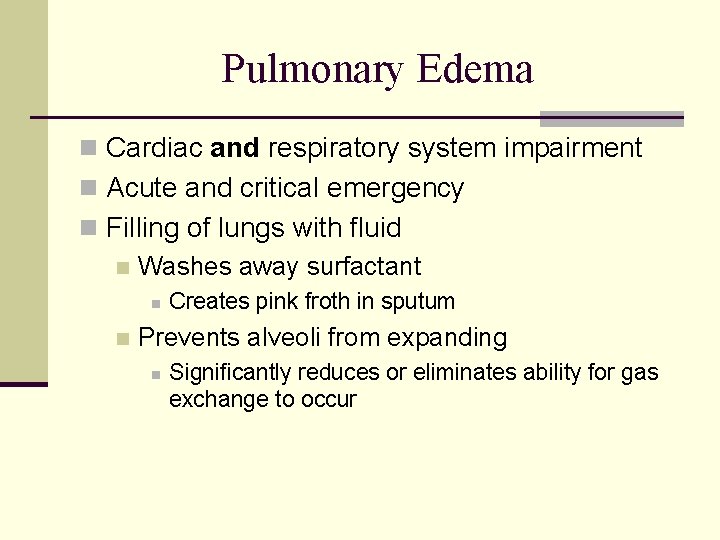
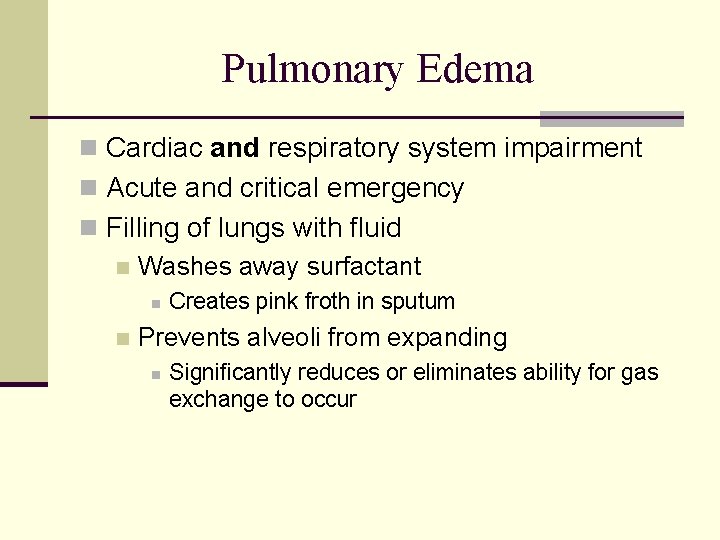
Pulmonary Edema n Cardiac and respiratory system impairment n Acute and critical emergency n Filling of lungs with fluid n Washes away surfactant n n Creates pink froth in sputum Prevents alveoli from expanding n Significantly reduces or eliminates ability for gas exchange to occur
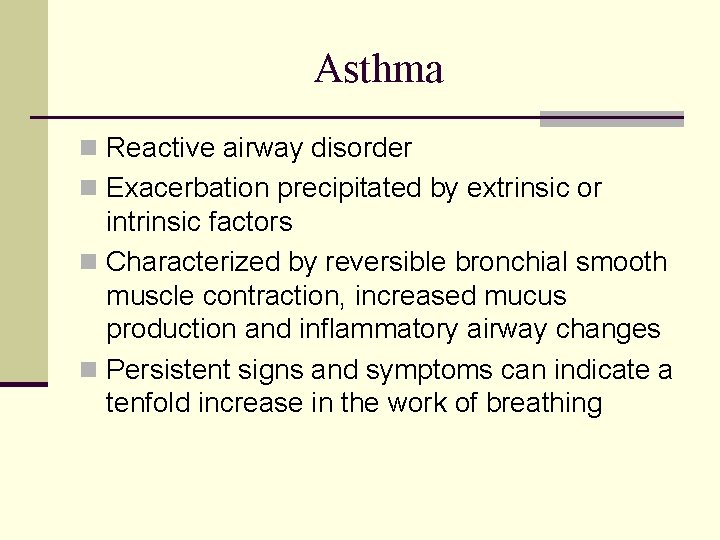
Asthma n Reactive airway disorder n Exacerbation precipitated by extrinsic or intrinsic factors n Characterized by reversible bronchial smooth muscle contraction, increased mucus production and inflammatory airway changes n Persistent signs and symptoms can indicate a tenfold increase in the work of breathing
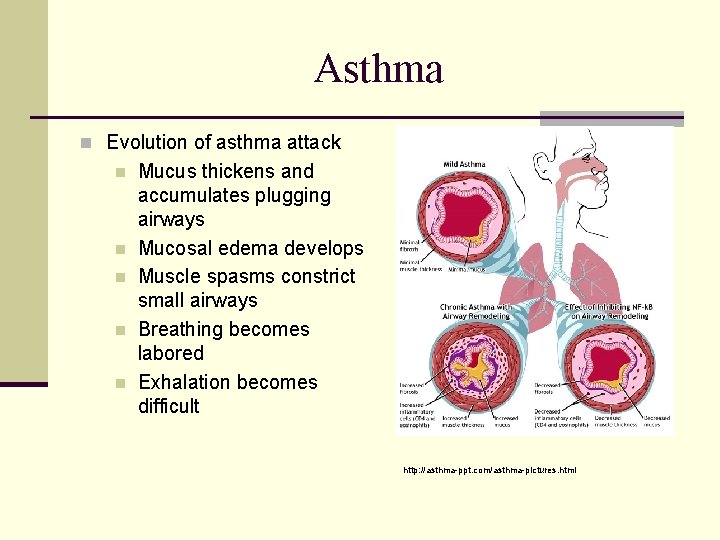
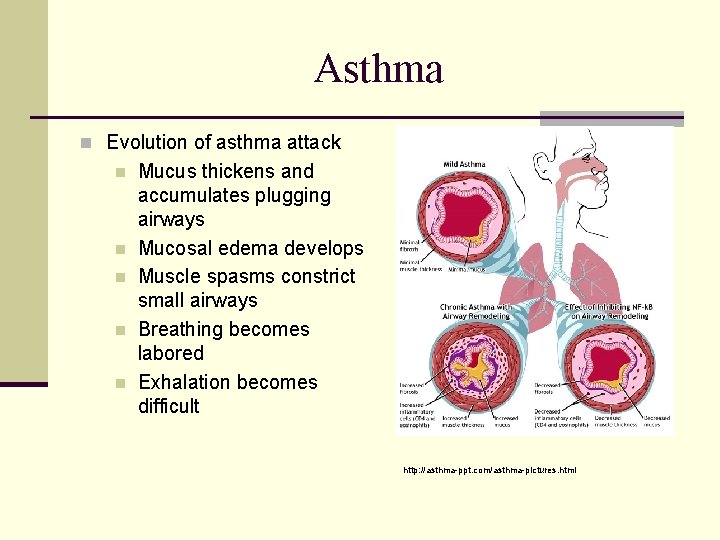
Asthma n Evolution of asthma attack n n n Mucus thickens and accumulates plugging airways Mucosal edema develops Muscle spasms constrict small airways Breathing becomes labored Exhalation becomes difficult http: //asthma-ppt. com/asthma-pictures. html
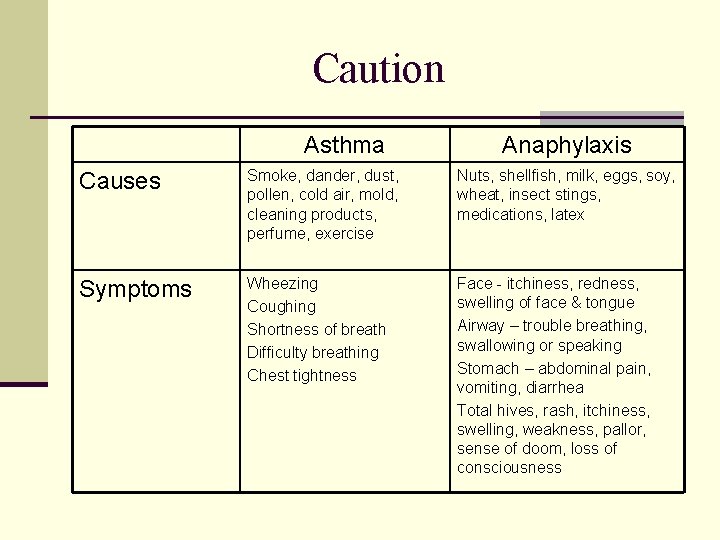
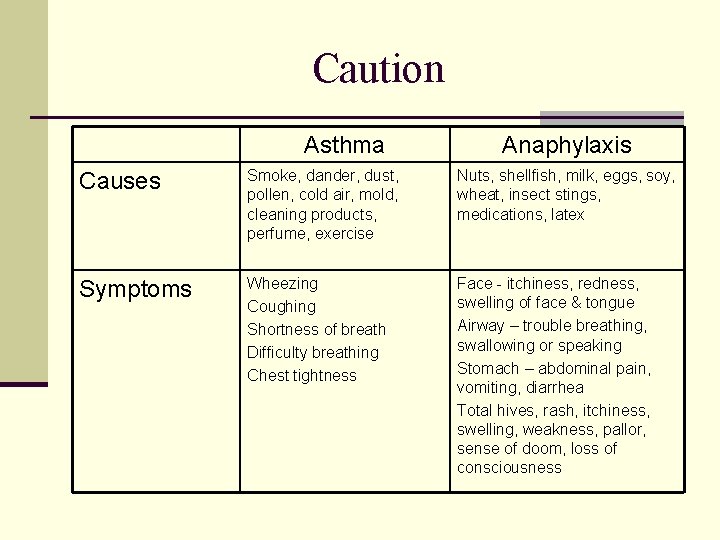
Caution Asthma Anaphylaxis Causes Smoke, dander, dust, pollen, cold air, mold, cleaning products, perfume, exercise Nuts, shellfish, milk, eggs, soy, wheat, insect stings, medications, latex Symptoms Wheezing Coughing Shortness of breath Difficulty breathing Chest tightness Face - itchiness, redness, swelling of face & tongue Airway – trouble breathing, swallowing or speaking Stomach – abdominal pain, vomiting, diarrhea Total hives, rash, itchiness, swelling, weakness, pallor, sense of doom, loss of consciousness
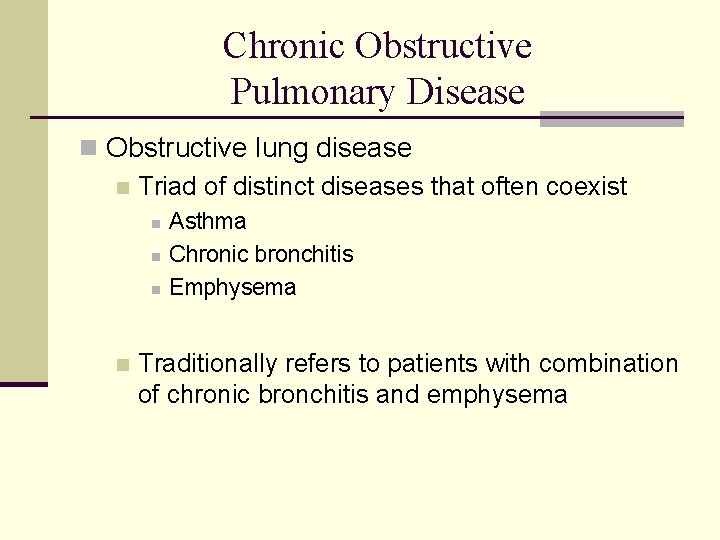
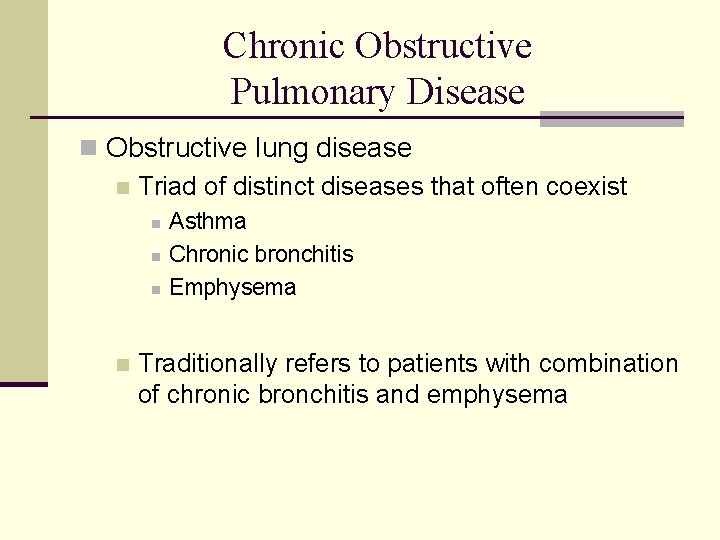
Chronic Obstructive Pulmonary Disease n Obstructive lung disease n Triad of distinct diseases that often coexist n n Asthma Chronic bronchitis Emphysema Traditionally refers to patients with combination of chronic bronchitis and emphysema
Chronic Bronchitis n Bronchi become filled with excessive mucus n Alveoli are not affected n Diffusion of gas remains relatively normal n Patients develop low oxygen pressures (PO 2) and hypoventilation n Hypoventilation leads to high levels of CO 2 and low levels of O 2
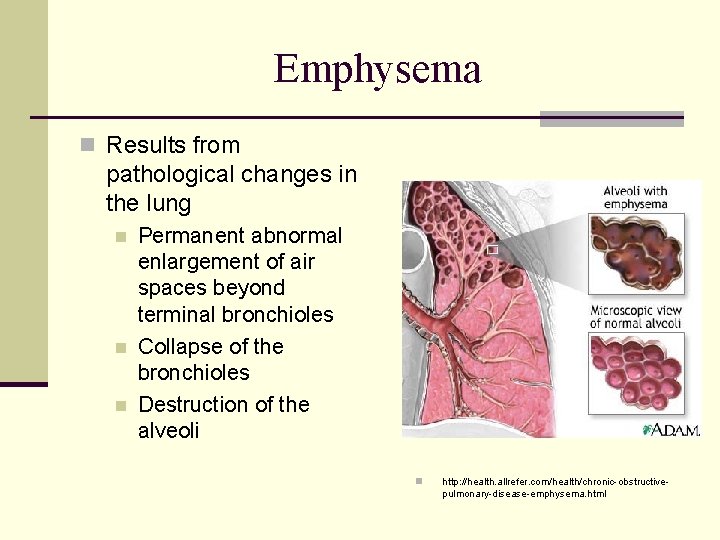
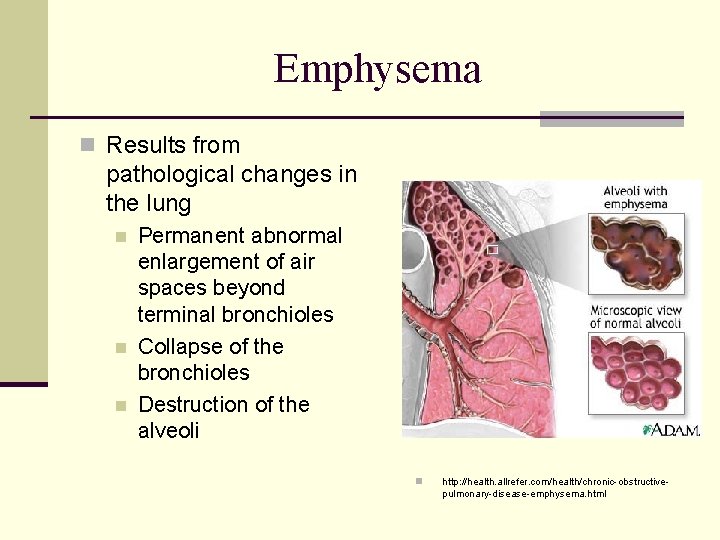
Emphysema n Results from pathological changes in the lung n n n Permanent abnormal enlargement of air spaces beyond terminal bronchioles Collapse of the bronchioles Destruction of the alveoli n http: //health. allrefer. com/health/chronic-obstructivepulmonary-disease-emphysema. html
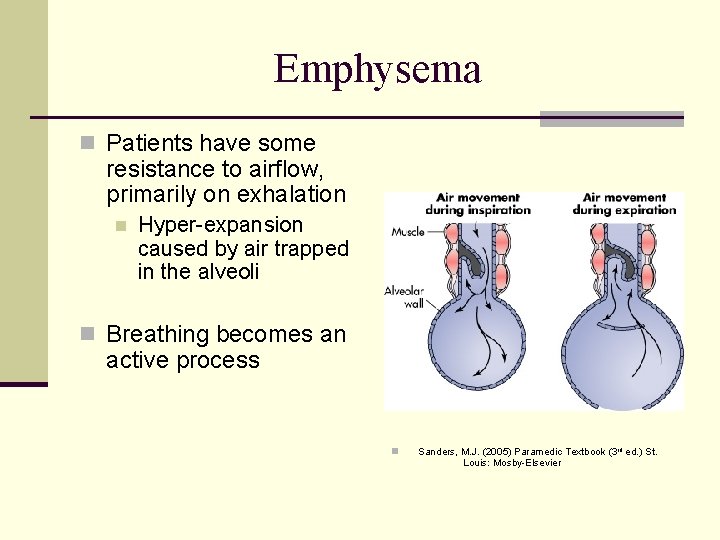
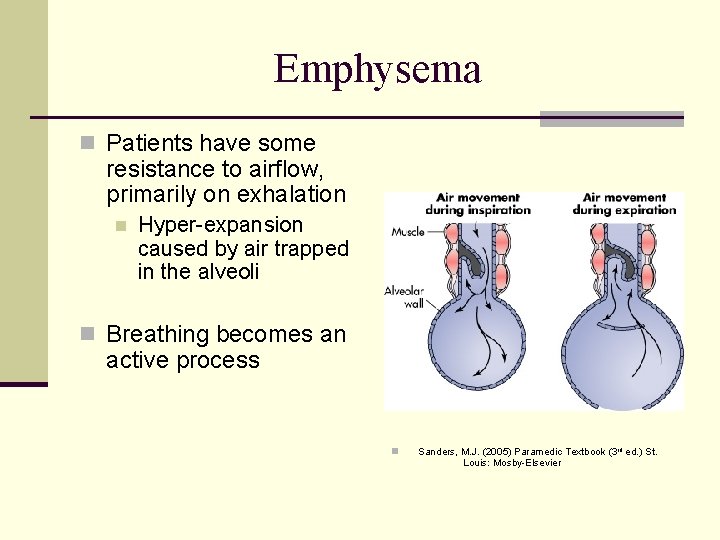
Emphysema n Patients have some resistance to airflow, primarily on exhalation n Hyper-expansion caused by air trapped in the alveoli n Breathing becomes an active process n Sanders, M. J. (2005) Paramedic Textbook (3 rd ed. ) St. Louis: Mosby-Elsevier
Emphysema n Bleb formation n Risk of pneumothorax n Interior airway pressure n CO 2 Retention n Potential worsening with CPAP
Continuous Positive Airway Pressure
The use of CPAP prehospitally reduces the need for intubation by 30% and reduces mortality by 20% n Annals of Emergency Medicine, September 2008
CPAP n Non-invasive ventilation n Continuous O 2 delivered at a set positive pressure throughout the respiratory cycle n www. ems 1. com/cpap-for-ems
Positive Pressure n PUSHES air into the chest n Overcomes airway resistance Bag valve mask n Demand valve n Intubation / mechanical ventilation n CPAP n
Effects of CPAP n Increases functional residual capacity n Increases alveolar surface area available for gas exchange n Increases oxygen diffusion across alveolar membranes n Reduced work of breathing
How CPAP Works n Maintains constant level of airway pressure n Keeps alveoli open (asthma, COPD) n Moves fluid into vasculature (pulmonary edema) n Improves gas exchange n Buys time for medications to work
Indications n Severe Respiratory Distress / Respiratory Failure Accessory muscle use? n Persistent hypoxia despite appropriate / aggressive oxygen therapy? n Marked increased work of breathing? n Inability to speak full sentences? n n Differentiate Pulmonary Edema versus other Respiratory Disorder
Contraindications n Respiratory rate < 10 breaths / minute n Systolic blood pressure < 100 mm. Hg n Confusion n Inability to understand directions and cooperate with application of CPAP n History of pneumothorax n History of recent tracheo-bronchial surgery n Active nausea or vomiting n Despite antiemetic therapy by paramedics
Limitations n CPAP is not a mechanical ventilator n Tight mask seal can create claustrophobic response n Consider allowing patient to self-seal (hold own mask) until initial benefits recognized n CPAP is powered by on-board oxygen supply
Oxygen Utilization Oxygen Demand
Summary Pre-hospital studies have proven the effectiveness of CPAP in treating patients with severe respiratory distress, regardless of disease process.
ANY QUESTIONS
Special Thanks To: Peter Canning for time and effort in initial development of program David Bailey for contributions of supplemental information to enhance presentation Richard Sanders for development of glossary of terms Nancy Brunet for final project coordination
Placeholder n Add specific manufacturer product information and local concerns
Practical Skills Session