Contents Classification HT In Pregnancy Pathogenesis and Risk
- Slides: 32
Contents Classification HT In Pregnancy Pathogenesis and Risk factors Diagnosis Prediction and prevention Management
Introduction v Hypertensive disorders of pregnancy remain a major health issue for women and their infants worldwide v The ACOG convened a task force of experts in the management of HT in pregnancy to review available data and publish evidence-based recommendations for clinical practice v Preclampsia is a dynamic process, by nature is progressive
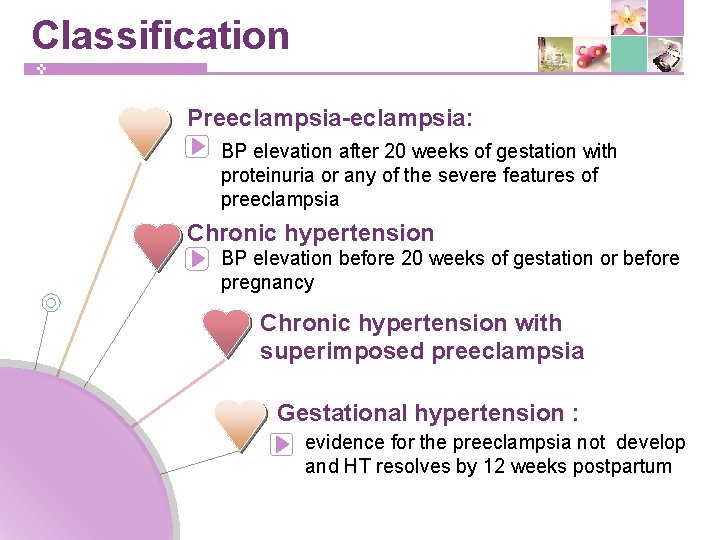
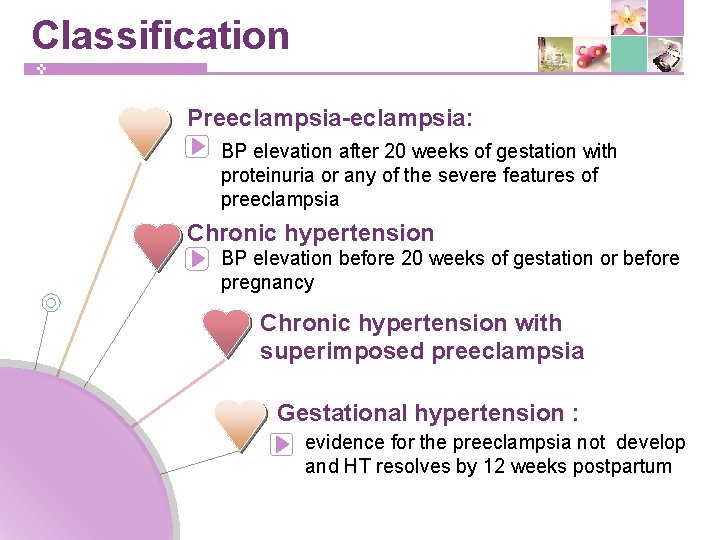
Classification Preeclampsia-eclampsia: BP elevation after 20 weeks of gestation with proteinuria or any of the severe features of preeclampsia Chronic hypertension BP elevation before 20 weeks of gestation or before pregnancy Chronic hypertension with superimposed preeclampsia Gestational hypertension : evidence for the preeclampsia not develop and HT resolves by 12 weeks postpartum
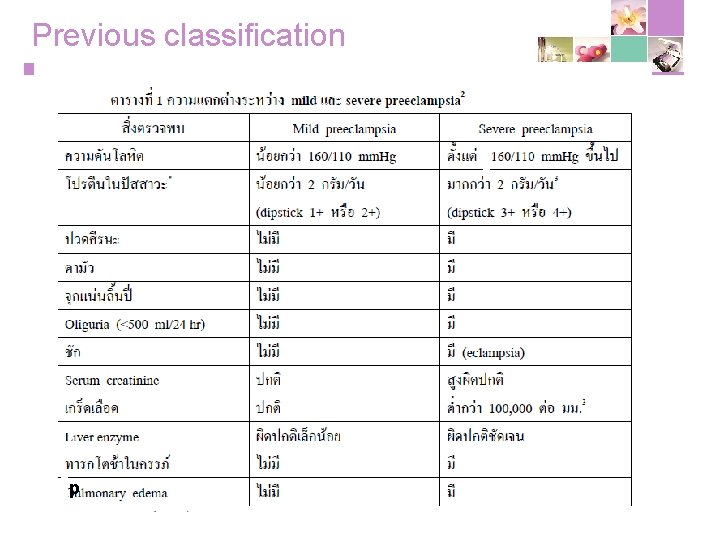
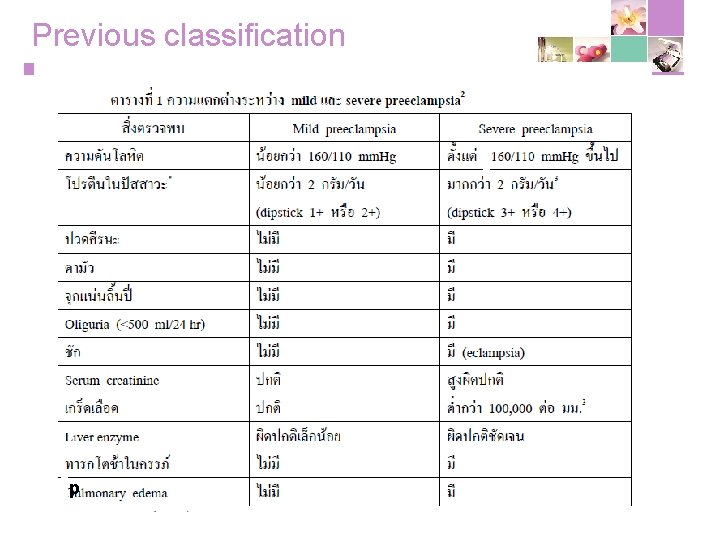
Previous classification p
Classification Avoid use of term mild preeclampsia >> replace with preeclampsia without severe features Severe preeclampsia >> preeclampsia with severe features
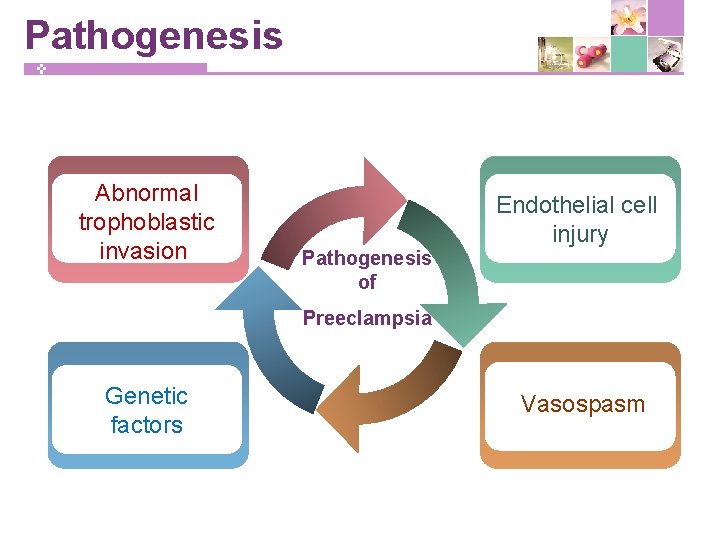
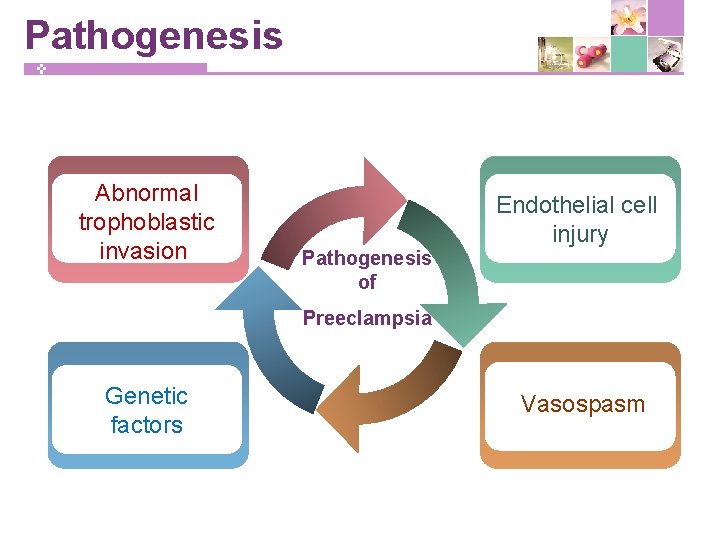
Pathogenesis Abnormal trophoblastic invasion Endothelial cell injury Pathogenesis of Preeclampsia Genetic factors Vasospasm
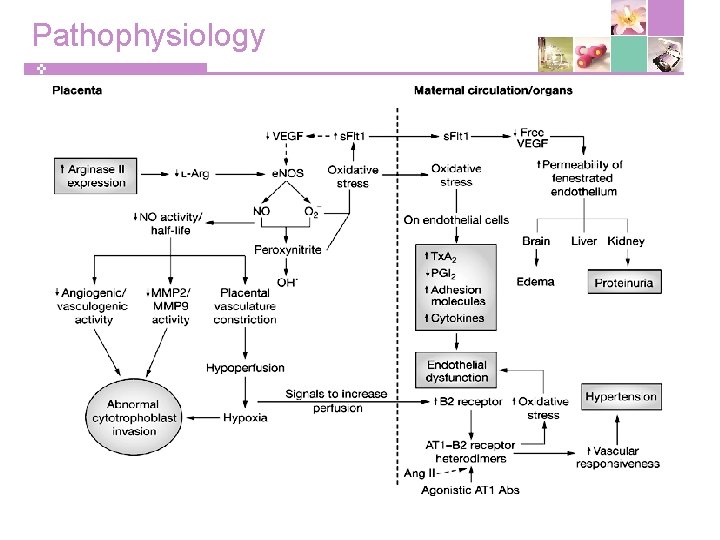
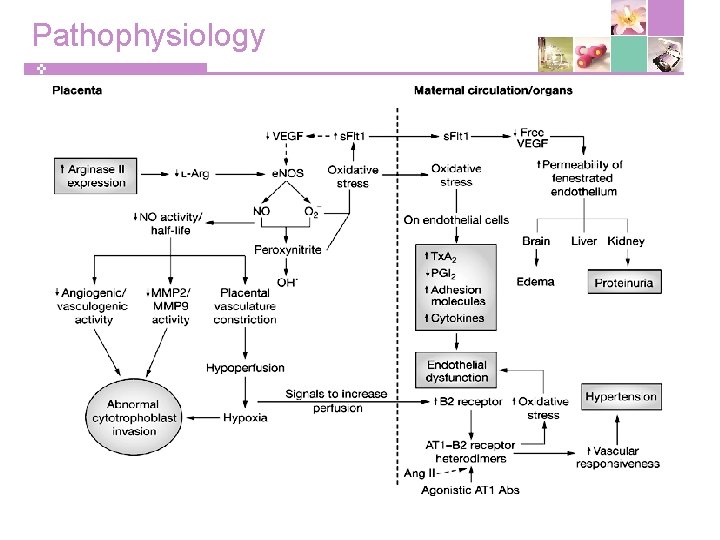
Pathophysiology
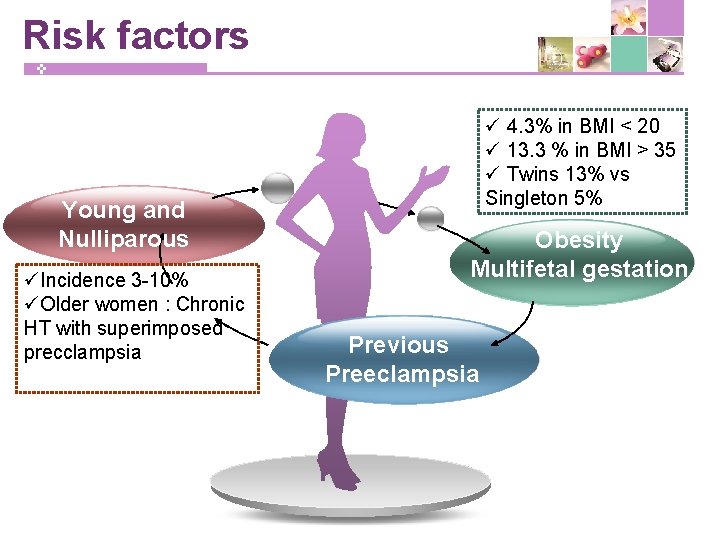
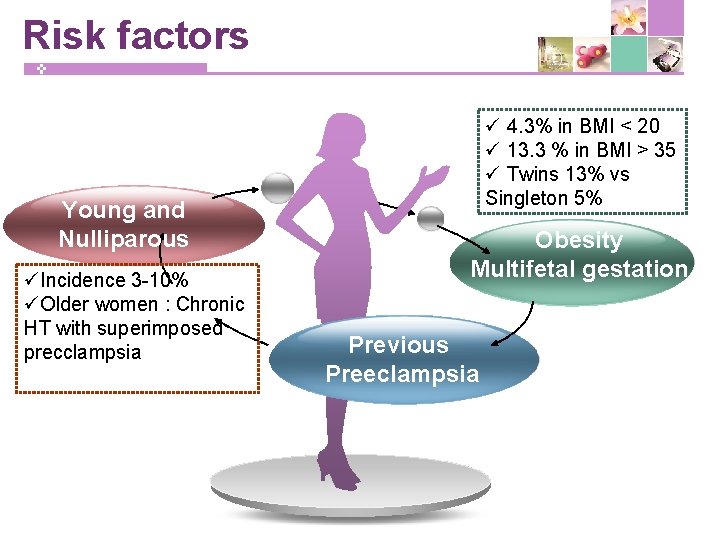
Risk factors Young and Nulliparous üIncidence 3 -10% üOlder women : Chronic HT with superimposed precclampsia ü 4. 3% in BMI < 20 ü 13. 3 % in BMI > 35 ü Twins 13% vs Singleton 5% Obesity Multifetal gestation Previous Preeclampsia
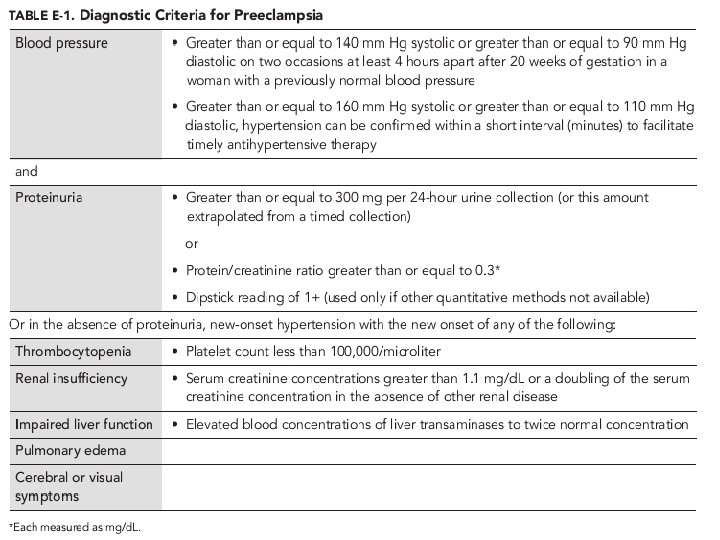
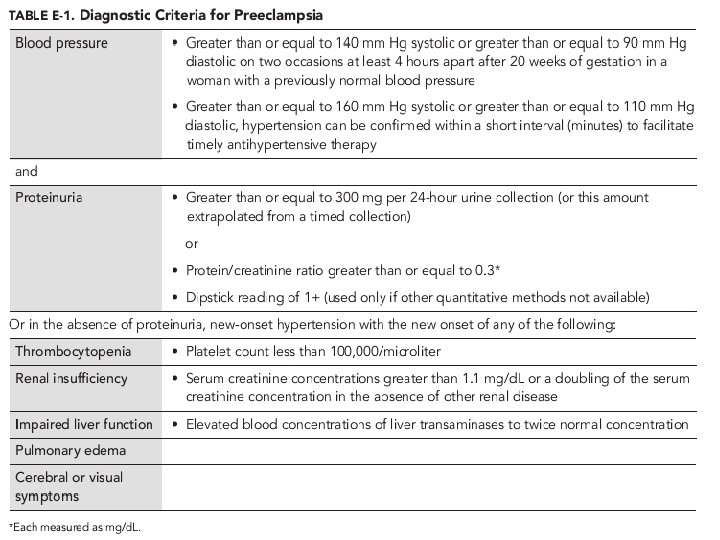
Diagnosis : Preeclampsia
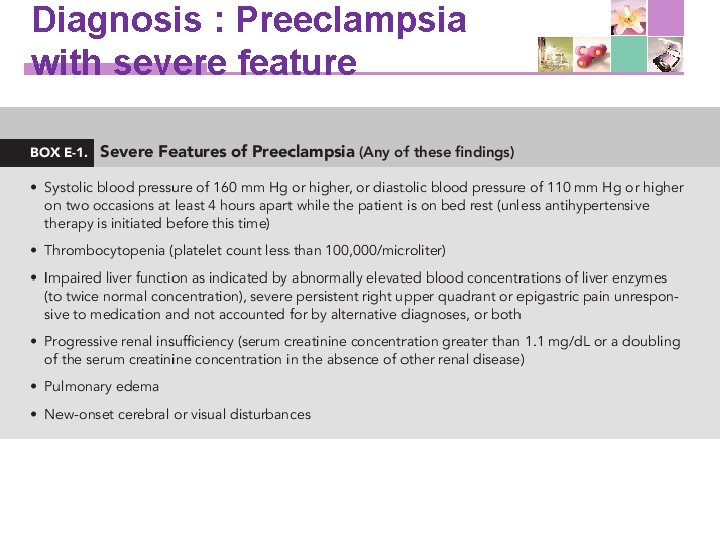
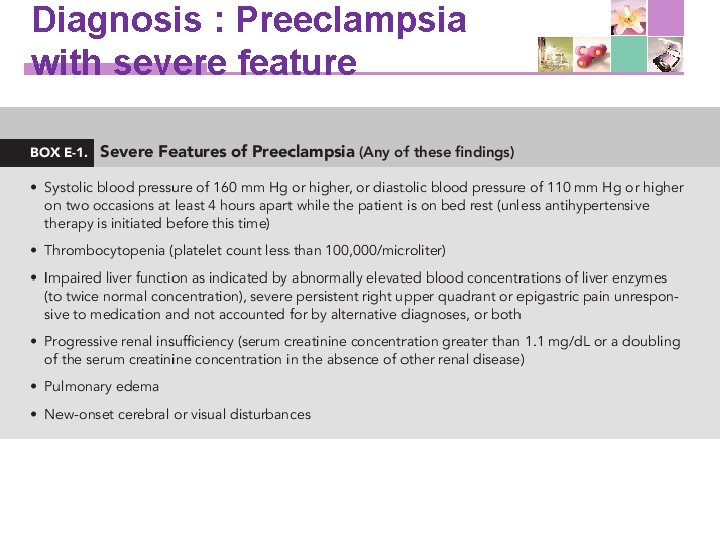
Diagnosis : Preeclampsia with severe feature
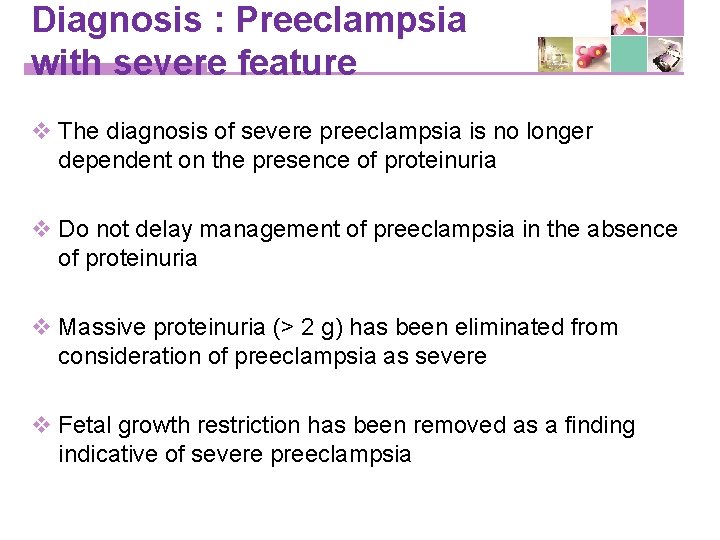
Diagnosis : Preeclampsia with severe feature v The diagnosis of severe preeclampsia is no longer dependent on the presence of proteinuria v Do not delay management of preeclampsia in the absence of proteinuria v Massive proteinuria (> 2 g) has been eliminated from consideration of preeclampsia as severe v Fetal growth restriction has been removed as a finding indicative of severe preeclampsia
Prediction of preeclampsia v Screening to predict preeclampsia beyond obtaining an appropriate medical history to evaluate for risk factors is not recommended TVS of a cervix and funneling
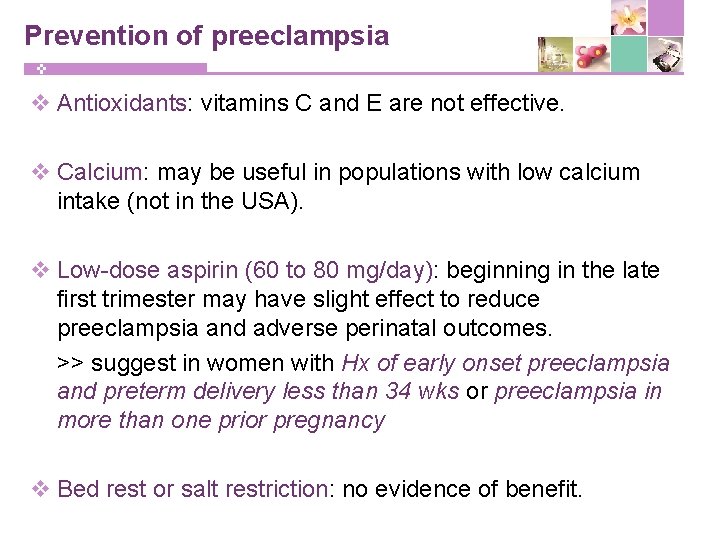
Prevention of preeclampsia v Antioxidants: vitamins C and E are not effective. v Calcium: may be useful in populations with low calcium intake (not in the USA). v Low-dose aspirin (60 to 80 mg/day): beginning in the late first trimester may have slight effect to reduce preeclampsia and adverse perinatal outcomes. >> suggest in women with Hx of early onset preeclampsia and preterm delivery less than 34 wks or preeclampsia in more than one prior pregnancy TVS of a cervix and funneling v Bed rest or salt restriction: no evidence of benefit.
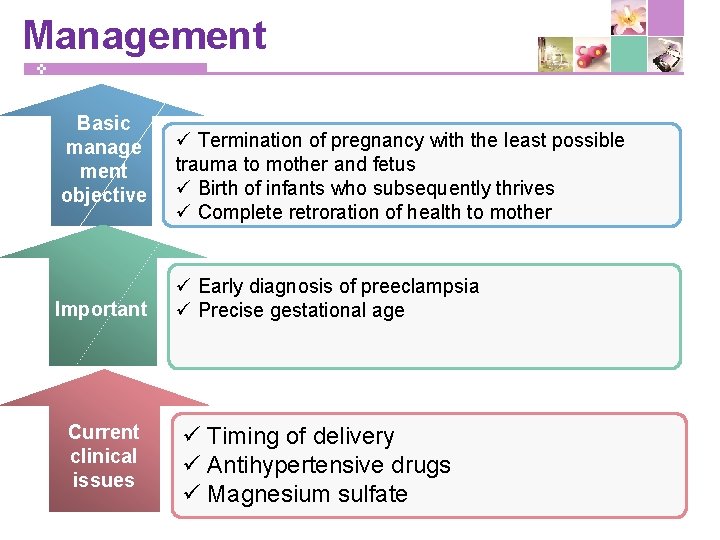
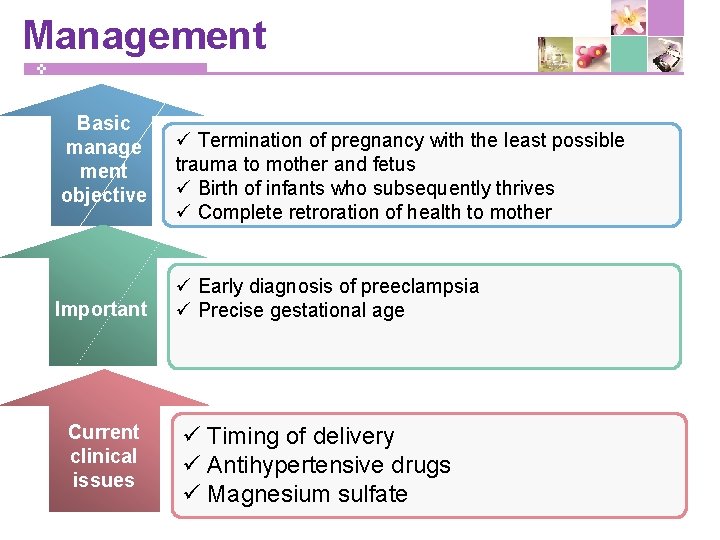
Management Basic manage ment objective Important Current clinical issues ü Termination of pregnancy with the least possible trauma to mother and fetus ü Birth of infants who subsequently thrives ü Complete retroration of health to mother ü Early diagnosis of preeclampsia ü Precise gestational age ü Timing of delivery ü Antihypertensive drugs ü Magnesium sulfate
Management v Hospitalization for women with new onset HT § Daily assessment of maternal symptoms, weight gain and fetal movement § Analysis for proteinuria § BP every 4 hours § Measurement of serum Cr, Hepatic enzymes, CBC (some recommend uric acid, LDH, coagulogram) § Evaluation of fetal size, amniotic volume, wellbeing
Management v Timing of delivery : § Preeclampsia without severe features; 37 weeks § Severe preeclampsia ; • < 34 weeks of gestation with stable maternal and fetal conditions, it is recommended that continued pregnancy be undertaken only at facilities with adequate maternal and neonatal intensive care resources • ≥ 34 weeks of gestation, and in those with unstable maternal or fetal conditions irrespective of gestational age, delivery soon after maternal stabilization is recommended § Chronic hypertension; 38 weeks
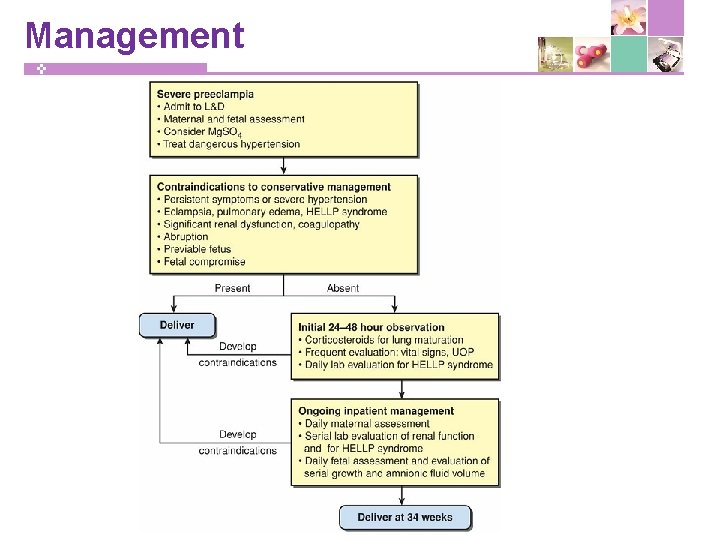
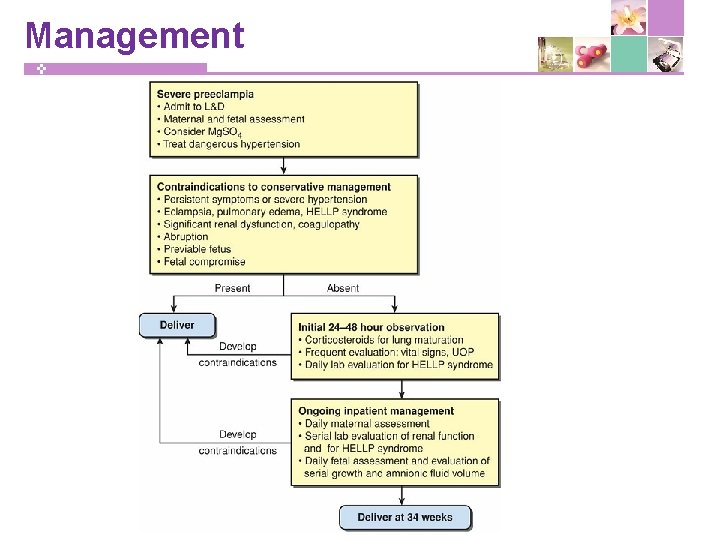
Management
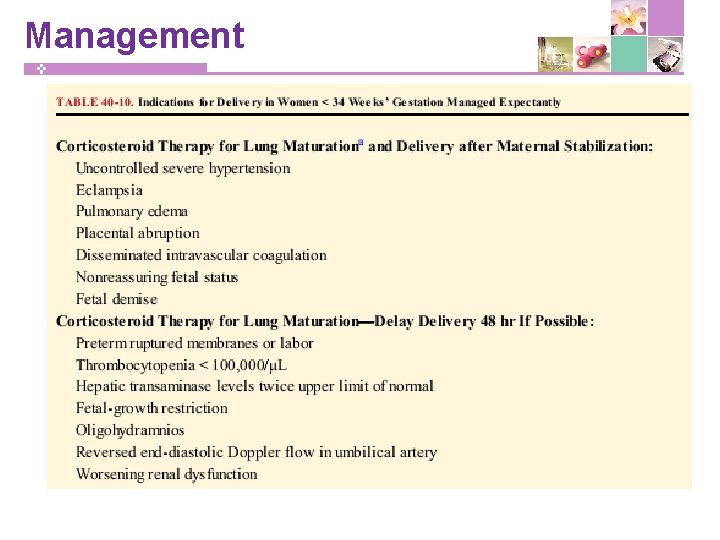
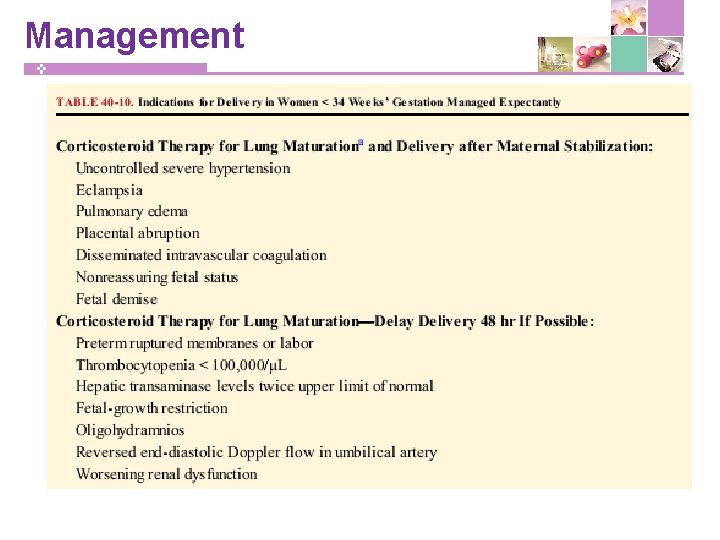
Management
Management v Antihypertensive drugs ; § preeclampsia with severe hypertension during pregnancy (sustained systolic BP of at least 160 or diastolic of at least 110) § persistent chronic hypertension with systolic BP of at least 160 or diastolic BP of at least 105
Management v Antihypertensive drugs ; § IV labetalol • bolus doses 20 -40 mg (max 300/hr) • continuous IV infusion (1 -2 mg/min) § IV bolus doses of hydralazine • 5, 10 mg q 20 min (max 25 mg) § Oral nifedipine • 10 -20 mg q 20 min (max 60 mg) § IV Sodium nitroprusside
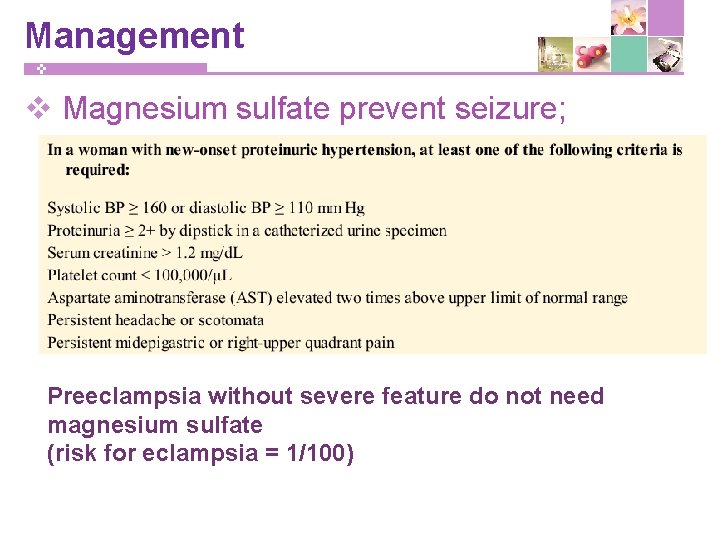
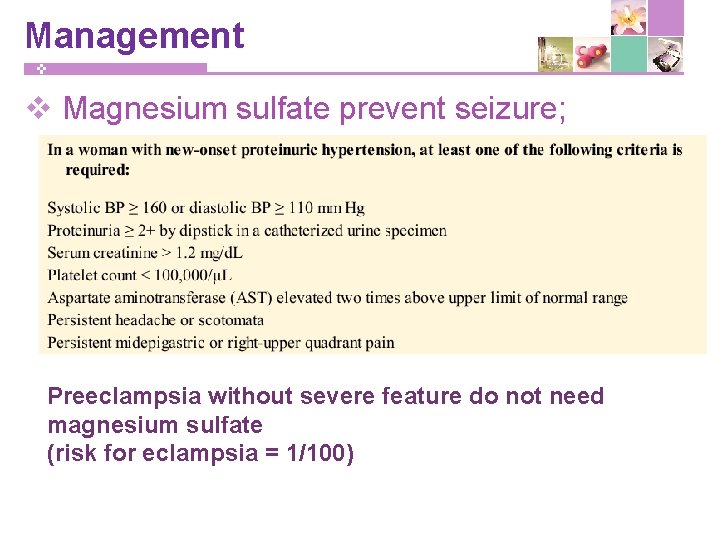
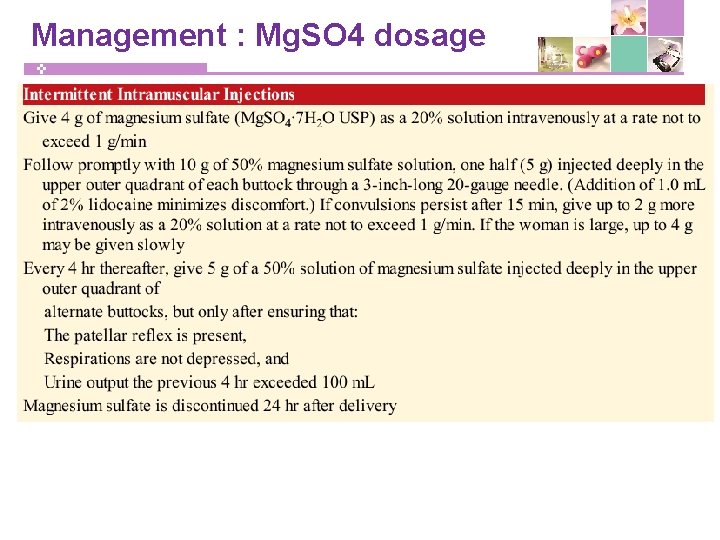
Management v Magnesium sulfate prevent seizure; Preeclampsia without severe feature do not need magnesium sulfate (risk for eclampsia = 1/100)
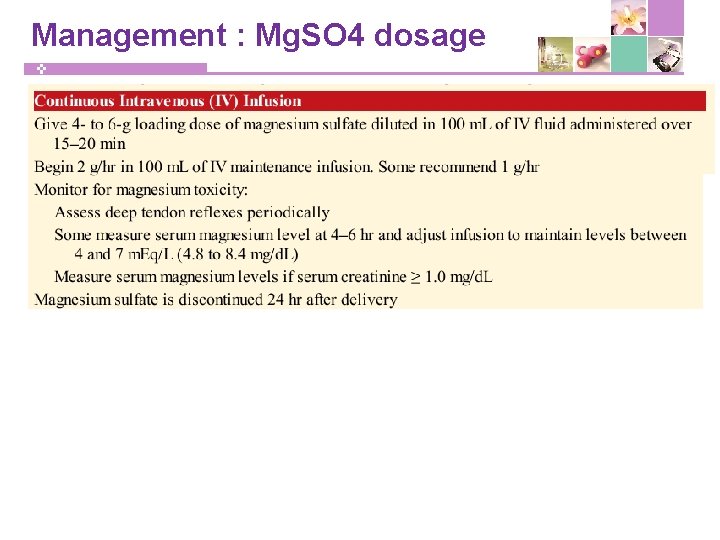
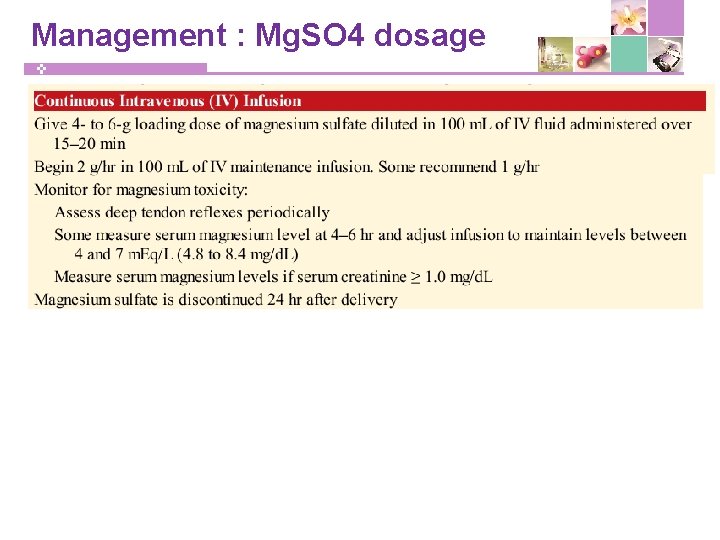
Management : Mg. SO 4 dosage
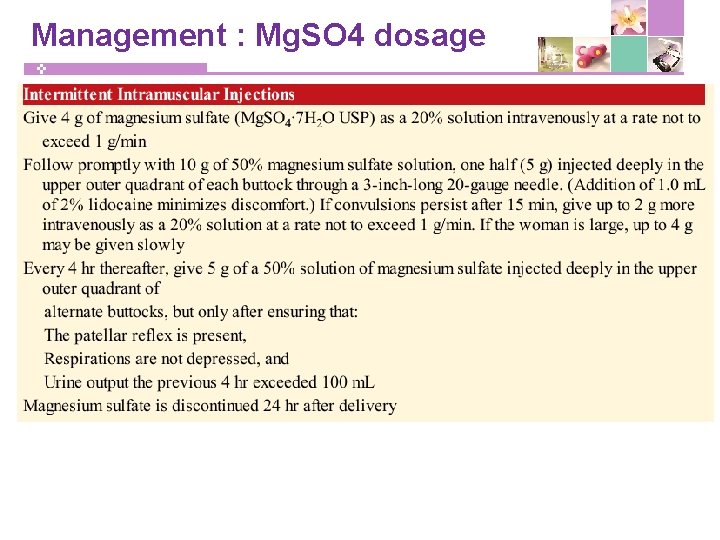
Management : Mg. SO 4 dosage
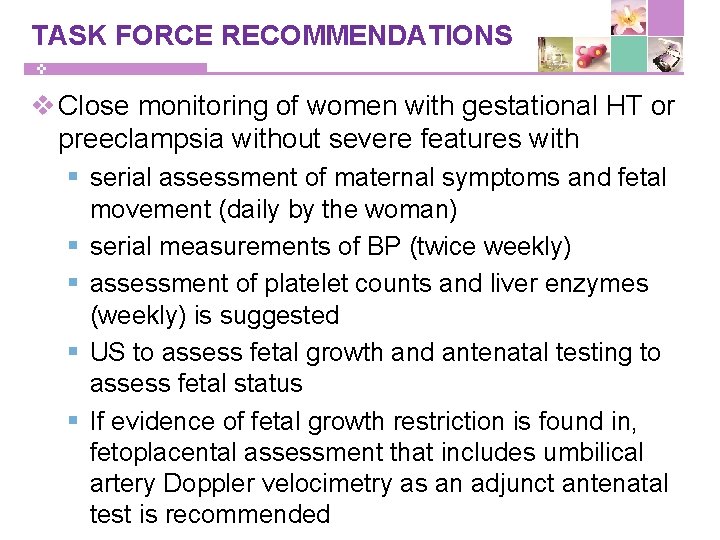
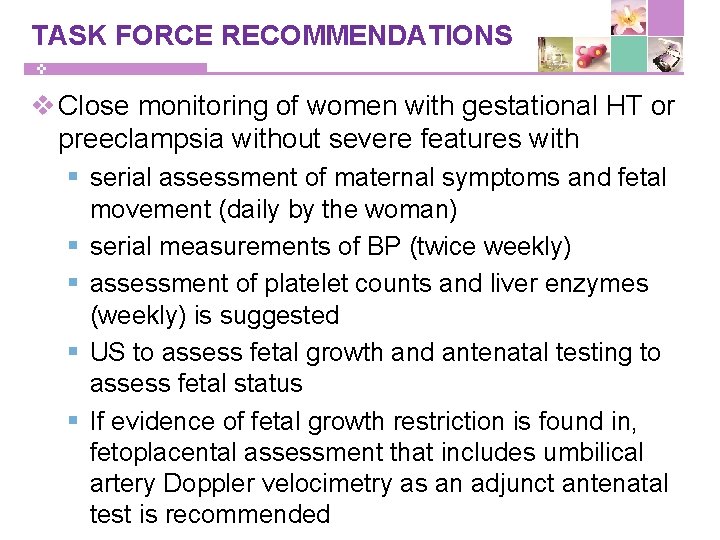
TASK FORCE RECOMMENDATIONS v Close monitoring of women with gestational HT or preeclampsia without severe features with § serial assessment of maternal symptoms and fetal movement (daily by the woman) § serial measurements of BP (twice weekly) § assessment of platelet counts and liver enzymes (weekly) is suggested § US to assess fetal growth and antenatal testing to assess fetal status § If evidence of fetal growth restriction is found in, fetoplacental assessment that includes umbilical artery Doppler velocimetry as an adjunct antenatal test is recommended
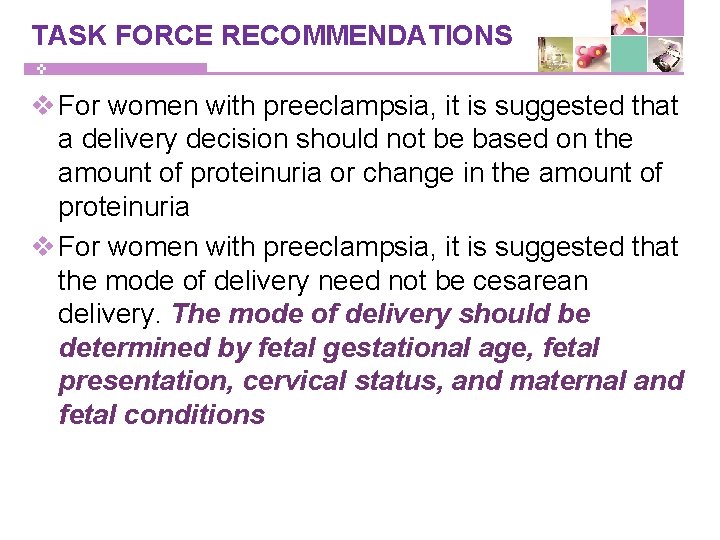
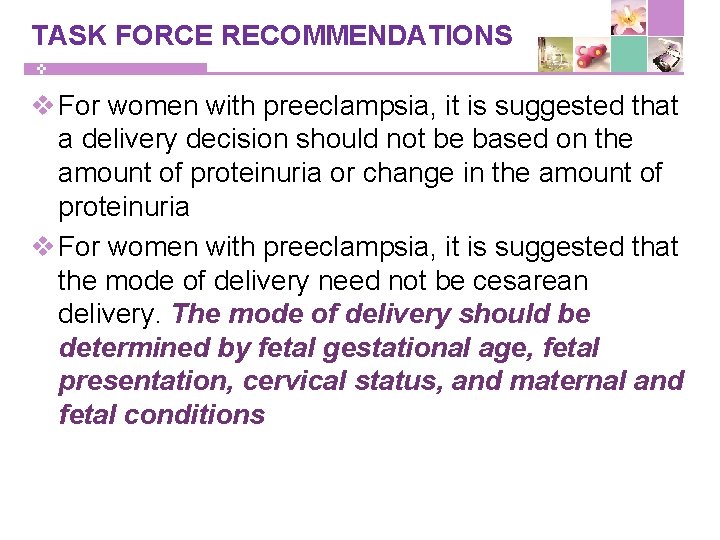
TASK FORCE RECOMMENDATIONS v For women with preeclampsia, it is suggested that a delivery decision should not be based on the amount of proteinuria or change in the amount of proteinuria v For women with preeclampsia, it is suggested that the mode of delivery need not be cesarean delivery. The mode of delivery should be determined by fetal gestational age, fetal presentation, cervical status, and maternal and fetal conditions
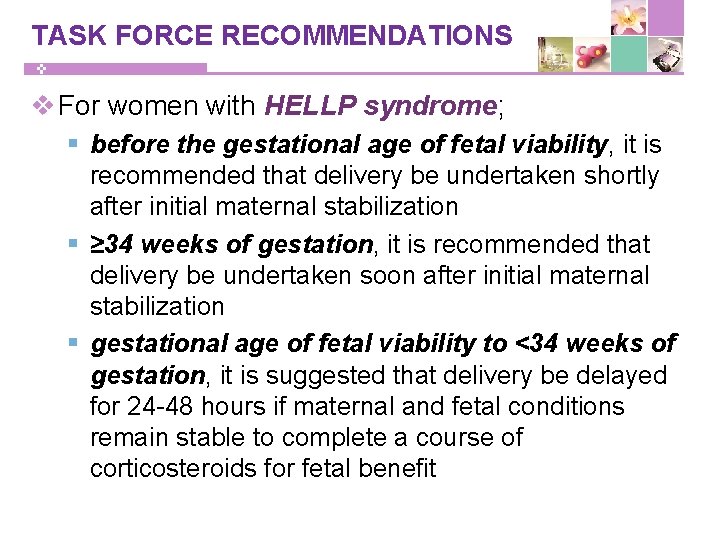
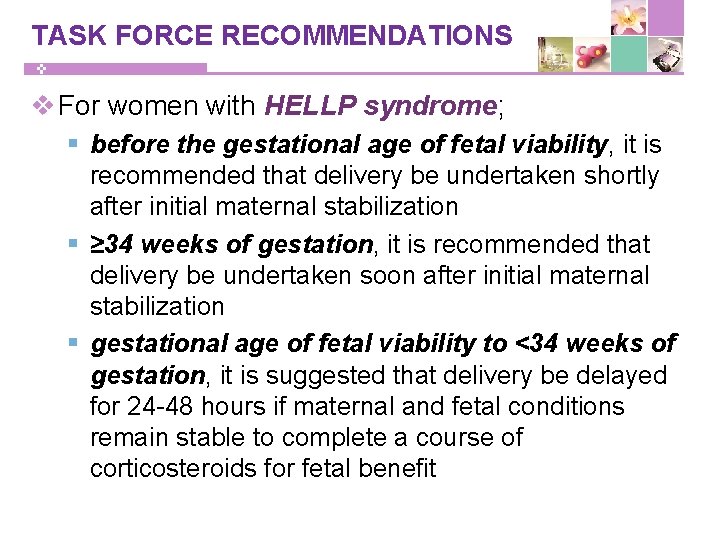
TASK FORCE RECOMMENDATIONS v For women with HELLP syndrome; § before the gestational age of fetal viability, it is recommended that delivery be undertaken shortly after initial maternal stabilization § ≥ 34 weeks of gestation, it is recommended that delivery be undertaken soon after initial maternal stabilization § gestational age of fetal viability to <34 weeks of gestation, it is suggested that delivery be delayed for 24 -48 hours if maternal and fetal conditions remain stable to complete a course of corticosteroids for fetal benefit
TASK FORCE RECOMMENDATIONS v Post partum period; § BP be monitored in the hospital or that equivalent outpatient surveillance be performed for at least 72 hours postpartum and again 7 -10 days after delivery or earlier in women with symptoms § discharge instructions include information about the signs and symptoms of preeclampsia as well as the importance of prompt reporting of this information to their health care providers
TASK FORCE RECOMMENDATIONS v Post partum period; § new-onset hypertension associated with headaches or blurred vision or preeclampsia with severe hypertension, the parenteral administration of magnesium sulfate is suggested § persistent postpartum hypertension, BP of 150 systolic or 100 diastolic or higher, on at least two occasions that are at least 4 -6 hours apart, antihypertensive therapy is suggested § Persistent BP of 160 systolic or 110 diastolic or higher should be treated within 1 hour
References v American College of Obstetricians and Gynecologists: Hypertension in pregnancy Executive summary, November 2013 v Williams Obstetrics, 24 ed
COMPANY NAME Thank You For Your Attention !