CONTENTS 1 Definition of normal Labour 2 Factors
CONTENTS 1. Definition of normal Labour 2. Factors influencing progress of Labour 3. Diagnosis of Labour 4. Stages of Labour 5. Management of Labour

LABOUR DEFINITION Labour is defined The onset of regular painful uterine contractions with progressive effacement and dilation of the cervix accompanied by decent of the presenting part leading to expulsion of the fetus or fetuses and placenta from the mother Normal Labour is defined to expel the viable(alive) products of conception
DIAGNOSIS OF LABOUR Signs that can clue into the onset of Labour • Show- evidence by mucus mixed with blood or mucus plug • Rupture of membranes- look for leaking liquor • painful, regular uterine contractions, at least (1: 10)
VAGINAL EXAMINATION Confirm degree of dilatation and effacement Identify the presenting part Fetal head engagement Confirm or artificially rupture if necessary (ROM) Exclude cord prolapse
FACTORS TO HELP DETERMINE IF LABOUR IS NORMAL Mature Fetus 37 -42 weeks Spontaneous expulsion Vertex is the presenting part Vaginal Delivery Time ( not < 3 hour but not >18 hours) Complications? ?
INFLUENTIAL FACTORS OF THE PROGRESS OF LABOUR 5 P’s • THE PASSENGER-Fetal head size, Fetal lie, presentation, attitude, position • THE PASSAGE WAY/PELVIS • THE POWERS • THE PLACENTA • PSYCHOLOGICAL RESPONSE

PHYSIOLOGY OF NORMAL LABOUR POWERS Physiology of normal labour complete into two steps UTERINE CONTRACTION RETRACTION 1. Uterine contraction : During contraction, uterus becomes hard and somewhat pushed anteriorly to make the long axis of the uterus in the line with that of pelvic axis 2. Uterine contraction : Probable cause of pain are a) Myometrial hypoxia during contractions. b) Stretching of the peritoneum over the fundus. c) Stretching of the cervix during dilatation. d) Compression of the nerve ganglion. e) The pain of uterine contractions is distributed along the cutaneous nerve distribution of T 10 to L 1
INTENSITY The intensity gradually increases with advancement of labour until it becomes maximum in the second stage during delivery of the baby. Intrauterine pressure is raised to 40 -50 mm Hg during first stage and about 100 -120 mm Hg in the second stage of labour during contractions.
In the first stage, the contractions last for about 30 second initially but gradually increases in duration with the progress of labour. Thus in the second stage, the contractions last longer than in the first stage. FREQUENCY In the early stage of labour, the contractions come at intervals of ten to fifteen minutes. The intervals gradually shorten with advancement of labour until in the second stage, when it comes every two or three minutes.

Retraction is a phenomenon of the uterus in labour in which the muscle fibers are permanently shortened. Unlike any other muscle of the body, the uterine muscles have this property to become shortened once and for all Contraction is a temporary reduction in length of the fibers, which attain their full length during relaxation. In contrast, retraction results in permanent shortening and the fibers are shortened once and for all.
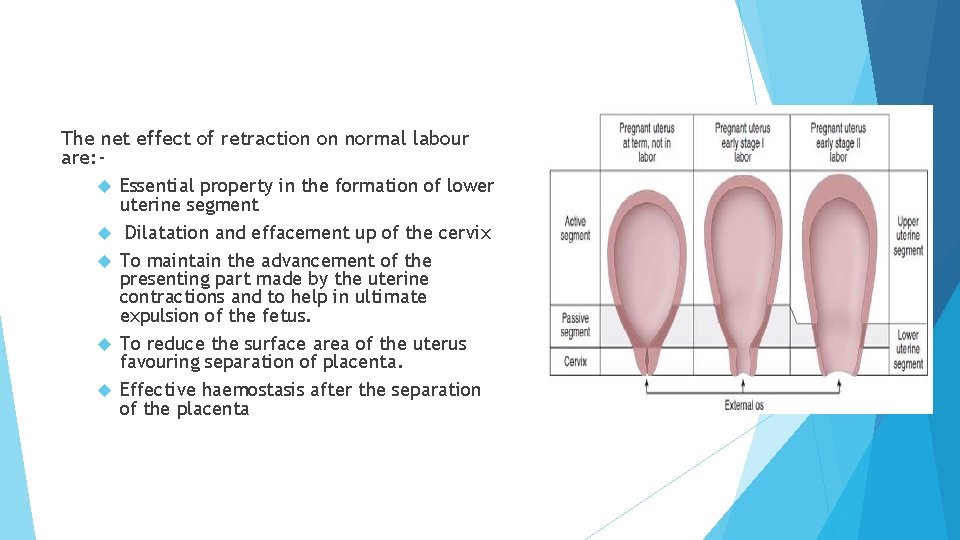
The net effect of retraction on normal labour are: Essential property in the formation of lower uterine segment Dilatation and effacement up of the cervix To maintain the advancement of the presenting part made by the uterine contractions and to help in ultimate expulsion of the fetus. To reduce the surface area of the uterus favouring separation of placenta. Effective haemostasis after the separation of the placenta
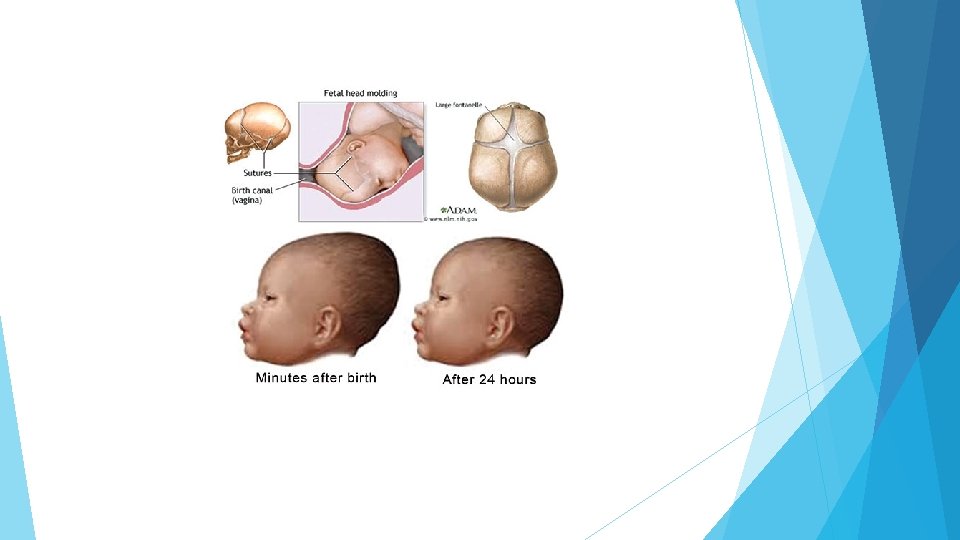
The Passenger The passage of the fetus through the birth canal is influenced by the size of the fetal head and shoulder the dimensions of the pelvic girdle the fetal presentation and position The bones of the cranial vault are not firmly united, and slight overlapping of the bones, or moulding of the shape of the head, occurs during labour. This capacity of the bones to slide over one another permits adaptation to the various diameters of the pelvis. Moulding can be extensive, but with most neonates the head assumes its normal shape within about 3 days after birth.
MOULDING The physiological gradual overlapping of the bones as the skull is compressed during its passage in the birth canal. One parietal bone overlaps the other and both overlap the occipital and frontal bones so fontanelles are no more detectable. It is of a good value in reducing the skull diameters but; severe and / or rapid moulding is dangerous as it may cause intracranial haemorrhage.
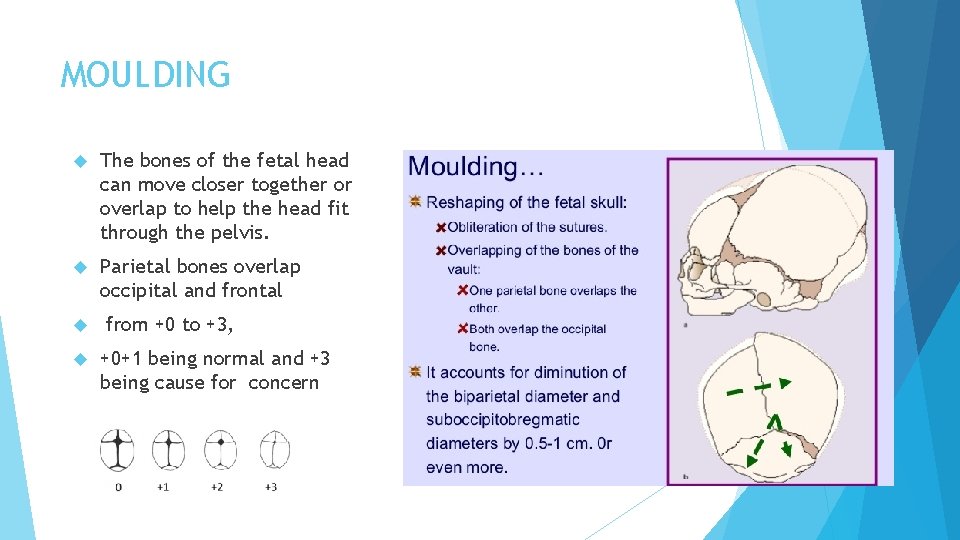
MOULDING The bones of the fetal head can move closer together or overlap to help the head fit through the pelvis. Parietal bones overlap occipital and frontal from +0 to +3, +0+1 being normal and +3 being cause for concern
The foetal head can move on the neck about 45 degrees in flexion or extension Shoulders and Pelvic girdle Because of their mobility, the position of the shoulder (the shoulder girdle) can be altered during labour, so that one shoulder may occupy a lower level than the other. This permits a small shoulder diameter to negotiate the passage. The circumference of the hips, or pelvic girdle, is usually small enough not to create problems.
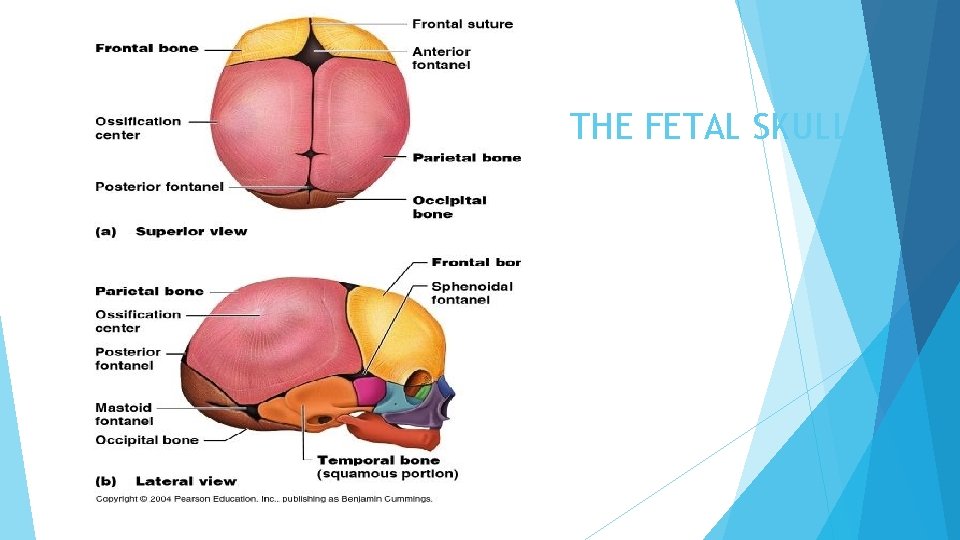
THE FETAL SKULL
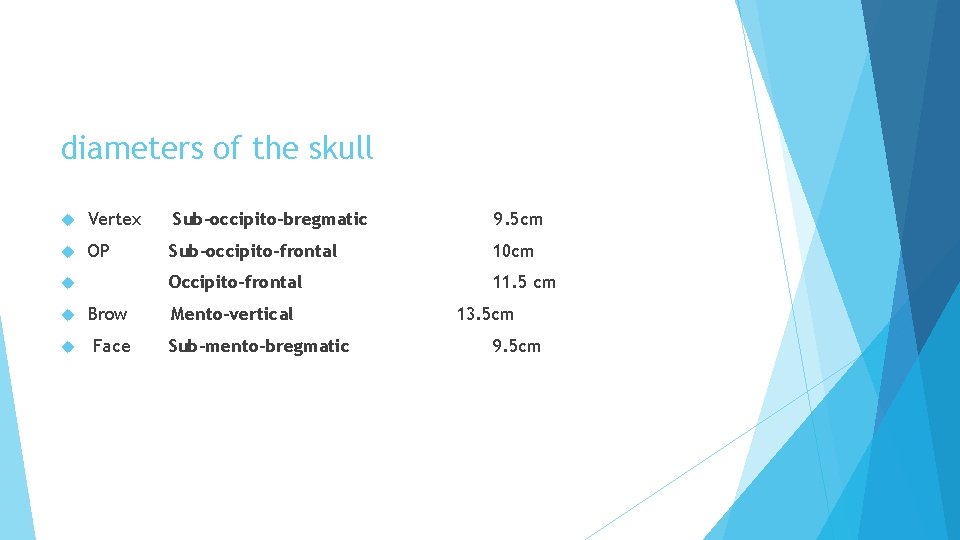
diameters of the skull Vertex Sub-occipito-bregmatic 9. 5 cm OP Sub-occipito-frontal 10 cm Occipito-frontal 11. 5 cm Brow Face Mento-vertical Sub-mento-bregmatic 13. 5 cm 9. 5 cm
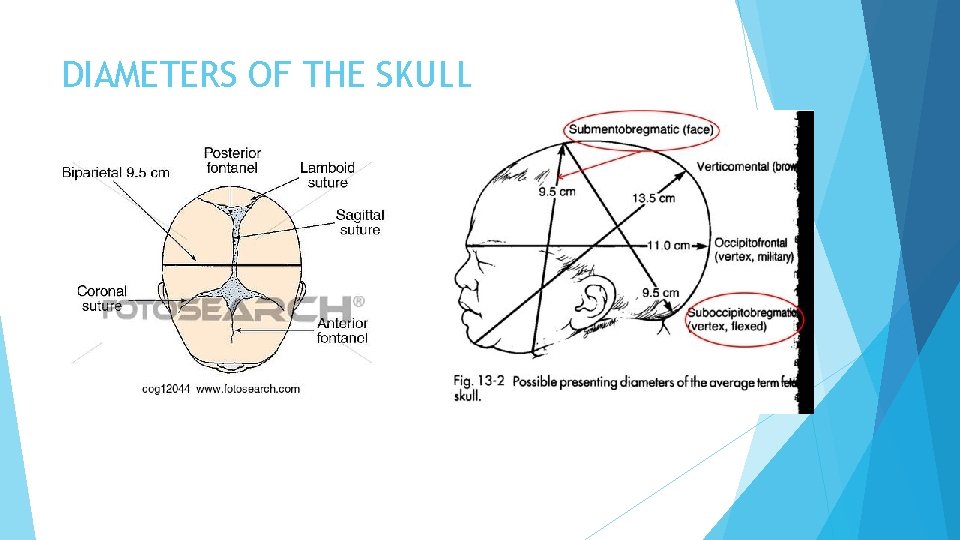
DIAMETERS OF THE SKULL
Caput succedaneum is a diffuse swelling of the scalp caused by the pressure of the scalp against the dilating cervix during labour. Caput can make it difficult to define the position of the fetal head. It is graded subjectively from 0 (none) to +3 (marked).
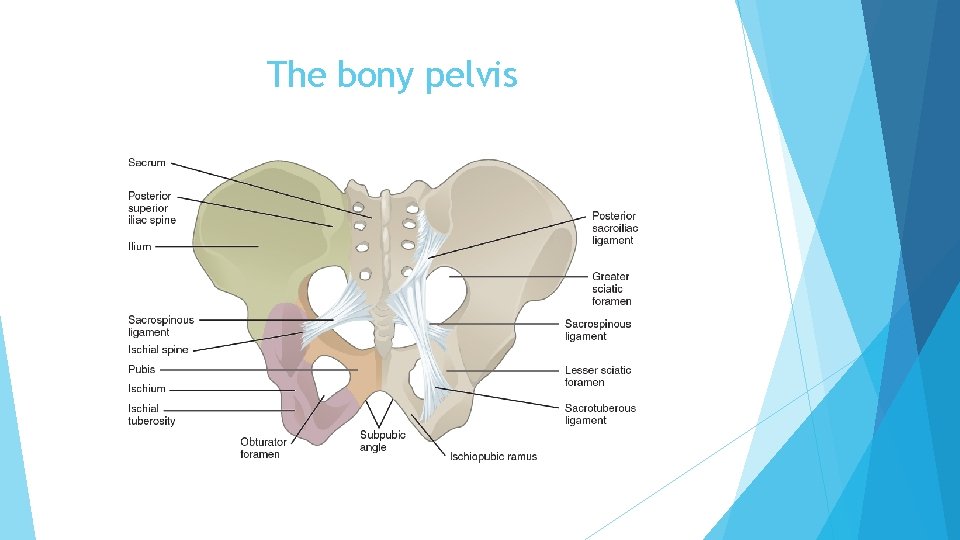
The bony pelvis
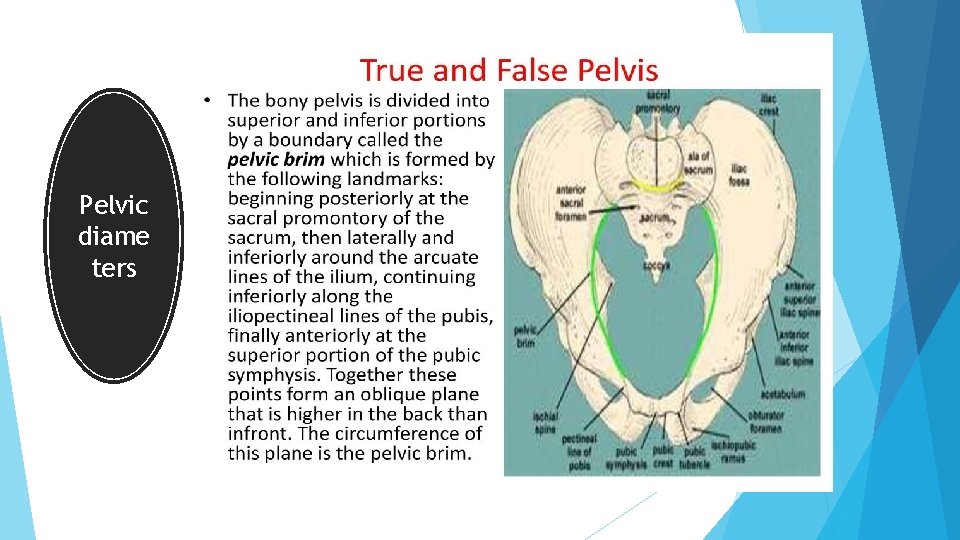
Pelvic diame ters
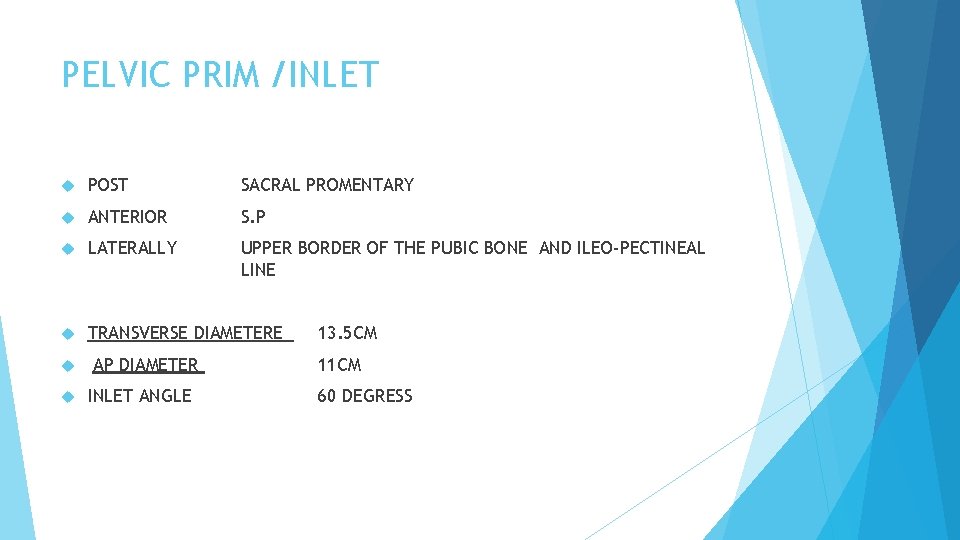
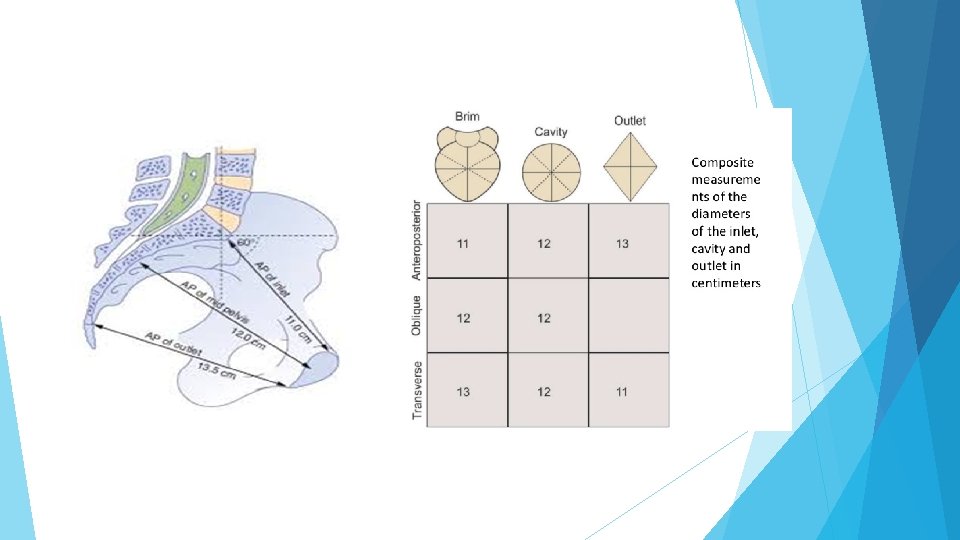
PELVIC PRIM /INLET POST SACRAL PROMENTARY ANTERIOR S. P LATERALLY UPPER BORDER OF THE PUBIC BONE AND ILEO-PECTINEAL LINE TRANSVERSE DIAMETERE AP DIAMETER INLET ANGLE 13. 5 CM 11 CM 60 DEGRESS
PELVIC MIDCAVITY middle of the S. P from the sides : pubic bone , inner aspect of the ischial bone Posteriorly : S 2 -S 3 Junction almost round AP Diameter 12 cm Feel ischial spine vaginally station
Pelvic outlet Anteriorly Lower margin of S. P Laterally Pubic bone descending rami , ischial tuberosity and Sacro-tuberous ligament Posteriorly end of sacrum Ap diameter 13. 5 Transverse diameter 11 cm
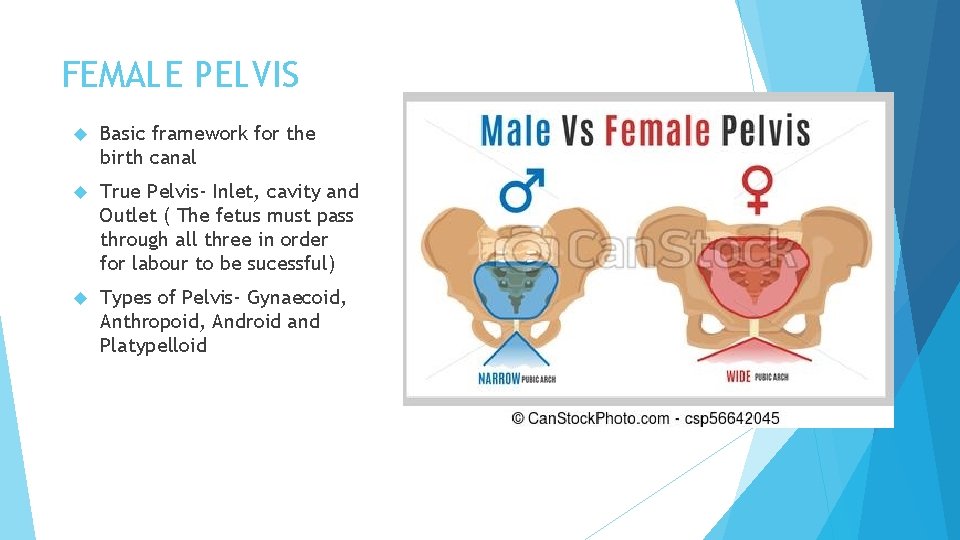
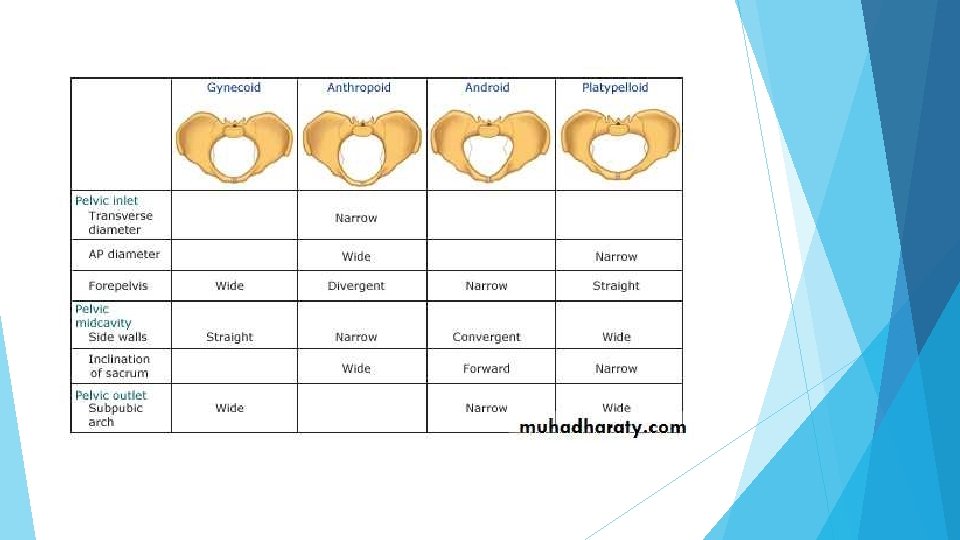
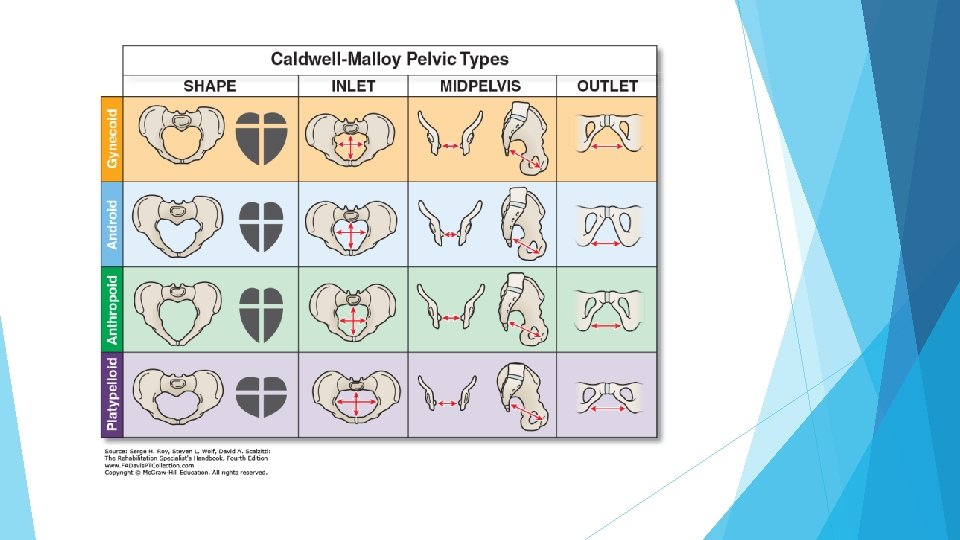
FEMALE PELVIS Basic framework for the birth canal True Pelvis- Inlet, cavity and Outlet ( The fetus must pass through all three in order for labour to be sucessful) Types of Pelvis- Gynaecoid, Anthropoid, Android and Platypelloid
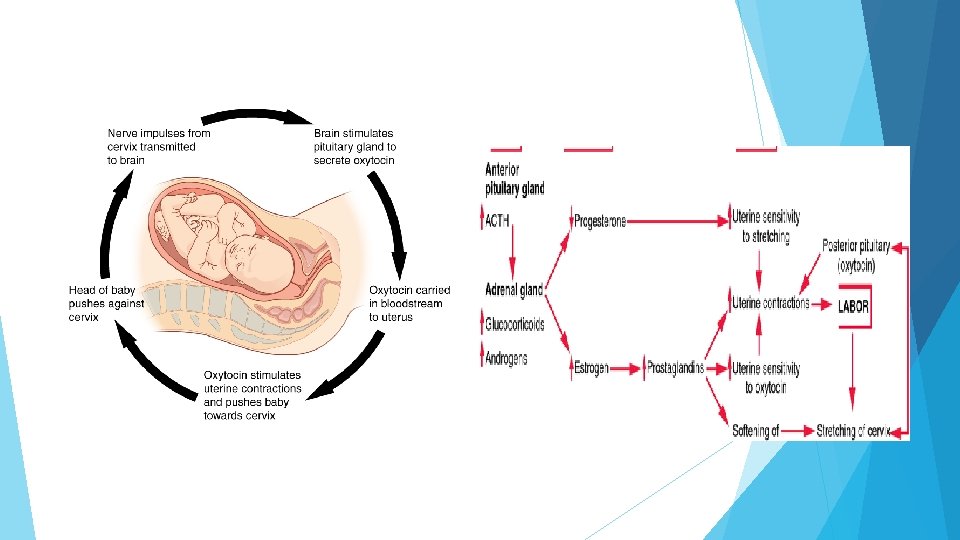
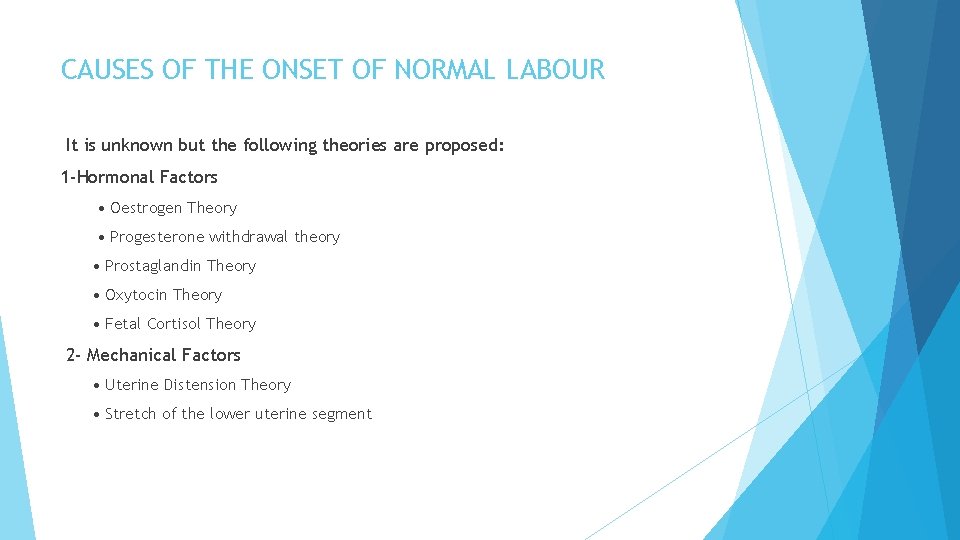
CAUSES OF THE ONSET OF NORMAL LABOUR It is unknown but the following theories are proposed: 1 -Hormonal Factors • Oestrogen Theory • Progesterone withdrawal theory • Prostaglandin Theory • Oxytocin Theory • Fetal Cortisol Theory 2 - Mechanical Factors • Uterine Distension Theory • Stretch of the lower uterine segment
Hormonal factors: (i) Oestrogen theory: During pregnancy, most of the oestrogens are present in a binding form. During the last trimester, more free oestrogen appears increasing the excitability of the myometrium and prostaglandins synthesis. (ii) Progesterone withdrawal theory: Before labour, there is a drop in progesterone synthesis leading to predominance of the excitatory action of oestrogens. (iii) Prostaglandins theory: Postaglandins E 2 and F 2 a are powerful stimulators of uterine muscle activity (iv) Oxytocin theory: Although oxytocin is a powerful stimulator of uterine contraction , its natural role in onset of labour is doubtful. The secretion of oxytocinase enzyme from the placenta is decreased near term due to placental ischaemia leading to predominance of oxytocin’s action. (v) Foetal cortisol theory: Increased cortisol production from the foetal adrenal gland before labour may influence its onset by increasing oestrogen production from the placenta
Clinical Picture of Labour Prodromal (pre - labour) stage: Shelfing Lightening It is the relief of upper abdominal pressure symptoms as dyspnoea, dyspepsia and palpitation due to Descent in the fundal level after engagement of the head Pelvic pressure symptoms With engagement of the presenting part the following symptoms may occur: Frequency of micturition. - Rectal tenesmus. - Difficulty in walking. Increased vaginal discharge False labour pain.
Onset of Labour: True labour pain The show Dilatation of the cervix
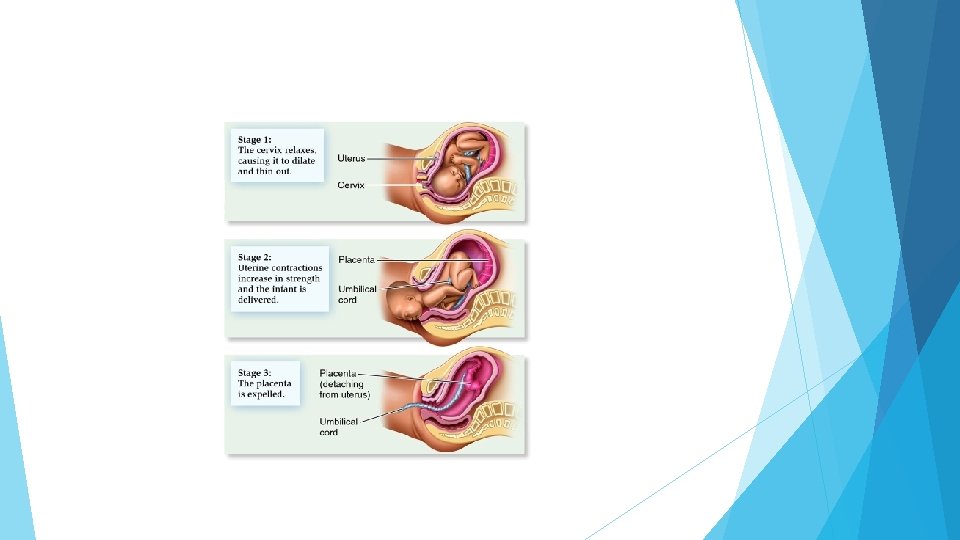
STAGES OF LABOUR First Stage Begins with the onset of true labour contractions and ends when the cervix is fully dilated (10 cm). Cervical effacement and dilatation occurs in this : Latent & Active Latent: From diagnosis of labour to 3 cm dilatation Active: From 3 cm to full dilatation (10 cm) It takes about 10 -14 hours in primi gravida and about 6 -8 hours in multi para. The second stage of labour begins with complete dilatation and ends with the birth of the baby. Approximately 2 hours in a nulliparous and 1 hour in a multi-para woman Third stage Begins after birth and ends with the expulsion of the placenta and membranes Shortest stage: After birth, up to 30 minutes
FIRST STAGE WHAT HAPPENS 1 - Contractions 1. Regular 2. Increasing Frequency 3. Stronger 2 - Cervical Dilatation and Effacement 3. Engagement of the presenting part
FIRST STAGE WHAT HAPPENS Latent phase: This is the first 3 -4 cm of cervical dilatation slow takes about 8 hours in nullipara and 4 hours in multipara. The latent phase begins with mild, irregular uterine contractions that soften and shorten the cervix Active phase Begin after 4 cm of cervical dilatation. The normal rate of cervical dilatation in active phase is 1 -1. 2 cm/ hour in primigravidae and 1. 5 cm/hour in multiparae. If the rate is < 1 cm / hour it is considered prolonged
Quantitatives Assessment Palpation External tocodynamometry Internal uterine pressure catheters. 95 % of women in labor will have 3 -5 contractions per 10 minutes.
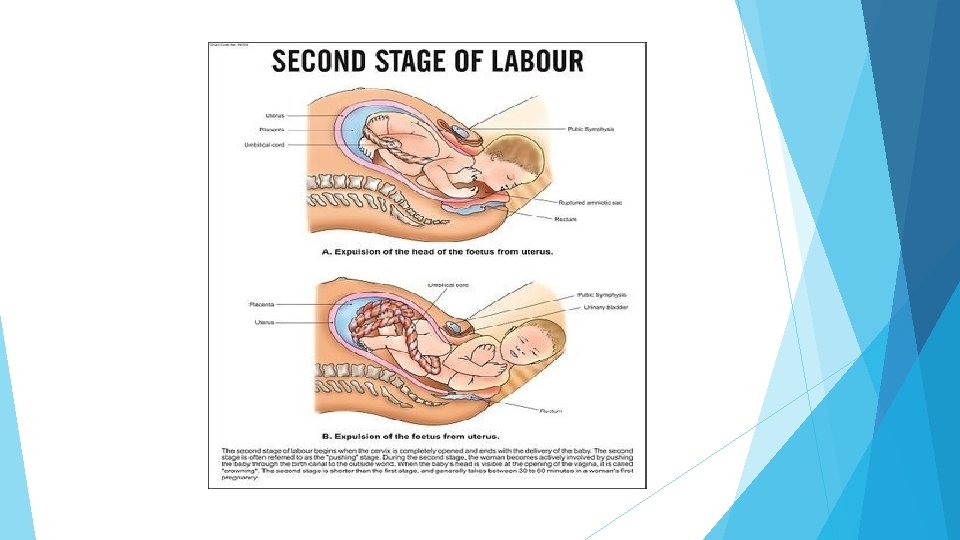
SECOND STAGE First sign of the second stage is the urge to push Full Dilatation to Delivery of the fetus The median duration varies in nulliparous and multiparous women is 60 and 30 minutes, respectively. Other factors may affect its duration: Epidural analgesia duration of the first stage parity maternal size birth weight station at complete dilation. Signs to look for: Distention of the perineum Satisfactory progress: - steady descent of the fetus through the birth canal & onset of the expulsive phase
(ACOG) has suggested that a prolonged second stage of labor should be considered when the second stage of labour exceeds 3 hours in nulliparous and 2 hours in multiparous

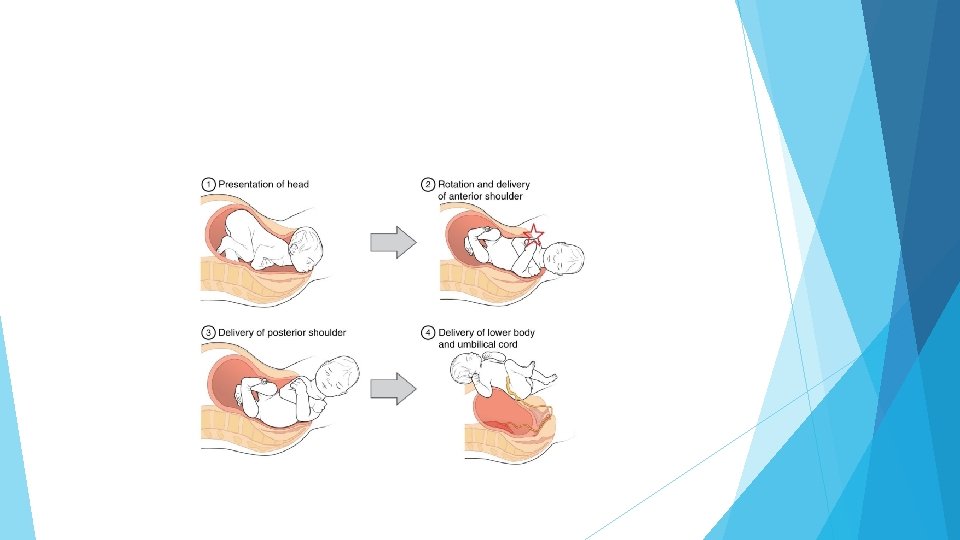
MECHANISM OF LABOUR
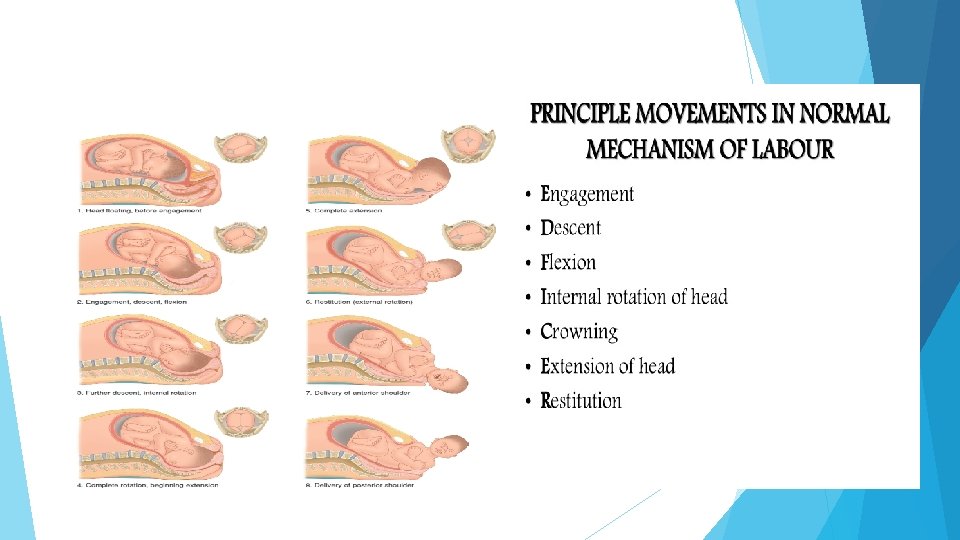
Delivery of the head: (1) Descent: It is continuous throughout labour particularly during the second stage and caused by: a. Uterine contractions and retractions. b. The auxiliary forces brought by contraction of the diaphragm and abdominal muscles. c. The unfolding of the foetus (2) Engagement: The head normally engages in the oblique or transverse diameter of the inlet.
Flexion Increased flexion of the head occurs when it meets the pelvic floor according to the lever theory. Increased flexion results in : a. The suboccipito - bregmatic diameter (9. 5 cm) passes through the birth canal instead of the suboccipito- frontal diameter (10 cm). Internal rotation The rule is that the part of foetus meets the pelvic floor first will rotate anteriorly. As the head descends, the presenting part, usually in the transverse position, is rotated about 45° to anteroposterior (AP) position under the symphysis Extension The suboccipital region lies under the symphysis then by head extension the vertex, forehead and face come out successively.
Restitution: After delivery, the head rotates 1/8 of a circle in the opposite direction of internal rotation to undo the twist produced by it. External rotation The shoulders enter the pelvis in the opposite oblique diameter to that previously passed by the head. When the anterior shoulder meets the pelvic floor it rotates anteriorly 1/8 of a circle. This movement is transmitted to the head so it rotates 1/8 of a circle in the same direction of restitution
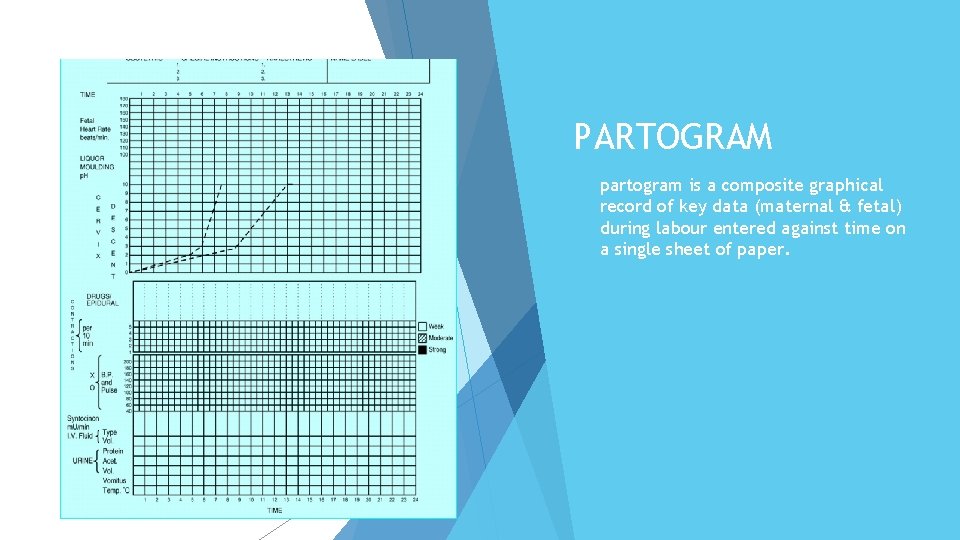
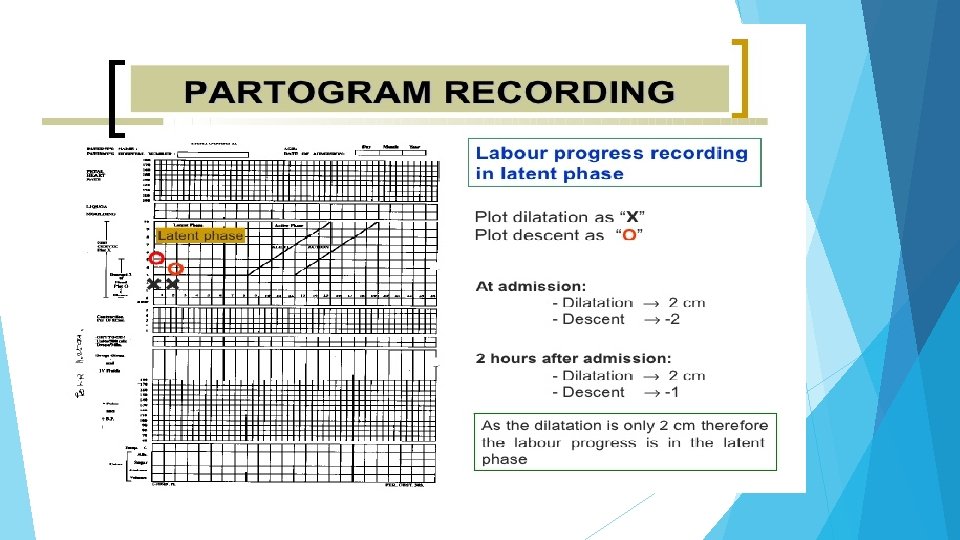
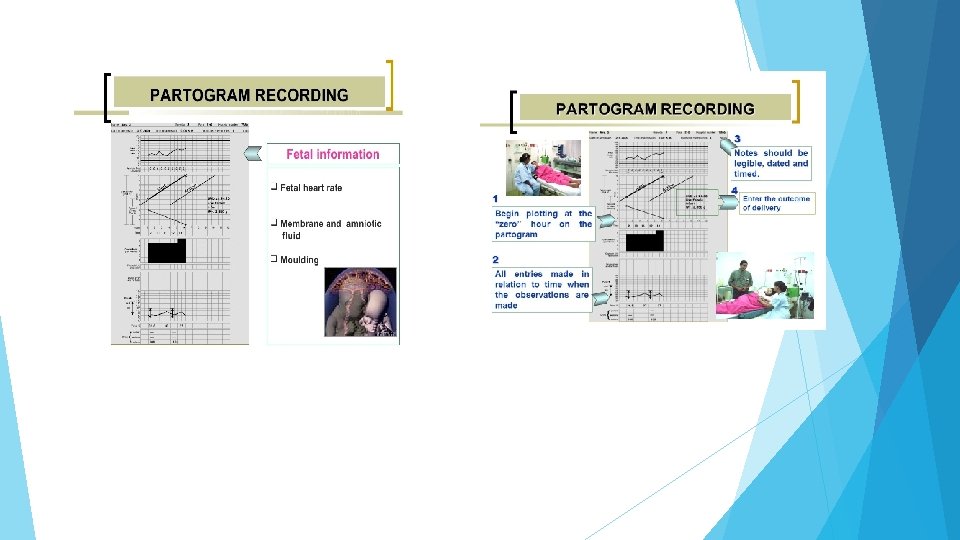
PARTOGRAM partogram is a composite graphical record of key data (maternal & fetal) during labour entered against time on a single sheet of paper.
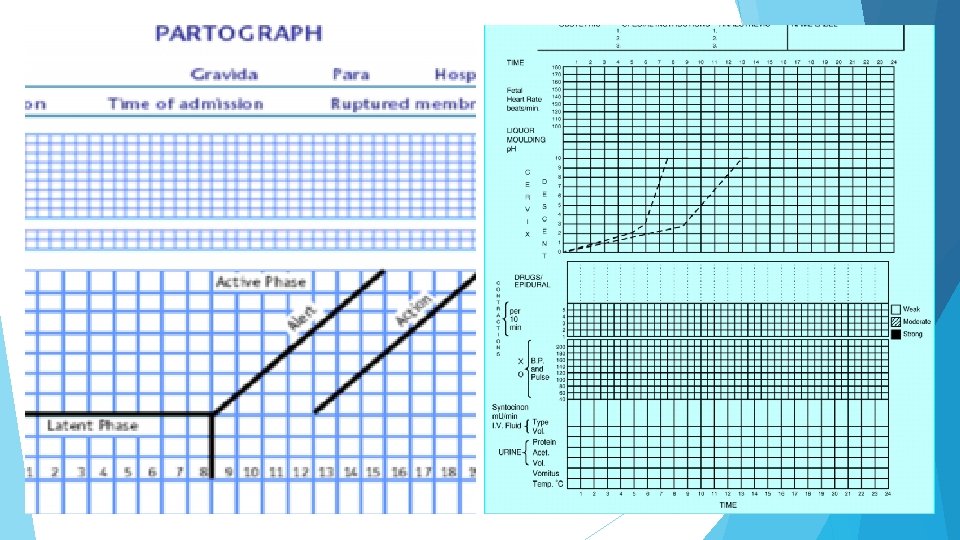
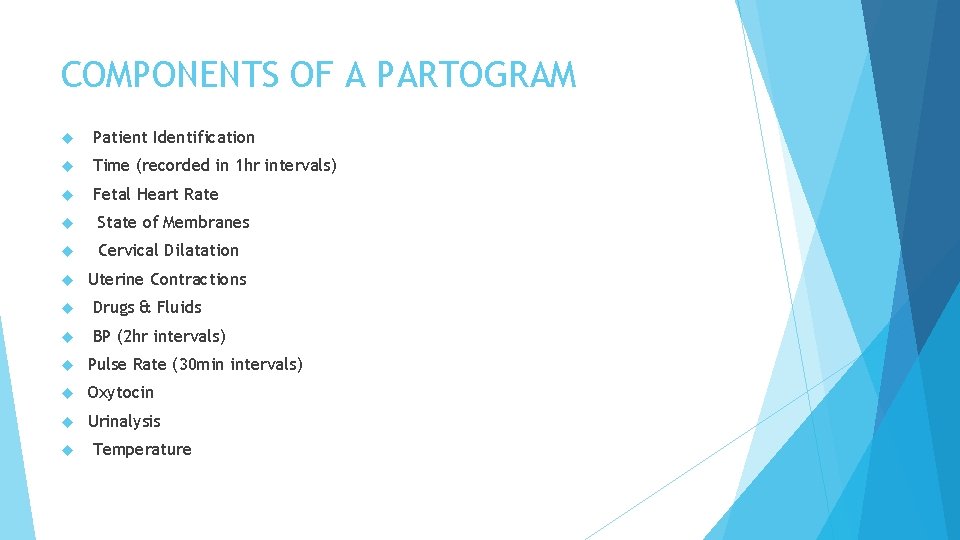
COMPONENTS OF A PARTOGRAM Patient Identification Time (recorded in 1 hr intervals) Fetal Heart Rate State of Membranes Cervical Dilatation Uterine Contractions Drugs & Fluids BP (2 hr intervals) Pulse Rate (30 min intervals) Oxytocin Urinalysis Temperature
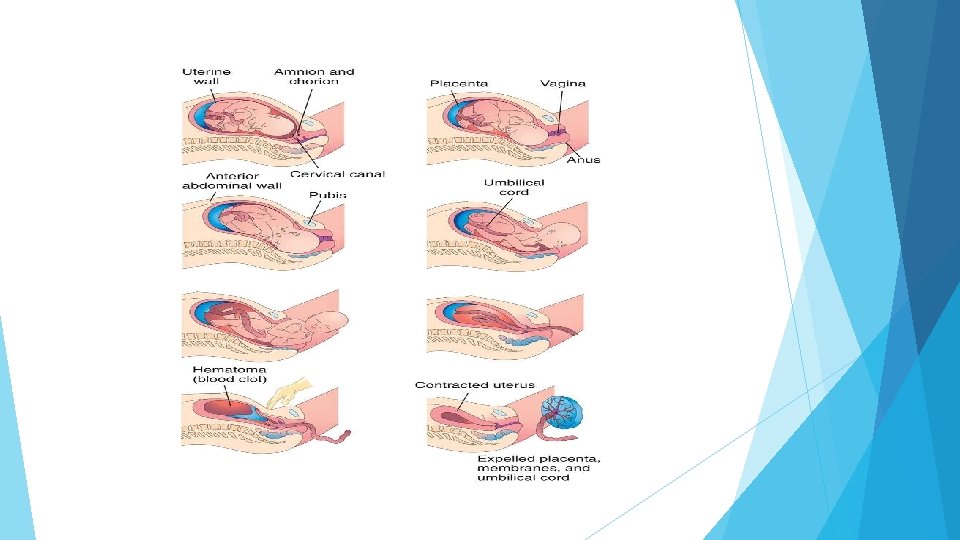
THIRD STAGE Begins with fetus delivery and ends with delivery of placenta/membranes Two phases: Separation and Expulsion 30 mins or less Average blood loss 150 -250 mld Birth of the placenta (Two stages) • Separation of the placenta from the wall of the uterus and into the lower uterine segment or vagina • Actual expulsion of the placenta out of the birth canal
BIRTH OF THE PLACENTA Two methods: Passive Management (wait for spontaneous expulsion of the placenta) Active Management Active management of 3 rd stage , helps to prevent PPH Includes: Use of oxytocin (given around the time of the anterior shoulder delivery, 10 units) Controlled cord traction Uterine massage
SIGNS OF SEPARATION Globular and hard uterus Sudden gush of blood Cord Lengthening (Most reliable clinical sign) EXAMINATION OF THE PERINEUM look for lacerations vulva outlet vaginal canal & cervix should be inspected Repair lacerations or episiotomies immediately or completeness and anomalies
IMMEDIATE CARE OF THE NEWBORN Assess baby Health baby with spontaneous respiration place on mother’s abdomen APGAR scores
Engagement: The fetus is engaged if the widest leading part (typically the widest circumference of the head) is entering the inlet Station: Relationship of the bony presenting part of the fetus to the maternal ischial spines. If at the level of the spines it is at “ 0 (zero)” station, if it passed it by 2 cm it is at “+2” station. Attitude: Relationship of fetal head to spine: flexed, neutral (“military”), or extended attitudes are possible. Position: Relationship of presenting part to maternal pelvis, i. e. ROP=right occiput posterior, or LOA=left occiput anterior. Presentation: Relationship between the leading fetal part and the pelvic inlet: cephalic, breech (complete, incomplete, frank or footling), face, brow, mentum or shoulder presentation. Lie: Relationship between the longitudinal axis of fetus and long axis of the uterus: longitudinal, oblique, and transverse.
Pelvic types Traditional obstetrics characterizes four types of pelvises: Gynecoid: Ideal shape, with round to slightly oval (obstetrical inlet slightly less transverse) inlet: best chances for normal vaginal delivery. Android: triangular inlet, and prominent ischial spines, more angulated pubic arch. Anthropoid: the widest transverse diameter is less than the anteroposterior (obstetrical) diameter. Platypelloid: Flat inlet with shortened obstetrical diameter.
- Slides: 60