CONTACT TRACING PURPOSE Promptly Identify any contacts of

- Slides: 18
CONTACT TRACING
PURPOSE Promptly Identify any contacts of a COVID -19 positive case to: • Assess exposure risk • Isolate/ Quarantine as appropriate • Monitor closely for development of symptoms • Give appropriate return to work instructions
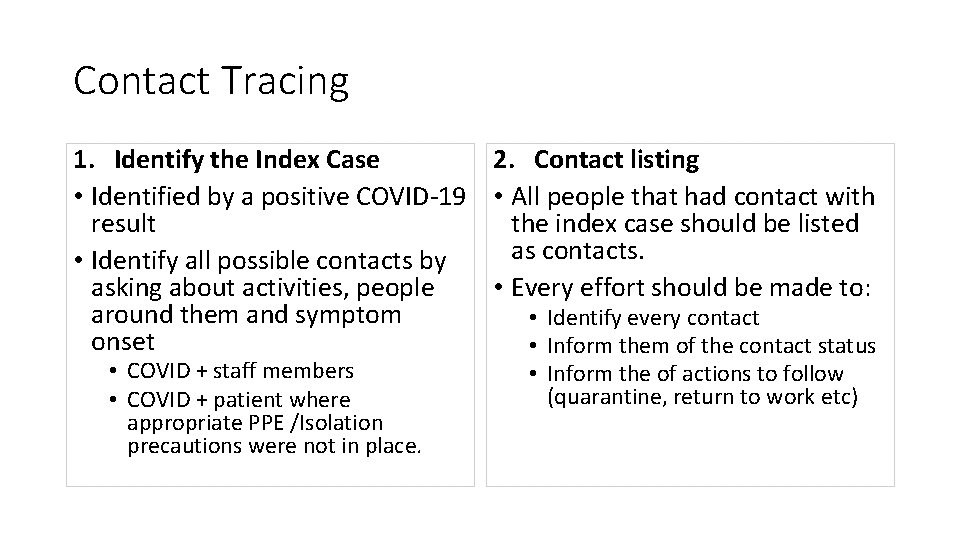
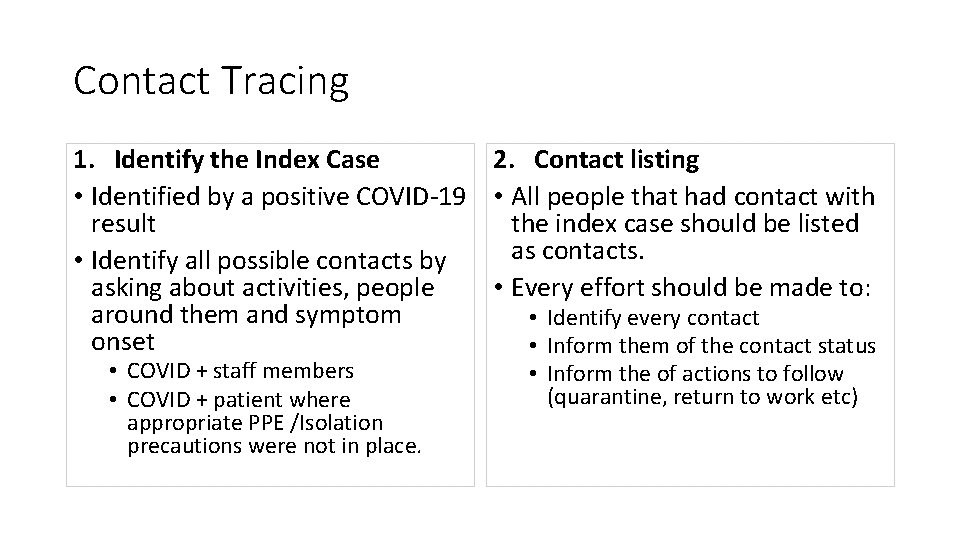
Contact Tracing 1. Identify the Index Case 2. Contact listing • Identified by a positive COVID-19 • All people that had contact with result the index case should be listed as contacts. • Identify all possible contacts by asking about activities, people • Every effort should be made to: around them and symptom • Identify every contact onset • Inform them of the contact status • COVID + staff members • COVID + patient where appropriate PPE /Isolation precautions were not in place. • Inform the of actions to follow (quarantine, return to work etc)
Identifying the Index Case • Infection Prevention will notify you of any new contact tracing needs (Staff or patient). • Any staff member with a positive COVID-19 test will require contact tracing • Any patient where a lapse/breech in PPE or Isolation Precautions is noted will require contact tracing.
Contact Listing- Staff Member Contact Tracing • Questions will be guided by Smartsheets • When did symptoms start • Look back 48 hours from symptom start for contact tracing • Identify all staff they may have come in contact with up to 48 hours prior to symptom development. • Work location(s), Lunch buddies etc • Identify all patients they may have come in contact with up to 48 hours prior to symptom development. • Patients they cared for and • PPE status at time of interaction. How to Identify Contacts for Staff • Interview Index Case • Contact Department Managers o Notification Distribution List with standard department heads will be shared o Template e-mail available • Build contact list based on feedback from Index case and department managers. • Assess risk based on mask use • HIGH RISK: If BOTH staff members do NOT have a mask in place. • Recommendation: 14 day quarantine • LOW RISK: One or BOTH staff members have a mask on • Recommendation: Enhanced symptom monitoring
Contact Listing- Patient Determine exposure window: • PPE Breech or Inadequate Isolation • New symptom onset Assess risk based on mask and face shield use • Questions will be guided by Smartsheets • Identify all staff they may have come in contact with up to 48 hours prior to symptom development. • Unit location, diagnostic locations How to Identify Contacts • EPIC Chart Review • Build list of staff members documenting in chart • Any surgeries/ procedures • Contact Department Managers o Notification Distribution List with standard department heads will be shared o Template e-mail available • Build contact list based on EPIC Chart review and department managers. • HIGH RISK: If BOTH mask AND Face shield were NOT worn by staff member(s). Recommendation: 14 day quarantine & Enhanced monitoring • LOW RISK: Mask and face shield in place ad no PPE breeches noted. • Recommendation: Enhanced symptom monitoring.
Contact Notification Staff • Any High Risk Contacts- 14 day quarantine • Notify via phone call • Template email also available • Any Low Risk Contact- Enhanced monitoring • Notify via UMMC/SOM email address • Template email available Patients • Notify attending physician to help facilitate • Notification of patient and/family of contact with COVID + individual • Place on Droplet Contact precautions
E-mail Templates
Department Leadership Notification • Purpose: Inform and Identify relevant staff Hello, This is to notify you that a staff member on <UNIT/LOCATION> tested POSITIVE for COVID-19. Please send to me the names of your staff members that worked in the <UNIT/LOCATION> on: <RELEVANT DATE (S)> If your staff worked at <UNIT/LOCATION> on any of the dates identified above, we will follow up with them via email with the instructions below (See low risk/high risk template). Feel free to share the following information with them. Thank you, <Your Name>
LOW RISK CONTACT Notification • Purpose: Provide Instruction Hello, You have been identified as someone possibly had contact with an individual who has tested positive for COVID-19, the novel coronavirus. Fortunately, this individual was compliant with Universal masking and social distancing and therefore all contacts (patient and staff) are considered low risk. The dates of contact we are working with are: <DATES & SHIFT > If you worked on any of these dates in <UNIT? DEPARTMENT>, please do the following: Click on this link and fill out the form: Employee Exposure to COVID-19 in the Community or from a Colleague • In the interest of keeping the staff member’s information private- staff may enter “Identity Unknown’ for the colleague’s name in the data collection form. • Contact date: Select the last date, based on the dates above, that you worked on either unit. Monitor for and report signs and symptoms for 14 days from the last day of contact (day of contact=day 1). • This means taking temperatures twice a day from the date of contact until the 14 th day after the last contact. • Monitor for symptoms twice a day, ideally at the same times each day. • Submit the Employee Exposure Daily Monitoring Form daily. § Additional symptoms may include new or progressive sore throat, cough, fever and shortness of breath. § It is also important to make sure that at a minimum, you are wearing a surgical mask with full face shield for every patient encounter while working You may continue to work during this 14 day self-monitoring period for as long as you are not sick o If signs and symptoms develop at home, call out immediately. o If signs and symptoms develop at work, immediately notify superior and go home. o If symptomatic, call 410 -328 -2793 for evaluation for COVID-19 testing. If you need to call out, please do so per the established departmental process. Additionally, please fill out the Employee Call Out Form Links to all the documents mentioned above can also be found on the Insider Infection Prevention page - COVID 19 Employee Forms. Additional information regarding COVID-19 can be found at the UMMS COVID-19 Response website or at the Centers for Disease Control and Prevention website For questions or concerns, please contact Employee Health at DTC: 410. 328. 6151 MC: 410. 225. 8325 or Infection Control at 410. 328. 5757 or via Pager at 410. 328. 2337 pager 5757#.
High Risk Contact Notification • Purpose: Provide Instruction (Also notified via phonecall) Hello, You have been identified as someone who has been in prolonged close contact with an individual who has tested positive for COVID-19, the novel coronavirus. Based on the Exposure Risk Category for COVID-19, we are recommending that you be placed on a 14 -day home quarantine effective immediately. The dates of contact we are working with is <INSERT DATE> Please do the following: Click on this link and fill out the form: Employee Exposure to COVID-19 in the Community or from a Colleague Monitor for and report signs and symptoms for 14 days from the last day of exposure (day of exposure=day 1) Please contact your manager to determine your date of exposure. This means taking temperatures twice a day from the date of exposure until the 14 th day after the last exposure. Ideally, take the temperature before coming to work and at least one additional time in the day. Please submit the Employee Exposure Daily Monitoring Form daily. Additional symptoms may include new or progressive sore throat, cough, fever and shortness of breath. If you do develop symptoms during the 14 day monitoring period, call 410 -328 -2793 for evaluation for COVID-19 testing. At home: To protect your family; practice social distancing (6 feet) You can wear a mask at home to help with social distancing. Sleep in a separate room/area if possible Use a separate bathroom (if unable to, clean/disinfect bathroom after using) Stay in a separate room as much as possible. Clean/disinfect common rooms after use Please do not leave your home (have someone bring food/items if necessary) Links to all the documents mentioned above can also be found on the Insider Infection Prevention page - COVID 19 Employee Forms. Additional information regarding COVID-19 can be found at the UMMS COVID-19 Response website or at the Centers for Disease Control and Prevention website For questions or concerns, please contact Employee Health at 410. 225. 8325 or Infection Control at 410. 328. 5757 or via Pager at 410. 328. 2337 pager 5757#.
Some Back Ground Isolation & Universal Masking
Universal Masking • Initiated April 6, 2020 • All staff MUST wear a mask while on any UMMC campus • Challenge • Congregating in common spaces • Lunch rooms, report rooms nursing station
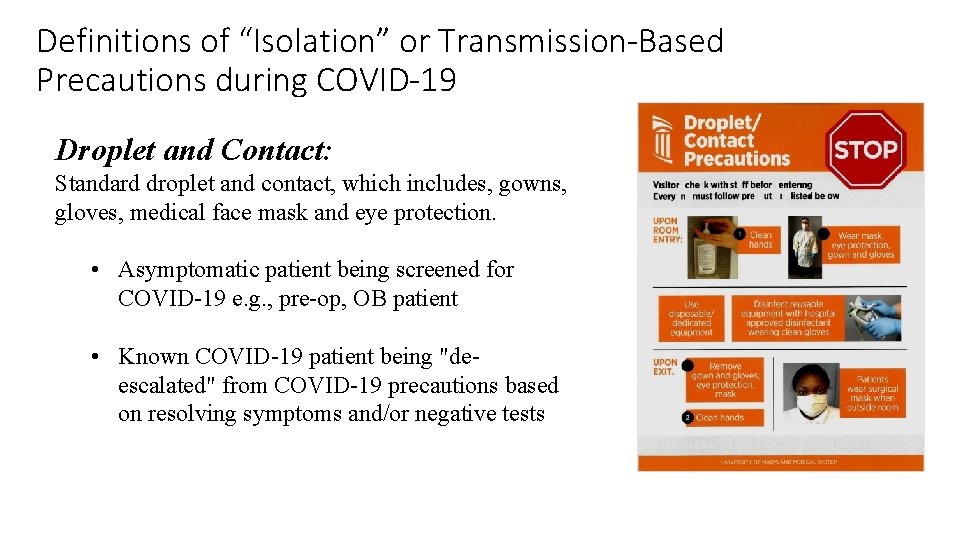
Definitions of “Isolation” or Transmission-Based Precautions during COVID-19 • Airborne/Droplet/contact: “Full PPE”, which includes gowns, gloves, respirator (i. e. , N 95 or elastomeric or PAPR) and eye protection, WITH negative pressure room. Keep patient room door closed to maintain negative pressure gradient. • For COVID-19 positive or PUI particularly critically ill and/or requiring aerosol generating procedures (AGP) • Enhanced Droplet and Contact: “Full PPE”, which includes gowns, gloves, respirator (i. e. , N 95 or elastomeric or PAPR) and eye protection, WITHOUT negative pressure room. Keep patient room door closed. • For stable COVID-19 patient or PUI NOT requiring AGP, or when negative pressure room not available • Non- COVID patient requiring continuous AGP • Droplet and Contact: Standard droplet and contact, which includes, gowns, gloves, medical face mask and eye protection. • Asymptomatic patient being screened for COVID-19 e. g. , pre-op, OB patient • Known COVID-19 patient being "de-escalated" from COVID-19 precautions based on resolving symptoms and/or negative tests • Standard precautions: No special PPE, use if indicated based on exposure to mucous membranes or body fluids. With universal masking, this implies that at least a face mask is worn by all individuals at all times, and eye protection worn when in contact with any patient.
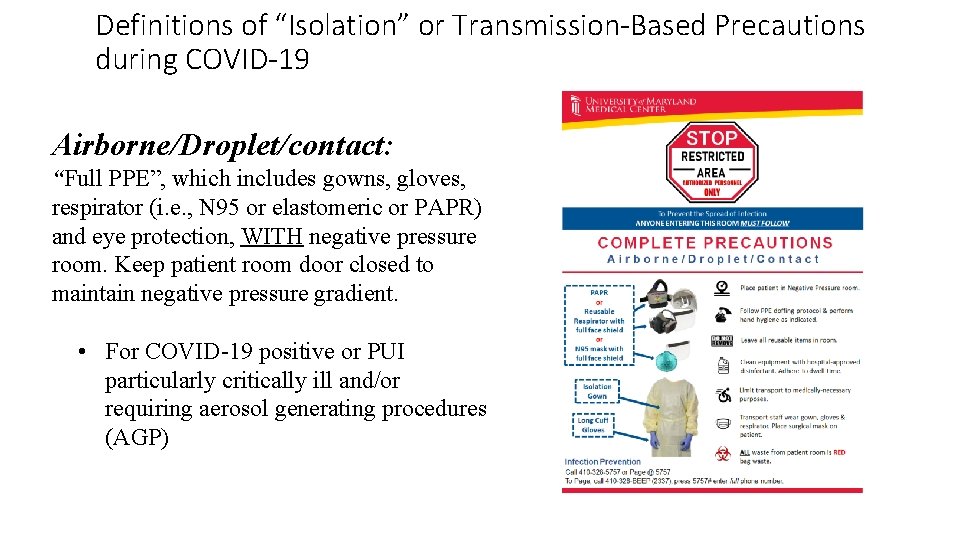
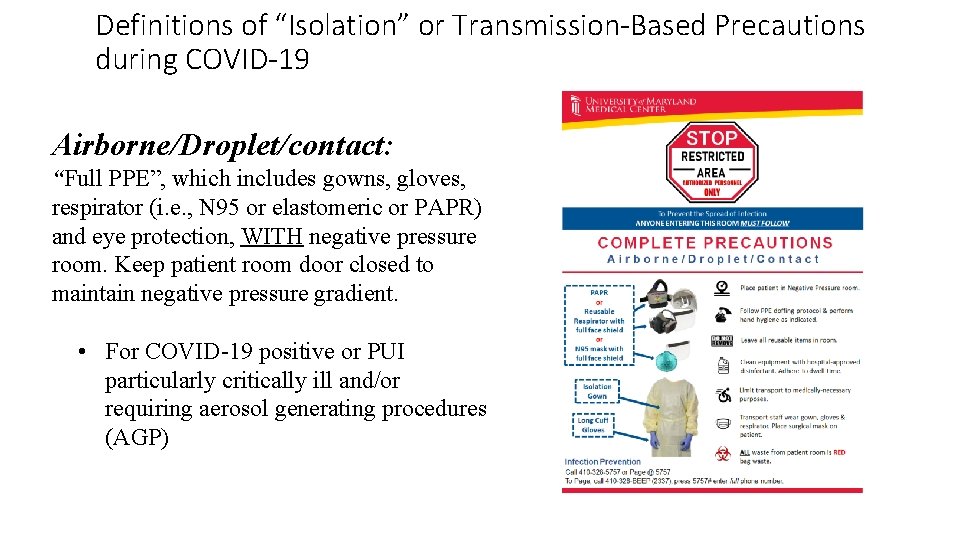
Definitions of “Isolation” or Transmission-Based Precautions during COVID-19 Airborne/Droplet/contact: “Full PPE”, which includes gowns, gloves, respirator (i. e. , N 95 or elastomeric or PAPR) and eye protection, WITH negative pressure room. Keep patient room door closed to maintain negative pressure gradient. • For COVID-19 positive or PUI particularly critically ill and/or requiring aerosol generating procedures (AGP)
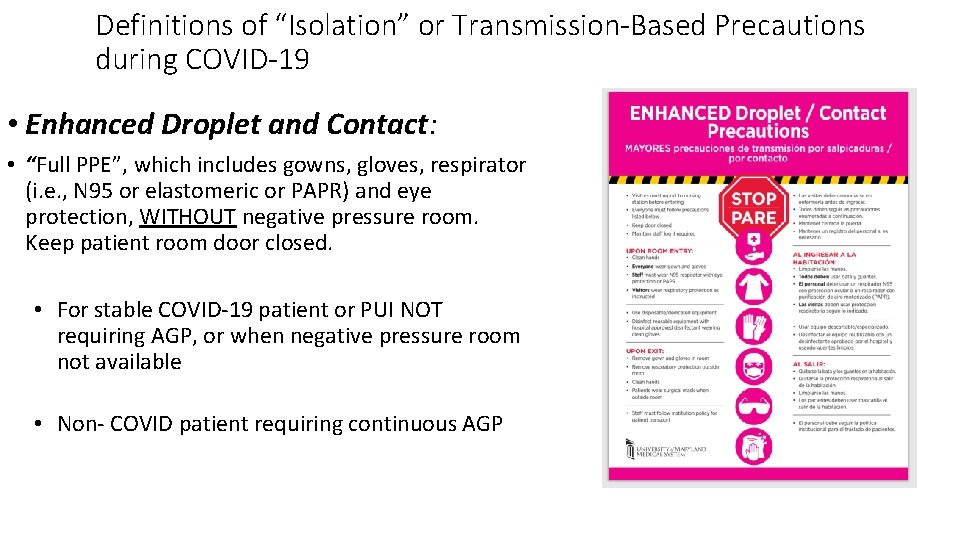
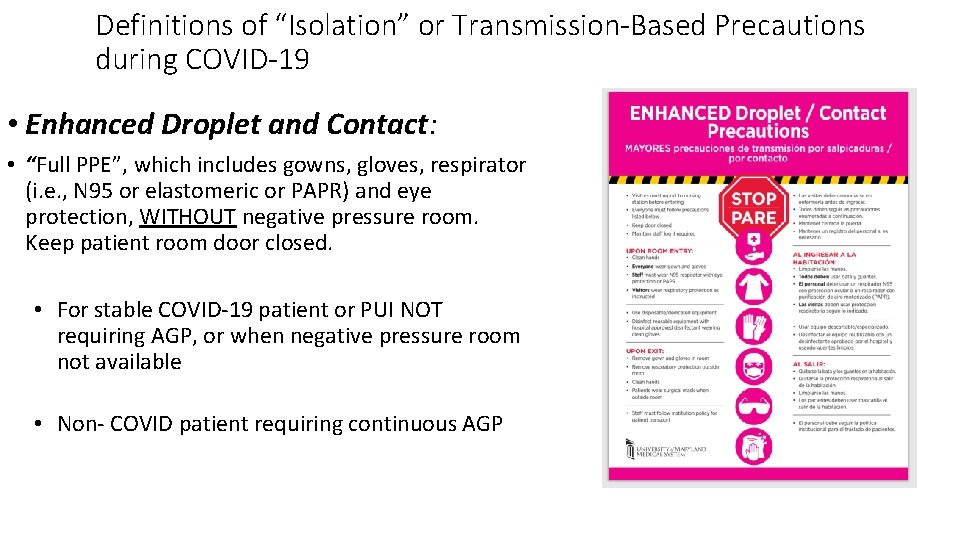
Definitions of “Isolation” or Transmission-Based Precautions during COVID-19 • Enhanced Droplet and Contact: • “Full PPE”, which includes gowns, gloves, respirator (i. e. , N 95 or elastomeric or PAPR) and eye protection, WITHOUT negative pressure room. Keep patient room door closed. • For stable COVID-19 patient or PUI NOT requiring AGP, or when negative pressure room not available • Non- COVID patient requiring continuous AGP
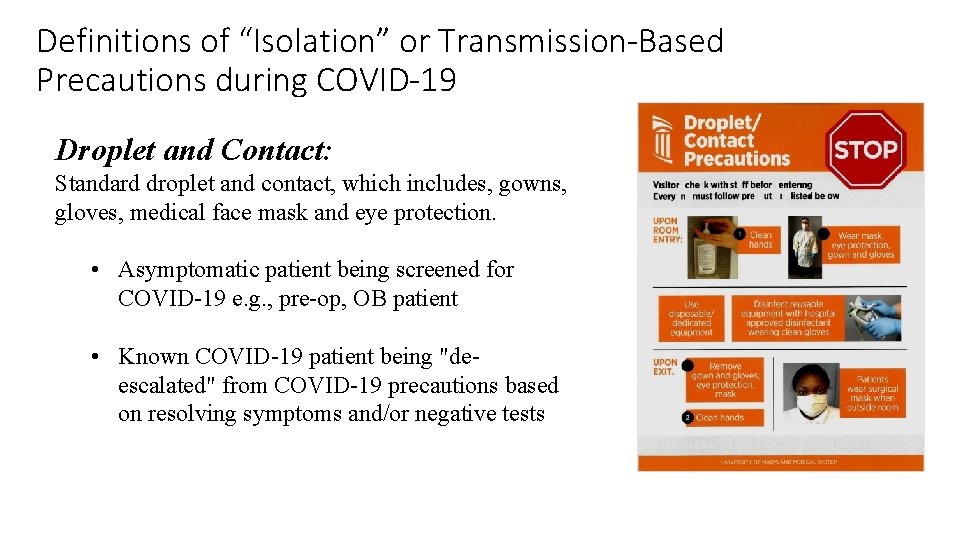
Definitions of “Isolation” or Transmission-Based Precautions during COVID-19 Droplet and Contact: Standard droplet and contact, which includes, gowns, gloves, medical face mask and eye protection. • Asymptomatic patient being screened for COVID-19 e. g. , pre-op, OB patient • Known COVID-19 patient being "deescalated" from COVID-19 precautions based on resolving symptoms and/or negative tests
