Constipation in the elderly All backed up and
Constipation in the elderly All backed up and no where to go Annette T. Carron, DO Director Geriatrics and Palliative Care Botsford Hospital
Objectives § Pathophysiology of constipation, with focus on changes with aging § Assessment and diagnosis of constipation § Standard of care treatment for constipation § Constipation and survey implications
Definition –constipation § Feeling of constipation is defined differently by different people § Defined by self-report or objective assessment-based § Clinical – finding fecal loading in the rectum on exam and/or colonic fecal loading on xray § Subtype – rectal outlet delay § Feeling of anal blockage at least a quarter of the time and prolonged defecation (>10 min to complete bowel movement) or need for selfdigitization on any occasion
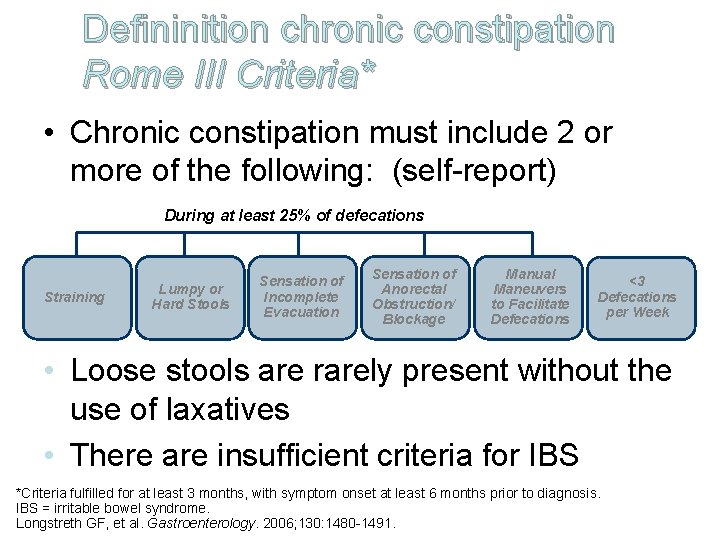
Defininition chronic constipation Rome III Criteria* • Chronic constipation must include 2 or more of the following: (self-report) During at least 25% of defecations Straining Lumpy or Hard Stools Sensation of Incomplete Evacuation Sensation of Anorectal Obstruction/ Blockage Manual Maneuvers to Facilitate Defecations <3 Defecations per Week • Loose stools are rarely present without the use of laxatives • There are insufficient criteria for IBS *Criteria fulfilled for at least 3 months, with symptom onset at least 6 months prior to diagnosis. IBS = irritable bowel syndrome. Longstreth GF, et al. Gastroenterology. 2006; 130: 1480 -1491.
Prevalence • North America: estimates range from 2% to 28%; 15% ≈ 63 million North Americans fulfill criteria for constipation – Variations due to • Criteria/symptoms definitions used (multiple definitions) • Survey collection methods • Self-report vs diagnosis • Worldwide – Similar rates in developed and undeveloped countries – 14%-30% (Spain, Sweden, Australia, China) Higgins PD, et al. Am J Gastroenterol. 2004; 99: 750 -759. Pare P, et al. Am J Gastroenterol. 2001; 96: 3130 -3137. Garrigues V, et al. Am J Epidemiol. 2004; 159: 520 -526. Walter S, et al. Scand J Gastroenterol. 2002; 37: 911 -916. Chiarelli P, et al. Int Urogynecol J. 2000; 11: 71 -78. Cheng C, et al. Aliment Pharmacol Ther. 2003; 18: 319 -326.
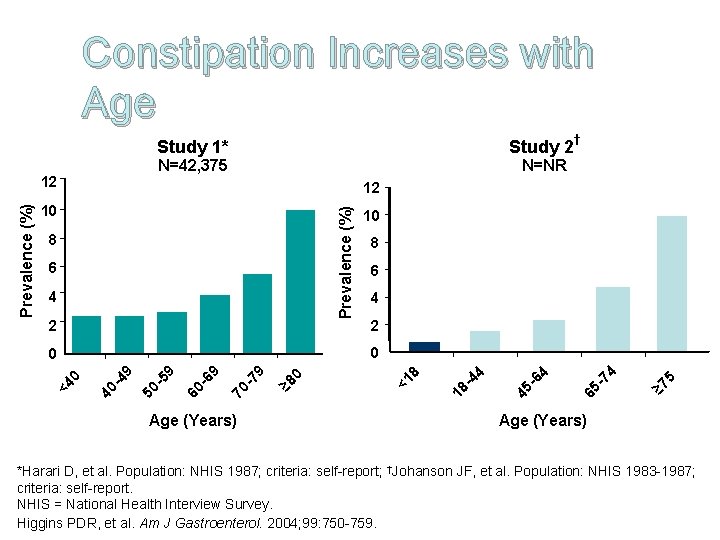
Constipation Increases with Age Study 1* N=42, 375 12 † N=NR 12 10 Prevalence (%) 8 6 4 2 10 8 6 4 2 5 ≥ 7 -7 4 65 -6 4 45 -4 4 18 0 ≥ 8 -7 9 70 -6 9 60 -5 9 50 -4 9 40 0 <4 Age (Years) 8 0 0 <1 Prevalence (%) Study 2 Age (Years) *Harari D, et al. Population: NHIS 1987; criteria: self-report; †Johanson JF, et al. Population: NHIS 1983 -1987; criteria: self-report. NHIS = National Health Interview Survey. Higgins PDR, et al. Am J Gastroenterol. 2004; 99: 750 -759.
Factors contributing to underestimation of constipation in elderly • Unable to report bowel-related symptoms • Have regular bowel movements despite have rectal or colonic fecal impaction • Have impaired rectal sensation and inhibited urge to go and so be unaware of rectal stool impaction • Nonspecific symptoms associated with colonic fecal impaction (e. g. , delirium, anorexia, functional decline)
Gut changes with aging • Collagen deposition in the left side of the colon increases • Total number of neurons in the myenteric plexus is decreased • Decrease in internal sphincter tone • Decline in external anal sphincter and pelvic muscle strength • Reduction in rectal motility with normal aging
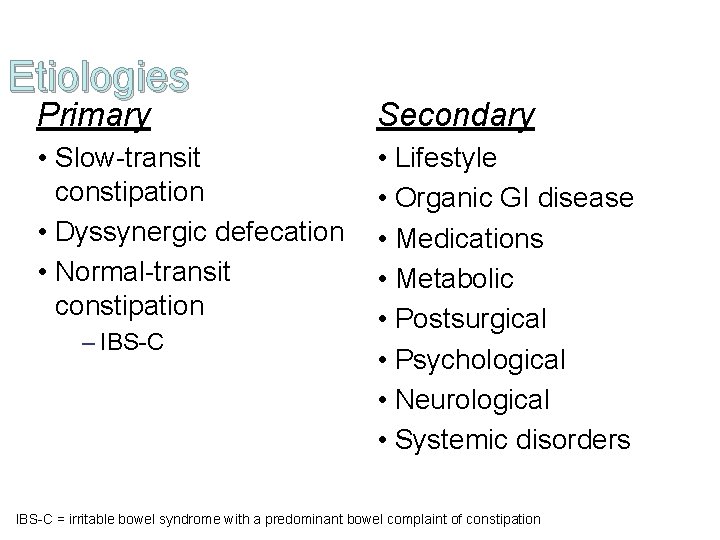
Etiologies Primary Secondary • Slow-transit constipation • Dyssynergic defecation • Normal-transit constipation • Lifestyle • Organic GI disease • Medications • Metabolic • Postsurgical • Psychological • Neurological • Systemic disorders – IBS-C = irritable bowel syndrome with a predominant bowel complaint of constipation
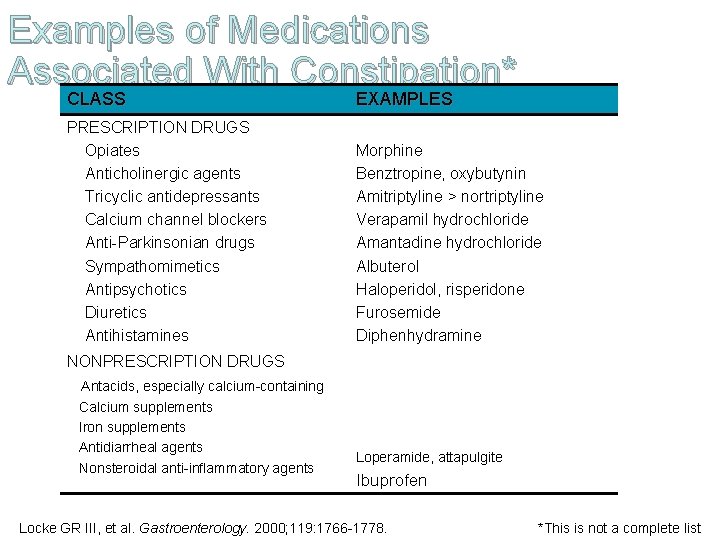
Examples of Medications Associated With Constipation* CLASS EXAMPLES PRESCRIPTION DRUGS Opiates Anticholinergic agents Tricyclic antidepressants Calcium channel blockers Anti-Parkinsonian drugs Sympathomimetics Antipsychotics Diuretics Antihistamines Morphine Benztropine, oxybutynin Amitriptyline > nortriptyline Verapamil hydrochloride Amantadine hydrochloride Albuterol Haloperidol, risperidone Furosemide Diphenhydramine NONPRESCRIPTION DRUGS Antacids, especially calcium-containing Calcium supplements Iron supplements Antidiarrheal agents Nonsteroidal anti-inflammatory agents Loperamide, attapulgite Ibuprofen Locke GR III, et al. Gastroenterology. 2000; 119: 1766 -1778. *This is not a complete list

Constipation Endemic in the Elderly Causes of Constipation in the Elderly Aluminum hydroxide–containing Hypothyroidism antacids Anticholinergics Immobility/Inactivity Calcium channel blockers Iron supplements Dehydration Low-fiber and carbohydrate diet Diabetes mellitus Narcotics Diuretics Parkinson’s disease Hypercalcemia/hypokalemia Stroke Approximately half of residents in nursing homes have constipation De Lillo AR, et al. Am J Gastroenterol. 2000; 95: 901 -905. Tariq SH. J Am Med Dir Assoc. 2007; 8: 209 -218.
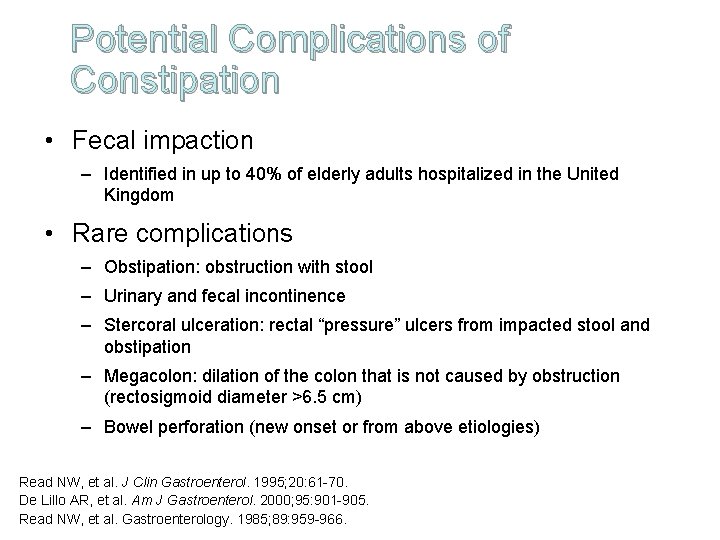
Potential Complications of Constipation • Fecal impaction – Identified in up to 40% of elderly adults hospitalized in the United Kingdom • Rare complications – Obstipation: obstruction with stool – Urinary and fecal incontinence – Stercoral ulceration: rectal “pressure” ulcers from impacted stool and obstipation – Megacolon: dilation of the colon that is not caused by obstruction (rectosigmoid diameter >6. 5 cm) – Bowel perforation (new onset or from above etiologies) Read NW, et al. J Clin Gastroenterol. 1995; 20: 61 -70. De Lillo AR, et al. Am J Gastroenterol. 2000; 95: 901 -905. Read NW, et al. Gastroenterology. 1985; 89: 959 -966.
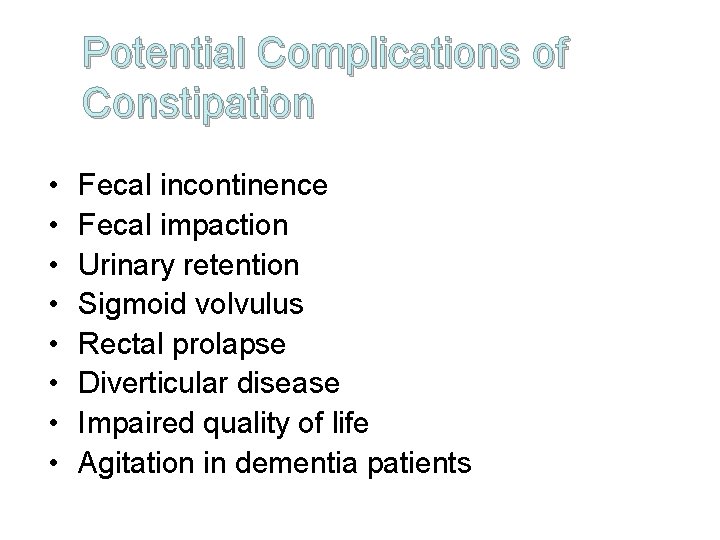
Potential Complications of Constipation • • Fecal incontinence Fecal impaction Urinary retention Sigmoid volvulus Rectal prolapse Diverticular disease Impaired quality of life Agitation in dementia patients
Chronic Constipation: Costs of Care • Direct costs (typically individual or third party) – Physician visits – Diagnostic tests – Medications • Indirect costs (individual or societal) – Reduced productivity – Lost wages – Impaired QOL = quality of life.
Medication Use in Older Adults With Chronic Constipation • In 2 large cross-sectional surveys of community-dwelling older adult patients: – Laxatives were third and fourth most frequently used nonprescription drugs • In cross-sectional survey of 4136 participants – Stimulant and bulking laxatives were most commonly used Ruby CM, et al. Am J Geriatr Pharmacother. 2003; 1: 11 -17. Passmore AP. Pharmacoeconomics. 1995; 7: 14 -24.
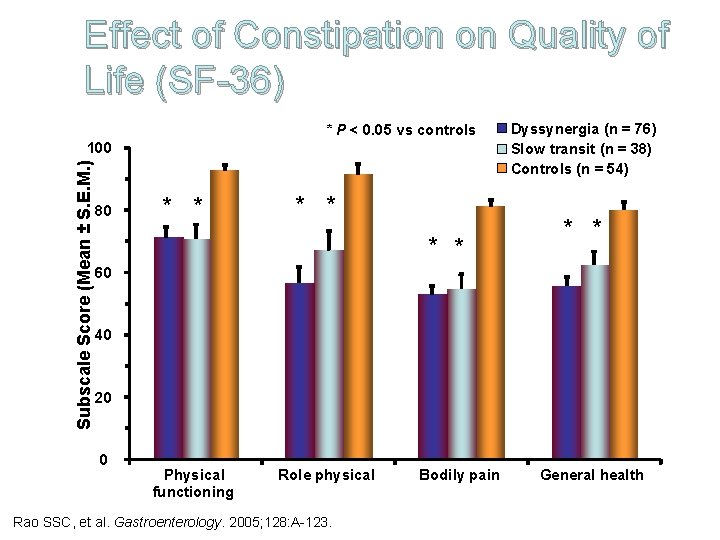
Effect of Constipation on Quality of Life (SF-36) * P < 0. 05 vs controls Subscale Score (Mean ± S. E. M. ) 100 80 * * * Dyssynergia (n = 76) Slow transit (n = 38) Controls (n = 54) * * 60 40 20 0 Physical functioning Role physical Rao SSC, et al. Gastroenterology. 2005; 128: A-123. Bodily pain General health
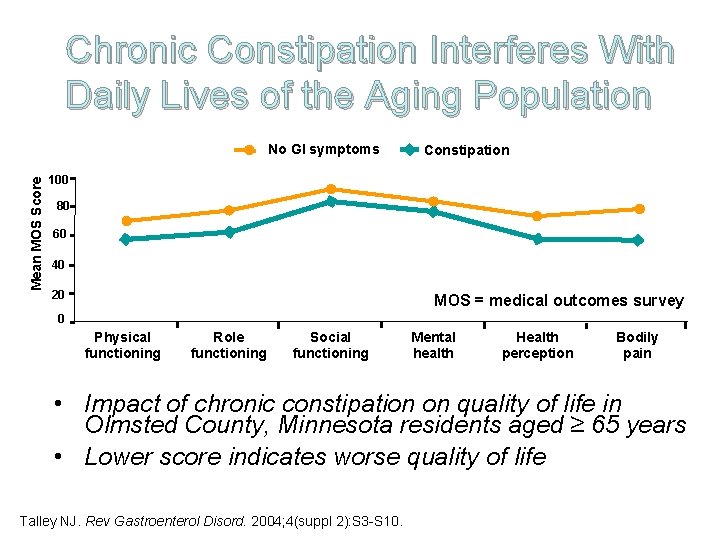
Chronic Constipation Interferes With Daily Lives of the Aging Population Mean MOS Score No GI symptoms Constipation 100 80 60 40 20 MOS = medical outcomes survey 0 Physical functioning Role functioning Social functioning Mental health Health perception Bodily pain • Impact of chronic constipation on quality of life in Olmsted County, Minnesota residents aged ≥ 65 years • Lower score indicates worse quality of life Talley NJ. Rev Gastroenterol Disord. 2004; 4(suppl 2): S 3 -S 10.
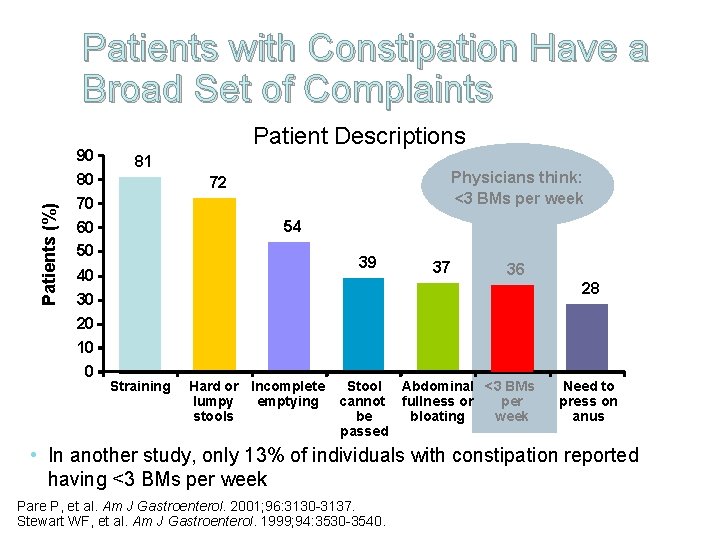
Patients (%) Patients with Constipation Have a Broad Set of Complaints 90 80 70 60 50 40 30 20 10 0 Patient Descriptions 81 Physicians think: <3 BMs per week 72 54 39 37 36 28 Straining Hard or Incomplete emptying lumpy stools Stool Abdominal <3 BMs cannot fullness or per be bloating week passed Need to press on anus • In another study, only 13% of individuals with constipation reported having <3 BMs per week Pare P, et al. Am J Gastroenterol. 2001; 96: 3130 -3137. Stewart WF, et al. Am J Gastroenterol. 1999; 94: 3530 -3540.
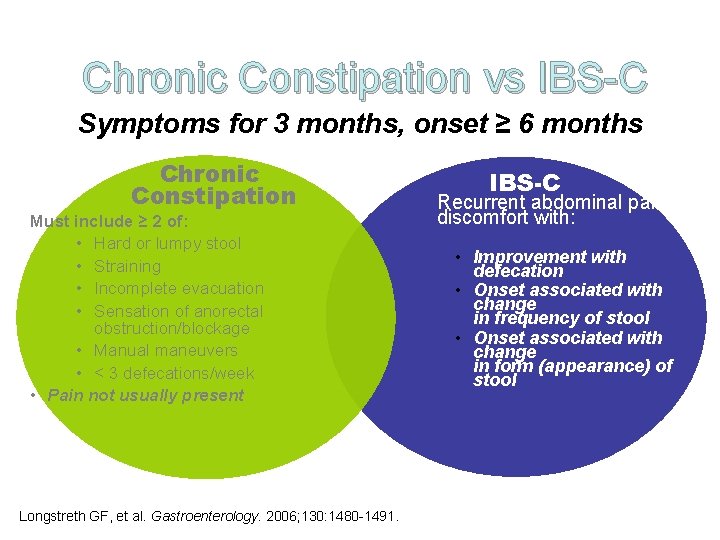
Chronic Constipation vs IBS-C Symptoms for 3 months, onset ≥ 6 months Chronic Constipation Must include ≥ 2 of: • Hard or lumpy stool • Straining • Incomplete evacuation • Sensation of anorectal obstruction/blockage • Manual maneuvers • < 3 defecations/week • Pain not usually present Longstreth GF, et al. Gastroenterology. 2006; 130: 1480 -1491. IBS-C Recurrent abdominal pain/ discomfort with: • Improvement with defecation • Onset associated with change in frequency of stool • Onset associated with change in form (appearance) of stool
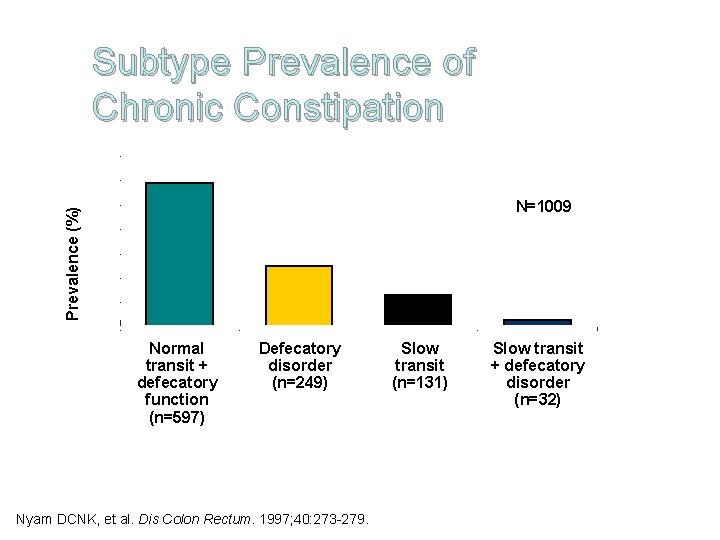
Subtype Prevalence of Chronic Constipation 70 Prevalence (%) 60 N=1009 50 40 30 20 10 0 Normal transit + defecatory function (n=597) Defecatory disorder (n=249) Nyam DCNK, et al. Dis Colon Rectum. 1997; 40: 273 -279. Slow transit (n=131) Slow transit + defecatory disorder (n=32)
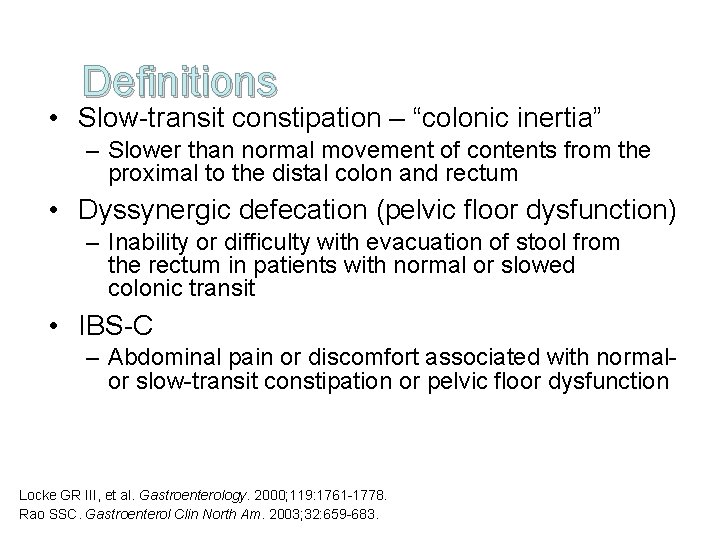
Definitions • Slow-transit constipation – “colonic inertia” – Slower than normal movement of contents from the proximal to the distal colon and rectum • Dyssynergic defecation (pelvic floor dysfunction) – Inability or difficulty with evacuation of stool from the rectum in patients with normal or slowed colonic transit • IBS-C – Abdominal pain or discomfort associated with normalor slow-transit constipation or pelvic floor dysfunction Locke GR III, et al. Gastroenterology. 2000; 119: 1761 -1778. Rao SSC. Gastroenterol Clin North Am. 2003; 32: 659 -683.
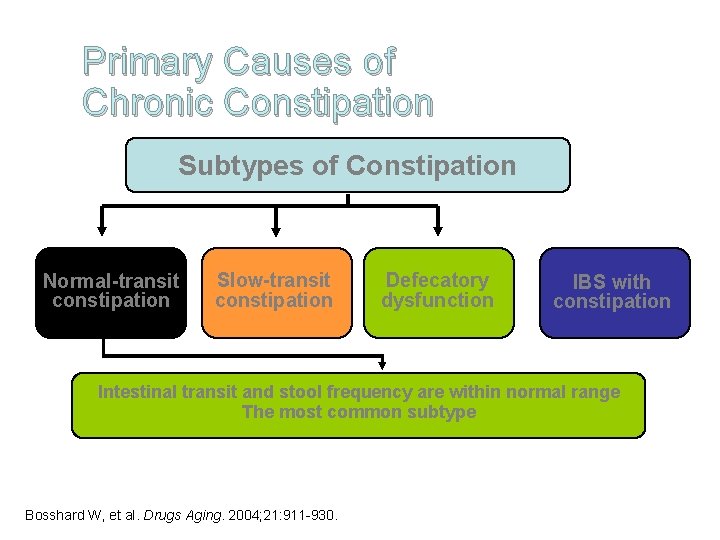
Primary Causes of Chronic Constipation Subtypes of Constipation Normal-transit constipation Slow-transit constipation Defecatory dysfunction IBS with constipation Intestinal transit and stool frequency are within normal range The most common subtype Bosshard W, et al. Drugs Aging. 2004; 21: 911 -930.
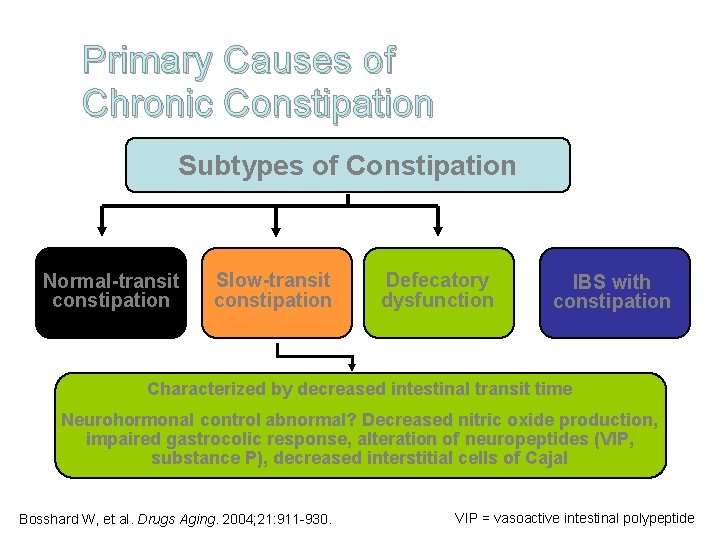
Primary Causes of Chronic Constipation Subtypes of Constipation Normal-transit constipation Slow-transit constipation Defecatory dysfunction IBS with constipation Characterized by decreased intestinal transit time Neurohormonal control abnormal? Decreased nitric oxide production, impaired gastrocolic response, alteration of neuropeptides (VIP, substance P), decreased interstitial cells of Cajal Bosshard W, et al. Drugs Aging. 2004; 21: 911 -930. VIP = vasoactive intestinal polypeptide

Primary Causes of Chronic Constipation Subtypes of Constipation Normal-transit constipation Slow-transit constipation Defecatory dysfunction IBS with constipation Pelvic floor dyssynergia, megarectum, rectocele, perineal descent More frequent in older women – childbirth trauma Pathogenesis may be multifactorial – structural problem Bosshard W, et al. Drugs Aging. 2004; 21: 911 -930.
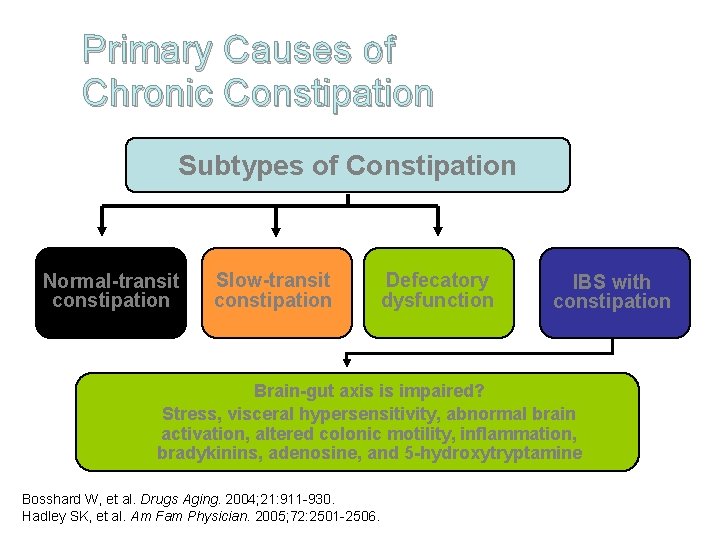
Primary Causes of Chronic Constipation Subtypes of Constipation Normal-transit constipation Slow-transit constipation Defecatory dysfunction IBS with constipation Brain-gut axis is impaired? Stress, visceral hypersensitivity, abnormal brain activation, altered colonic motility, inflammation, bradykinins, adenosine, and 5 -hydroxytryptamine Bosshard W, et al. Drugs Aging. 2004; 21: 911 -930. Hadley SK, et al. Am Fam Physician. 2005; 72: 2501 -2506.
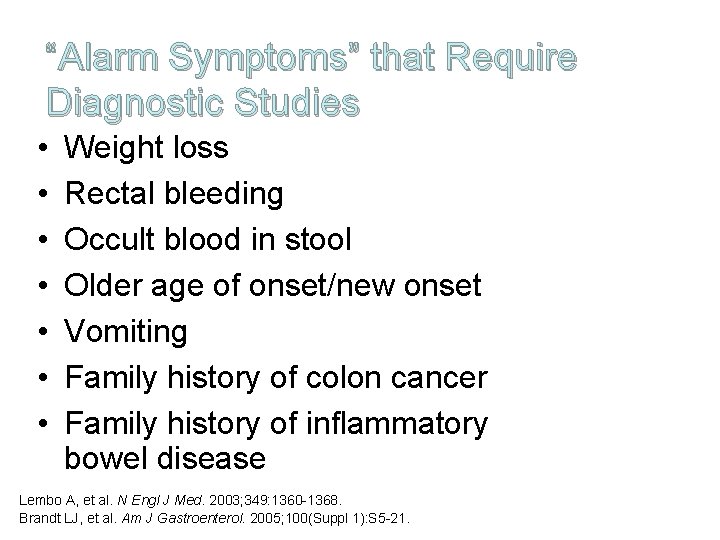
“Alarm Symptoms” that Require Diagnostic Studies • • Weight loss Rectal bleeding Occult blood in stool Older age of onset/new onset Vomiting Family history of colon cancer Family history of inflammatory bowel disease Lembo A, et al. N Engl J Med. 2003; 349: 1360 -1368. Brandt LJ, et al. Am J Gastroenterol. 2005; 100(Suppl 1): S 5 -21.
ACG Task Force Recommendations on Diagnostic Testing • Among chronic constipation patients without alarm symptoms or signs, routine use of diagnostic tests is not recommended – The routine approach to a patient with symptoms of chronic constipation without alarm signs or symptoms should be empiric treatment without performance of diagnostic testing • Diagnostic studies are indicated in patients with alarm signs or symptoms • Routine use of colon cancer screening tools is recommended in patients aged ≥ 50 ACG years = American College Brandt LJ, et al. Am J Gastroenterol. 2005; 100(Suppl 1): S 5 -S 21. of Gastroenterology
Assessment of Constipation in Nursing Facilities • Multidisciplinary approach – MD, nursing, pharmacist, dietician • MDS initial evaluation – Bowel function – Ability to use toilet • Accurate bowel history – From resident, if possible • Rule out secondary factors – Medications, disease states, diet
Non-Medical Risk Factors for Constipation in Nursing Facilities • Immobility • Inadequate fluid intake • Diet – not enough fiber, reduced intake • Medications – Narcotics – Iron – Anticholinergic side effects
Laxative Use in Nursing Facilities • 59%-78% of residents use laxatives at least on an intermittent basis • 50% were on more than 1 laxative • Most commonly used: – Stool softeners – Saline laxatives – Stimulant laxatives – Osmotic laxatives Phillips C, et al. J Am Med Dir Assoc. 2001; 2: 149 -154.
Opioid-Induced Constipation • 41% of patients on long-term opioids develop constipation – Delayed gastric emptying – Delayed stool transit throughout the GI tract – Decreased peristalsis – These changes can be seen almost immediately, therefore, start laxatives prophylactically • Treat with stimulant or osmotic laxatives Kalso E, et al. Pain. 2004; 112: 372 -380.
Dietary Fiber • Trials of fiber have been inconsistent, but generally fiber in diet leads to laxative use and bowel movements • No set guidelines for the elderly – American Dietetic Association– 10 -13 Gm/1000 kcal • Studies have used: – “laxative” pudding (dates & prunes) – Bran, applesauce, & prune juice mixture – Fiber-rich porridge Tariq SH. J Am Med Dir Assoc. 2007; 8: 209 -218.
Fluids • May only be helpful in dehydrated patients, not in chronic constipation • Adequate hydration is important to general health Exercise • Convincing data is lacking as to efficacy, but overall well-being may improve
Toileting • Set time for defecation – Morning or 30 minutes after meal • Comfortable, safe toilet or commode • Privacy
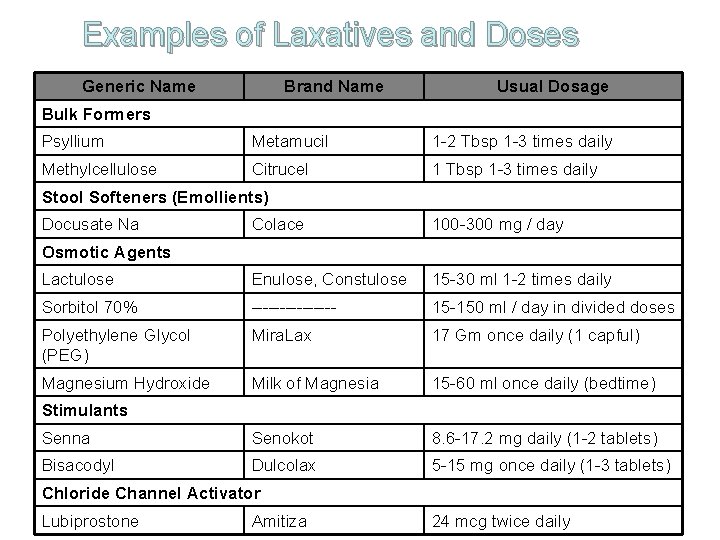
Examples of Laxatives and Doses Generic Name Brand Name Usual Dosage Bulk Formers Psyllium Metamucil 1 -2 Tbsp 1 -3 times daily Methylcellulose Citrucel 1 Tbsp 1 -3 times daily Stool Softeners (Emollients) Docusate Na Colace 100 -300 mg / day Lactulose Enulose, Constulose 15 -30 ml 1 -2 times daily Sorbitol 70% -------- 15 -150 ml / day in divided doses Polyethylene Glycol (PEG) Mira. Lax 17 Gm once daily (1 capful) Magnesium Hydroxide Milk of Magnesia 15 -60 ml once daily (bedtime) Senna Senokot 8. 6 -17. 2 mg daily (1 -2 tablets) Bisacodyl Dulcolax 5 -15 mg once daily (1 -3 tablets) Osmotic Agents Stimulants Chloride Channel Activator Lubiprostone Amitiza 24 mcg twice daily
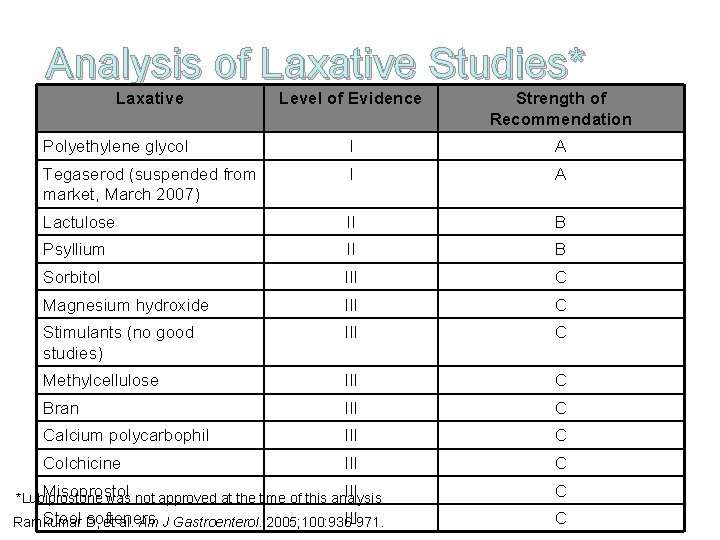
Analysis of Laxative Studies* Laxative Level of Evidence Strength of Recommendation Polyethylene glycol I A Tegaserod (suspended from market, March 2007) I A Lactulose II B Psyllium II B Sorbitol III C Magnesium hydroxide III C Stimulants (no good studies) III C Methylcellulose III C Bran III C Calcium polycarbophil III C Colchicine III C Misoprostol III *Lubiprostone was not approved at the time of this analysis C Stool D, softeners III Ramkumar et al. Am J Gastroenterol. 2005; 100: 936 -971. C
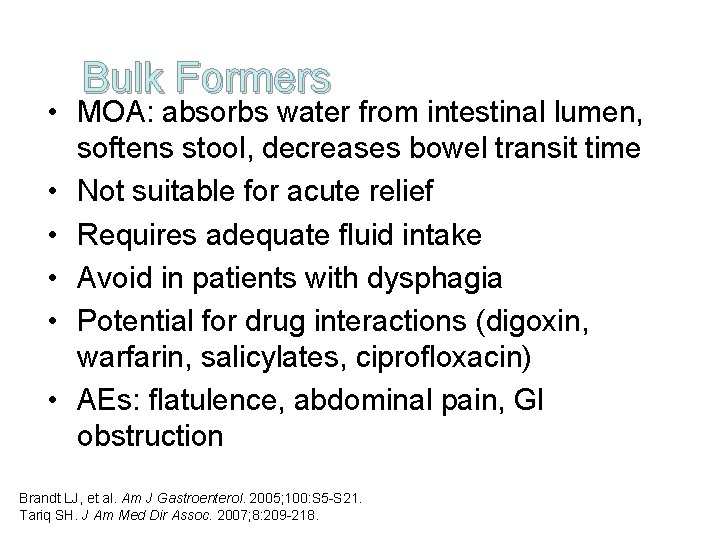
Bulk Formers • MOA: absorbs water from intestinal lumen, softens stool, decreases bowel transit time • Not suitable for acute relief • Requires adequate fluid intake • Avoid in patients with dysphagia • Potential for drug interactions (digoxin, warfarin, salicylates, ciprofloxacin) • AEs: flatulence, abdominal pain, GI obstruction Brandt LJ, et al. Am J Gastroenterol. 2005; 100: S 5 -S 21. Tariq SH. J Am Med Dir Assoc. 2007; 8: 209 -218.
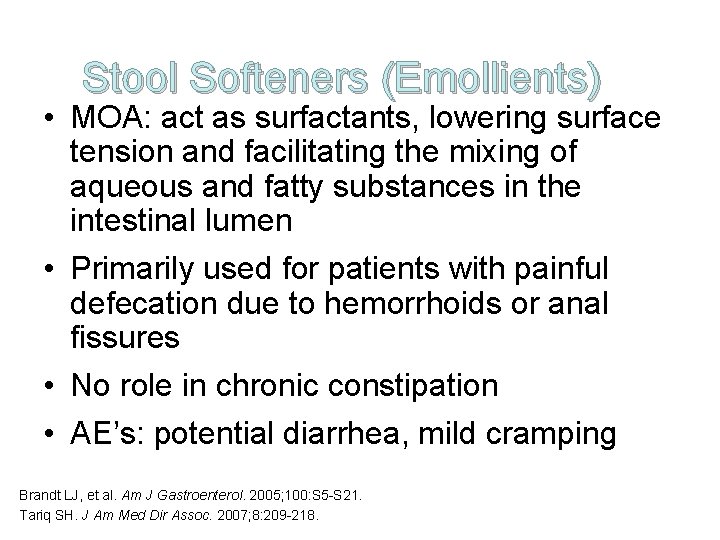
Stool Softeners (Emollients) • MOA: act as surfactants, lowering surface tension and facilitating the mixing of aqueous and fatty substances in the intestinal lumen • Primarily used for patients with painful defecation due to hemorrhoids or anal fissures • No role in chronic constipation • AE’s: potential diarrhea, mild cramping Brandt LJ, et al. Am J Gastroenterol. 2005; 100: S 5 -S 21. Tariq SH. J Am Med Dir Assoc. 2007; 8: 209 -218.
Osmotic Laxatives • MOA: draws fluid into the intestinal lumen by osmotic action, thus increasing intraluminal pressure & stimulating gut motility • PEG – no studies yet in older adults • Lactulose & sorbitol – similar effects in older adults • Saline laxatives can cause electrolyte imbalance – Avoid use in patients with renal impairment • AE’s: diarrhea, abdominal discomfort, flatulence Brandt LJ, et al. Am J Gastroenterol. 2005; 100: S 5 -S 21. Tariq SH. J Am Med Dir Assoc. 2007; 8: 209 -218.
Stimulant Laxatives • MOA: stimulates nerve plexus of intestines, increases peristalsis, increases secretion of fluid & electrolytes • Use in lowest effective dose • Chronic use leads to tolerance • Useful in opioid-induced constipation • AE’s: abdominal pain, electrolyte imbalance, melanosis coli (long-term use) Brandt LJ, et al. Am J Gastroenterol. 2005; 100: S 5 -S 21. Tariq SH. J Am Med Dir Assoc. 2007; 8: 209 -218.
• Prokinetic Agents Metoclopramide & erythromycin work on the upper GI tract to promote peristalsis – Little benefit for constipation • Tegaserod was approved for chronic constipation in persons <65 yo, but voluntarily suspended from market by the manufacturer in March 2007 after a pooled analysis of 29 placebo-controlled shortterm trials found a statistically significant increase in cardiovascular ischemic events, including heart attack, angina, and stroke – July 2007 – FDA approved restricted use under investigational treatment protocol for women <55 yo with IBS-C or chronic idiopathic constipation Tariq SH. J Am Med Dir Assoc. 2007; 8: 209 -218.
Chloride Channel Activator Lubiprostone • MOA: enhances chloride-rich fluid secretion into intestinal lumen without affecting Na+, K+, or Cl- levels. No effect on selected smooth muscle (ileum longitudinal smooth muscle, ileum circular smooth muscle, vas deferens, and iris sphincter) contraction • Approved for treatment of chronic idiopathic constipation in adults • Minimal systemic absorption, no significant drug interactions • Compared to placebo, increases bowel movements, decreases straining, improves stool consistency Tariq SH. J Am Med Dir Assoc. 2007; 8: 209 -218. Johanson JF, et al. Gastroenterology. 2004; 126(Suppl 2): A 100. Abstract 749. Johanson JF. Gastroenterology. 2003; 124: A-48.
Enemas • Reserve for acute situations • Avoid soap suds • Small volume tap water enemas are preferred • Phosphate containing enemas may cause hyperphosphatemia, especially in renal impairment • Watch for abuse in the elderly Tariq SH. J Am Med Dir Assoc. 2007; 8: 209 -218.

When to refer for treatment constipation • Refractory constipation for anorectal testing • Dyssynergic defecation may benefit from biofeedback therapy • Alarm symptoms or over age 50 for colonoscopy • Surgery for severe colonic inertia • If chronic complaint but having BMs – consider depression, refer psych
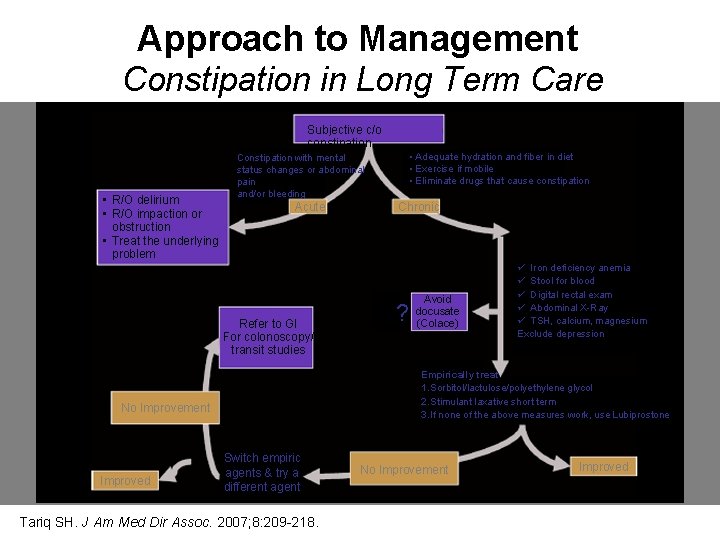
Approach to Management Constipation in Long Term Care Subjective c/o constipation • R/O delirium • R/O impaction or obstruction • Treat the underlying problem Acute Refer to GI For colonoscopy/ transit studies Chronic ? Avoid docusate (Colace) ü Iron deficiency anemia ü Stool for blood ü Digital rectal exam ü Abdominal X-Ray ü TSH, calcium, magnesium Exclude depression Empirically treat 1. Sorbitol/lactulose/polyethylene glycol 2. Stimulant laxative short term 3. If none of the above measures work, use Lubiprostone No Improvement Improved • Adequate hydration and fiber in diet • Exercise if mobile • Eliminate drugs that cause constipation Constipation with mental status changes or abdominal pain and/or bleeding Switch empiric agents & try a different agent Tariq SH. J Am Med Dir Assoc. 2007; 8: 209 -218. No Improvement Improved
Constipation and survey implications • • Care plan Quality of Life evaluation Medication review Scheduled treatment, not prn Know adult bowel history Doctor involved Refer when appropriate Quality Indicator
Constipation and survey implications • F 309 Quality of Care –Each resident must receive and the facility must provide the necessary care and services to attain the highest practicable physical, mental and psychosocial well-being, in accordance with the comprehensive assessment and plan of care – May include fecal impaction
Constipation and survey implications • F 309 - Highest possible level of functioning and well-being, limited by individual recognized pathology and normal aging – Determine if avoidable or unavoidable – Need: • Accurate and complete assessment • Care plan • Evaluation of the results of the interventions and revising the interventions as necessary
Constipation Summary • Know your patient • Common problem in elderly related to aging process and multiple illnesses in elderly • Medications for etiology and treatment • Exercise/increase activity • Fiber • Care plan • Quality of life
- Slides: 49