Consequences of cancer treatments Karen Morgan Macmillan Consultant


- Slides: 21
Consequences of cancer treatments Karen Morgan Macmillan Consultant Radiographer Jan 13 th 2015
Background - UK / year Macmillan facts and figures – ▫ 2 million are living with consequences of cancer treatment ▫ Estimated 500, 000 people living with more than one problem ▫ Physical and emotional ▫ Cancer survivors estimated to rise to 4 million in next 20 years (Source - Throwing light on the consequences of cancer and its treatment, Macmillan Cancer Support 2013)
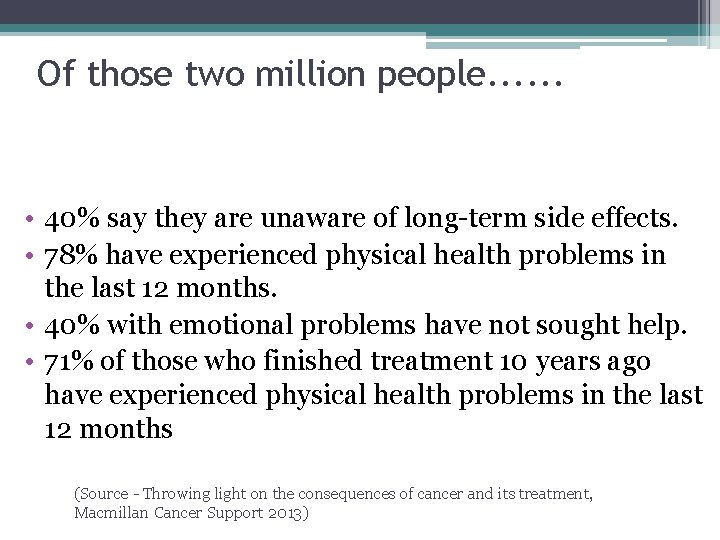
Of those two million people. . . • 40% say they are unaware of long-term side effects. • 78% have experienced physical health problems in the last 12 months. • 40% with emotional problems have not sought help. • 71% of those who finished treatment 10 years ago have experienced physical health problems in the last 12 months (Source - Throwing light on the consequences of cancer and its treatment, Macmillan Cancer Support 2013)
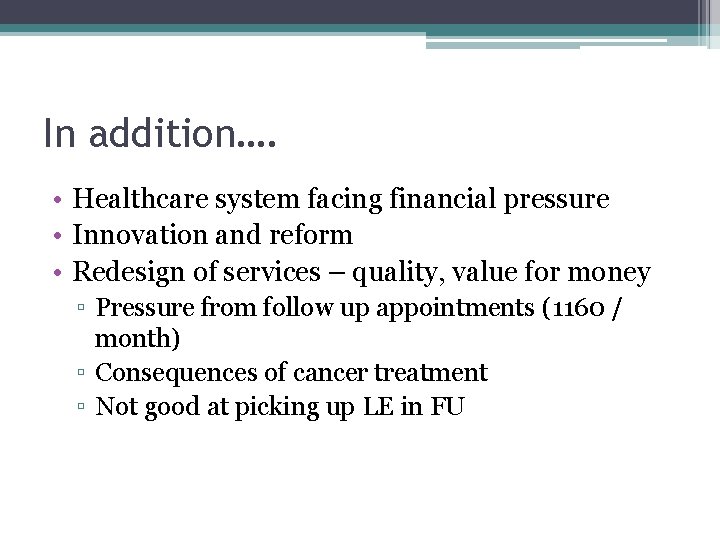
In addition…. • Healthcare system facing financial pressure • Innovation and reform • Redesign of services – quality, value for money ▫ Pressure from follow up appointments (1160 / month) ▫ Consequences of cancer treatment ▫ Not good at picking up LE in FU
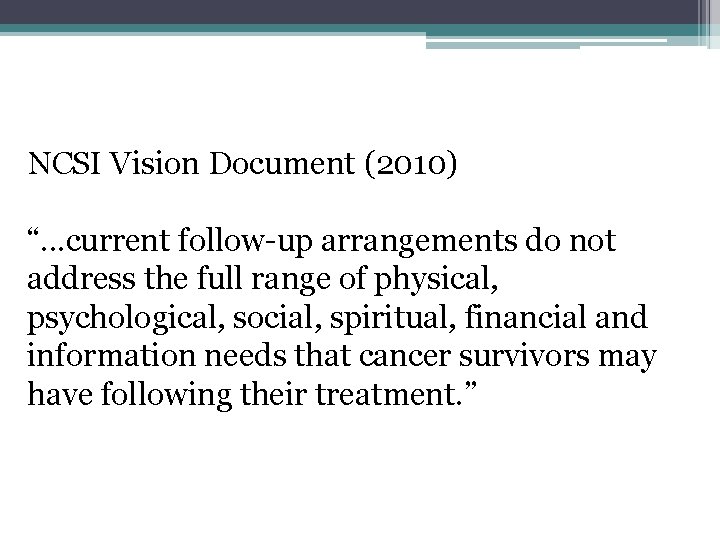
NCSI Vision Document (2010) “. . . current follow-up arrangements do not address the full range of physical, psychological, social, spiritual, financial and information needs that cancer survivors may have following their treatment. ”

Quality of Life (Radiotherapy) Acute toxicities • Occur in tissues with rapid cell turnover, (eg mucous membranes) • Acute inflammatory response • Peaks at 2 -3 weeks • Usually short lived, resolve within 3 months • Patients recover, but often need supportive therapeutic and pharmacological strategies
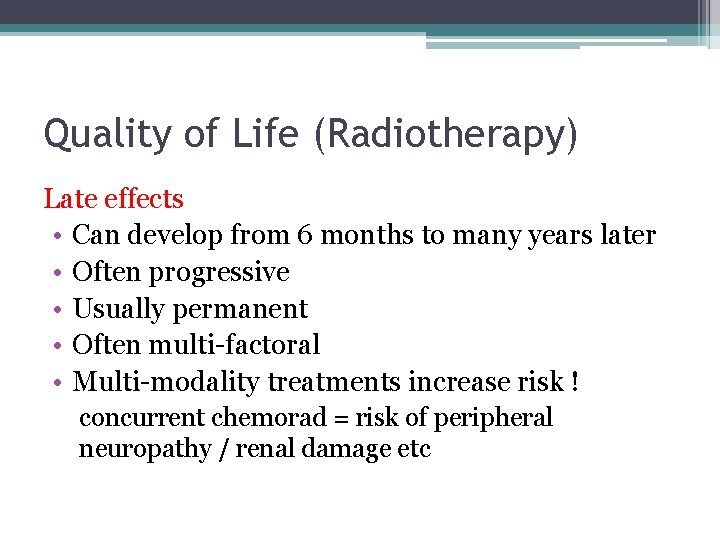
Quality of Life (Radiotherapy) Late effects • Can develop from 6 months to many years later • Often progressive • Usually permanent • Often multi-factoral • Multi-modality treatments increase risk ! concurrent chemorad = risk of peripheral neuropathy / renal damage etc
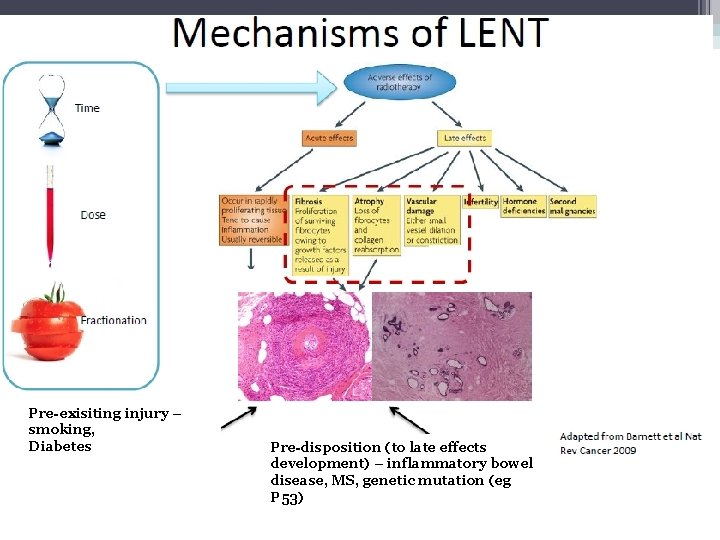
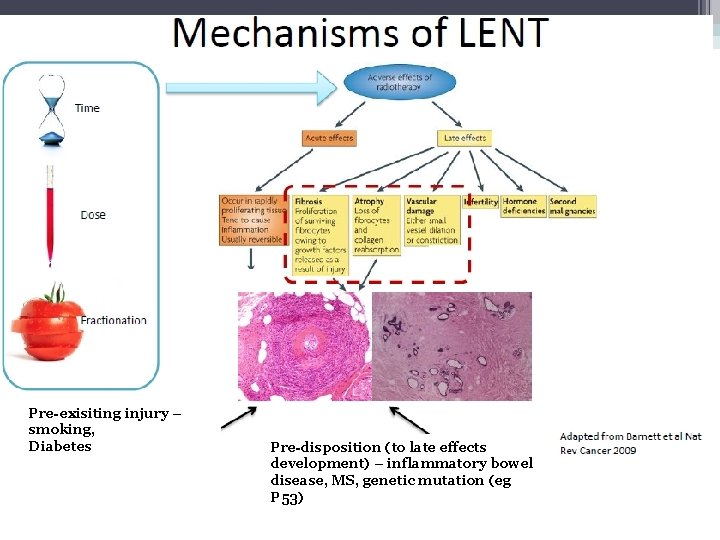
Pre-exisiting injury – smoking, Diabetes Pre-disposition (to late effects development) – inflammatory bowel disease, MS, genetic mutation (eg P 53)
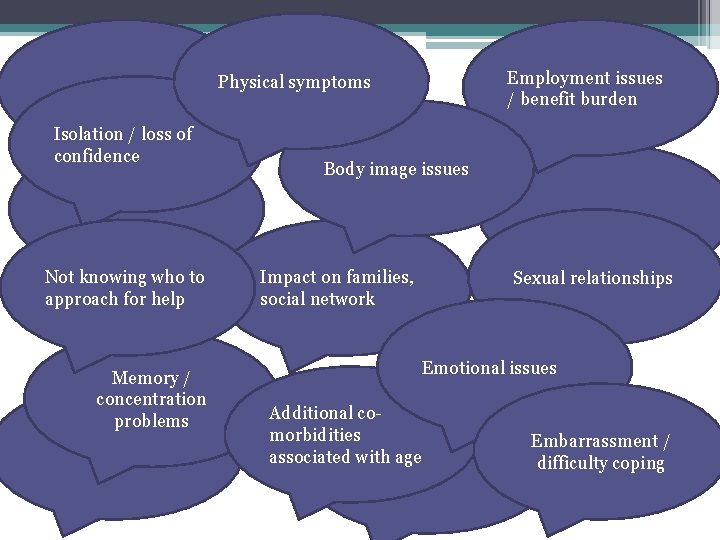
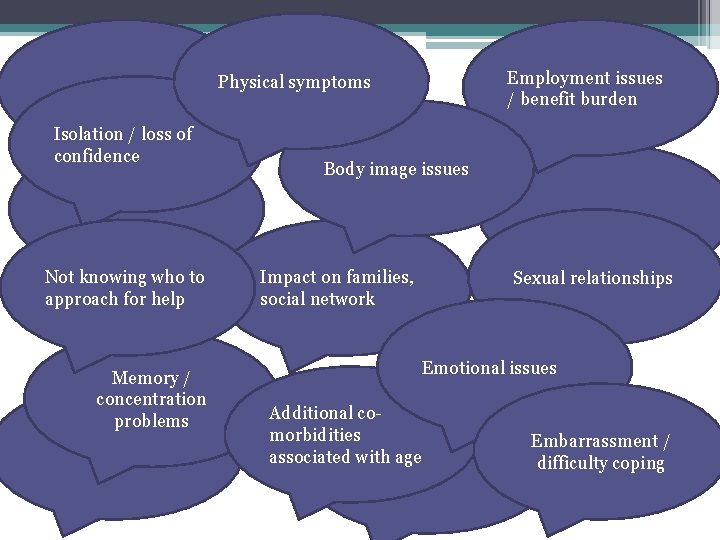
Employment issues / benefit burden Physical symptoms Isolation / loss of confidence Not knowing who to approach for help Memory / concentration problems Body image issues Impact on families, social network Sexual relationships Emotional issues Additional comorbidities associated with age Embarrassment / difficulty coping
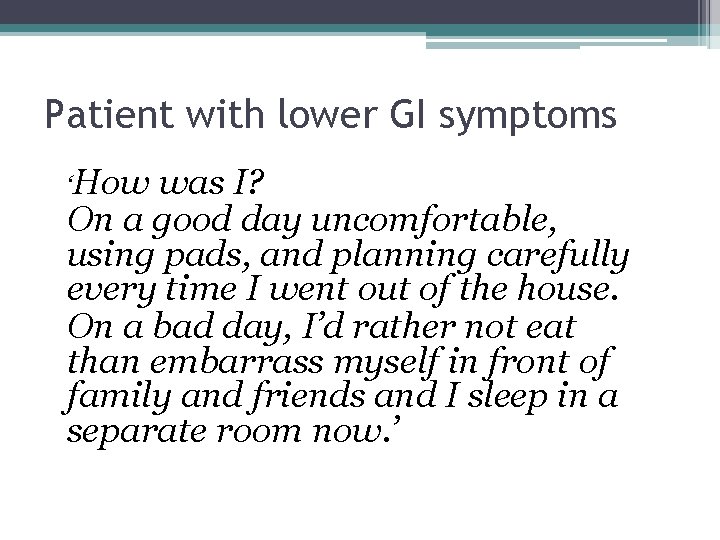
Patient with lower GI symptoms ‘How was I? On a good day uncomfortable, using pads, and planning carefully every time I went out of the house. On a bad day, I’d rather not eat than embarrass myself in front of family and friends and I sleep in a separate room now. ’
Main issues (1) • Historical legacy – patient treated elsewhere • SW – Age profile – LE combined with other co-morbidities • Little information on the scale of the problem! • Symptoms managed poorly, no guidance ! • Unnecessary investigations / ineffective treatments • Impact on NHS resources • Who takes responsibility ?

Main issues (2) * LE services – few specialist services over large geographical area. * Some services regionally (referrals, funding, travel) * LE services traditionally associated with paediatric oncology * NCSI recovery package (approach is not standardised)
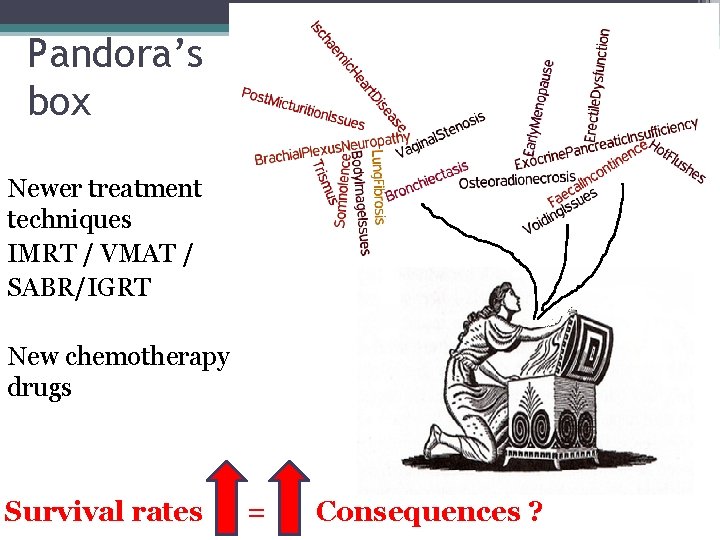
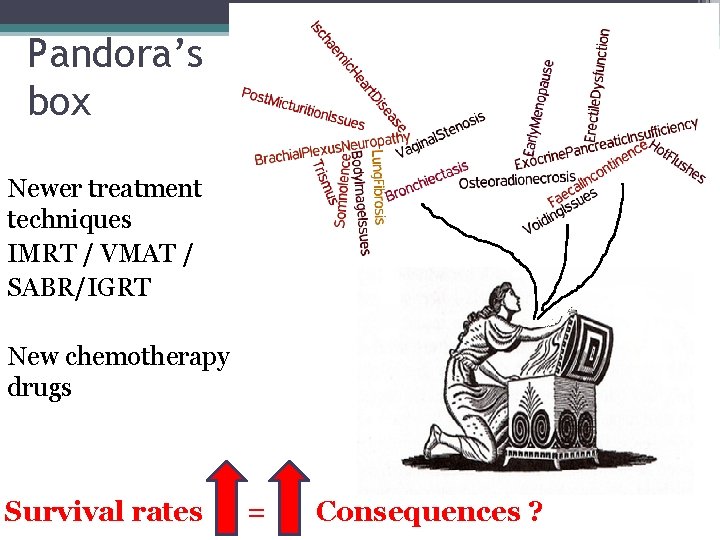
Pandora’s box Newer treatment techniques IMRT / VMAT / SABR/IGRT New chemotherapy drugs Survival rates = Consequences ?
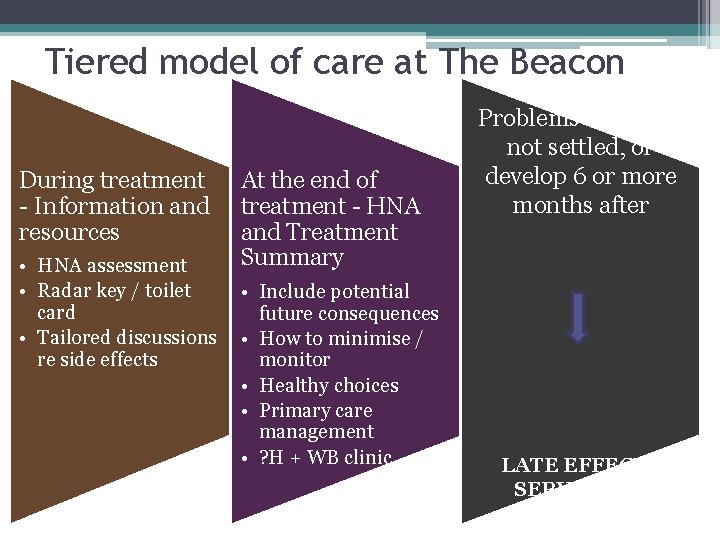
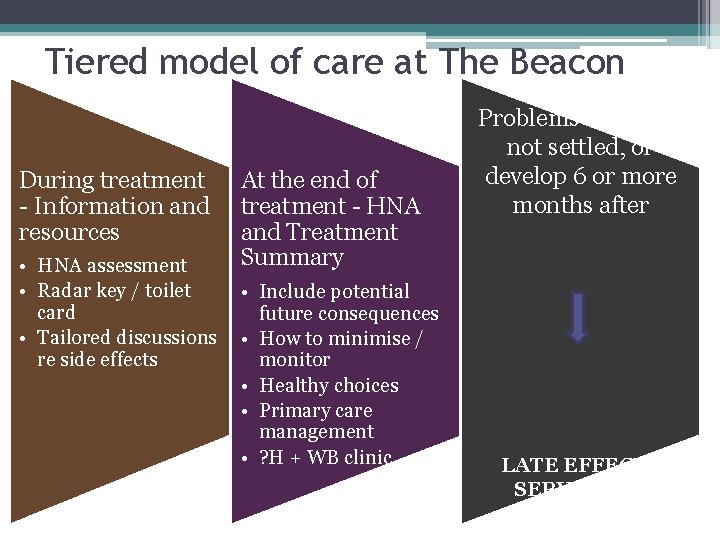
Tiered model of care at The Beacon During treatment - Information and resources • HNA assessment • Radar key / toilet card • Tailored discussions re side effects At the end of treatment - HNA and Treatment Summary • Include potential future consequences • How to minimise / monitor • Healthy choices • Primary care management • ? H + WB clinic Problems that have not settled, or develop 6 or more months after LATE EFFECTS SERVICES + THOSE
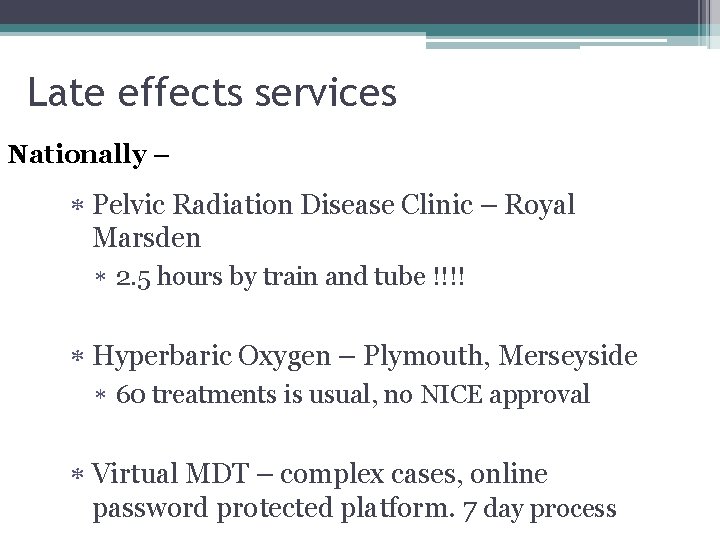
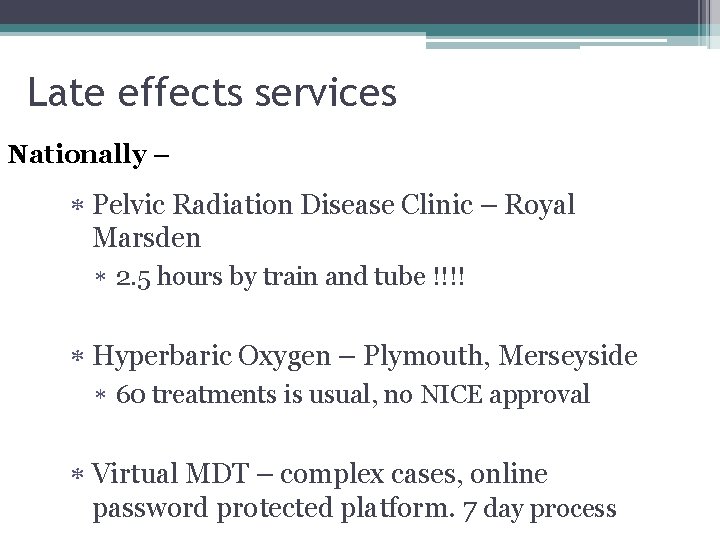
Late effects services Nationally – Pelvic Radiation Disease Clinic – Royal Marsden 2. 5 hours by train and tube !!!! Hyperbaric Oxygen – Plymouth, Merseyside 60 treatments is usual, no NICE approval Virtual MDT – complex cases, online password protected platform. 7 day process
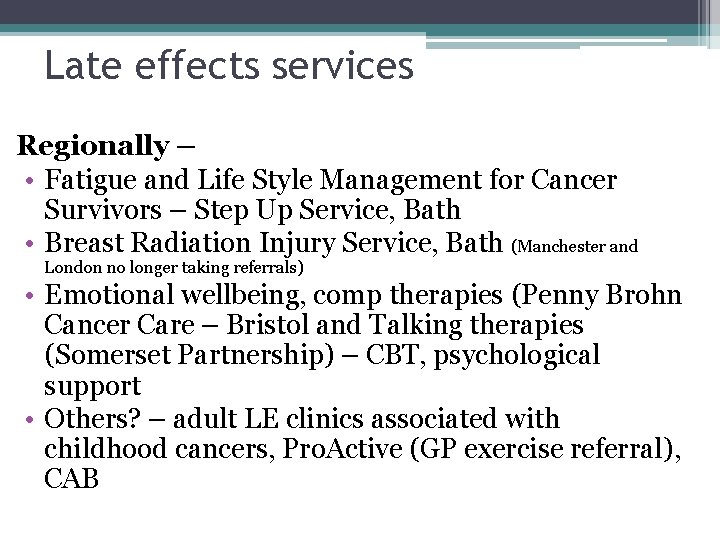
Late effects services Regionally – • Fatigue and Life Style Management for Cancer Survivors – Step Up Service, Bath • Breast Radiation Injury Service, Bath (Manchester and London no longer taking referrals) • Emotional wellbeing, comp therapies (Penny Brohn Cancer Care – Bristol and Talking therapies (Somerset Partnership) – CBT, psychological support • Others? – adult LE clinics associated with childhood cancers, Pro. Active (GP exercise referral), CAB
Late effects services Locally • Gastroenterologist (interest in PRD) • Endocrinologist • Local therapists – (SLT, dietician, physio, lymphoedema) • ED clinic • Pain clinic • Women’s health • Nurse Counsellors
Where are we now? • New guidance for LE symptoms, other sites to follow – implementation? Succinct algorithms for ease ? • Education for primary care / self development (RMH e module) • Assessment / screening tools / PROMS vital ! • Tiered model of care • Utilisation of services and resources • Referral pathways? CCG / Regional Survivorship groups
Making a difference ! * Prevention to minimise wherever possible * Inform patients of potential LE * Identify those at risk * Assessment – HNA address unmet needs * Support patients through local and regional LE pathways * Patients gain independence / return to work * Prevents unnecessary hospital admissions / GP consultations * Saves NHS money!. . . .
Golden nuggets ! • For every £ 1 spent on lymphoedema treatments, the service estimates the NHS saves £ 100 in reduced hospital admissions. • If just half of breast cancer survivors who initially return to work but then leave were helped to stay in work, the economy could save £ 30 M every year. Reference: NHS London (2012) Allied Health Professional QIPP pathway for cancer
Further information or direct referrals Karen Morgan, Macmillan Consultant Radiographer (Late Effects), c/o The Radiotherapy Dept, The Beacon Centre, Taunton, TA 1 5 DA. Telephone 01823 342933 Email: karen. morgan@tst. nhs. uk
 Macmillan professional
Macmillan professional Why did macmillan resign
Why did macmillan resign Motores macmillan
Motores macmillan London joint stock bank v macmillan and arthur
London joint stock bank v macmillan and arthur Empresa e iniciativa emprendedora macmillan
Empresa e iniciativa emprendedora macmillan Dr patrick macmillan
Dr patrick macmillan Macmillan professional
Macmillan professional Macmillan profesional
Macmillan profesional Macmillan professional
Macmillan professional Macmillan profesional
Macmillan profesional Recursos humanos macmillan
Recursos humanos macmillan Punto continuo intradermico
Punto continuo intradermico Macmillan publishers
Macmillan publishers Macmillan next steps
Macmillan next steps Myeloma cure on the horizon
Myeloma cure on the horizon Macmillan plumbing
Macmillan plumbing Ukons acute oncology guidelines
Ukons acute oncology guidelines Adams and miles llp
Adams and miles llp Electricidad basica macmillan
Electricidad basica macmillan Macmillan concerns checklist
Macmillan concerns checklist Alternating treatments design
Alternating treatments design Insomnia treatments
Insomnia treatments