Connective Tissue Diseases Connective tissue diseases CTDs are







- Slides: 36
Connective Tissue Diseases
� Connective tissue diseases (CTDs) are defined as a group of acquired diseases resulting from persistent immune mediated inflammation. � Generation of autoreactive T cells or autoantibodies. � Autoantibodies/autoreactive T cells can attack any organ of the body, resulting in a wide array of signs and symptoms.
The classic autoimmune CTDs include: � Systemic lupus erythematosus (SLE), � Juvenile dermatomyositis/polymyositis � (JDM/PM), � Sjögren’s systemic sclerosis (SSc), syndrome (SS), � undifferentiated � overlap CTD (UTCD) syndromes (mixed CTD (MCTD)
� The clinical presentation of CTD in childhood can range from an acute severe illness mimicking a serious infection, to an insidious onset of disease with gradual accumulation of symptoms and signs over weeks to months. � Should suspect CTD when a child has a multi system disease with no apparent cause.
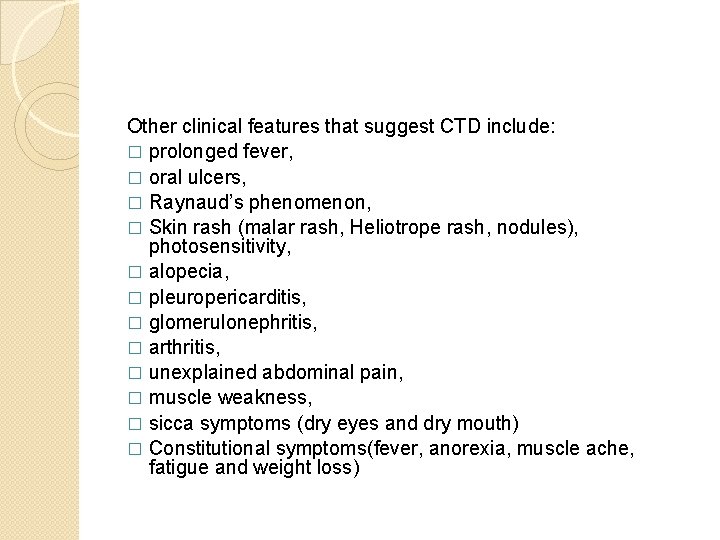
Other clinical features that suggest CTD include: � prolonged fever, � oral ulcers, � Raynaud’s phenomenon, � Skin rash (malar rash, Heliotrope rash, nodules), photosensitivity, � alopecia, � pleuropericarditis, � glomerulonephritis, � arthritis, � unexplained abdominal pain, � muscle weakness, � sicca symptoms (dry eyes and dry mouth) � Constitutional symptoms(fever, anorexia, muscle ache, fatigue and weight loss)
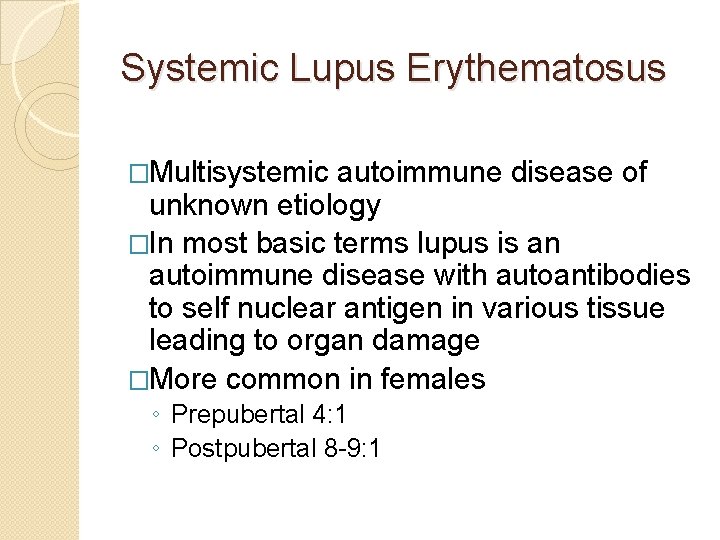
Systemic Lupus Erythematosus �Multisystemic autoimmune disease of unknown etiology �In most basic terms lupus is an autoimmune disease with autoantibodies to self nuclear antigen in various tissue leading to organ damage �More common in females ◦ Prepubertal 4: 1 ◦ Postpubertal 8 -9: 1
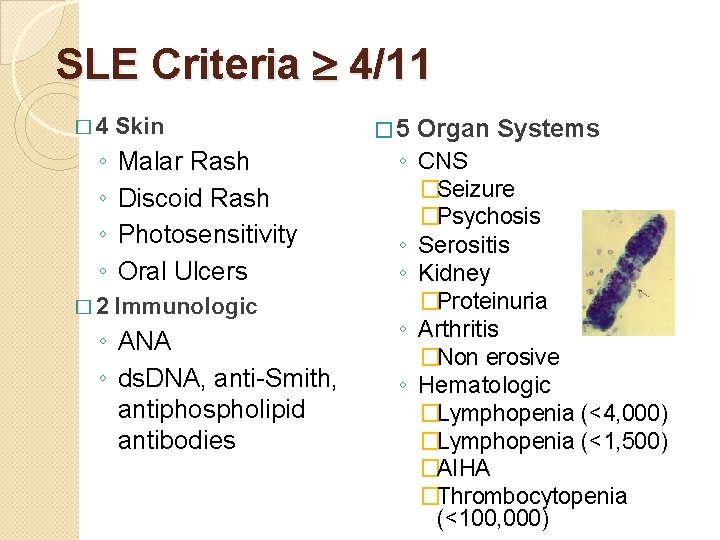
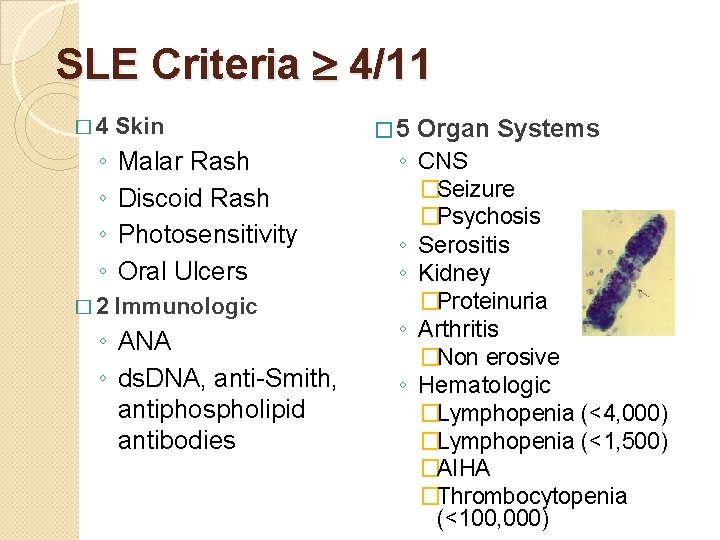
SLE Criteria 4/11 � 4 ◦ ◦ � 2 Skin Malar Rash Discoid Rash Photosensitivity Oral Ulcers Immunologic ◦ ANA ◦ ds. DNA, anti-Smith, antiphospholipid antibodies � 5 Organ Systems ◦ CNS ◦ ◦ �Seizure �Psychosis Serositis Kidney �Proteinuria Arthritis �Non erosive Hematologic �Lymphopenia (<4, 000) �Lymphopenia (<1, 500) �AIHA �Thrombocytopenia (<100, 000)
�In order to make the diagnosis, must have 4 of the 11 criteria at one time or over period of observation.
Clinical Features Hematological system: � Thrombocytopenia, Auto immune hemolytic anemia, Leucopenia, lymphopenia; Renal disease: � Nephrotic syndrome, Acute nephritis, Hypertension; Central nervous system involvement: � Seizures, Psychosis, Stroke, Organic brain syndrome, Chorea Lung disease: � Pleural effusion or acute/chronic pneumonitis; Cardiovascular system: � Pericarditis, myocarditis, Libman Sacks endocarditis;
Mucocutaneous disease: � Photosensitivity, malar rash, alopecia, oral and nasal ulcers; Gastro-intestinal involvement: � GI vasculitis, sterile peritonitis; Musculoskeletal: � Arthritis, arthralgia, myalgia, inflammatory myositis.
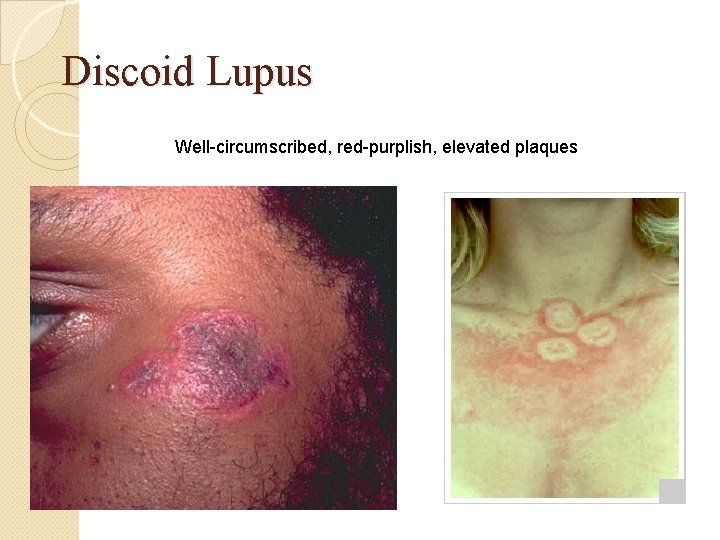
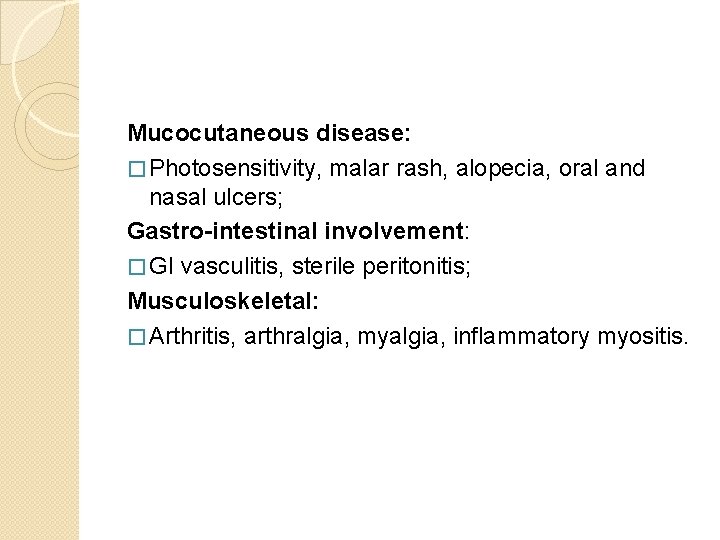
Discoid Lupus Well-circumscribed, red-purplish, elevated plaques
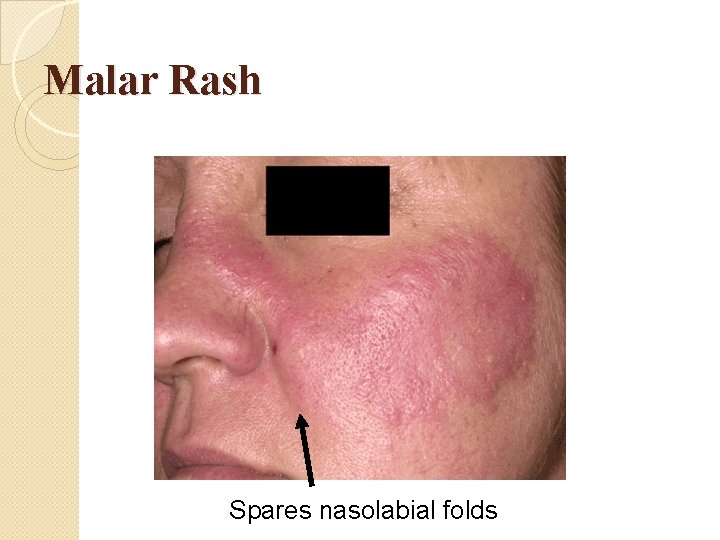
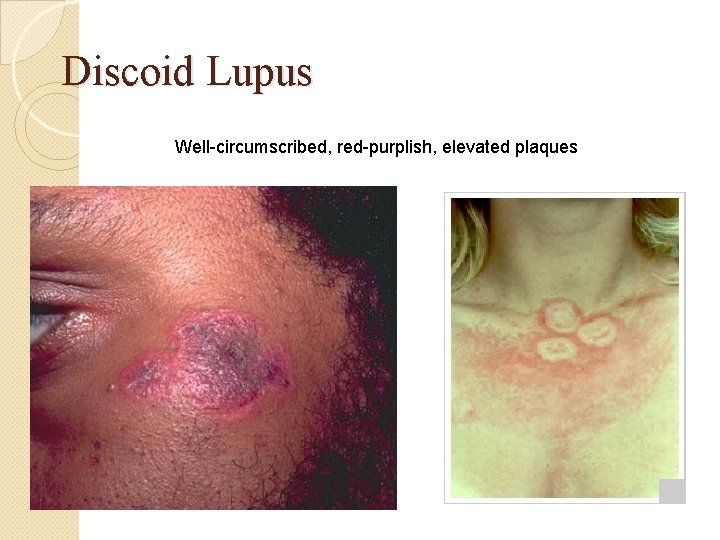
Malar Rash Spares nasolabial folds

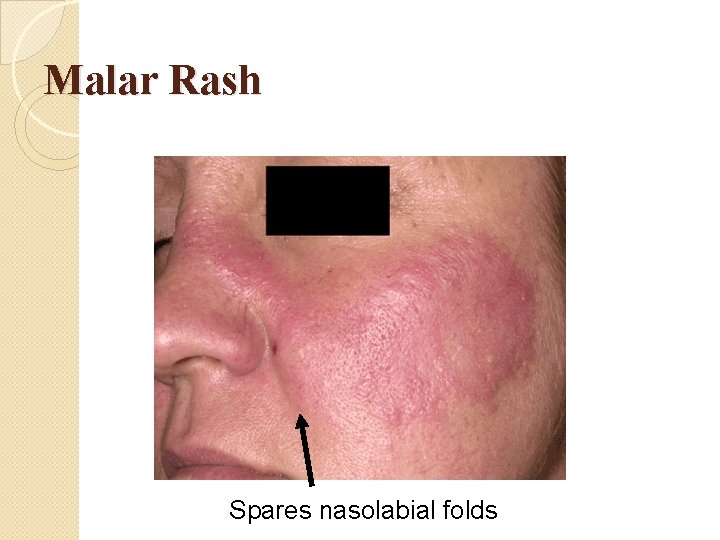
Oral Ulcers

� Malar rash and ulcers on the lips in a child with SLE
Differantial Dx �The important differential diagnosis to be considered are: ◦ ◦ Infections (bacterial and viral), Malignancy, Vasculitis, Chronic granulomatous diseases like sarcoid and autoinflammatory syndrome.

Treatment �NSAIDS �Hydroxychloroquine (Plaquenil) ◦ Ototoxic, ocular side effects �Steroids �Immunosuppressants ◦ Cyclophosphamide ◦ Azathioprine ◦ Cellcept �Sunscreen
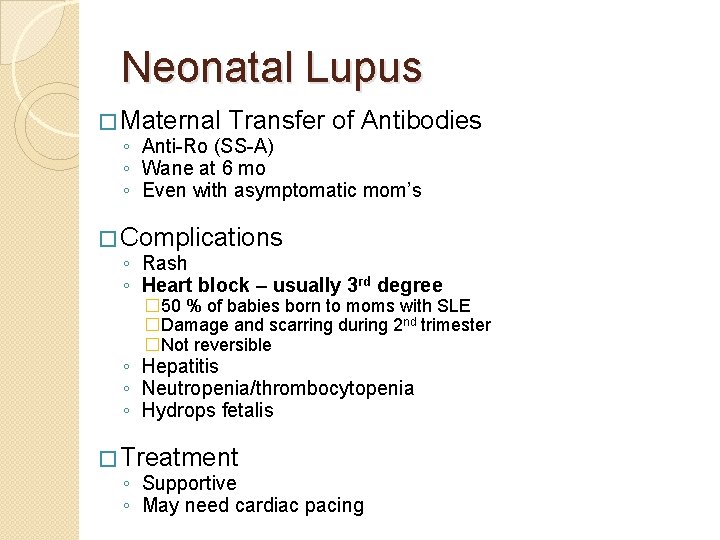
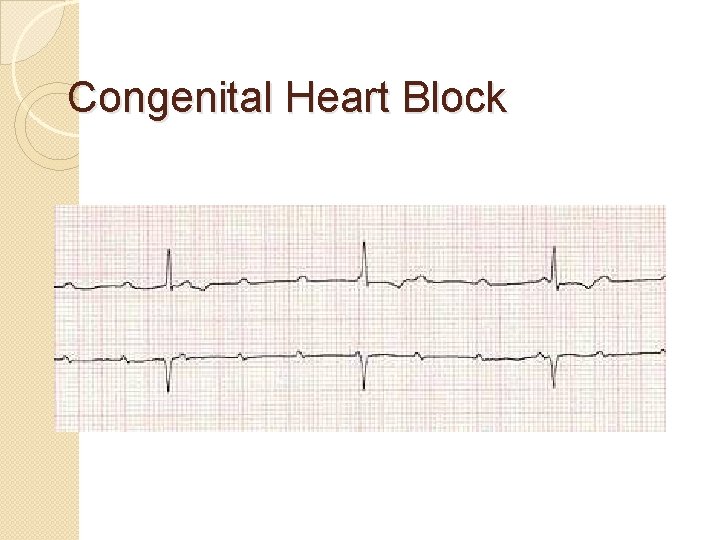
Neonatal Lupus � Maternal Transfer of Antibodies ◦ Anti-Ro (SS-A) ◦ Wane at 6 mo ◦ Even with asymptomatic mom’s � Complications ◦ Rash ◦ Heart block – usually 3 rd degree � 50 % of babies born to moms with SLE �Damage and scarring during 2 nd trimester �Not reversible ◦ Hepatitis ◦ Neutropenia/thrombocytopenia ◦ Hydrops fetalis � Treatment ◦ Supportive ◦ May need cardiac pacing
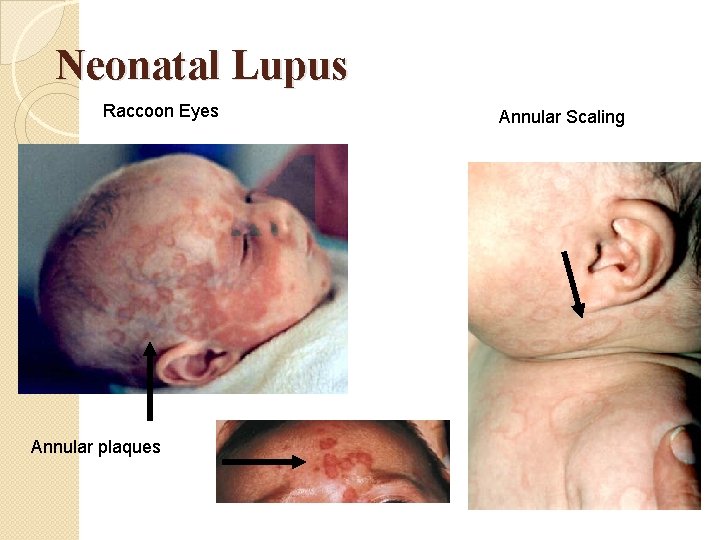
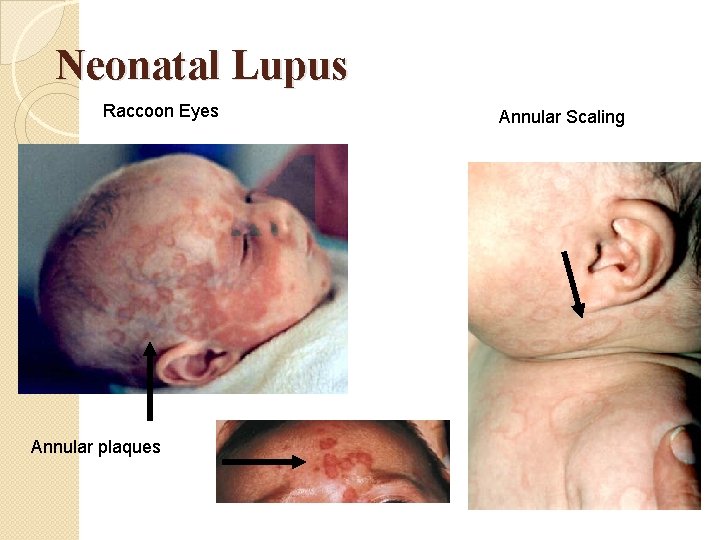
Neonatal Lupus Raccoon Eyes Annular plaques Annular Scaling
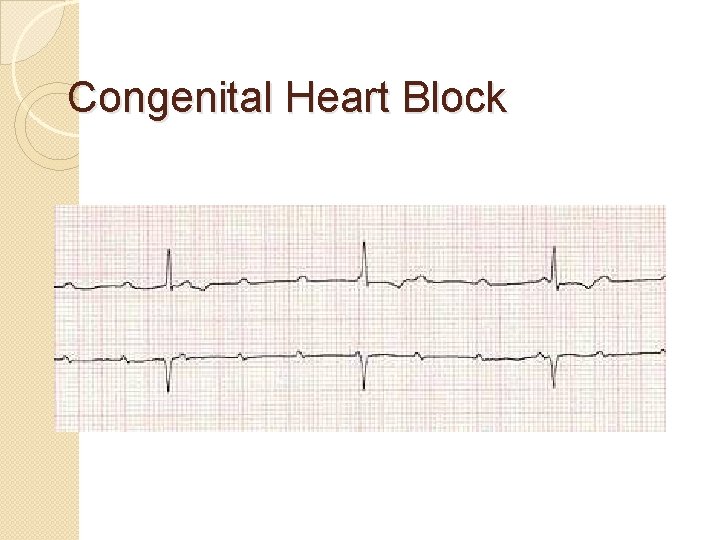
Congenital Heart Block

Drug Induced Lupus � D-SLE ◦ ◦ D = Drugs for the Heart (procainimide) S = Sulfonamides L = Lithium E = Epilepsy medications (anticonvulsants) � Others ◦ INH ◦ Minocycline � Most often reversible � ANA � Anti-histone Ab

Juvenile Dermatomyositis (JDM) �Myopathy and Vasculopathy �Myopathy Symmetrical weakness �Vasculopathy proximal muscle Skin Manifestations
� The age of onset has two peaks, between 5 and 9 yrs and between 11 and 14 yrs, with a predominance of females � Heliotrope rash on the eyelids, Gottrons papules on the knuckles and proximal muscle weakness are the classical features of JDM.
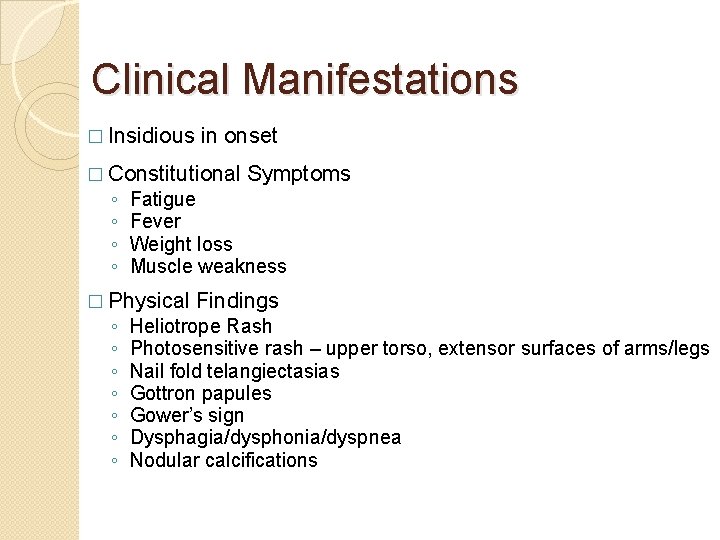
Clinical Manifestations � Insidious in onset � Constitutional ◦ ◦ Fatigue Fever Weight loss Muscle weakness � Physical ◦ ◦ ◦ ◦ Symptoms Findings Heliotrope Rash Photosensitive rash – upper torso, extensor surfaces of arms/legs Nail fold telangiectasias Gottron papules Gower’s sign Dysphagia/dysphonia/dyspnea Nodular calcifications
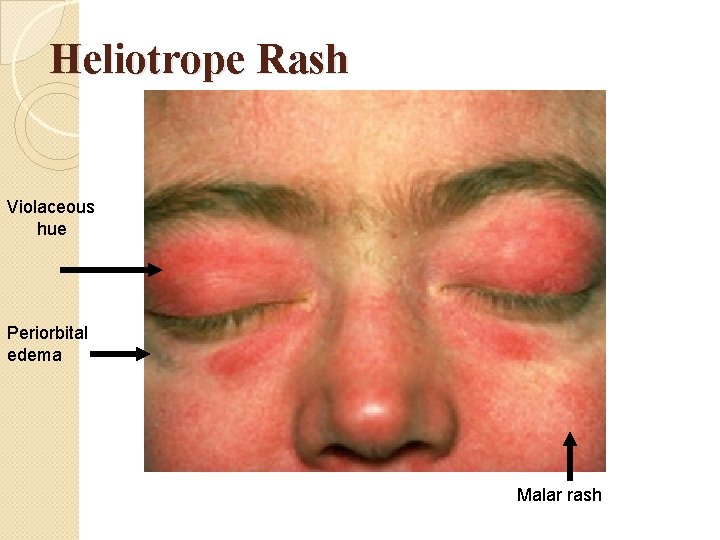
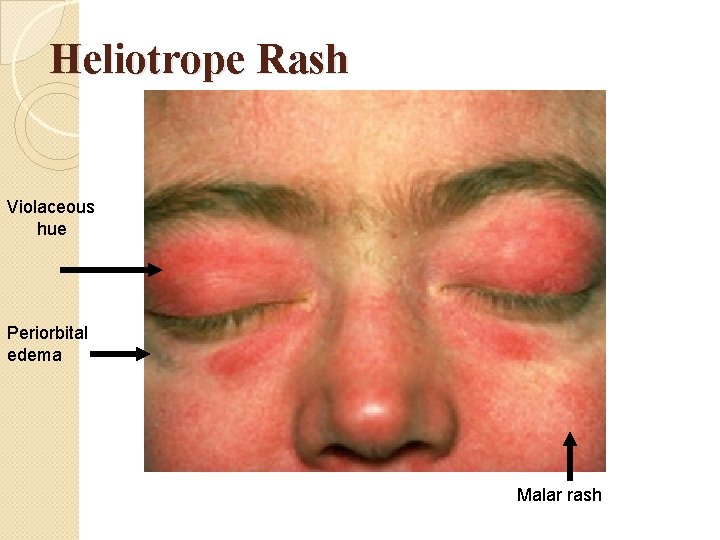
Heliotrope Rash Violaceous hue Periorbital edema Malar rash

Gottron’s Sign Pathognomonic for JDM Red, thickened, scaly skin overlying PIPs
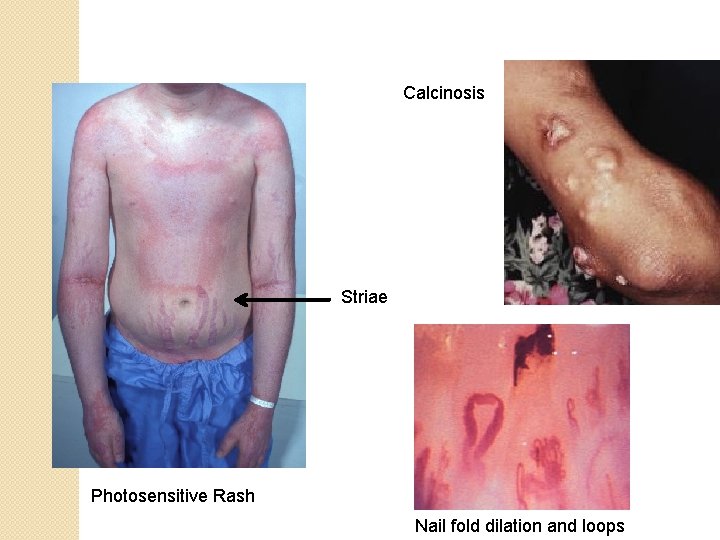
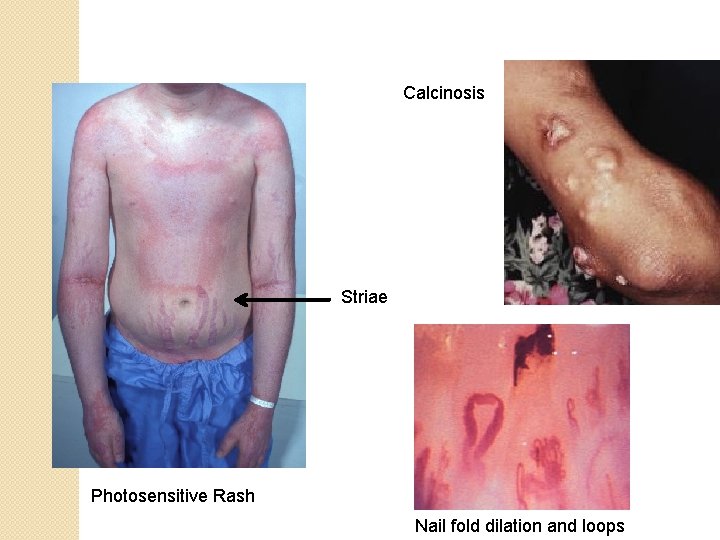
Calcinosis Striae Photosensitive Rash Nail fold dilation and loops
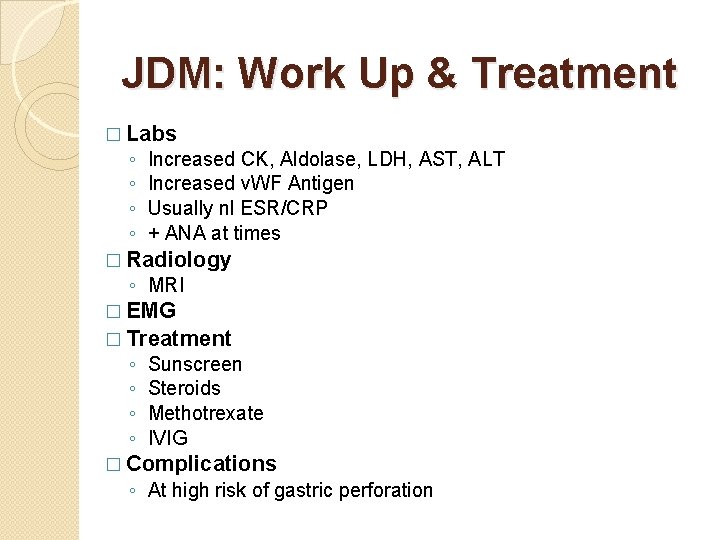
JDM: Work Up & Treatment � Labs ◦ ◦ Increased CK, Aldolase, LDH, AST, ALT Increased v. WF Antigen Usually nl ESR/CRP + ANA at times � Radiology ◦ MRI � EMG � Treatment ◦ ◦ Sunscreen Steroids Methotrexate IVIG � Complications ◦ At high risk of gastric perforation
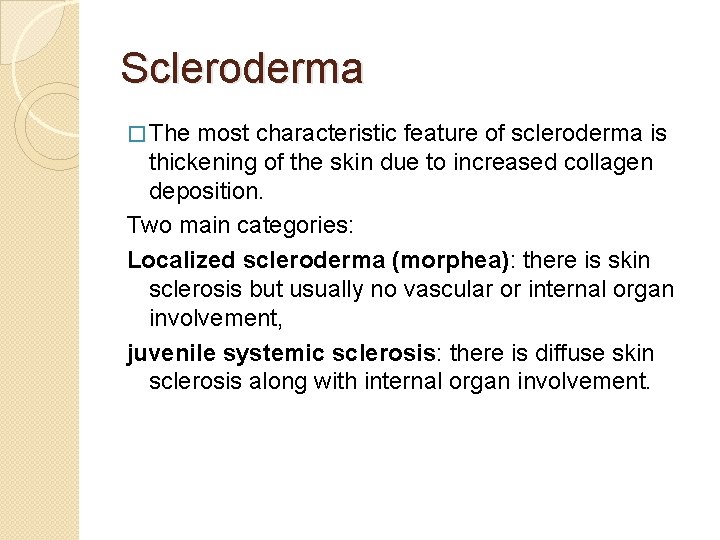
Scleroderma � The most characteristic feature of scleroderma is thickening of the skin due to increased collagen deposition. Two main categories: Localized scleroderma (morphea): there is skin sclerosis but usually no vascular or internal organ involvement, juvenile systemic sclerosis: there is diffuse skin sclerosis along with internal organ involvement.
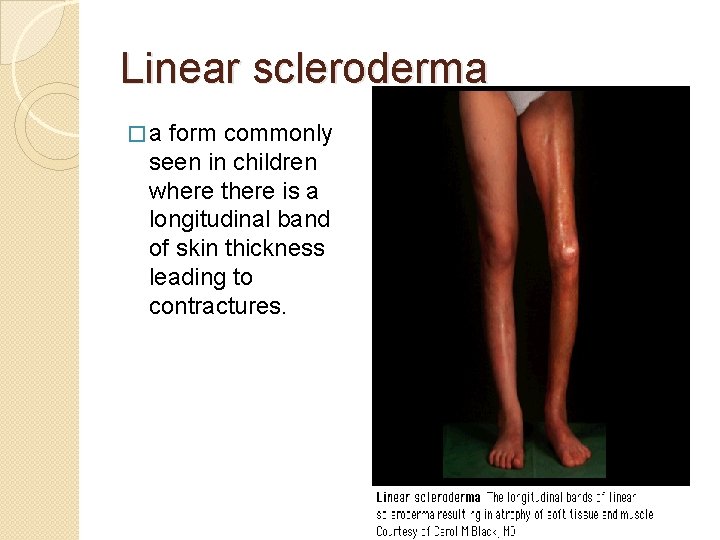
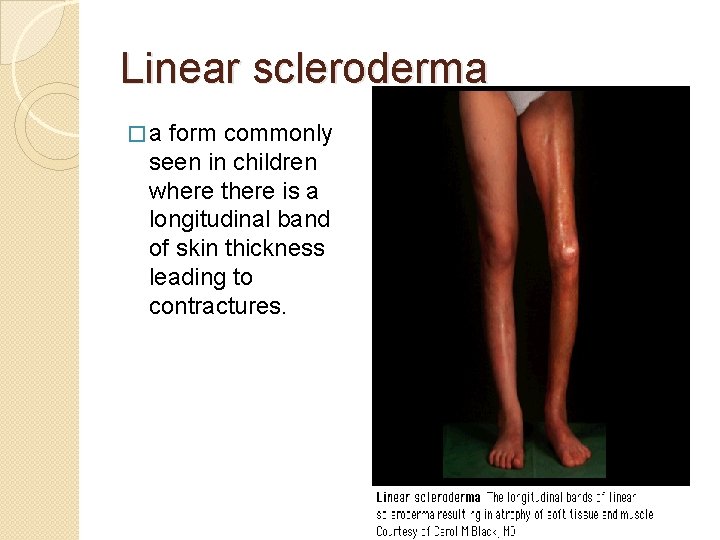
Linear scleroderma �a form commonly seen in children where there is a longitudinal band of skin thickness leading to contractures.
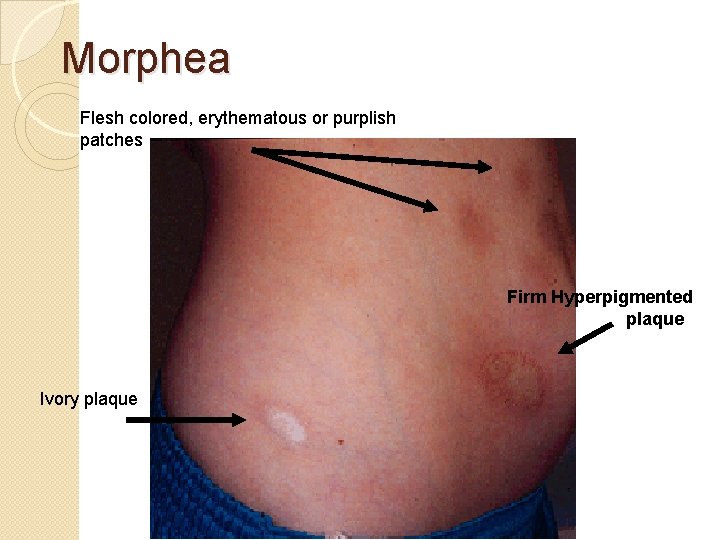
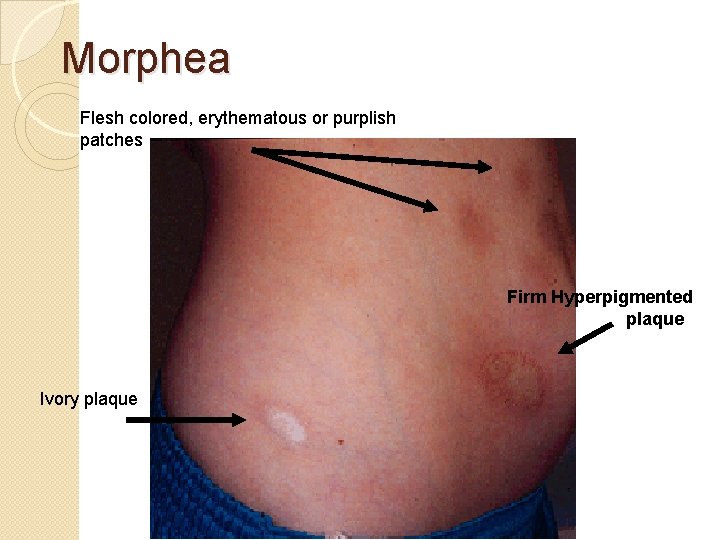
Morphea Flesh colored, erythematous or purplish patches Firm Hyperpigmented plaque Ivory plaque
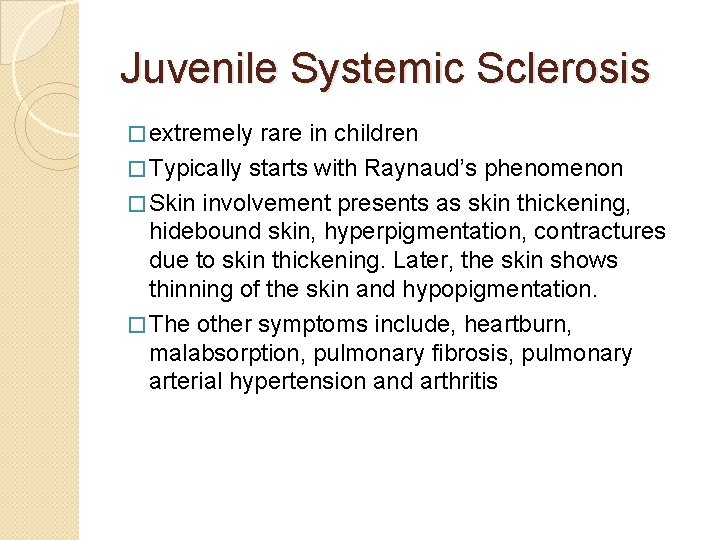
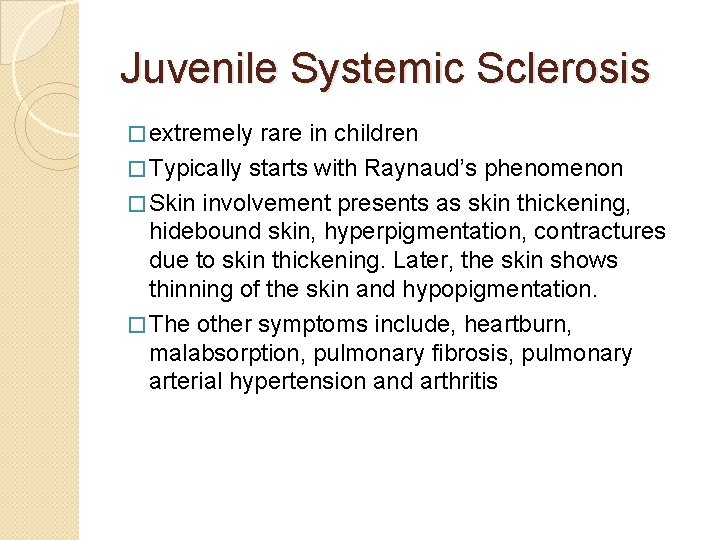
Juvenile Systemic Sclerosis � extremely rare in children � Typically starts with Raynaud’s phenomenon � Skin involvement presents as skin thickening, hidebound skin, hyperpigmentation, contractures due to skin thickening. Later, the skin shows thinning of the skin and hypopigmentation. � The other symptoms include, heartburn, malabsorption, pulmonary fibrosis, pulmonary arterial hypertension and arthritis
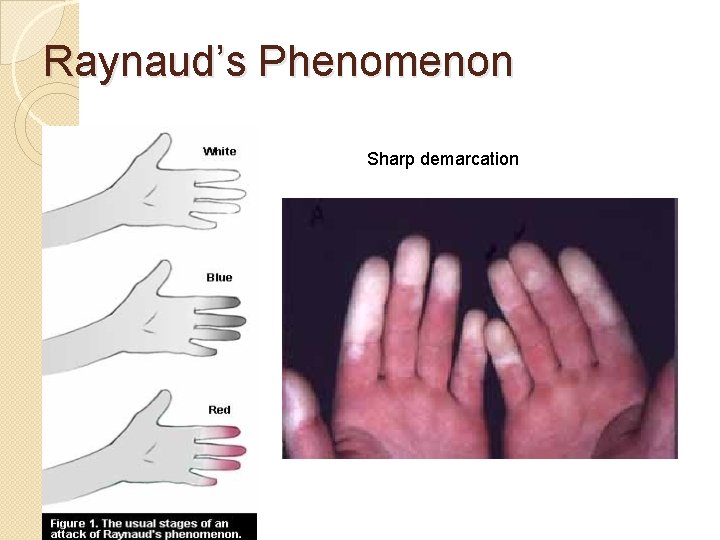
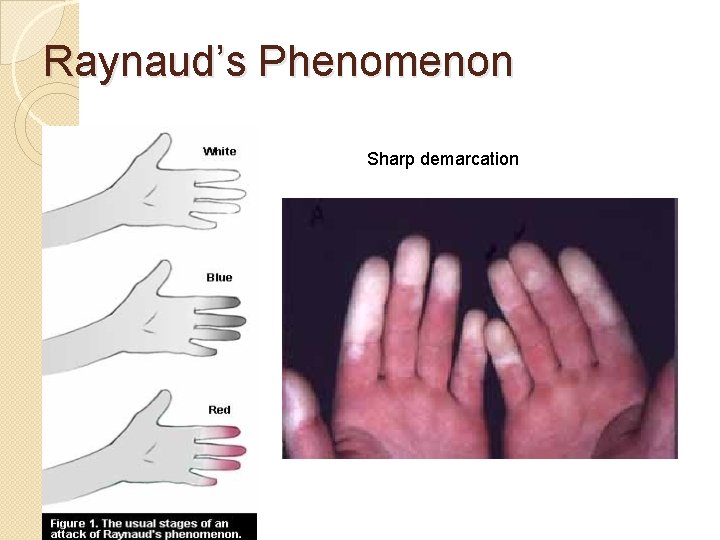
Raynaud’s Phenomenon Sharp demarcation

CREST Sclerodactyly Telangiectasia Calcinosis Raynaud
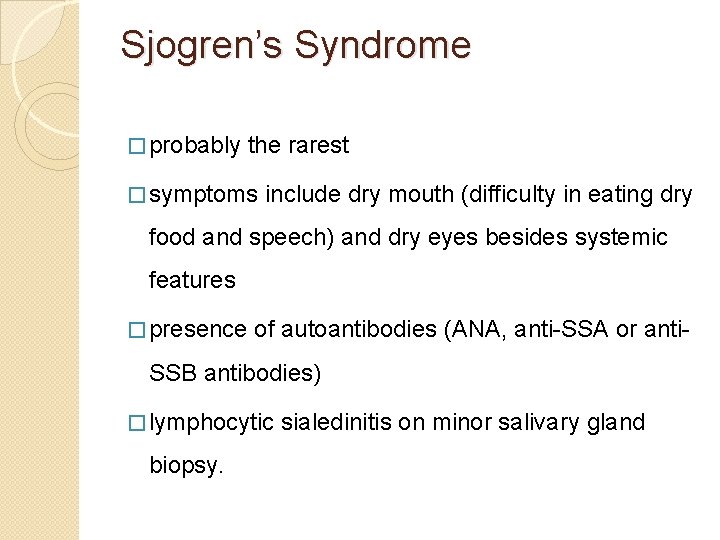
Sjogren’s Syndrome � probably the rarest � symptoms include dry mouth (difficulty in eating dry food and speech) and dry eyes besides systemic features � presence of autoantibodies (ANA, anti-SSA or anti- SSB antibodies) � lymphocytic biopsy. sialedinitis on minor salivary gland
Mixed Connective Tissue Disease (MCTD) �MCTD is a syndrome where clinical features of multiple CTDs are present along with presence of high titre anti-RNP antibodies. �Raynaud’s phenomenon is present in nearly 95% of patients.
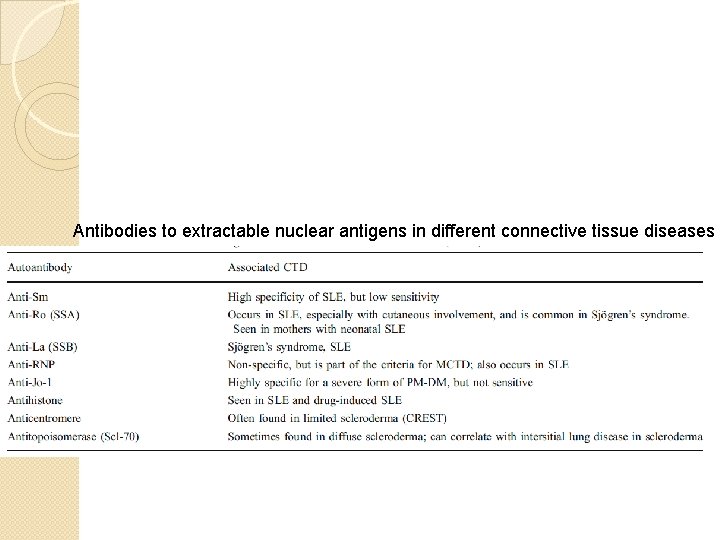
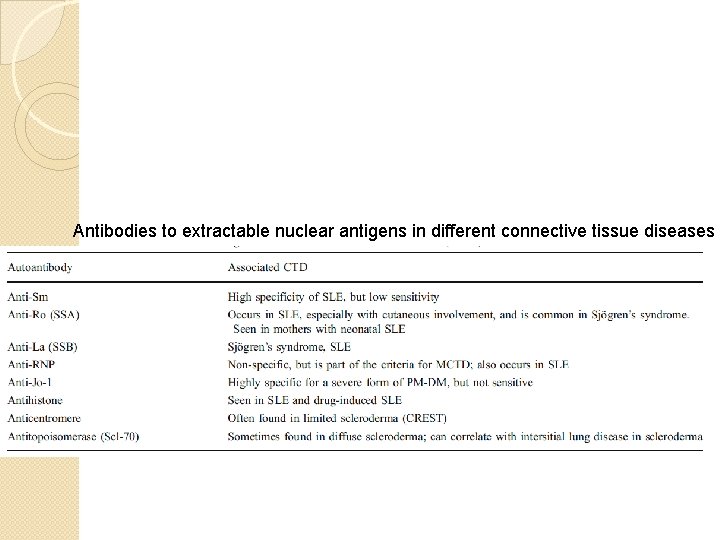
Antibodies to extractable nuclear antigens in different connective tissue diseases