Connecting with Clients and Their Families in Audiological

![Facilitate family involvement “We organised it. She [audiologist] always called us in together. There Facilitate family involvement “We organised it. She [audiologist] always called us in together. There](https://slidetodoc.com/presentation_image/7783f709ed9f841be58ca598eb96e3f8/image-16.jpg)
![Addressing psychosocial concerns (1) [C 11 -1 at 31: 04] 1 A: U: : Addressing psychosocial concerns (1) [C 11 -1 at 31: 04] 1 A: U: :](https://slidetodoc.com/presentation_image/7783f709ed9f841be58ca598eb96e3f8/image-26.jpg)
![Addressing psychosocial concerns (2) [C 11 -1 at 43: 37] 1 2 3 4 Addressing psychosocial concerns (2) [C 11 -1 at 43: 37] 1 2 3 4](https://slidetodoc.com/presentation_image/7783f709ed9f841be58ca598eb96e3f8/image-27.jpg)
![Family member involvement (1) [C 09 -1 00: 10] 1 2 3 4 5 Family member involvement (1) [C 09 -1 00: 10] 1 2 3 4 5](https://slidetodoc.com/presentation_image/7783f709ed9f841be58ca598eb96e3f8/image-30.jpg)
- Slides: 38
Connecting with Clients and Their Families in Audiological Rehabilitation Louise Hickson; Nerina Scarinci; Carly Meyer; Katie Ekberg; Caitlin Grenness HEARing CRC, The University of Queensland, The University of Melbourne British Society of Hearing Aid Audiologists, 15 th May 2015 TM creatingsound value creating value TM www. hearingcrc. org

The HEARing CRC Member Organisations creating sound value. TM
Overview • Why think about connecting with clients and families? • What do clients, families and clinicians want in hearing rehabilitation? • What actually happens in hearing rehabilitation? • What can you do in your clinics? Research evidence Clinician’s experience Client’s preferences & goals Clinical Context creating sound value. TM
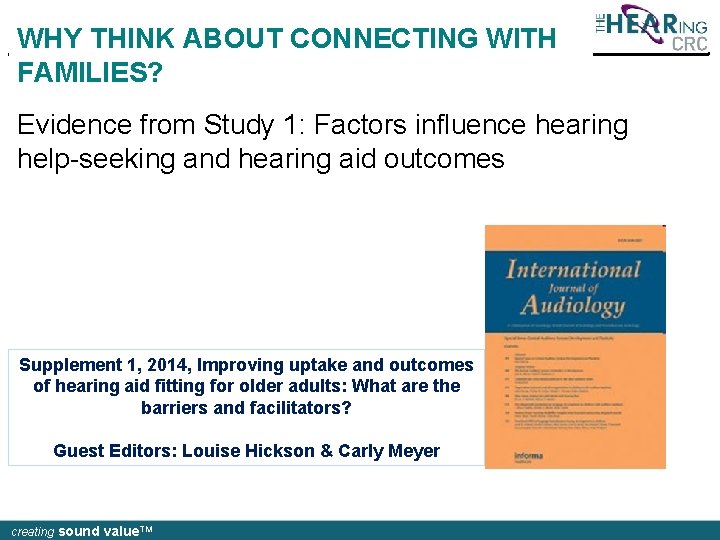
WHY THINK ABOUT CONNECTING WITH FAMILIES? Evidence from Study 1: Factors influence hearing help-seeking and hearing aid outcomes Supplement 1, 2014, Improving uptake and outcomes of hearing aid fitting for older adults: What are the barriers and facilitators? Guest Editors: Louise Hickson & Carly Meyer creating sound value. TM
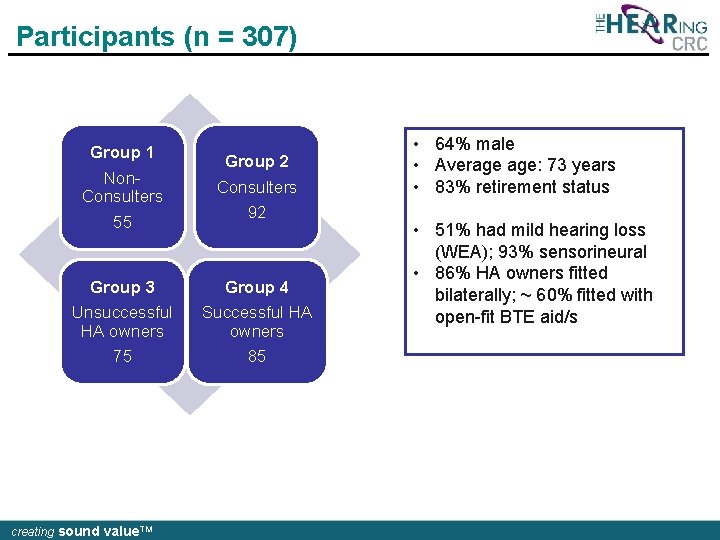
Participants (n = 307) Group 1 Non. Consulters 55 Group 2 Consulters 92 Group 3 Unsuccessful HA owners 75 Group 4 Successful HA owners 85 creating sound value. TM • 64% male • Average age: 73 years • 83% retirement status • 51% had mild hearing loss (WEA); 93% sensorineural • 86% HA owners fitted bilaterally; ~ 60% fitted with open-fit BTE aid/s
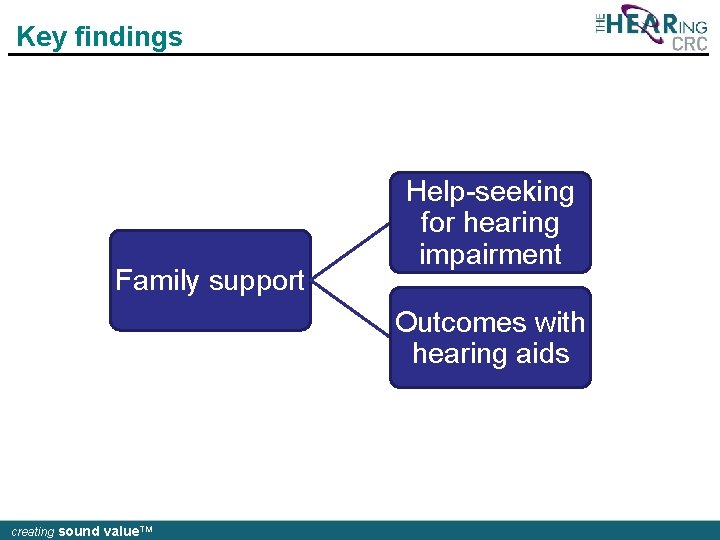
Key findings Family support Help-seeking for hearing impairment Outcomes with hearing aids creating sound value. TM
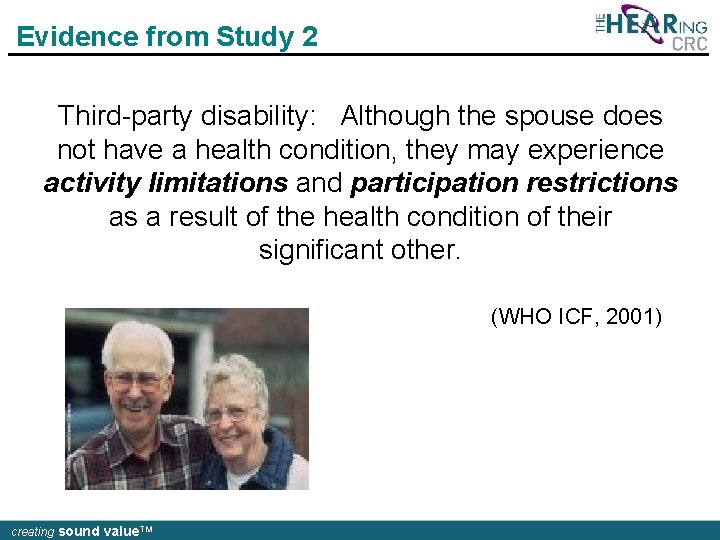
Evidence from Study 2 Third-party disability: Although the spouse does not have a health condition, they may experience activity limitations and participation restrictions as a result of the health condition of their significant other. (WHO ICF, 2001) creating sound value. TM
Third-party hearing disability • In a study of 100 spouses of older adults with hearing impairment, 94% of spouses reported some degree of thirdparty hearing disability on the SOS-HEAR (Scarinci et al. , 2009) • Most spouses reported mild problems • Greater disability reported in the areas of: • Emotional consequences (e. g. , frustration) • Communication activities (e. g. , reduced talking) • Everyday activities (e. g. , television viewing) Scarinci, N. , Worrall, L. , & Hickson, L. (2012). Factors associated with third-party disability in spouses of older people with hearing impairment. Ear & Hearing, 33, 698 -708. creating sound value. TM
WHAT DO CLIENTS, FAMILIES AND CLINICIANS WANT? creating sound value. TM
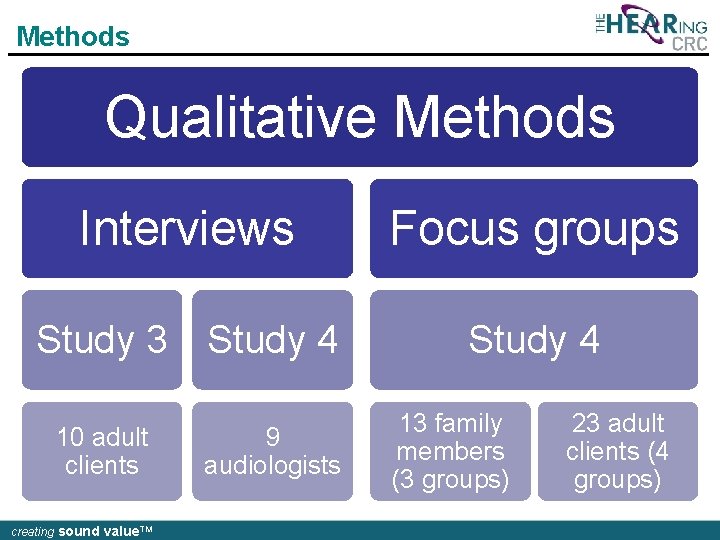
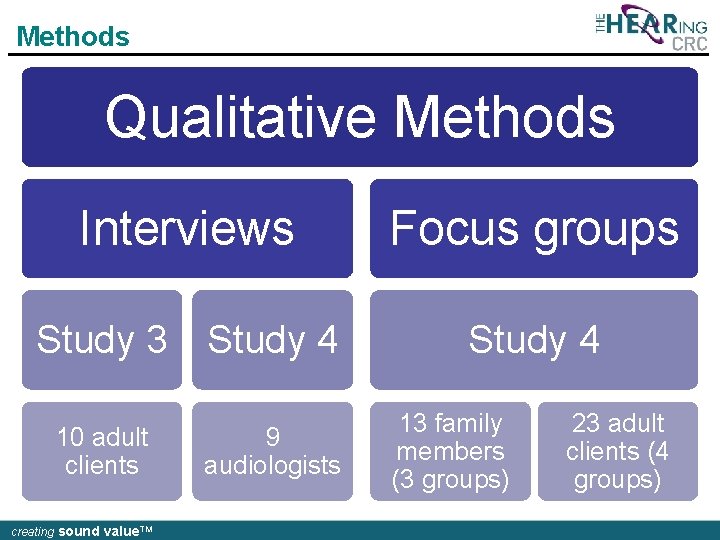
Methods Qualitative Methods Interviews Focus groups Study 3 Study 4 10 adult clients creating sound value. TM 9 audiologists 13 family members (3 groups) 23 adult clients (4 groups)
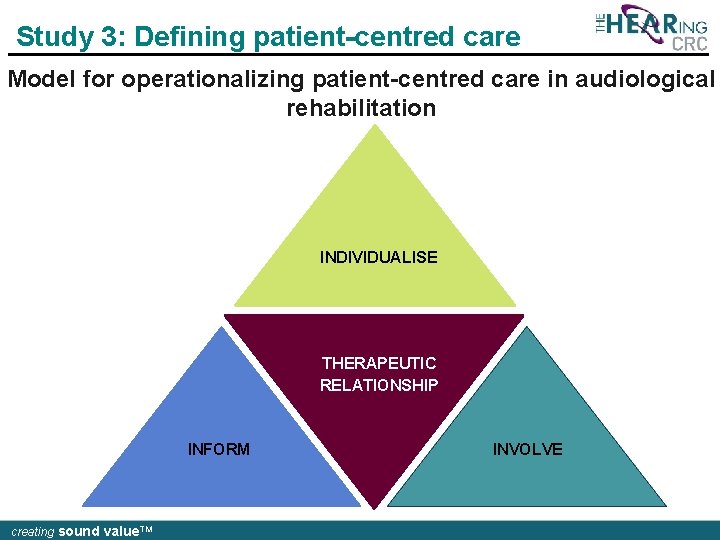
Study 3: Defining patient-centred care Model for operationalizing patient-centred care in audiological rehabilitation INDIVIDUALISE THERAPEUTIC RELATIONSHIP INFORM creating sound value. TM INVOLVE
“. . . An unhurried conversation focused on the patient’s perceptions of “ifdetermining “Most it’s a human audiologists being are thattoo I can interested relate to, in “Next timejust I (Iget hearing aids Ithat’s will tell the “When Inot leave feel) anhearing. element of frustration, “Iselling amdifficulties some punter the with And it come would that makes you hearing it so much aids. better, They so don’t much really “It’s notaudiologist anot question of clinician, it’s “The saying I know just audiologist I want tothe be morebest involved that Ijust am that being fully listened to” INDIVIDUALISE through the door” a question the patient, and the two also focus on eliciting that other doesn’t hack itdifficulties anymore” the decision” easier. have that And much ifofin it’s care… going to they cost test me your 10% ears have got to #3; come together. ” (Participant female, age 71) of their people have with them, like members 20% and(Participant test extra, what I’d level be happy of hearing to pay you’ve for that” lost, (Participant #8; male, age 72) #2; 68 year-old female) (Participant #7; male, age 70) (Participant #8; family. ” male, 72) aids. ” own and then it’s straight awayage hearing (Participant #10; male, age 77) THERAPEUTIC RELATIONSHIP (Participant #7, male, (Participant #10; male, age 70) 77) INFORM creating sound value. TM INVOLVE
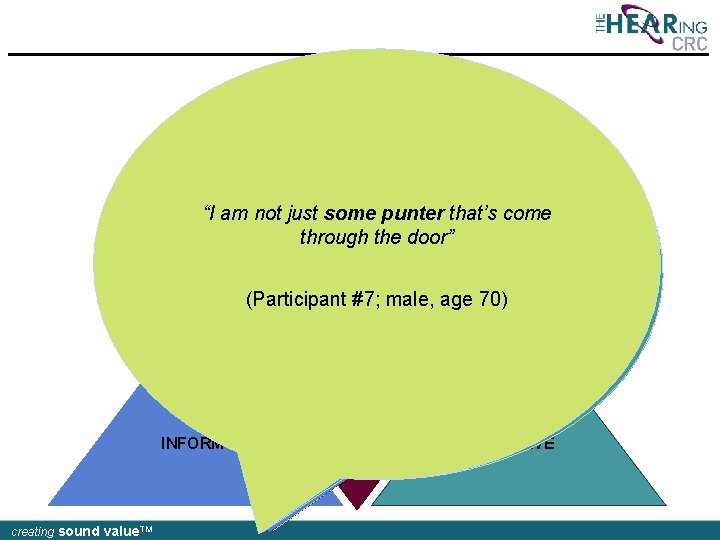
Implications for audiological rehabilitation “Technical audiological skills are assumed, interaction skills are valued…” creating sound value. TM
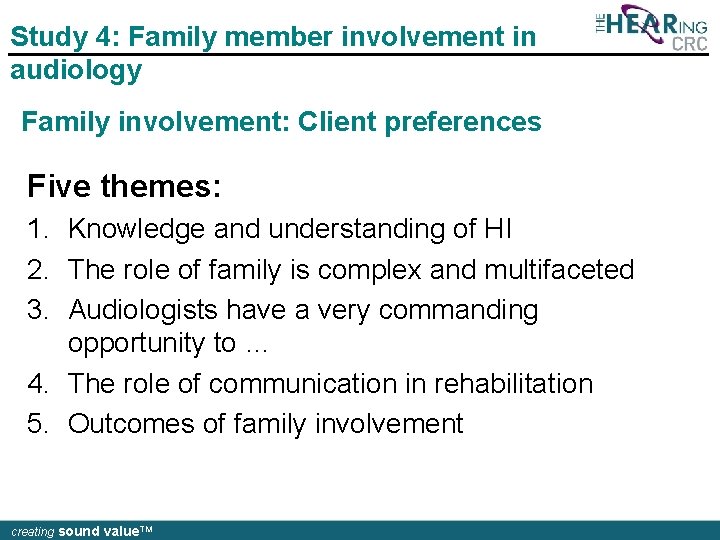
Study 4: Family member involvement in audiology Family involvement: Client preferences Five themes: 1. Knowledge and understanding of HI 2. The role of family is complex and multifaceted 3. Audiologists have a very commanding opportunity to … 4. The role of communication in rehabilitation 5. Outcomes of family involvement creating sound value. TM
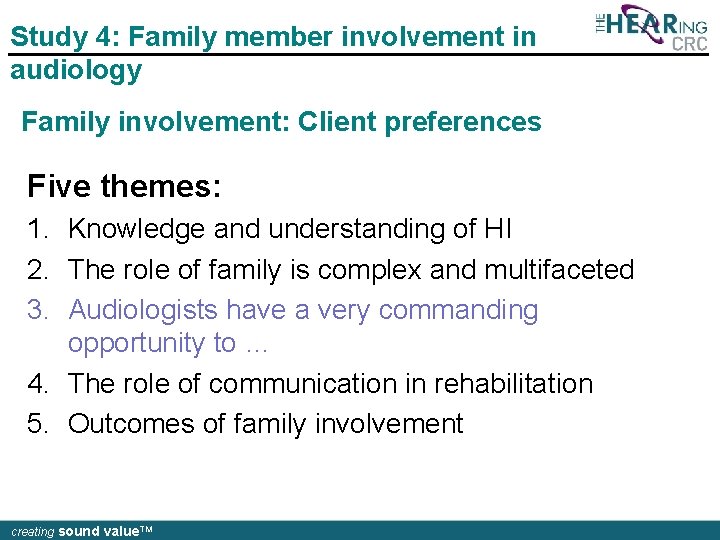
Study 4: Family member involvement in audiology Family involvement: Client preferences Five themes: 1. Knowledge and understanding of HI 2. The role of family is complex and multifaceted 3. Audiologists have a very commanding opportunity to … 4. The role of communication in rehabilitation 5. Outcomes of family involvement creating sound value. TM
![Facilitate family involvement We organised it She audiologist always called us in together There Facilitate family involvement “We organised it. She [audiologist] always called us in together. There](https://slidetodoc.com/presentation_image/7783f709ed9f841be58ca598eb96e3f8/image-16.jpg)
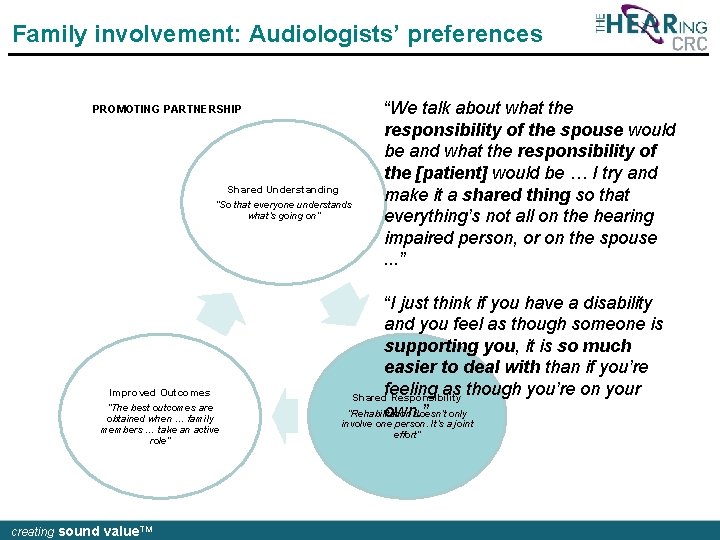
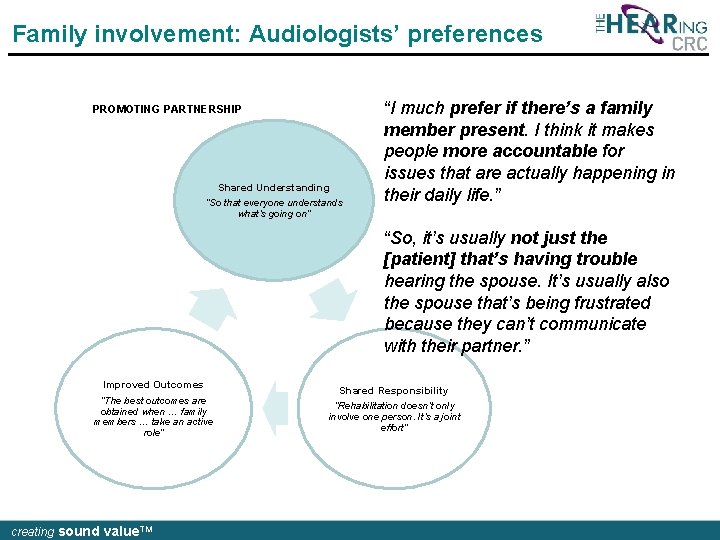
Facilitate family involvement “We organised it. She [audiologist] always called us in together. There was always a chair for us” Include family in goal setting “I guess I’d be hoping that I’d be asked what impact actually is on the people around her and the things that I’ve observed that she can’t hear” Audiologists have a commanding opportunity to … Provide education “It would be good to be there to hear the unbiased professional opinion” creating sound value. TM Build understanding & empathy “How do we get … our spouses, partners here [at appointments]’. You’ve got to give them a reason and the reason is, you’ll understand him or her better”
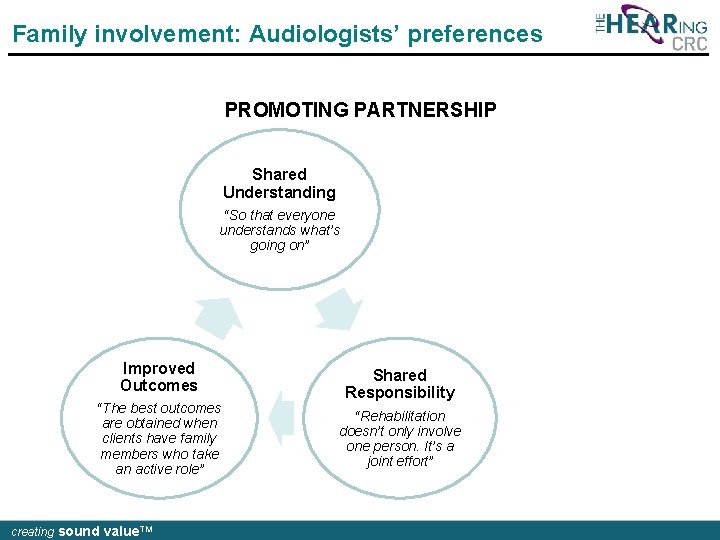
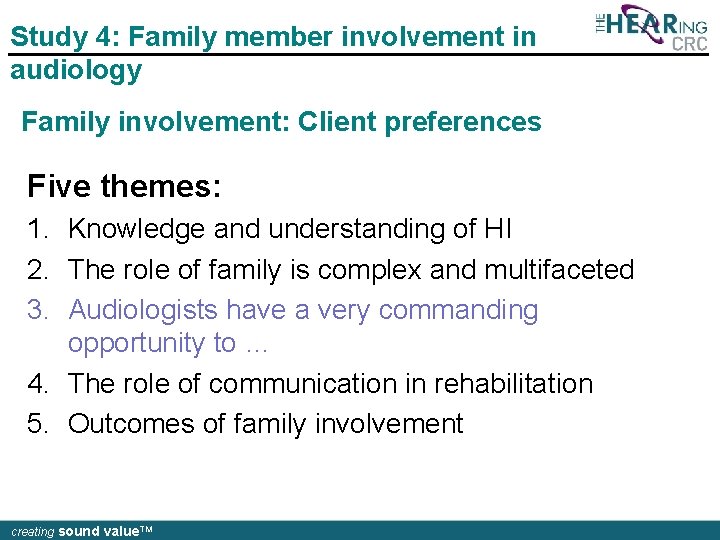
Family involvement: Audiologists’ preferences PROMOTING PARTNERSHIP Shared Understanding “So that everyone understands what’s going on” Improved Outcomes “The best outcomes are obtained when clients have family members who take an active role” creating sound value. TM Shared Responsibility “Rehabilitation doesn’t only involve one person. It’s a joint effort”
Family involvement: Audiologists’ preferences PROMOTING PARTNERSHIP Shared Understanding “So that everyone understands what’s going on” “I much prefer if there’s a family member present. I think it makes people more accountable for issues that are actually happening in their daily life. ” “So, it’s usually not just the [patient] that’s having trouble hearing the spouse. It’s usually also the spouse that’s being frustrated because they can’t communicate with their partner. ” Improved Outcomes “The best outcomes are obtained when … family members … take an active role” creating sound value. TM Shared Responsibility “Rehabilitation doesn’t only involve one person. It’s a joint effort”
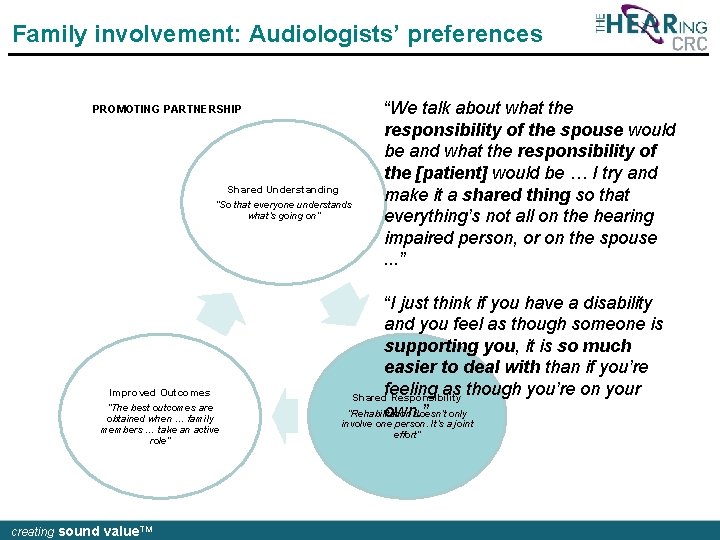
Family involvement: Audiologists’ preferences PROMOTING PARTNERSHIP Shared Understanding “So that everyone understands what’s going on” Improved Outcomes “The best outcomes are obtained when … family members … take an active role” creating sound value. TM “We talk about what the responsibility of the spouse would be and what the responsibility of the [patient] would be … I try and make it a shared thing so that everything’s not all on the hearing impaired person, or on the spouse. . . ” “I just think if you have a disability and you feel as though someone is supporting you, it is so much easier to deal with than if you’re feeling as though you’re on your Shared Responsibility “Rehabilitation doesn’t only own. ” involve one person. It’s a joint effort”
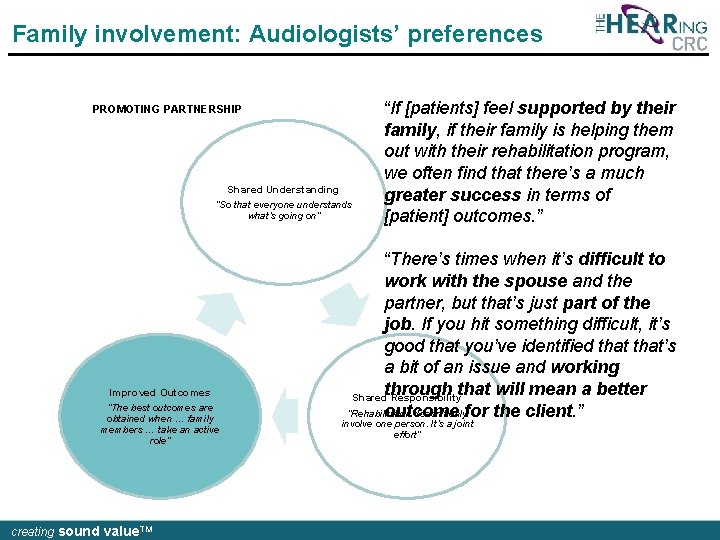
Family involvement: Audiologists’ preferences PROMOTING PARTNERSHIP Shared Understanding “So that everyone understands what’s going on” Improved Outcomes “The best outcomes are obtained when … family members … take an active role” creating sound value. TM “If [patients] feel supported by their family, if their family is helping them out with their rehabilitation program, we often find that there’s a much greater success in terms of [patient] outcomes. ” “There’s times when it’s difficult to work with the spouse and the partner, but that’s just part of the job. If you hit something difficult, it’s good that you’ve identified that’s a bit of an issue and working through that will mean a better Shared Responsibility “Rehabilitation doesn’t onlyfor the client. ” outcome involve one person. It’s a joint effort”
What are patients and clinicians saying? HOW OFTEN ARE FAMILY MEMBERS INVOLVED IN APPOINTMENTS? “Not as much as I’d like them to, but I’d probably say 30% to 40% of my appointments have a family member” [AUD] “As a guesstimate I think it’s relatively low… I would guesstimate it is certainly less than 50, closer to 20 or 30” [AUD] “I didn’t know he was going” [FM] “I was there, but just observing I guess … I just sit in the corner” [FM] creating sound value. TM
WHAT ACTUALLY HAPPENS? Grenness, C. , Hickson, L. , Laplante. Lévesque, A. , Meyer, C. , & Davidson, B. (2015). Communication patterns in audiologic rehabilitation history-taking: Audiologists, patients, and their companions. Ear & Hear, 36(2), 191 -204. Grenness, C. , Hickson, L. , Laplante. Lévesque, A. , Meyer, C. , & Davidson, B. (2015). The nature of communication throughout diagnosis and management planning in initial audiologic rehabilitation consultations. JAAA, 26, 36 -50. creating sound value. TM
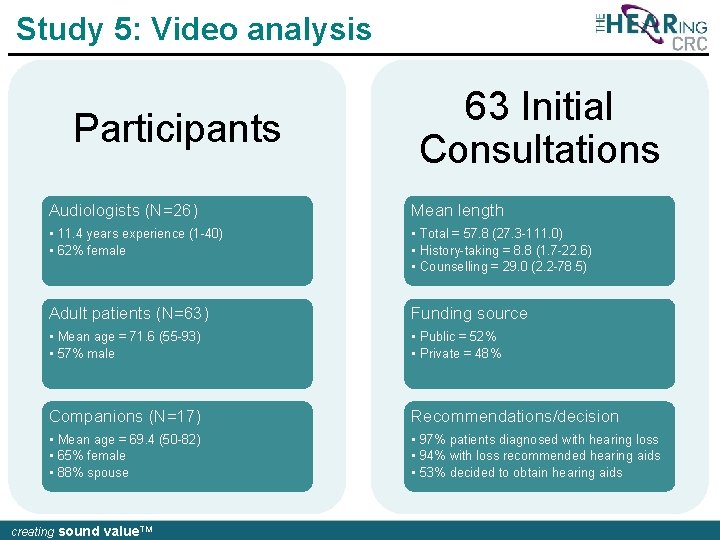
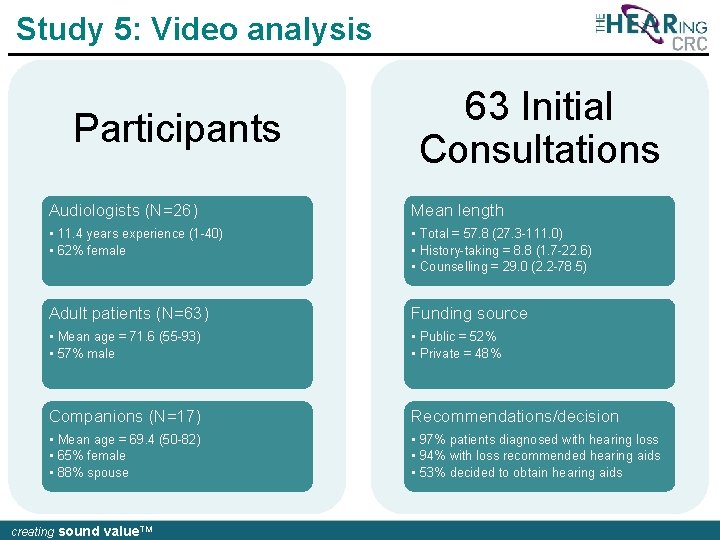
Study 5: Video analysis Participants 63 Initial Consultations Audiologists (N=26) Mean length • 11. 4 years experience (1 -40) • 62% female • Total = 57. 8 (27. 3 -111. 0) • History-taking = 8. 8 (1. 7 -22. 6) • Counselling = 29. 0 (2. 2 -78. 5) Adult patients (N=63) Funding source • Mean age = 71. 6 (55 -93) • 57% male • Public = 52% • Private = 48% Companions (N=17) Recommendations/decision • Mean age = 69. 4 (50 -82) • 65% female • 88% spouse • 97% patients diagnosed with hearing loss • 94% with loss recommended hearing aids • 53% decided to obtain hearing aids creating sound value. TM
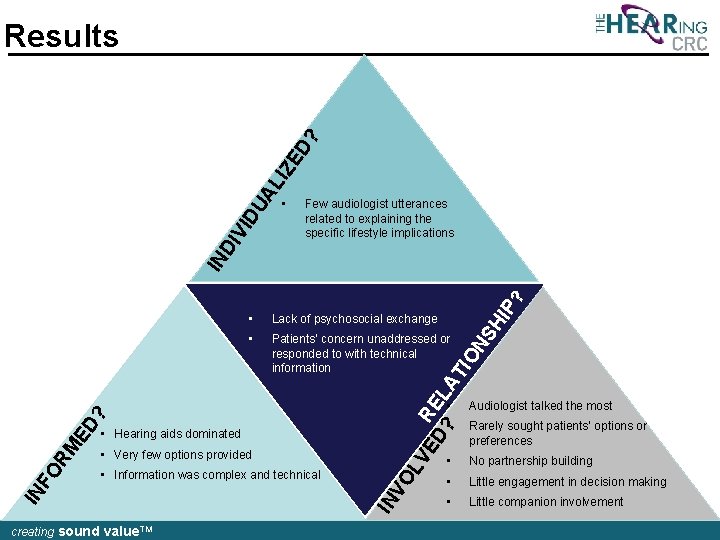
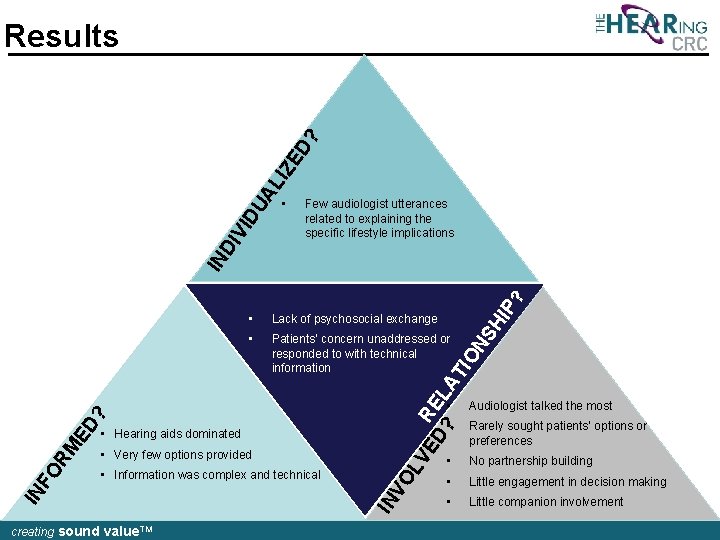
• Few audiologist utterances related to explaining the specific lifestyle implications • Patients’ concern unaddressed or responded to with technical information IO Lack of psychosocial exchange VE • Hearing aids dominated • Information was complex and technical creating sound value. TM VO L • Very few options provided IN IN FO RM ED ? R D? EL AT • NS HI P? IN DI VI DU AL IZ ED ? Results • Audiologist talked the most • Rarely sought patients’ options or preferences • No partnership building • Little engagement in decision making • Little companion involvement
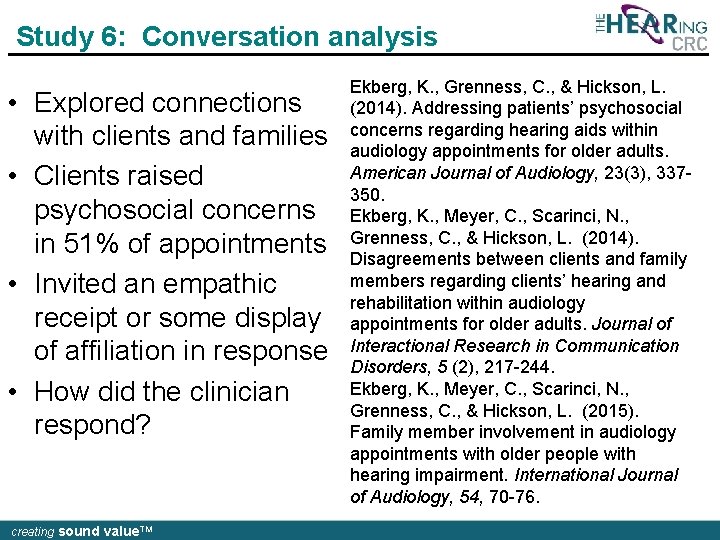
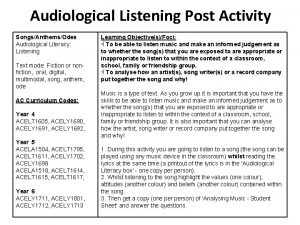
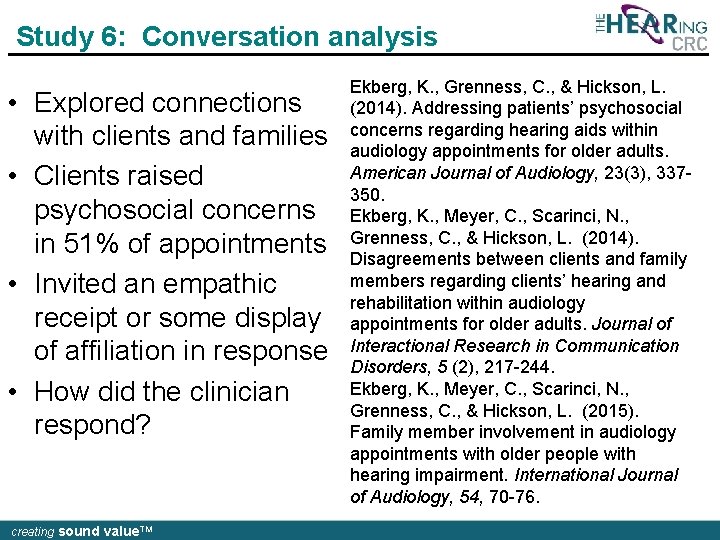
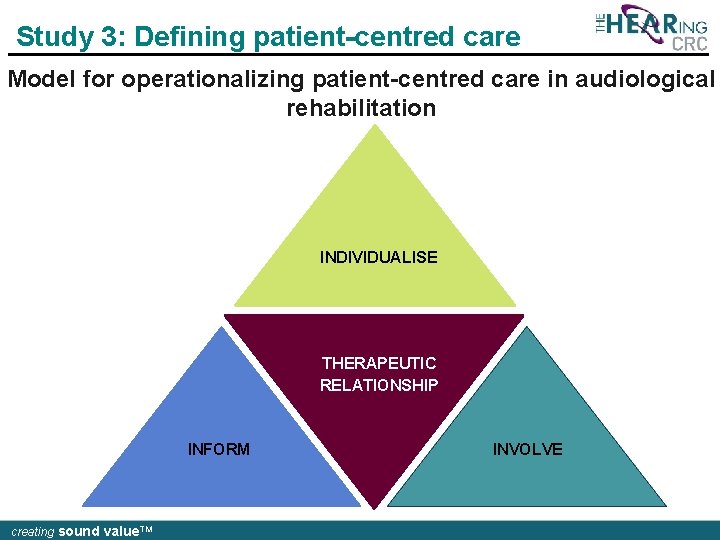
Study 6: Conversation analysis • Explored connections with clients and families • Clients raised psychosocial concerns in 51% of appointments • Invited an empathic receipt or some display of affiliation in response • How did the clinician respond? creating sound value. TM Ekberg, K. , Grenness, C. , & Hickson, L. (2014). Addressing patients’ psychosocial concerns regarding hearing aids within audiology appointments for older adults. American Journal of Audiology, 23(3), 337350. Ekberg, K. , Meyer, C. , Scarinci, N. , Grenness, C. , & Hickson, L. (2014). Disagreements between clients and family members regarding clients’ hearing and rehabilitation within audiology appointments for older adults. Journal of Interactional Research in Communication Disorders, 5 (2), 217 -244. Ekberg, K. , Meyer, C. , Scarinci, N. , Grenness, C. , & Hickson, L. (2015). Family member involvement in audiology appointments with older people with hearing impairment. International Journal of Audiology, 54, 70 -76.
![Addressing psychosocial concerns 1 C 11 1 at 31 04 1 A U Addressing psychosocial concerns (1) [C 11 -1 at 31: 04] 1 A: U: :](https://slidetodoc.com/presentation_image/7783f709ed9f841be58ca598eb96e3f8/image-26.jpg)
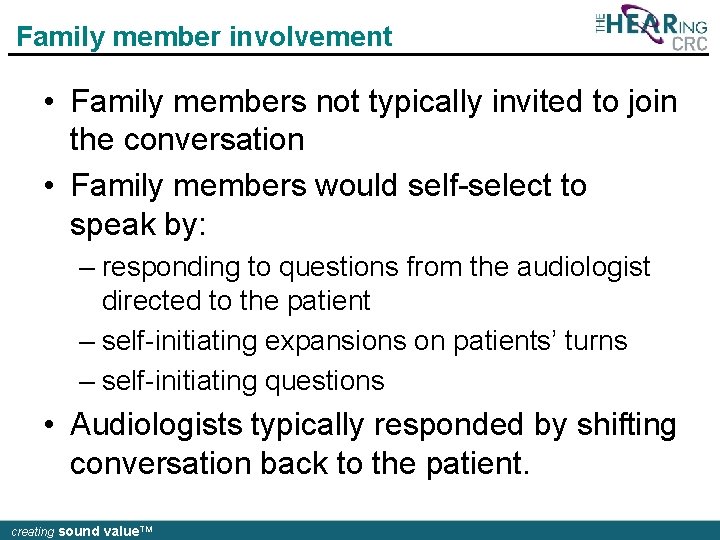
Addressing psychosocial concerns (1) [C 11 -1 at 31: 04] 1 A: U: : : m (0. 5). tch have you thought about 2 a hearing aid: um [before now? ] 3 P: [I don’t know] 4 whether I can s: : tand it actually. 5 A: Ye: s hah. hhh sure. hh u: : m well 6 look lets go to my office: , and I’ll 7 just (. ) we’ll have a bit more of a 8 chat and I’ll show you a couple what 9 they look like: : , creating sound value. TM
![Addressing psychosocial concerns 2 C 11 1 at 43 37 1 2 3 4 Addressing psychosocial concerns (2) [C 11 -1 at 43: 37] 1 2 3 4](https://slidetodoc.com/presentation_image/7783f709ed9f841be58ca598eb96e3f8/image-27.jpg)
Addressing psychosocial concerns (2) [C 11 -1 at 43: 37] 1 2 3 4 5 6 7 8 9 10 11 12 13 A: So you know you [d↑on’t really] see it anyway P: [ Hah hah ] A: because your hair’s there. P: I don’t think I’ll be bothered with that (0. 8) because I’ve been used t(h)o huh not getting everything now huh huh £you know what I mean£ [. HHHH] so um (3. 0) A: [ °Mm°] P: actually I wouldn’t have come if I wasn’t invited heh [heh hah ] A: [Oh: : I see] C: hah hah A: £Yeah£ creating sound value. TM
Discussion • Patients expressed concerns regarding hearing aids, but these concerns were not typically addressed during the appointment • Audiologists progressed a discussion about hearing aids • Mismatch in communication between audiologist and patient • Typically led to expanded sequences of interaction • Patients persistently re-raised their concerns creating sound value. TM
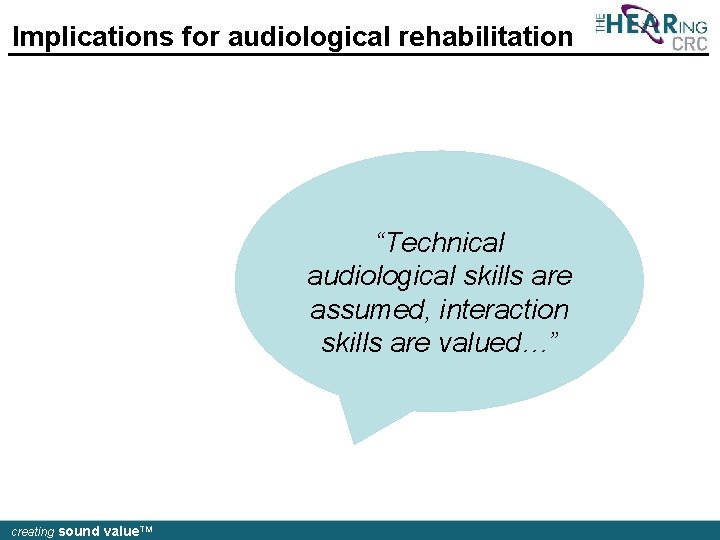
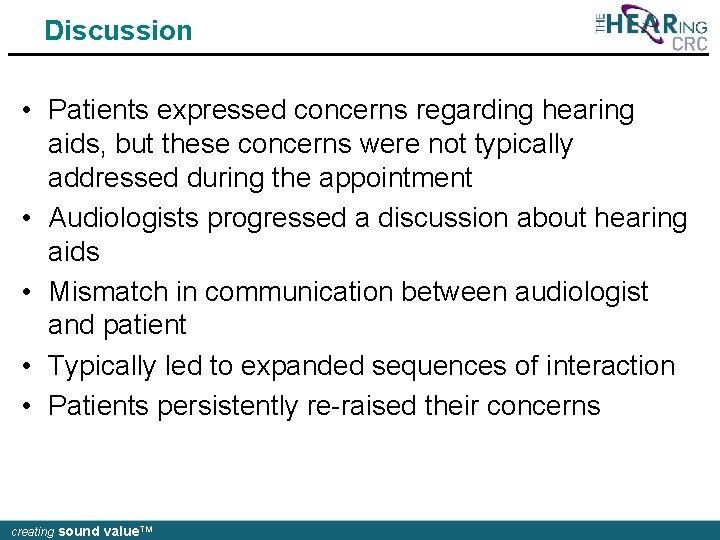
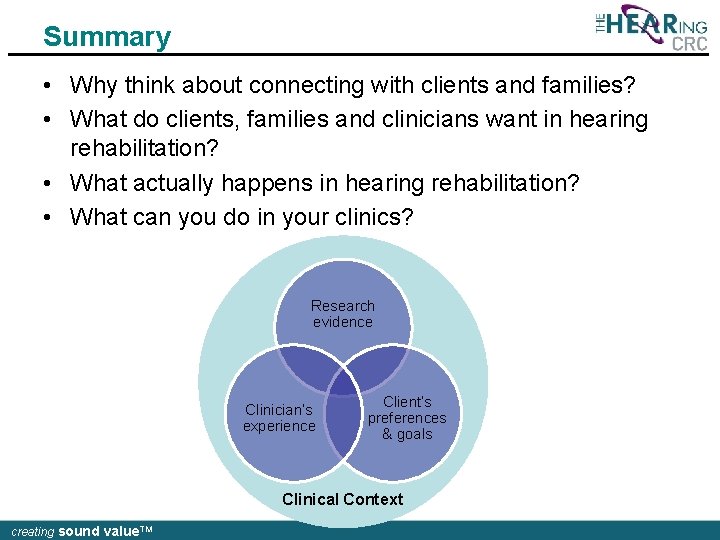
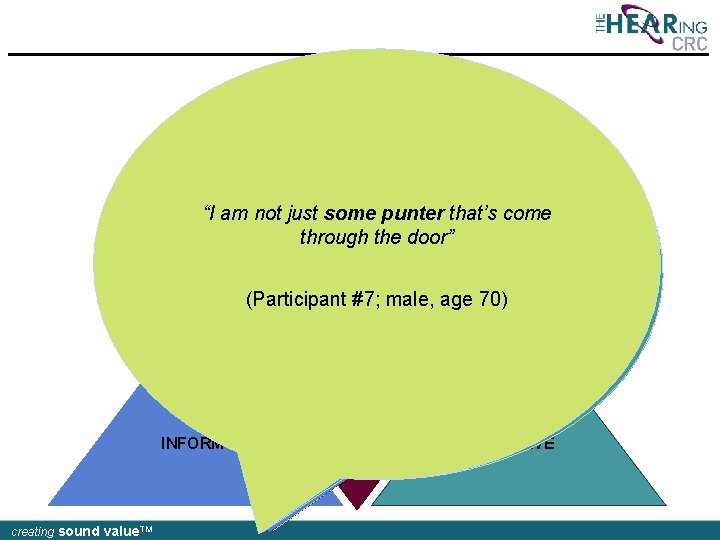
Family member involvement • Explored family members’ involvement in initial audiology consultations – how family members systematically became involved in the interaction – how their involvement was managed by the other parties creating sound value. TM
![Family member involvement 1 C 09 1 00 10 1 2 3 4 5 Family member involvement (1) [C 09 -1 00: 10] 1 2 3 4 5](https://slidetodoc.com/presentation_image/7783f709ed9f841be58ca598eb96e3f8/image-30.jpg)
Family member involvement (1) [C 09 -1 00: 10] 1 2 3 4 5 6 7 8 9 10 11 12 A: ↑So you feel you’re hearing– you’ve got a bit of a hearing loss, you’ve noticed? (0. 6) P: [Well, he seems to think I have] F: [Well she says she hasn’t but] [ when-] A: [Ri: ght] F: when we had the test done she was down a little bit on one ear I think. ((10 lines omitted where receptionist interrupts to deliver forms)) A: Okay so you haven’t noticed it yourse: lf a lot? creating sound value. TM
Family member involvement • Family members not typically invited to join the conversation • Family members would self-select to speak by: – responding to questions from the audiologist directed to the patient – self-initiating expansions on patients’ turns – self-initiating questions • Audiologists typically responded by shifting conversation back to the patient. creating sound value. TM
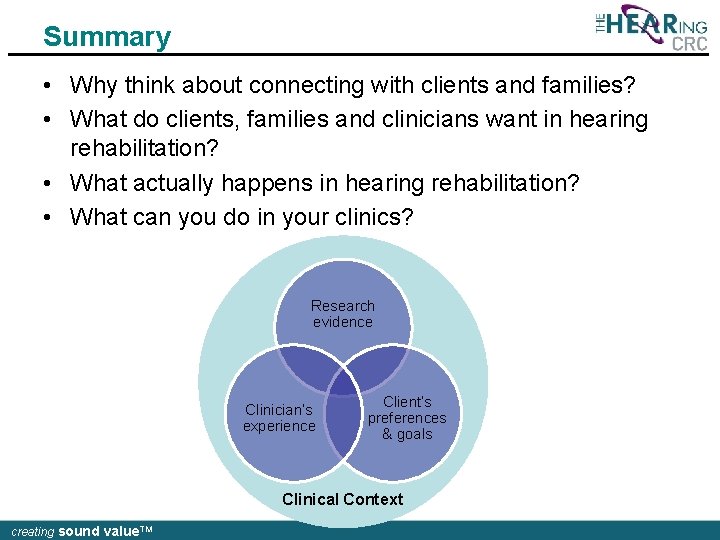
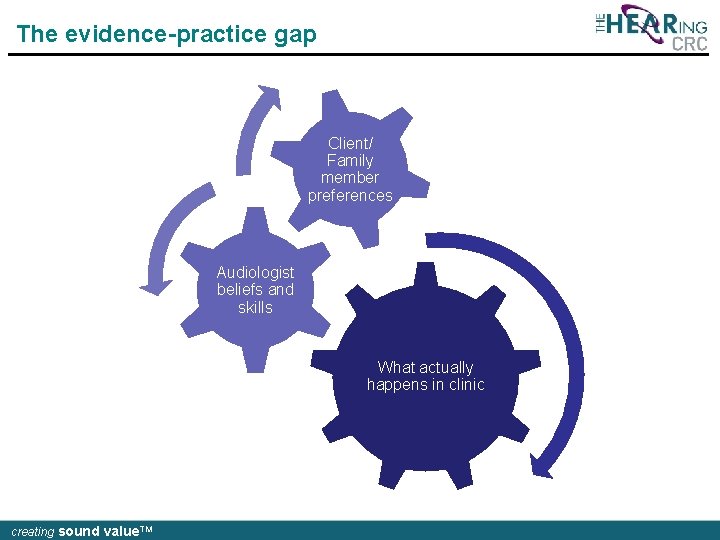
Summary • Why think about connecting with clients and families? • What do clients, families and clinicians want in hearing rehabilitation? • What actually happens in hearing rehabilitation? • What can you do in your clinics? Research evidence Clinician’s experience Client’s preferences & goals Clinical Context creating sound value. TM
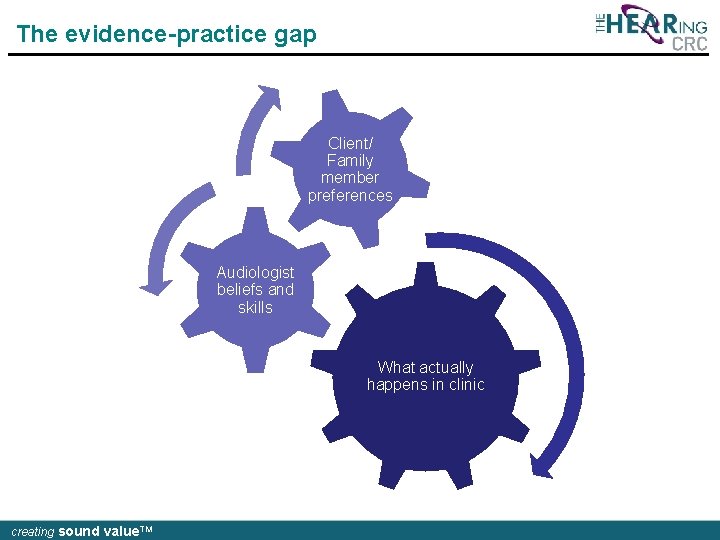
The evidence-practice gap Client/ Family member preferences Audiologist beliefs and skills What actually happens in clinic creating sound value. TM
WHAT CAN YOU DO IN YOUR CLINIC? creating sound value. TM
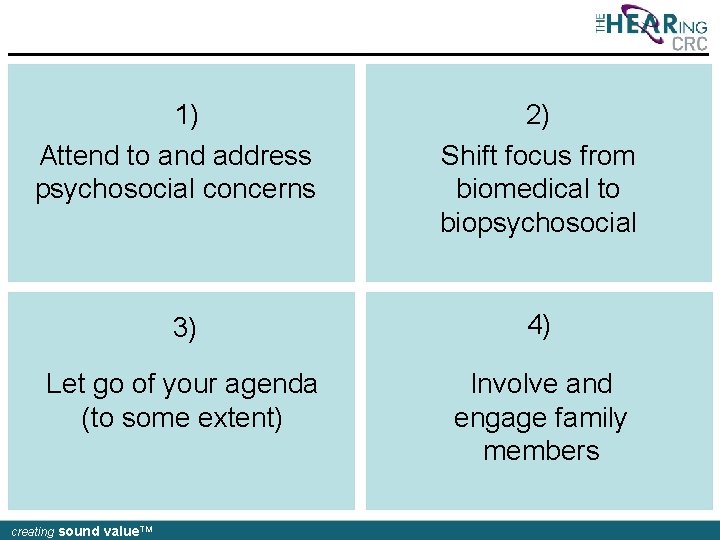
1) Attend to and address psychosocial concerns 2) Shift focus from biomedical to biopsychosocial 3) 4) Let go of your agenda (to some extent) Involve and engage family members creating sound value. TM
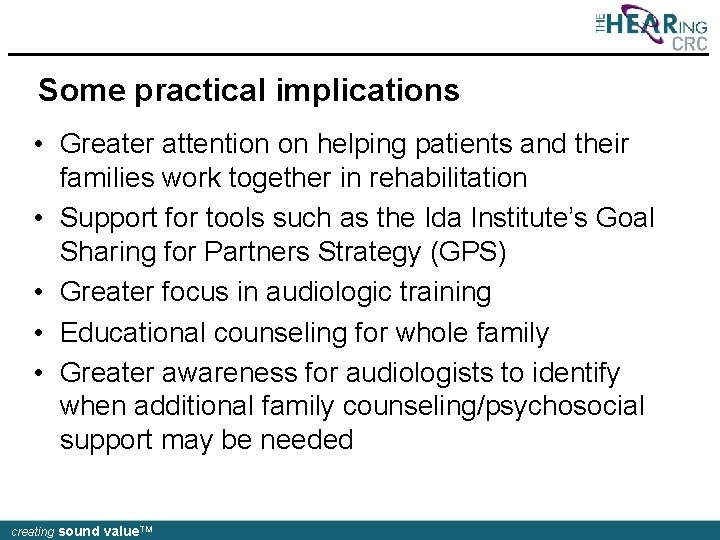
Some practical implications • Greater attention on helping patients and their families work together in rehabilitation • Support for tools such as the Ida Institute’s Goal Sharing for Partners Strategy (GPS) • Greater focus in audiologic training • Educational counseling for whole family • Greater awareness for audiologists to identify when additional family counseling/psychosocial support may be needed creating sound value. TM
Why can you do to bridge the gap? creating sound value. TM
Acknowledgements Please contact us for more information …. • • • Louise Hickson: l. hickson@uq. edu. au Nerina Scarinci: n. scarinci@uq. edu. au Carly Meyer: carly. meyer@uq. edu. au Katie Ekberg: k. ekberg@uq. edu. au Caitlin Grenness: caitlin. grenness@unimelb. edu. au This research was financially supported by the HEARing CRC established and supported under the Australian Government’s Cooperative Research Centres Program creating sound value. TM
 Connecting families
Connecting families Connecting families bath
Connecting families bath Little families
Little families Characteristics of ttl logic family
Characteristics of ttl logic family Sabre helps its clients through dashboards and analytics
Sabre helps its clients through dashboards and analytics Web essentials clients servers and communication
Web essentials clients servers and communication Clients often criticize public relations firms for
Clients often criticize public relations firms for Calling script for us it recruiter
Calling script for us it recruiter Principe de protection des clients
Principe de protection des clients Flux de données clients
Flux de données clients Typologie des clients insatisfaits
Typologie des clients insatisfaits Ibm thin client
Ibm thin client How to schedule appointments with clients
How to schedule appointments with clients Trauma-informed questions for clients
Trauma-informed questions for clients Social assessment questions
Social assessment questions Nudge for clients
Nudge for clients Multicultural view of existentialism
Multicultural view of existentialism Characteristics of a profession
Characteristics of a profession Adlerian basic mistakes examples
Adlerian basic mistakes examples Counseling multicultural clients
Counseling multicultural clients Prospecting and qualifying
Prospecting and qualifying List and describe two types of professional draping
List and describe two types of professional draping Clients needs assessment
Clients needs assessment Gnutella file sharing
Gnutella file sharing Thin client nachteile
Thin client nachteile 10 step consultation method milady
10 step consultation method milady Interactive drawing therapy
Interactive drawing therapy Ece 450
Ece 450 Ucm service en ligne
Ucm service en ligne Allontois
Allontois Design procedure of connecting rod
Design procedure of connecting rod Contrast conjunction
Contrast conjunction Connecting rod material
Connecting rod material Connecting a verbal description to table and graph
Connecting a verbal description to table and graph Pistons rings and connecting rods
Pistons rings and connecting rods Copyright
Copyright Name two segments skew to xy
Name two segments skew to xy Function of connecting rod
Function of connecting rod Compare and contrast the bach and marsalis families
Compare and contrast the bach and marsalis families