Congenital Anomalies IAnomalies of the Nipple 1 Athelia


- Slides: 53
Congenital Anomalies
I-Anomalies of the Nipple 1. Athelia: Congenital absence of the nipple (rare). 2. Polythelia: Multiple nipples that may occur anywhere along the mammary line extending from the anterior axillary fold to the inguinal region, due to persistence of milk line cells. They may be mistaken for moles or warts. 3. Retraction of the Nipple: It is present since birth & should be differentiated later from nipple retraction due to breast cancer or chronic inflammation. It is treated by massage, stretching, or surgery
II. Anomalies of the Breast 1. Amazia ; Absence of the breast (usually unilateral). May be associated with absence of the sternal part of the pectoralis major muscle. 2. Micromazia: A unilateral or bilateral small breast. Usually associated with congenital anomalies of the ovary. 3. Polymazia: Multiple or accessory breasts due to persistence of the extramammary part of the milk line (very rare). Usually present (along the milk line) in the axilla, groin, thigh or vulva or, most commonly, on the chest wall. May function during lactation and may suffer from disease as the ordinary breast. 4. Ectopic breast: • Another breast present outside the milk line such as in axillary LNs (reported cases). 5. Gynecomastia: Painless enlargement of the male breast (unilateral or bilateral) that may occur at puberty. Treatment: surgical excision. 6. Gicantomazia (Gicantomastia = Massive or Diffuse Hypertrophy of the Breast: Due to abnormal sensitivity of the breast to estrogen. Usually occurs at puberty & rarely during the first pregnancy. Treatment: Reduction mammoplasty (i. e. reduction of the breast size).
3. Traumatic Lesions 1. Cracks of the Nipple: • Etiology: Trauma of the nipple during suckling & lack of hygiene lead to cracks in the skin of the nipple & predispose to breast abscess formation due to entrance of infection through the ducts (staphylococcus) or through the lymphatics (streptococcus). C/P: Pain & bleeding during suckling. It may proceed to acute mastitis or milk retention. Treatment: Washing the nipple & areola with normal saline solution, and applying an antiseptic ointment or cream + stopping lactation (but milk is evacuated & given to the baby). Prognosis'. Healing usually occurs within 24 -48 hours
Hematoma: 1. Etiology: It occurs within half an hour after trauma, which is usually evident 2. by the bluish discoloration of the overlying skin. Sequelae: It has no relation to breast cancer, but, if not absorbed, organization will lead to the formation of a lump with subsequent nipple retraction that may simulate breast cancer. Calcification & abscess formation (infection) are other possible sequelae. 3. Treatment: a) b) c) d) In the first 24 hours -> cold (ice) compresses. In the next 24 hours —> warm compresses + antibiotics. If non-resolving or infected -» incision and drainage. If chronic or calcified —> excision
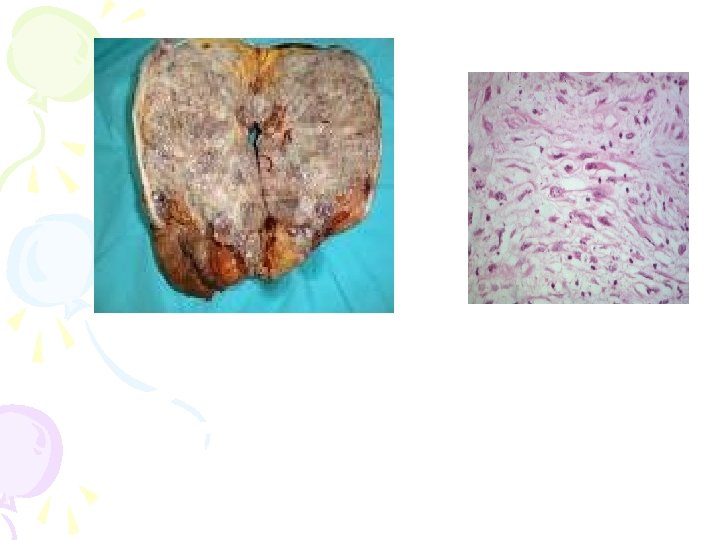
3. Traumatic Mastitis 1. Etiology: It may follow local irritation by tight brassieres or ill-fitting braces. 2. Treatment: Warm fomentations, analgesics, and antibiotics. 4. Traumatic Fat Necrosis (TFN): Pathogenesis: On trauma of the breast by a blow or SC infusion fat is crushed & fat cells are liberated. Fatty acids unite with calcium salts to form calcium soaps, which will be surrounded by fibrous tissue leading to the formation of a hard mas • C/P: Overlying skin is puckered & retracted simulating cancer, but enlarged LNs are never present & cut section shows a characteristic chalky white appearance without the yellow specks nor the gritty texture of carcinoma. It is not liable to complications or malignant transformation. 1. Treatment: It could be left alone or excised to rule out malignancy N. B. Fat Necrosis is not necessarily due to trauma but may be 2^ to mammary duct ectasia or fibrocystic disease due to rupture of cystic or dilated structures which results in extravasation of the intra-luminal contents leading to tissue necrosis & 2 ry inflammatory reaction
5. Milk Fistula: Definition: A track lined by granulation tissue between the skin and the major ducts Clinical Examination: A probe can be passed through the duct & out through the nipple. Etiology: 1. Congenital: due to abnormality in the ampulla of a major duct -> blockage by a plug of cornified cells —> stagnation —> abscess —> fistula formation. 2. Acquired: As a variant of MDE or due to incision-drainage of an abscess in a lactating breast or trauma causing duct injury. Treatment: Excision of the fistula & the related duct involved.
Inflammatory Diseases I. ACUTE MASTITIS 1. Plasma Cell Mastitis (Mammary Duct Ectasia: MDE): Definition: Dilatation of the major Subareolar milk ducts (bilateral) with stagnation of secretions (this is why it is called MDE) & infiltration with plasma cells, it is also known as varicocele tumor (worm-like dilated ducts), comedo mastitis & chemical mastitis. Clinical Picture: Nipple retraction or inversion discharge which is mostly serous but may be yellow, green, brown, thick & toothpaste-like or bloody due to congestion. 1. Breast lump: firm to hard, worm-like, painful lump (periductal mastitis) in a perimenopausal female with skin puckering & enlargement of axillary LNs. Breast cancer must be ruled out by biopsy. 2. When acute, it may present as a breast abscess. Calcification is common (tubular, annular or linear). but there is usually no epithelial hyperplasia or apocrine metaplasia
Treatment: Many patients with MDE require reassurance that there is no carcinoma & analgesics as necessary. MDE often becomes quiescent & requires no further R. Surgery is indicated for drainage of an abscess, Excisional biopsy of a mass, laying open of a fistula, or excision of subareo. Lar ducts if nipple discharge is severe. . 2. MASTITS NEONATORUM Milk secretion (witches milk) occurs from the breast at birth or on the 4 th day of life due to the presence of maternal galactogogue hormone in the infant's blood. It is as common in males as in females & usually disappears
Pubertal Mastitis: 1. More common in males. Unilateral in 80% of cases, but the opposite breast may affected later. 2. The breast is enlarged, tender, painful & indurated. 3. It is a kind of hormonal mastitis & no R' is required. It occurs at the age of 14 years & subsides spontaneously within 14 days, but induration may often persist for several weeks. 4. In some instances, enlarged tender breast may persist in males for a longer period or even years & in such cases local excision will be necessary. Traumatic Mastitis: 1. Etiology: It may follow local irritation by tight brassieres or illfitting braces. 2. Treatment: Warm fomentations, analgesics, and antibiotics. Metastatic Mastitis: May occur as a complication of mumps. Usually unilateral & more common in females.
Lactational Mastitis (Milk Engorgement): Etiology: Obstruction of the lactiferous ducts during lactation results in milk engorgement. The affected lobe forms a wedge-shaped indurated painful swelling (sector mastitis), which may proceed to abscess formation due to infection of the retained milk. Treatment: Evacuation of the breast by a breast pump, rest, and antibiotics to prevent infection. Acute Suppurative Mastitis (Breast Abscess): Predisposing Factors: milk engorgement, cracked nipple, retracted nipple. Etiology: Occurs usually during lactation & the portal of entry of infection may be through: 1. Lactiferous ducts (staphylococcus - the commonest): Usually from the child's nasopharynex. It results in localized infection due to production of coagulase enzyme. 2. Lymphatics (streptococcus - less common): Usually due to cracks in the nipple. It results in a diffuse infection due to production of fibrinolysin enzyme. 3. Blood stream. 4. Direct spread: usually from a boil in the skin.

Pathology: Inflammation causes obstruction of milk ducts & stagnation of milk (a good medium for bacterial growth), and as infection is confined under tension by fibrous septa, the affected area undergoes extensive necrosis & the abscess bursts Sites of breast abscesses: Into adjacent lobes -» multilocular intramammary If superficial, it points under the skin —» premammary abscess. If very deep (rare), it opens between the deep surface of the breast & the chest wall —» retromammary abscess
Clinical Features: A. Cellulitis Stage: 1. Severe pain & swelling of the breast with hyperemia & edema of the overlying skin. 2. Inflammation of axillary lymph nodes & General toxic manifestations. B. Abscess Stage: The swelling is at first hard & indurated but after suppuration the following occurs: 1. Fever —» hectic (due to attacks of septicemia). 2. Pain —» throbbing. 3. Edema —> hard & pitting (brawny edema) but softening & fluctuation usually occur very late. 4. Aspiration —» pus.
Investigations: Blood examination shows PNL leucocytosis. Treatment: A. Cellulitis Stage —> medical treatment: 1. Rest in bed & suspensory bandage or bra to support the breast. 2. Empty the breast regularly by the patient's own hands. 3. Stilbosterol, 5 mg/day may be given to decrease milk engorgement. 4. Hot fomentations & good hygiene. 5. Antibiotics, analgesics & anti-inflammatory drugs. 6. Weaning is indicated if the baby is close to the age of weaning or if the condition is bilateral.
Abscess Stage —> surgical treatment: 1. Do not give antibiotics at this stage (except after drainage of the abscess) to avoid the formation of hard antibioma (which simulates carcinoma). 1. On draining the abscess, start with the most fluctuant, most pointing, and most dependent area by a radial incision away from the areola. If the abscess is in the upper 1/2 of the breast, it is drained by a counter-incision in the lower half. A finger is inserted inside the abscess to break all the loculi & evacuate pus completely. A drain is put to avoid chronic abscess formation due to incomplete drainage. 1. Daily dressings & appropriate antibiotics are used till the abscess cavity obliterates. It is advisable to wean the child & the mother is given Stilbosterol tablets (5 mg t. d. s
11. CHRONIC BREAST ABSCESS A. Chronic Non-Specific (Pyogenic) Breast Abscess: Etiology: 1. A chronic abscess following an acute abscess: due to improper treatment by antibiotics, non- dependent incision, or non-breaking of all loculi. 2. A chronic abscess from the start: in this case there is equilibrium between host resistance & infection. It occurs on top of a specific lesion (cyst or tumor) or due to blood infection with an attenuated organism. Pathology: 1. A multilocular abscess. Pus may be sterile with the organism residing the wall of the abscess. 2. The abscess wall consists of fibrous tissue & is lined with a pyogenic membrane, and the surrounding zone shows evidence of chronic inflammation.
Clinical Picture: 1. General constitutional manifestations are very mild & become evident during acute exacerbations. 2. The mass is firm or hard, painless, ill-defined, fixed within the breast substance, and may be attached to the skin. It may cause nipple retraction. 3. Axillary lymph nodes may be enlarged & slightly tender. Investigations 1. General investigations + aspiration (pus). 2. Excisional biopsy (for doubtful lesions). Treatment: It must be excised because it may be mistaken for a carcinoma & to avoid complications Complications: Acute exacerbations, toxemia, breast tissue destruction, carcinoma may develop in its wall
B. Chronic Specific Inflammation (Chronic Specific Breast Abscess): 1. Syphilis ($) Clinical Picture • $ is not present nowadays but may occur in one of the following forms: 1. 1 ry $: may affect the nipple or areola, from kissing or from nursing a syphilitic child who can only infect a healthy wet nurse, but not his own mother (Colle's law). The chancre appears as a painless indurated ulcer with enlarged axillary LNs. 2. 2 ry $ : may be associated with a painful breast swelling (syphilitic mastitis) or with condylomata in the submammary fold. 3. 3 r/ $: rare and occurs in the form of diffuse fibrosis or gumtna that may form a gummatous ulcer. Axillary LNs are not enlarged except after 2 iy infection & WR is +ve. Treatment: Doubtful lumps should be excised (biopsy) + anti-$ treatment.
2. Tuberculosis (TB) Routes of Infection: 1. Direct Spread: from TB ribs (tuberculous osteomyelitis) or pleura (empyema necessitans). 2. lymphatic Spread: from axillary & mediastinal LNs or retrograde from cervical tuberculous lymphadenitis 3. Blood Spread (rare): multiple foci as a part of miliary TB. Clinical Picture: 1. Caseous Form: If resistance is low and virulence is high tubercles or nodules (single or multiple) that undergo caseation to form cold abscesses and may be also sinuses. 2. Sclerosing Form: If resistance is high & virulence is low —» fibrosis (a dense fibrous mass that may retract the nipple or adhere to the skin simulating carcinoma. 3. Fibrocaseous Form: If both resistance & virulence are moderate. 4. Disseminated Form: Multiple nodules with multiple cold abscesses. 5. Suppurative Form: When a cold abscess becomes infected. 6. Signs of TB toxemia may be present. Axillary LNs may enlarge, caseate & form multiple sinuses Investigations: Sputum culture & Plain X-ray chest + examination of he discharge + Biopsy. mastectomy.
Treatment : A. General Treatment: Anti-tuberculous drugs. B. Local Treatment: 1. TB nodule ~» excision & biopsy. 2. Cold abscess -> valvular non-dependent aspiration + local injection of anti-tuberculous drugs. 3. If the breast is shrunken & fibrocaseous -» simple mastectomy.
3. Actinomycosis Incidence: A very rare disease. Routes of Infection: 1. 1 ry: from direct spread along the lactiferous ducts. 2. 2 ry: due to local spread from the lungs and pleura. Clinical Picture: The affected breast shows multiple abscesses & sinuses discharging sulfur granules. Treatment: Simple mastectomy if conservative treatment fails.
Fibrocystic Disease (FCD)
Synonyms: Fibroadenosis (the most commonly used term), mammary dysplasia (the best descriptive term), fibrocystic changes, dysplastic mastitis, chronic interstitial mastitis, chronic cyclical mastitis, Proliferative & non-proliferative breast disease, ANDI (Abberation of Normal Development & Involution). Definition: Epithelial hyperplasia in the ducts & acini (epitheliosis), increase in number of acini & ductules (adenosis) with fibrosis & cyst formation (fibrocystic) & round cell infiltration in the connective tissue stroma.
Etiology: 1. Inflammation: Formerly, it was considered to be a chronic inflammatory lesion (interstitial mastitis) resulting from irritation by stagnant secretions or abnormal involution at menopause. This theory is no longer valid. 2. Hormonal Imbalance: Increased prolactin or unopposed estrogen by progesterone & testosterone. in This theory is supported by the following observations: 1. The disease is limited to the child-bearing period (20 years to menopause). 2. It occurs more in unmarried & nulliparous women. 3. It improves markedly by testosterone or by castration (radiological or surgical). 4. It can be produced in rats by the injection of estrin (estrogen). 5. A similar affection occurs in males receiving estrogen for R/ of prostatic carcinoma. 3. Recently, Methyl Xanthines (caffeine) have been suggested as causative agents. 4. Immunological Theory suggesting target organ defect.
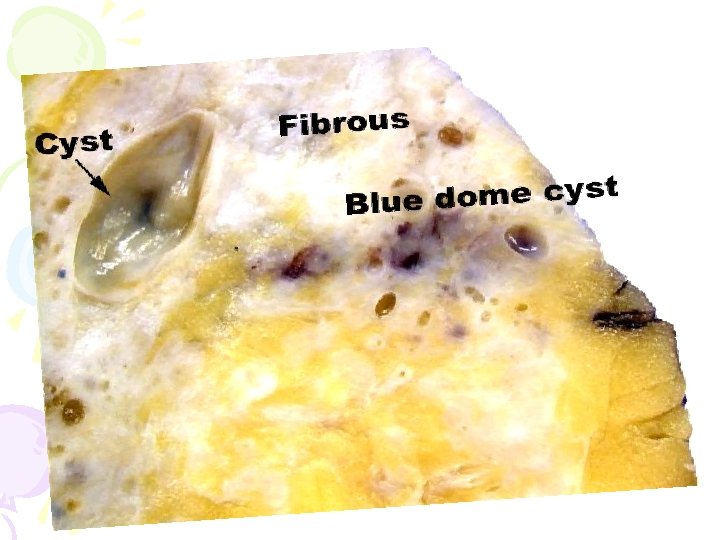
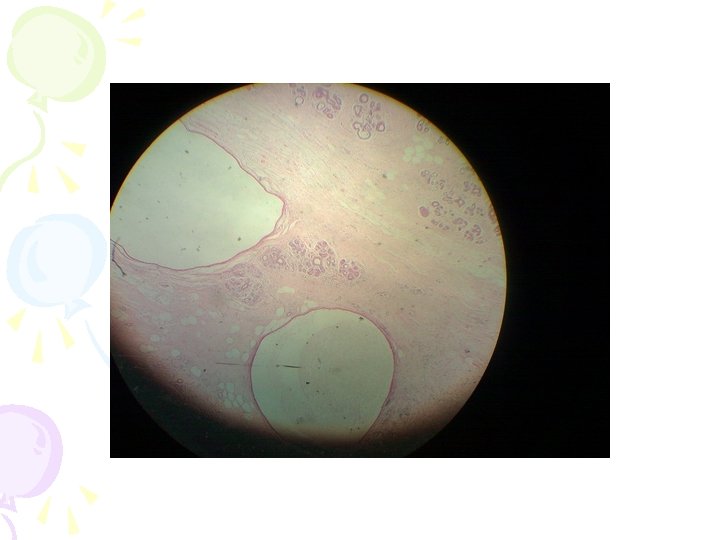
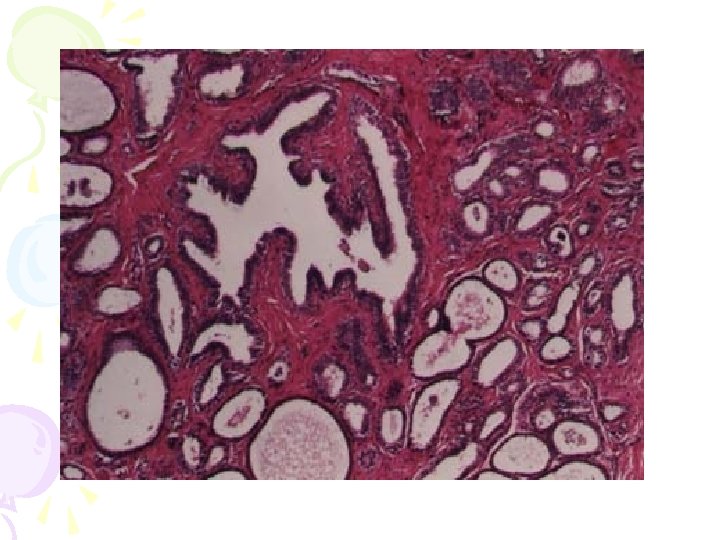
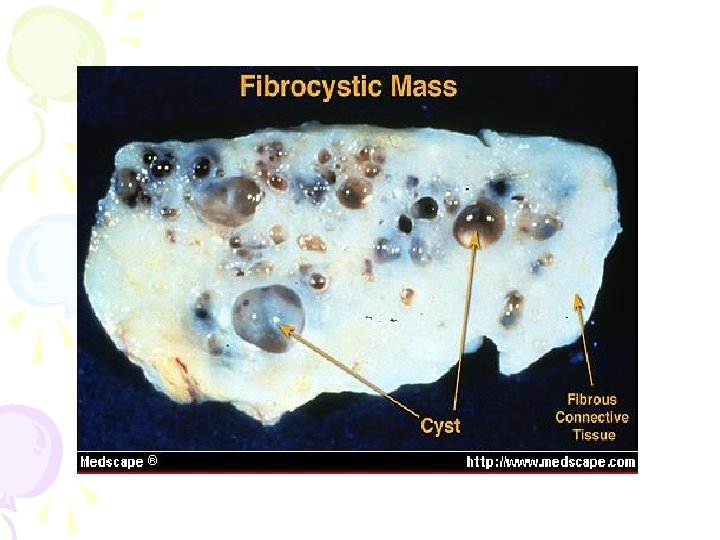
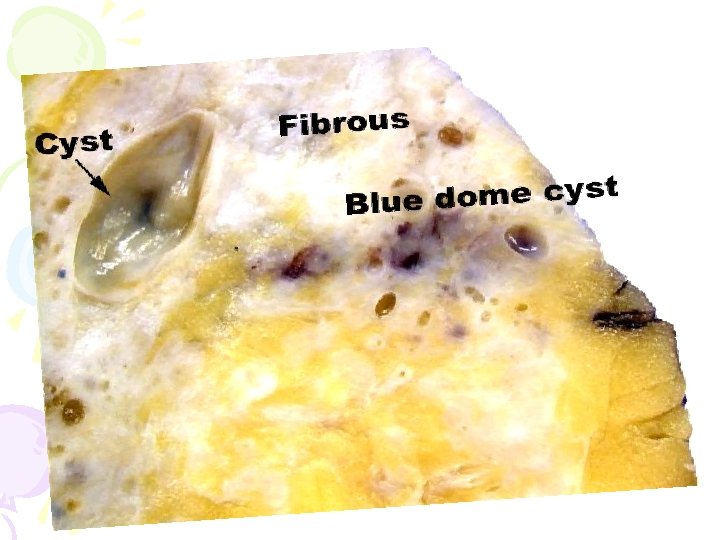
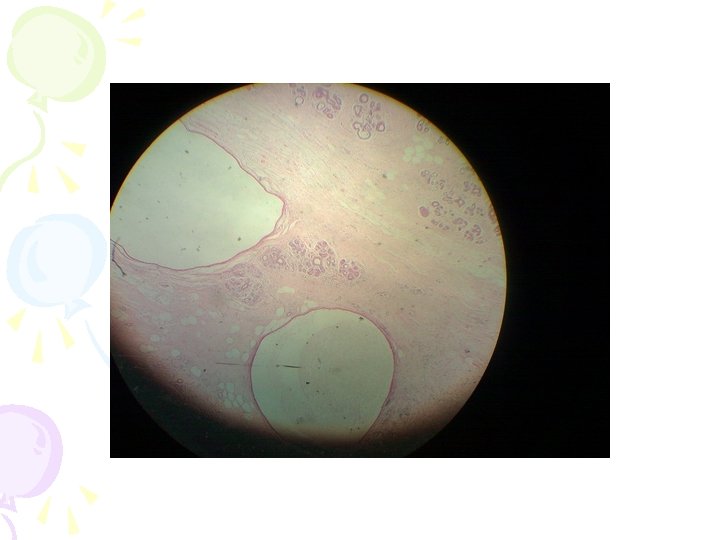
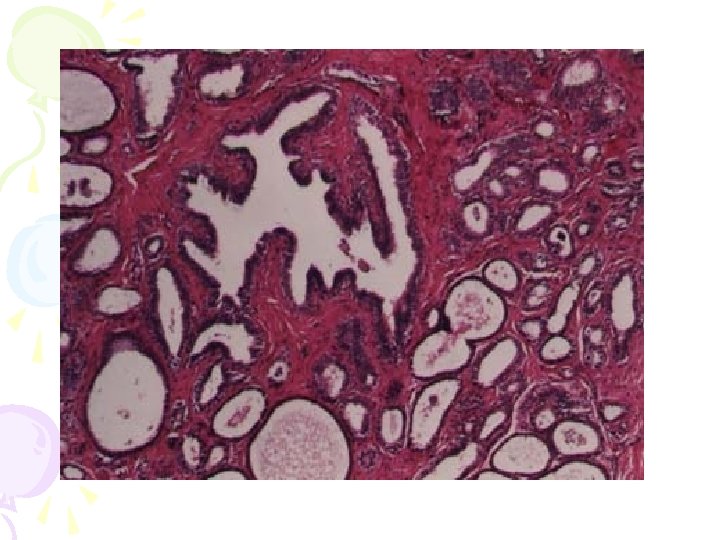
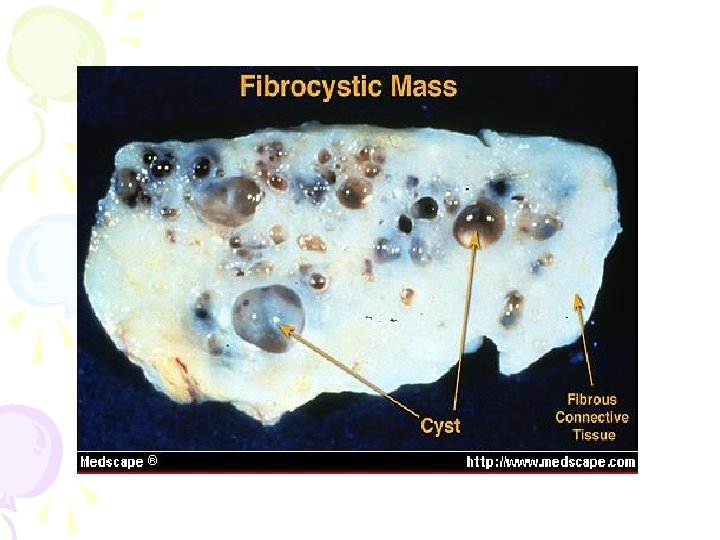
Pathology: NEA: The affected area becomes thickened, tough & rubbery. The cut surface is white or yellow (never gray as in carcinoma) & often shows multiple cysts of different sizes, and may be visible papillomatous projections into the larger cysts as well (Brodie 's Tumor). Microscopic Picture: 1. Epithelial proliferation: a- Adenosis: ↑ in number of acini & ductules, which may produce small tumor-like masses similar to fibroadenomata. Adenosis is shown by budding of acini & overall ↑ in glandular tissue. b- Epitheliosis: Hyperplasia of the cells lining the acini reaching 3 or 4 layers & when severe, may project into the lumen as small duct papillomata (duct papillomatosis). 2. Fibrosis: Periacinar & periductal tissues are infiltrated with lymphocytes & plasma cells & are replaced by dense fibrous tissue (F. T). 3 - Cyst Formation: Proliferation of cells & constriction by F. T. cause duct obstruction & retention cysts of different sizes, which are lined by columnar epithelium & filled with clear or yellow fluid, which may be discolored by altered blood.
A. Special Cysts: • Microcysts (Brodie's Tumor): Multiple small cysts lined by columnar epithelium Macrocyst (Blue-domed Cyst of Bloodgood) It is a solitary large cyst, lined by flattened epithelium & contains clear fluid shining inside Histological Types of FCD: . Non-proliferative: This type does not turn malignant and may show one of the following: a)Fibrosis (diffuse —» shrunken breast, or localized —> breast lump). b)Cysts: retention cysts of different sizes due to stenosis of the ducts. c)Fibroadenosis: multiple masses in the breast with well formed acini surrounded by fibrous tissue. Proliferative‘: This type is liable to turn malignant and it may show any of the following: a)Epithelial hyperplasia —> breast lump. b)Ductal hyperplasia -> increased duct formation. c)Ductal papillomatosis —> bleeding per nipple.
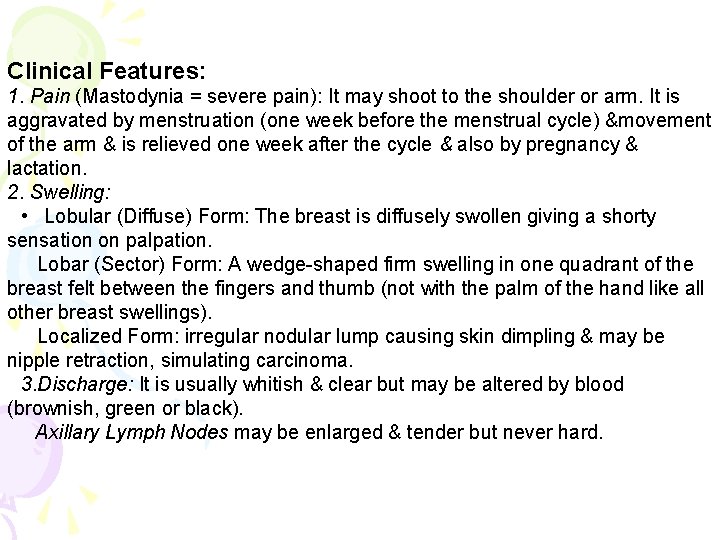
Clinical Features: 1. Pain (Mastodynia = severe pain): It may shoot to the shoulder or arm. It is aggravated by menstruation (one week before the menstrual cycle) &movement of the arm & is relieved one week after the cycle & also by pregnancy & lactation. 2. Swelling: • Lobular (Diffuse) Form: The breast is diffusely swollen giving a shorty sensation on palpation. Lobar (Sector) Form: A wedge-shaped firm swelling in one quadrant of the breast felt between the fingers and thumb (not with the palm of the hand like all other breast swellings). Localized Form: irregular nodular lump causing skin dimpling & may be nipple retraction, simulating carcinoma. 3. Discharge: It is usually whitish & clear but may be altered by blood (brownish, green or black). Axillary Lymph Nodes may be enlarged & tender but never hard.
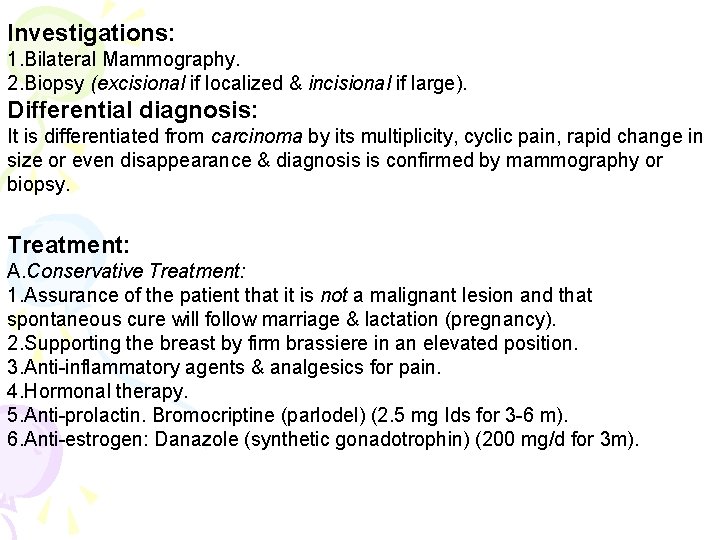
Investigations: 1. Bilateral Mammography. 2. Biopsy (excisional if localized & incisional if large). Differential diagnosis: It is differentiated from carcinoma by its multiplicity, cyclic pain, rapid change in size or even disappearance & diagnosis is confirmed by mammography or biopsy. Treatment: A. Conservative Treatment: 1. Assurance of the patient that it is not a malignant lesion and that spontaneous cure will follow marriage & lactation (pregnancy). 2. Supporting the breast by firm brassiere in an elevated position. 3. Anti-inflammatory agents & analgesics for pain. 4. Hormonal therapy. 5. Anti-prolactin. Bromocriptine (parlodel) (2. 5 mg Ids for 3 -6 m). 6. Anti-estrogen: Danazole (synthetic gonadotrophin) (200 mg/d for 3 m).
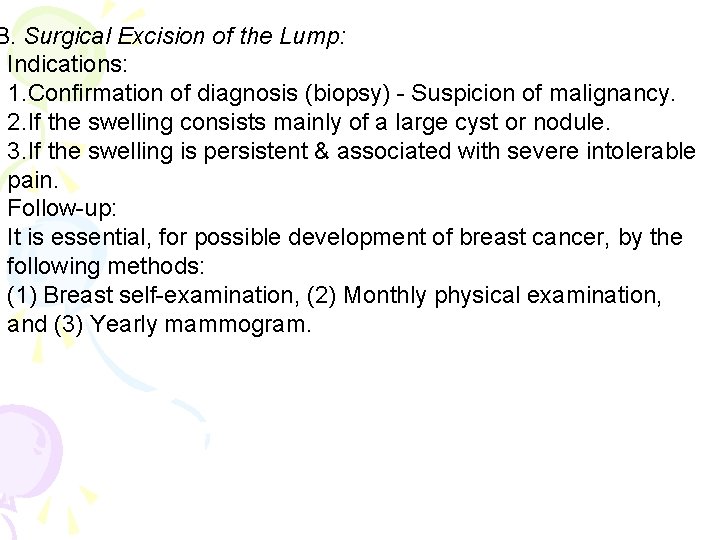
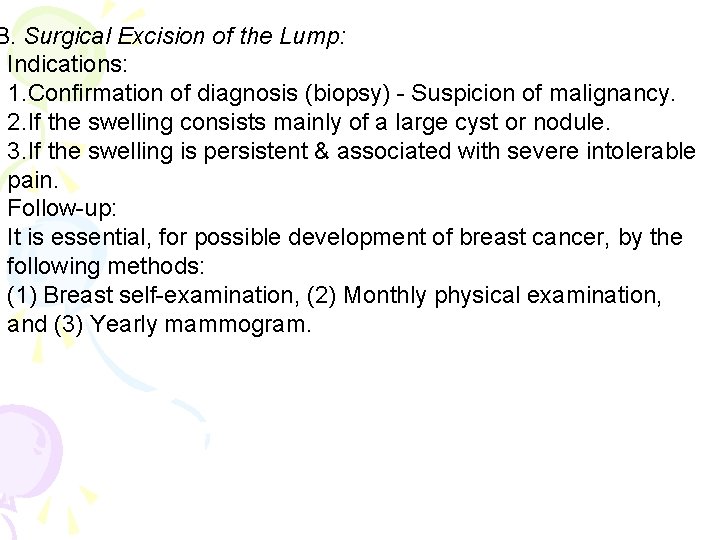
B. Surgical Excision of the Lump: Indications: 1. Confirmation of diagnosis (biopsy) - Suspicion of malignancy. 2. If the swelling consists mainly of a large cyst or nodule. 3. If the swelling is persistent & associated with severe intolerable pain. Follow-up: It is essential, for possible development of breast cancer, by the following methods: (1) Breast self-examination, (2) Monthly physical examination, and (3) Yearly mammogram.
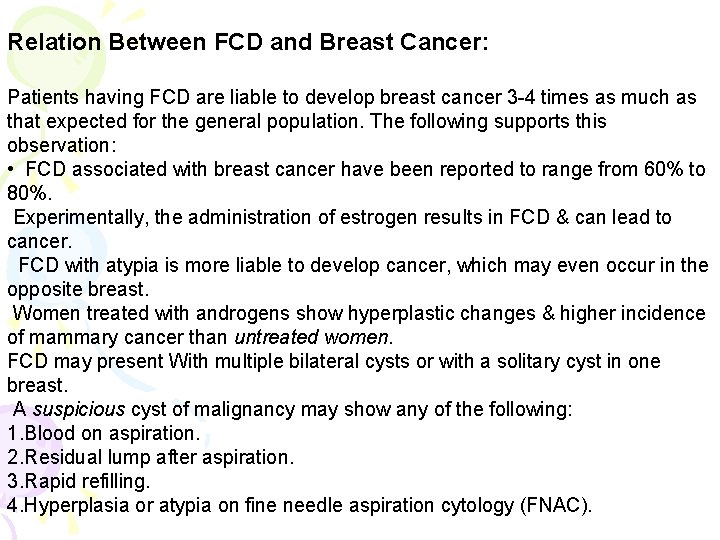
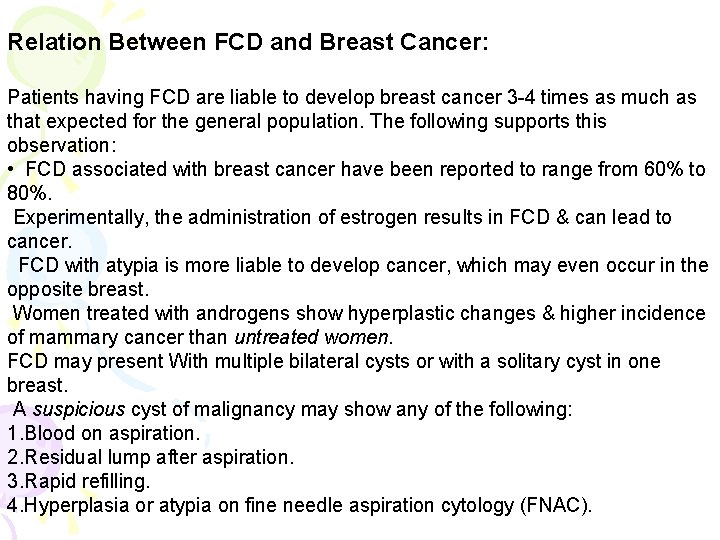
Relation Between FCD and Breast Cancer: Patients having FCD are liable to develop breast cancer 3 -4 times as much as that expected for the general population. The following supports this observation: • FCD associated with breast cancer have been reported to range from 60% to 80%. Experimentally, the administration of estrogen results in FCD & can lead to cancer. FCD with atypia is more liable to develop cancer, which may even occur in the opposite breast. Women treated with androgens show hyperplastic changes & higher incidence of mammary cancer than untreated women. FCD may present With multiple bilateral cysts or with a solitary cyst in one breast. A suspicious cyst of malignancy may show any of the following: 1. Blood on aspiration. 2. Residual lump after aspiration. 3. Rapid refilling. 4. Hyperplasia or atypia on fine needle aspiration cytology (FNAC).
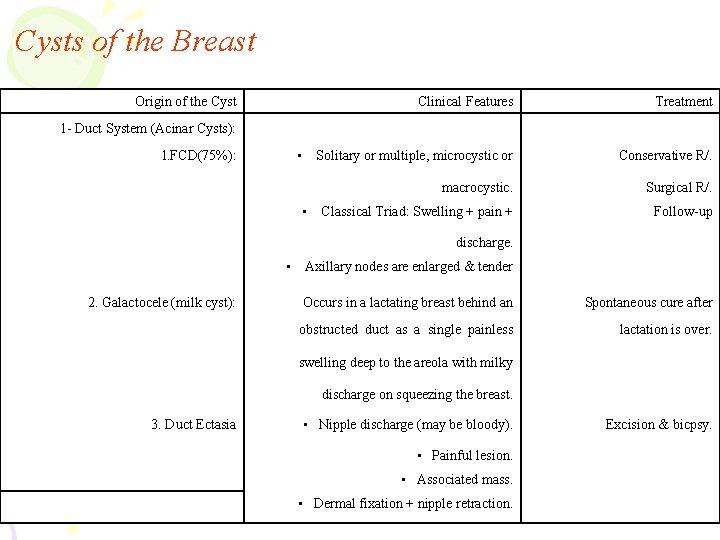
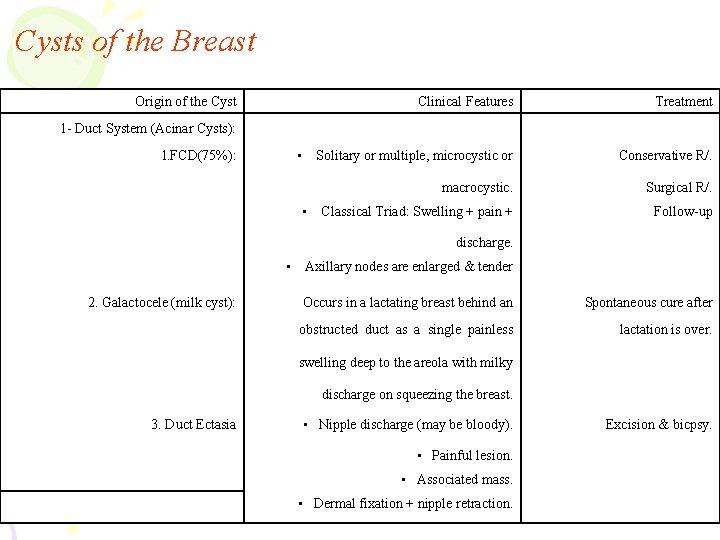
Cysts of the Breast Origin of the Cyst Clinical Features Treatment Solitary or multiple, microcystic or Conservative R/. macrocystic. Surgical R/. Classical Triad: Swelling + pain + Follow-up 1 - Duct System (Acinar Cysts): • l. FCD(75%): • discharge. • 2. Galactocele (milk cyst): Axillary nodes are enlarged & tender Occurs in a lactating breast behind an Spontaneous cure after obstructed duct as a single painless lactation is over. swelling deep to the areola with milky discharge on squeezing the breast. 3. Duct Ectasia • Nipple discharge (may be bloody). • Painful lesion. • Associated mass. • Dermal fixation + nipple retraction. Excision & bicpsy.
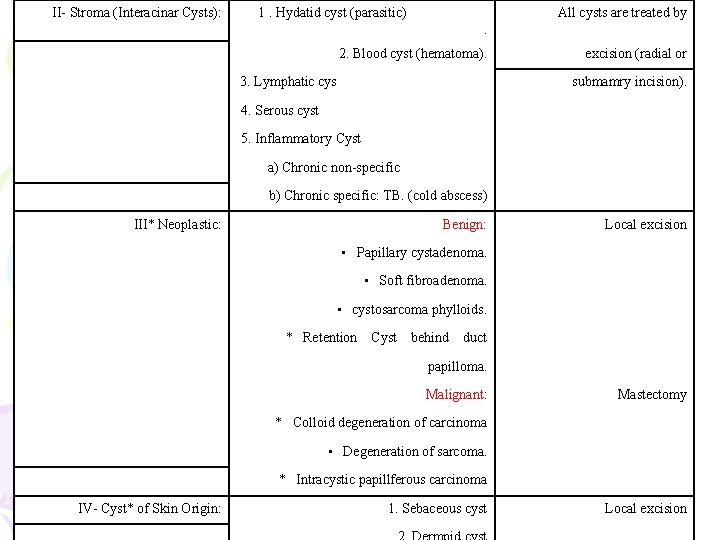
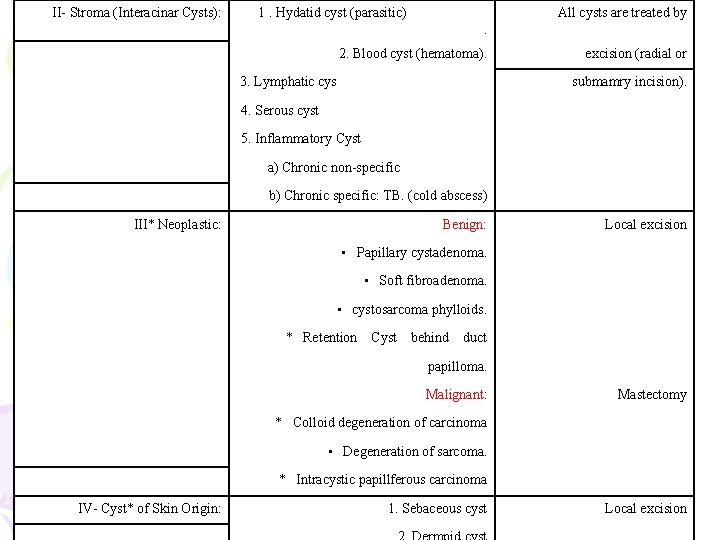
II- Stroma (Interacinar Cysts): 1. Hydatid cyst (parasitic) All cysts are treated by. 2. Blood cyst (hematoma). 3. Lymphatic cys excision (radial or submamry incision). 4. Serous cyst 5. Inflammatory Cyst a) Chronic non-specific b) Chronic specific: TB. (cold abscess) III* Neoplastic: Benign: Local excision • Papillary cystadenoma. • Soft fibroadenoma. • cystosarcoma phylloids. * Retention Cyst behind duct papilloma. Malignant: Mastectomy * Colloid degeneration of carcinoma • Degeneration of sarcoma. * Intracystic papillferous carcinoma IV- Cyst* of Skin Origin: 1. Sebaceous cyst Local excision
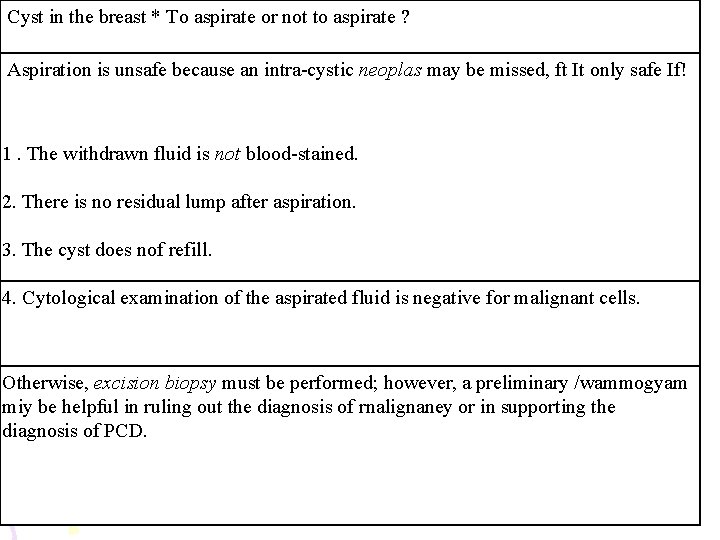
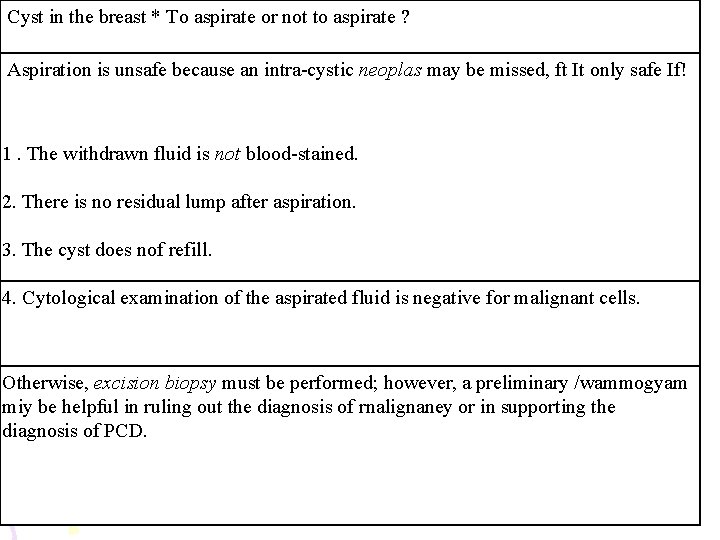
Cyst in the breast * To aspirate or not to aspirate ? Aspiration is unsafe because an intra-cystic neoplas may be missed, ft It only safe If! 1. The withdrawn fluid is not blood-stained. 2. There is no residual lump after aspiration. 3. The cyst does nof refill. 4. Cytological examination of the aspirated fluid is negative for malignant cells. Otherwise, excision biopsy must be performed; however, a preliminary /wammogyam miy be helpful in ruling out the diagnosis of rnalignaney or in supporting the diagnosis of PCD.
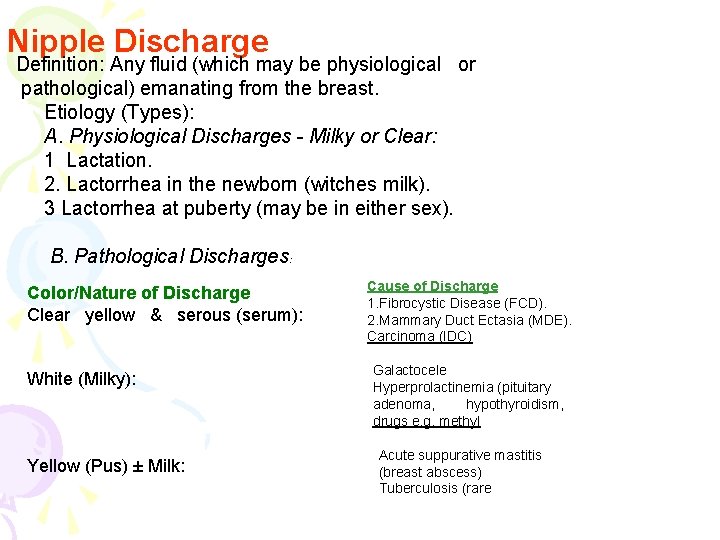
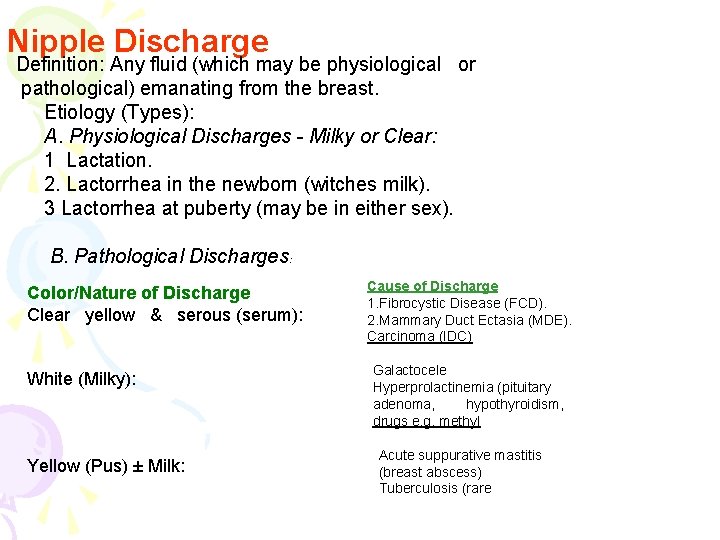
Nipple Discharge Definition: Any fluid (which may be physiological or pathological) emanating from the breast. Etiology (Types): A. Physiological Discharges - Milky or Clear: 1 Lactation. 2. Lactorrhea in the newborn (witches milk). 3 Lactorrhea at puberty (may be in either sex). B. Pathological Discharges: Color/Nature of Discharge Clear yellow & serous (serum): White (Milky): Yellow (Pus) ± Milk: Cause of Discharge 1. Fibrocystic Disease (FCD). 2. Mammary Duct Ectasia (MDE). Carcinoma (IDC) Galactocele Hyperprolactinemia (pituitary adenoma, hypothyroidism, drugs e. g. methyl Acute suppurative mastitis (breast abscess) Tuberculosis (rare
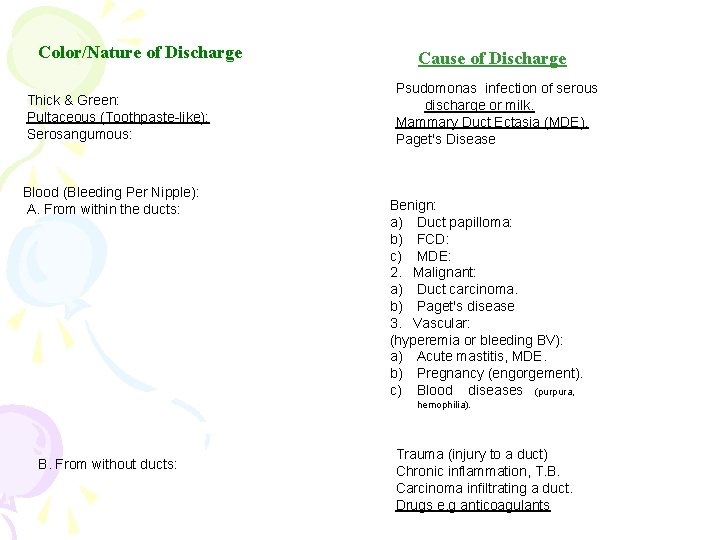
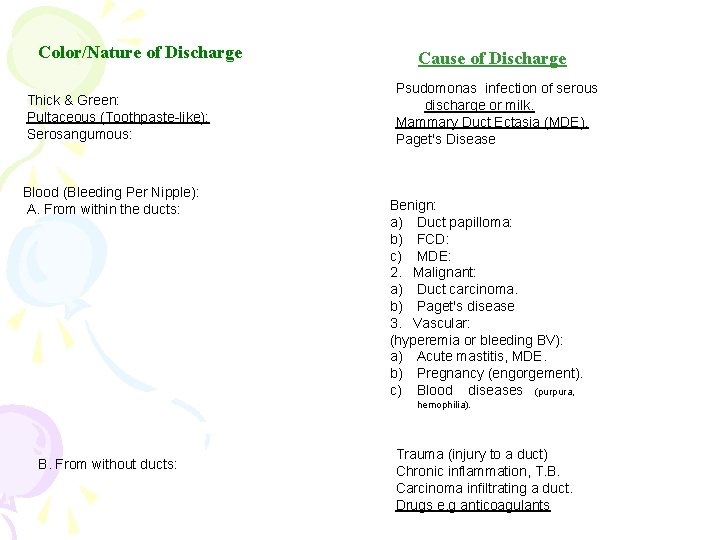
Color/Nature of Discharge Thick & Green: Pultaceous (Toothpaste-like): Serosangumous: Blood (Bleeding Per Nipple): A. From within the ducts: Cause of Discharge Psudomonas infection of serous discharge or milk. Mammary Duct Ectasia (MDE). Paget's Disease Benign: a) Duct papilloma: b) FCD: c) MDE: 2. Malignant: a) Duct carcinoma. b) Paget's disease 3. Vascular: (hyperemia or bleeding BV): a) Acute mastitis, MDE. b) Pregnancy (engorgement). c) Blood diseases (purpura, hemophilia). B. From without ducts: Trauma (injury to a duct) Chronic inflammation, T. B. Carcinoma infiltrating a duct. Drugs e. g anticoagulants
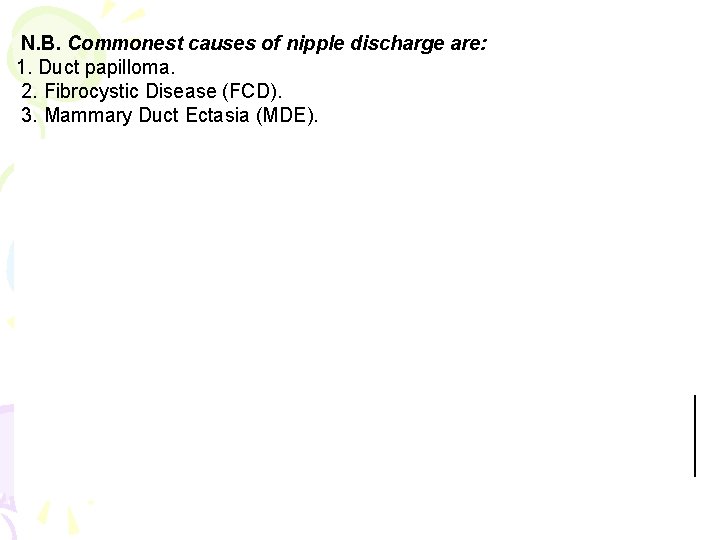
N. B. Commonest causes of nipple discharge are: 1. Duct papilloma. 2. Fibrocystic Disease (FCD). 3. Mammary Duct Ectasia (MDE).
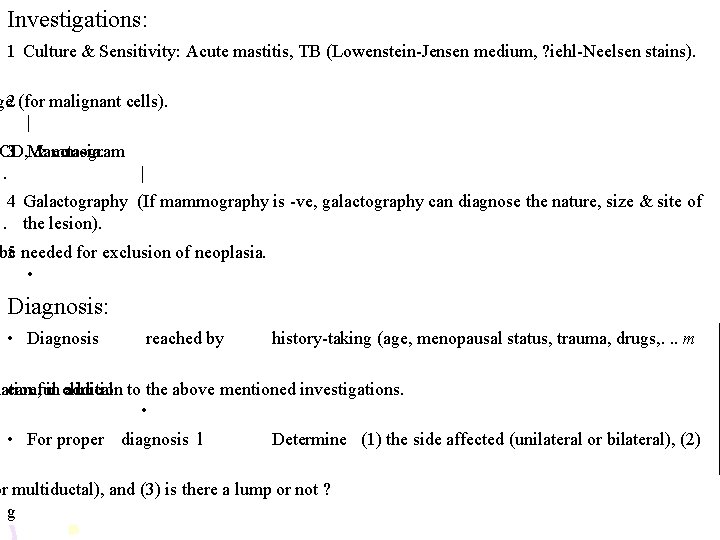
Investigations: 1 Culture & Sensitivity: Acute mastitis, TB (Lowenstein-Jensen medium, ? iehl-Neelsen stains). ge 2 (for malignant cells). | CD, 3 Mammogram & ectasia. . | 4 Galactography (If mammography is -ve, galactography can diagnose the nature, size & site of. the lesion). be 5 needed for exclusion of neoplasia. • Diagnosis: • Diagnosis reached by history-taking (age, menopausal status, trauma, drugs, . . . m nation, careful in clinical addition to the above mentioned investigations. • • For proper diagnosis l Determine (1) the side affected (unilateral or bilateral), (2) or multiductal), and (3) is there a lump or not ? g
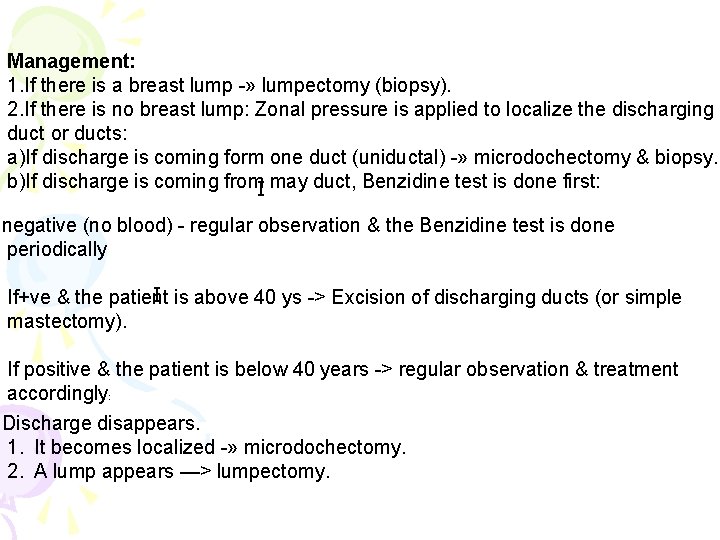
Management: 1. If there is a breast lump -» lumpectomy (biopsy). 2. If there is no breast lump: Zonal pressure is applied to localize the discharging duct or ducts: a)If discharge is coming form one duct (uniductal) -» microdochectomy & biopsy. b)If discharge is coming from. I may duct, Benzidine test is done first: negative (no blood) - regular observation & the Benzidine test is done periodically I is above 40 ys -> Excision of discharging ducts (or simple If+ve & the patient mastectomy). If positive & the patient is below 40 years -> regular observation & treatment accordingly: Discharge disappears. 1. It becomes localized -» microdochectomy. 2. A lump appears —> lumpectomy.
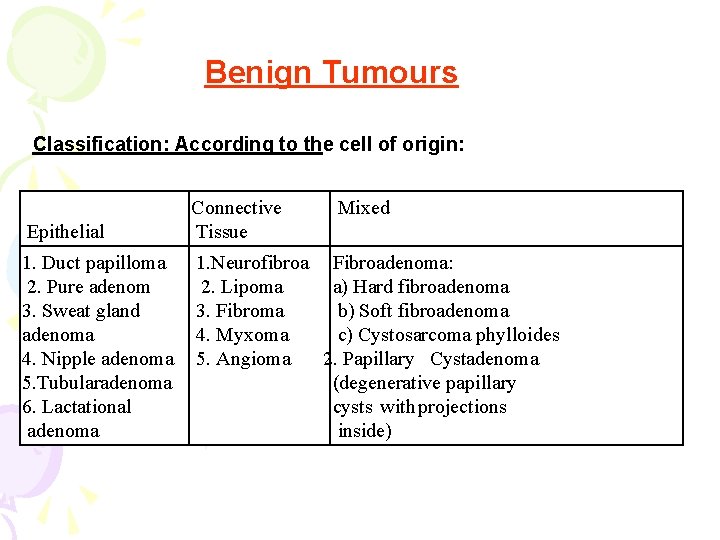
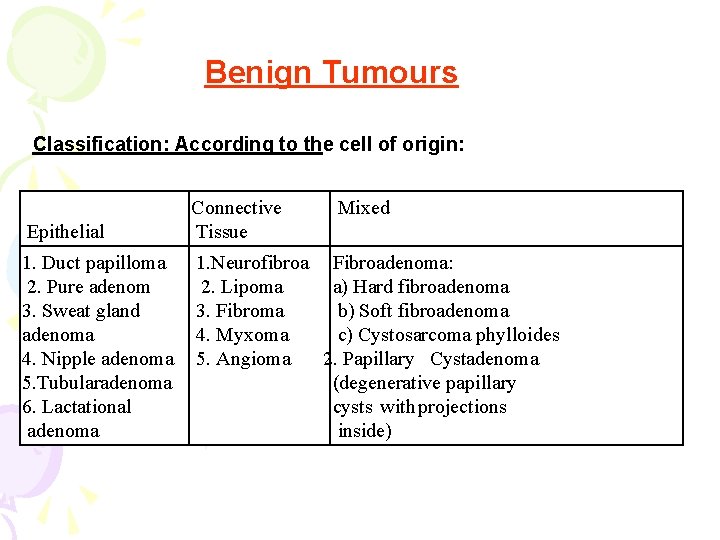
Benign Tumours Classification: According to the cell of origin: Epithelial Connective Tissue Mixed 1. Duct papilloma 2. Pure adenom 3. Sweat gland adenoma 4. Nipple adenoma 5. Tubularadenoma 6. Lactational adenoma 1. Neurofibroa Fibroadenoma: 2. Lipoma a) Hard fibroadenoma 3. Fibroma b) Soft fibroadenoma 4. Myxoma c) Cystosarcoma phylloides 5. Angioma 2. Papillary Cystadenoma (degenerative papillary cysts with projections inside)
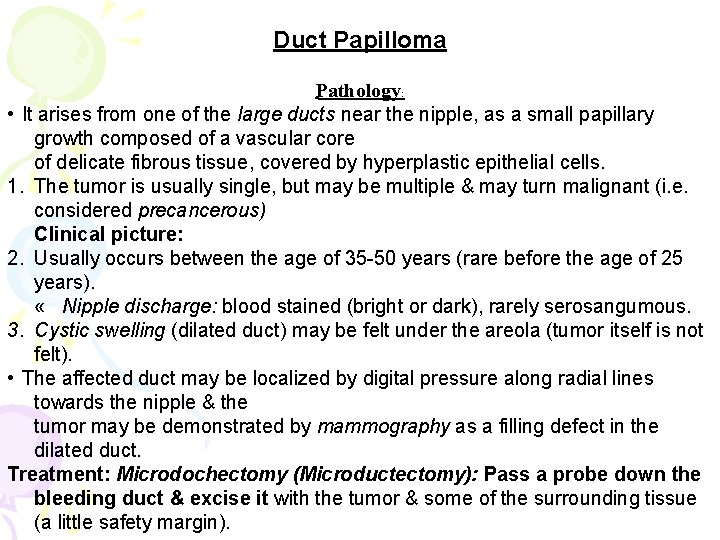
Duct Papilloma Pathology: • It arises from one of the large ducts near the nipple, as a small papillary growth composed of a vascular core of delicate fibrous tissue, covered by hyperplastic epithelial cells. 1. The tumor is usually single, but may be multiple & may turn malignant (i. e. considered precancerous) Clinical picture: 2. Usually occurs between the age of 35 -50 years (rare before the age of 25 years). « Nipple discharge: blood stained (bright or dark), rarely serosangumous. 3. Cystic swelling (dilated duct) may be felt under the areola (tumor itself is not felt). • The affected duct may be localized by digital pressure along radial lines towards the nipple & the tumor may be demonstrated by mammography as a filling defect in the dilated duct. Treatment: Microdochectomy (Microductectomy): Pass a probe down the bleeding duct & excise it with the tumor & some of the surrounding tissue (a little safety margin).
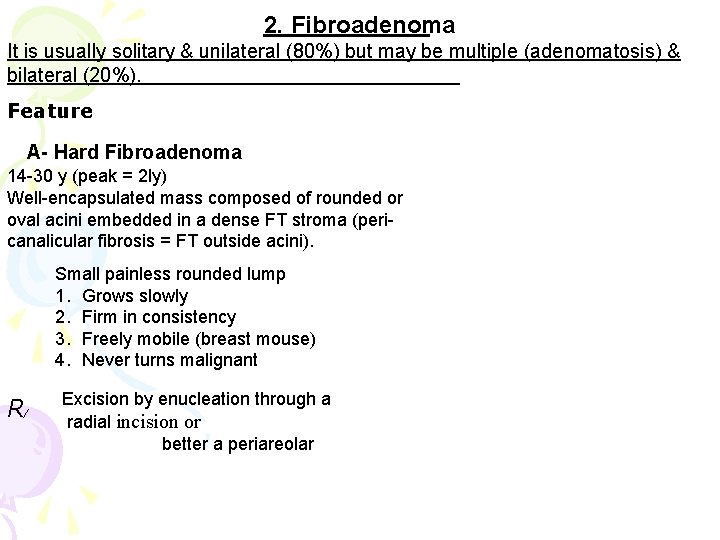
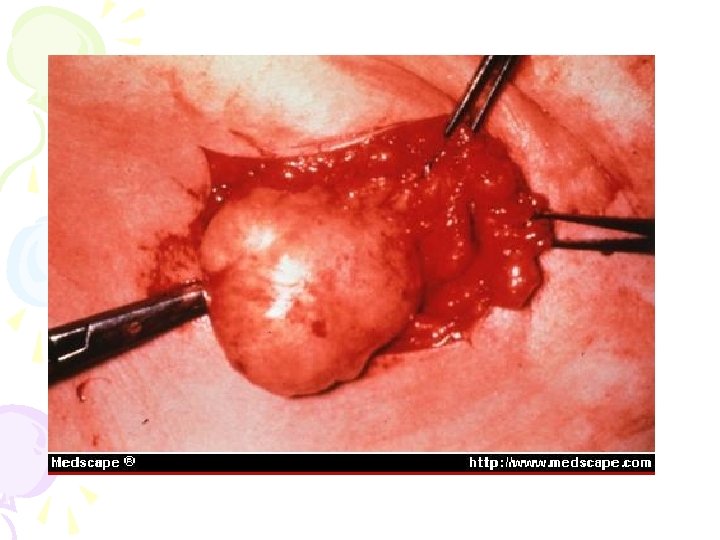
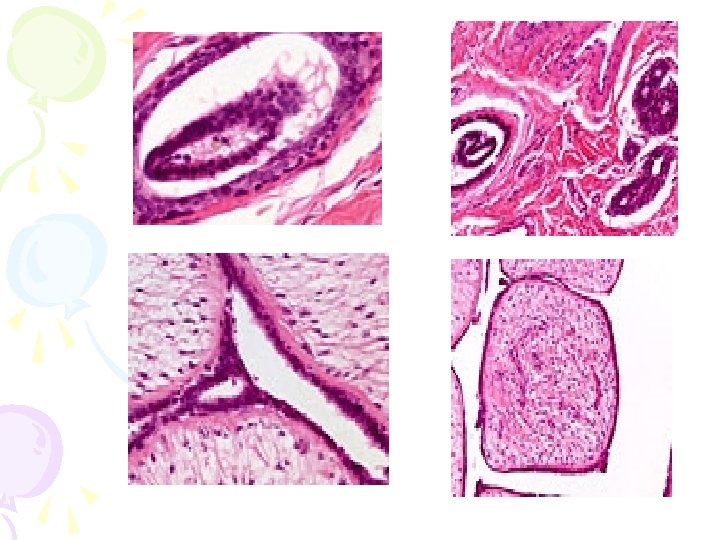
2. Fibroadenoma It is usually solitary & unilateral (80%) but may be multiple (adenomatosis) & bilateral (20%). Feature A- Hard Fibroadenoma 14 -30 y (peak = 2 ly) Well-encapsulated mass composed of rounded or oval acini embedded in a dense FT stroma (pericanalicular fibrosis = FT outside acini). Small painless rounded lump 1. Grows slowly 2. Firm in consistency 3. Freely mobile (breast mouse) 4. Never turns malignant R/ Excision by enucleation through a radial incision or better a periareolar
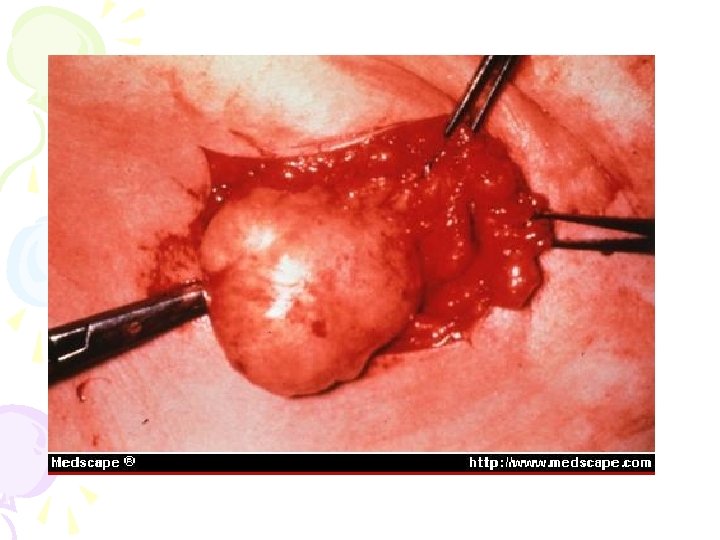
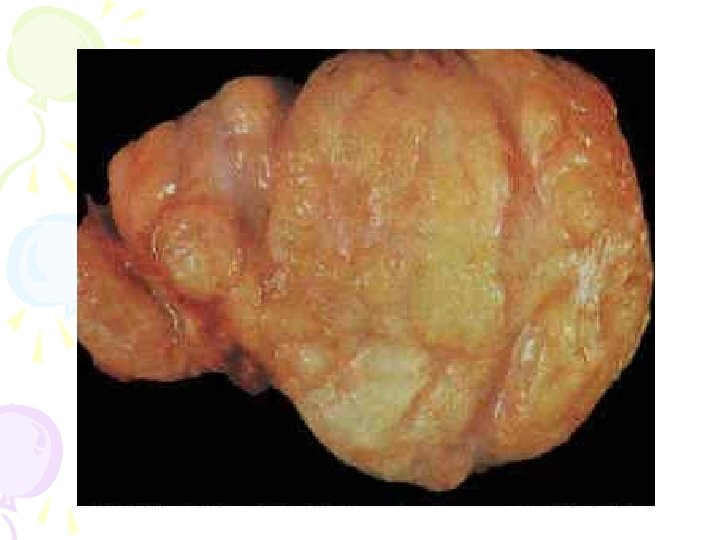
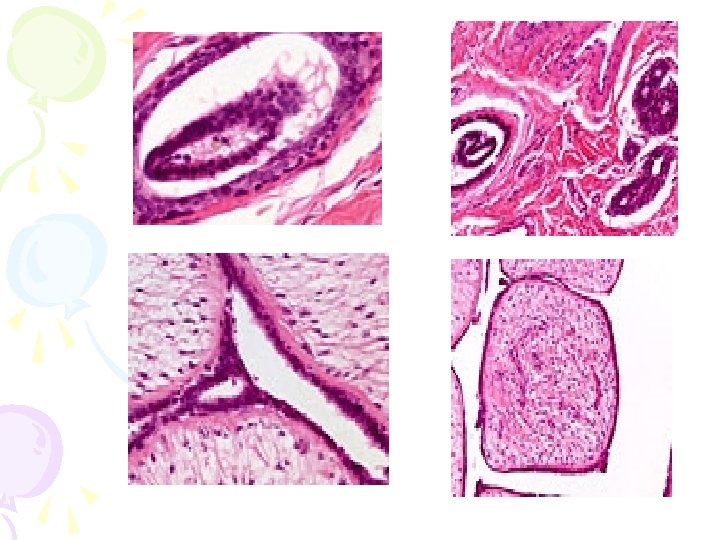
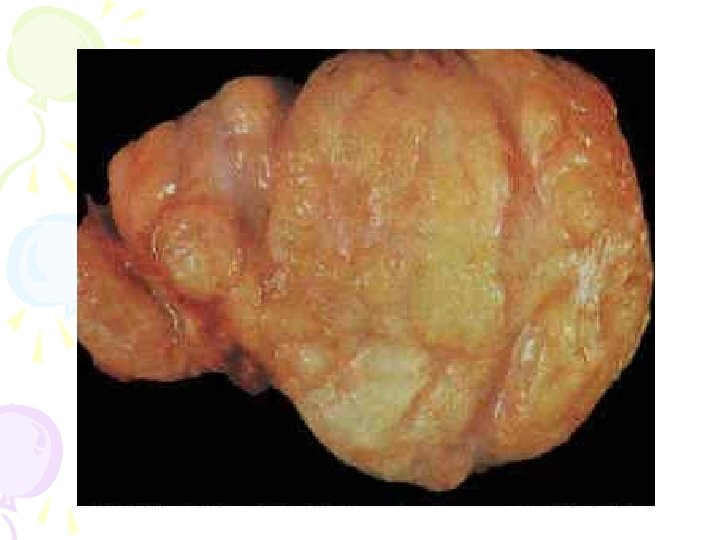
B- Soft Fibroadenoma Older age (30 -50 y) A mass, not well-capsulated partly solid & partly cystic, composed of delicate FT projections into the lumen of dilated ducts (intracanalicular fibrosis). C /p 1. Larger lobulated lump (painless). 2. Grows more rapidly 3. Soft ± cystic (cystadenoma) 4. Less mobile, may fungate 5. May turn sarcomatous Excision (submammary incision) or simple mastectomy (may be required).
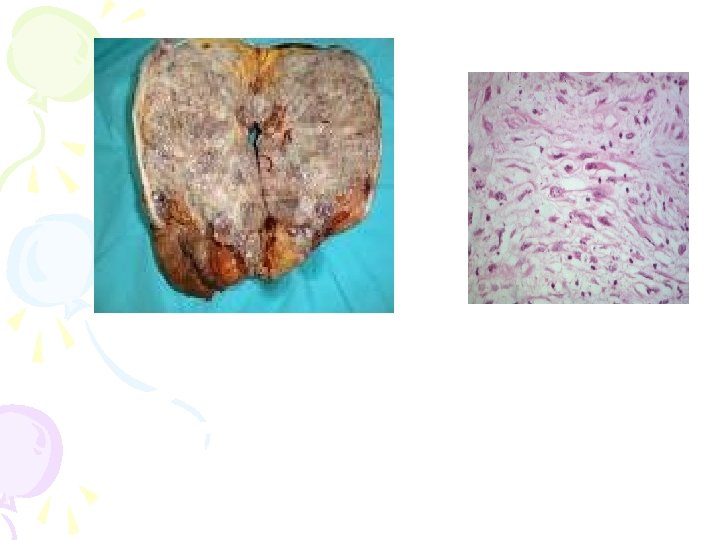
C. Cystosarcoma Phylloides Definition: Phylloides means leaf-like pattern (Greek). It is a giant soft fibroadenoma (intracanalicular) & is called sarcoma because it is a rapidly growing fleshy hot tumor with dilated veins & stretched areola & skin, but without LN enlargement or fixation to the skin or muscles. Clinical picture: » The patient, usually > 40 y, presents with a large, wellcircumscribed, rounded or lobular, mobile mass that usually attains a large tear drop appearance of profile & has a heterogenous consistency. 1. The overlying skin is red, shiny, warm, stretched & may show dilated veins, but no tenderness. 2. If malignant transformation occurs it involves the stromal mesothelial cells of the tumor so that metastases are usually hematogenous to the lungs, rather than to axillary LNs. Treatment: Simple mastectomy (Local excision -> recurrence & ↑ chance of turning into sarcoma