Conductive system of heart Elongated branching cells containing
Conductive system of heart
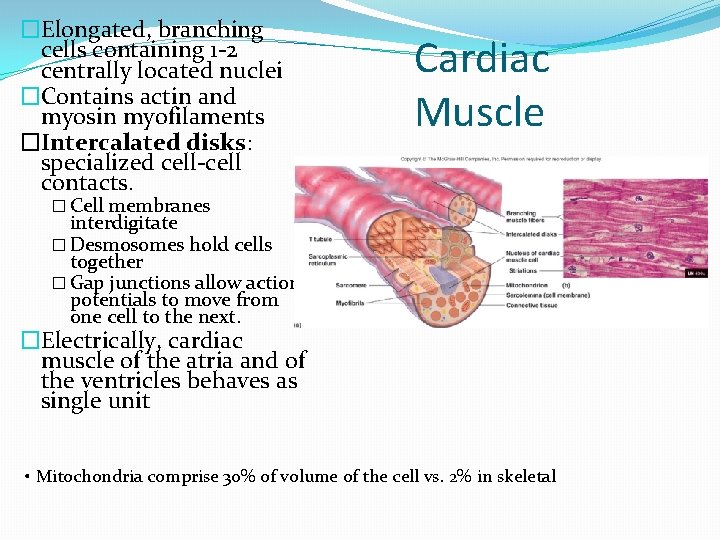
�Elongated, branching cells containing 1 -2 centrally located nuclei �Contains actin and myosin myofilaments �Intercalated disks: specialized cell-cell contacts. Cardiac Muscle � Cell membranes interdigitate � Desmosomes hold cells together � Gap junctions allow action potentials to move from one cell to the next. �Electrically, cardiac muscle of the atria and of the ventricles behaves as single unit • Mitochondria comprise 30% of volume of the cell vs. 2% in skeletal
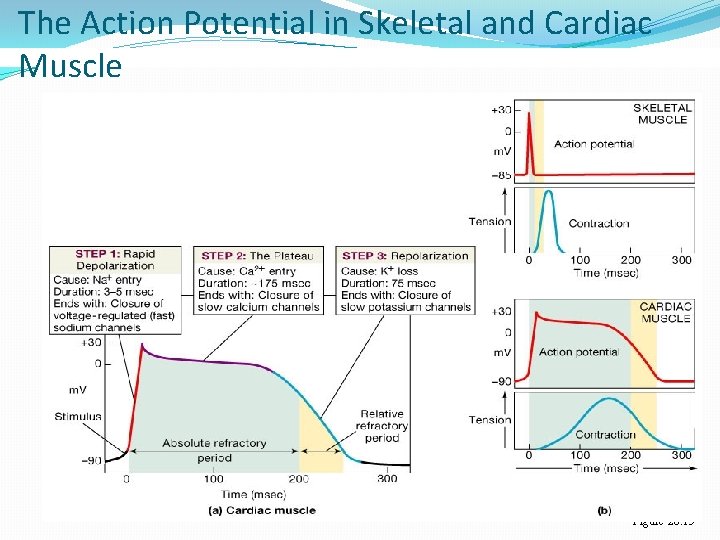
The Action Potential in Skeletal and Cardiac Muscle Figure 20. 15
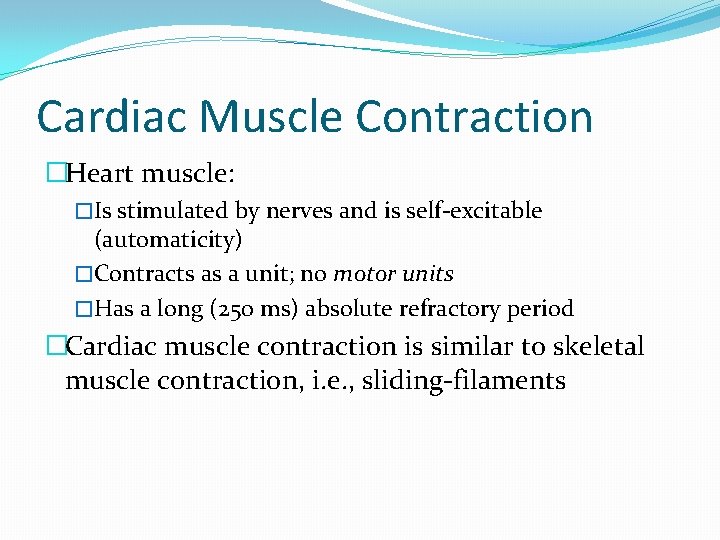
Cardiac Muscle Contraction �Heart muscle: �Is stimulated by nerves and is self-excitable (automaticity) �Contracts as a unit; no motor units �Has a long (250 ms) absolute refractory period �Cardiac muscle contraction is similar to skeletal muscle contraction, i. e. , sliding-filaments
Conductive System of Heart
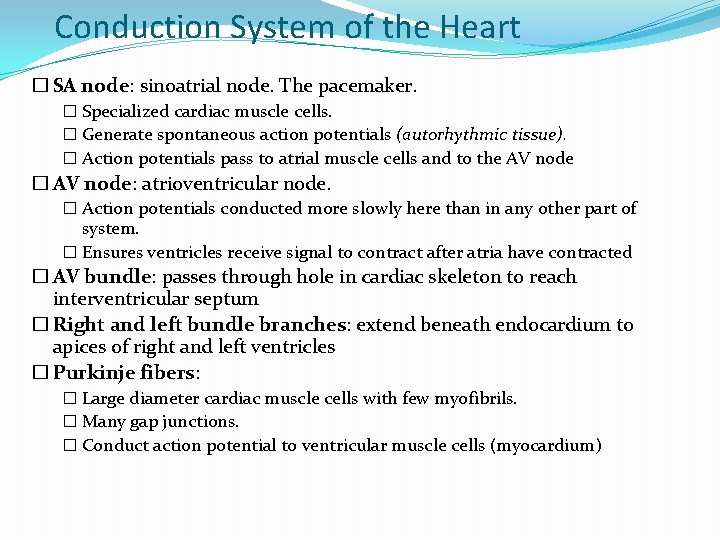
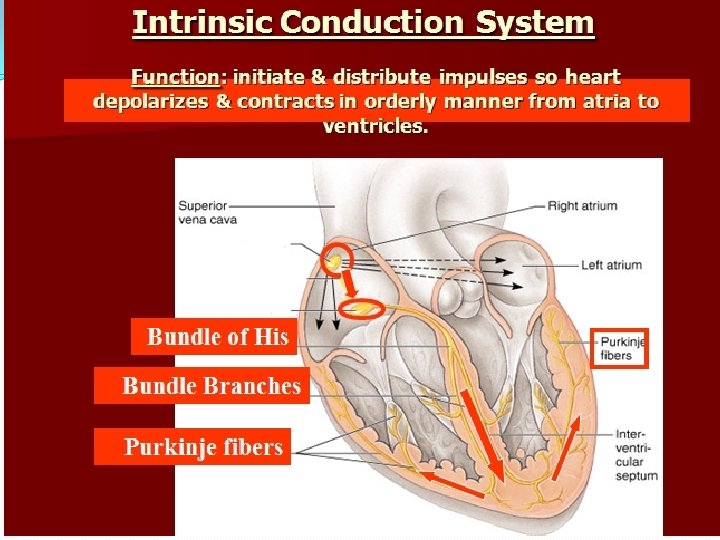
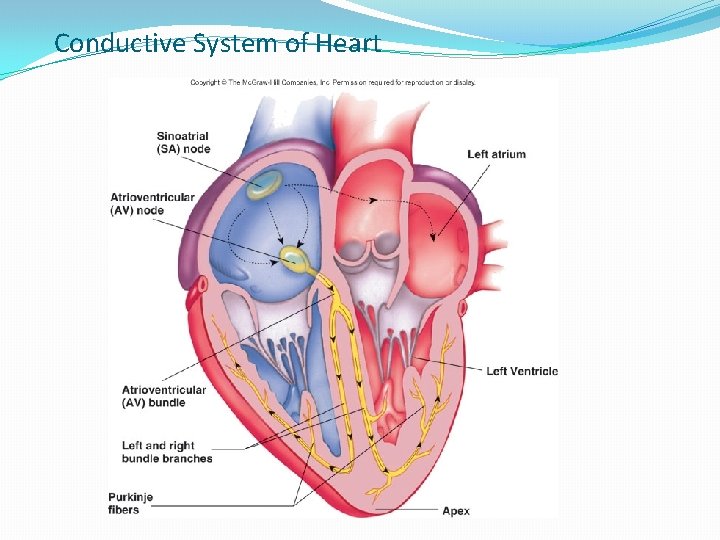
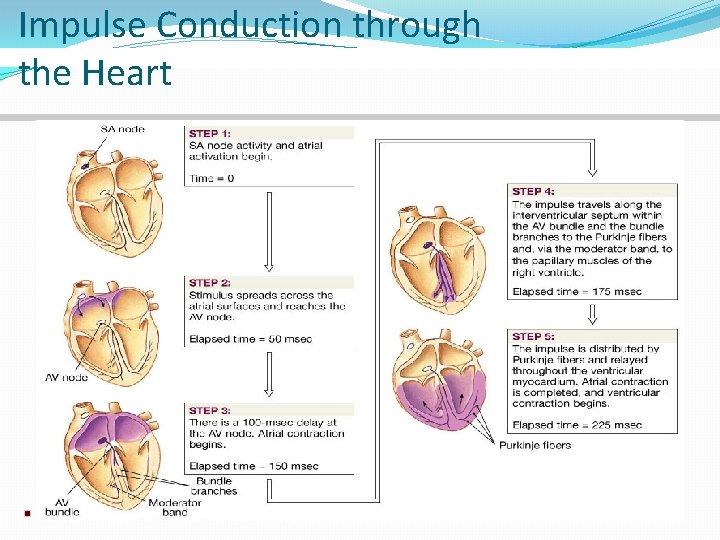
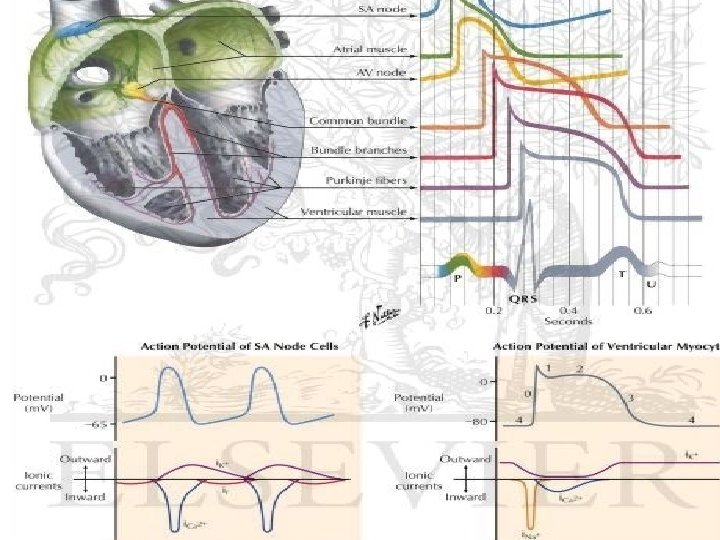
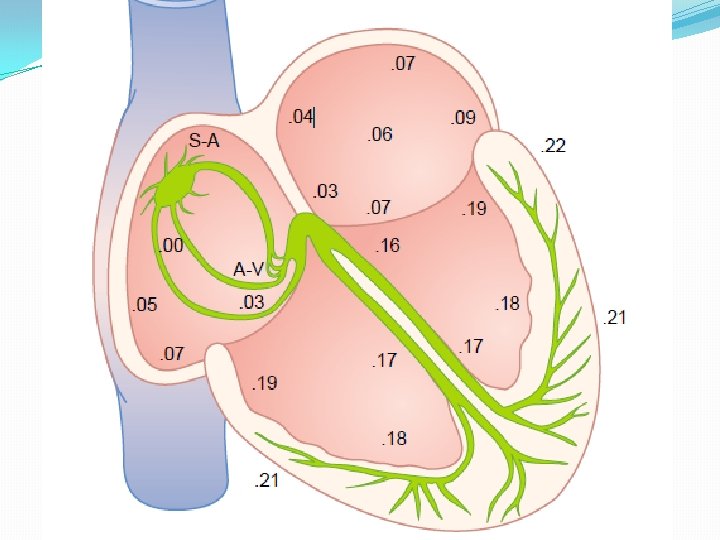
Conduction System of the Heart � SA node: sinoatrial node. The pacemaker. � Specialized cardiac muscle cells. � Generate spontaneous action potentials (autorhythmic tissue). � Action potentials pass to atrial muscle cells and to the AV node � AV node: atrioventricular node. � Action potentials conducted more slowly here than in any other part of system. � Ensures ventricles receive signal to contract after atria have contracted � AV bundle: passes through hole in cardiac skeleton to reach interventricular septum � Right and left bundle branches: extend beneath endocardium to apices of right and left ventricles � Purkinje fibers: � Large diameter cardiac muscle cells with few myofibrils. � Many gap junctions. � Conduct action potential to ventricular muscle cells (myocardium)
�Autorhythmic cells: �Initiate action potentials �Have unstable resting potentials called pacemaker potentials �Use calcium influx (rather than sodium) for rising phase of the action potential
Sequence of Excitation �Sinoatrial (SA) node generates impulses about 75 times/minute �Atrioventricular (AV) node delays the impulse approximately 0. 1 second �Impulse passes from atria to ventricles via the atrioventricular bundle (bundle of His) to the Purkinje fibers and finally to the myocardial fibers
Impulse Conduction through the Heart
Pacemaker and Action Potentials of the Heart
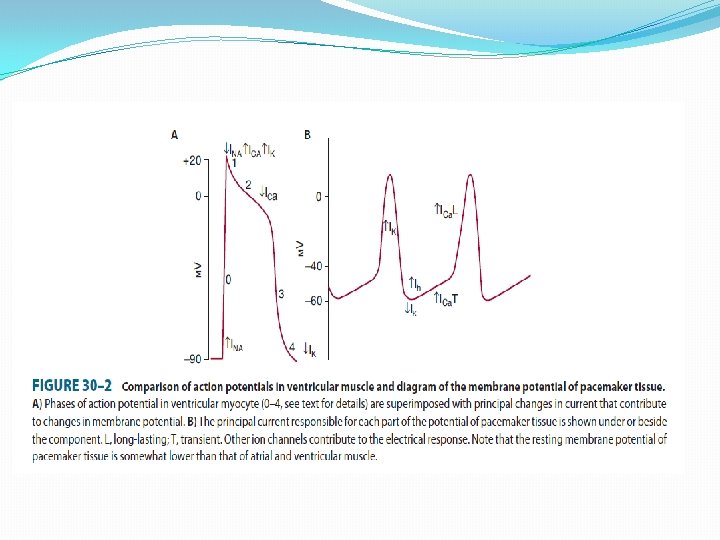
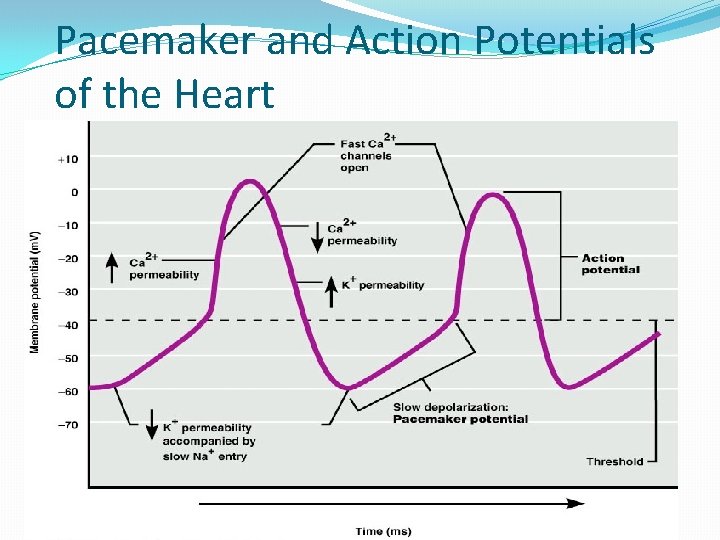
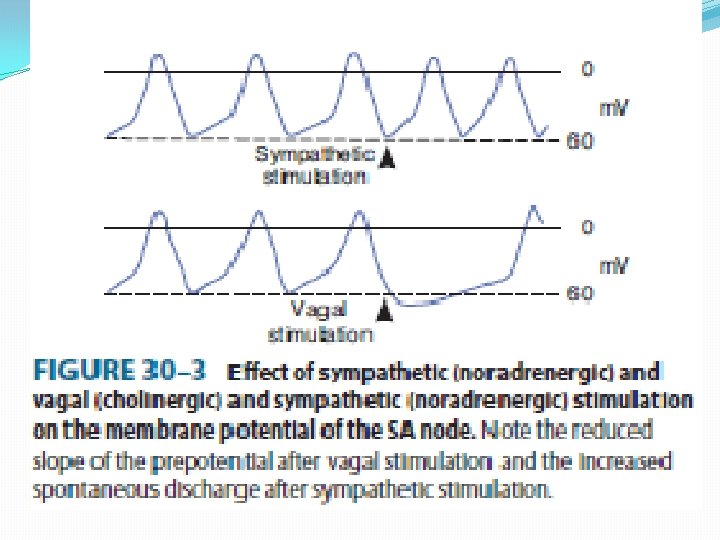
Pacemaker potentials �Rhythmically discharging cells have a membrane potential that, after each impulse, declines to the firing level. Thus, this Prepotential pacemaker potential triggers the next impulse �At the peak of each impulse, IK begins and brings about repolarization. IK then declines, and a channel that can pass both Na+ and K+ is activated. Because this channel is activated following hyperpolarization, it is referred to as an “h” channel; however, because of its unusual (funny) activation this has also been dubbed an “f” channel �As I h increases, the membrane begins to depolarize, forming the first part of the prepotential. Ca 2+ channels then open
�These are of two types in the heart, the T(for transient)channels and the L(for longlasting)channels. �The action potentials in the SA and AV nodes are largely due to Ca 2+ , with no contribution by Na+ influx. Consequently, there is no sharp, rapid depolarizing spike before the plateau, as there is in other parts of the conduction system and the atrial and ventricular fibers
�In addition, prepotentials are normally prominent only in the SA and AV nodes. However, “latent pacemakers” are present in other portions of the conduction system that can take over when the SA and AV nodes are depressed or conduction from them is blocked. Atrial and ventricular muscle fibers do not have prepotentials, and they discharge spontaneously only when injured or abnormal
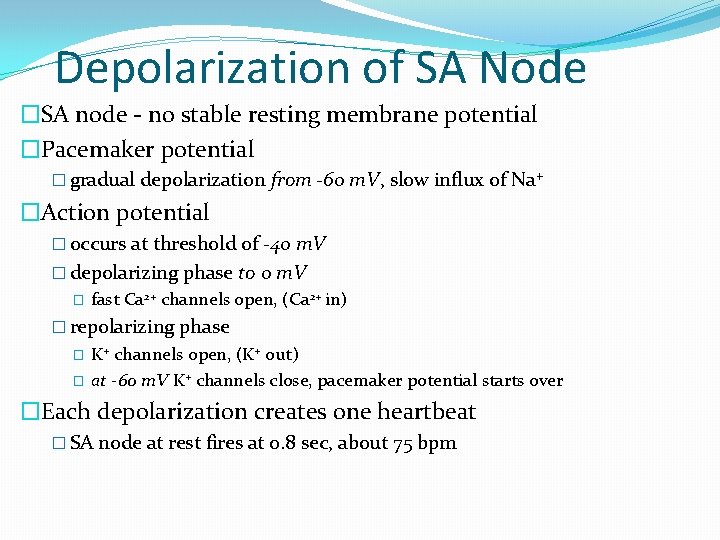
Depolarization of SA Node �SA node - no stable resting membrane potential �Pacemaker potential � gradual depolarization from -60 m. V, slow influx of Na+ �Action potential � occurs at threshold of -40 m. V � depolarizing phase to 0 m. V � fast Ca 2+ channels open, (Ca 2+ in) � repolarizing phase � � K+ channels open, (K+ out) at -60 m. V K+ channels close, pacemaker potential starts over �Each depolarization creates one heartbeat � SA node at rest fires at 0. 8 sec, about 75 bpm
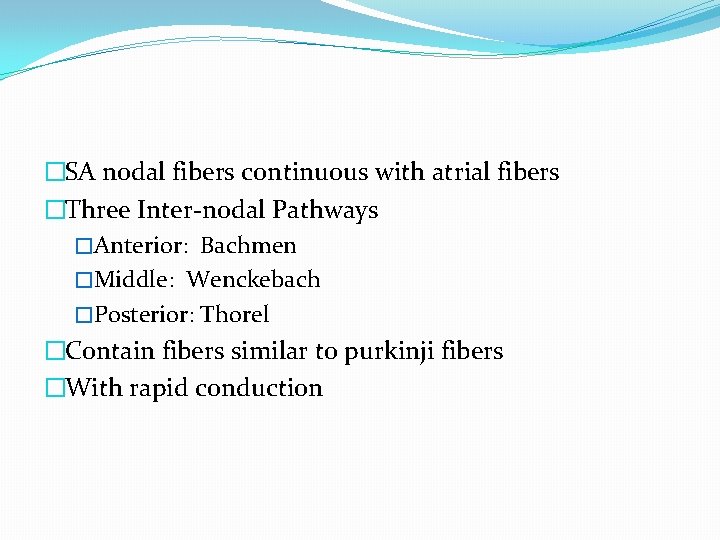
�SA nodal fibers continuous with atrial fibers �Three Inter-nodal Pathways �Anterior: Bachmen �Middle: Wenckebach �Posterior: Thorel �Contain fibers similar to purkinji fibers �With rapid conduction
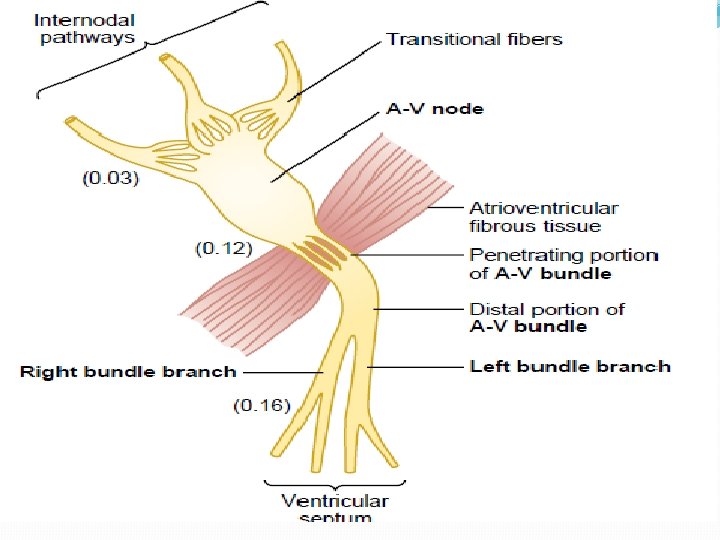
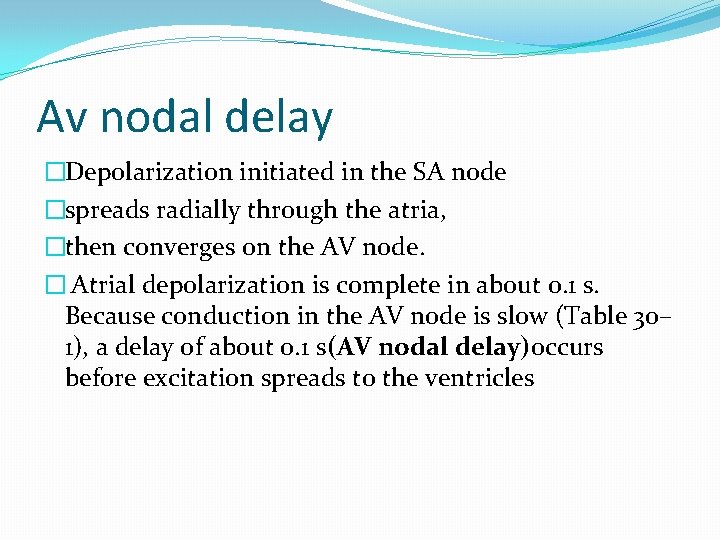
Av nodal delay �Depolarization initiated in the SA node �spreads radially through the atria, �then converges on the AV node. � Atrial depolarization is complete in about 0. 1 s. Because conduction in the AV node is slow (Table 30– 1), a delay of about 0. 1 s(AV nodal delay)occurs before excitation spreads to the ventricles
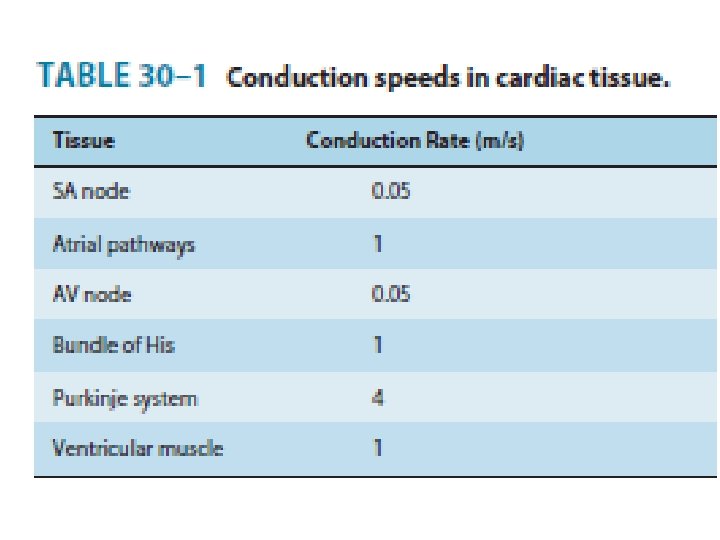
�The slow conduction in transitional nodal and penetrating A-V bundle fibers which is caused by lesser number of gap junctions between the cells in conducting pathways result in great resistance to conduction of excitatory ions from one fiber to next. �Rapid transmission in ventricular purkenji system at a velocity of 1. 5 – 4 m/s. �Rapid transmission in purkenji system is caused by high level of permeability of gap junction between the cells. �One way conduction through A-V bundle.
�The A-V bundle passes downward in ventricular septum from 5 -15 mm dividing into left and right bundle branches. �Left bundle branch gives of anterior fascicle and posterior fascicle �Purkenji fibers penetrate the ventricular muscle �Velocity of transmission in ventricular m uscle 0. 3 - 0. 5 m/s.
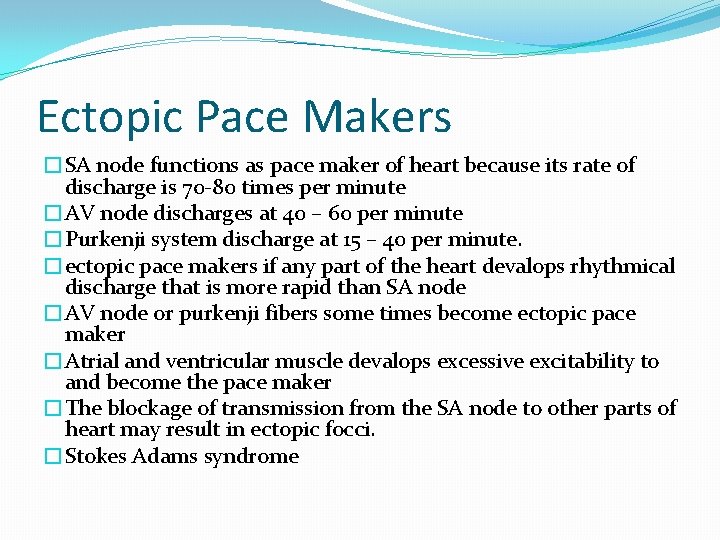
Ectopic Pace Makers �SA node functions as pace maker of heart because its rate of discharge is 70 -80 times per minute �AV node discharges at 40 – 60 per minute �Purkenji system discharge at 15 – 40 per minute. �ectopic pace makers if any part of the heart devalops rhythmical discharge that is more rapid than SA node �AV node or purkenji fibers some times become ectopic pace maker �Atrial and ventricular muscle devalops excessive excitability to and become the pace maker �The blockage of transmission from the SA node to other parts of heart may result in ectopic focci. �Stokes Adams syndrome
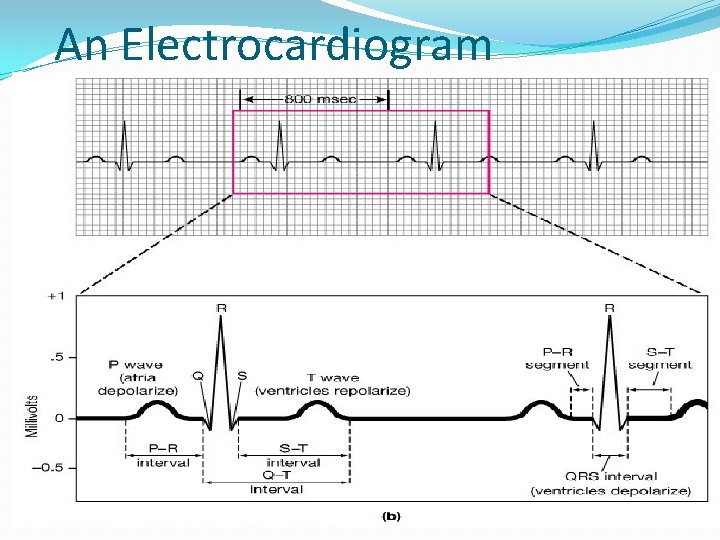
An Electrocardiogram
- Slides: 28