Concussions A Regions Playbook William Lewis MD Brittany
Concussions: A Region’s Playbook William Lewis, MD, Brittany Gusic, MD (PGY-2), Yusuf Khan, MD, Ryan Miller (MS-4) WVU Department of Family Medicine – Eastern Division FMEC 11/2/13
West Virginia's Eastern Panhandle O 15 – High Schools O 8 – counties O 1 – West Virginia Area Health Education Center (WV AHEC) O 1 – Division of WVU School of Medicine O 1 – Family Medicine Residency (Harpers Ferry Rural Family Medicine Residency)
Project Im. PACT O Started 2008 to provide concussion testing in the eastern panhandle O Supported by our regional AHEC group O 10 High Schools now participating
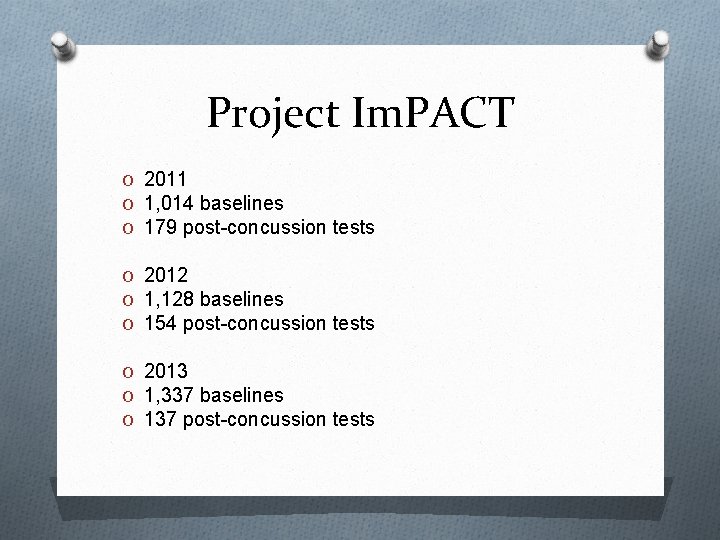
Project Im. PACT O 2011 O 1, 014 baselines O 179 post-concussion tests O 2012 O 1, 128 baselines O 154 post-concussion tests O 2013 O 1, 337 baselines O 137 post-concussion tests
Im. PACT testing O Piece of the overall concussion evaluation and management process O Neurocognitive tests O Symptom monitoring O Extensively researched O Used to track recovery following concussion O Not a tool for diagnose concussion or a substitution for medical evaluation
Symptom monitoring O Most recent concussion date O Hours slept last night O Current medications O Rate the current severity of 22 concussion symptoms on a 7 -point Likert scale
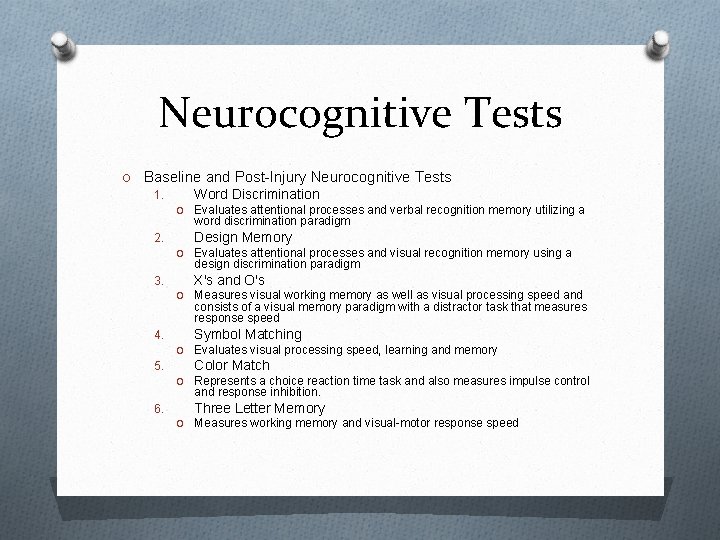
Neurocognitive Tests O Baseline and Post-Injury Neurocognitive Tests 1. Word Discrimination O Evaluates attentional processes and verbal recognition memory utilizing a word discrimination paradigm 2. Design Memory O Evaluates attentional processes and visual recognition memory using a design discrimination paradigm 3. X's and O's O Measures visual working memory as well as visual processing speed and consists of a visual memory paradigm with a distractor task that measures response speed 4. Symbol Matching O Evaluates visual processing speed, learning and memory 5. Color Match O Represents a choice reaction time task and also measures impulse control and response inhibition. 6. Three Letter Memory O Measures working memory and visual-motor response speed
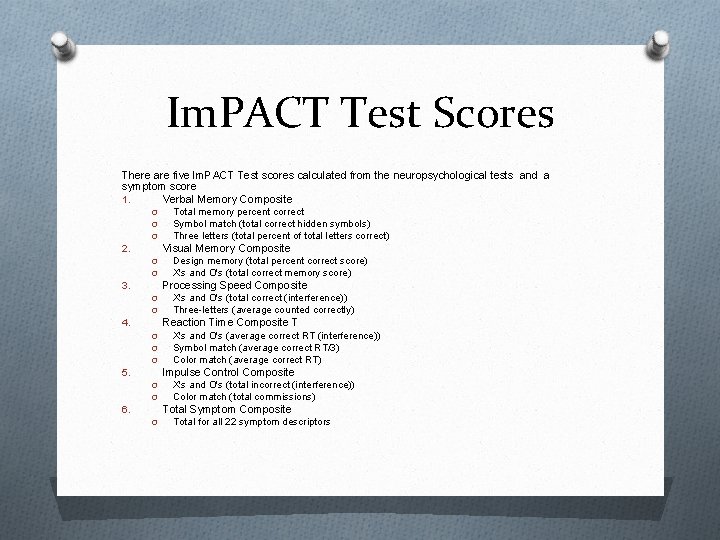
Im. PACT Test Scores There are five Im. PACT Test scores calculated from the neuropsychological tests and a symptom score 1. Verbal Memory Composite O O O Total memory percent correct Symbol match (total correct hidden symbols) Three letters (total percent of total letters correct) Visual Memory Composite 2. O O Design memory (total percent correct score) X's and O's (total correct memory score) Processing Speed Composite 3. O O X's and O's (total correct (interference)) Three-letters (average counted correctly) Reaction Time Composite T 4. O O O X's and O's (average correct RT (interference)) Symbol match (average correct RT/3) Color match (average correct RT) Impulse Control Composite 5. O O X's and O's (total incorrect (interference)) Color match (total commissions) Total Symptom Composite 6. O Total for all 22 symptom descriptors
Our testing program O Athletic trainers with support of AHEC conduct baseline testing O All contact sports athletes can receive baseline test O Usually repeat baseline every 2 years
Our testing program O Athletes with clinical concussion receive post injury test O Results sent to an Im. PACT trained provider for interpretation O Can access results through web or app O Results can also be placed into PDF to be emailed
Our testing program O First positive test repeat 1 week O Second positive recommend seeing physician O Trainer will notify teachers to adjust class work O Can not return to participation until Im. PACT back to baseline AND symptom free for 1 week
Our data from 5 years of testing
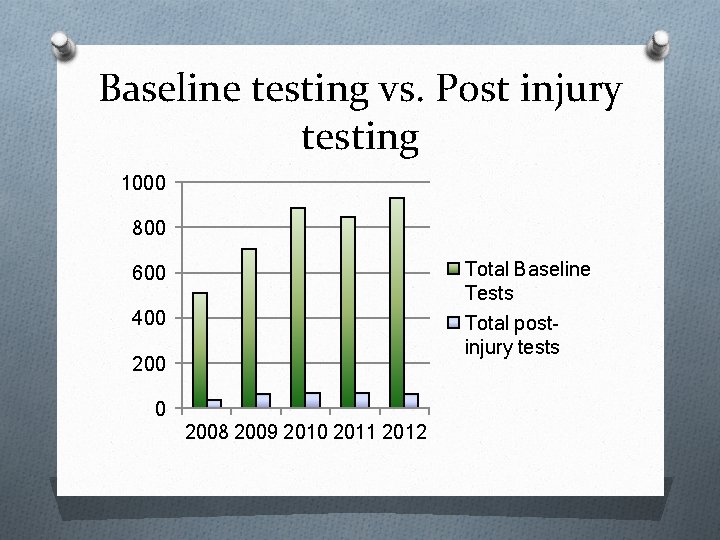
Baseline testing vs. Post injury testing 1000 800 Total Baseline Tests Total postinjury tests 600 400 2008 2009 2010 2011 2012
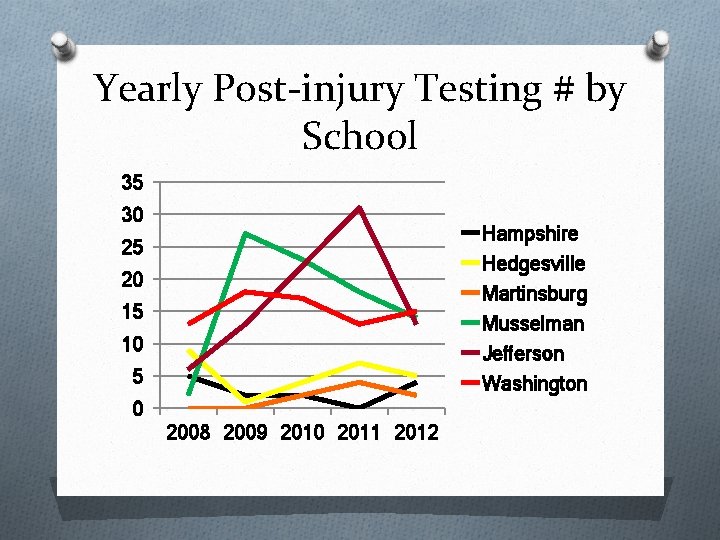
Yearly Post-injury Testing # by School 35 30 Hampshire Hedgesville Martinsburg Musselman Jefferson Washington 25 20 15 10 5 0 2008 2009 2010 2011 2012
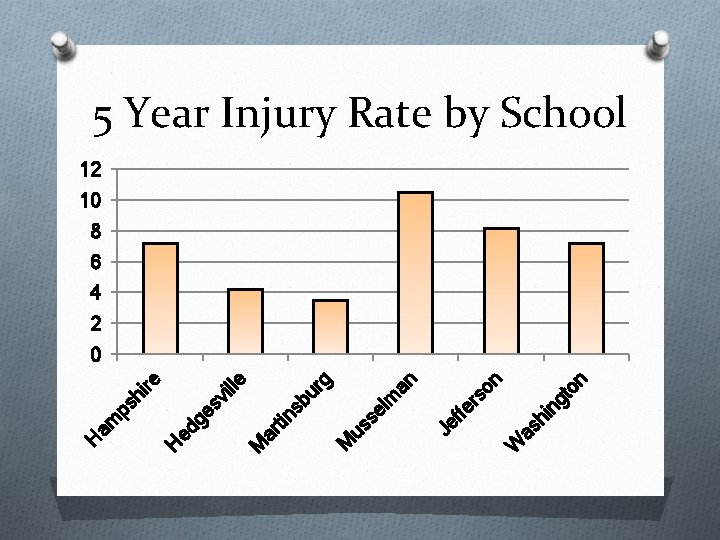
n in gt o as h W n so fe r Je f an el m us s ns bu rg ar ti M M vi lle ire ps h ed ge s H am H 5 Year Injury Rate by School 12 10 8 6 4 2 0
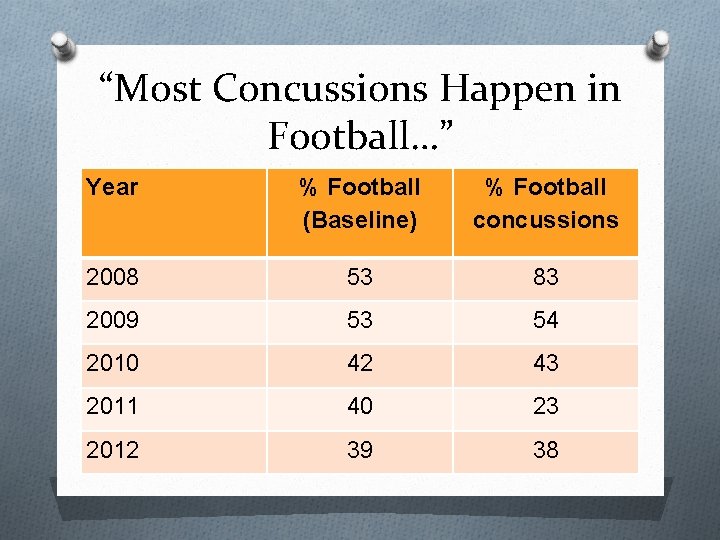
“Most Concussions Happen in Football…” Year % Football (Baseline) % Football concussions 2008 53 83 2009 53 54 2010 42 43 2011 40 23 2012 39 38

Trends in the data
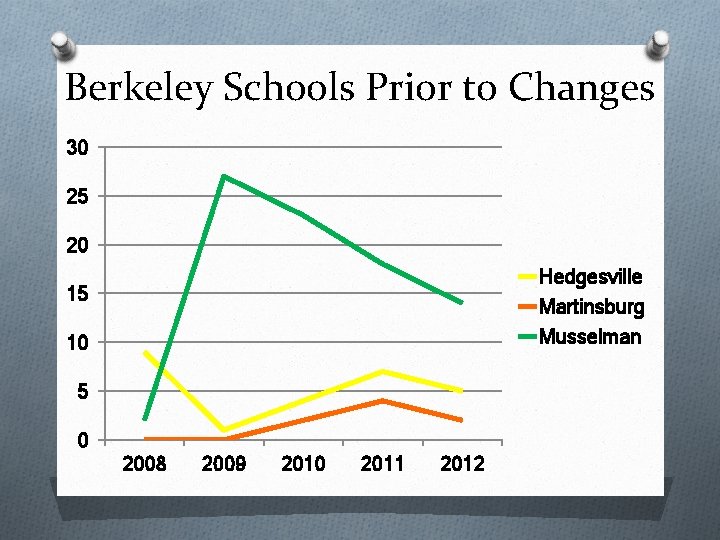
Berkeley Schools Prior to Changes 30 25 20 Hedgesville Martinsburg Musselman 15 10 5 0 2008 2009 2010 2011 2012
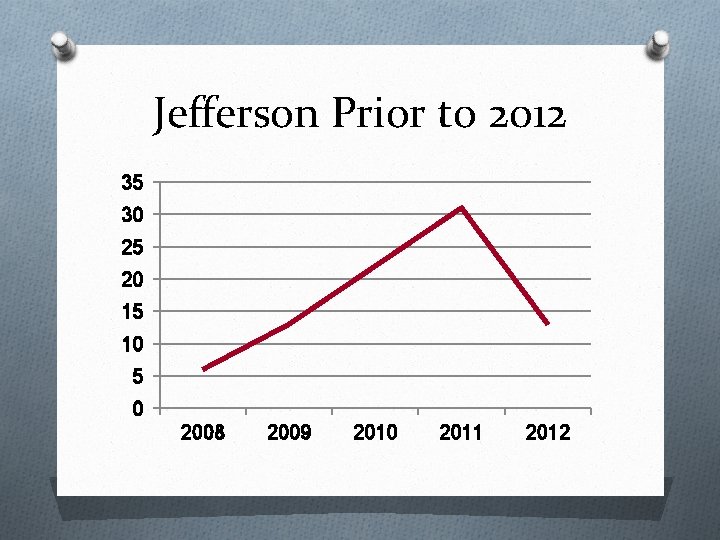
Jefferson Prior to 2012 35 30 25 20 15 10 5 0 2008 2009 2010 2011 2012
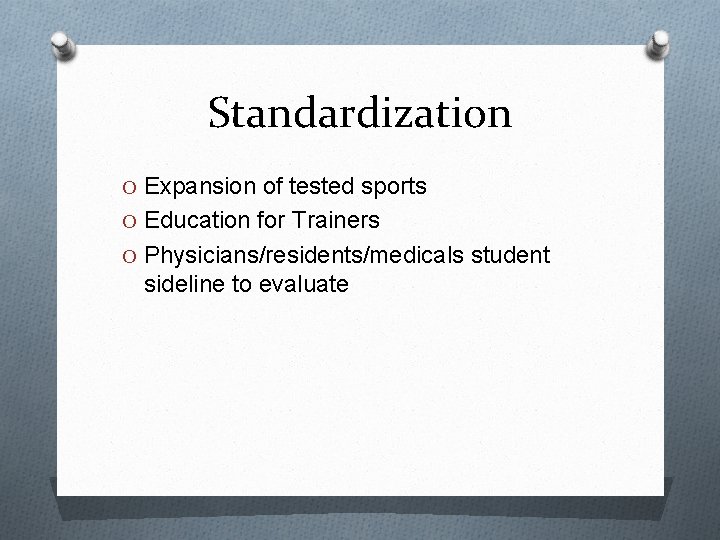
Standardization O Expansion of tested sports O Education for Trainers O Physicians/residents/medicals student sideline to evaluate
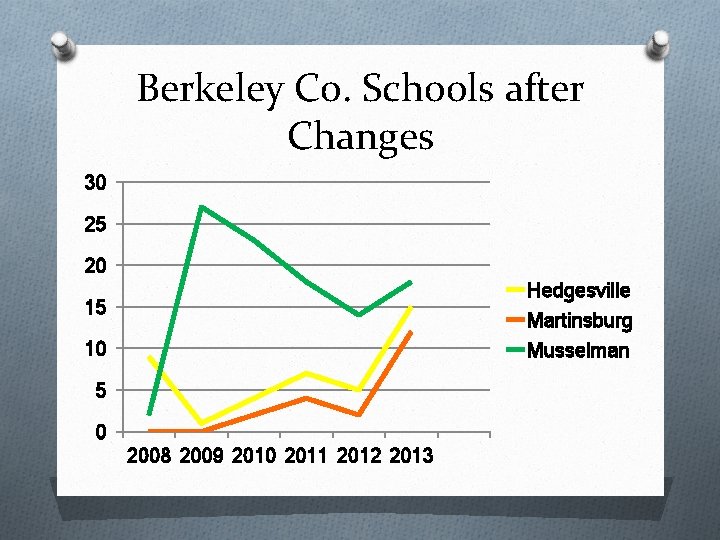
Berkeley Co. Schools after Changes 30 25 20 Hedgesville Martinsburg Musselman 15 10 5 0 2008 2009 2010 2011 2012 2013
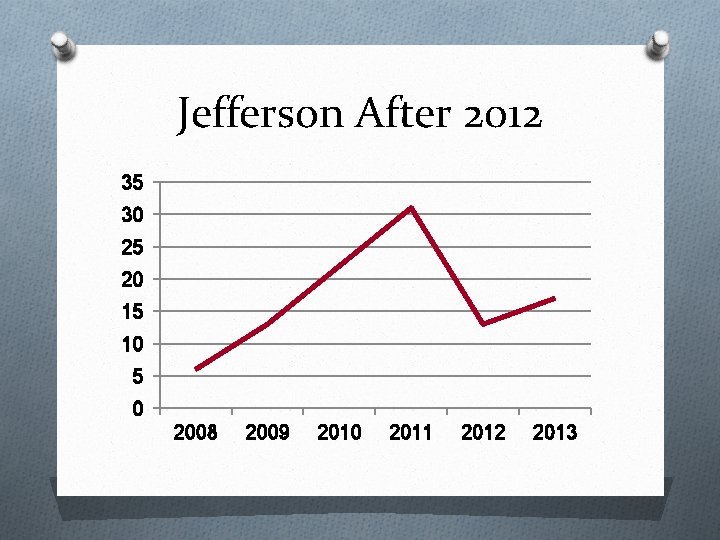
Jefferson After 2012 35 30 25 20 15 10 5 0 2008 2009 2010 2011 2012 2013
WV Return to Play O “An athlete removed from a contest that shows signs/symptoms of a concussion shall be immediately evaluated by an appropriate health care professional. If no appropriate health care professional is available, the athlete shall not be allowed to RTP. ” O “…if it is determined the athlete has suffered a concussion, the athlete shall not be permitted to RTP the same day as the concussion. ”
WV RTP O “RTP shall be delayed until athlete is asymptomatic and has undergone a progression of tests to determine if they are able to RTP. ” O O O No activity Light aerobic activity Sport specific exercise Non-contact training drills Full participation practice RTP O If symptoms occur during progression, drop back to previous level after a 24 hour rest period.
What to do on the sideline
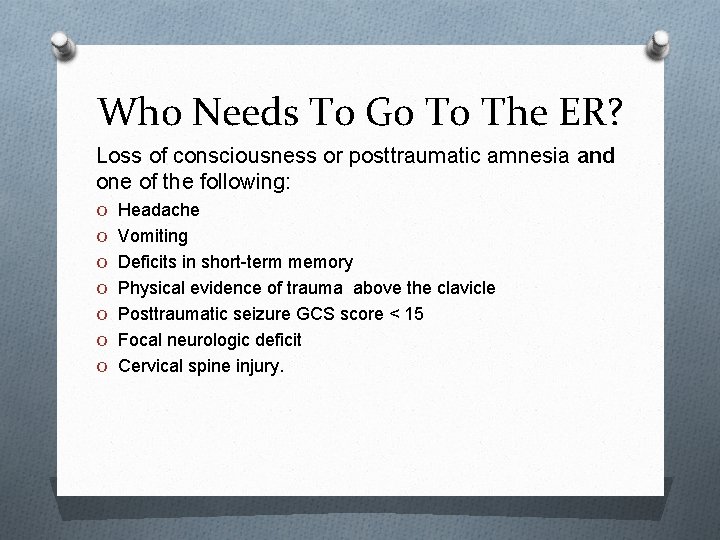
Who Needs To Go To The ER? Loss of consciousness or posttraumatic amnesia and one of the following: O Headache O Vomiting O Deficits in short-term memory O Physical evidence of trauma above the clavicle O Posttraumatic seizure GCS score < 15 O Focal neurologic deficit O Cervical spine injury.
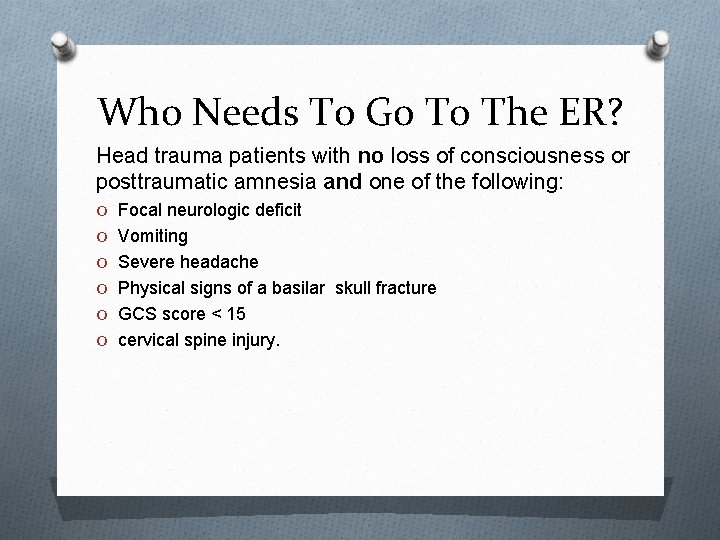
Who Needs To Go To The ER? Head trauma patients with no loss of consciousness or posttraumatic amnesia and one of the following: O Focal neurologic deficit O Vomiting O Severe headache O Physical signs of a basilar skull fracture O GCS score < 15 O cervical spine injury.
Sideline Tools: An Overview OSubtle changes ONo treatment or rehab ONumerous assessment tools OCombination of tools OBaseline measurements
Symptom Checklists O Most commonly used O Cost effective O Self-reporting O Symptom reporting can become complicated.
Neuropsychological Tests O Subtle Cognitive Deficits O Written vs Computer Based O Tests are not yet validated; data O Under age 12 – Still being developed O Balance Error Scoring System (BESS) O Im. PACT – Sway test with Iphone application.
BESS Score Card O FIRM Surface O FOAM Surface O Balance Error Scoring System – Types of Errors – Out of Position O 1. Hands lifted off iliac crest O 2. Opening eyes O 3. Step, stumble, or fall O 4. Moving hip into > 30 degrees abduction O 5. Lifting forefoot or heel O 6. Remaining out of test position >5 sec O The BESS is calculated by adding one error point for each error during the 6 20 -second tests.
Sideline Assessment Tools OMaddocks Questions OStandardized Assessment of Concussion (SAC) OSport Concussion Assessment Tool (SCAT) O(SCAT 2) O(SCAT 3), (Child-SCAT 3)
CDC Guidelines For Return To Play O Athletes should not return to play the same day of injury. O Under the supervision of a healthcare provider O Stepwise symptom-limited program with stages of progression: 1. 2. 3. 4. 5. 6. Rest until asymptomatic (physical and mental rest) Light aerobic exercise (e. g. , stationary cycle) Sport-specific exercise Non-contact training drills (light resistance) Full contract training after medical clearance Return to competition
Bibliography O Sports Health. 2011 May; 3(3): 287– 295. doi: 10. 1177/1941738111403122 PMCID: PMC 3445164 O O Systematic Review of the Balance Error Scoring System David R. Bell, Ph. D, ATC, * Kevin M. Guskiewicz, Ph. D, ATC, † Micheal A. Clark, DPT, MS, PES, CES, § and Darin A. Padua, Ph. D, ATC†‡ O http: //www. momsteam. com/health-safety/sports-concussion-safety/concussion-recognitionevaluation/maddocks-questions-test-concussion#ixzz 2 j 8 hu. VXDK O Scorza, Keith, MD, MBA, Raleigh, Meghan F. , MD, O’Connor, Francis G. , MD, MPH, Current Concepts in Concussion: Evaluation and Management, Am Fam Physician, 2012 Jan 15; 85(2): 123132 O Mc. Crory, P. , Meeuwisse, W. , Johnston, K. , Dvorak, J, Aubry, M. , Molloy, M. , Cantu, R, Consensu Statement on Concussion in Sport: the 3 rd International Conference on Concussion in Sport held O in Zurich, November 2008, Br J Sports Med 2009; 43 (Suppl 1): i 76 -i 84 www. cdc. gov O www. impact. com accessed 10/30/13 O www. stockton. com accessed 10/30/13
- Slides: 34