Concussion Management in Pediatric Patients Amanda Jones MSN







- Slides: 43
Concussion Management in Pediatric Patients Amanda Jones, MSN, RN, CPNP-PC Blue Bird Circle Clinic for Pediatric Neurology Texas Children’s Hospital Baylor College of Medicine
Objectives • Define concussion and identify common symptoms • Understand appropriate evaluation of patients with suspected concussion • Management of concussion symptoms and comorbidities • Determine when to refer to Neurology and other specialties
How many of you know someone who has experienced a concussion at some point in their life?

Concussion Statistics • It is estimated that between 1. 6 and 3. 6 million people are affected by concussion annually • 80 -90% of athletes will rec 0 ver within 7 -10 days (Mc. Crory 2005) CDC, Mc. Crory
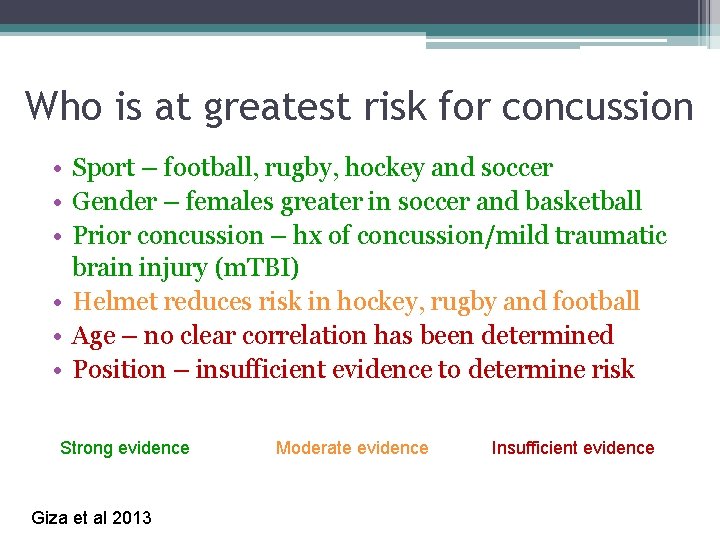
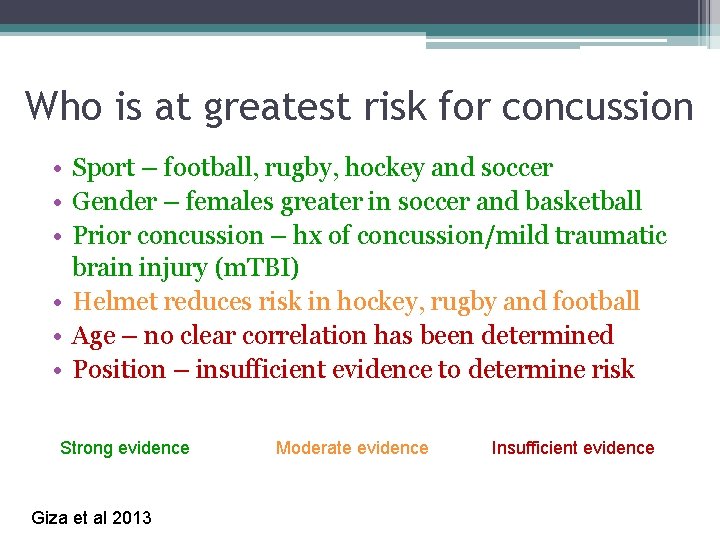
Who is at greatest risk for concussion • Sport – football, rugby, hockey and soccer • Gender – females greater in soccer and basketball • Prior concussion – hx of concussion/mild traumatic brain injury (m. TBI) • Helmet reduces risk in hockey, rugby and football • Age – no clear correlation has been determined • Position – insufficient evidence to determine risk Strong evidence Giza et al 2013 Moderate evidence Insufficient evidence
WHAT IS A CONCUSSION?
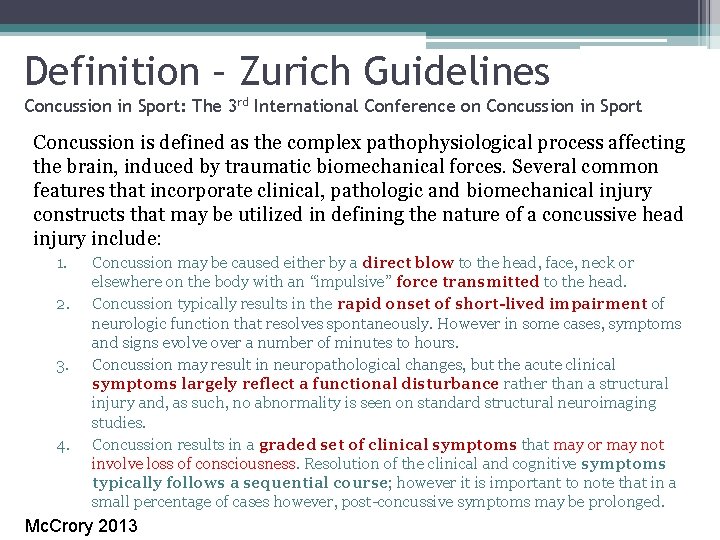
Definition – Zurich Guidelines Concussion in Sport: The 3 rd International Conference on Concussion in Sport Concussion is defined as the complex pathophysiological process affecting the brain, induced by traumatic biomechanical forces. Several common features that incorporate clinical, pathologic and biomechanical injury constructs that may be utilized in defining the nature of a concussive head injury include: 1. 2. 3. 4. Concussion may be caused either by a direct blow to the head, face, neck or elsewhere on the body with an “impulsive” force transmitted to the head. Concussion typically results in the rapid onset of short-lived impairment of neurologic function that resolves spontaneously. However in some cases, symptoms and signs evolve over a number of minutes to hours. Concussion may result in neuropathological changes, but the acute clinical symptoms largely reflect a functional disturbance rather than a structural injury and, as such, no abnormality is seen on standard structural neuroimaging studies. Concussion results in a graded set of clinical symptoms that may or may not involve loss of consciousness. Resolution of the clinical and cognitive symptoms typically follows a sequential course; however it is important to note that in a small percentage of cases however, post-concussive symptoms may be prolonged. Mc. Crory 2013
Definition – American Medical Society for Sports Medicine A concussion is defined as a traumatically induced transient disturbance of brain function and is caused by a complex pathophysiological process. Concussions have also been referred to as mild traumatic brain injuries (MTBI). While all concussions are MTBIs, not all MTBIs are concussion. Concussions are a subset of MTBIs, on the less-severe end of the brain injury spectrum and are generally self-limiting in duration and resolution. Harmon 2012
Definition – American Academy of Neurology A clinical syndrome of biomechanically induced alteration of brain function, typically affecting memory and orientation, which may involve loss of consciousness (LOC).

Evaluation of Concussion
Approach to Child with Suspected Concussion 1. Emergency management of the athlete with caution of cervical spine 2. Following first aid, use assessment tool for evaluation of severity of concussion 3. Thorough H&P in Emergency Center or in office (PCP or Sport’s Medicine)

“The diagnosis of sports-related concussion (SRC) is a clinical diagnosis based on salient features from the history and examination…no single test score can be the basis of a concussion diagnosis” AAN 2013
Checklists/Screening Tools ▫ ▫ ▫ Post Concussion Symptom Scale Graded Symptom Checklist (GSC) Standardized Assessment of Concussion (SAC) Balance Error Scoring System (BESS) Sport Concussion Assessment Tool 3 (SCAT 3)
Additional Screening Tools • • • Military Acute Concussion Evaluation King-Devick Test Clinical Reaction Time Test Sensory Organization Test Acute Concussion Evaluation – CDC Concussion Symptom Inventory Health and Behavior Inventory Rivermead Post-Concussion Symptoms Questionnaire Several Computerized Testing programs – Im. PACT (Immediate Post-Concussion Assessment and Cognitive Testing)
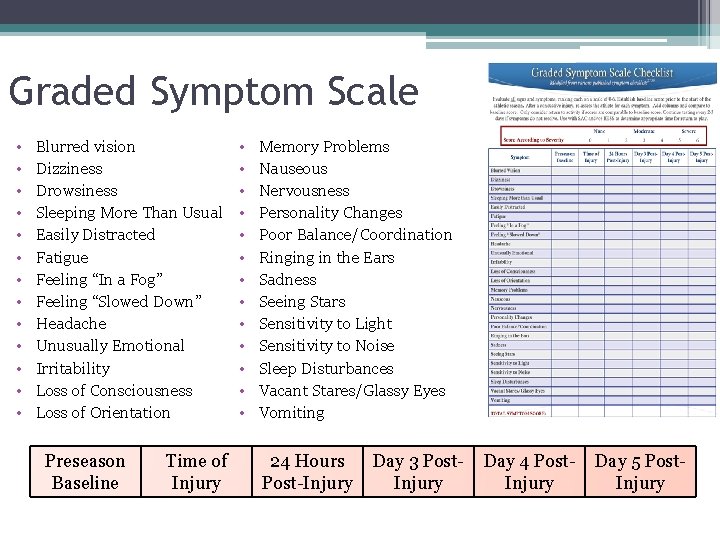
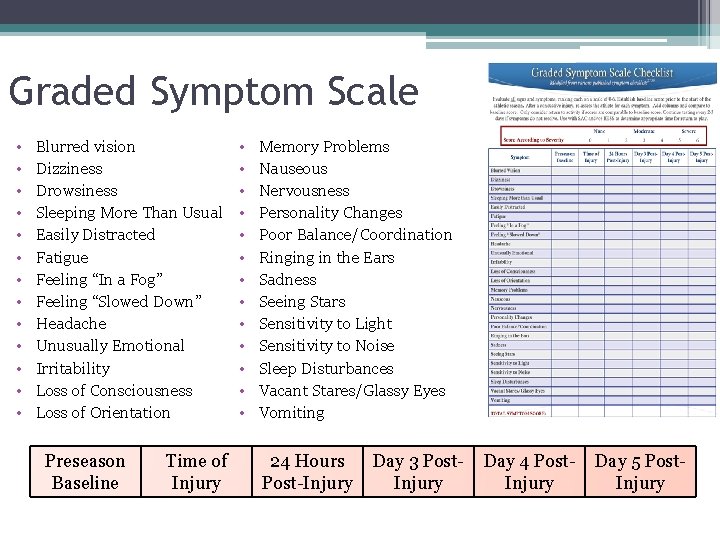
Graded Symptom Scale • • • • Blurred vision Dizziness Drowsiness Sleeping More Than Usual Easily Distracted Fatigue Feeling “In a Fog” Feeling “Slowed Down” Headache Unusually Emotional Irritability Loss of Consciousness Loss of Orientation Preseason Baseline Time of Injury • • • • Memory Problems Nauseous Nervousness Personality Changes Poor Balance/Coordination Ringing in the Ears Sadness Seeing Stars Sensitivity to Light Sensitivity to Noise Sleep Disturbances Vacant Stares/Glassy Eyes Vomiting 24 Hours Post-Injury Day 3 Post. Injury Day 4 Post. Injury Day 5 Post. Injury
Standardized Assessment of Concussion (SAC) Evaluation of SIX key areas 1. Orientation 4. Concentration 2. Immediate Memory 5. Exertional Maneuvers 3. Neurological Screening 6. Delayed Memory Recall Recollection of injury Sensation Coordination Strength
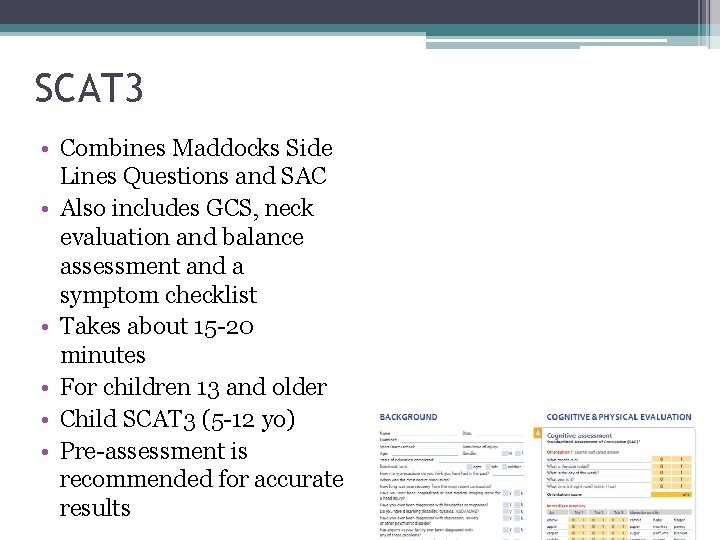
SCAT 3 • Combines Maddocks Side Lines Questions and SAC • Also includes GCS, neck evaluation and balance assessment and a symptom checklist • Takes about 15 -20 minutes • For children 13 and older • Child SCAT 3 (5 -12 yo) • Pre-assessment is recommended for accurate results
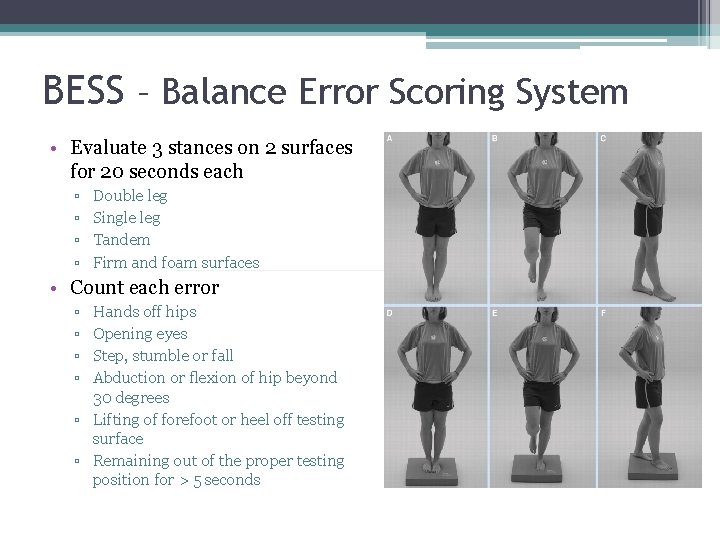
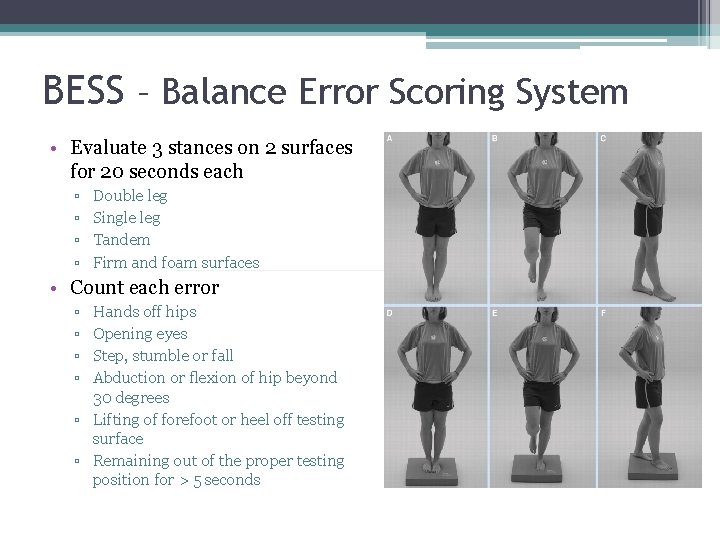
BESS – Balance Error Scoring System • Evaluate 3 stances on 2 surfaces for 20 seconds each ▫ ▫ Double leg Single leg Tandem Firm and foam surfaces • Count each error ▫ ▫ Hands off hips Opening eyes Step, stumble or fall Abduction or flexion of hip beyond 30 degrees ▫ Lifting of forefoot or heel off testing surface ▫ Remaining out of the proper testing position for > 5 seconds
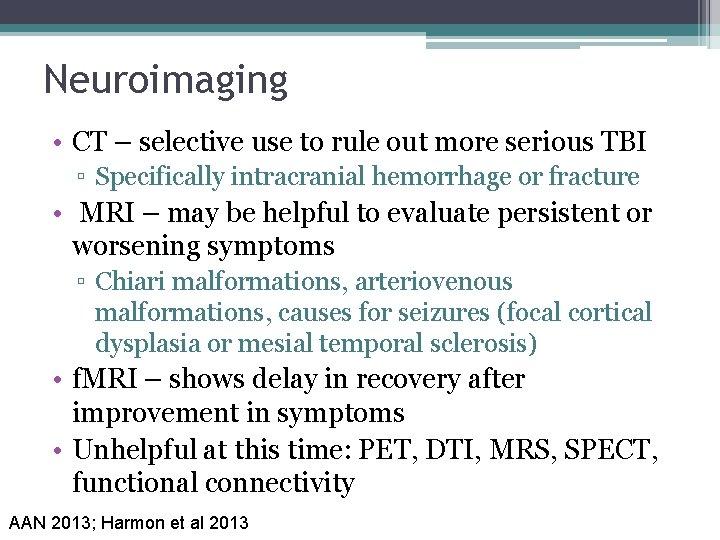
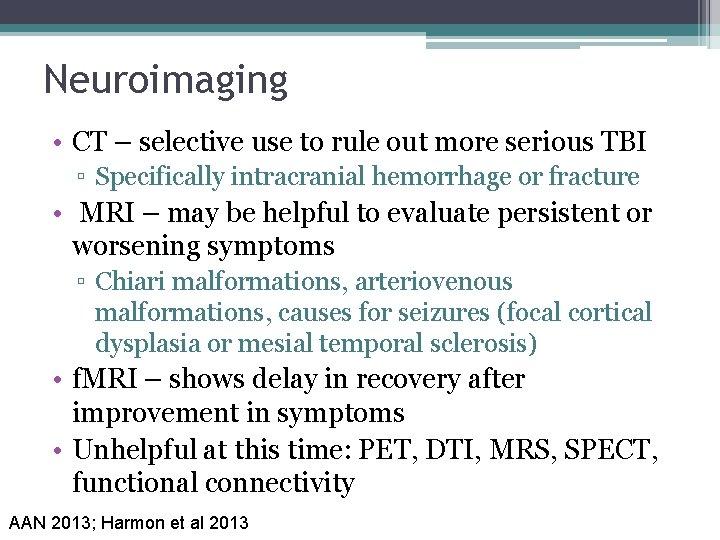
Neuroimaging • CT – selective use to rule out more serious TBI ▫ Specifically intracranial hemorrhage or fracture • MRI – may be helpful to evaluate persistent or worsening symptoms ▫ Chiari malformations, arteriovenous malformations, causes for seizures (focal cortical dysplasia or mesial temporal sclerosis) • f. MRI – shows delay in recovery after improvement in symptoms • Unhelpful at this time: PET, DTI, MRS, SPECT, functional connectivity AAN 2013; Harmon et al 2013
Symptoms of Concussion

Suspect concussion if 1 or more of the following are present: • • • Symptoms – somatic, cognitive and/or emotional Physical signs Behavioral changes Cognitive impairment Sleep disturbances Mc. Crory 2013

Common Symptoms Associated with Concussion • • • • Blurred vision Dizziness Drowsiness Sleeping More Than Usual Easily Distracted Fatigue Feeling “In a Fog” Feeling “Slowed Down” Headache Unusually Emotional Irritability Loss of Consciousness Loss of Orientation • • • • Memory Problems Nauseous Nervousness Personality Changes Poor Balance/Coordination Ringing in the Ears Sadness Seeing Stars Sensitivity to Light Sensitivity to Noise Sleep Disturbances Vacant Stares/Glassy Eyes Vomiting
Management of Concussion Returning to Activities
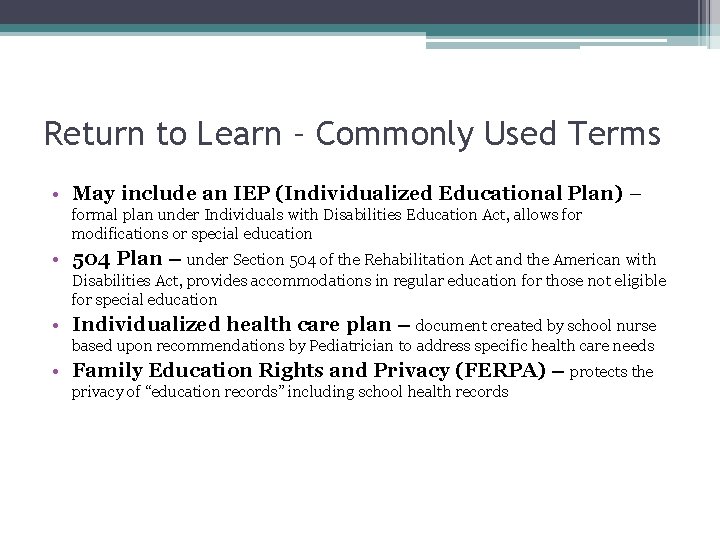
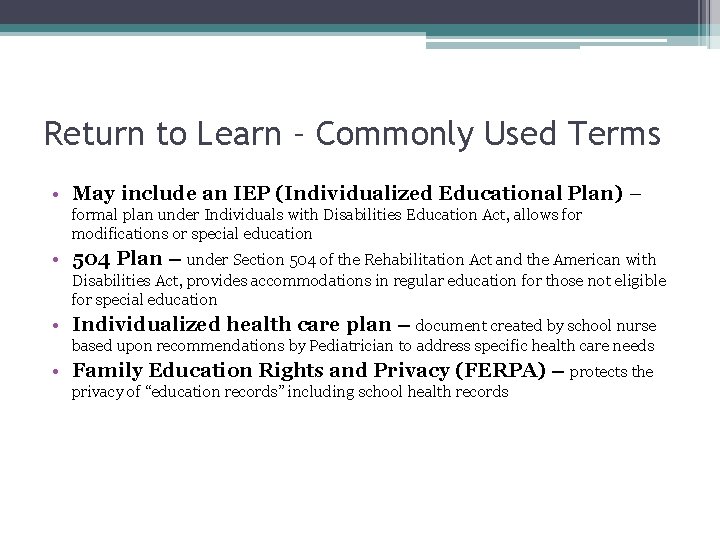
Return to Learn – Commonly Used Terms • May include an IEP (Individualized Educational Plan) – formal plan under Individuals with Disabilities Education Act, allows for modifications or special education • 504 Plan – under Section 504 of the Rehabilitation Act and the American with Disabilities Act, provides accommodations in regular education for those not eligible for special education • Individualized health care plan – document created by school nurse based upon recommendations by Pediatrician to address specific health care needs • Family Education Rights and Privacy (FERPA) – protects the privacy of “education records” including school health records
Return to Learn • *INDIVIDUALIZED*
Practice Recommendations • Pre-participation Counseling • Return to Play (RTP) ▫ No same day return to play EVER • Retirement from Play
Return to Play • 4 th International Conference on Concussion in Sport (Nov. 2012) – graduated protocol • American Medical Society for Sports Medicine position statement: concussion in sport – confers with graduated protocol • CDC also endorses a 5 step return to play protocol • American Academy of Neurology – recommends no return to play until asymptomatic off medications which could mask s/s of concussion; it may be beneficial to use graduated approach to return to play

Retirement from Play • Overall poor consensus on this topic • 4 th International Conference on Concussion provides no guidance • AAN – athletes with multiple concussion should have neurological/neuropsychological evaluation which can provide guidance on recommendations for retirement; counsel on the risk for permanent neurobehavioral or cognitive impairments in athletes with a history of multiple concussions or persistent neurobehavioral impairments
Management of Concussion Treating the Symptoms
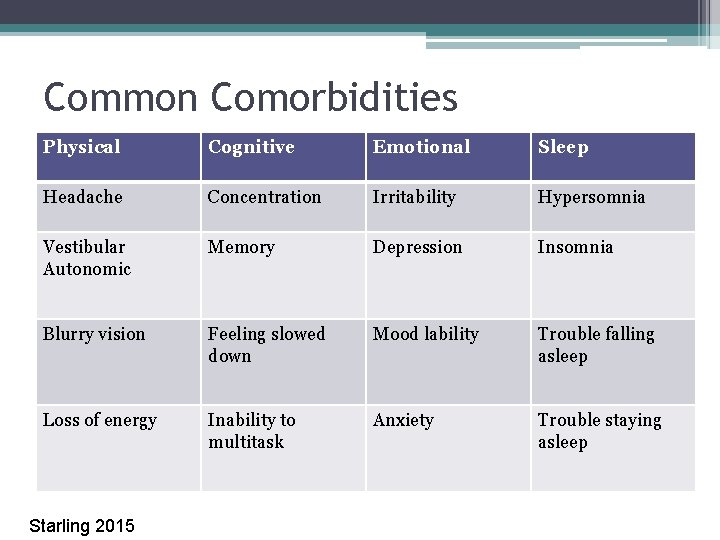
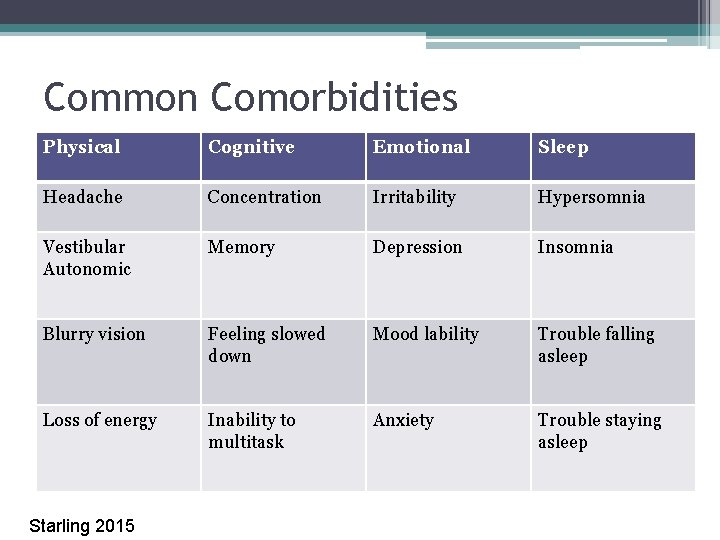
Common Comorbidities Physical Cognitive Emotional Sleep Headache Concentration Irritability Hypersomnia Vestibular Autonomic Memory Depression Insomnia Blurry vision Feeling slowed down Mood lability Trouble falling asleep Loss of energy Inability to multitask Anxiety Trouble staying asleep Starling 2015
Multidisciplinary Approach • Sports Medicine Clinic • Physical Therapy • Occasionally, Neurology or Neuropsychology for persistent symptoms
Supplements/Medications • Sleep – melatonin • Anxiety - anxiolytics
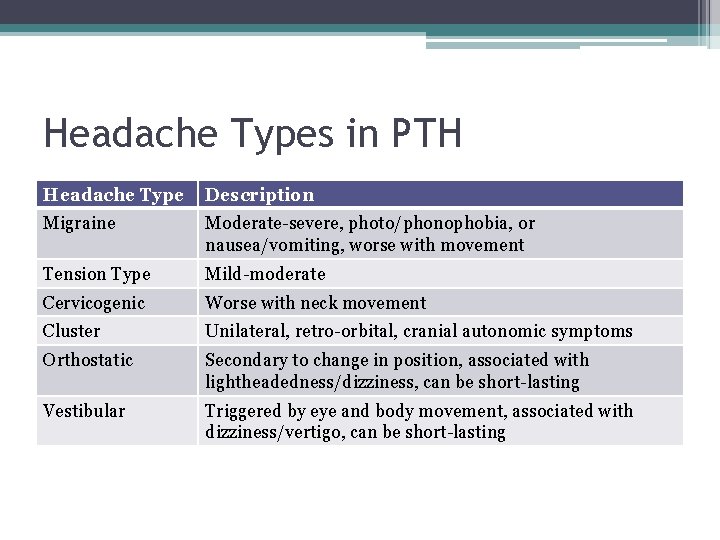
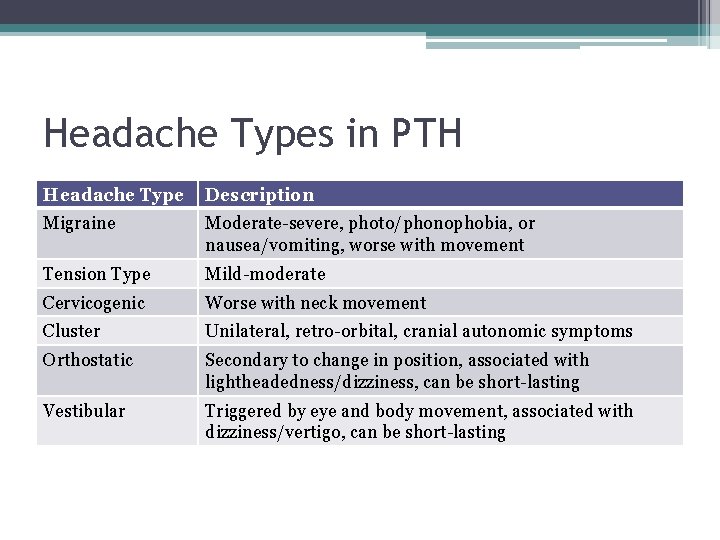
Headache Types in PTH Headache Type Description Migraine Moderate-severe, photo/phonophobia, or nausea/vomiting, worse with movement Tension Type Mild-moderate Cervicogenic Worse with neck movement Cluster Unilateral, retro-orbital, cranial autonomic symptoms Orthostatic Secondary to change in position, associated with lightheadedness/dizziness, can be short-lasting Vestibular Triggered by eye and body movement, associated with dizziness/vertigo, can be short-lasting
Treatment of headache • Topamax “dopamax” • Amitriptyline • Beta blockers
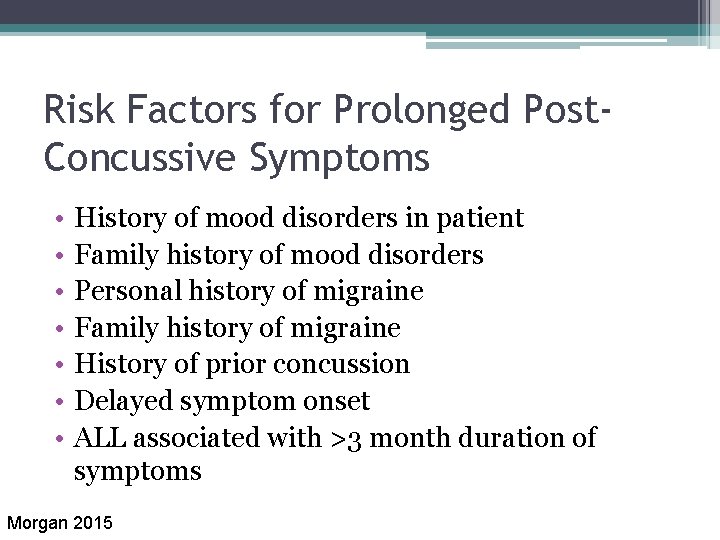
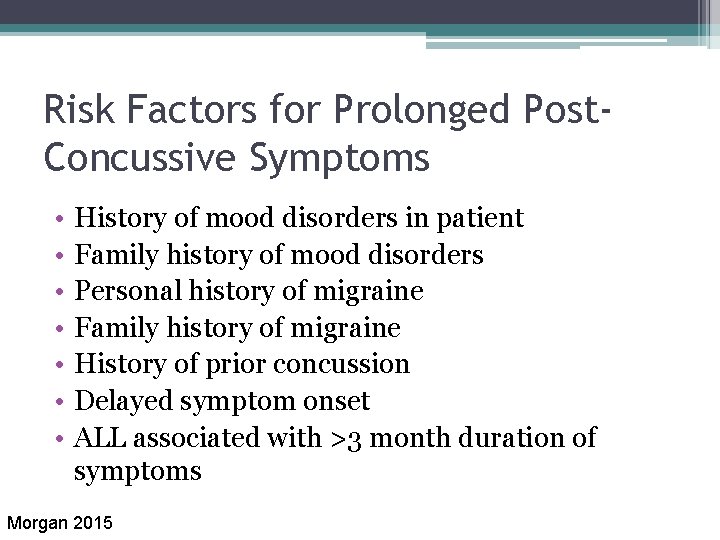
Risk Factors for Prolonged Post. Concussive Symptoms • • History of mood disorders in patient Family history of mood disorders Personal history of migraine Family history of migraine History of prior concussion Delayed symptom onset ALL associated with >3 month duration of symptoms Morgan 2015
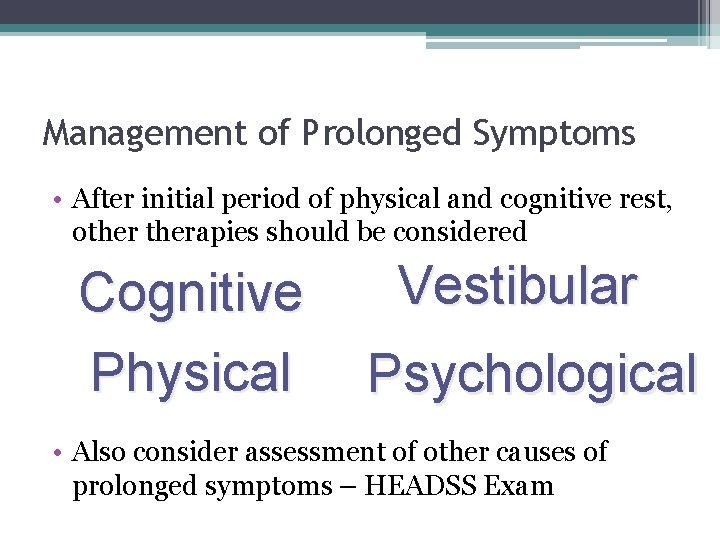
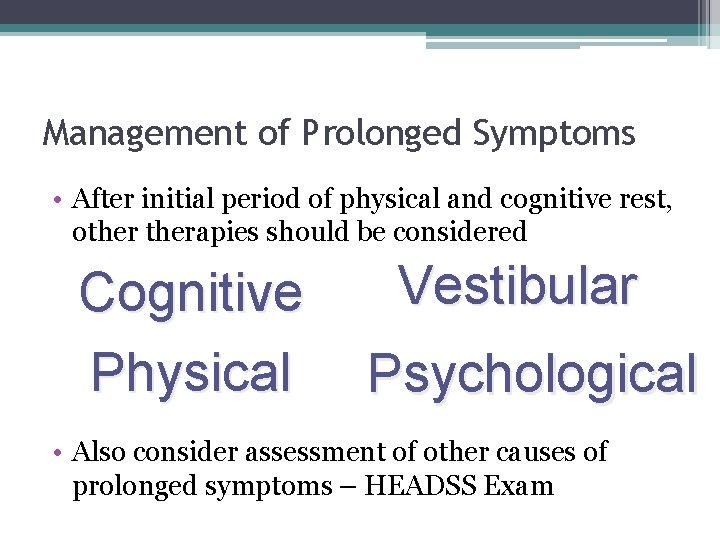
Management of Prolonged Symptoms • After initial period of physical and cognitive rest, otherapies should be considered Cognitive Physical Vestibular Psychological • Also consider assessment of other causes of prolonged symptoms – HEADSS Exam
Helpful Handouts • CDC HEADS UP – ▫ Online training course http: //www. cdc. gov/concussion/headsup/clinicians/ ▫ Fact sheets for parents, coaches, athletes and sport’s officials
Moving Forward with Concussion • President Obama requested $5 million in 2017 budget for a National Concussion Surveillance System which would help provide more accurate information about the actual number of children and adults affected by concussion each year.
References Giza, C. C. , Kutchner, J. S. , Ashwal, S. , Barth, J. , Getchius, T. S. D. , et al. (2013). Summary of Evidenced-based Guideline Update: Evaluation and Management of Concussion in Sports. Neurology, 80: 2250 -7. doi: 10. 1212/WNL. 0 b 013 e 31828 d 57 dd Halstead, M. E. , Mc. Avoy, K. , Devore, C. D. , Carl, R. , Lee, M. , et al. (2013). Returning to Learning Following a Concussion. Pediatrics, 132, 948 -57. doi: 10. 1542/peds. 2013 -2867 Harmon, K. G. , Drezner, J. A. , Gammons, M. , Guzkiewicz, K. M. , Halstead, M. , et al. (2013). American Medical Society for Sports Medicine position statement: Concussion in Sport. British Journal for Sports Medicine, 47, 15 -26. doi: 10. 1136/bjsports-2012 -091941 Mc. Crory, P. , Johnston, K. , Meeuwisse, W. , Aubry, M. , Cantu, R. , Dvorak, J. , et al. (2005). Summary and agreement statement of the 2 nd International Conference on Concussion in sport, Prague 2004. British Journal of Sports Medicine, 39(4): 196 -204. Mc. Crory, p. , Meeuwisse, W. , Aubry, M. , Cantu, B. , Dvorak, J. , et al. (2013). Consensus Statement on Concussion in Sport – The 4 th International Conference on Concussion in Sport held in Zurich, November 2012. British Journal of Sports Medicine, 47, 250 -258.

References Continued Morgan, C. D. , Zuckerman, S. L. , Lee, Y. M. , King, L. , Beaird, S. et. al. (2015). Predictors of Postconcussion Syndrome After Sports-Related Concussion in Young Athletes: a matched case-control study. Journal of Pediatric Neurosurgery, 15: 589 -598. doi: 10. 3171/2014. 10. PEDS 14356 Resch, J. E. & Kutcher, J. S. (2015). The Acute Management of Sport Concussion in Pediatric Athletes. Journal of Child Neurology, 1 -9. doi: 10. 1177/0883073815574335 Starling, A. (2015). Treatment of TBI, Concussion, PTH Cases and Thoughts on Current and Future Research [Powerpoint Slides]. Presented at American Headache Society 2015 Scottsdale Headache Symposium. American Academy of Neurology (2013). Summary of Evidence-based Guideline for Clinicians, Update: Evaluation and Management of Concussion in Sports. Retrieved from http: //www. neurology. org/content/80/24/2250. full
QUESTIONS?