CONCUSSION CPD 2018 Continuing Professional Development April 2018








- Slides: 50
CONCUSSION – CPD 2018 Continuing Professional Development April 2018 Eb Friedrich Clinical Manager Colbrow Medical Mechanism +1
CONCUSSION I know most of you have trouble assessing a patient, so please ask questions Mechanism +1
CONCUSSION Mechanism +1 A large part of Colbrow business is the provision of medics to sporting events Consequently we take medical issues relating to sports very seriously. In Particular: Ø Concussion Management Ø Spinal Management Ø Soft tissue Injuries
CONCUSSION What is concussion? Mechanism +1
CONCUSSION Mechanism +1 Concussion in sport has been recognised as a significant medical issue, highlighted by: Ø Short & long term memory, cognitive and psychological trauma Ø Recognition of potential permanent consequences, particularly in regard to successive concussive events (Chronic Traumatic Encephalopathy) Ø Massive liability issues in NFL (USA), further highlighted by the film “Concussion” Ø Recognition of biochemical changes in the brain Ø Recognition by sporting bodies in Australia such as the AFL and Australian Institute of Sports and the Australian Medical Association

Over a $billion USD set aside for concussion liability claims in US Mechanism +1
Mechanism +1
CONCUSSION – Teenage Tragedy Mechanism +1 Joseph Barajas 15 years old After sustaining a concussion in a junior varsity game, Barajas experienced blurred vision and headaches. A doctor told Barajas to sit out one week and later cleared him to play. In his third game back, Barajas collided head on with another player, walked to the sideline and lost consciousness. He died after developing a blood clot in his brain
CONCUSSION – Teenage Tragedy Mechanism +1 Will Benson 17 years old Benson sustained a striking helmet to helmet hit in a game but played on. He sat out the next week with headaches but returned the following week. He left in the second quarter saying he felt “weird” and had splotchy vision. He slipped into coma and was pronounced brain dead a week later
CONCUSSION – Teenage Tragedy Mechanism +1 Matthew Colby 17 years After sustaining a concussion Sept 15, Colby was cleared by doctors to play despite still experiencing headaches that kept him out until Sept. 28. Witnesses said he looked sluggish early in the game before he jogged to the sideline and collapsed. He died the next day of bleeding and swelling in the brain.

CONCUSSION – Teenage Tragedy Mechanism +1 Rowan Stringer – Female Age 17, A talented rugby player, died on May 12, 2013 — Mother’s Day — after suffering two concussions within a week while playing the game she loved. This lead to a scathing coroners report and the enactment of “Rowan’s Law” in Ontario Canada, mandating concussion procedures and education All 50 U. S. states have laws dictating the management of youth concussions. (Australia has none)
CONCUSSION – Teenage Tragedy Mechanism +1 The Adolescent Brain – At Greater Risk “We do think the adolescent brain is the most sensitive brain to the effects of concussion. We used to think the infant brain was the most sensitive to trauma, but it appears now, because of the huge number of connections that are being made during adolescence, there’s a reason to worry more about adolescents getting concussed. They certainly take longer than adults to recover. ” Dr Karen Barlow, a paediatric neurologist specializing in traumatic brain injury and concussion at the Alberta Children’s Hospital
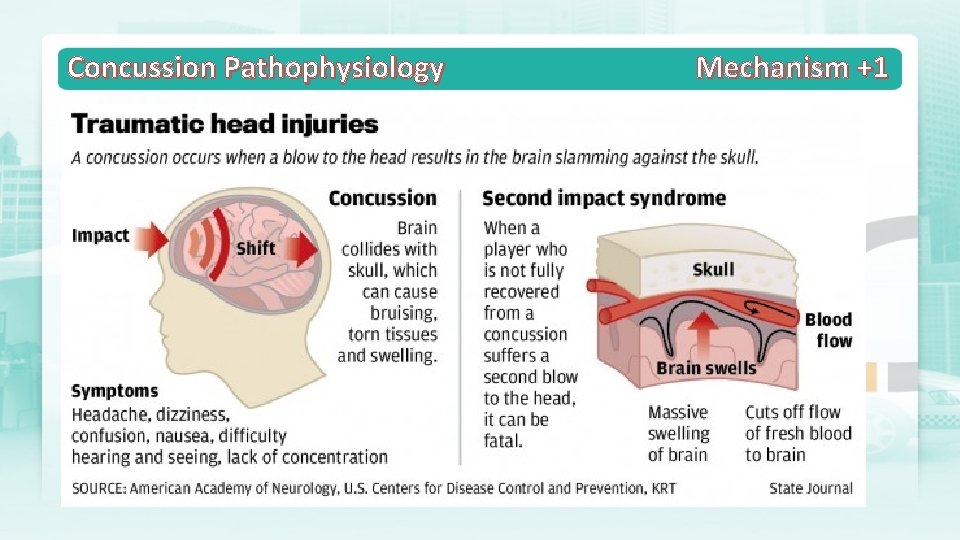
Concussion – The Deadly SIS Mechanism +1 WHAT IS SECOND IMPACT SYNDROME (SIS) ? Second impact syndrome (SIS) is a rare fatal condition that develops as a result of two separate events. Initially, the athlete sustains a concussion/traumatic brain injury, which causes them to suffer from concussion signs and symptoms such as fatigue, headache, nausea, disorientation, as well as sensory, motor and mental disturbances. The second event occurs when the athlete returns to play before the concussive symptoms have resolved and receives a second blow to the head.
Concussion – The Deadly SIS Mechanism +1 This second impact does not need to be forceful in order to be fatal. It may be a minor blow to the chest in which enough accelerating forces on the brain are created to cause major damage. These forces result in massive swelling of the brain (cerebral oedema), which can lead to the death of the athlete within two to five minutes after the injury has been sustained. When exploring SIS and the first hit versus the second hit, the first hit (and resulting concussion) is considered less severe than the second because of an internal regulatory system known as auto-regulation. This system reduces the stress placed on the brain by limiting the amount of blood flow in an attempt to prevent swelling.
Concussion – The Deadly SIS Mechanism +1 Researchers believe that once the brain loses its ability to auto-regulate, ( i. e. during the healing process) it becomes more vulnerable and therefore more susceptible to traumatic brain injuries and SIS. If an athlete were to sustain a second injury before the brain has properly healed, the auto-regulatory mechanism would not function properly, there would be no alteration in the amount of blood flow to the brain, and it would result in massive swelling of the brain tissue.
Concussion – The Deadly SIS Mechanism +1 After the second impact, the athlete may remain conscious but appears to be stunned; however, sometimes within seconds or minutes, the athlete will suddenly collapse, their pupils will become dilated and they will eventually stop breathing, resulting in death.
CONCUSSION – What is it? Mechanism +1
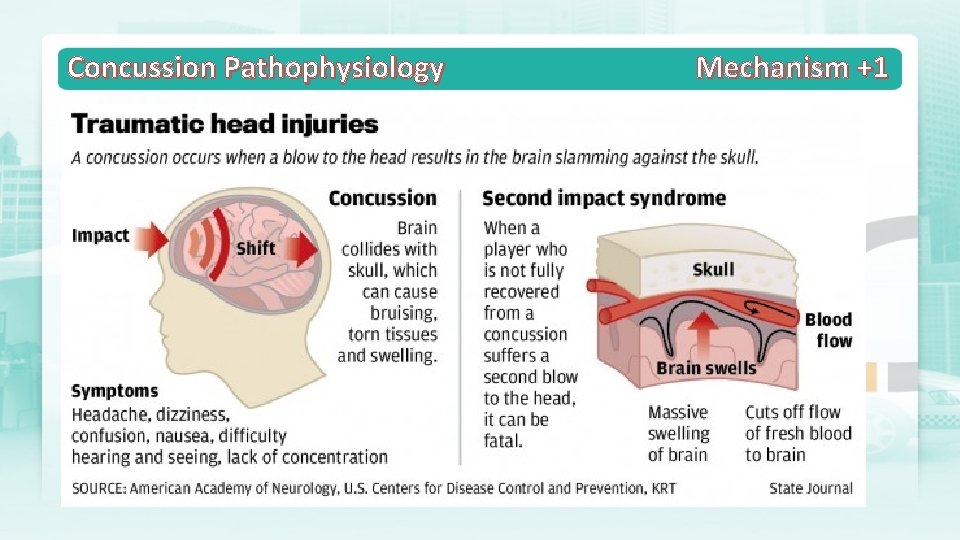
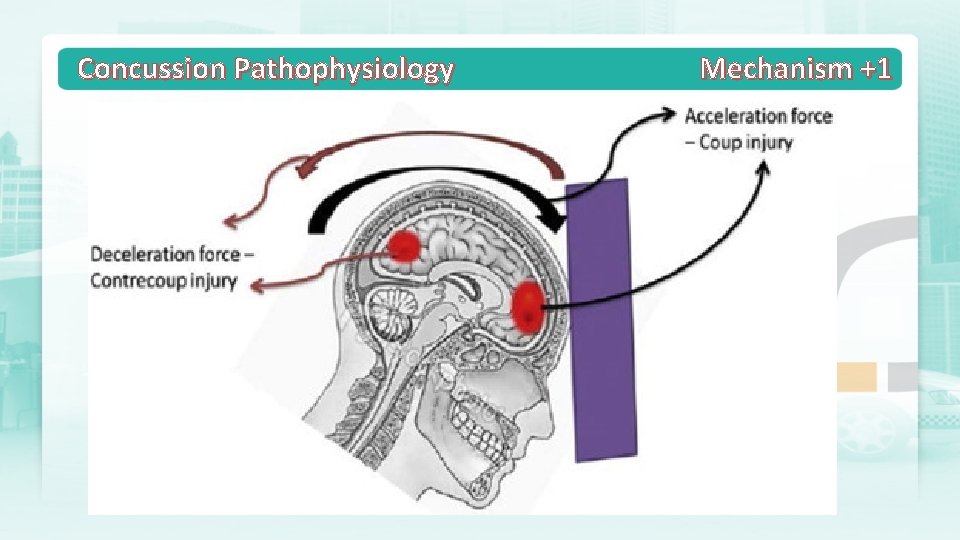
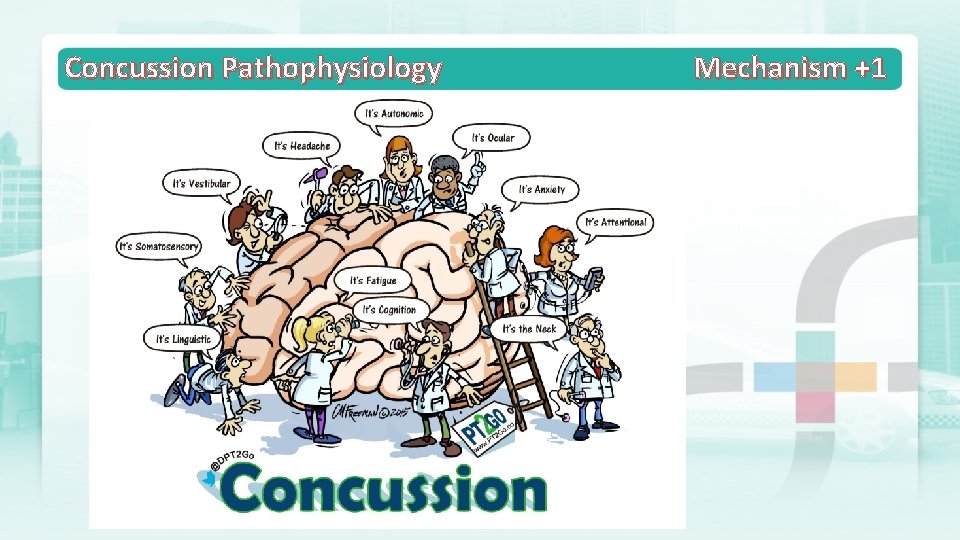
Concussion Pathophysiology Mechanism +1
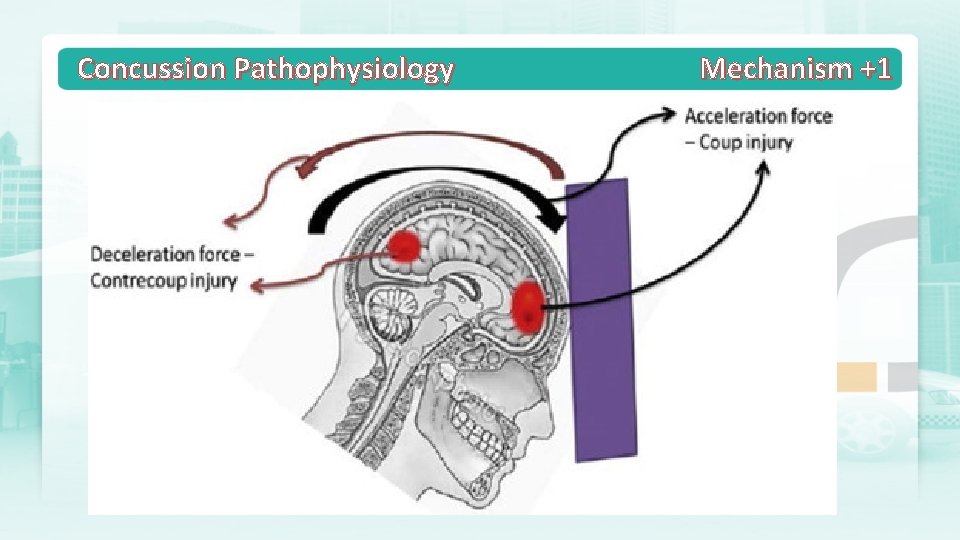
Concussion Pathophysiology Mechanism +1
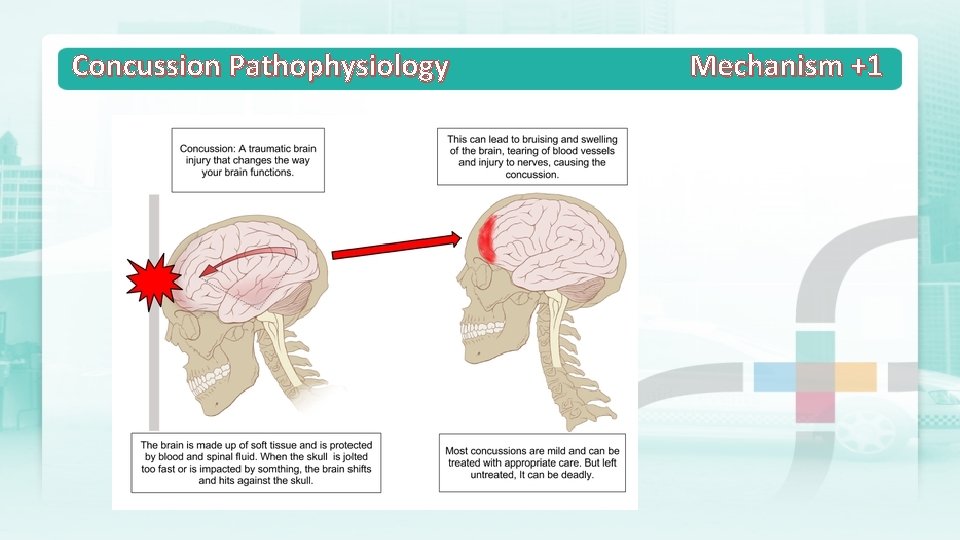
Concussion Pathophysiology Mechanism +1
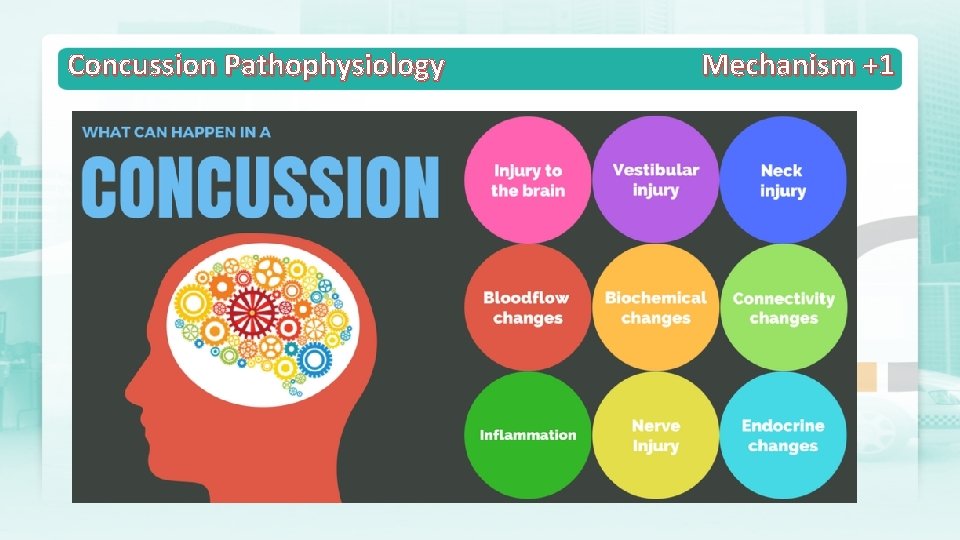
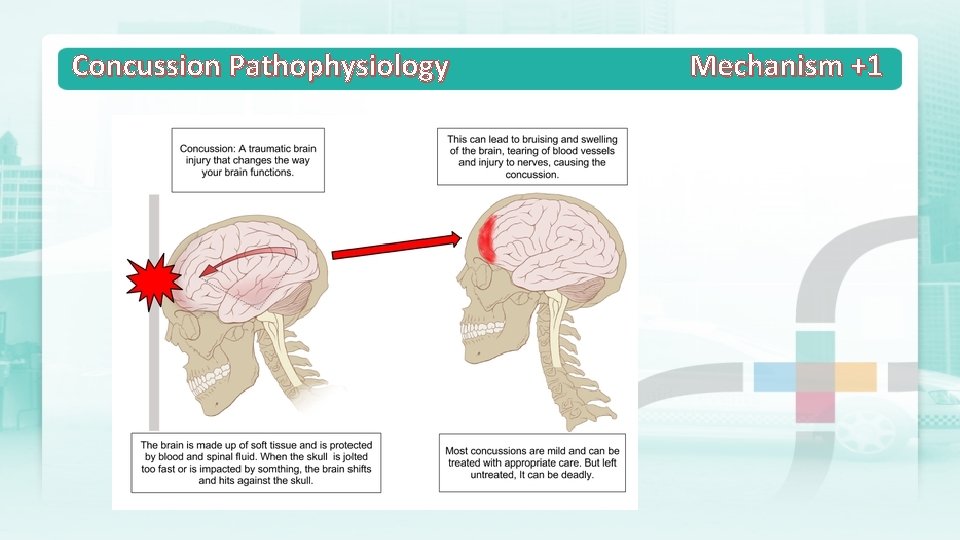
Concussion Pathophysiology Mechanism +1
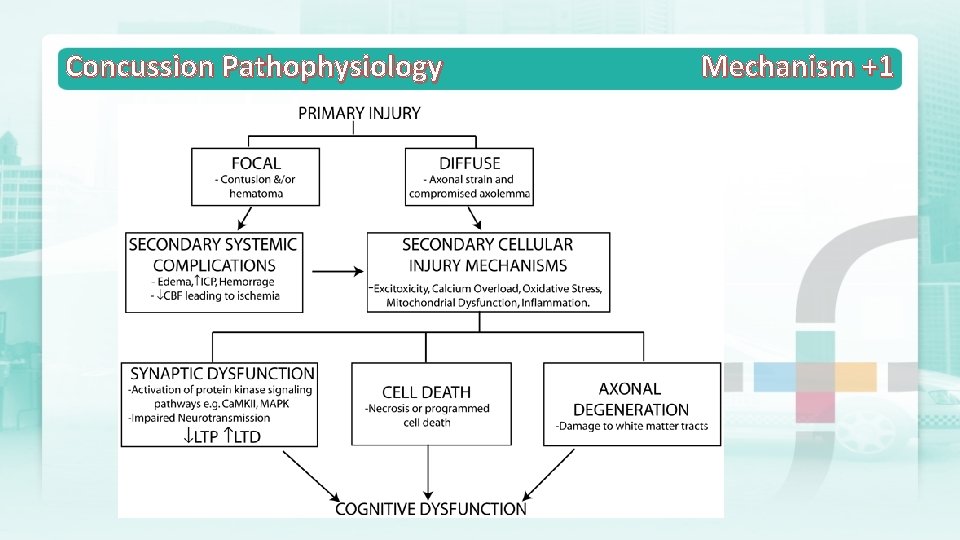
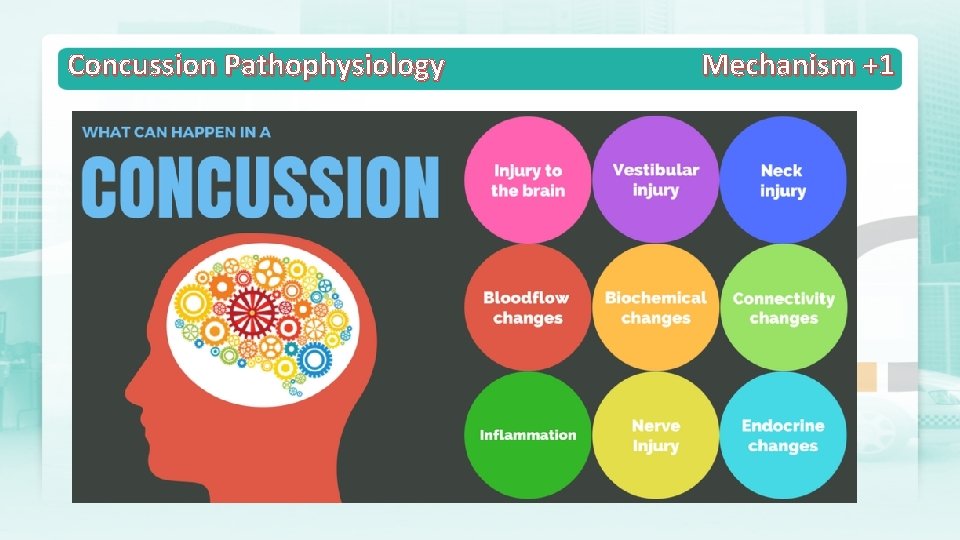
Concussion Pathophysiology Mechanism +1
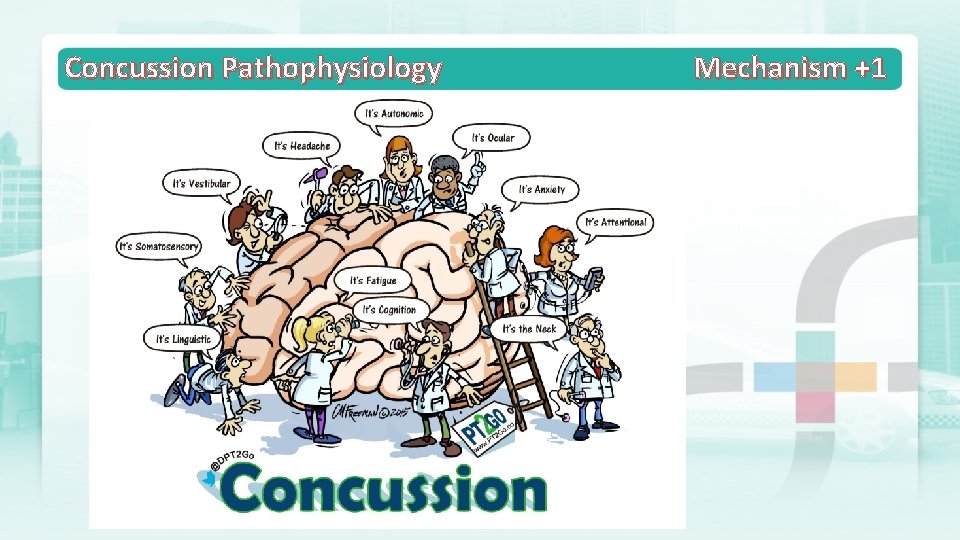
Concussion Pathophysiology Mechanism +1

Concussion Pathophysiology Mechanism +1
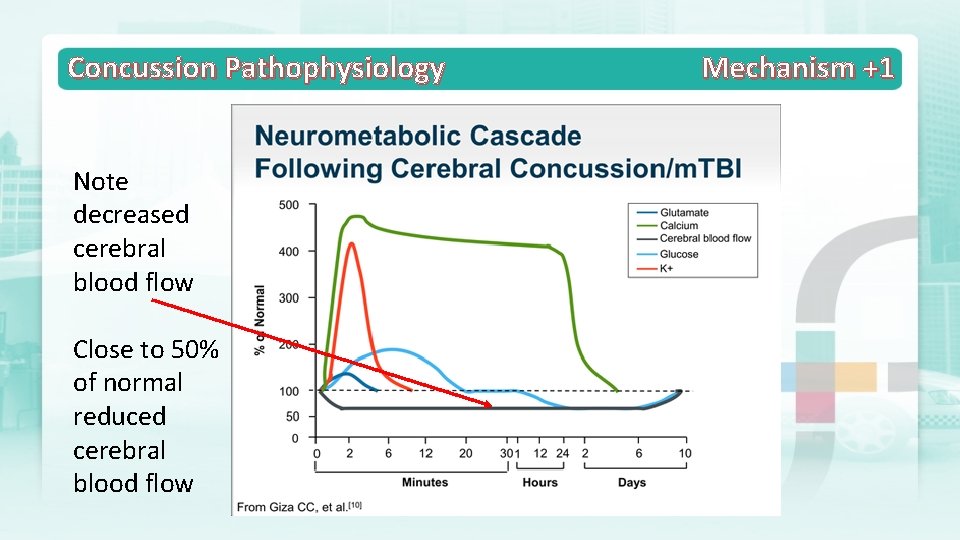
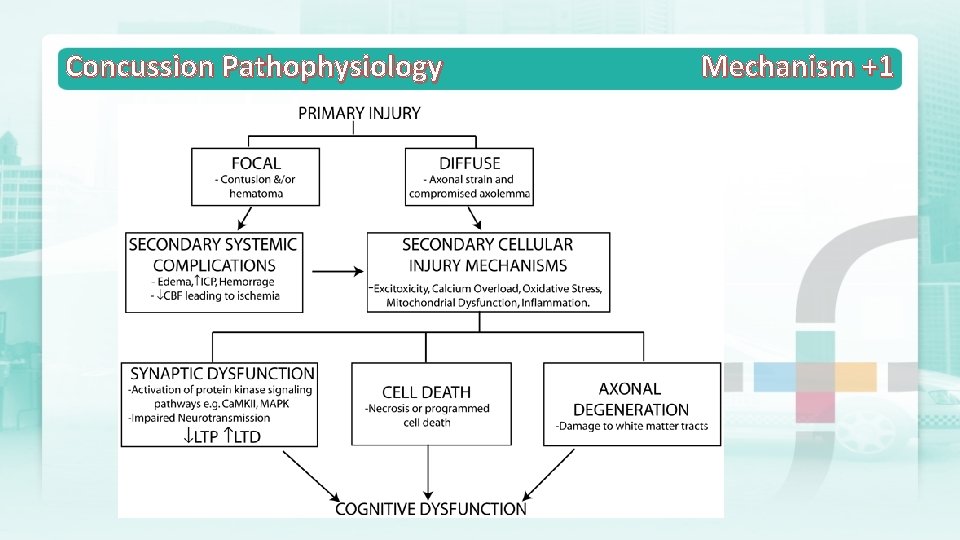
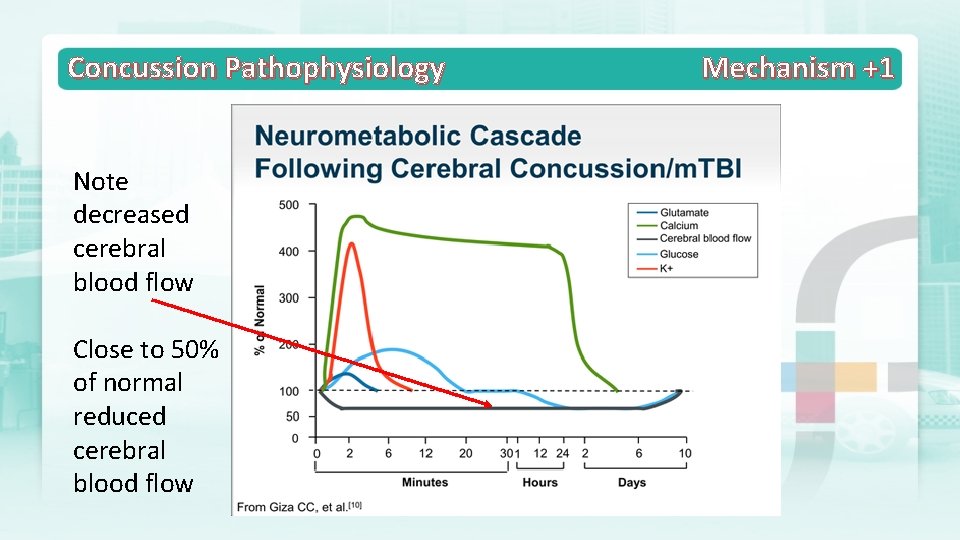
Concussion Pathophysiology Note decreased cerebral blood flow Close to 50% of normal reduced cerebral blood flow Mechanism +1
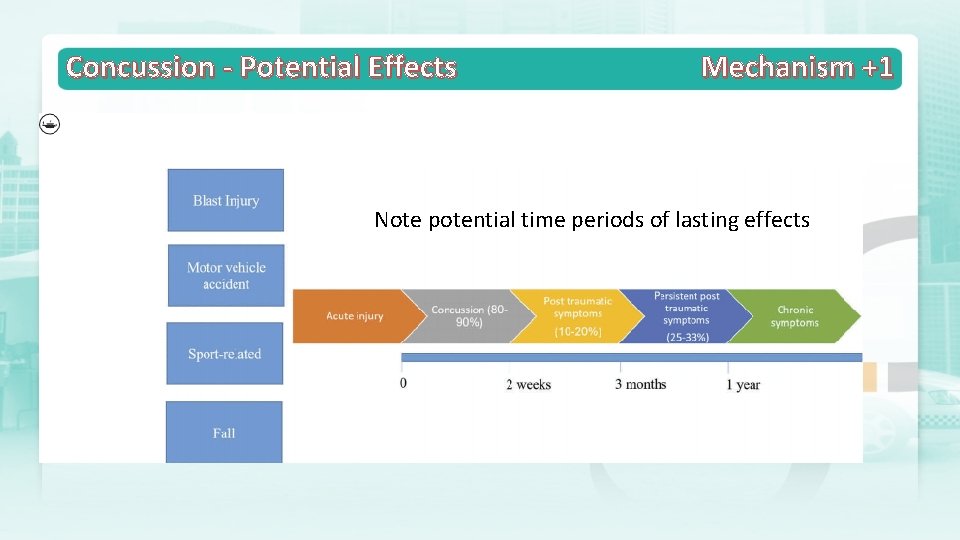
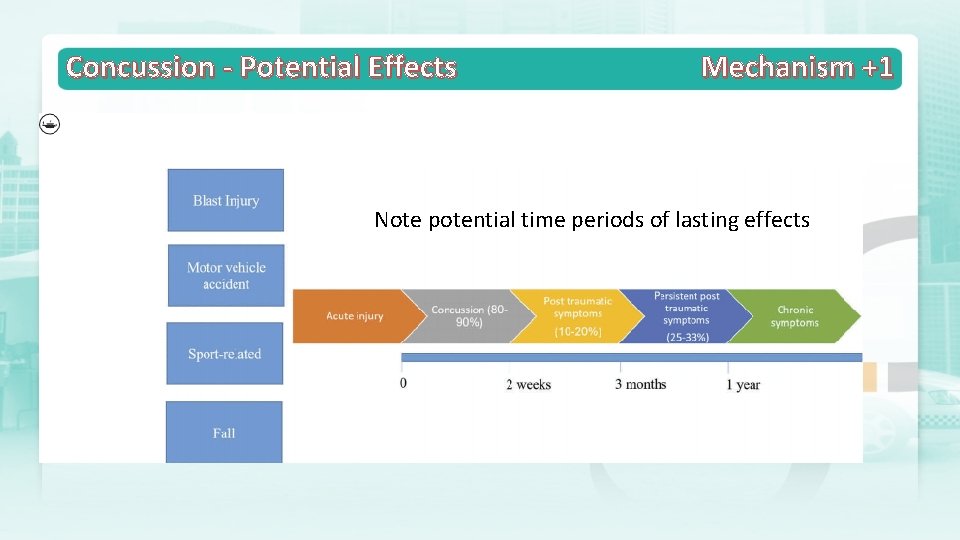
Concussion - Potential Effects Mechanism +1 Note potential time periods of lasting effects
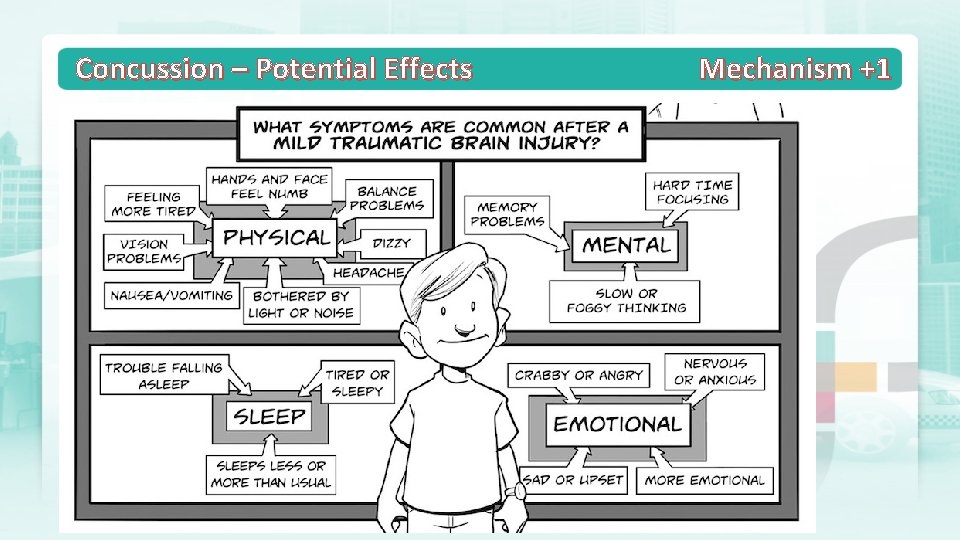
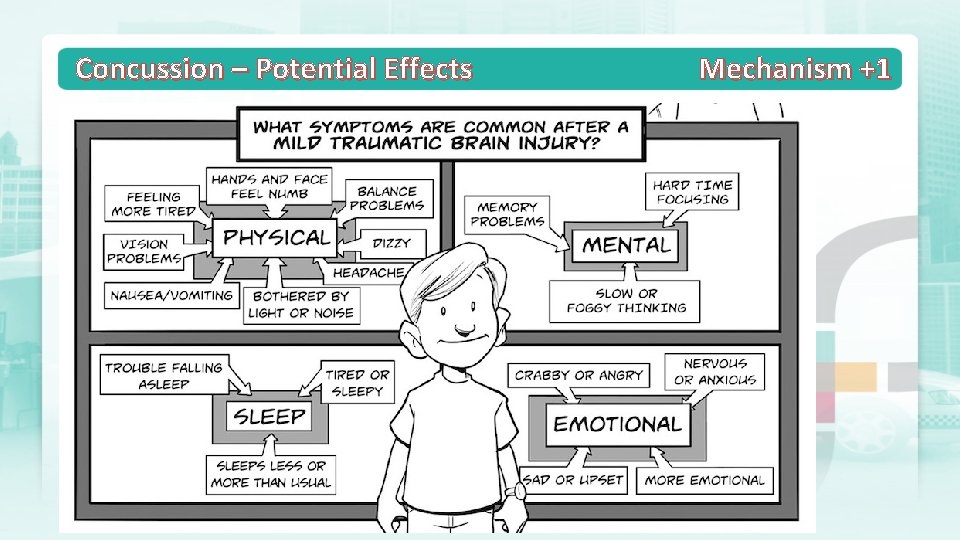
Concussion – Potential Effects Mechanism +1
Concussion – Potential Effects Mechanism +1
Concussion – Potential Effects No need for alarm, just recognition and management Mechanism +1
You only need 1 symptom to define concussion and these may be many and varied, in isolation or several Mechanism +1 Concussion – Definition

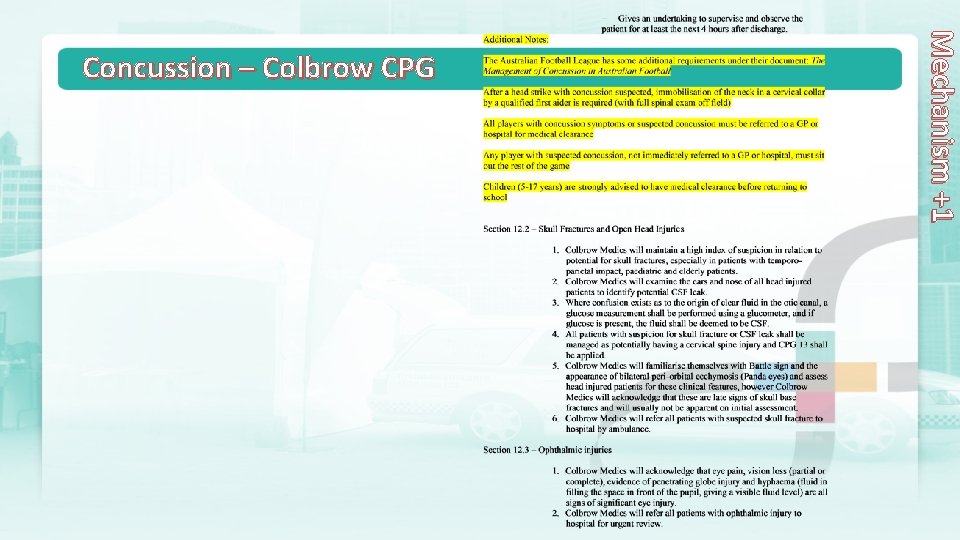
Colbrow CPG for Head Trauma & Concussion(link under VT/Home Page/Notices) Mechanism +1 Concussion – Colbrow CPG
Mechanism +1 Concussion – Colbrow CPG
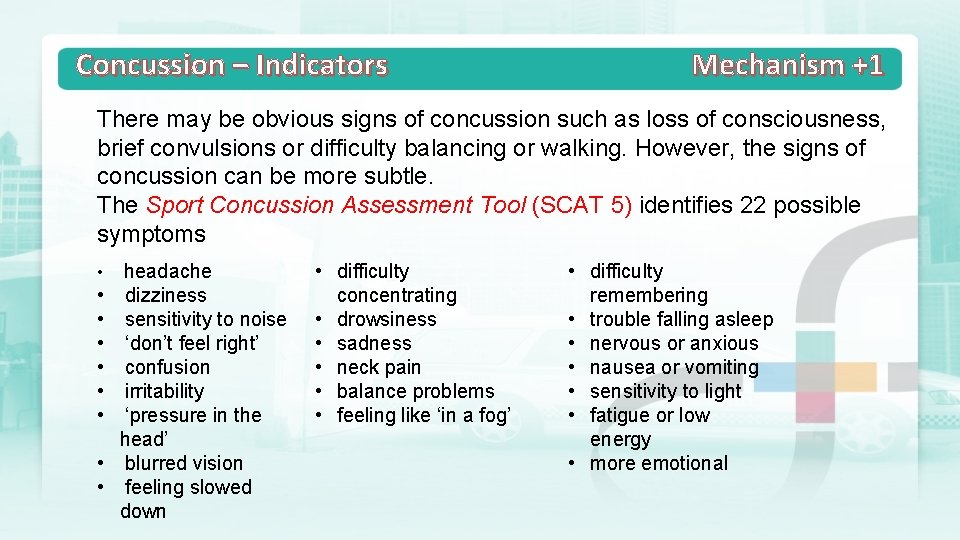
Concussion – Indicators Mechanism +1 There may be obvious signs of concussion such as loss of consciousness, brief convulsions or difficulty balancing or walking. However, the signs of concussion can be more subtle. The Sport Concussion Assessment Tool (SCAT 5) identifies 22 possible symptoms • • • headache dizziness sensitivity to noise ‘don’t feel right’ confusion irritability ‘pressure in the head’ blurred vision feeling slowed down • difficulty concentrating • drowsiness • sadness • neck pain • balance problems • feeling like ‘in a fog’ • difficulty remembering • trouble falling asleep • nervous or anxious • nausea or vomiting • sensitivity to light • fatigue or low energy • more emotional
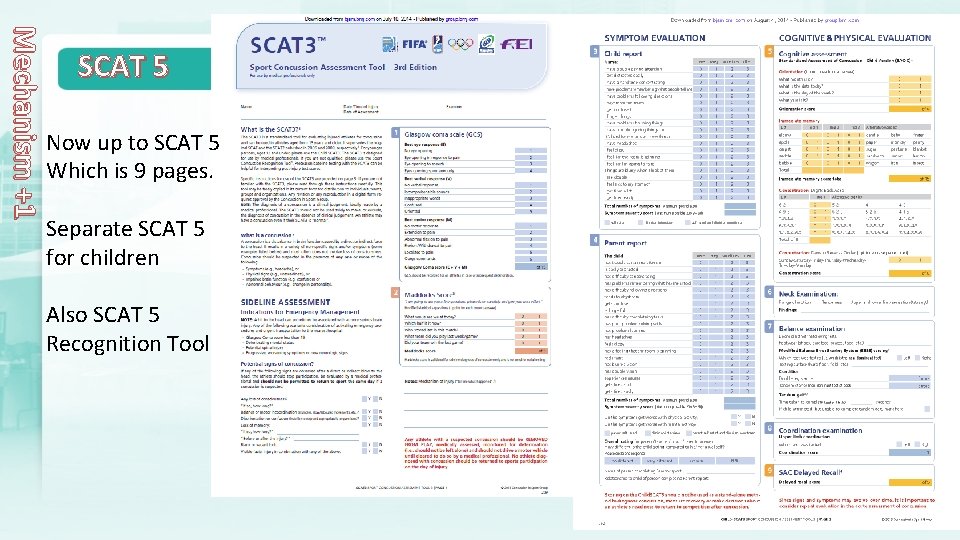
Mechanism +1 SCAT 5 Now up to SCAT 5 Which is 9 pages. Separate SCAT 5 for children Also SCAT 5 Recognition Tool
Concussion – Indicators Mechanism +1 Sometimes there will be clear signs that an athlete has sustained a concussion. Medical practitioners covering sporting events should immediately remove an athlete with any of the following clinical features: Ø loss of consciousness Ø no protective action in fall to ground directly observed or on video Ø impact seizure or tonic posturing Ø confusion, disorientation Ø memory impairment
Concussion – Indicators Mechanism +1 Ø balance disturbance (e. g. ataxia) Ø athlete reports significant, new or progressive concussion symptoms Ø dazed, blank/vacant stare or not their normal selves Ø behaviour change atypical of the athlete. Athletes displaying any one of these signs should be treated as concussed and not be returned to sport
Concussion – Indicators Mechanism +1 Some features suggest more serious injury and athletes displaying any of these signs should be immediately referred to the nearest emergency department: Ø neck pain Ø increasing confusion or irritability Ø repeated vomiting Ø seizure or convulsion Ø weakness or tingling/burning in the arms or legs
Concussion – Indicators Ø deteriorating conscious state Ø severe or increasing headache Ø unusual behavioural change Ø double vision. Mechanism +1

Concussion – First Aid Management of Concussion: § DRABC/VSS (repeat!) § Consider Spinal Precautions § Recognition of signs and symptoms (Consider TBI) § Colbrow CPG § Referral advocacy - Club - Parents - Player

Concussion – Actions Mechanism +1 1. The immediate removal of a young athlete from play if a concussion is suspected. 2. Avoid all further sports activities. Require written permission to resume sport/training 3. Inform the injureds' emergency contact, i. e. parents or guardians about the possible concussion 4. Ensure that the injured is evaluated by a healthcare professional experienced in dealing with concussions as soon as possible. Do not try to judge the seriousness of the injury yourself. 5. The injured should not return to sports activities until a healthcare professional, experienced in evaluating concussions, confirms they are symptom-free. 6. Strict adherence to return-to-learn and return-to-play protocols for youth athletes with concussions. 7. Mandatory concussion education for all young athletes, parents and coaches 8. Give Colbrow Concussion Advice Recommendation Handout
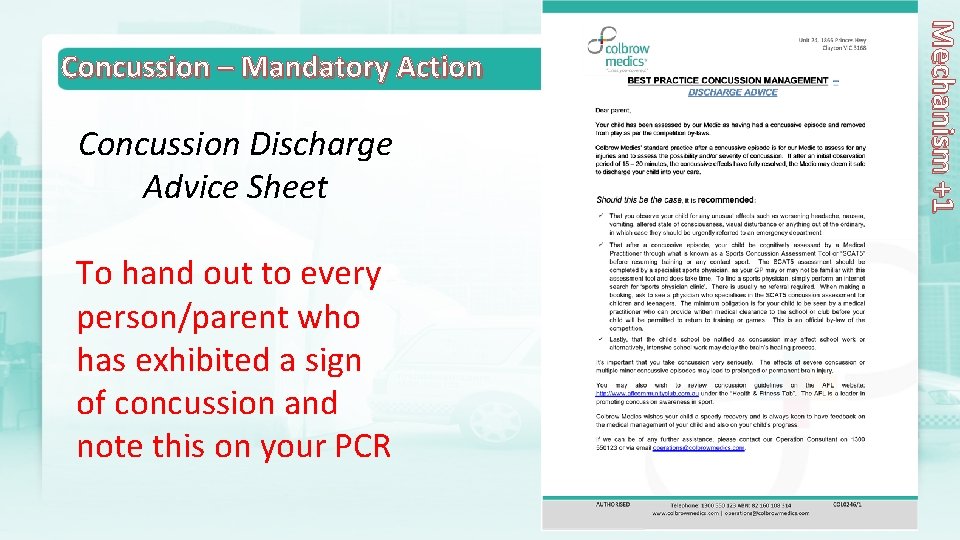
Concussion Discharge Advice Sheet To hand out to every person/parent who has exhibited a sign of concussion and note this on your PCR Mechanism +1 Concussion – Mandatory Action
Colbrow is proud to be a leader in concussion management first aid. We have developed the Concussion Advice Sheet to close the cracks in concussion management by: ü Recognising that many GP’s may not be experienced in providing concussion advice or performing a concussion assessment ü By recognising that whilst an imperfect science, concussion assessment must be performed by a specialist trained in using the SCAT 5 assessment tool. Usually by sports physicians & experts such as at Olympic Park Sports Medicine, Melbourne ü Emphasising to parents & coaches the seriousness of concussion management and to recommend the concussion discharge advice sheet and education Mechanism +1 Concussion Discharge Advice Sheet – a leading initiative
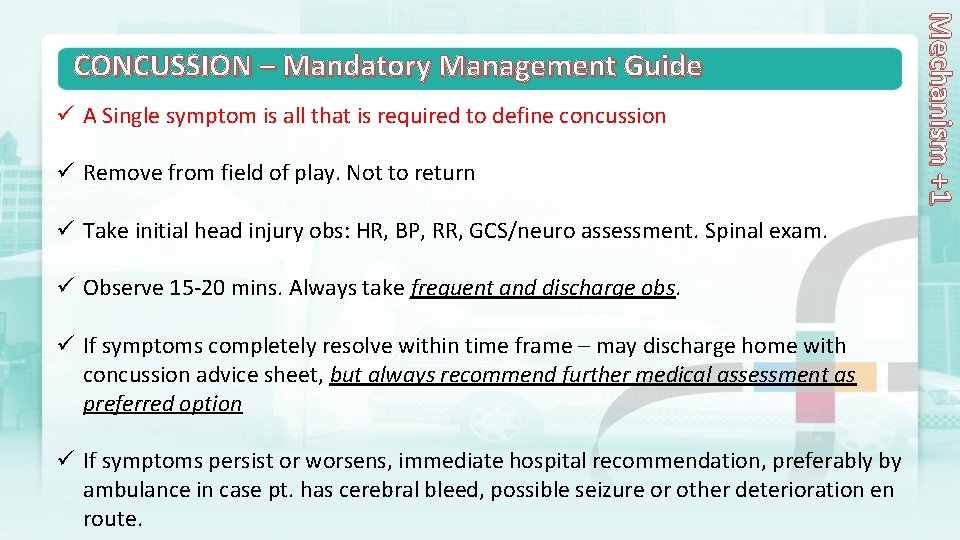
ü A Single symptom is all that is required to define concussion ü Remove from field of play. Not to return ü Take initial head injury obs: HR, BP, RR, GCS/neuro assessment. Spinal exam. ü Observe 15 -20 mins. Always take frequent and discharge obs. ü If symptoms completely resolve within time frame – may discharge home with concussion advice sheet, but always recommend further medical assessment as preferred option ü If symptoms persist or worsens, immediate hospital recommendation, preferably by ambulance in case pt. has cerebral bleed, possible seizure or other deterioration en route. Mechanism +1 CONCUSSION – Mandatory Management Guide

CONCUSSION – Sporting Body Guidelines Mechanism +1 In addition to the CPG’s, Colbrow Medics will be familiar with and apply the following guidelines: ü The AFL “Management of Concussion in Australian Football” ü The AFL Pocket Concussion Recognition Tool ü The Australian Institute of Sport and Australian Medical Association Concussion in ü Sport Position Statement
CONCUSSION – Sporting Body Guidelines Mechanism +1 ü Medics will also be familiar with (but not apply) the Sports Concussion Assessment Tool (SCAT 5). Medics have no role to use SCAT 5. ü Colbrow Medics Only Concussion Tool is: Mechanism +1 ü Associated Grammar Schools of Victoria Concussion Guidelines: http: //www. agsvsport. com. au/files/36296/files/Policies%20 and%20 Guidelines/A GSV%20 Concussion%20 Guidelines%20 Final%20 Feb%202014. pdf (only a doctor can clear a student to return to play or training)

CONCUSSION Mechanism +1
CONCUSSION Mechanism +1
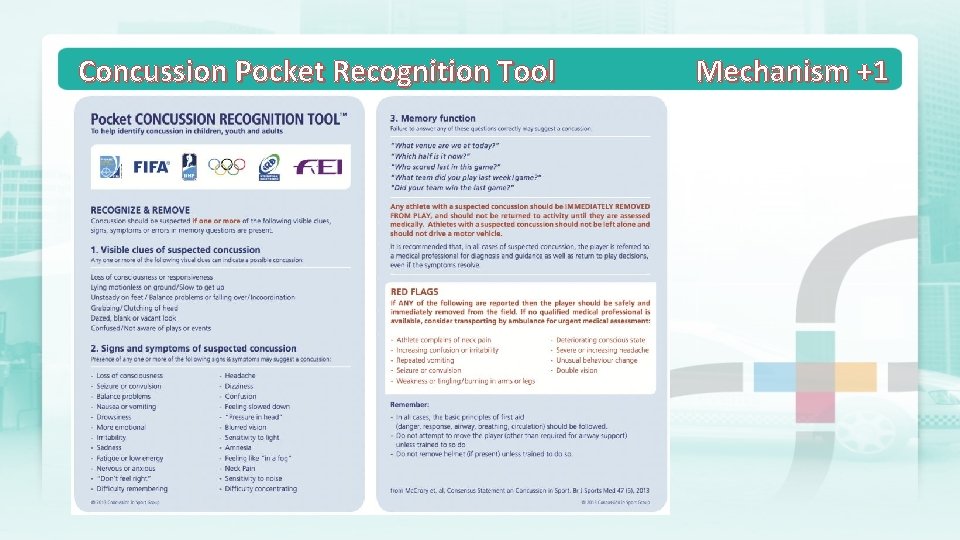
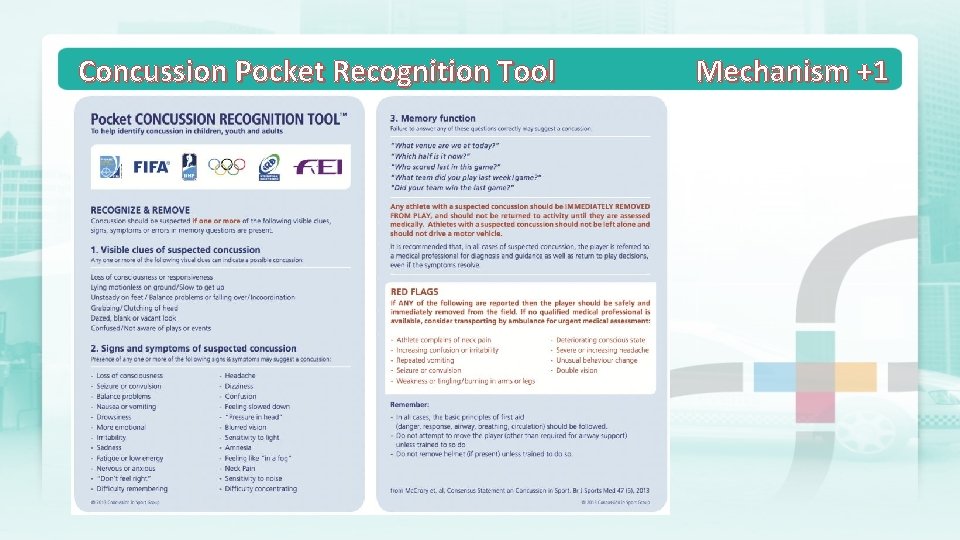
Concussion Pocket Recognition Tool Mechanism +1
Concussion Documentation Mechanism +1 PCR Tips… P/History – particularly previous concussion/when? Mechanism/force (estimate) Obs – VSSS - head injury. Initial and frequent including discharge. HR/RR/BP/GCS Head to Toe – emphasis on head and neck. Spinal obs. Concussive symptoms? Only need 1 – YOUR SOLE CRITERIA Remove from play Observe 15 -20 mins If complete resolution – recommend ED attendance/concussion assessment/concussion discharge advice handout ü If no complete resolution or worsening symptoms, 000 immediately. ü ü ü ü
Concussion Mechanism +1 Concussion has no treatment, except “Brain Rest” Remember: MECHANISM + 1 IS ALL THAT IS REQUIRED TO DEFINE CONCUSSION