Concepts of Health Care Processes and Process Analysis

- Slides: 56

Concepts of Health Care Processes and Process Analysis Slides contributed by Drs. Zhang and Shahriar
Topics • Workflow Analysis Concepts and importance • IOM 6 Quality Areas and Meaningful Use • Clinical activities examples • Clinical defect 2
Why is Health Care Process Analysis and Redesign Important? • Medical errors rank behind heart disease and cancer as the third leading cause of death in the U. S. , Johns Hopkins researchers say. • 250, 000 or more people die annually in the US due to medical errors • call for changes in death certificates to better tabulate fatal lapses in care • http: //www. npr. org/sections/healthshots/2016/05/03/476636183/death-certificatesundercount-toll-of-medical-errors 3 Public domain images obtained from National Academy Press, http: //www. nap. edu/
Why is Health Care Process Analysis and Redesign Important? • Lack of information and care fragmentation called out as leading contributors • Meaningful use of Health IT should decrease this number 4 Public domain images obtained from National Academy Press, http: //www. nap. edu/
Definitions • • Process Analysis Process Redesign Workflow Analysis Data, Information, and Knowledge Data and Information Flow 5
Process • a series of actions or operations conducing to an end • a continuous operation or treatment • Procedure: The steps in a process and how these steps are to be performed 6
Process Analysis • Understanding process elements and the relationships between them • Identification of opportunities for improvement 7
Process Redesign The revision of a process to improve it in some way. 8
Workflow • “The flow of work” • The way in which work progresses, including order of steps and selection between alternative steps. 9
What is Clinical Workflow? • Workflow is an established business process describing how tasks are done, by whom, in what order and how quickly • Workflow is defined as the coordination of tasks, data, and people to make a business process more efficient, effective, and adaptable to change • Clinical Workflow is an established clinical business process describing how tasks are done in the health care setting, by whom, in what order and how efficiently 10
Workflow Analysis • Understanding workflow elements and the relationships between them • Identification of opportunities for improvement 11
Data, Information, and Knowledge • Data: – Factual information – A difference • Information: data + meaning • Knowledge: justified true belief – Declarative knowledge – Procedural knowledge 12
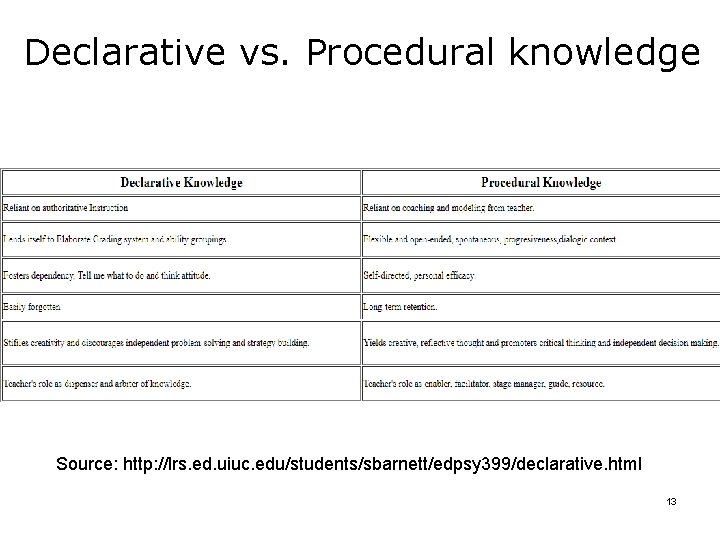
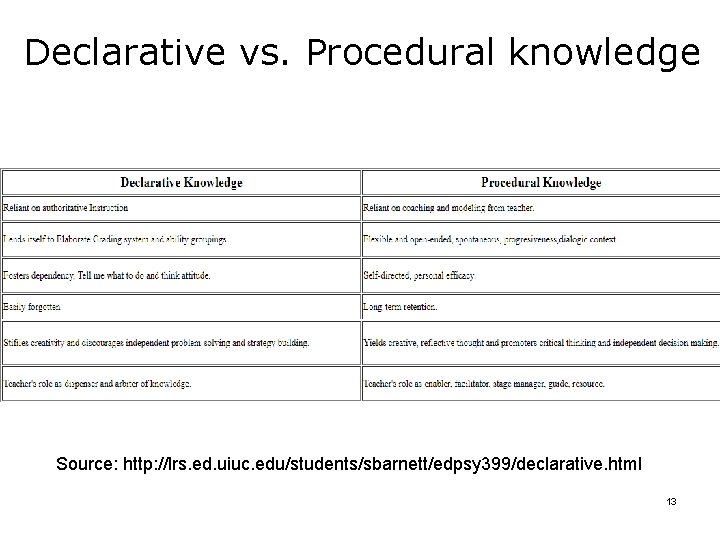
Declarative vs. Procedural knowledge Source: http: //lrs. ed. uiuc. edu/students/sbarnett/edpsy 399/declarative. html 13
Data and Information Flow The steps or path by which data are moved through a work process or a system or some combination of both, including the order of steps, and operations performed on the data (or information) 14
A Workflow Process Analyst and Redesign Specialist Uses knowledge and understanding of 1. an organizations objectives, structure and procedures, and 2. how to use information technology to analyze and make recommendation on how to improve an organization’s operation to achieves its goals 15
Process Analyst Role • • Describe the Dance Overcome communications problems in analysis – Natural difficulty in describing procedure – Inappropriateness of narrative text for describing procedures – Lack of common language between the user and analyst 16
Process Analysis Involves • Understanding process elements and the relationships between them • Identification of opportunities for improvement 17
Process Analysis Skills • • • Knowledge of data and data system concepts Knowledge of clinical workflow concepts Able to communicate such concepts Able to identify problem areas Ability to combine organizational knowledge and technology to create a better way 18
The Six Domains of Health Care Quality • Analytic frameworks for quality assessment have guided measure development initiatives in the public and private sectors. One of the most influential is the framework put forth by the Institute of Medicine (IOM) • Six aims for the health care system 1. care should be safe 2. care and service should be cost effective 3. science and evidence behind health care (efficient) 4. no waits or delays in receiving service (timely) 5. system of care should revolve around the patient (patient centered) 6. disparities in care should be eradicated (equitable) 19
EHR Meaningful Use • Meaningful Use” of EHRs is used to collectively describe criteria established by the (American Recovery and Reinvestment Act) ARRA to qualify health care providers for Electronic Health Record incentives to be provided • Addresses national health policy priorities – Improve quality, safety and efficiency and reduce health disparities – Engage patients and families – Improve care coordination, and population and public health – Maintain privacy and security of patient health information https: //www. healthit. gov/providers-professionals/meaningful-use-definition -objectives 20
Meaningful Use • Qualified EHR - an electronic record of health-related information that: • Includes patient demographic and clinical health information • Has the capacity to: • • Provide clinical decision support Support physician order entry Capture and query information relevant to health care quality Exchange electronic health information with, and integrate such information from, other sources 21
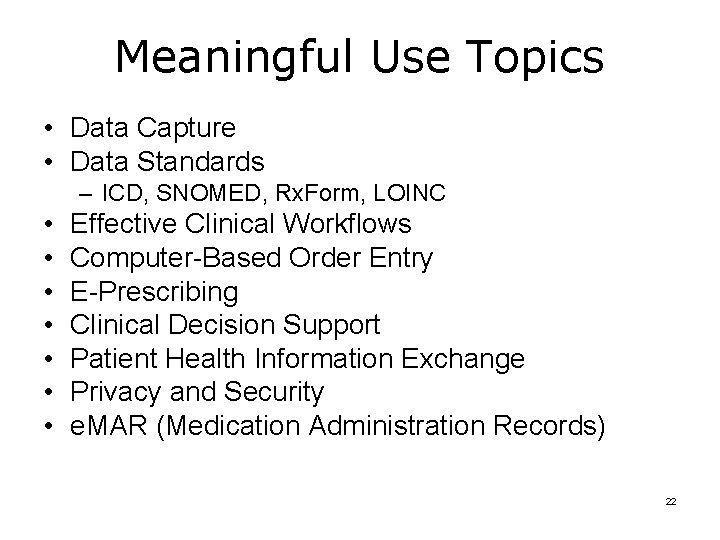
Meaningful Use Topics • Data Capture • Data Standards – ICD, SNOMED, Rx. Form, LOINC • • Effective Clinical Workflows Computer-Based Order Entry E-Prescribing Clinical Decision Support Patient Health Information Exchange Privacy and Security e. MAR (Medication Administration Records) 22
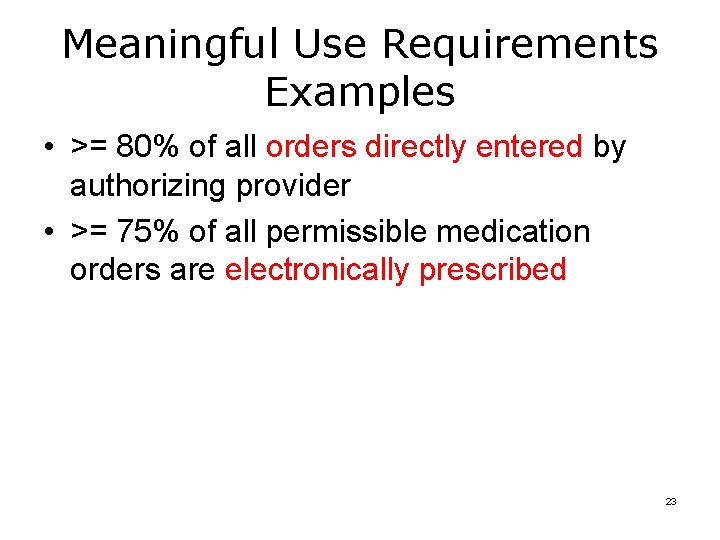
Meaningful Use Requirements Examples • >= 80% of all orders directly entered by authorizing provider • >= 75% of all permissible medication orders are electronically prescribed 23
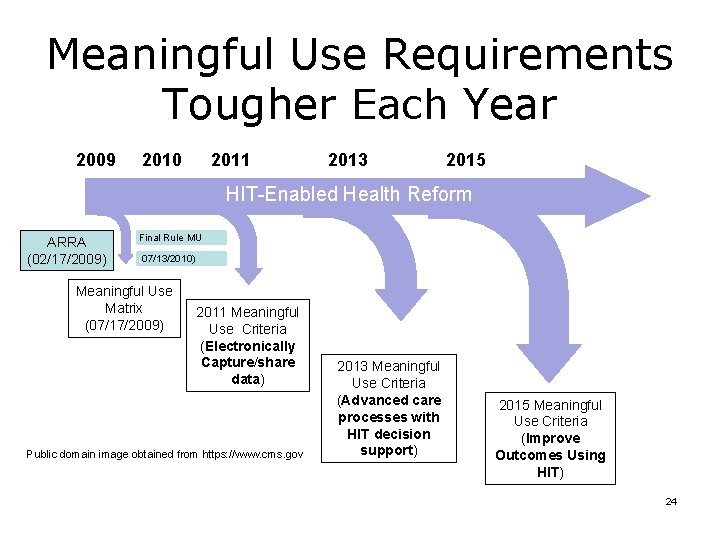
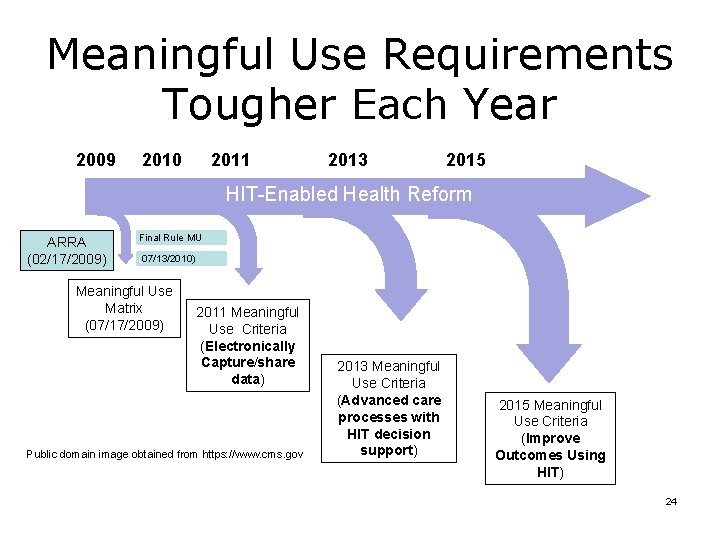
Meaningful Use Requirements Tougher Each Year 2009 2011 2010 2013 2015 HIT-Enabled Health Reform ARRA (02/17/2009) Final Rule MU (07/13/2010) Meaningful Use Matrix (07/17/2009) 2011 Meaningful Use Criteria (Electronically Capture/share data) Public domain image obtained from https: //www. cms. gov 2013 Meaningful Use Criteria (Advanced care processes with HIT decision support) 2015 Meaningful Use Criteria (Improve Outcomes Using HIT) 24
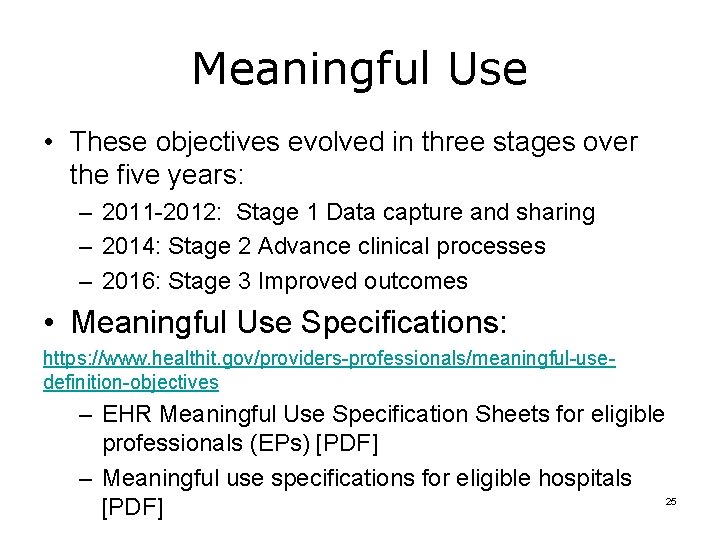
Meaningful Use • These objectives evolved in three stages over the five years: – 2011 -2012: Stage 1 Data capture and sharing – 2014: Stage 2 Advance clinical processes – 2016: Stage 3 Improved outcomes • Meaningful Use Specifications: https: //www. healthit. gov/providers-professionals/meaningful-usedefinition-objectives – EHR Meaningful Use Specification Sheets for eligible professionals (EPs) [PDF] – Meaningful use specifications for eligible hospitals 25 [PDF]
Pause!! Workflow Analysis and Redesign 26
Workflow is a Process Workflow includes: • How tasks are accomplished • By whom • Task order • Task priority • Choices and decisions • Location • Information needs 27
Clinical Care Activities • • • Interaction with patients Verbal and physical assessment Prescribing and conducting diagnostic tests Decision making and diagnosis Developing a treatment plan Assessing compliance with treatment regimen Patient education Records creation and management Determination of confidentiality / privacy requirements 28
Administrative Activities • Patient flow and efficient intake – Scheduling • Patient tracking internally and externally – Transportation • Coordination of billing for services • Making consultations and referrals • Facilities and supplies services and maintenance 29
Grouped Activities (Tasks) • • • Admission Surgery Specimen collection Reimbursement Discharge Handling of inpatient emergencies 30
Roles • • • Providers Medical Assistants Phlebotomists (primarily draw blood) Receptionists Billing Coordinators 31
Location, Location • Where tasks are performed can be important • Physical layout of a clinic impacts workflow – – Patient transportation Hallway traffic Distance clinic staff must travel to accomplish tasks Patient privacy 32
Information Needs • What information is used and generated in the course of a patient encounter? • Do providers and clinic staff have readyaccess to information they need when they need it? • Do patients have access to information about their health before, after and between visits? 33
Unique Healthcare Requirements 1. System of “experts” – Physicians and physician extenders are ultimately ethically, morally and legally responsible for everything that happens to a patient – Physicians have taken an oath to “above all, do no harm” 2. Patient care involves teams of people 3. Patterns of fundamental clinical routines are the product of years and decades of evolution 34
Complexities of Healthcare • Each situation is unique • Involve multiple people and organizations – Many opportunities for delays and variability • • Must take patient preference into account Continually changing priorities Many interruptions, options and exceptions Have overlapping roles and responsibilities Involves Humans and organizations Vary from practice to practice Subject to time and resource pressures Pause the slides and view the videos below about healthcare complexity http: //www. youtube. com/watch? v=4 k. W 4 b. Ir. Yq. PY http: //www. youtube. com/profile? user=Saferhealthcare#p/u/4/jmh 4 FWapa 80 35
Pulling it all Together Clinical Workflow Impacts Patients • Problems, errors and delays are not just aggravating, inefficient or even infuriating • In medicine, more than in other fields, problems, errors and delays can kill people 36
Common Processes in Physician Practices • • • Appointment scheduling New patient intake Existing patient intake Exam and patient assessment Ordering labs/receiving & communicating results Prescriptions Referrals out/in Diagnostic testing Billing 37
Lab Process Example • • Locate the Lab Tests Ordering scenario doc file in content module As you read it, write down or highlight the following things: 1. 2. 3. 4. 5. Activities or steps in the process and their order, Roles or people that take part in the process, Where the steps are performed, Choices or decisions, and Information needs. Pause the slides until you finish the above requirements. 38
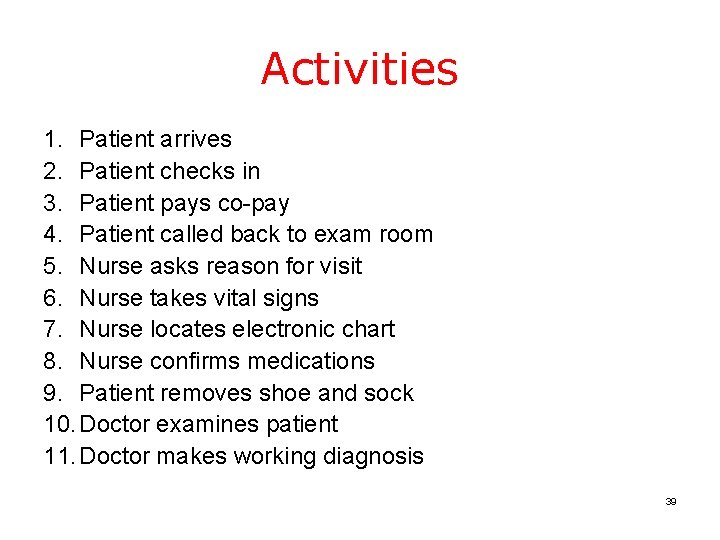
Activities 1. Patient arrives 2. Patient checks in 3. Patient pays co-pay 4. Patient called back to exam room 5. Nurse asks reason for visit 6. Nurse takes vital signs 7. Nurse locates electronic chart 8. Nurse confirms medications 9. Patient removes shoe and sock 10. Doctor examines patient 11. Doctor makes working diagnosis 39
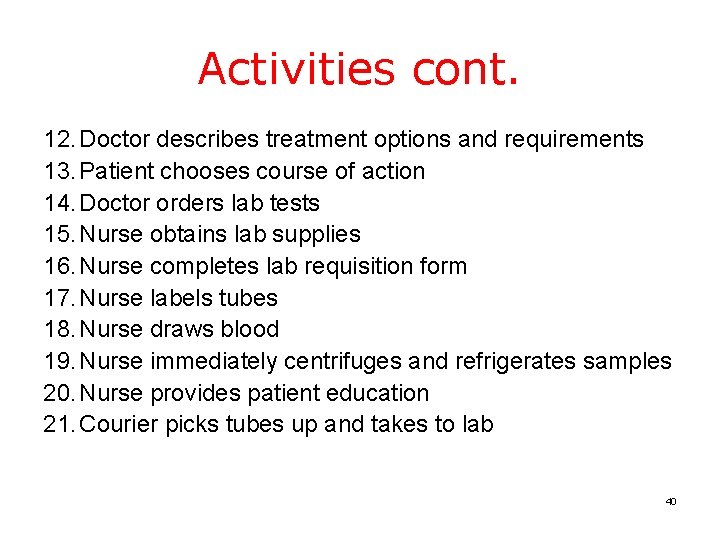
Activities cont. 12. Doctor describes treatment options and requirements 13. Patient chooses course of action 14. Doctor orders lab tests 15. Nurse obtains lab supplies 16. Nurse completes lab requisition form 17. Nurse labels tubes 18. Nurse draws blood 19. Nurse immediately centrifuges and refrigerates samples 20. Nurse provides patient education 21. Courier picks tubes up and takes to lab 40
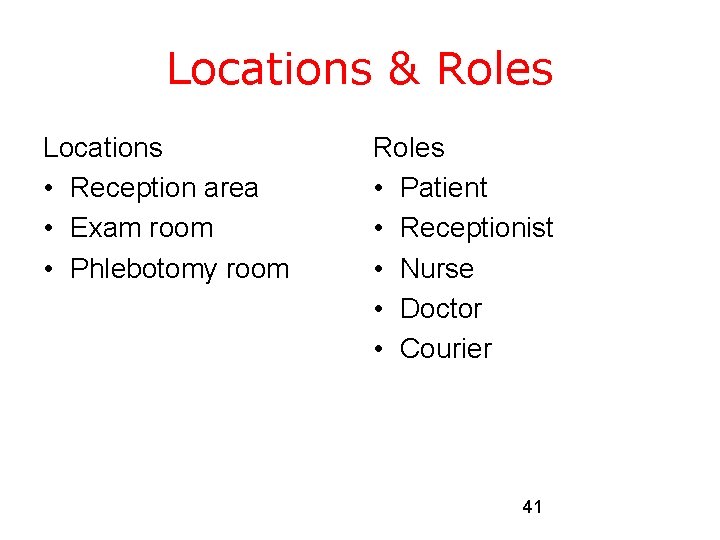
Locations & Roles Locations • Reception area • Exam room • Phlebotomy room Roles • Patient • Receptionist • Nurse • Doctor • Courier 41
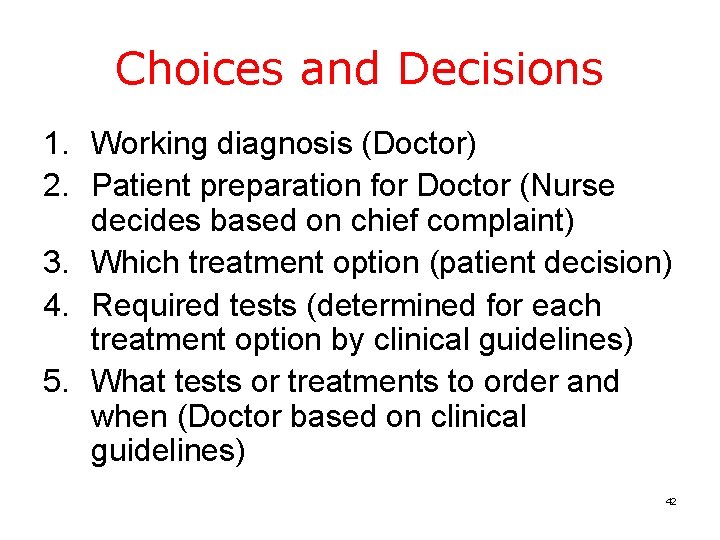
Choices and Decisions 1. Working diagnosis (Doctor) 2. Patient preparation for Doctor (Nurse decides based on chief complaint) 3. Which treatment option (patient decision) 4. Required tests (determined for each treatment option by clinical guidelines) 5. What tests or treatments to order and when (Doctor based on clinical guidelines) 42
Information Needs • Co-pay amount • Existing medications for medication reconciliation • Treatment options for working diagnosis • Required tests / follow-up for treatment options • Patient and provider identifiers for lab test requisition 43
Confusion about Workflow • Most people are not accustomed to thinking of what they do everyday in terms of workflow • Terms used in healthcare that may be confused with workflow or process analysis: – Regimented care – Clinical pathways, clinical guidelines – Accreditation and audit 44
Workflow Changes • Must first, do no harm • Must improve processes – Increase efficiency – Decrease delays and cost – Increase quality and safety – Improve the work environment – Improve ability to care for patients – Create a better overall patient experience 45
In Summary What a Workflow Analysis and Process Redesign Specialist Does • Document context and process so that it can be analyzed • Analyze process • Recommend redesign options • Implement redesign • Evaluate, adjust and maintain changes 46
Defect in Clinical Process http: //www. mehi. masstech. org/sites/mehi/files/documents/CPOE_Clinic al_Workflow_Analysis. pdf 47
Clinical process defect • Nonconformance to requirements or functional / program specification • A blemish, imperfection or deficiency that impairs worth or utility • The non-fulfillment of intended usage requirements • Any abnormality lowering the value of a product no matter why, when, or how it developed • An imperfection which, if great enough, can prevent an item from working properly or being usable • A lack of something necessary for completeness, adequacy, or perfection 48
Defects, Warranties, Guarantees, Remedies • Human mistakes are not just “oops” moments • Technology glitches are not just aggravating, inefficient or even infuriating • In business, if you fail→ you lose money • In engineering, if you fail → things don’t work • In medicine, if you fail → patients die 49
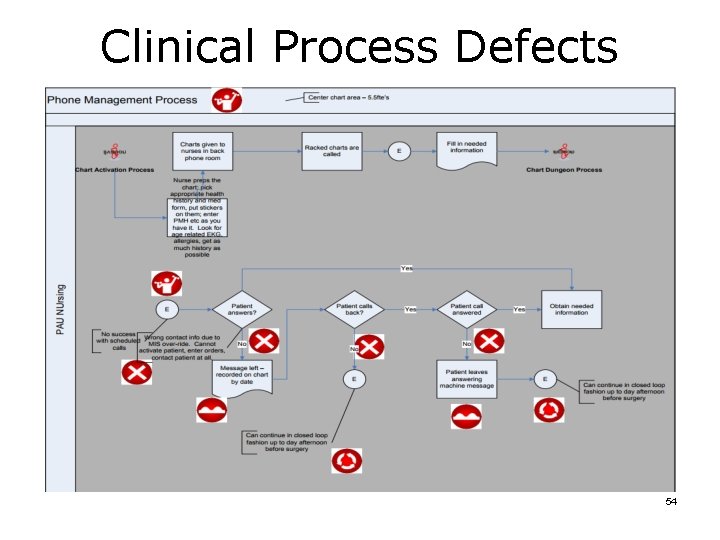
Clinical Process Defects • Not all errors kill people • However, the domino effect in clinical care is significant • Inefficiencies, redundancies, bottlenecks, errors – – – Slow down processes and progress Impede task completion Reduce quality of care Result in “unintended consequences” Facilitate poor outcomes • None of these are desirable when life hangs in the balance. • Life ALWAYS hangs in the balance in healthcare – sometimes obviously, sometimes subtly 50
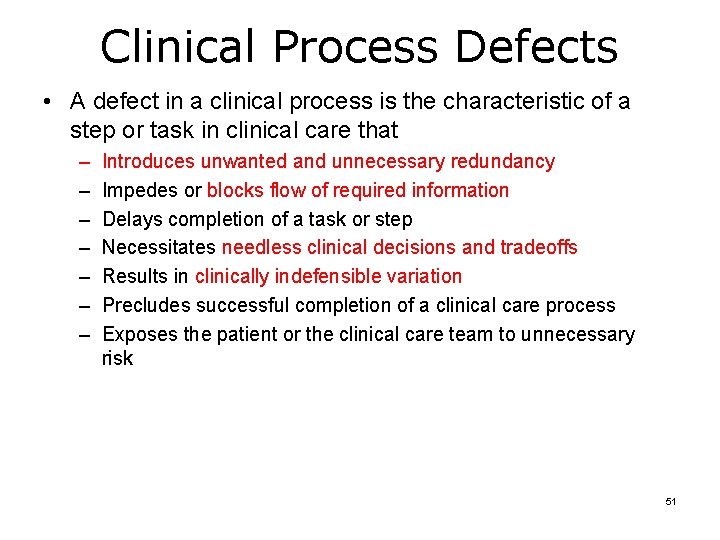
Clinical Process Defects • A defect in a clinical process is the characteristic of a step or task in clinical care that – – – – Introduces unwanted and unnecessary redundancy Impedes or blocks flow of required information Delays completion of a task or step Necessitates needless clinical decisions and tradeoffs Results in clinically indefensible variation Precludes successful completion of a clinical care process Exposes the patient or the clinical care team to unnecessary risk 51
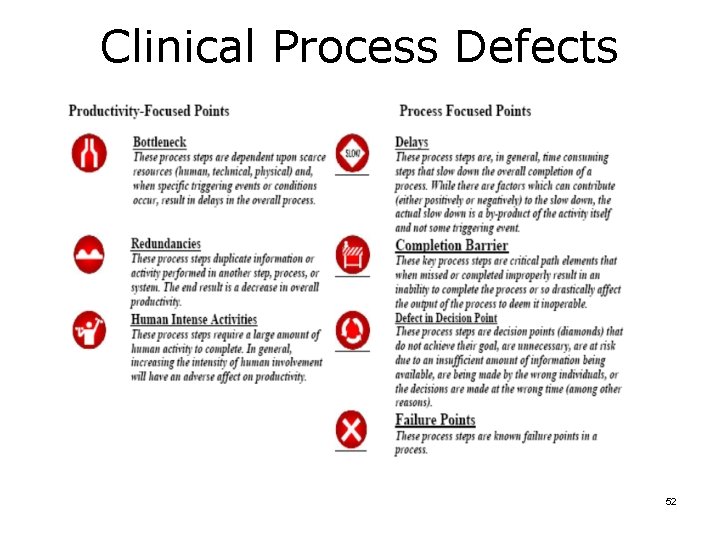
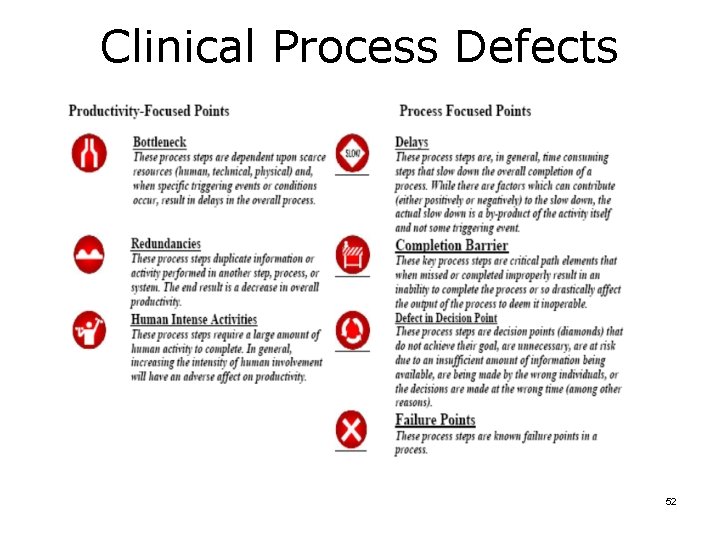
Clinical Process Defects 52
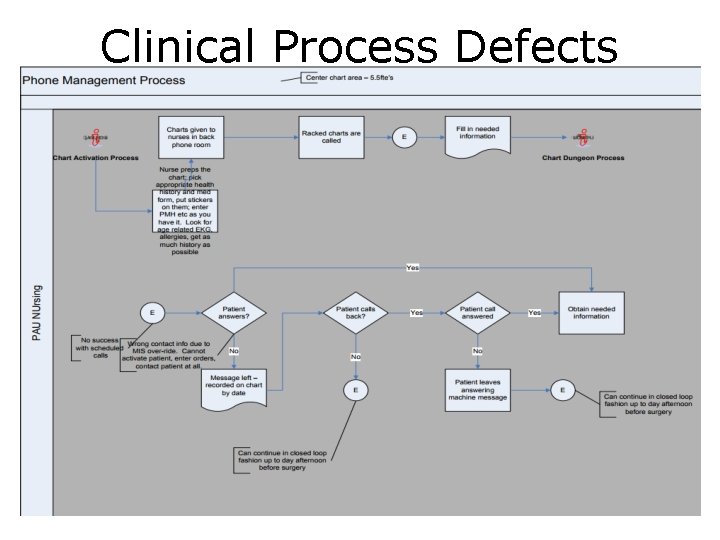
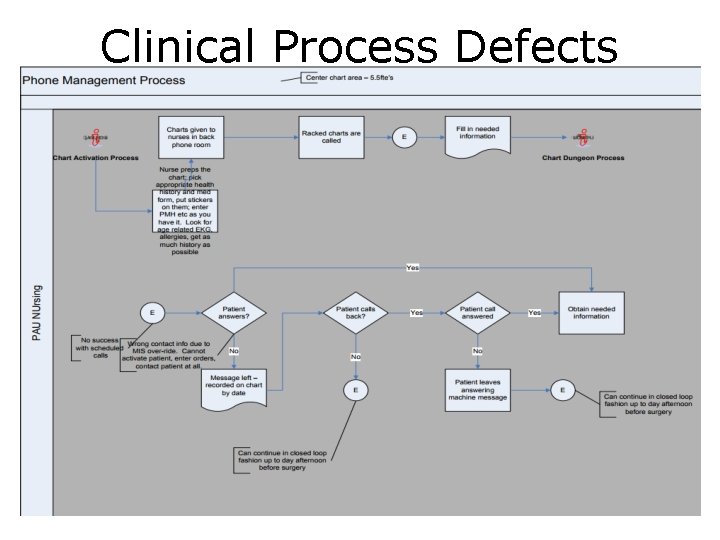
Clinical Process Defects 53
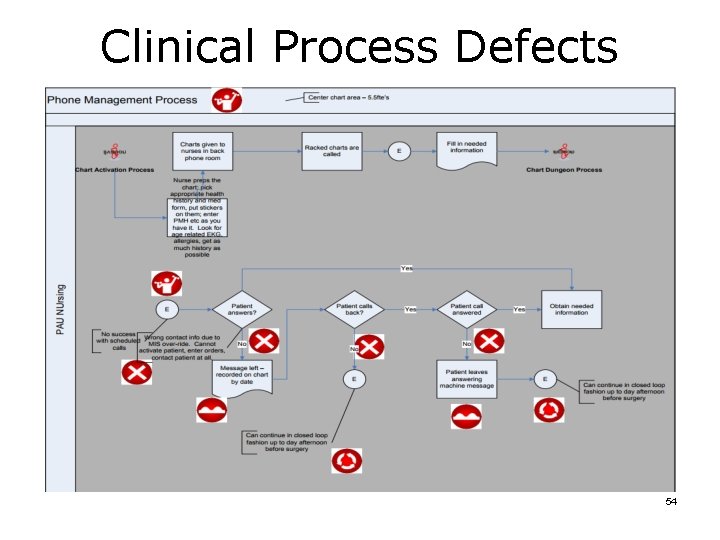
Clinical Process Defects 54
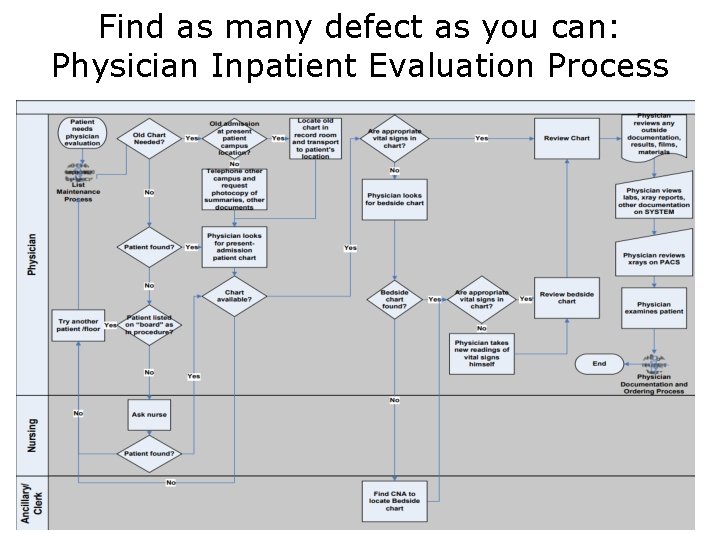
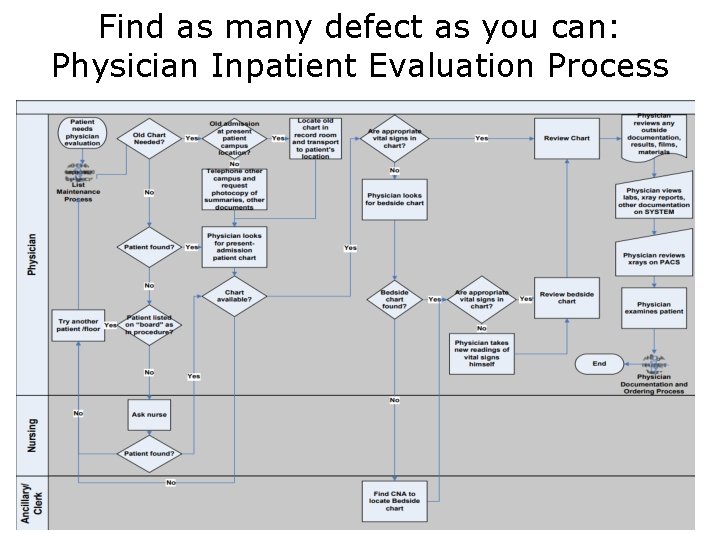
Find as many defect as you can: Physician Inpatient Evaluation Process 55
References • Approaches to Workflow Analysis in Healthcare Settings, by Barbara Sheehan, Suzanne Bakken, https: //www. ncbi. nlm. nih. gov/pmc/articles/PMC 3799136/pdf/amia_2012_ni_371. pdf • Clinical Process Defects, http: //www. mehi. masstech. org/sites/mehi/files/documents/CPOE_Clinical_Workflow_Anal ysis. pdf 56