CONCEPT Comfort Concept Definition A state of physical
- Slides: 67
CONCEPT: Comfort
Concept Definition A state of physical ease
Comfort Concept: Objectives • Explain the concept of comfort (including definition, antecedents, and attributes). • Analyze conditions which place a patient at risk for impaired comfort. • Identify when impaired comfort is developing or has developed. • Discuss exemplars of common disruptions of patient comfort. (Pain) • Apply the nursing process (including collaborative interventions) for individuals experiencing comfort imbalance.
Positive Consequences • Social interactions • Perform ADL’s • Adapt to stressors • Calm demeanor
Sub-Concepts of Comfort • Neuropathic pain • Chronic and Acute pain • Theory of pain control • Nociceptive Pain • Mixed Pain Syndromes
Neuropathic Pain • “Neuropathic pain results from the abnormal processing of sensory input by the nervous system as a result of damage to the brain, spinal cord, or peripheral nerve”. • Neuropathic pain is pathologic. • Postherpetic neuralgia, diabetic neuropathy, phantom pain, and post stroke pain syndrome • Burning, sharp, or shooting
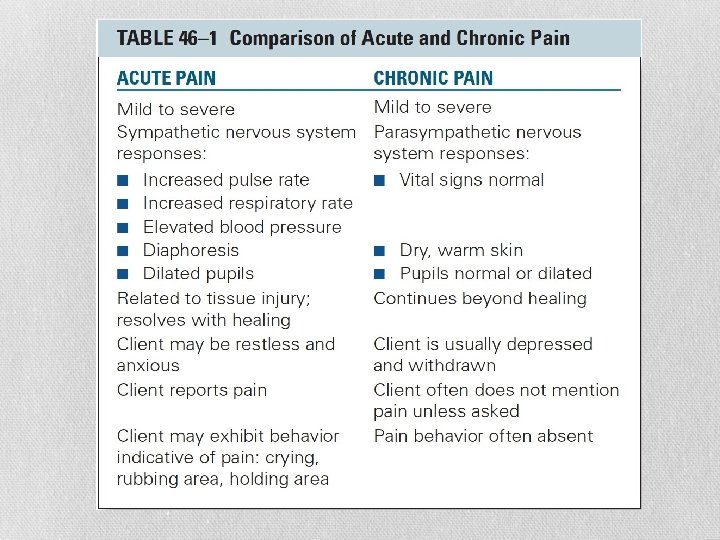
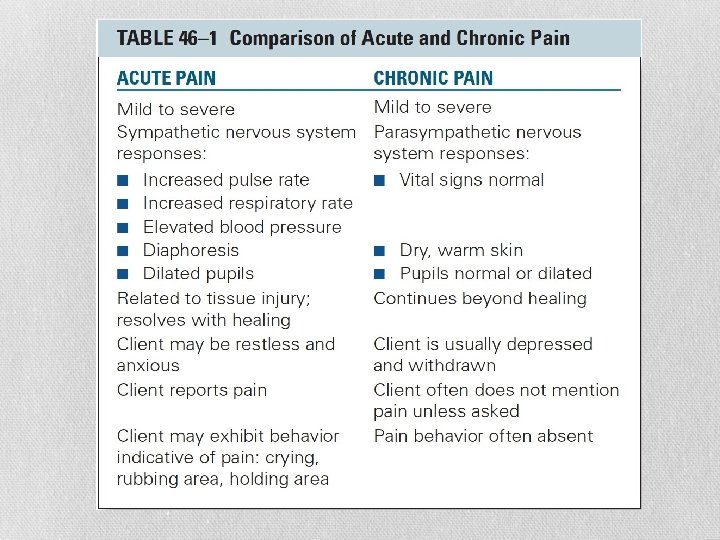
Acute and Chronic Pain • Acute pain-usually short lived • Chronic pain-cancer, osteoarthritis, pain from an underlying medical condition, may last a lifetime • Acute and Chronic pain combination
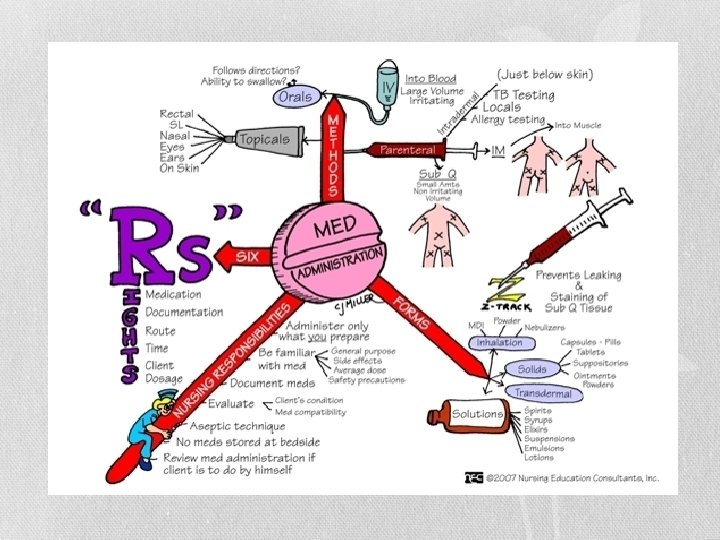
Pain Control • Pharmacologic Strategies • Oral medications • Intravenous medications • Epidural analgesia • Patient-controlled analgesia • Local anesthesia
Federal Drug Classification Schedules With the Controlled Substances Act of 1970, a major illegal substance control campaign began. Americans have witnessed a corresponding shift of resources and public attention onto the growing problem of substance abuse and its effects on society. • Schedule I (a) The drug or other substance has a high potential for abuse. (b) The drug or other substance has no currently accepted medical use in treatment in the United States. (c) There is a lack of accepted safety for use of the drug or other substance under medical supervision.
Federal Drug Classification Schedules • Schedule II (a) The drug or other substance has a high potential for abuse. (b) The drug or other substance has a currently accepted medical use in treatment in the United States or a currently accepted medical use with severe restrictions. (c) Abuse of the drug or other substances may lead to severe psychological or physical dependence.
Federal Drug Classification Schedules • Schedule III (a) The drug or other substance has a potential for abuse less than the drugs or other substances in schedules I and II. (b) The drug or other substance has a currently accepted medical use in treatment in the United States. (c) Abuse of the drug or other substance may lead to moderate or low physical dependence or high psychological dependence.
Federal Drug Classification Schedules • Schedule IV (a) The drug or other substance has a low potential for abuse relative to the drugs or other substances in schedule III. (b) The drug or other substance has a currently accepted medical use in treatment in the United States. (c) Abuse of the drug or other substance may lead to limited physical dependence or psychological dependence relative to the drugs or other substances in schedule III.
Federal Drug Classification Schedules • Schedule V (A) The drug or other substance has a low potential for abuse relative to the drugs or other substances in schedule IV. (B) The drug or other substance has a currently accepted medical use in treatment in the United States. (C) Abuse of the drug or other substance may lead to limited physical dependence or psychological dependence relative to the drugs or other substances in schedule IV.
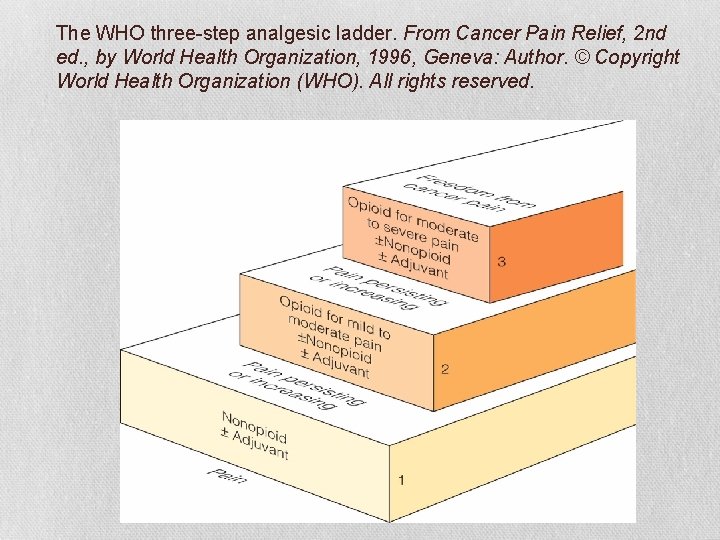
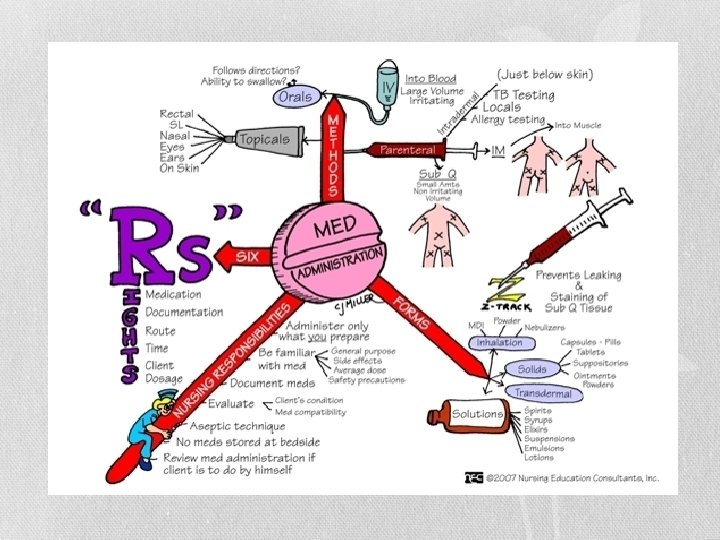
Implementing: Pharmacologic Interventions • Opioids (narcotics) • Nonopioids/nonsteroidal anti-inflammatory drugs (NSAIDS) • Co-analgesic drugs • WHO 3 -step analgesic ladder
WHO Ladder Step • Step 1 • For clients with mild pain (1 - 3 on a 0 - 10 scale) • Use nonopioid analgesics (with or without a coanalgesic)
WHO Ladder Step (cont’d) • Step 2 • For client with mild pain that persists or increases • Pain is moderate (4 - 6 on a 0 - 10 scale) • Use of a weak opioid (e. g. , codeine, tramadol, pentazocine) or a combination of opioid and nonopioid medicine (oxycodone with acetaminophen, hydrocodone with ibuprofen)
WHO Ladder Step (cont’d) • Step 3 • Client with moderate pain that persists or increases or with severe pain • Pain is severe (7 - 10 on a 0 - 10 scale) • Strong opioids (e. g. , morphine, hydromorphone, fentanyl)
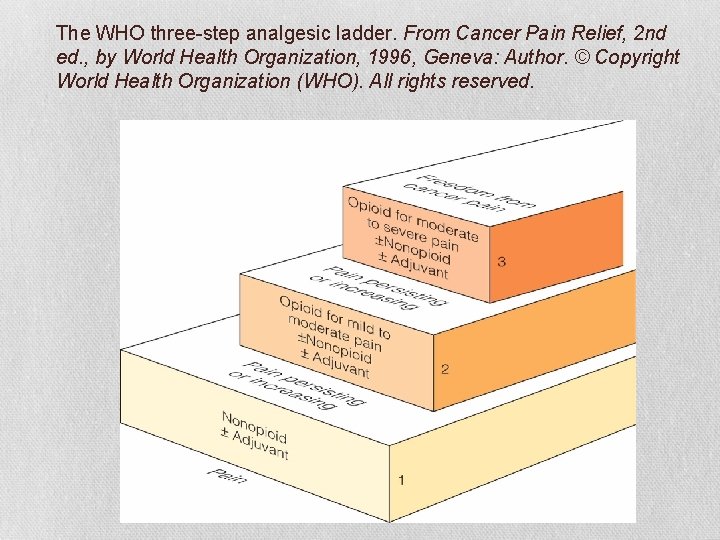
The WHO three-step analgesic ladder. From Cancer Pain Relief, 2 nd ed. , by World Health Organization, 1996, Geneva: Author. © Copyright World Health Organization (WHO). All rights reserved.
Nonopioid Analgesics Warnings: • Acetaminophen • • • (potentially lethal drug with taken in overdose amounts. Can cause hepatic toxicity) NSAIDs • cardiovascular risk (thrombotic events, myocardial infarction, and stroke • Do not use perioperative of coronary artery bypass graft surgery)
Nonopioid Analgesics NSAIDs-cont. gastrointestinal (increased risk of bleeding, ulceration, and perforation of the stomach and or intestines).
Nonopioid Analgesics • NSAID-includes aspirin, cyclo-oxygenase-2 inhibitors(Celebrex), Ibuprofen (Motrin, Advil) Aleve, many others. • commonly used for management of pain associated with arthritis because of the antiinflammatory and analgesic effects • Acetaminophen-(Tylenol)most widely used nonopioid analgesic • most commonly used for fever and mild to moderate pain. • Tramadol Hydrochloride-Ultram
Nonopioids/NSAIDS • Vary little in analgesic potency but do vary in anti-inflammatory effects, metabolism, excretion, and side effects • Have a ceiling effect • Increasing a dose beyond an upper limit, provides no greater analgesia • They do not produce tolerance or physical dependence • Many are available without prescription
Nonopioids/NSAIDS • Narrow therapeutic index • Not much margin for safety between the dose that produces a desired effect and the dose that may produce a toxic even lethal effect • Most common side effect GI • Effective for mild to moderate pain • Often used in conjunction with opioid because they allow for effective pain relief using lower opioid doses • Examples are acetaminophen, ibuprofen, aspirin, naproxen
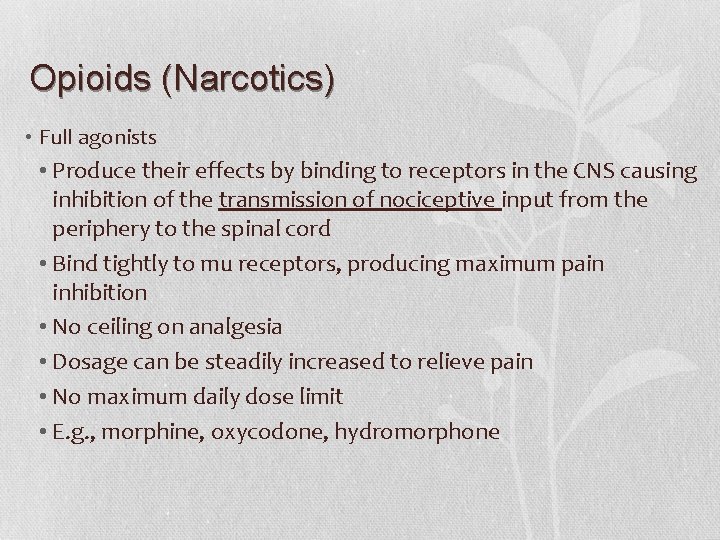
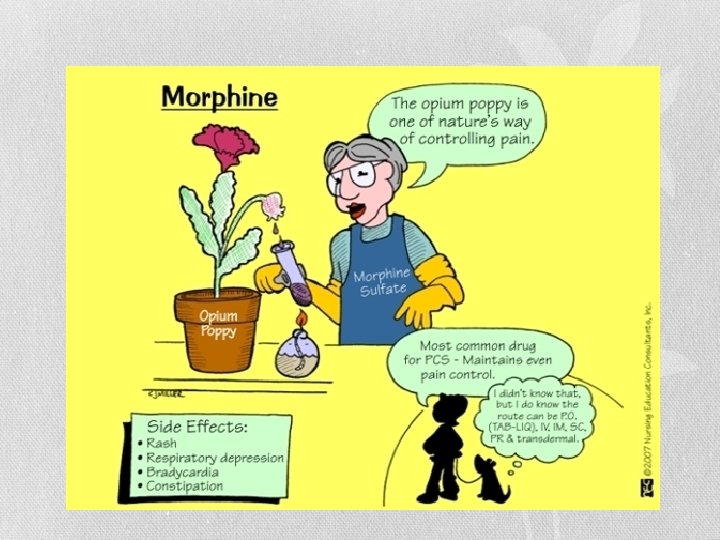
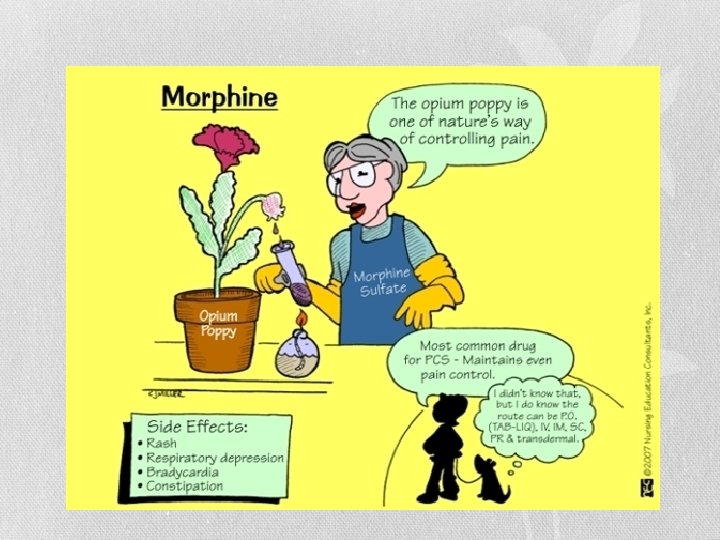
Opioids (Narcotics) • Full agonists • Produce their effects by binding to receptors in the CNS causing inhibition of the transmission of nociceptive input from the periphery to the spinal cord • Bind tightly to mu receptors, producing maximum pain inhibition • No ceiling on analgesia • Dosage can be steadily increased to relieve pain • No maximum daily dose limit • E. g. , morphine, oxycodone, hydromorphone
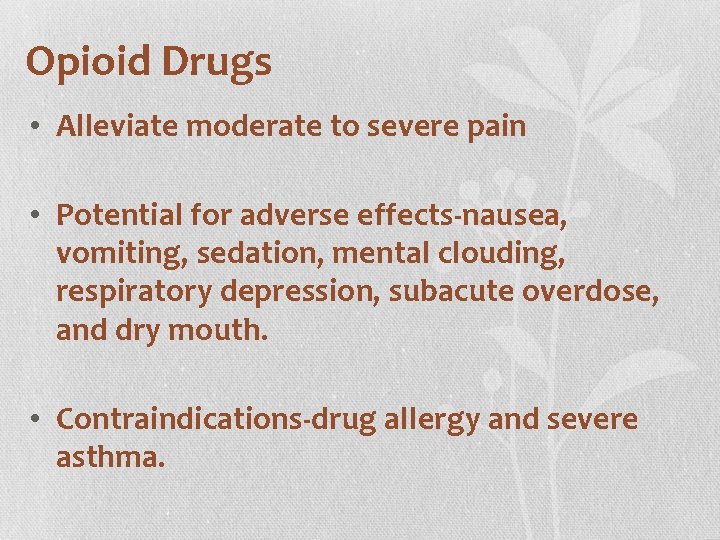
Opioid Drugs • Alleviate moderate to severe pain • Potential for adverse effects-nausea, vomiting, sedation, mental clouding, respiratory depression, subacute overdose, and dry mouth. • Contraindications-drug allergy and severe asthma.
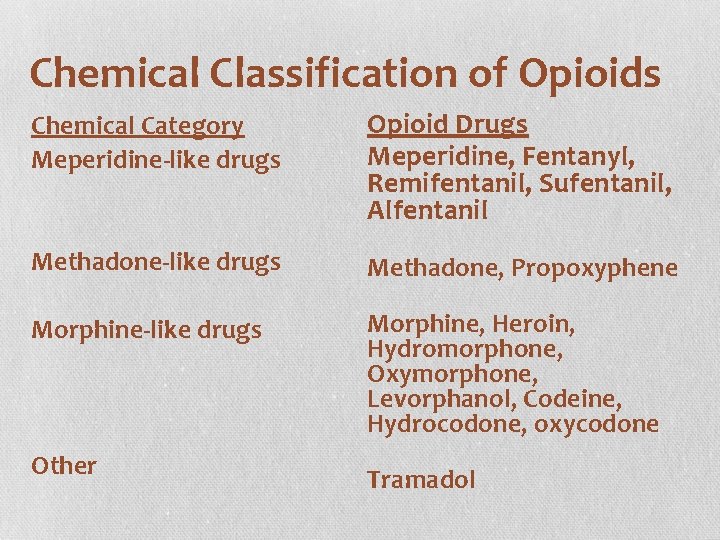
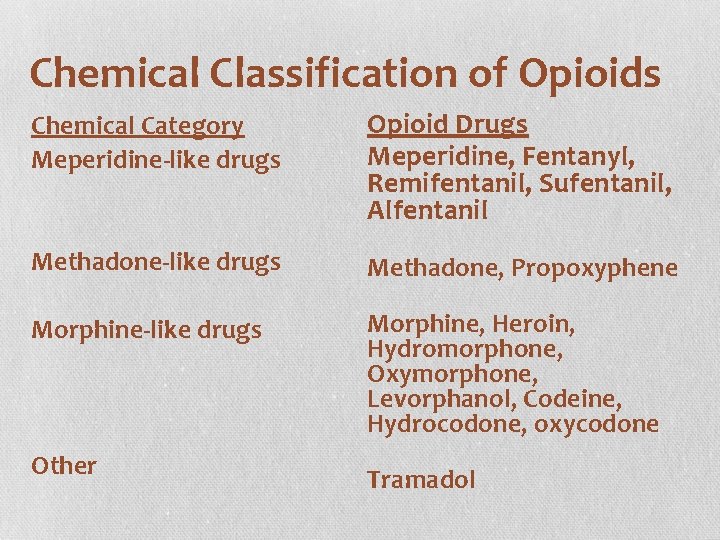
Chemical Classification of Opioids Chemical Category Meperidine-like drugs Opioid Drugs Meperidine, Fentanyl, Remifentanil, Sufentanil, Alfentanil Methadone-like drugs Methadone, Propoxyphene Morphine-like drugs Morphine, Heroin, Hydromorphone, Oxymorphone, Levorphanol, Codeine, Hydrocodone, oxycodone Other Tramadol
Pain Control • Nonpharmacologic Strategies • Massage • Splinting • Relaxation and guided imagery • Distraction • TENS • Counterirritation • Nutrition • Physical Therapy
Pain Theory-Pattern Specificity Theory • Von Frey (1895) • Certain pain receptors are stimulated by specific stimuli • Does not take into account tolerance to pain • Does not taken into account psychological components of pain Smith, S. F. , Duell, D. J. , & Martin, B. C. (2012). Clinical nursing skills (8 th ed. ) Retrieved from Skyscape.
Pain Theory-Pattern Theory • Goldschneider (1920) • Pain originates in the dorsal horn of the spinal cord • Specific pain sensory reacts with intense receptor stimulation • Does not taken into account psychological components of pain Smith, S. F. , Duell, D. J. , & Martin, B. C. (2012). Clinical nursing skills (8 th ed. ) Retrieved from Skyscape.
Pain Theory-Pattern Gate-Control Theory • Melzack • Transmission of neurologic impulses • Gate mechanisms along the spinal cord control the transmission of pain • If the gate is open the pain impulse is experienced • If the gate is closed the pain impulse is not experienced • Smith, S. F. , Duell, D. J. , & Martin, B. C. (2012). Clinical nursing skills (8 th ed. ) Retrieved from Skyscape.
Nociceptive Pain • “Refers to the normal functioning of physiologic systems that leads to the perception of noxious stimuli (tissue injury) as being painful” • Normal pain transmission • Surgery, trauma, burns, and tumor growth • Aching, cramping, or throbbing • Giddens, J. F. (2013). Concepts for nursing practice. Pain (pp. 270 -279). St. Louis, Mo: Mosby.
Mixed Pain Syndromes • “Unique with multiple underlying and poorly understood mechanisms” • Fibromyalgia, some low back pain, and myofascial pain • Giddens, J. F. (2013). Concepts for nursing practice. Pain (pp. 270 -279). St. Louis, Mo: Mosby.
Antecedents for Comfort • Effective circulatory system • Able to discern from comfort to discomfort • Without noxious stimuli • Intact neurological/sensory system
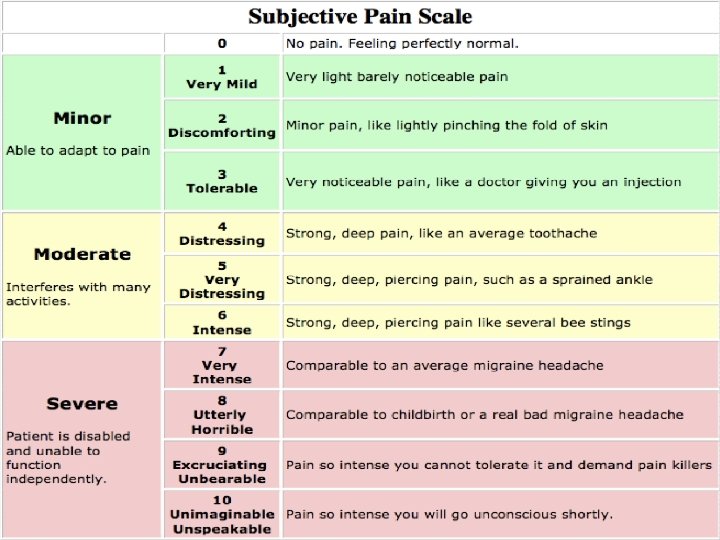
How will knowing the Antecendents affect your Nursing Assessment? -use of open ended questions -use of pain scale -ability to assess patient’s comfort level -ability to assess patient’s ability to distinguish between comfort and discomfort
Risk Factors • All populations with increased risk for older adults, neonates, and persons unable to report pain.
Comfort Imbalance-Assessment How does the nurse know when there is an imbalance in comfort? • Comprehensive History • Physical & Psychological • Diagnostic Test(s)
Comprehensive History • Assessment of comfort/discomfort • triggers, • location of pain, • numeric rating scale, • intensity of pain, • quality of pain, • onset and duration of pain, • alleviating and relieving factors, • effect of pain on function and quality of life
Assessment • Location(s) of pain: • Intensity: • Quality: • Onset and duration: • Alleviating and relieving factors: • Effect of pain on function and quality of life: • Comfort-function (pain) goal • Pain history • Vital signs
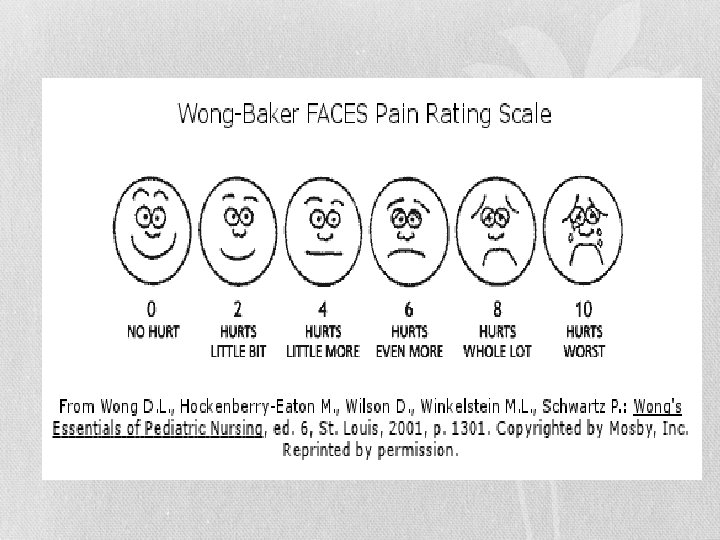
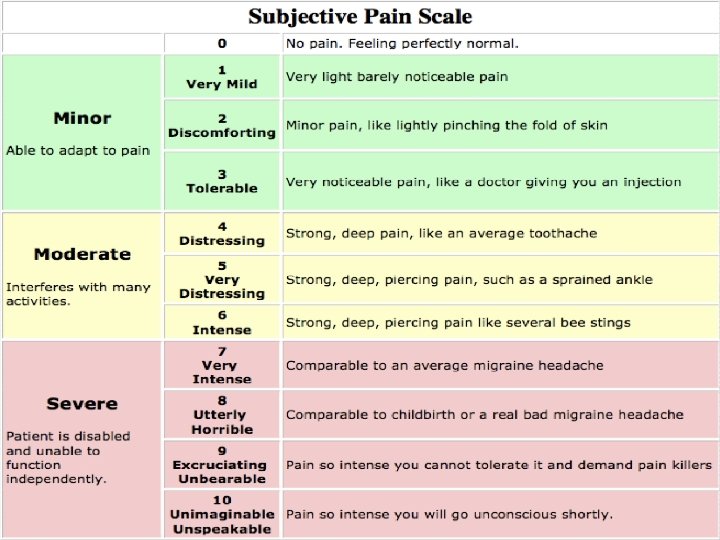
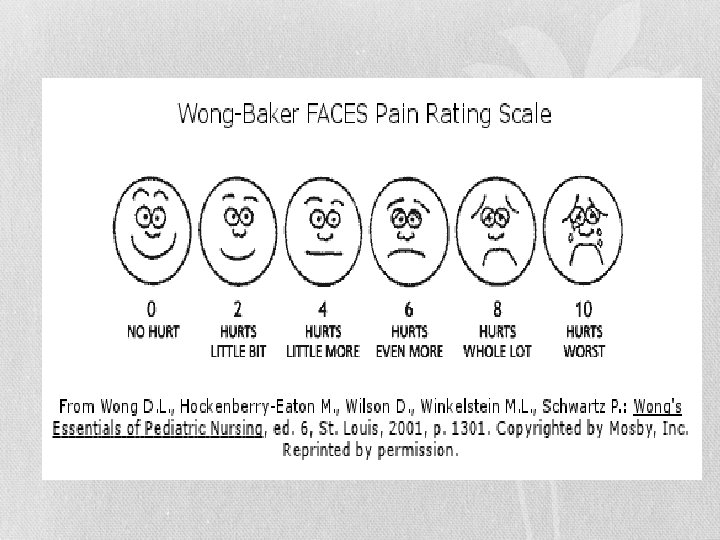
Measurement of Comfort • Pain assessment: • COMFORT Scale • CRIES Pain Scale • FLACC Scale • Wong-Baker Faces Pain Rating Scale • 0 -10 Numeric Rating Scale • Checklist of Nonverbal Indicators • Oucher Pain Scale • FPS-R (Faces Pain Scale, Revised) • Payen Behavioral Pain Scale
Monahan, Neighbors, & Green (2011) found the following: • Select a Pain Intensity Rating Scale appropriate to patient and use it consistently to ensure comparability of assessments • Numeric rating scales (NRSs) of 0 (no pain) to 10 (worst possible pain) and descriptive scales (no pain, mild pain, moderate pain, severe pain, very severe pain, worst possible pain) are used commonly to assess intensity in adults who are cognitively intact
Monahan, Neighbors, & Green (2011) found the following: • The Faces pain scale (Kim and Buschmann, 2006) is an alternative that may best meet the needs of older adults (Taylor and Herr, 2001) • The Pain Assessment in Advanced Dementia (PAINAD) scale based on vocalizations, facial grimacing, bracing, rubbing, and restlessness has a pain intensity rating that can be converted to a numeric equivalent (D'Arcy, 2007) • The Payen Behavioral Pain scale (BPS) contains an assessment of compliance with ventilation and is used for critically ill, intubated patients (D'Arcy, 2007). (p. 14)
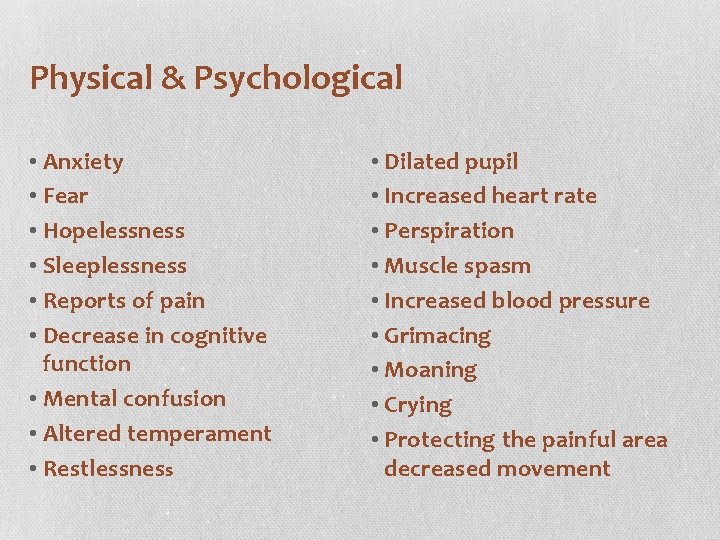
Physical & Psychological • ,
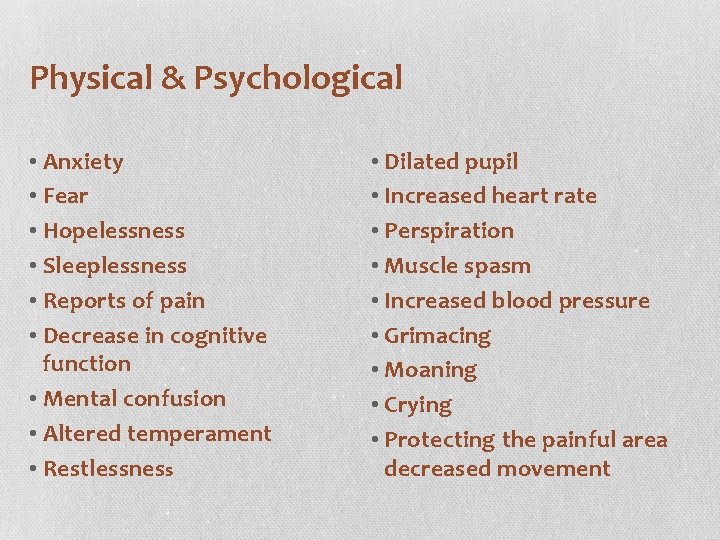
Physical & Psychological • Anxiety • Fear • Hopelessness • Sleeplessness • Reports of pain • Decrease in cognitive function • Mental confusion • Altered temperament • Restlessness • Dilated pupil • Increased heart rate • Perspiration • Muscle spasm • Increased blood pressure • Grimacing • Moaning • Crying • Protecting the painful area decreased movement
Diagnostic Test(s) • Vital Signs • Pain Scale • Laboratory studies • Diagnostic studies
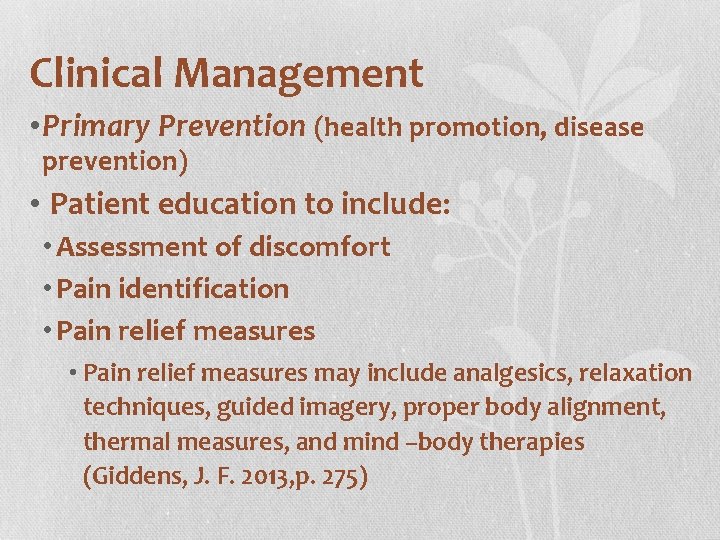
Clinical Management • Primary Prevention (health promotion, disease prevention) • Patient education to include: • Assessment of discomfort • Pain identification • Pain relief measures may include analgesics, relaxation techniques, guided imagery, proper body alignment, thermal measures, and mind –body therapies (Giddens, J. F. 2013, p. 275)
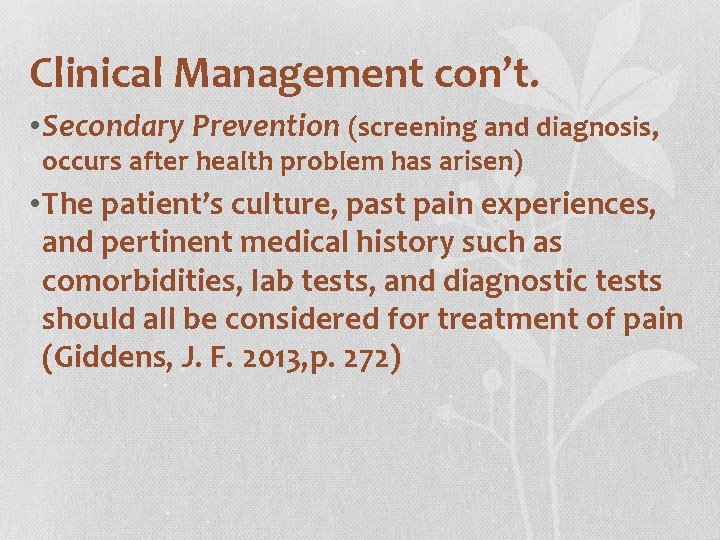
Clinical Management con’t. • Secondary Prevention (screening and diagnosis, occurs after health problem has arisen) • The patient’s culture, past pain experiences, and pertinent medical history such as comorbidities, lab tests, and diagnostic tests should all be considered for treatment of pain (Giddens, J. F. 2013, p. 272)
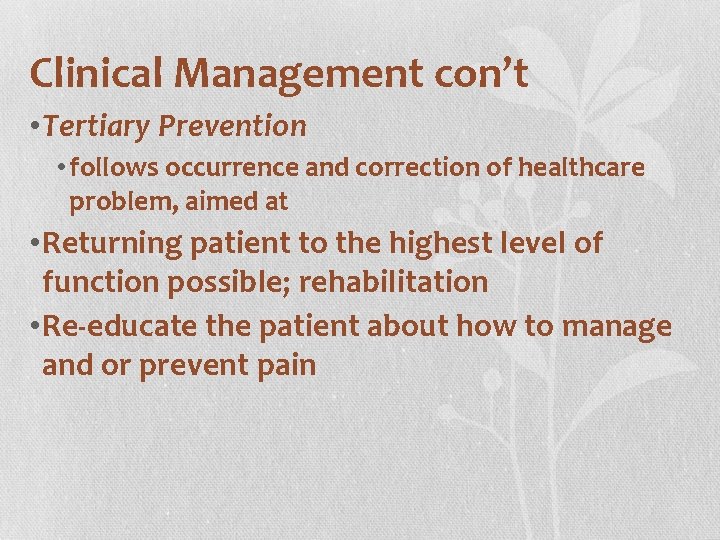
Clinical Management con’t • Tertiary Prevention • follows occurrence and correction of healthcare problem, aimed at • Returning patient to the highest level of function possible; rehabilitation • Re-educate the patient about how to manage and or prevent pain
Clinical Management con’t • Educate the patient about how to learn to modify his or her reaction to pain • Rehabilitative efforts to encourage the patient to follow analgesic schedule, physical therapy, nutritional suggestions, and or other pain relief strategies
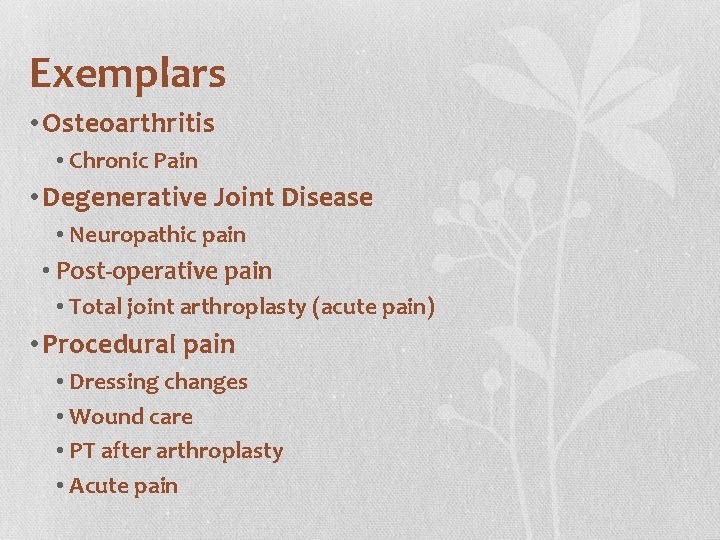
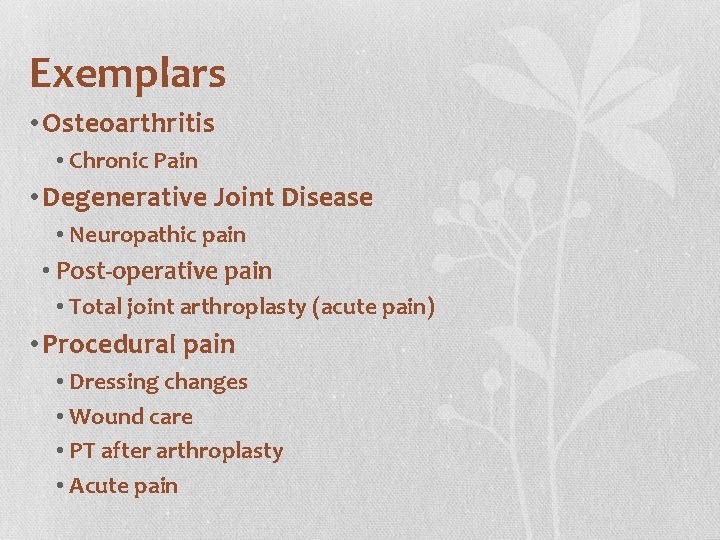
Exemplars • Osteoarthritis • Chronic Pain • Degenerative Joint Disease • Neuropathic pain • Post-operative pain • Total joint arthroplasty (acute pain) • Procedural pain • Dressing changes • Wound care • PT after arthroplasty • Acute pain
Pre-procedure pain • Potential pain and or actual pain prior to a procedure
Pre-procedure pain • Nursing interventions: • Assess location, onset, duration, and factors that increase pain and or reduce pain • Use a pain scale to assess pain for comparison to patients pain pre-procedure and post procedure • Assess vital signs
Pre-procedure pain • Nursing interventions: • Assess for drug allergies • Treat pain or expected pain with analgesics prior to procedure (before physical therapy, before a dressing change) • Provide patient education about requesting pain medication, request prior to procedure, understand action and effects of the medication
Pre-procedure pain • Diagnostic studies • to find the causative factor in pre-procedure pain • Culture • to identify the offending organism • Platelet count • if any bleeding is present • Vital signs • assess for changes in vital signs and the correlation to increased pain
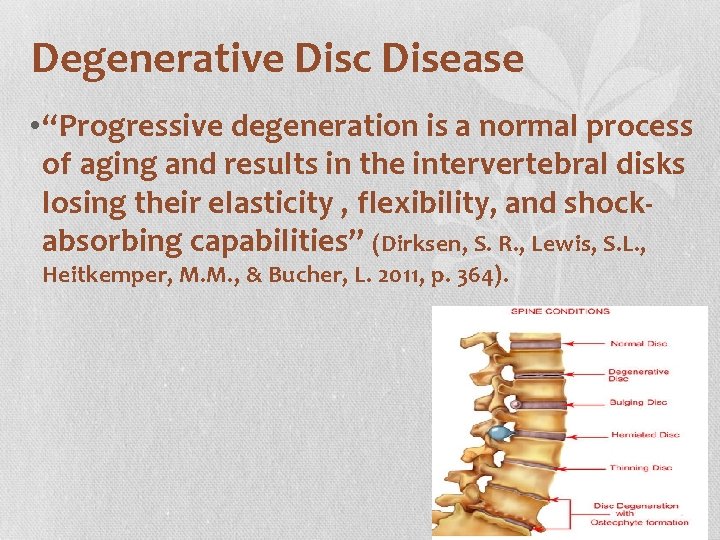
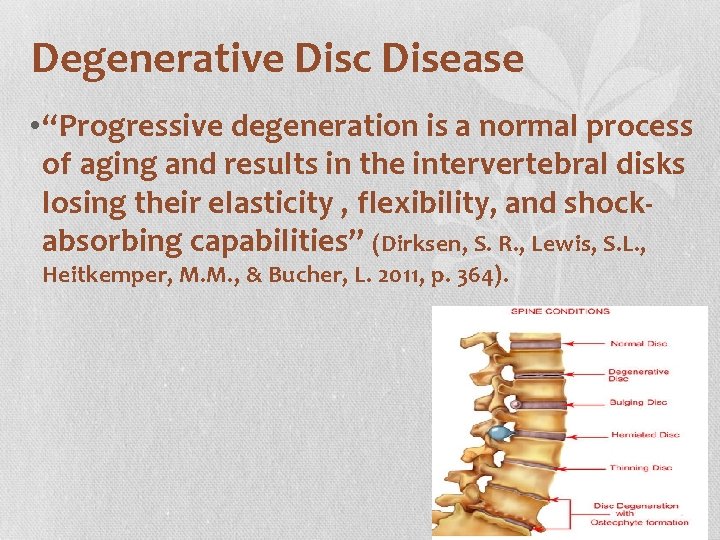
Degenerative Disc Disease • “Progressive degeneration is a normal process of aging and results in the intervertebral disks losing their elasticity , flexibility, and shockabsorbing capabilities” (Dirksen, S. R. , Lewis, S. L. , Heitkemper, M. M. , & Bucher, L. 2011, p. 364).
Degenerative Disc Disease • Nursing interventions: • Assess location, onset, duration, and factors that increase pain and or reduce pain • Use a pain scale to assess pain • Assess vital signs • Assess for drug allergies • Administer prescribed analgesics • Provide rest , heat and or cold therapies • Patient education about exercise and weight control
painconsortium. nih. gov/pain scales • painconsortium. nih. gov/pain_scales/FLACCScale. pdf • painconsortium. nih. gov/pain_scales/Numeric. Rating. Scale. pdf • painconsortium. nih. gov/pain_scales/COMFORT_Scale. pdf • painconsortium. nih. gov/pain_scales/CRIESPain. Scale. pdf • painconsortium. nih. gov/pain_scales/Wong-Baker_Faces. pdf • painconsortium. nih. gov/pain_scales/Checklistof. Nonverbal. pdf
Resources • http: //www. oucher. org/the_scales. html • http: //consultgerirn. org/uploads/File/trythis/try_this _d 2. pdf • http: //www. iasppain. org/Content/Navigation. Menu/General. Resource Links/Faces. Pain. Scale. Revised/default. htm
References Ackley, B. , & Ladwig, G. (n. d. ). Nursing Diagnosis Handbook. Retrieved from Skyscape. Ankner, G. M. (2012). Clinical decision making: Case studies in medical-surgical nursing (2 nd ed. ). Cengage Learning. Giddens, J. F. (2013). Concepts for nursing practice. Pain (pp. 270 - 279). St. Louis, Mo: Mosby. Lilley, L. L. , Harrington, S. , & Snyder, J. S. (2007). Pharmacology and the nursing process (5 th ed. ). St. Louis, MO: Mosby/Elsevier Lynn, P. (2011). Taylor’s clinical nursing skills: A nursing process approach. Comfort (3 rd ed. , pp. 521 -560). Philadelphia, PA: Lippincott Williams & Wilkins.
References Monahan, F. D. , Neighbors, M. , & Green, C. J. (2011). Manual of medical-surgical nursing (7 th ed. ). Maryland Heights, MO: Elsevier/Mosby. Smith, S. F. , Duell, D. J. , & Martin, B. C. (2012). Clinical nursing skills (8 th ed. ) Retrieved from Skyscape. Weber, J. (2010). Nurses’ handbook of health assessment (7 th ed. ). Retrieved from Skyscape.
A state of physical ease