Concept Basic Fluid and Electrolyte Balance Exemplar Fluid
Concept: Basic Fluid and Electrolyte Balance Exemplar: Fluid and Electrolyte Balance and Imbalance Copyright © 2016, 2013, 2010, 2006, 2002 by Saunders, an imprint of Elsevier Inc.

Homeostasis Proper functioning of all body systems; requires fluid and electrolyte balance Ø Ø Extracellular fluid (ECF) Intracellular fluid (ICF) Interstitial fluid Transcellular fluids 2 Copyright © 2016, 2013, 2010, 2006, 2002 by Saunders, an imprint of Elsevier Inc. 2
3 Copyright © 2016, 2013, 2010, 2006, 2002 by Saunders, an imprint of Elsevier Inc.

Filtration Movement of fluid through cell or blood vessel membrane because of differences in water pressure (hydrostatic pressure) This is related to water volume pressing against confining walls 4 Copyright © 2016, 2013, 2010, 2006, 2002 by Saunders, an imprint of Elsevier Inc. 4
Hydrostatic Pressure “Water-pushing pressure” Force that pushes water outward from a confined space through a membrane Amount of water in any body fluid space determines pressure Example: Blood pressure Ø Moving whole blood from the heart to capillaries where filtration occurs to exchange water, nutrients, and waste products between the blood and tissues 5 Copyright © 2016, 2013, 2010, 2006, 2002 by Saunders, an imprint of Elsevier Inc. 5
Diffusion Free movement of particles (solute) across permeable membrane from area of higher to lower concentration Important in transport of most electrolytes; other particles diffuse through cell membranes Sodium pumps Glucose cannot enter most cell membranes without help of insulin 6 Copyright © 2016, 2013, 2010, 2006, 2002 by Saunders, an imprint of Elsevier Inc. 6
Osmosis & Filtration Act together at capillary membrane to maintain normal ECF and ICF volumes Thirst mechanism is example of how osmosis helps maintain homeostasis Feeling of thirst caused by activation of brain cells responding to changes in ECG osmolarity 7 Copyright © 2016, 2013, 2010, 2006, 2002 by Saunders, an imprint of Elsevier Inc. 7

Fluid Balance Closely linked to/affected by electrolyte concentrations Fluid intake Fluid loss Ø Ø Minimum urine amount needed to excrete toxic waste products = 400 to 600 m. L/day Insensible water loss – Through skin, lungs, stool 8 Copyright © 2016, 2013, 2010, 2006, 2002 by Saunders, an imprint of Elsevier Inc. 8
Hormonal Regulation of Fluid Balance Aldosterone Antidiuretic hormone Natriuretic peptides 9 Copyright © 2016, 2013, 2010, 2006, 2002 by Saunders, an imprint of Elsevier Inc. 9
Significance of Fluid Balance: Renin-Angiotensin II Pathway Blood (plasma) volume and intracellular fluid most important to keep in balance Kidneys are major regulator of water and sodium balance; maintain blood and perfusion pressure to all tissues/organs When the kidneys sense a low parameter, they secrete renin Renin-angiotensin II pathway is greatly stimulated with shock, or when stress response is stimulated 10 Copyright © 2016, 2013, 2010, 2006, 2002 by Saunders, an imprint of Elsevier Inc. 10
ACE Inhibitors Disrupt renin-angiotensin II pathway by reducing amount of ACE produced With less angiotensin II, less vasoconstriction and reduced peripheral resistance Greater excretion of water and sodium in urine By locking angiotensin II receptors, blood pressure lowers Patients with hypertension often take ACEinhibitor medications 11 Copyright © 2016, 2013, 2010, 2006, 2002 by Saunders, an imprint of Elsevier Inc. 11
Dehydration related to a car 12 Copyright © 2016, 2013, 2010, 2006, 2002 by Saunders, an imprint of Elsevier Inc.
Fluid and Electrolyte Imbalance Factors affecting ability to maintain balance Ø Ø Illness (burns, heart failure, sepsis, etc. ) Trauma, surgery Medications (Which ones? ) Result of therapeutic measures (IV fluid replacement) 13 Copyright © 2016, 2013, 2010, 2006, 2002 by Saunders, an imprint of Elsevier Inc.

Pathophysiology and Etiology, Third spacing Ø Ø Fluid shifts from vascular space to other area Trapped fluid = volume loss • Ø Ø Not available to support normal physiologic processes Often occurs in interstitial tissues Assessing extent of FVD difficult • No change in weight 14 Copyright © 2016, 2013, 2010, 2006, 2002 by Saunders, an imprint of Elsevier Inc.

Dehydration: Collaborative Care Fluid intake/retention does not meet body’s fluid needs; results in fluid volume deficit Assessment History Physical assessment/clinical manifestations: Ø Ø Ø Cardiovascular Respiratory Skin Neurologic Renal 15 Copyright © 2016, 2013, 2010, 2006, 2002 by Saunders, an imprint of Elsevier Inc. 15
Risk Factors for Dehydration Age Ø Older adults Physical changes • Lack of free access to fluids • Voluntary fluid restriction • Increased insensitive fluid losses • Ø Children • Higher body surface area and metabolic rate Pregnancy 16 Copyright © 2016, 2013, 2010, 2006, 2002 by Saunders, an imprint of Elsevier Inc.
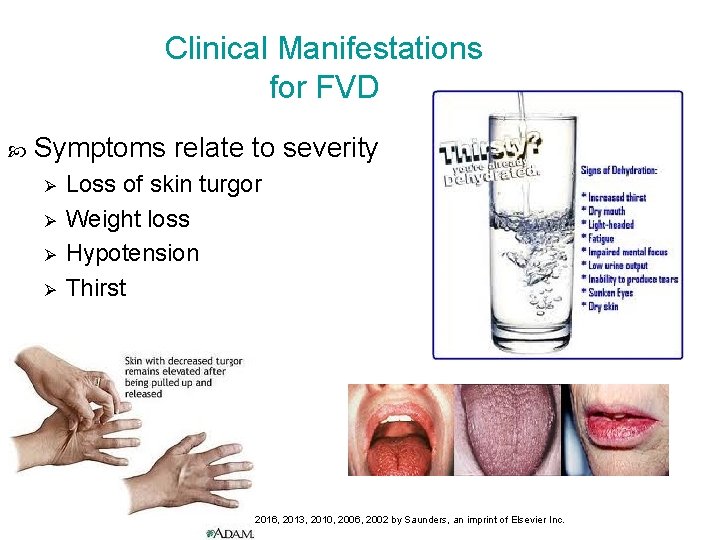
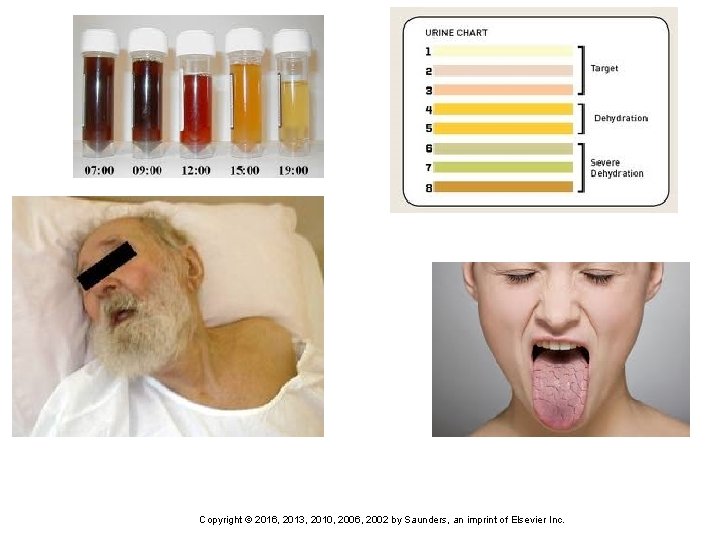
Clinical Manifestations for FVD Symptoms relate to severity Ø Ø Loss of skin turgor Weight loss Hypotension Thirst 17 Copyright © 2016, 2013, 2010, 2006, 2002 by Saunders, an imprint of Elsevier Inc.
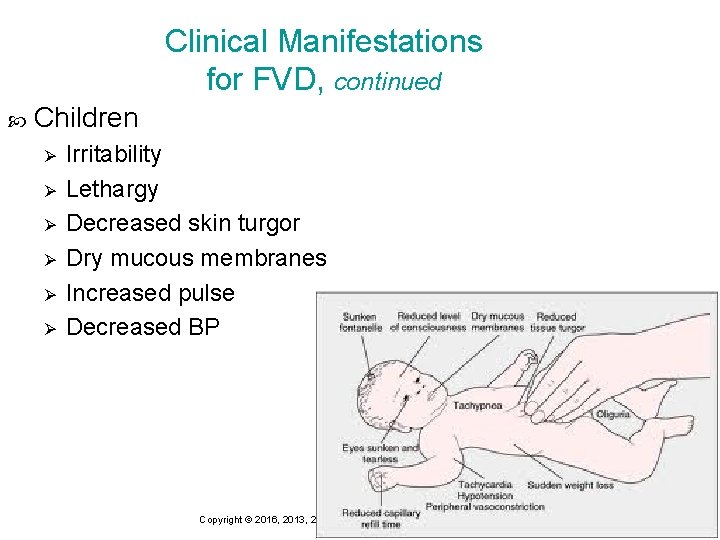
Clinical Manifestations for FVD, continued Children Ø Ø Ø Irritability Lethargy Decreased skin turgor Dry mucous membranes Increased pulse Decreased BP 18 Copyright © 2016, 2013, 2010, 2006, 2002 by Saunders, an imprint of Elsevier Inc.
Clinical Manifestations for FVD, continued Older adults Ø Ø Ø Altered mental status Lack of attention Decreased memory Itchy skin Brittle hair 19 Copyright © 2016, 2013, 2010, 2006, 2002 by Saunders, an imprint of Elsevier Inc.
Collaboration Diagnostic tests (What abnormals would you expect to see? ) Ø Ø Ø CBC Serum electrolyte panel BUN and creatinine Urine specific gravity Serum osmolality Clinical therapies Ø Ø Oral rehydration Intravenous fluids 20 Copyright © 2016, 2013, 2010, 2006, 2002 by Saunders, an imprint of Elsevier Inc.
Implementation Accurate I & O Ø Weigh daily Ø When should you report decreased urine output? 1 kg of weight=increase of 1 L of fluid OR 1 lb of weight=increase of 450 m. L of fluid Vital signs (at least every 4 hrs) Ø Ø Ø Check orthostatics (why? ) Remember blood pressure is related to the amount of blood the heart pumps. Fluid volume affects the amount of blood to the heart; therefore assessing blood pressure also assesses a patient’s fluid status Copyright © 2016, 2013, 2010, 2006, 2002 by Saunders, an imprint of Elsevier Inc. 21
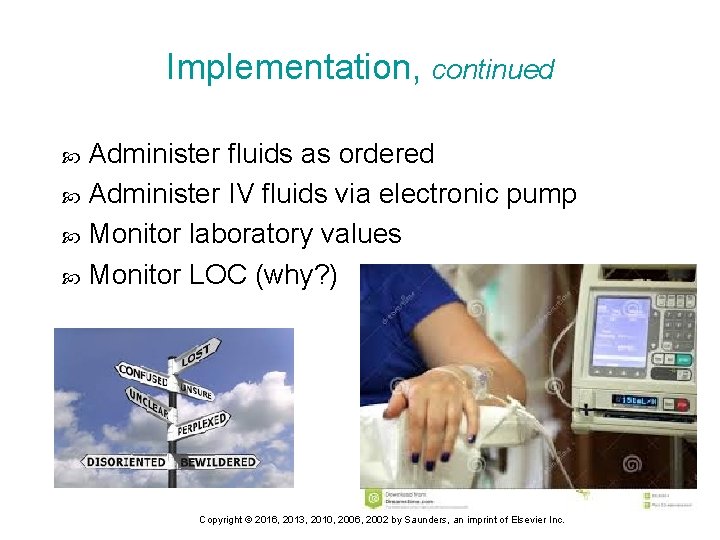
Implementation, continued Administer fluids as ordered Administer IV fluids via electronic pump Monitor laboratory values Monitor LOC (why? ) 22 Copyright © 2016, 2013, 2010, 2006, 2002 by Saunders, an imprint of Elsevier Inc.
Implementation, continued Reposition every 2 hours (why? ) Institute fall precautions (are they at greater risk? ) Listen to patient’s concerns Answer questions Respect cultural differences Teach Ø Ø Prevention of orthostatic hypotension (what are some strategies? ) Maintaining fluid intake Prevention of fluid deficit The hydrant Copyright © 2016, 2013, 2010, 2006, 2002 by Saunders, an imprint of Elsevier Inc. 23
24 Copyright © 2016, 2013, 2010, 2006, 2002 by Saunders, an imprint of Elsevier Inc.
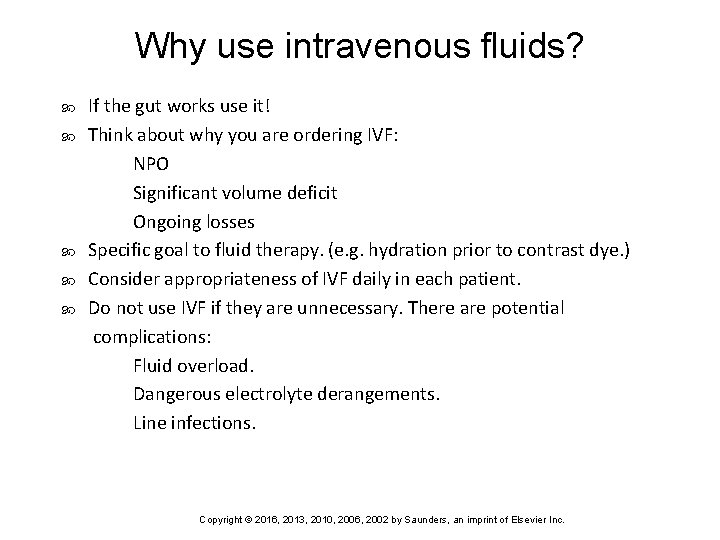
Why use intravenous fluids? If the gut works use it! Think about why you are ordering IVF: NPO Significant volume deficit Ongoing losses Specific goal to fluid therapy. (e. g. hydration prior to contrast dye. ) Consider appropriateness of IVF daily in each patient. Do not use IVF if they are unnecessary. There are potential complications: Fluid overload. Dangerous electrolyte derangements. Line infections. 25 Copyright © 2016, 2013, 2010, 2006, 2002 by Saunders, an imprint of Elsevier Inc.
Fluid Requirements Normal adult requires approximately 35 cc/kg/day. This assumes normal fluid loss. Urine Stool Insensible Watch I/O carefully and be aware of other losses. Fever increases insensible loss by 200 cc/day for each degree (C). Monitor abnormal GI loss e. g. NGT suctioning 26 Copyright © 2016, 2013, 2010, 2006, 2002 by Saunders, an imprint of Elsevier Inc.
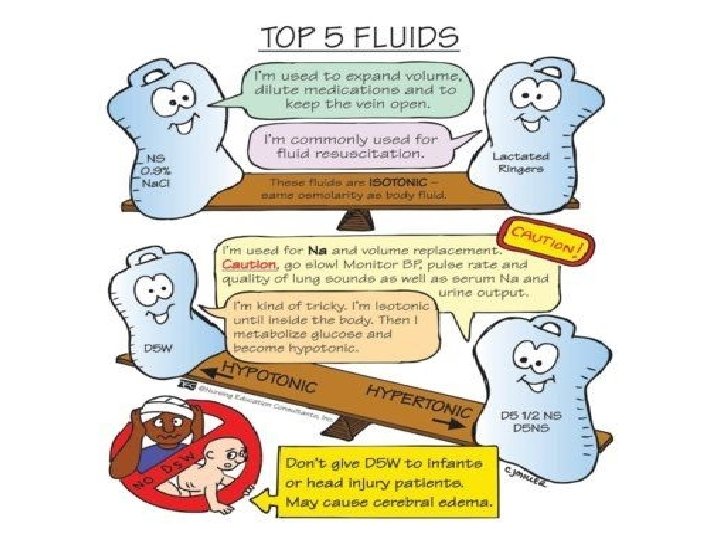
Which fluid to Choose? 1: What is your goal for therapy? Maintenance Rehydration Volume resuscitation 2: Any baseline electrolyte abnormalities? ALWAYS look at basic chemistry prior to ordering fluids. 3: Where is the fluid going to go? 27 Copyright © 2016, 2013, 2010, 2006, 2002 by Saunders, an imprint of Elsevier Inc.

Fluid Bolus Will always be NS or LR Given rapidly over 15 -30 minutes Monitoring Effects Complications 28 Copyright © 2016, 2013, 2010, 2006, 2002 by Saunders, an imprint of Elsevier Inc. 28
29 Copyright © 2016, 2013, 2010, 2006, 2002 by Saunders, an imprint of Elsevier Inc.

Nursing Action Rationale • Document all nursing observations and actions accurately and contemporaneously • To ensure clear, accurate and timely communication between all health professionals caring for a patient. • Daily weight (same scales, same clothes) • This is the best indication of fluid status. • Check cognitive status regularly • Anxiety and restlessness may indicate worsening fluid status • Check serum electrolytes as ordered • Sodium, potassium, urea and creatinine are important indicators of fluid status and renal function. • Regular position change • To prevent pressure areas due to dry skin. • Maintain patent IV access and monitor IV site regularly. • To ensure fluids are administered as ordered • Encourage oral fluids as ordered / tolerated by patient. • To increase fluid intake • Maintain oxygen therapy via nasal prongs or Hudson mask and hourly oxygen sats • To ensure adequate oxygen delivery • Monitor hemodynamic status closely • To identify improvement or deterioration in patient’s condition • Reassure patient • To maintain psychosocial wellbeing • Provide regular oral care • To manage dry mouth and tongue and to promote patient comfort • Check specific gravity of urine • To monitor changes in fluid status Copyright © 2016, 2013, 2010, 2006, 2002 by Saunders, an imprint of Elsevier Inc. 30
Facts to Remember. . . 1 L of water weighs 2. 2 lb, equal to 1 kg Weight change of 1 lb = fluid volume change of about 500 m. L 31 Copyright © 2016, 2013, 2010, 2006, 2002 by Saunders, an imprint of Elsevier Inc. 31
Consequences of fluid overload 32 Copyright © 2016, 2013, 2010, 2006, 2002 by Saunders, an imprint of Elsevier Inc.

Fluid Overload: Collaborative Care Assessment Patient safety Pulmonary edema Drug therapy Nutrition therapy Monitoring of intake and output (I&O) 33 Copyright © 2016, 2013, 2010, 2006, 2002 by Saunders, an imprint of Elsevier Inc. 33
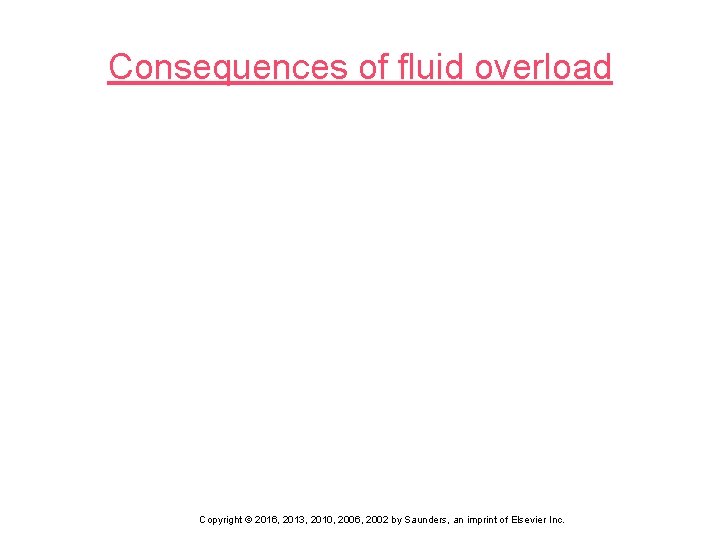
Clinical Manifestations Weight gain > 5% of body weight Circulatory overload Ø Ø Ø Full bounding pulse Distended neck and peripheral veins Increased central venous pressure (CVP) Cough, dyspnea, orthopnea Moist crackles Orthopneic position Copyright © 2016, 2013, 2010, 2006, 2002 by Saunders, an imprint of Elsevier Inc. 34
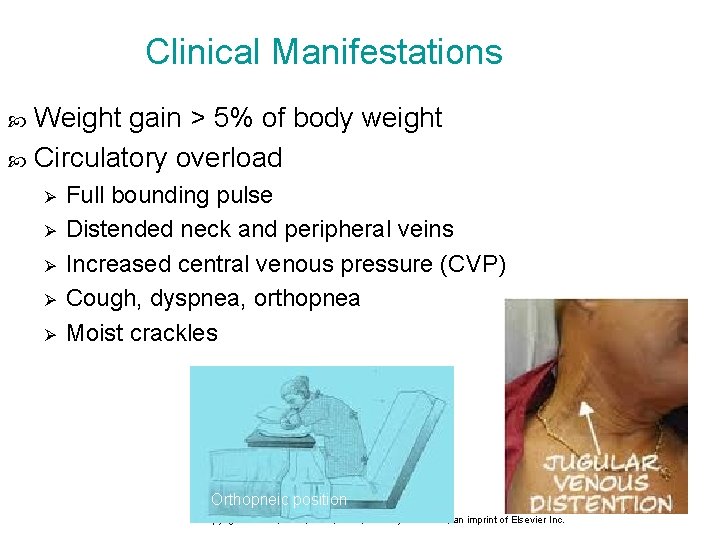
Clinical Manifestations Circulatory overload, continued Ø Ø Ø Periorbital Edema Polyuria Ascites Peripheral edema Anasarca Tachycardia, dyspnea Ascites Peripheral pitting edema Copyright © 2016, 2013, 2010, 2006, 2002 by Saunders, an imprint of Elsevier Inc. 35
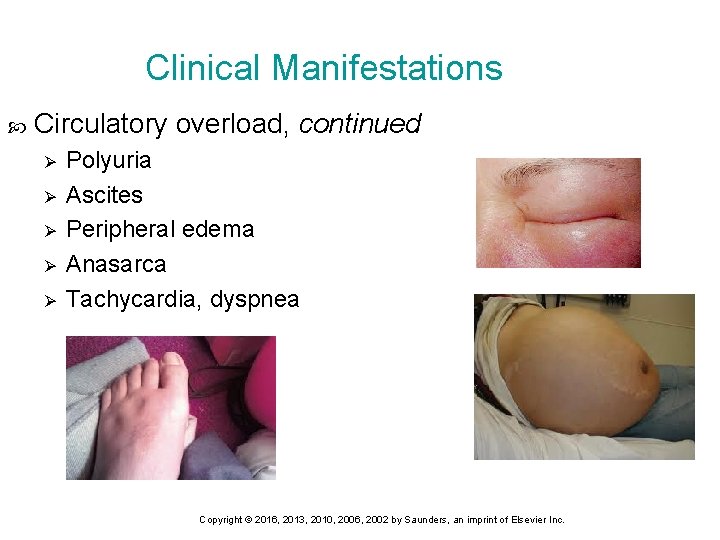
Clinical Significance: Edema Develops with changes in normal hydrostatic pressure differences 36 Copyright © 2016, 2013, 2010, 2006, 2002 by Saunders, an imprint of Elsevier Inc. 36
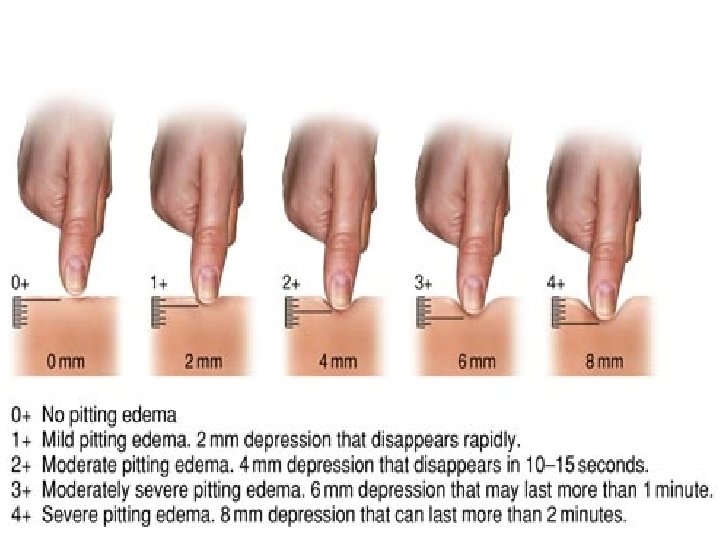
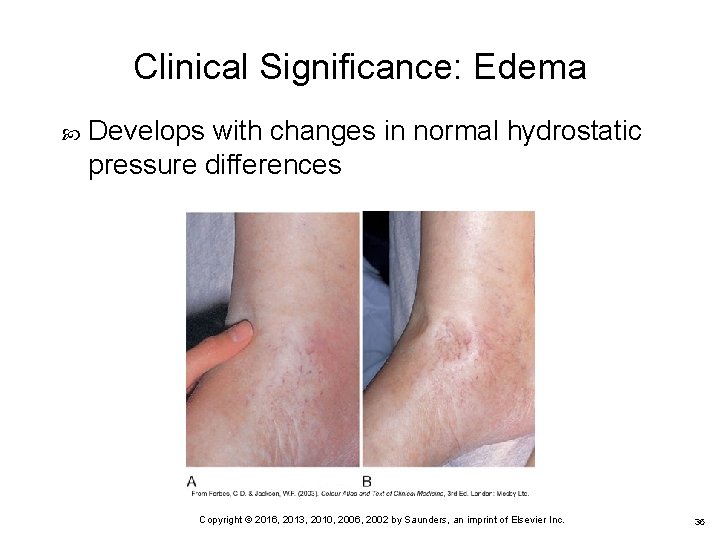
Figure 11 -22 Grading pitting edema. 37 Copyright © 2016, 2013, 2010, 2006, 2002 by Saunders, an imprint of Elsevier Inc.
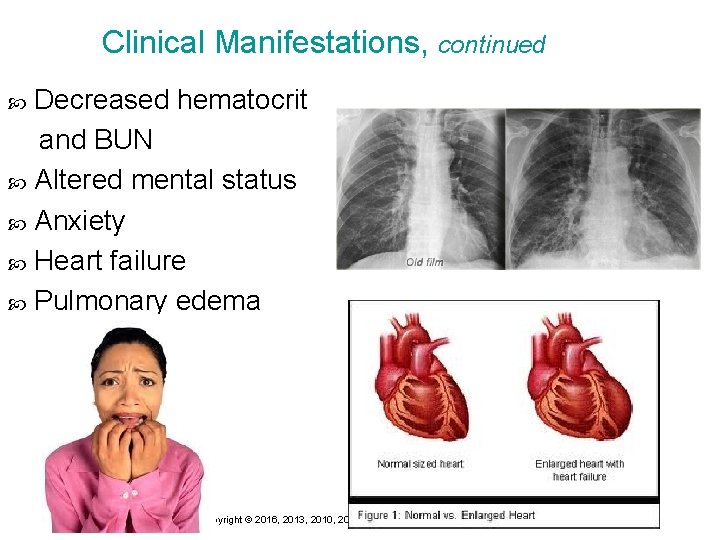
Clinical Manifestations, continued Decreased hematocrit and BUN Altered mental status Anxiety Heart failure Pulmonary edema 38 Copyright © 2016, 2013, 2010, 2006, 2002 by Saunders, an imprint of Elsevier Inc.
Collaboration Diagnostic tests Ø Ø Serum electrolytes, osmolality Serum hematocrit, hemoglobin Renal, liver function studies BUN and creatinine Pharmacologic therapies Ø Ø Ø Loop diuretics Thiazide-type diuretics Potassium-sparing diuretics 39 Copyright © 2016, 2013, 2010, 2006, 2002 by Saunders, an imprint of Elsevier Inc.
Implementation Weigh daily Maintain I & O records Administer oral fluids carefully Oral hygiene every 2 hours Teach about sodium restriction Administer medications Report imbalances 40 Copyright © 2016, 2013, 2010, 2006, 2002 by Saunders, an imprint of Elsevier Inc.
Implementation, continued Teach client medication safety Reposition every 2 hours Reduce skin shearing Provide alternative mattress, foot cradle Position in Fowler’s position Monitor laboratory results Elevate area with edema 41 Copyright © 2016, 2013, 2010, 2006, 2002 by Saunders, an imprint of Elsevier Inc.
Restrict Fluids Guidelines Ø Ø Ø Ø Required fluids Divide between shifts Explain to client and family Identify fluids Place allowed amounts in small glasses Ice chips Frequent mouth care Sugarless gum 42 Copyright © 2016, 2013, 2010, 2006, 2002 by Saunders, an imprint of Elsevier Inc.
Low Sodium Diet Foods high in sodium Ø Ø Ø Processed meat and fish Selected dairy products Processed grains Most canned goods Snack foods Condiments 43 Copyright © 2016, 2013, 2010, 2006, 2002 by Saunders, an imprint of Elsevier Inc.
Priority Nursing Interventions” Priority Nursing Interventions “RESTRICT” R educe IV flow rate E valuate breath sounds and ABGs S emi-Fowler’s position T reat with oxygen and diuretics as ordered R educe fluid and sodium intake I & O and weight C irculation, color, and presence of edema T urn and position at least every 2 hrs 44 Copyright © 2016, 2013, 2010, 2006, 2002 by Saunders, an imprint of Elsevier Inc.
Electrolyte Imbalance Can occur in healthy people as result of changes in fluid I&O Can be life threatening if severe; can occur in any setting 45 Copyright © 2016, 2013, 2010, 2006, 2002 by Saunders, an imprint of Elsevier Inc. 45
Electrolyte Imbalance Serum electrolyte value provides information about concentration of that specific electrolyte in blood Electrolytes gained and lost in relatively equal amounts body in balance Monitoring for signs of imbalance important for at -risk clients Ø Signs can be subtle 46 Copyright © 2016, 2013, 2010, 2006, 2002 by Saunders, an imprint of Elsevier Inc.
Electrolyte Imbalance, continued Moderate to severe imbalance produces multisystem effects can lead to death Important to understand interaction between all electrolytes and fluid Ø Ø Ø Loss of sodium loss of chloride Excess fluid dilutes other electrolytes Gastric suctioning loss of magnesium, sodium, chloride, acid–base imbalance 47 Copyright © 2016, 2013, 2010, 2006, 2002 by Saunders, an imprint of Elsevier Inc.
Sodium Normal 135 -145 m. Eq/L Imbalances typically associated with parallel changes in osmolality “Where sodium goes, water follows” Plays a major role in Ø Ø Ø ECF volume and concentration Generation and transmission of nerve impulses Acid–base balance 48 Copyright © 2016, 2013, 2010, 2006, 2002 by Saunders, an imprint of Elsevier Inc.
Hyponatremia < 136 m. Eq/L Decreased serum sodium occurring from diuretics, kidney disease, vomiting, diarrhea, GI suctioning, excessive tap water, heart failure Manifestations: depend on severity of onset and cause Serum sodium levels must be increased gradually to avoid cerebral edema 49 Copyright © 2016, 2013, 2010, 2006, 2002 by Saunders, an imprint of Elsevier Inc.
Hyponatremia Nursing Management Nursing Implementation Monitor ECG Treat underlying cause Sodium containing fluids administered: normal saline or hypertonic saline Fluid restriction if needed Monitor I&O Monitor CNS, neuromuscular changes, intestinal changes and cardiovascular changes Weigh daily Replace slowly Protect skin 50 Copyright © 2016, 2013, 2010, 2006, 2002 by Saunders, an imprint of Elsevier Inc.
Hypernatremia >145 m. Eq/L Elevated serum sodium occurring with water loss or sodium gain (profuse sweating, diarrhea) Causes hyperosmolality leading to cellular dehydration Primary protection is thirst from hypothalamus Manifestations: Ø Thirst, lethargy, agitation, increased temperature, muscle twitching, seizures, decreasing LOC and coma Ø Produced by clinical states: Central or nephrogenic diabetes insipidus Serum sodium levels must be reduced gradually to avoid cerebral edema 51 Copyright © 2016, 2013, 2010, 2006, 2002 by Saunders, an imprint of Elsevier Inc.
Hypernatremia Nursing Management Nursing Implementation � Monitor ECG � Treat underlying cause � If oral fluids cannot be ingested, IV solution of 5% dextrose in water or hypotonic saline � Diuretics to increase sodium excretion � Severe symptoms (seizures) � Institute safety precautions � Abnormal � Fluid fluid loss replacement with sodium-containing solution 52 Copyright © 2016, 2013, 2010, 2006, 2002 by Saunders, an imprint of Elsevier Inc.
Potassium (K+) Normal 3. 5 -5. 0 m. Eq/L Major ICF cation Necessary for Ø Transmission and conduction of nerve and muscle impulses Ø Maintenance of cardiac rhythms Ø Acid–base balance Sources Ø Almost all foods contain potassium, but especially meat, fish, and many vegetables and fruits Ø Salt substitutes Ø Potassium medications (PO, IV) Ø Stored blood 53 Copyright © 2016, 2013, 2010, 2006, 2002 by Saunders, an imprint of Elsevier Inc.
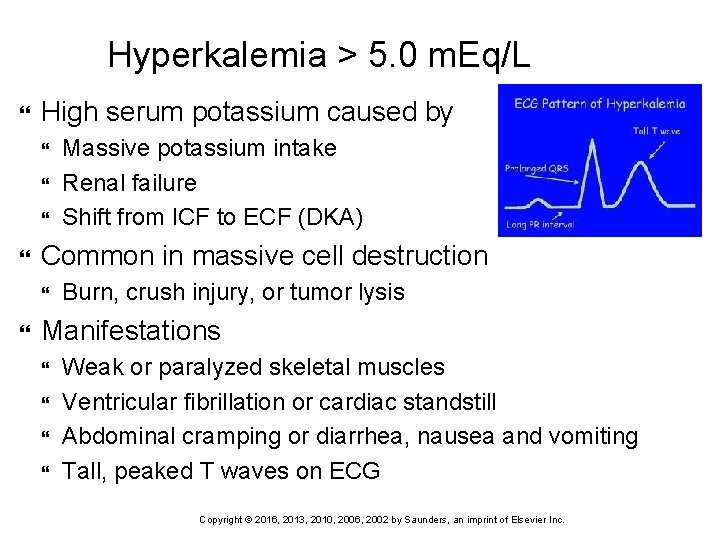
Hyperkalemia > 5. 0 m. Eq/L High serum potassium caused by Common in massive cell destruction Massive potassium intake Renal failure Shift from ICF to ECF (DKA) Burn, crush injury, or tumor lysis Manifestations Weak or paralyzed skeletal muscles Ventricular fibrillation or cardiac standstill Abdominal cramping or diarrhea, nausea and vomiting Tall, peaked T waves on ECG 54 Copyright © 2016, 2013, 2010, 2006, 2002 by Saunders, an imprint of Elsevier Inc.
Hyperkalemia Nursing Management Nursing Implementation Monitor ECG Eliminate oral and parenteral K+ intake Increase elimination of K+ Ø Potassium excreting diuretics (Furosemide) Ø Dialysis Ø Kayexalate) • Kayexelate-acationexchange resin (K moves into bowel space and Na moves into the bowel cells ) Force K from ECF to ICF by IV insulin and IV glucose Ø D 50 (50 ml) 1 amp and regular IV insulin (Regular) 10 -20 units (to facilitate K movement into the cells) Ø Bicarbonate 1 amp-drives K into the cells Reverse membrane effects of elevated ECF potassium by administering calcium gluconate IV Ø 1 amp Ca gluconate (cardioprotective) Ø Ca gluconate (10%) IV infusion over 2 -5 minutes to counteract the myocardial depressant effects of hyperkalemia-MUST be on a monitor/Needs repeat Rx 55 Copyright © 2016, 2013, 2010, 2006, 2002 by Saunders, an imprint of Elsevier Inc.
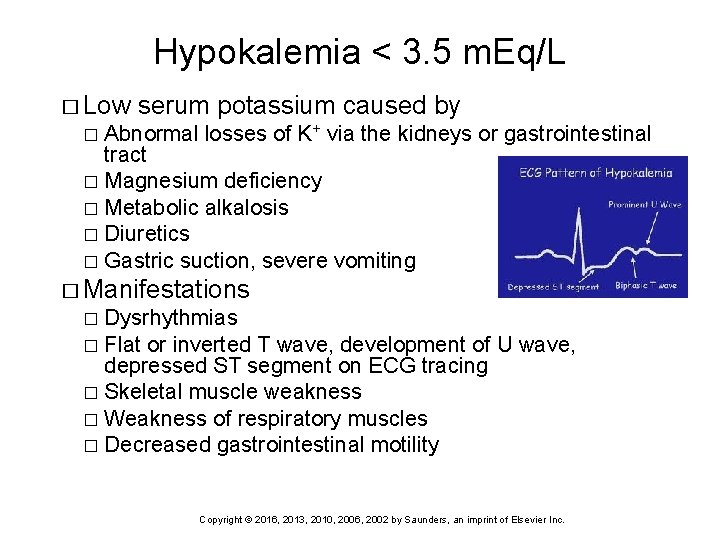
Hypokalemia < 3. 5 m. Eq/L � Low serum potassium caused by Abnormal losses of K+ via the kidneys or gastrointestinal tract � Magnesium deficiency � Metabolic alkalosis � Diuretics � Gastric suction, severe vomiting � � Manifestations Dysrhythmias � Flat or inverted T wave, development of U wave, depressed ST segment on ECG tracing � Skeletal muscle weakness � Weakness of respiratory muscles � Decreased gastrointestinal motility � 56 Copyright © 2016, 2013, 2010, 2006, 2002 by Saunders, an imprint of Elsevier Inc.
Hypokalemia Nursing Management Nursing Implementation Preventing loss of potassium ECG monitoring Monitor digitalis level Treat associated electrolyte disorders (low Mg) Reverse underlying cause (diuretics)/ alkalosis Severe hypokalemia can cause a paralytic ileus 57 Copyright © 2016, 2013, 2010, 2006, 2002 by Saunders, an imprint of Elsevier Inc.
Hypokalemia Nursing Management Nursing Implementation 58 Copyright © 2016, 2013, 2010, 2006, 2002 by Saunders, an imprint of Elsevier Inc.
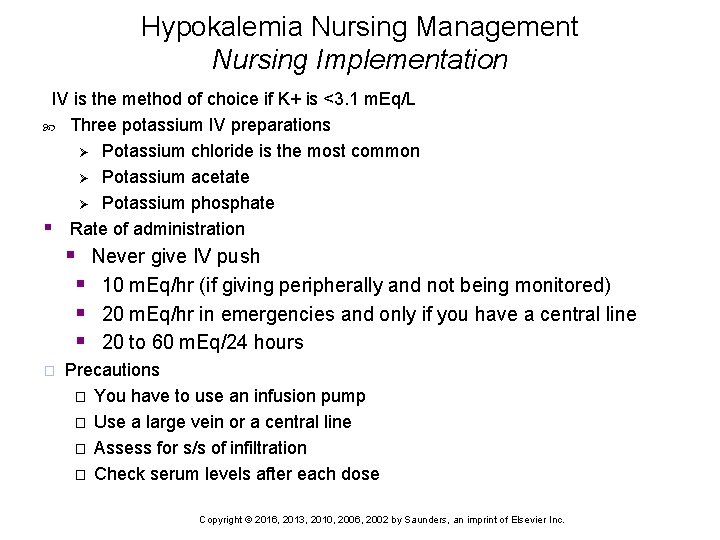
Hypokalemia Nursing Management Nursing Implementation IV is the method of choice if K+ is <3. 1 m. Eq/L Three potassium IV preparations Ø Potassium chloride is the most common Ø Potassium acetate Ø Potassium phosphate § Rate of administration § Never give IV push § 10 m. Eq/hr (if giving peripherally and not being monitored) § 20 m. Eq/hr in emergencies and only if you have a central line § 20 to 60 m. Eq/24 hours � Precautions � You have to use an infusion pump � Use a large vein or a central line � Assess for s/s of infiltration � Check serum levels after each dose 59 Copyright © 2016, 2013, 2010, 2006, 2002 by Saunders, an imprint of Elsevier Inc.
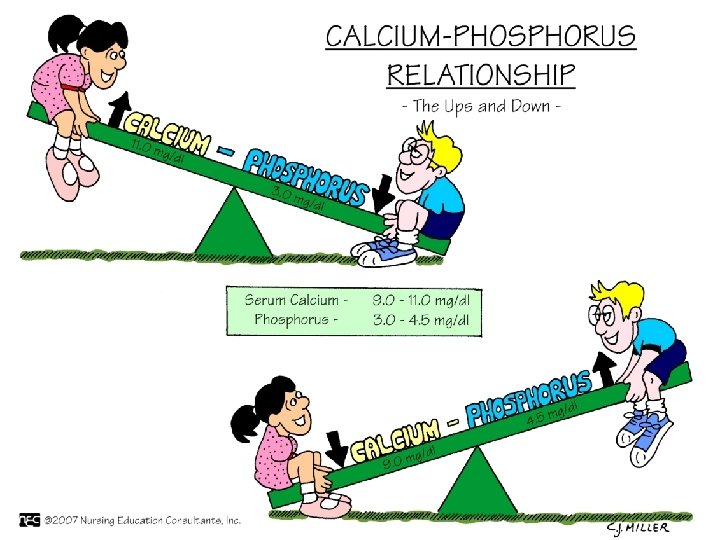
Calcium: Normal 9. 0 -10. 5 mg/d. L � � � � Obtained from ingested foods More than 99% combined with phosphorus and concentrated in skeletal system Inverse relationship with phosphorus Stored in bones Blocks sodium transport and stabilizes cell membrane Ionized form is biologically active Functions � Transmission of nerve impulses � Myocardial contractions � Blood clotting � Formation of teeth and bone � Muscle contractions Balance controlled by � Parathyroid hormone � Calcitonin � Absorption requires active form of Vitamin D 60 Copyright © 2016, 2013, 2010, 2006, 2002 by Saunders, an imprint of Elsevier Inc.
Hypercalcemia >10. 5 mg/dl � High serum calcium levels caused by � Hyperparathyroidism (two thirds of cases) � Malignancy or tumors � Vitamin D overdose � Prolonged immobilization � Chronic renal failure � Manifestations � Decreased memory � Confusion � Disorientation � Fatigue, muscle weakness � Constipation 61 Copyright © 2016, 2013, 2010, 2006, 2002 by Saunders, an imprint of Elsevier Inc.
Hypercalcemia Nursing Management Nursing Implementation ECG monitoring (may lead to heart blocks) Excretion of Ca with loop diuretic Hydration with isotonic saline infusion Synthetic calcitonin Calcium chelators (calcium binders) 62 Copyright © 2016, 2013, 2010, 2006, 2002 by Saunders, an imprint of Elsevier Inc.
Hypocalcemia < 9. 0 mg/dl Low serum Ca levels caused by Ø Decreased production of PTH Ø Acute pancreatitis, alcoholism Ø Immobility Ø Alkalosis Ø Decreased intake Manifestations Ø Positive Trousseau’s or Chvostek’s sign Ø Frequent, painful muscle spasms (“charley horse”) in the calf or foot during rest or sleep Ø Dysphagia Ø Tingling around the mouth or in the extremities 63 Copyright © 2016, 2013, 2010, 2006, 2002 by Saunders, an imprint of Elsevier Inc.
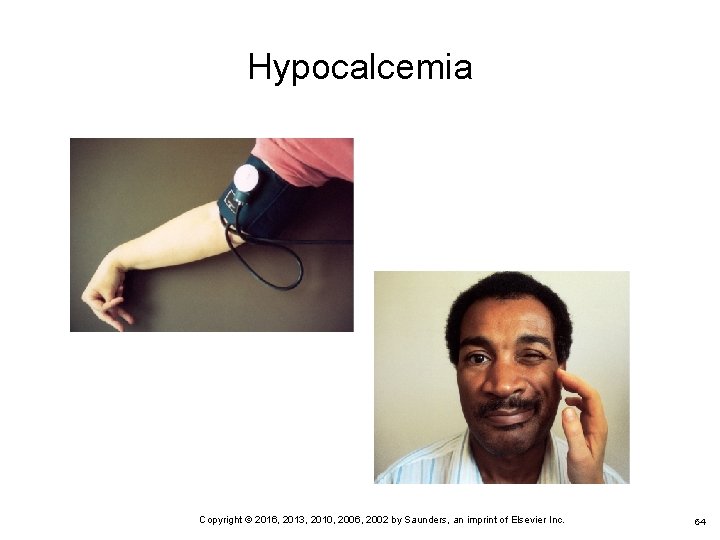
Hypocalcemia 64 Copyright © 2016, 2013, 2010, 2006, 2002 by Saunders, an imprint of Elsevier Inc. 64
Hypocalcemia Nursing Management Nursing Implementation ECG monitoring Treat cause Oral or IV calcium supplements Ø Ø Not IM to avoid local reactions Calculate adjusted calcium based on albumin level Treat pain and anxiety to prevent hyperventilation-induced respiratory alkalosis 65 Copyright © 2016, 2013, 2010, 2006, 2002 by Saunders, an imprint of Elsevier Inc.
66 Copyright © 2016, 2013, 2010, 2006, 2002 by Saunders, an imprint of Elsevier Inc.
Phosphorus (PO 4) Normal 3. 0 -4. 5 mg/d. L Primary anion in ICF Found in bones Activates vitamins and enzymes; assists in cell growth and metabolism Plasma levels of calcium and phosphorus exist in a balanced reciprocal relationship Deposited with calcium for bone and tooth structure Involved in acid–base buffering system, ATP production, and cellular uptake of glucose Maintenance requires adequate renal functioning 67 Copyright © 2016, 2013, 2010, 2006, 2002 by Saunders, an imprint of Elsevier Inc.
Hyperphosphatemia > 4. 5 mg/d. L High serum PO 43 - caused by Ø Ø Ø Acute or chronic renal failure Chemotherapy Excessive ingestion of phosphate or vitamin D Sepsis Disruptions in calcium levels Manifestations Ø Ø Ø Calcified deposition in soft tissue such as joints, arteries, skin, kidneys, and corneas Muscle spasms and tetany Circumoral and peripheral paresthesias 68 Copyright © 2016, 2013, 2010, 2006, 2002 by Saunders, an imprint of Elsevier Inc.
Hyperphosphatemia Nursing management Management Ø Ø Ø Identify and treat underlying cause Restrict foods and fluids containing PO 43 Adequate hydration and correction of hypocalcemic conditions 69 Copyright © 2016, 2013, 2010, 2006, 2002 by Saunders, an imprint of Elsevier Inc.
Hypophosphatemia < 3. 0 mg/dl � Low � � � serum PO 43 - caused by Malnourishment/malabsorption Alcohol withdrawal Use of phosphate-binding antacids During parenteral nutrition with inadequate replacement IV glucose administration Respiratory alkalosis � Manifestations � � � CNS depression Confusion Muscle weakness and pain Seizures, coma Dysrhythmias Cardiomyopathy 70 Copyright © 2016, 2013, 2010, 2006, 2002 by Saunders, an imprint of Elsevier Inc.
Hypophosphatemia Nursing Management Ø Ø Oral supplementation Ingestion of foods high in PO 43 IV administration of sodium or potassium phosphate Drugs that promote phosphorous loss (antacids, osmotic diuretics, calcium supplements) would be discontinued 71 Copyright © 2016, 2013, 2010, 2006, 2002 by Saunders, an imprint of Elsevier Inc.
Magnesium (MG) Normal 1. 3 -2. 1 m. Eq/L 50% to 60% contained in bone Critical for skeletal muscle contraction, carbohydrate metabolism, ATP formation, vitamin activation, cell growth Factors that regulate calcium balance appear to influence magnesium balance Important for normal cardiac function Blood coagulation 72 Copyright © 2016, 2013, 2010, 2006, 2002 by Saunders, an imprint of Elsevier Inc.
Hypomagnesemia > 2. 1 m. Eq/L High serum Mg caused by Ø Increased intake or ingestion of products containing magnesium when renal insufficiency or failure is present Manifestations Ø Ø Ø Lethargy or drowsiness Nausea/vomiting Impaired deep tendon reflexes Hypotension Flushing/sweating, feeling of warmth Respiratory and cardiac arrest 73 Copyright © 2016, 2013, 2010, 2006, 2002 by Saunders, an imprint of Elsevier Inc.
Hypermagnesemia Nursing Management Ø Ø ECG monitoring Prevention Dialysis Emergency treatment • Ø IV Ca. Cl or calcium gluconate Fluids to promote urinary excretion 74 Copyright © 2016, 2013, 2010, 2006, 2002 by Saunders, an imprint of Elsevier Inc.
Hypomagnesemia < 1. 3 m. Eq/L � Low � � � serum Mg caused by Prolonged fasting or starvation Chronic alcoholism Fluid loss from gastrointestinal tract (suction, diarrhea) Prolonged parenteral nutrition without supplementation Diuretics Endocrine disorders (DKA) � Manifestations � � � � Confusion Hyperactive deep tendon reflexes (tetany) Positive Chvostek’s sign Positive Trousseau’s sign Intestinal changes Seizures Cardiac dysrhythmias 75 Copyright © 2016, 2013, 2010, 2006, 2002 by Saunders, an imprint of Elsevier Inc.
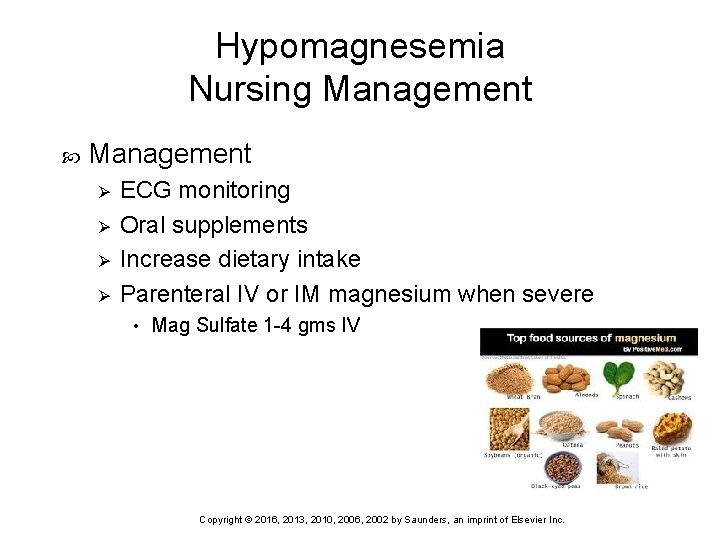
Hypomagnesemia Nursing Management Ø Ø ECG monitoring Oral supplements Increase dietary intake Parenteral IV or IM magnesium when severe • Mag Sulfate 1 -4 gms IV 76 Copyright © 2016, 2013, 2010, 2006, 2002 by Saunders, an imprint of Elsevier Inc.
Chloride Normal level: 98 to 106 m. Eq/L Major anion of the ECF Works with sodium to maintain ECF osmotic pressure. Important formation of hydrochloric acid in the stomach Imbalance occurs as a result of other electrolyte imbalances Treat underlying electrolyte imbalance or acid -base problem 77 Copyright © 2016, 2013, 2010, 2006, 2002 by Saunders, an imprint of Elsevier Inc. 77
Considerations for Older Adults At risk for most electrolyte imbalances from age-related organ changes Have less total body water than younger adults; more at risk for fluid imbalances; more likely to be taking drugs affecting fluid or electrolyte balance 78 Copyright © 2016, 2013, 2010, 2006, 2002 by Saunders, an imprint of Elsevier Inc. 78
- Slides: 78