CONCEPT AND COMPETENCY REQUIREMENT FOR ADVANCE CLINICAL PHARMACY
![Competencies of a Clinical Pharmacist: Pharmacotherapy knowledge: Pharmacotherapeutic knowledge needed for clinical pharmacist[5]. Characteristic Competencies of a Clinical Pharmacist: Pharmacotherapy knowledge: Pharmacotherapeutic knowledge needed for clinical pharmacist[5]. Characteristic](https://slidetodoc.com/presentation_image_h2/66163f4d9a6d9ac49a2f5806c7225ec5/image-9.jpg)
- Slides: 25
CONCEPT AND COMPETENCY REQUIREMENT FOR ADVANCE CLINICAL PHARMACY PRACTICE Presented by: Muhammad Sajjad Hussain M. Phil. Pharmacy Practice College Of Pharmacy UOS 1
Definition: Clinical Pharmacy: Clinical pharmacy is relatively a new discipline in pharmacy practice in which emphasis is transferred from product oriented to patient oriented practice. However definition of clinical pharmacy and clinical pharmacy practice has not been universally standardized. American College Of Clinical Pharmacy (ACCP) defined Clinical pharmacy/ clinical pharmacy practice as: q Clinical pharmacy is a health science discipline in which pharmacist provide patient care that optimize medication therapy and promote health, wellness and disease prevention. Clinical pharmacy/ clinical pharmacy practice can also be defined as: q A specialized pharmacy practice which involves in providing pharmaceutical care through patient medication history, patient profile review, adverse drug management, drug information management and discharge patient counseling. 2
Definition: Advance clinical pharmacy practice: q Clinical pharmacy practice which includes collaborative agreement between the clinical pharmacist and physicians allowing clinical pharmacist to prescribe medication is called advance clinical pharmacy practice. Clinical pharmacist: q Hospital or community pharmacist responsible for any of the clinical activities : patient medication history, patient profile review, discharge patient counseling, therapeutic drug monitoring, adverse drug reaction management and information management along with traditional responsibilities is called a clinical pharmacist[1]. 3
Definition: Competency: q A “competency” is a “distinct skill, ability or attitude which is necessary for one to be competent in his/her profession”. q The ability of a person to make accurate decisions, interact with a physician, nurses, and other colleagues appropriately and perform their duties at their best. q While professional competence is characterized by good decision-making abilities, a sound knowledge, having good problem-solving skills and expert in dealing with diverse patient care situations[2] 4
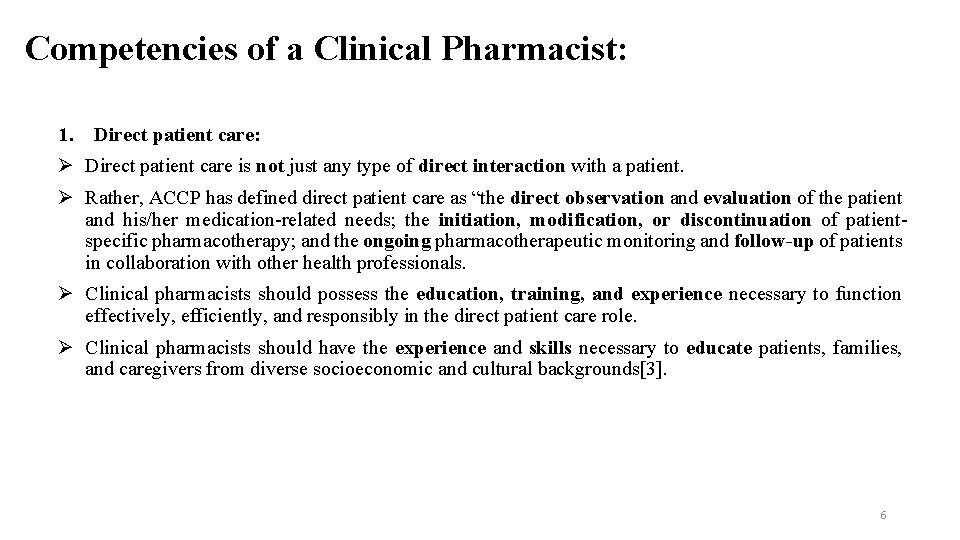
Competencies of a Clinical Pharmacist: The purpose of the American College of Clinical Pharmacy (ACCP) is to advance human health by extending the frontiers of clinical pharmacy. Consistent with this mission and its core values, ACCP is committed to ensuring that clinical pharmacists possess the knowledge, skills, attitudes, and behaviors necessary to deliver comprehensive medication management (CMM) in team-based, direct patient care environments. According to ACCP clinical pharmacist must posses six competency domains. 1. Direct patient care. 2. Pharmacotherapy knowledge. 3. Systems-based care and population health. 4. Communication. 5. Professionalism. 6. Continuing professional development. 5
Competencies of a Clinical Pharmacist: 1. Direct patient care: Direct patient care is not just any type of direct interaction with a patient. Rather, ACCP has defined direct patient care as “the direct observation and evaluation of the patient and his/her medication-related needs; the initiation, modification, or discontinuation of patientspecific pharmacotherapy; and the ongoing pharmacotherapeutic monitoring and follow-up of patients in collaboration with other health professionals. Clinical pharmacists should possess the education, training, and experience necessary to function effectively, efficiently, and responsibly in the direct patient care role. Clinical pharmacists should have the experience and skills necessary to educate patients, families, and caregivers from diverse socioeconomic and cultural backgrounds[3]. 6
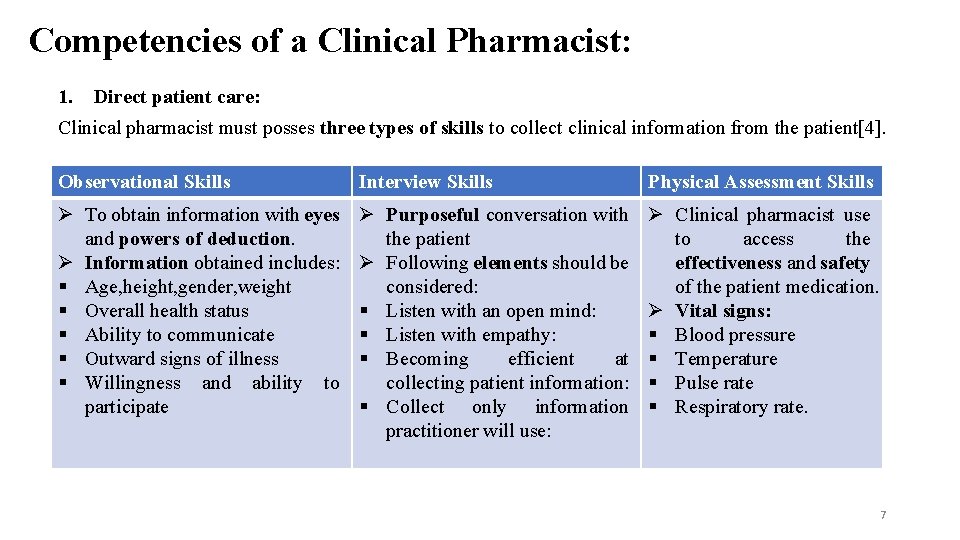
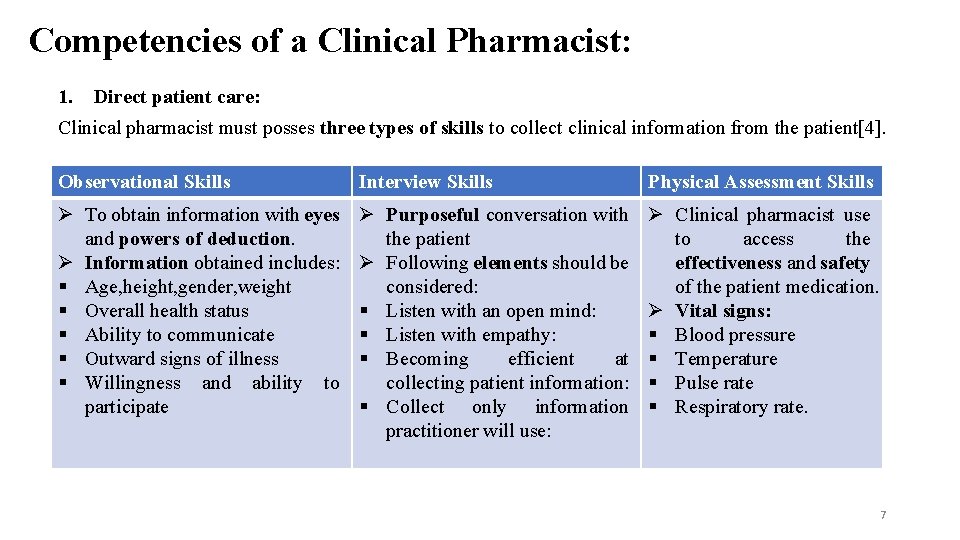
Competencies of a Clinical Pharmacist: 1. Direct patient care: Clinical pharmacist must posses three types of skills to collect clinical information from the patient[4]. Observational Skills Interview Skills Physical Assessment Skills To obtain information with eyes and powers of deduction. Information obtained includes: § Age, height, gender, weight § Overall health status § Ability to communicate § Outward signs of illness § Willingness and ability to participate Purposeful conversation with the patient Following elements should be considered: § Listen with an open mind: § Listen with empathy: § Becoming efficient at collecting patient information: § Collect only information practitioner will use: Clinical pharmacist use to access the effectiveness and safety of the patient medication. Vital signs: § Blood pressure § Temperature § Pulse rate § Respiratory rate. 7
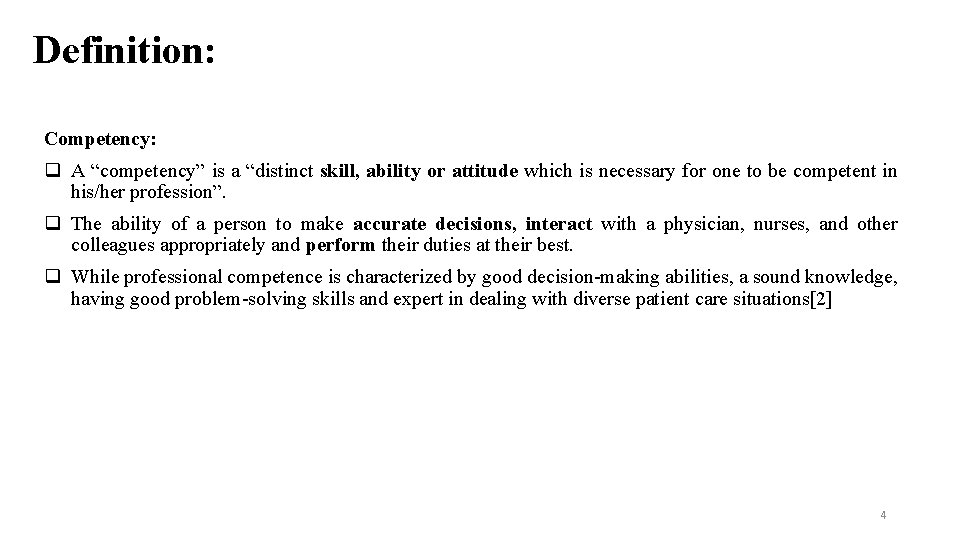
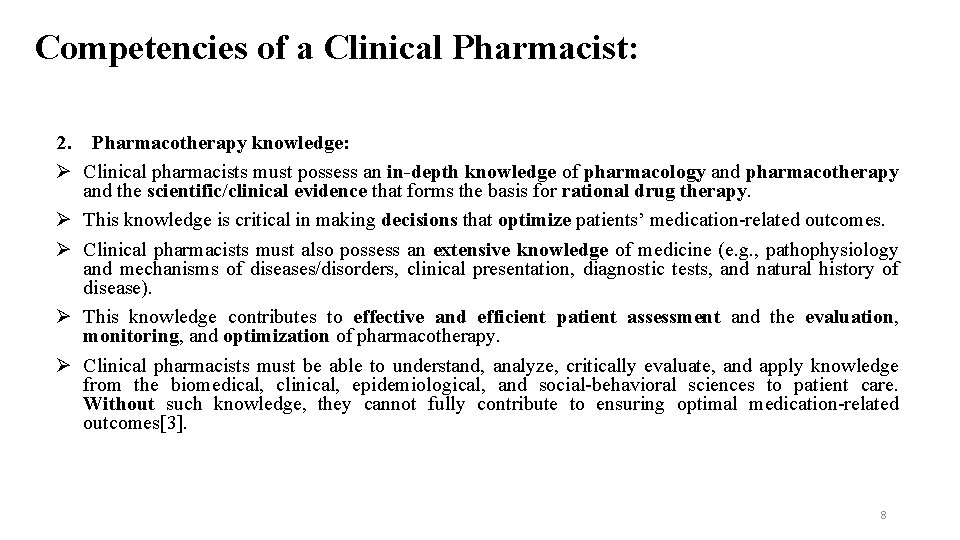
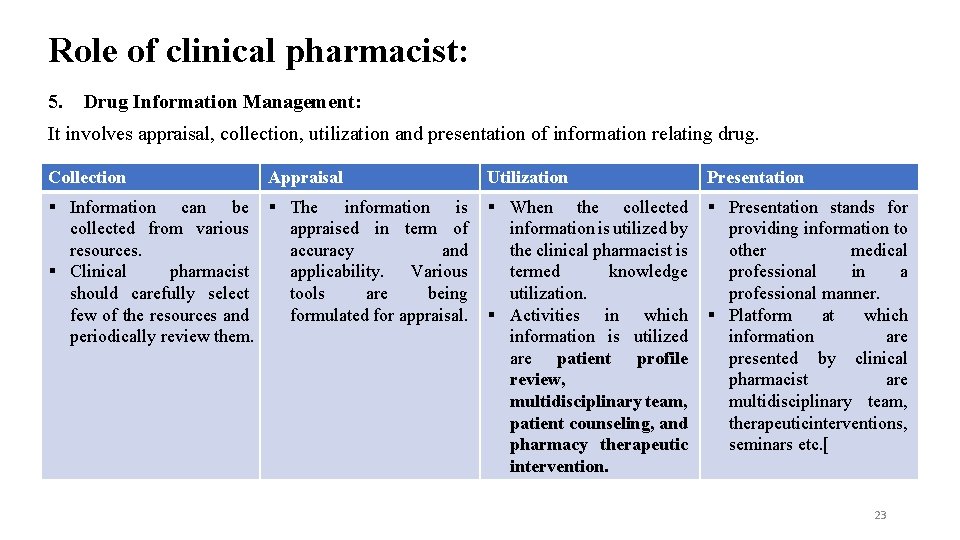
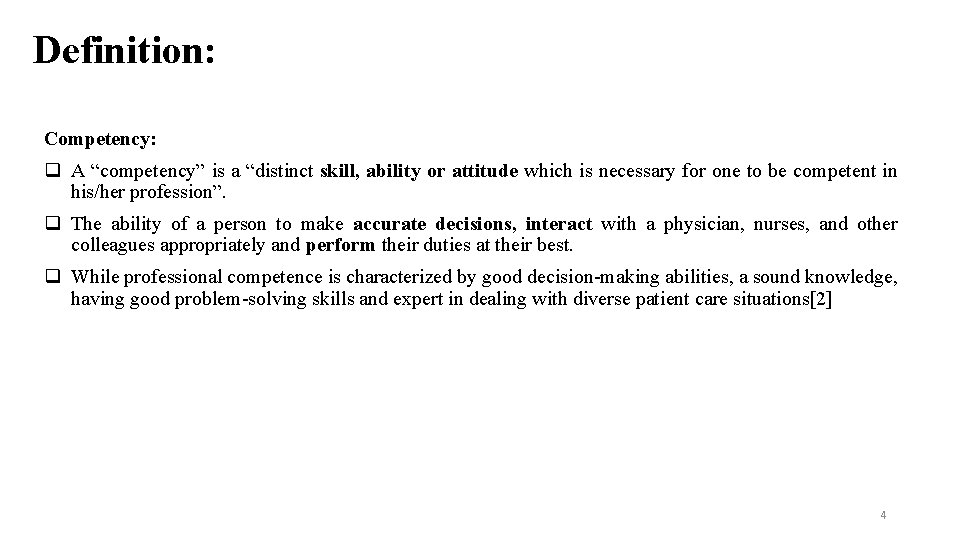
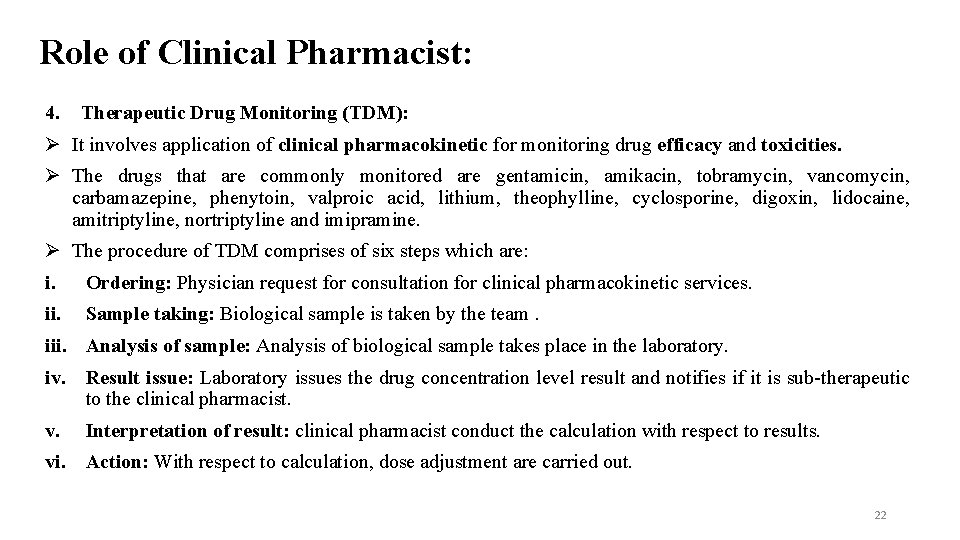
Competencies of a Clinical Pharmacist: 2. Pharmacotherapy knowledge: Clinical pharmacists must possess an in-depth knowledge of pharmacology and pharmacotherapy and the scientific/clinical evidence that forms the basis for rational drug therapy. This knowledge is critical in making decisions that optimize patients’ medication-related outcomes. Clinical pharmacists must also possess an extensive knowledge of medicine (e. g. , pathophysiology and mechanisms of diseases/disorders, clinical presentation, diagnostic tests, and natural history of disease). This knowledge contributes to effective and efficient patient assessment and the evaluation, monitoring, and optimization of pharmacotherapy. Clinical pharmacists must be able to understand, analyze, critically evaluate, and apply knowledge from the biomedical, clinical, epidemiological, and social-behavioral sciences to patient care. Without such knowledge, they cannot fully contribute to ensuring optimal medication-related outcomes[3]. 8
![Competencies of a Clinical Pharmacist Pharmacotherapy knowledge Pharmacotherapeutic knowledge needed for clinical pharmacist5 Characteristic Competencies of a Clinical Pharmacist: Pharmacotherapy knowledge: Pharmacotherapeutic knowledge needed for clinical pharmacist[5]. Characteristic](https://slidetodoc.com/presentation_image_h2/66163f4d9a6d9ac49a2f5806c7225ec5/image-9.jpg)
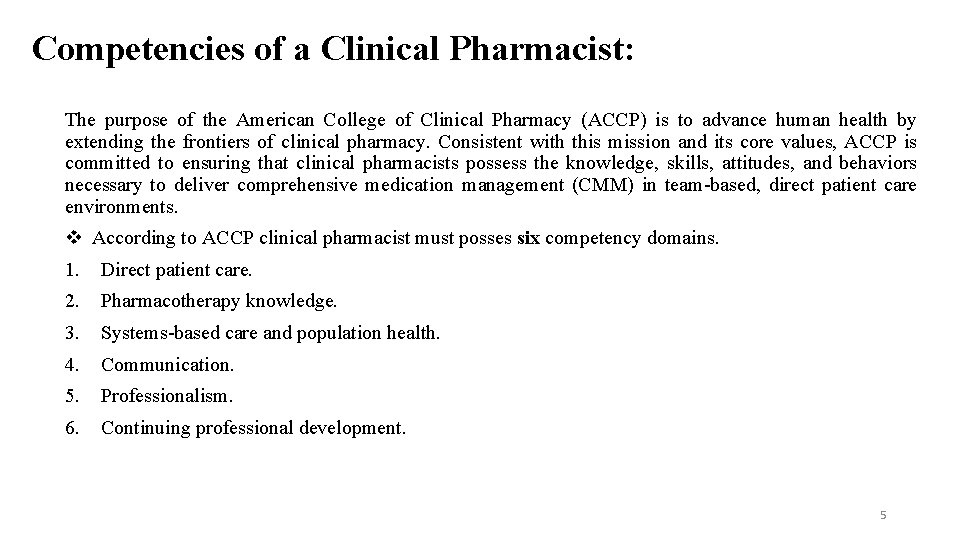
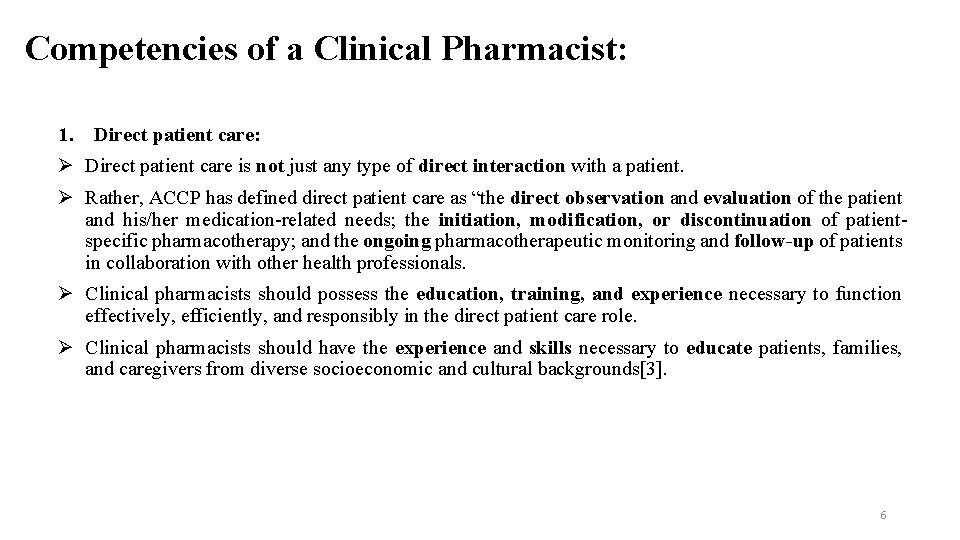
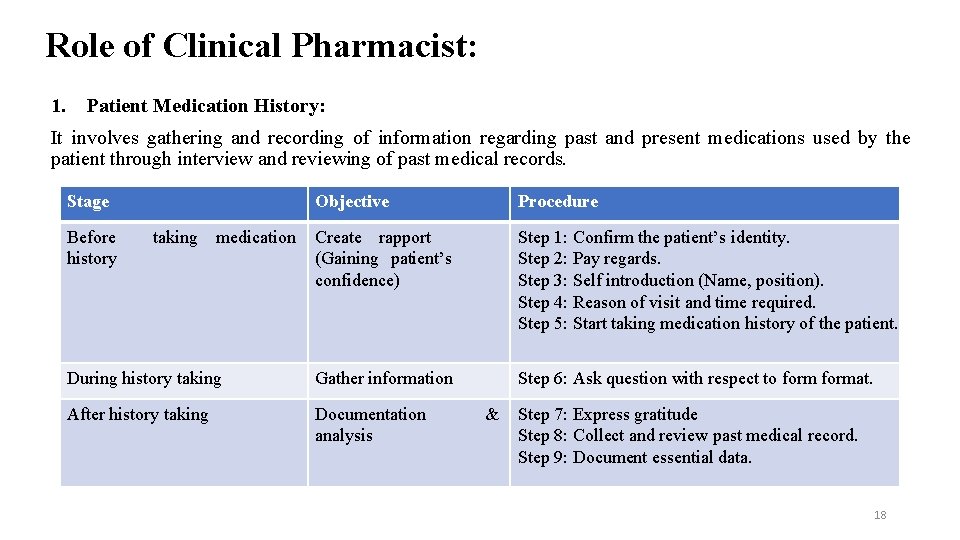
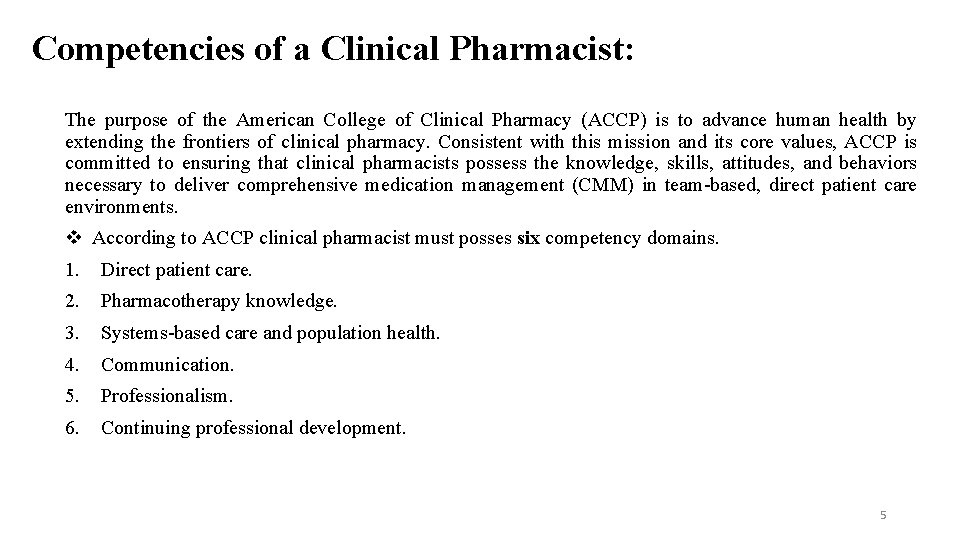
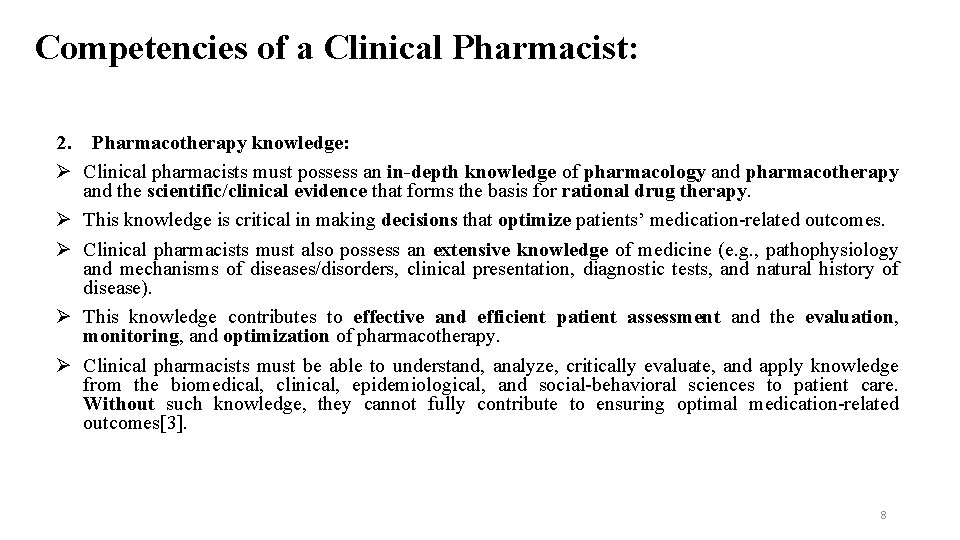
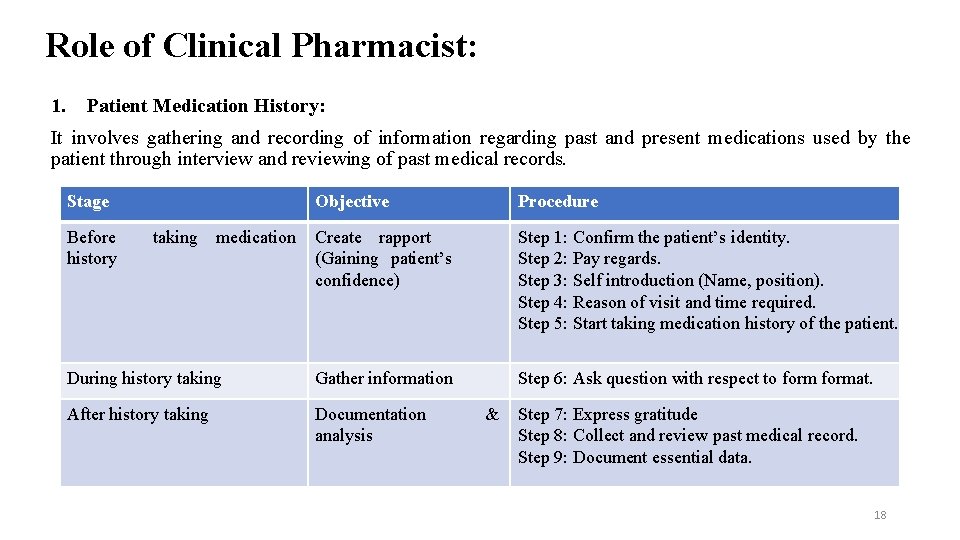
Competencies of a Clinical Pharmacist: Pharmacotherapy knowledge: Pharmacotherapeutic knowledge needed for clinical pharmacist[5]. Characteristic of drug Efficacy for an indication: § Dosage regimen for the drug § Dose (initial and maintenance) § Dosing interval § Frequency § Duration Pharmacology: § Mechanism of action § Sites of action Toxicology: § Contraindications § Adverse effects § Precautions Activity of drug in the patient Outcomes of drug therapy § § § § Therapeutic process: § Effectiveness § Improvement in signs, sympt oms, and/or laboratory findin gs § Safety § Undesirable or harmful effec ts and adverse drug reactions Pharmaceutical process: Bioavailability Physicochemical properties Formulations and dosage forms Methods of drug administrations Pharmacokinetic process: ADME Pharmacodynamics process: Impact of a drug on cell, tissue, or organ § Time course of the effects 9
Competencies of a Clinical Pharmacist: 3. Systems-based Care and Population Health: Clinical pharmacists’ contributions to public health, global health, and population health directly and indirectly affect medication management, including chronic disease prevention and treatment. This has been facilitated by the expansion of health informatics, which has become an important, multidimensional health care tool. Clinical pharmacists use health informatics to optimize patient care at both the health system and population levels by engaging in developing, implementing, and disseminating system-wide protocols, clinical pathways, and clinical decision support systems. Health informatics data allow opportunities to improve health care metrics/outcomes and reduce costs. Clinical pharmacists should be able to conduct pharmacotherapy-related evaluations and critically interpret data to improve health within a population[3]. 10
Competencies of a Clinical Pharmacist: 4. Communication. Clinical pharmacists must communicate effectively with patients, caregivers, families, and laypersons of diverse backgrounds; other health professionals; staff of health-related agencies; and other stakeholders. Clinical pharmacists must be able to develop professional written communications in professional settings. Documenting direct patient care activities appropriately in the medical record is an essential expectation. Clinical pharmacists are required to use writing styles appropriate to the context of the communication. For example, accurate, clear, and concise messages are necessary for follow-up medical record notations and e-mail communications; more detailed and extensive writing may be required for consultative, admission, or discharge medical record entries. 11
Competencies of a Clinical Pharmacist: 4. Communication: i. Patient Focused Communication: Patient focused communication involves the relationship between the practitioner and patient. Such communication will create an environment where patient feel comfortable with the practitioner and share his medical history with the practitioner. Objectives: Clinical pharmacist have three objectives to communicate with the patient: To elicit necessary information from the patient to make the decision. To negotiate the terms of goal of therapy and the patient role in achieving them. To educate the patient about drug therapy he/she is receiving. 12
Competencies of a Clinical Pharmacist: 4. Communication: Clinical pharmacist shall provide following information to the patient: The reason the patient taking each medication. (Indication) The specific instruction of how to take the medication explained in a manner the patient can understand. A description of how the patient will know that the medication I am taking working well. (Effectiveness) Explain the undesirable effects that might be expected. (safety) Be clear about what the patient should do if the dose of the medication is missed or taken an extra dose of the medication. (Compliance) Inform the patient of when and how you intend to follow up to evaluate the effectiveness and safety of medication. Provide the patient with a way to contact you if the medication is not working within a given timeframe. 13
Competencies of a Clinical Pharmacist: 4. Communication: Written correspondence with the patient: Practitioner also shall provide information regarding drug therapy in written form to the patient. It should be written in easily readable form. Practitioner shall not provide excessive information to the patient. It should include all the elements that are being discussed in verbal communication. ii. Practitioner Focused Communication: Practitioner shall communicate effectively with other health care provider and colleagues to ensure the optimum therapy of the patient. Communication must be verbal and non-verbal. Practitioner must use standard terms and practice vocabulary whenever to communicate. Communication must be concise, precise and patient oriented[4]. 14
Competencies of a Clinical Pharmacist: 5. Professionalism. The oath of a pharmacist declares a commitment to serve patients, pursue optimal health outcomes and act according to the highest moral, ethical, and legal conduct. Professionalism is expected of all health care providers and should be central to pharmacists’ practices over their lifetime. As professionals, clinical pharmacists must make it their primary obligation to establish a “fiducial” relationship with those they serve. In exchange for this “gift of trust, ” they promise to work in the patient’s best interests. This covenantal relationship lies at the core of the clinical pharmacist’s relationship with the patient. Teaching and demonstrating professionalism are essential components of the postgraduate training competency areas, goals, and objectives. Clinical pharmacists must serve as credible role models for students and trainees by both exhibiting and providing guidance on the values and behaviors of a professional[3]. 15
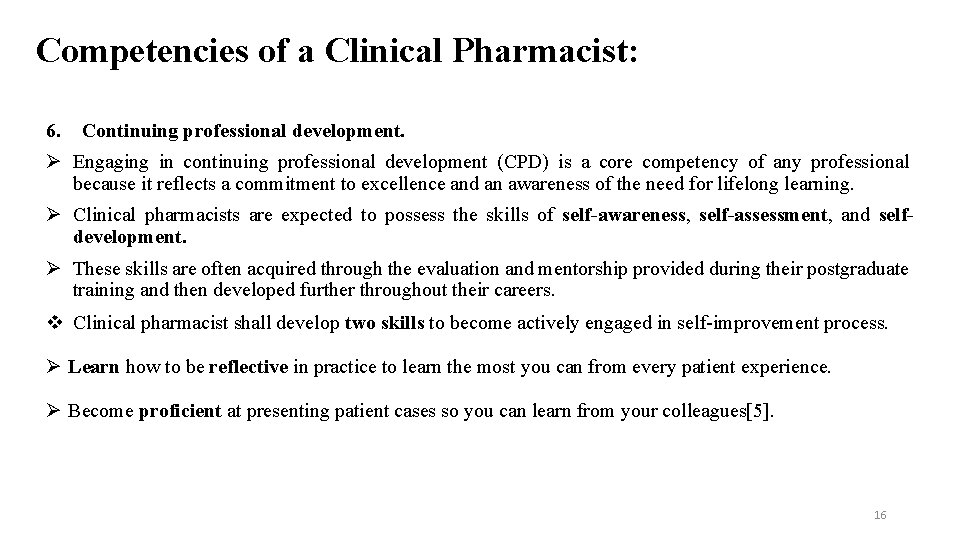
Competencies of a Clinical Pharmacist: 6. Continuing professional development. Engaging in continuing professional development (CPD) is a core competency of any professional because it reflects a commitment to excellence and an awareness of the need for lifelong learning. Clinical pharmacists are expected to possess the skills of self-awareness, self-assessment, and selfdevelopment. These skills are often acquired through the evaluation and mentorship provided during their postgraduate training and then developed further throughout their careers. Clinical pharmacist shall develop two skills to become actively engaged in self-improvement process. Learn how to be reflective in practice to learn the most you can from every patient experience. Become proficient at presenting patient cases so you can learn from your colleagues[5]. 16
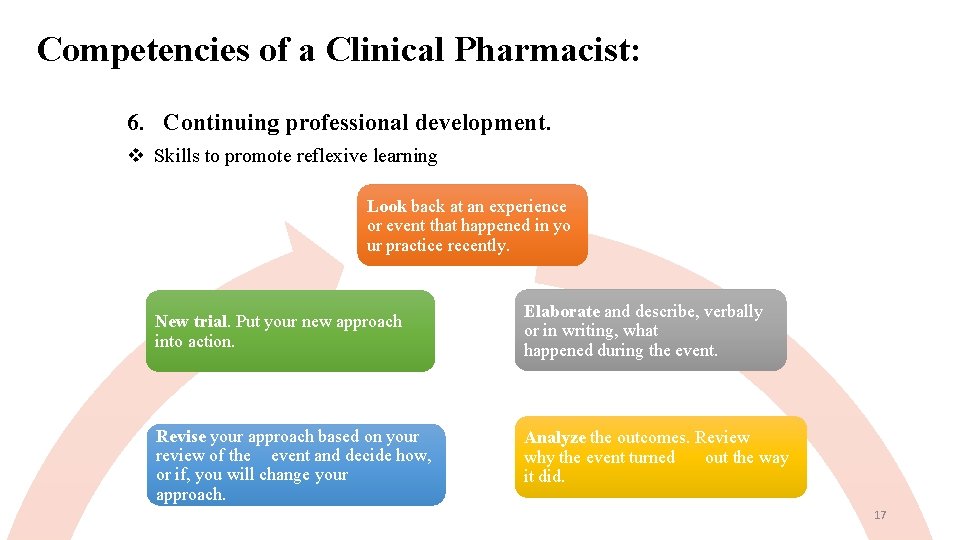
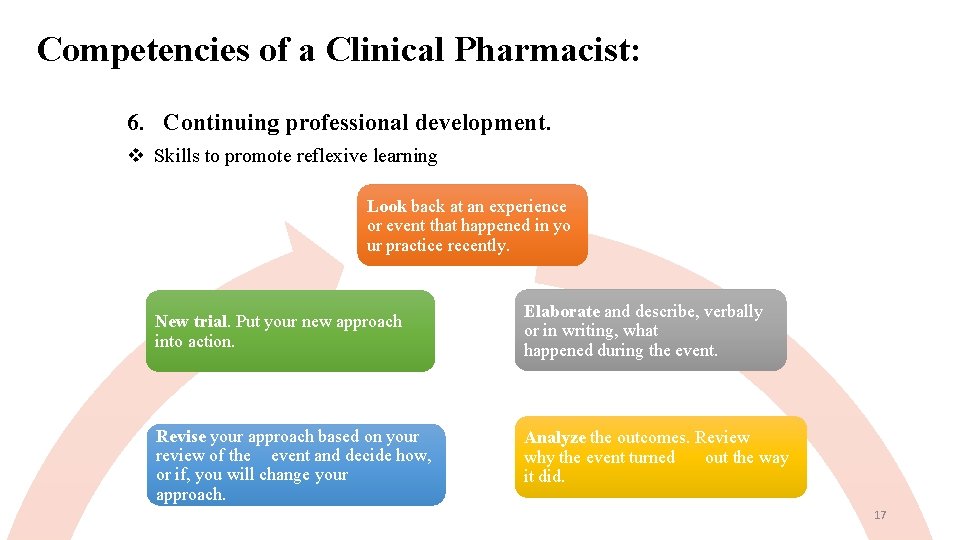
Competencies of a Clinical Pharmacist: 6. Continuing professional development. Skills to promote reflexive learning Look back at an experience or event that happened in yo ur practice recently. New trial. Put your new approach into action. Elaborate and describe, verbally or in writing, what happened during the event. Revise your approach based on your review of the event and decide how, or if, you will change your approach. Analyze the outcomes. Review why the event turned out the way it did. 17
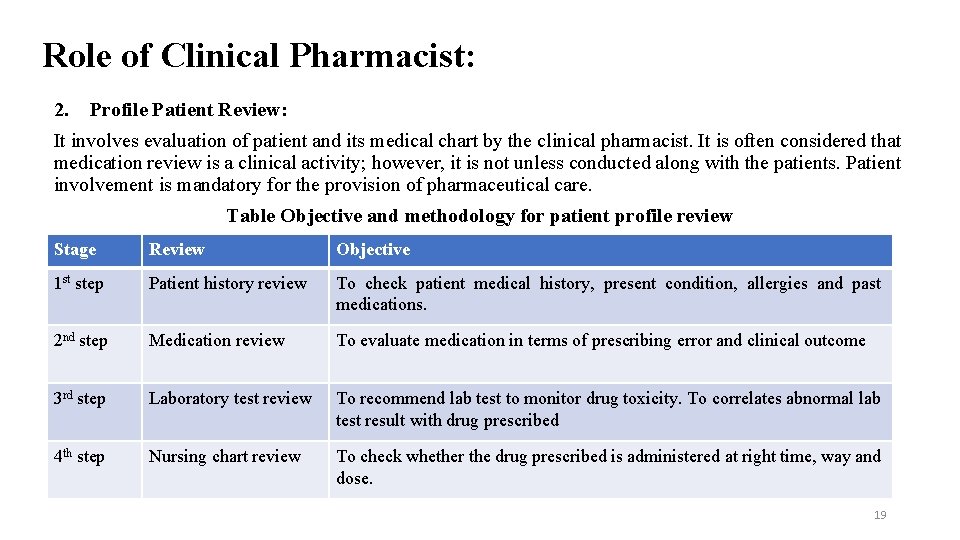
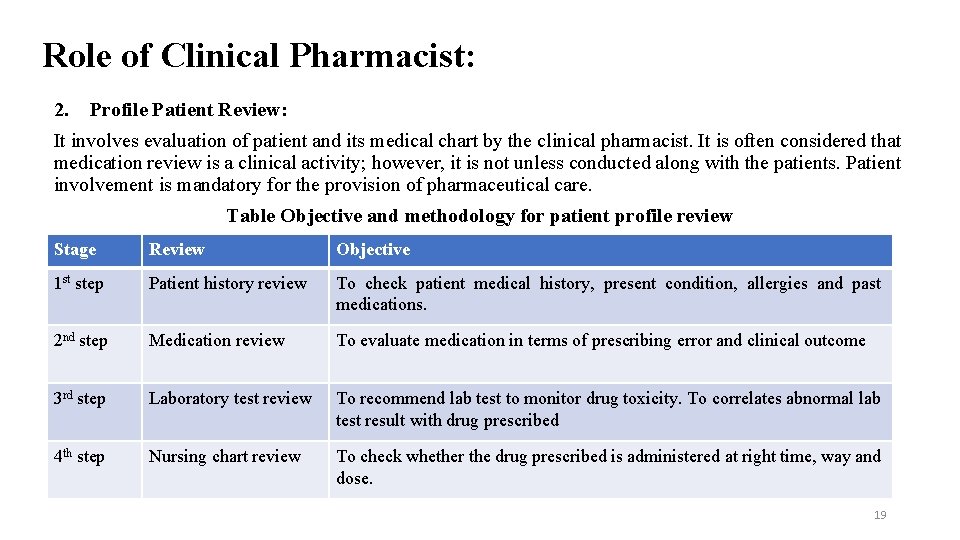
Role of Clinical Pharmacist: 1. Patient Medication History: It involves gathering and recording of information regarding past and present medications used by the patient through interview and reviewing of past medical records. Stage Objective Procedure Create rapport (Gaining patient’s confidence) Step 1: Confirm the patient’s identity. Step 2: Pay regards. Step 3: Self introduction (Name, position). Step 4: Reason of visit and time required. Step 5: Start taking medication history of the patient. During history taking Gather information Step 6: Ask question with respect to format. After history taking Documentation analysis Before history taking medication & Step 7: Express gratitude Step 8: Collect and review past medical record. Step 9: Document essential data. 18
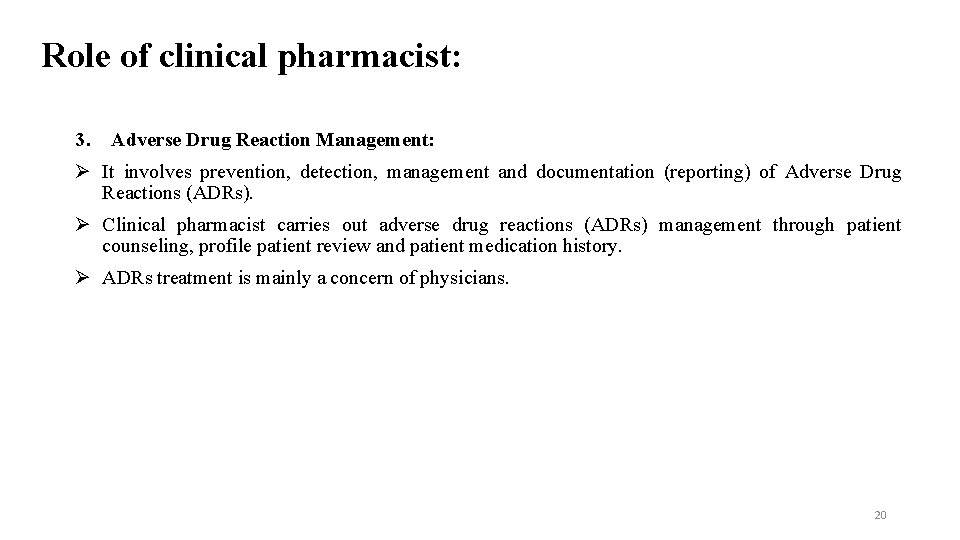
Role of Clinical Pharmacist: 2. Profile Patient Review: It involves evaluation of patient and its medical chart by the clinical pharmacist. It is often considered that medication review is a clinical activity; however, it is not unless conducted along with the patients. Patient involvement is mandatory for the provision of pharmaceutical care. Table Objective and methodology for patient profile review Stage Review Objective 1 st step Patient history review To check patient medical history, present condition, allergies and past medications. 2 nd step Medication review To evaluate medication in terms of prescribing error and clinical outcome 3 rd step Laboratory test review To recommend lab test to monitor drug toxicity. To correlates abnormal lab test result with drug prescribed 4 th step Nursing chart review To check whether the drug prescribed is administered at right time, way and dose. 19
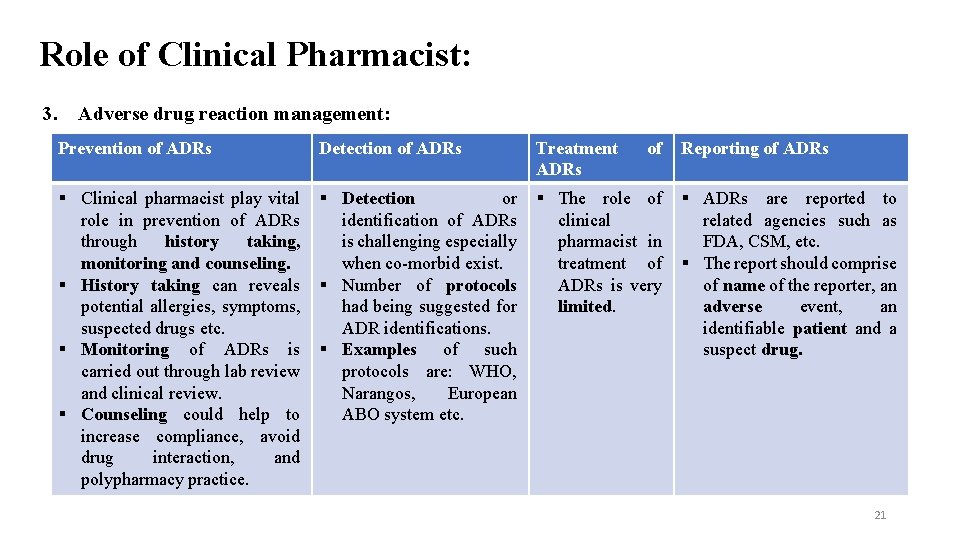
Role of clinical pharmacist: 3. Adverse Drug Reaction Management: It involves prevention, detection, management and documentation (reporting) of Adverse Drug Reactions (ADRs). Clinical pharmacist carries out adverse drug reactions (ADRs) management through patient counseling, profile patient review and patient medication history. ADRs treatment is mainly a concern of physicians. 20
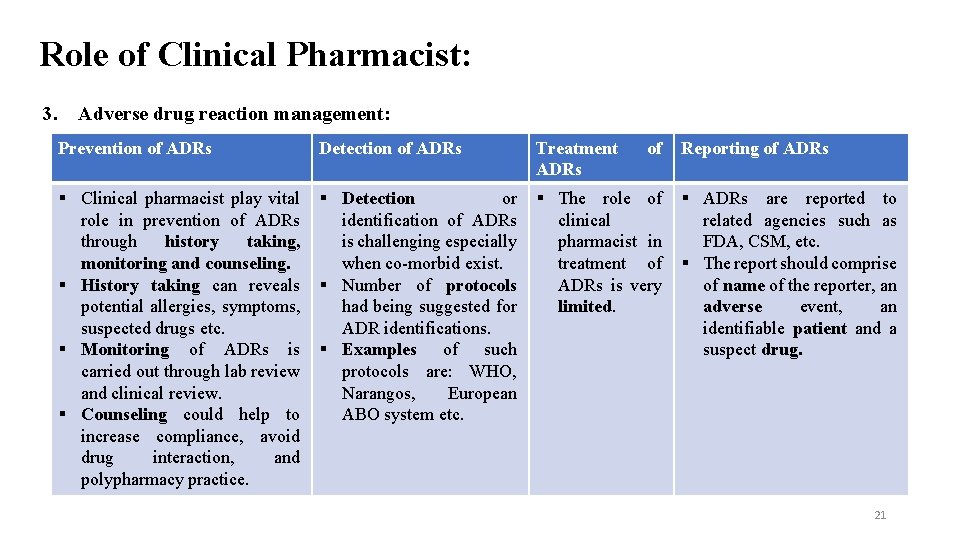
Role of Clinical Pharmacist: 3. Adverse drug reaction management: Prevention of ADRs Detection of ADRs Treatment ADRs of § Clinical pharmacist play vital role in prevention of ADRs through history taking, monitoring and counseling. § History taking can reveals potential allergies, symptoms, suspected drugs etc. § Monitoring of ADRs is carried out through lab review and clinical review. § Counseling could help to increase compliance, avoid drug interaction, and polypharmacy practice. § Detection or identification of ADRs is challenging especially when co-morbid exist. § Number of protocols had being suggested for ADR identifications. § Examples of such protocols are: WHO, Narangos, European ABO system etc. § The role of clinical pharmacist in treatment of ADRs is very limited. Reporting of ADRs § ADRs are reported to related agencies such as FDA, CSM, etc. § The report should comprise of name of the reporter, an adverse event, an identifiable patient and a suspect drug. 21
Role of Clinical Pharmacist: 4. Therapeutic Drug Monitoring (TDM): It involves application of clinical pharmacokinetic for monitoring drug efficacy and toxicities. The drugs that are commonly monitored are gentamicin, amikacin, tobramycin, vancomycin, carbamazepine, phenytoin, valproic acid, lithium, theophylline, cyclosporine, digoxin, lidocaine, amitriptyline, nortriptyline and imipramine. The procedure of TDM comprises of six steps which are: i. Ordering: Physician request for consultation for clinical pharmacokinetic services. ii. Sample taking: Biological sample is taken by the team. iii. Analysis of sample: Analysis of biological sample takes place in the laboratory. iv. Result issue: Laboratory issues the drug concentration level result and notifies if it is sub-therapeutic to the clinical pharmacist. v. Interpretation of result: clinical pharmacist conduct the calculation with respect to results. vi. Action: With respect to calculation, dose adjustment are carried out. 22
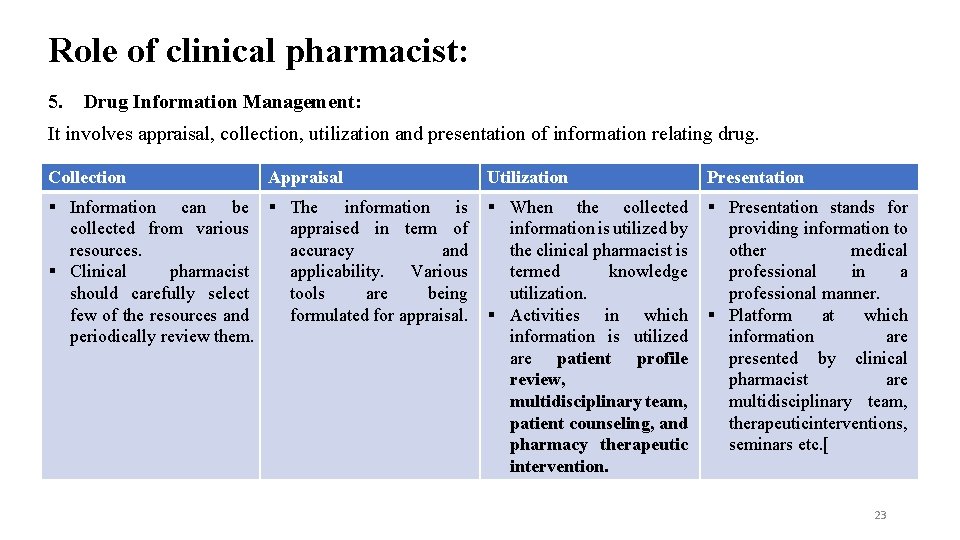
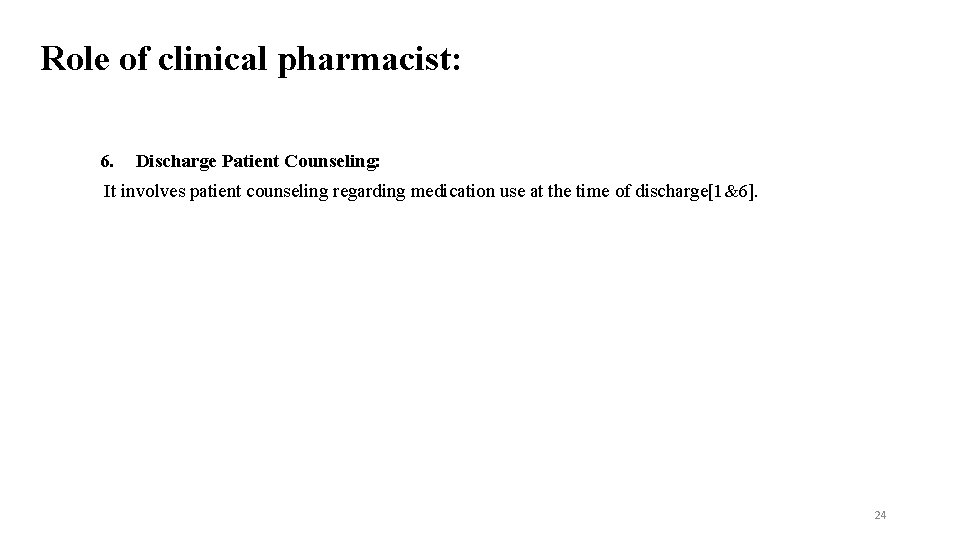
Role of clinical pharmacist: 5. Drug Information Management: It involves appraisal, collection, utilization and presentation of information relating drug. Collection Appraisal § Information can be § The information is collected from various appraised in term of resources. accuracy and § Clinical pharmacist applicability. Various should carefully select tools are being few of the resources and formulated for appraisal. periodically review them. Utilization Presentation § When the collected information is utilized by the clinical pharmacist is termed knowledge utilization. § Activities in which information is utilized are patient profile review, multidisciplinary team, patient counseling, and pharmacy therapeutic intervention. § Presentation stands for providing information to other medical professional in a professional manner. § Platform at which information are presented by clinical pharmacist are multidisciplinary team, therapeuticinterventions, seminars etc. [ 23
Role of clinical pharmacist: 6. Discharge Patient Counseling: It involves patient counseling regarding medication use at the time of discharge[1&6]. 24
References: 1. Amir, M. , 2012. Clinical pharmacy practice: An activity based definition for pharmacy students of developing countries. Archives of Pharmacy Practice, 3(3), p. 193. 2. Khan, F. U. , Waqas, N. , Ihsan, A. U. , Khongorzul, P. , Wazir, J. , Gang, W. , Mengqi, Y. , Xiaoqian, L. , Han, L. and Xiaohui, Z. , 2019. Analysis of the Qualities Matching New Classification of Clinical Pharmacist. Indian Journal of Pharmaceutical Sciences, 81(1), pp. 2 -10. 3. Saseen, J. J. , Ripley, T. L. , Bondi, D. , Burke, J. M. , Cohen, L. J. , Mc. Bane, S. , Mc. Connell, K. J. , Sackey, B. , Sanoski, C. , Simonyan, A. and Taylor, J. , 2017. ACCP clinical pharmacist competencies. Pharmacotherapy: The Journal of Human Pharmacology and Drug Therapy, 37(5), pp. 630 -636. 4. Pharmaceutical Care Practice: The Clinician's Guide > Chapter 12. Acquiring the Clinical Skills You Need to Practice > 5. Pharmaceutical Care Practice: The Clinician's Guide > Chapter 11. Acquiring the Knowledge You Need to Practice > 6. American College of Clinical Pharmacy, 2014. Standards of practice for clinical pharmacists. Pharmacotherapy: The Journal of Human Pharmacology and Drug Therapy, 34(8), pp. 794797. 25