Computed Tomography RAD 309 Data Acquisition Data Acquisition
- Slides: 40
Computed Tomography RAD 309 Data Acquisition
Data Acquisition Data acquisition represents the first step in process of image production ¢ X-ray tube & detectors collect information systematically ¢ Collect large number of x ray transmissions around the patient ¢
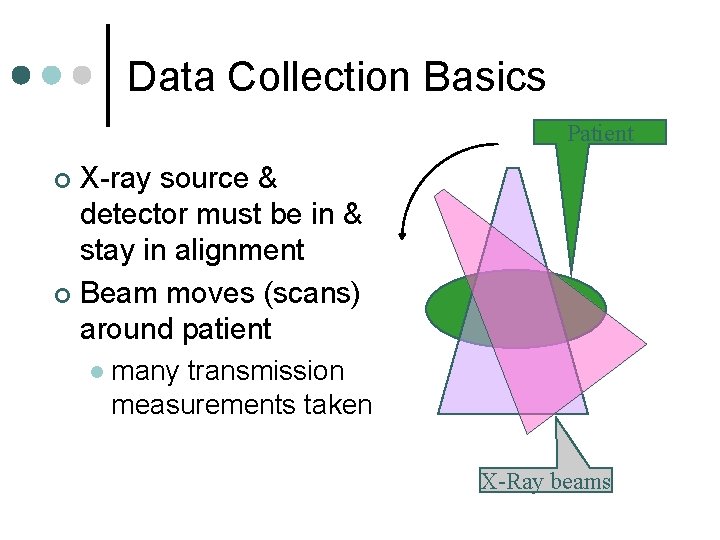
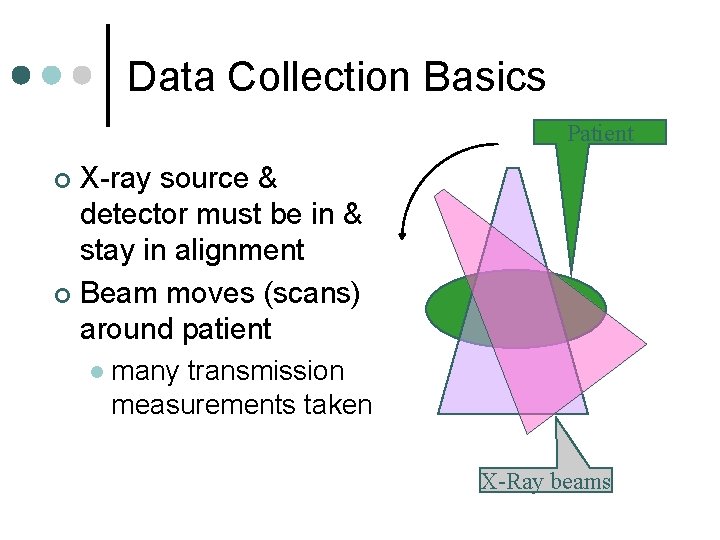
Data Collection Basics Patient X-ray source & detector must be in & stay in alignment ¢ Beam moves (scans) around patient ¢ l many transmission measurements taken X-Ray beams
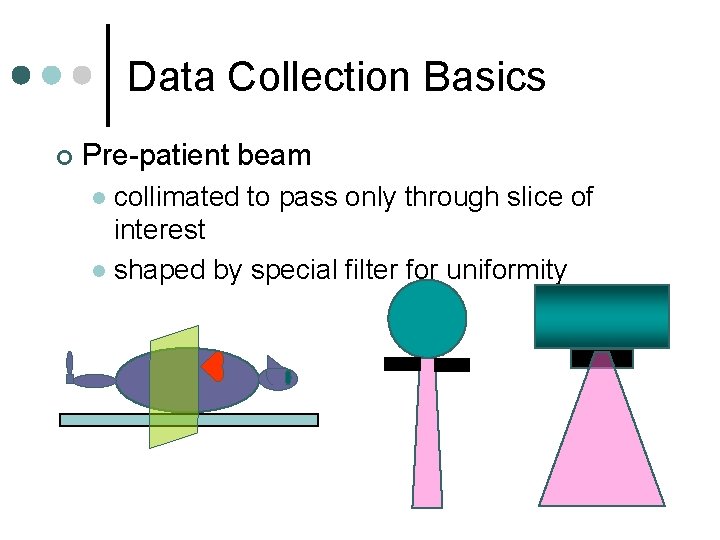
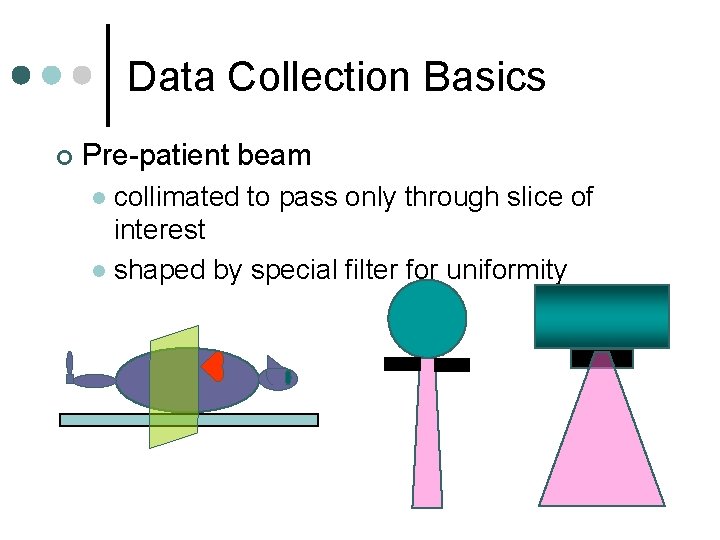
Data Collection Basics ¢ Pre-patient beam collimated to pass only through slice of interest l shaped by special filter for uniformity l
Data Collection Basics (cont) Beam attenuated by patient ¢ Transmitted photons detected by scanner ¢ Detected photon intensity converted to electrical signal (analog) ¢ Electrical signal converted to digital value ¢ l ¢ A to D converter Digital value sent to reconstruction computer
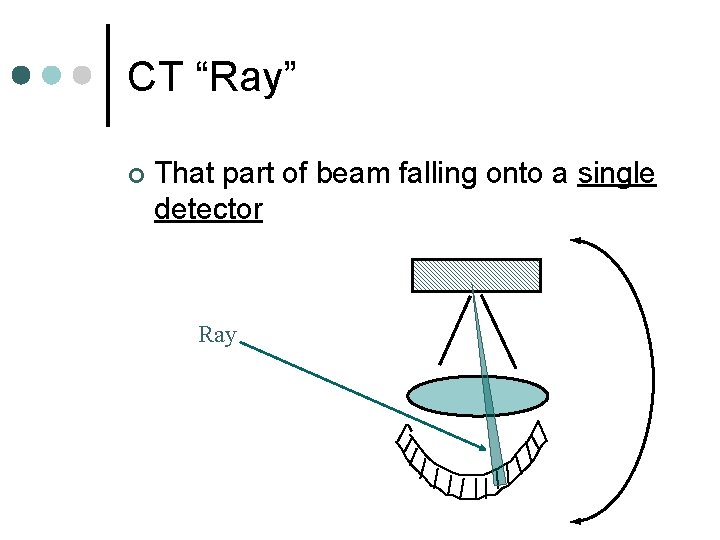
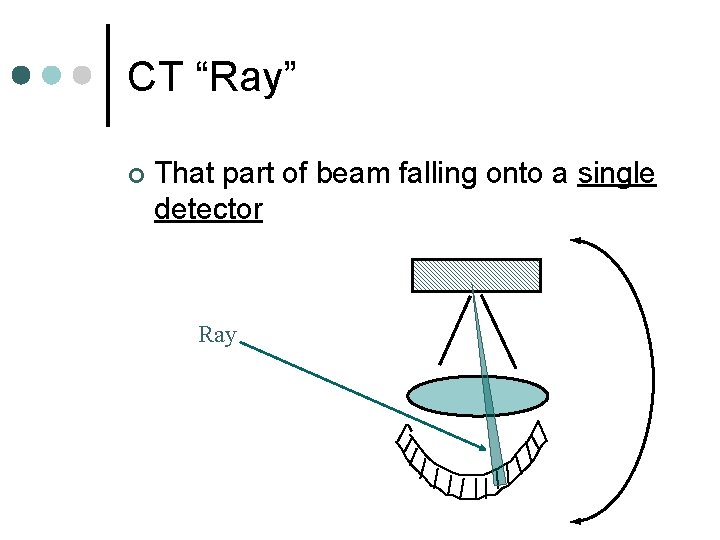
CT “Ray” ¢ That part of beam falling onto a single detector Ray
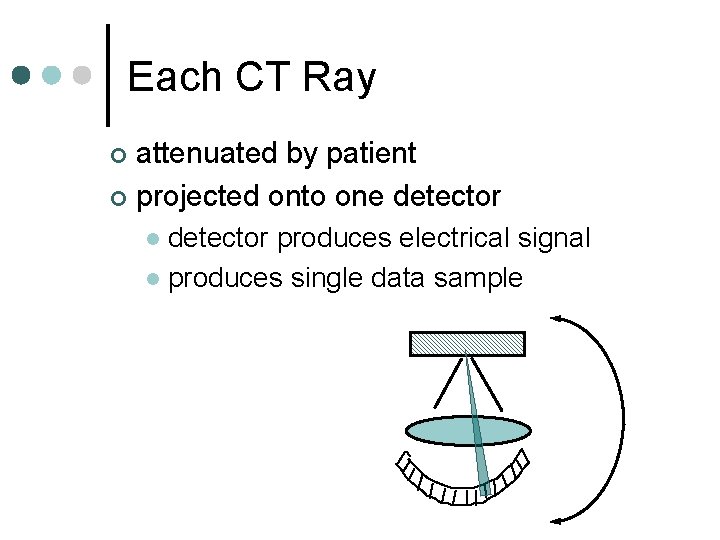
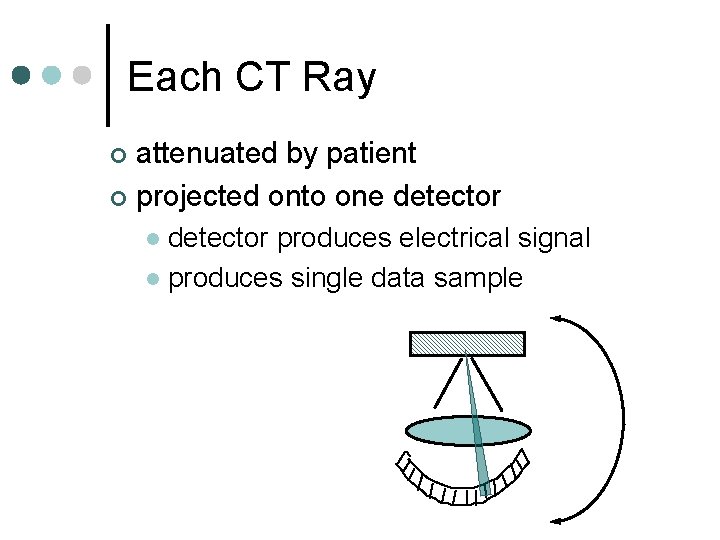
Each CT Ray attenuated by patient ¢ projected onto one detector ¢ detector produces electrical signal l produces single data sample l
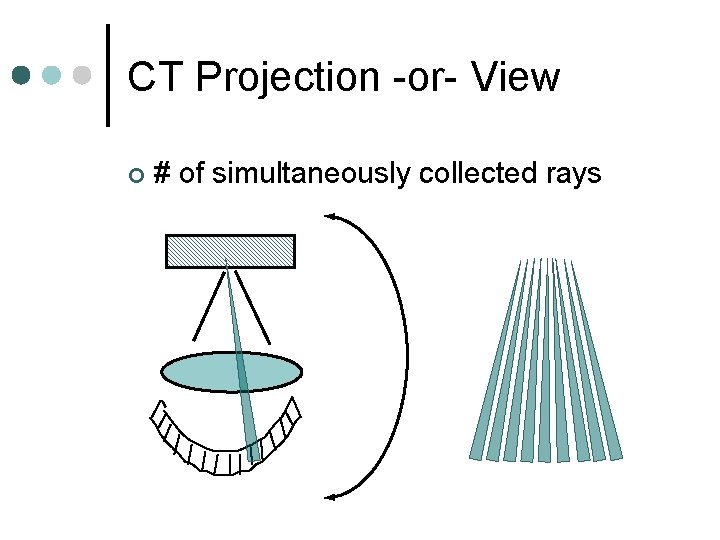
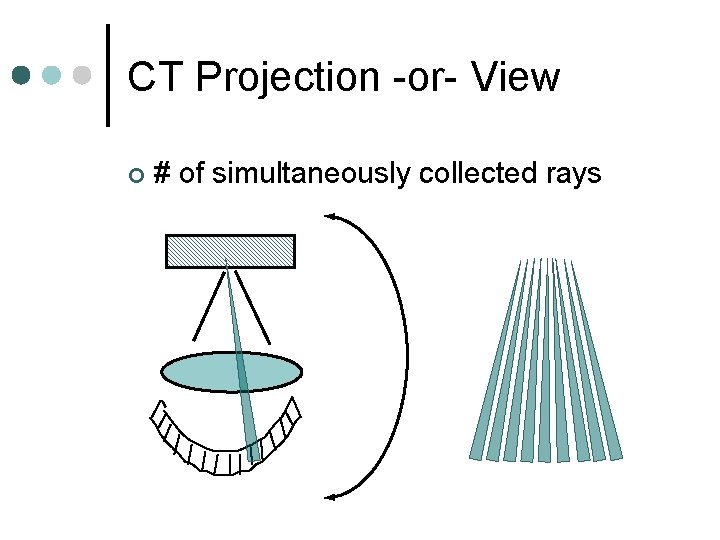
CT Projection -or- View ¢ # of simultaneously collected rays
Acquisition Geometries ¢ Pencil Beam ¢ Fan Beam ¢ Spiral
DA Geometries 1. 2. 3. 4. 5. 6. 7. Parallel beam, translate rotate motion Fan beam, complete rotation tube/detector Fan beam, complete rotation of tube around stationary ring of detectors Special: high speed CT, stationary/stationary, multiple targets tube Spiral, rotate/translate Multiple detector rows
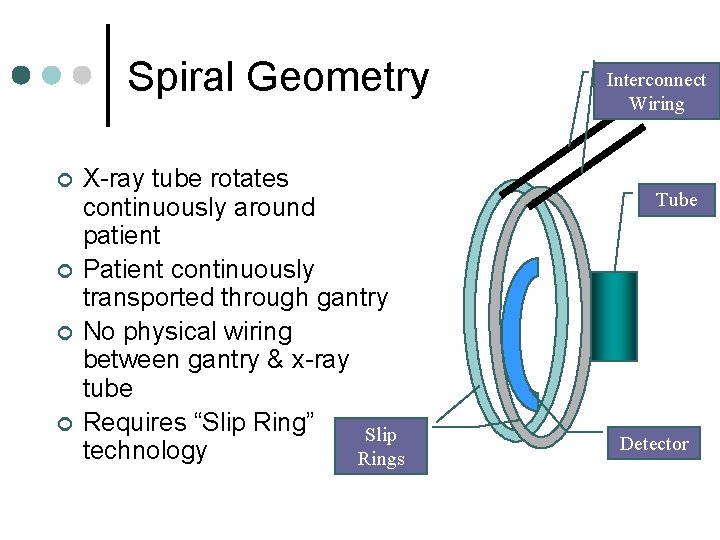
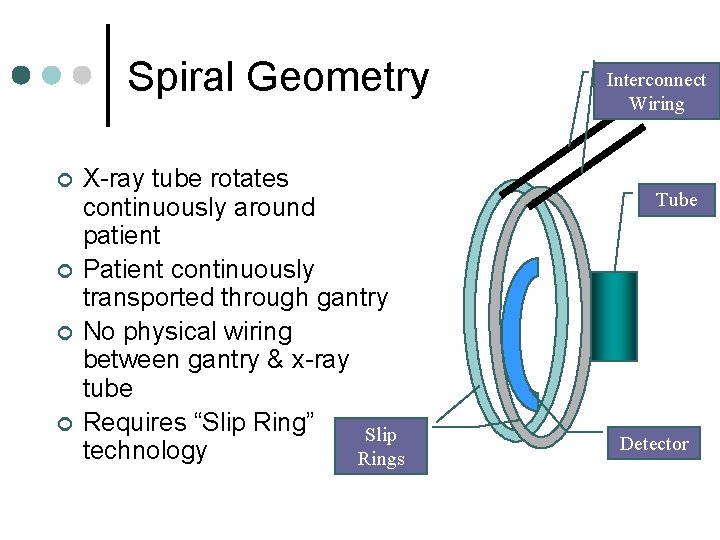
Spiral Geometry ¢ ¢ X-ray tube rotates continuously around patient Patient continuously transported through gantry No physical wiring between gantry & x-ray tube Requires “Slip Ring” Slip technology Rings Interconnect Wiring Tube Detector
X Ray System Initially used low energy gamma rays ¢ Problem: low radiation intensity rate, large source size, low source strength, high cost ¢ Use of X ray tubes ¢ Benefit: high radiation intensity, high contrast ct scanning ¢ Problem: heterogeneous beam , does not obay Lamber-Beer Exponential Law ¢
Radioactive Source instead of an X-Ray Tube? ¢ High intensity required l ¢ X-ray tubes produce higher intensities than sources Single energy spectrum desired Produced by radioactive source l X-ray tubes produce spectrum of energies l
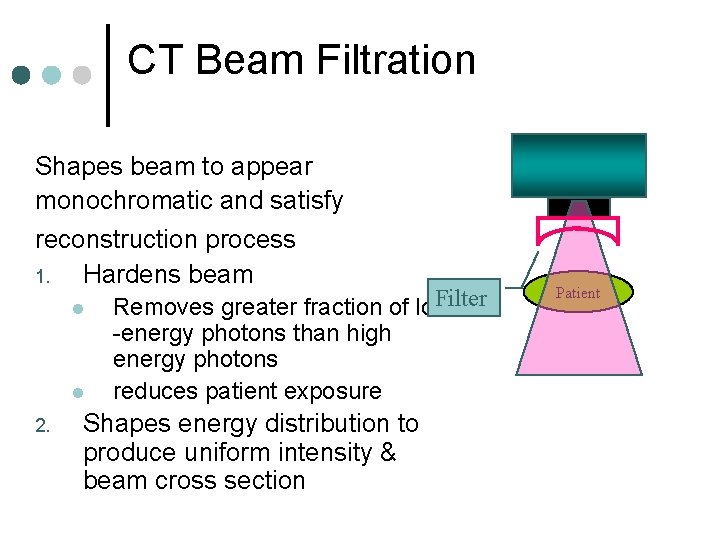
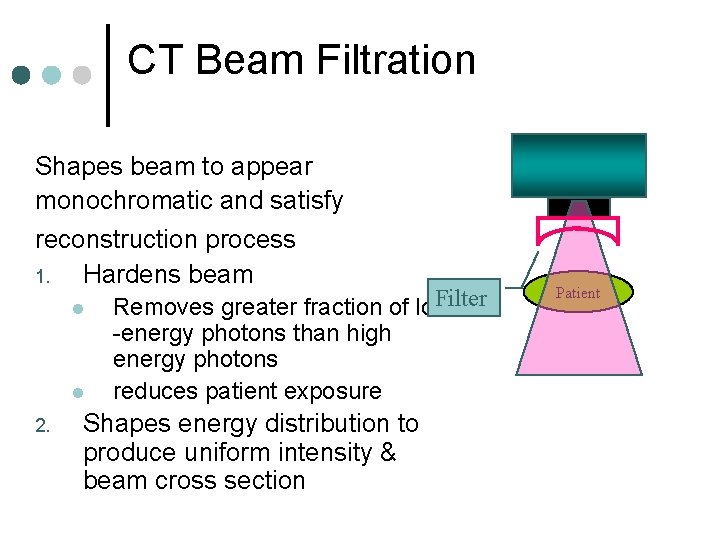
CT Beam Filtration Shapes beam to appear monochromatic and satisfy reconstruction process 1. Hardens beam l l 2. Filter Removes greater fraction of low -energy photons than high energy photons reduces patient exposure Shapes energy distribution to produce uniform intensity & beam cross section Patient
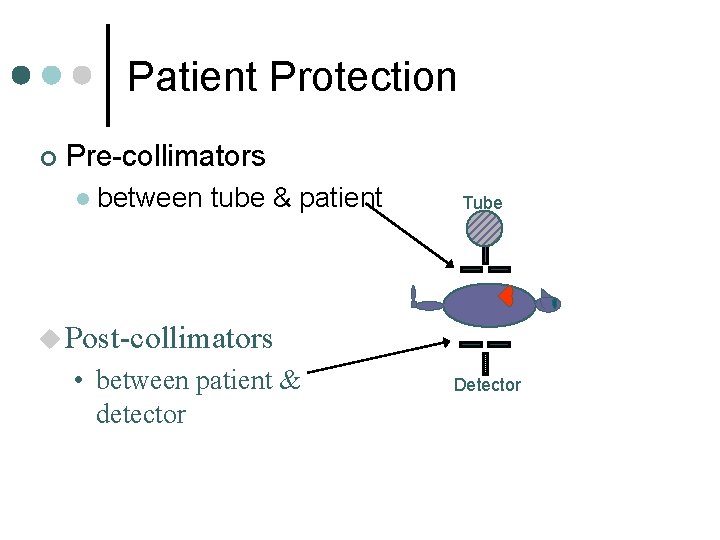
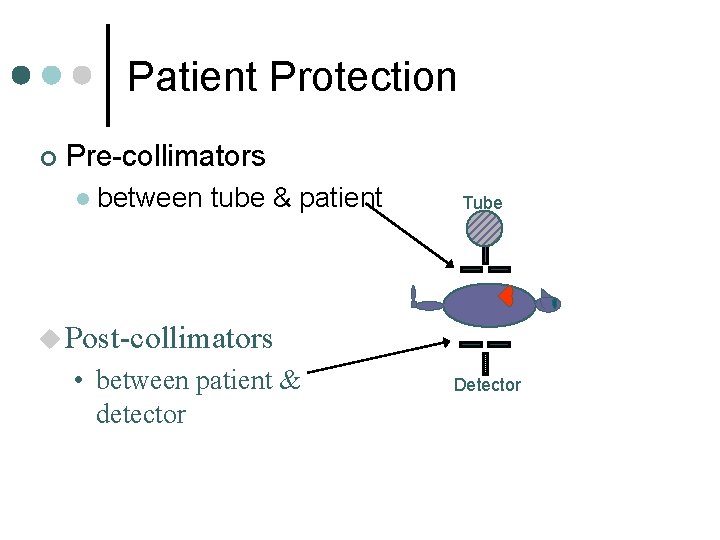
Patient Protection ¢ Pre-collimators l between tube & patient Tube u Post-collimators • between patient & detector Detector
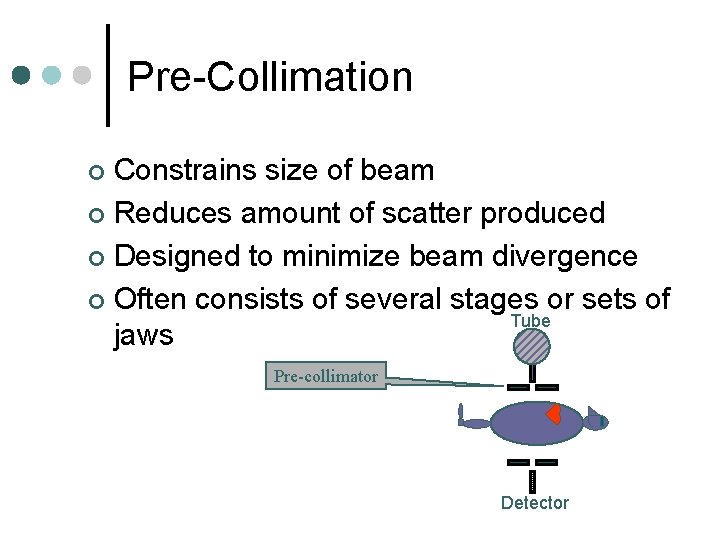
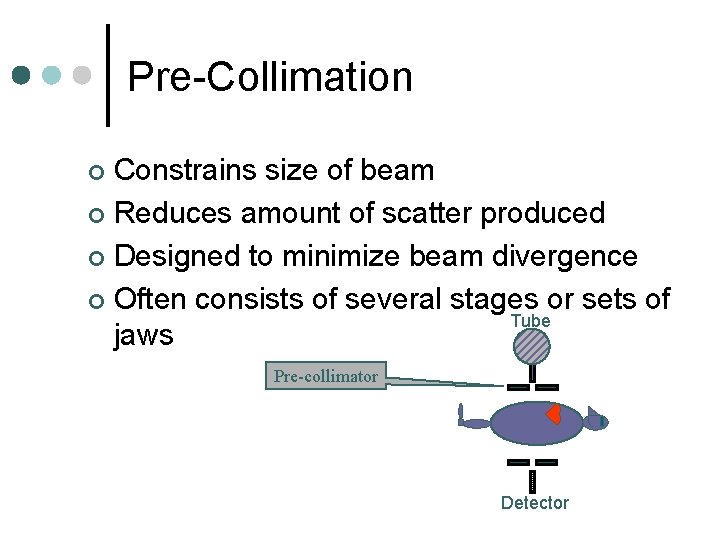
Pre-Collimation Constrains size of beam ¢ Reduces amount of scatter produced ¢ Designed to minimize beam divergence ¢ Often consists of several stages or sets of Tube jaws ¢ Pre-collimator Detector
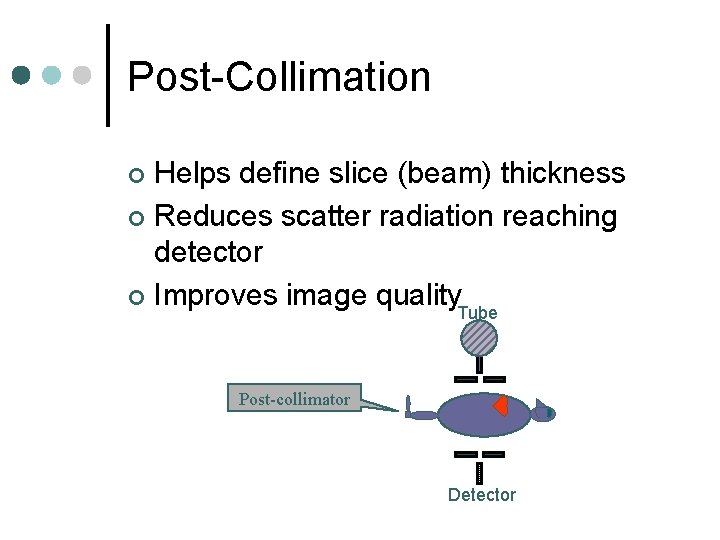
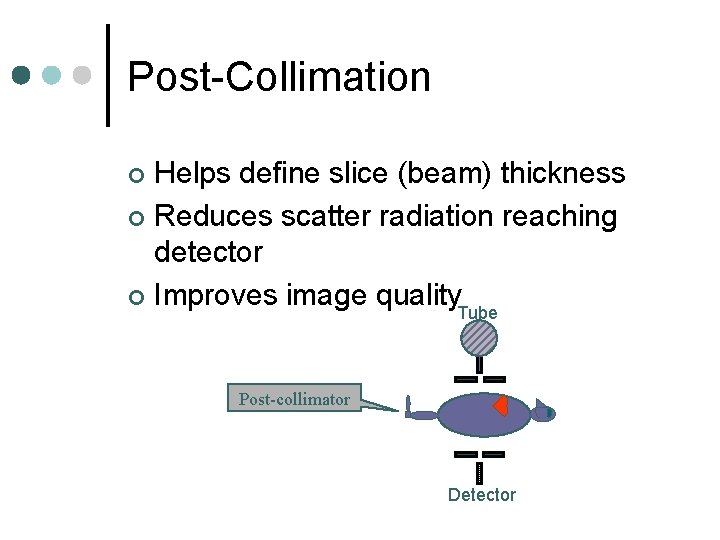
Post-Collimation Helps define slice (beam) thickness ¢ Reduces scatter radiation reaching detector ¢ Improves image quality Tube ¢ Post-collimator Detector
Detectors Capture radiation from patient ¢ Converts to electrical signal ¢ Then they are converted to binary coded information ¢
CT Detector Characteristics Efficiency ¢ Response time ¢ Dynamic range ¢ Reproducibility and Stability ¢
1. Efficiency ¢ Ability to capture, absorb & convert x-ray photons to electrical signals
Efficiency Components a. Capture efficiency Efficiency of detector to obtain transmitted photons from patient l Size of detector area, distance between 2 detectors l b. Absorption efficiency no. of photons absorbed l Z , density, size, thickness of detector l c. Conversion efficiency l fraction of absorbed energy which produce signal
Overall Detector Efficiency capture efficiency X absorption efficiency X conversion efficiency
Absorption Efficiency ¢ Depends upon detector’s atomic # l density l size l thickness l ¢ Depends on beam spectrum
2. Response Time “Speed with which detector can detect an x ray event and recover to detect the next one” ¢ Minimum time after detection of 1 st event when detector can detect 2 nd event ¢ If time between events shorter than response time, second event may not be detected ¢ Shorter response time better ¢
3. Dynamic Range Ability to faithfully detect large range of intensities ¢ “Ratio of largest signal to be measured to the precision of the smallest signal to be discriminated” ¢ Typical dynamic range: 1, 000: 1 ¢ l much better than film
4. Stability “Steadiness” of detector system ¢ Consistency of detector signal over time ¢ The less stable, the more frequently calibration required ¢
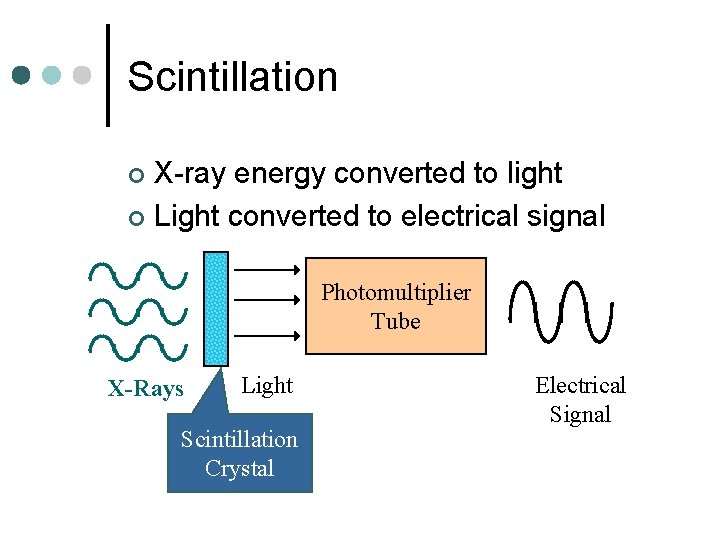
Detector Types 2 principles: ¢ Convert x-ray into light ---electrical signal ¢ Scintillation detector Convert x-ray directly into electrical signal ¢ Gas ionization detector ¢
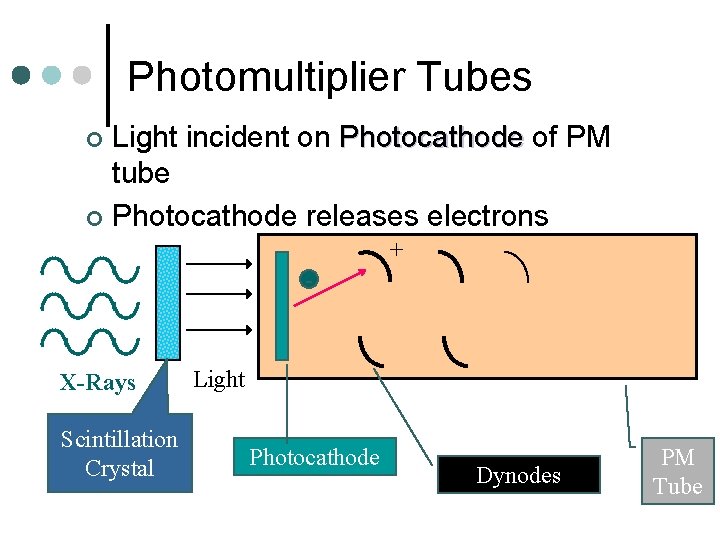
Scintillation Detectors Crystal couple to photomultiplier tube ¢ X ray falls on crystal ---light flashes (glow) ¢ Light directed to PM ¢ Light hits Photocathode in PM and releases electrons ¢
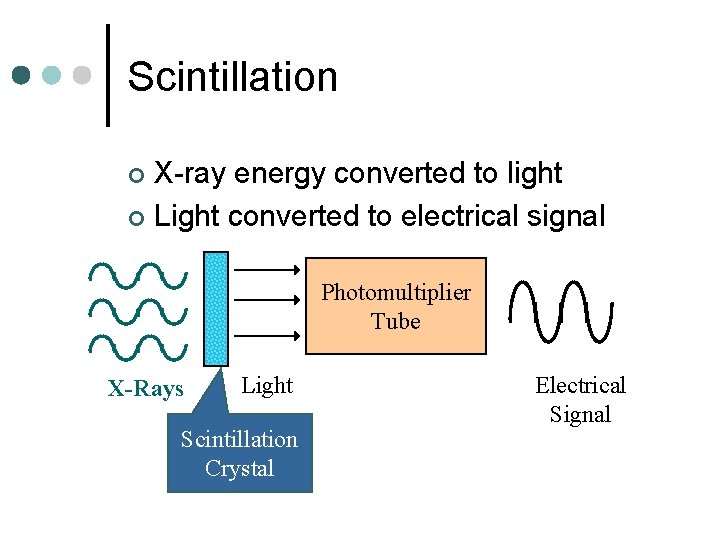
Scintillation X-ray energy converted to light ¢ Light converted to electrical signal ¢ Photomultiplier Tube X-Rays Light Scintillation Crystal Electrical Signal
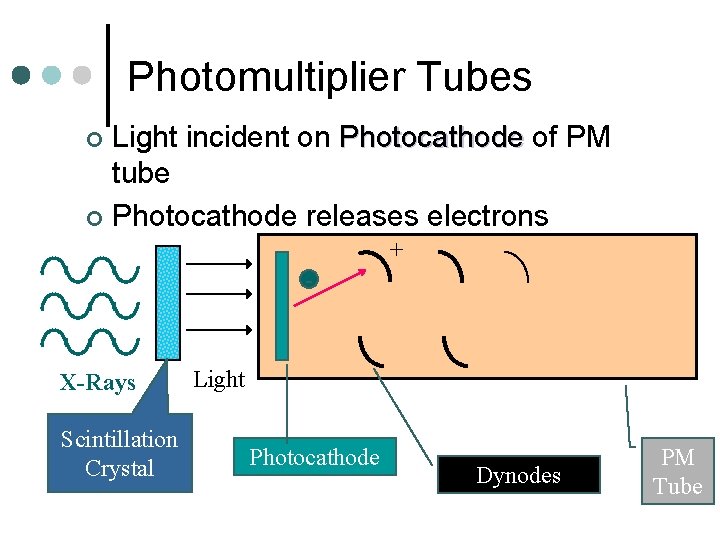
Photomultiplier Tubes Light incident on Photocathode of PM tube ¢ Photocathode releases electrons ¢ + - X-Rays Scintillation Crystal Light Photocathode Dynodes PM Tube
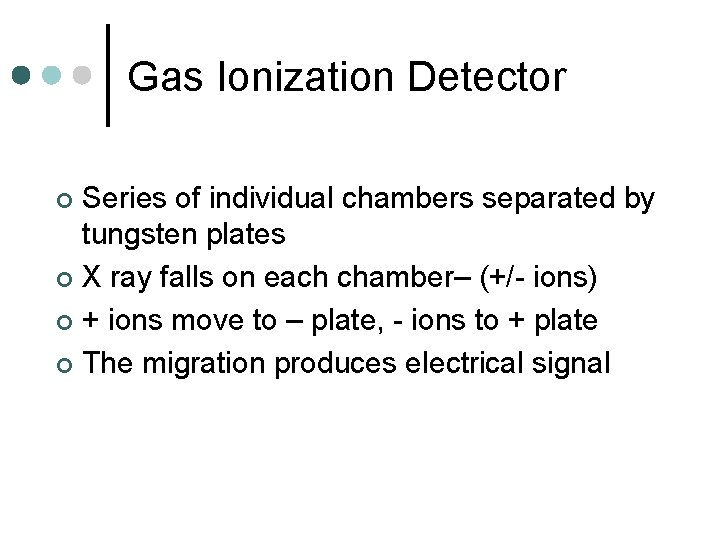
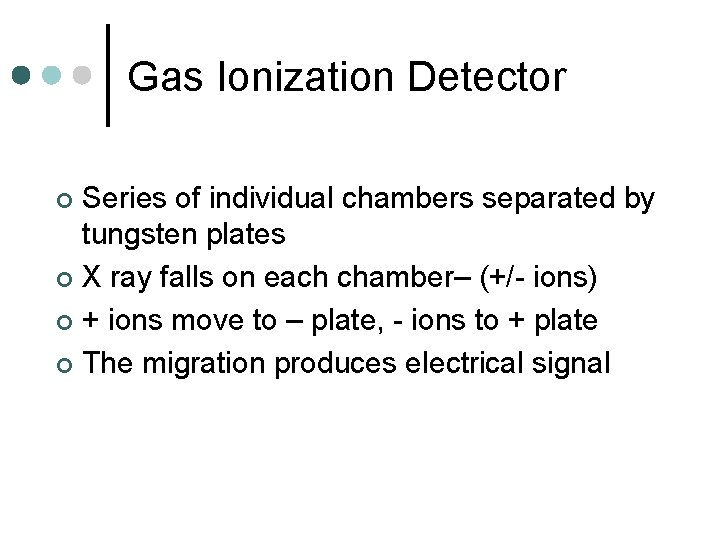
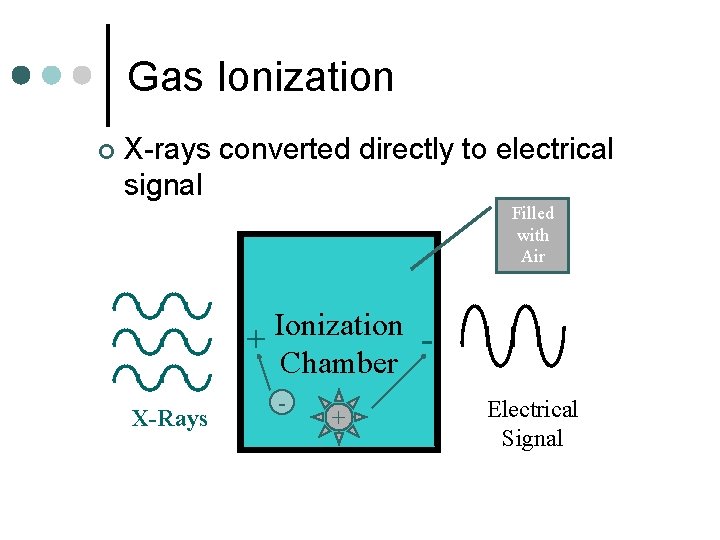
Gas Ionization Detector Series of individual chambers separated by tungsten plates ¢ X ray falls on each chamber– (+/- ions) ¢ + ions move to – plate, - ions to + plate ¢ The migration produces electrical signal ¢
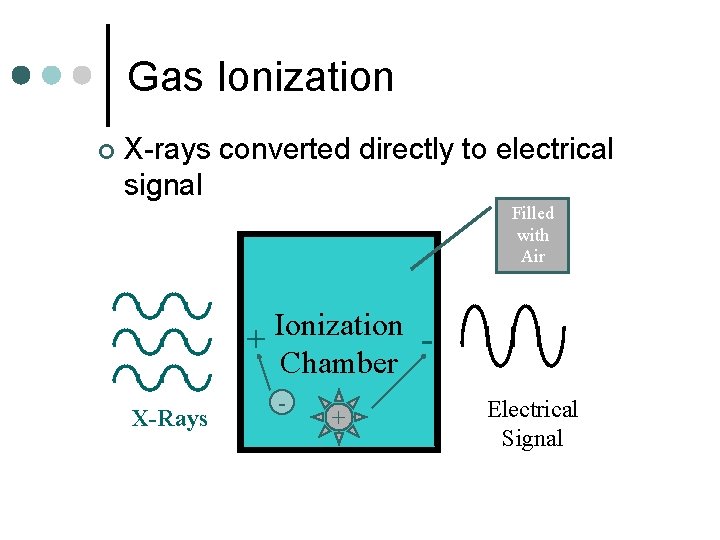
Gas Ionization ¢ X-rays converted directly to electrical signal Filled with Air Ionization + Chamber X-Rays - + Electrical Signal
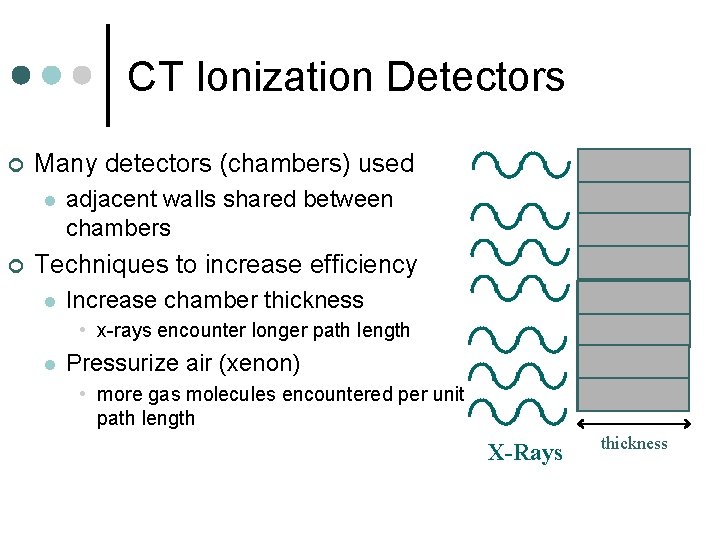
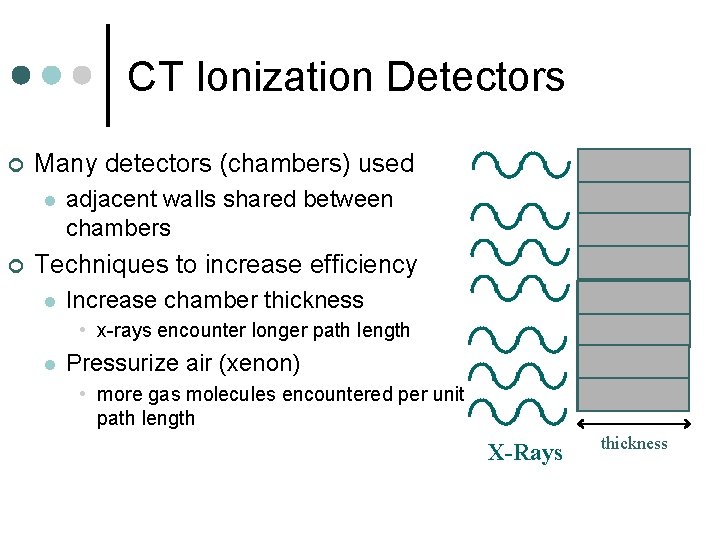
CT Ionization Detectors ¢ Many detectors (chambers) used l ¢ adjacent walls shared between chambers Techniques to increase efficiency l Increase chamber thickness • x-rays encounter longer path length l Pressurize air (xenon) • more gas molecules encountered per unit path length X-Rays thickness
Detector Array Slice by Slice – one arc of detector array ¢ Volume – one arc of detector array, acquires volume of tissue then separated by computed to slice by slice ¢
DAS Detector electronics ¢ Location: between detector and computer ¢ Role of translator ¢ Measure transmitted radiation beam l Encodes measurement to binary data l Transmits binary data to computer l
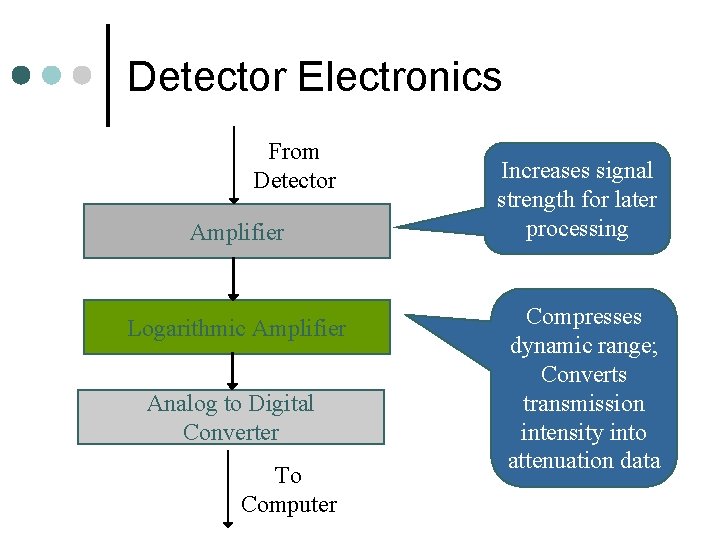
Components of DAS Amplifier ¢ Log Amplifier ¢ Analog to Digital Converter (digital data) ¢ Digital Transmission to computer ¢
Log Amplification Transmission measurement data must be changed into attenuation and thickness data ¢ Attenuation = log of transmission x thickness ¢
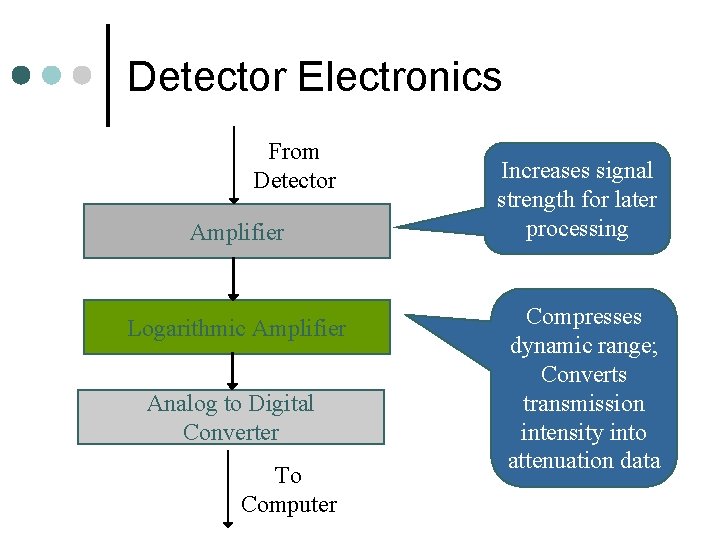
Detector Electronics From Detector Amplifier Logarithmic Amplifier Analog to Digital Converter To Computer Increases signal strength for later processing Compresses dynamic range; Converts transmission intensity into attenuation data
DA and Sampling Radiation falling on detector ¢ Each samples the beam intensity on it ¢ Not enough samples = artifacts appear ¢ To increase number of measurement/samples available for reconstruction and improve image quality ¢
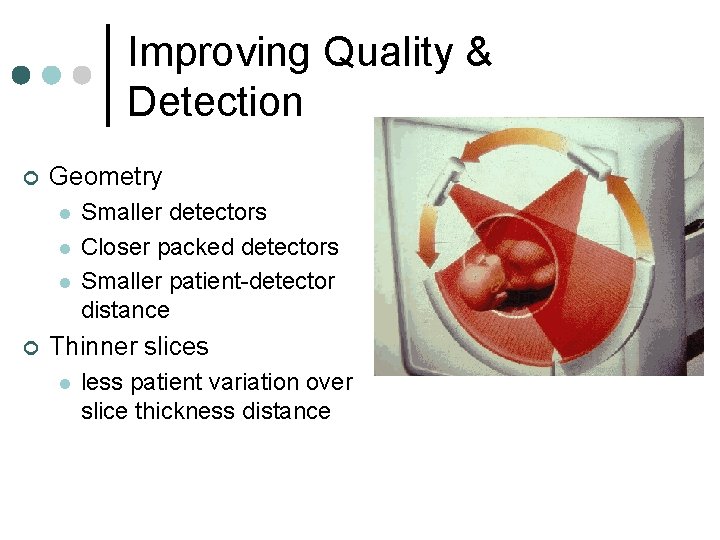
Improving Quality & Detection ¢ Geometry l l l ¢ Smaller detectors Closer packed detectors Smaller patient-detector distance Thinner slices l less patient variation over slice thickness distance