Compression Devices In the hospital all compression devices

- Slides: 11
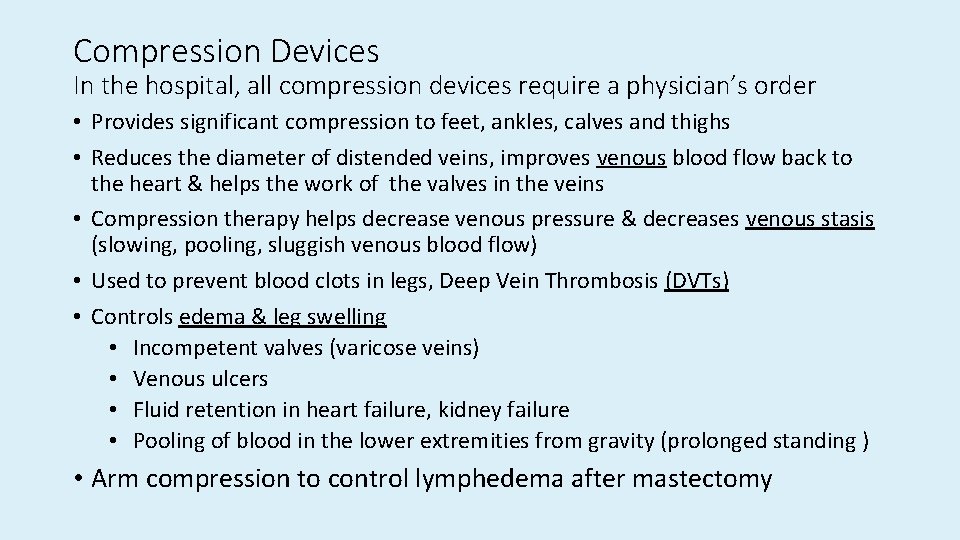
Compression Devices In the hospital, all compression devices require a physician’s order • Provides significant compression to feet, ankles, calves and thighs • Reduces the diameter of distended veins, improves venous blood flow back to the heart & helps the work of the valves in the veins • Compression therapy helps decrease venous pressure & decreases venous stasis (slowing, pooling, sluggish venous blood flow) • Used to prevent blood clots in legs, Deep Vein Thrombosis (DVTs) • Controls edema & leg swelling • Incompetent valves (varicose veins) • Venous ulcers • Fluid retention in heart failure, kidney failure • Pooling of blood in the lower extremities from gravity (prolonged standing ) • Arm compression to control lymphedema after mastectomy
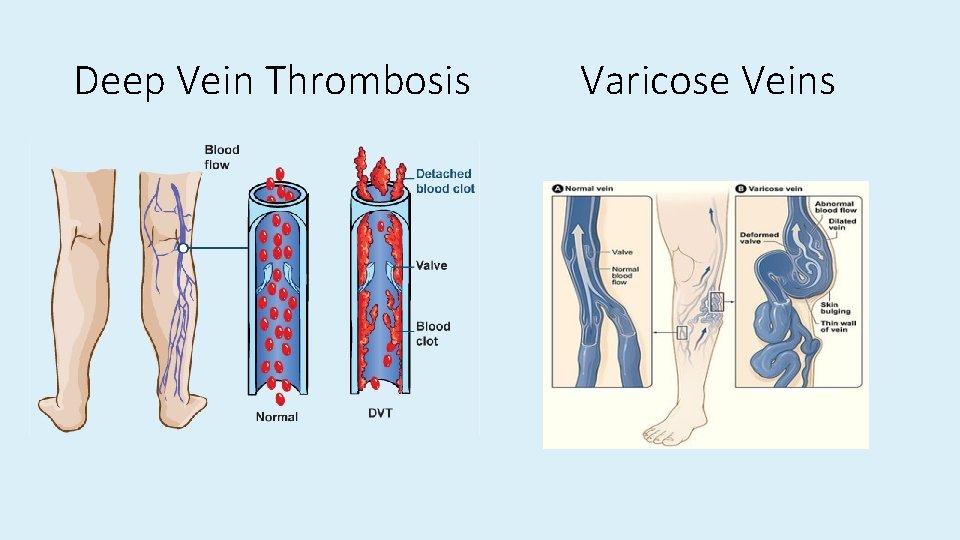
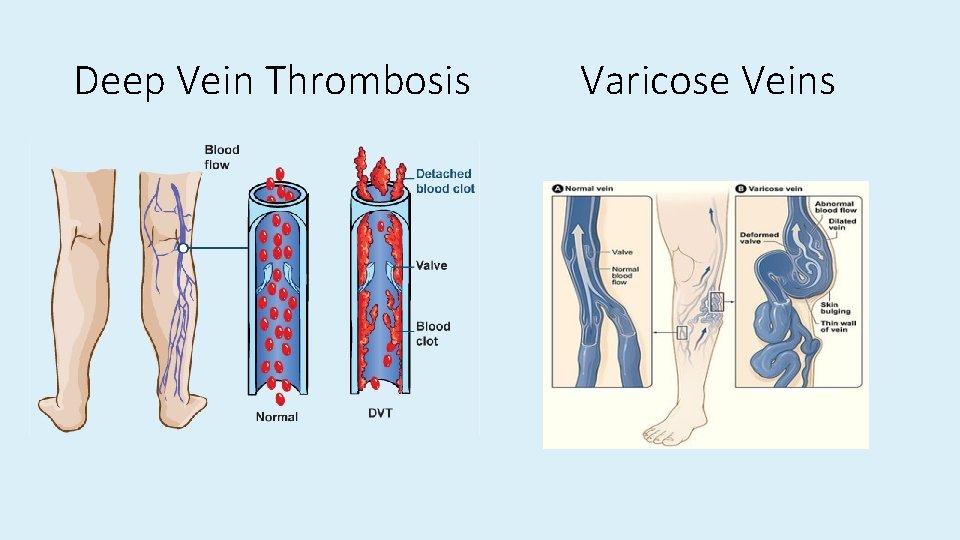
Deep Vein Thrombosis Varicose Veins
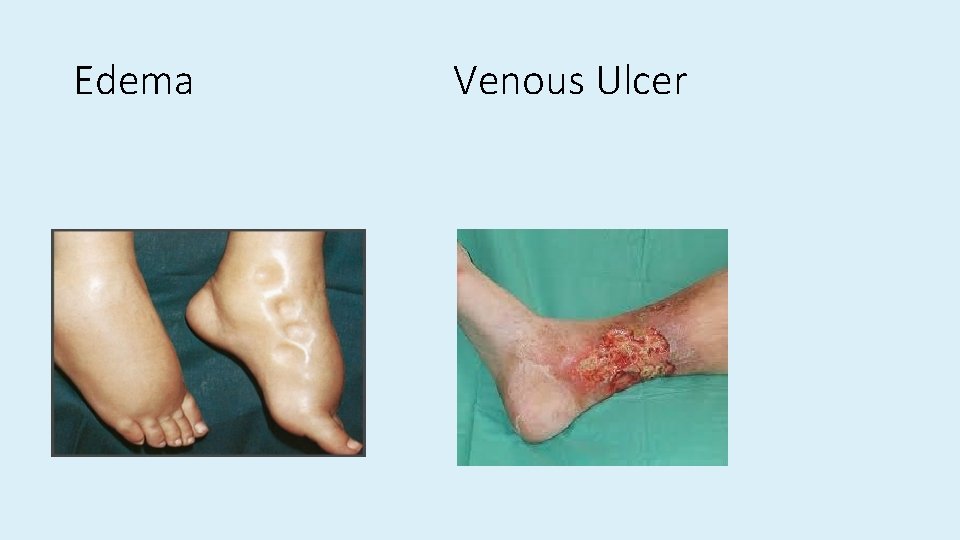
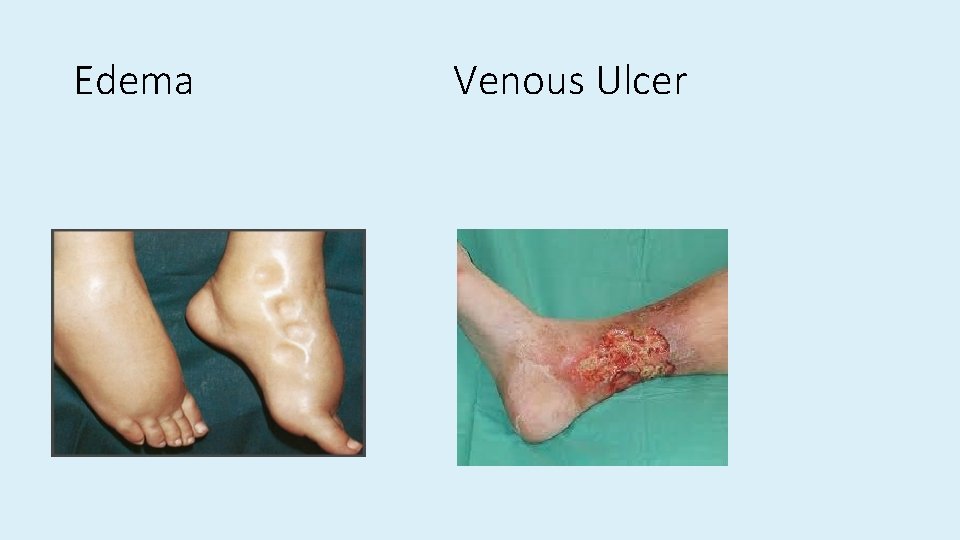
Edema Venous Ulcer

Compression Stockings • Also known as: • Elastic stockings • Anti-embolism stockings • T. E. D Hose • 2 Types: knee high, thigh • Come in various sizes • Medical graduated compression stockings (medium, or heavy) weight 30 -40 mm Hg) • Arm-Compression stockings: control lymphedema
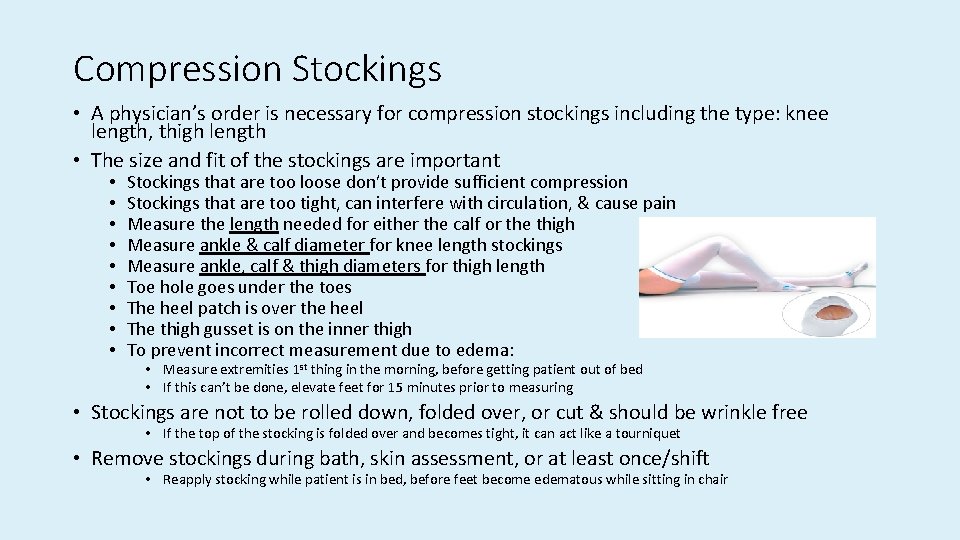
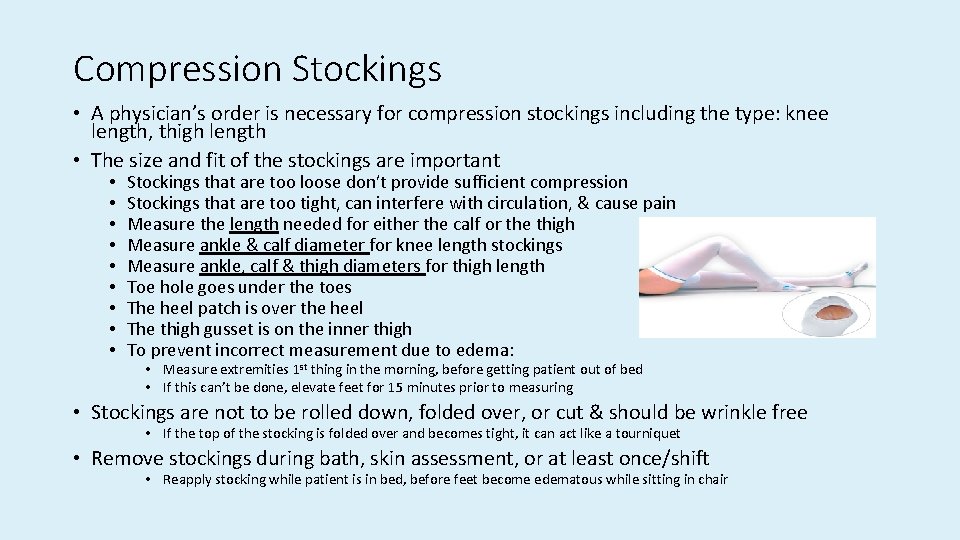
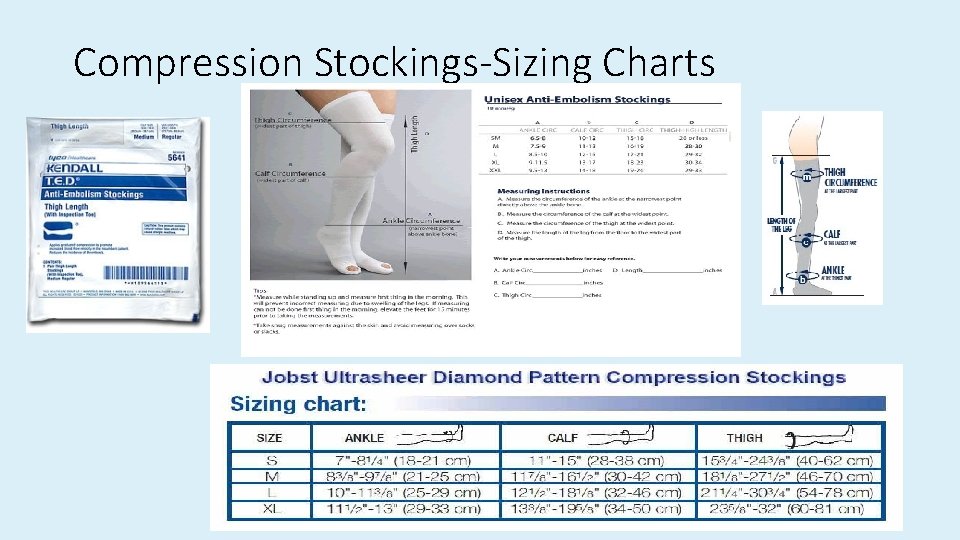
Compression Stockings • A physician’s order is necessary for compression stockings including the type: knee length, thigh length • The size and fit of the stockings are important • • • Stockings that are too loose don’t provide sufficient compression Stockings that are too tight, can interfere with circulation, & cause pain Measure the length needed for either the calf or the thigh Measure ankle & calf diameter for knee length stockings Measure ankle, calf & thigh diameters for thigh length Toe hole goes under the toes The heel patch is over the heel The thigh gusset is on the inner thigh To prevent incorrect measurement due to edema: • Measure extremities 1 st thing in the morning, before getting patient out of bed • If this can’t be done, elevate feet for 15 minutes prior to measuring • Stockings are not to be rolled down, folded over, or cut & should be wrinkle free • If the top of the stocking is folded over and becomes tight, it can act like a tourniquet • Remove stockings during bath, skin assessment, or at least once/shift • Reapply stocking while patient is in bed, before feet become edematous while sitting in chair
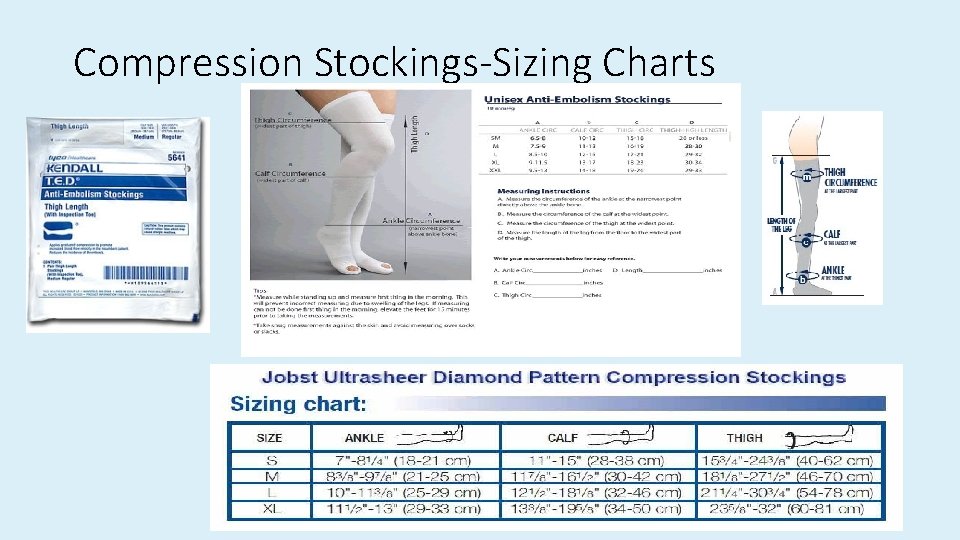
Compression Stockings-Sizing Charts
Contraindications to Support Stockings: • Dermatitis or open skin lesions or some wounds • Recent skin graft to lower leg • Decreased arterial circulation in lower extremity (assess color, temperature, distal pulses)
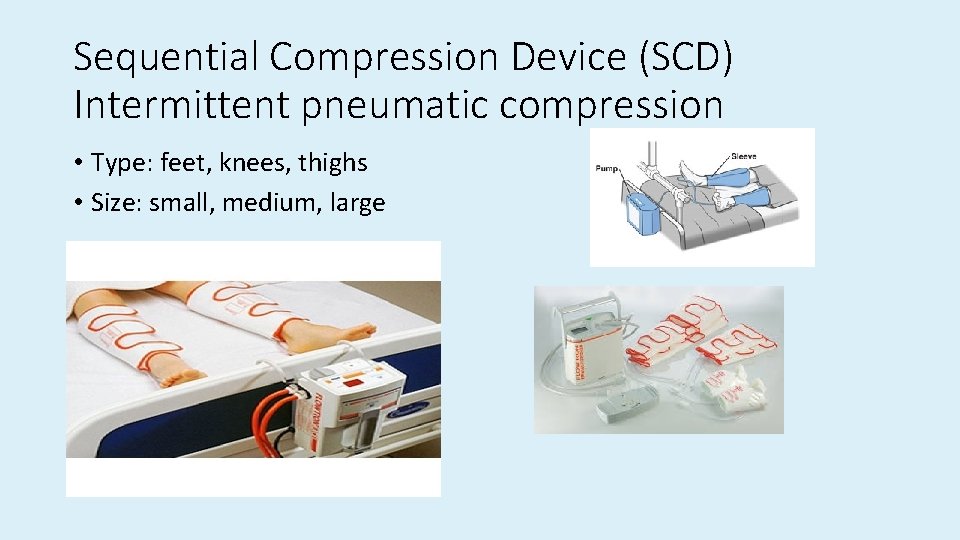
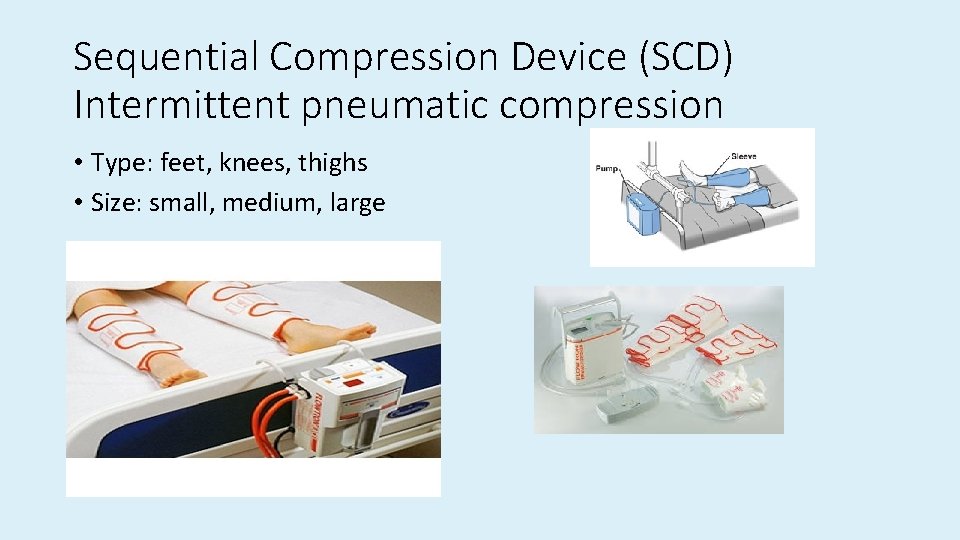
Sequential Compression Device (SCD) Intermittent pneumatic compression • Type: feet, knees, thighs • Size: small, medium, large
SCDs • Inflatable garments wrapped around lower extremities • Applies external, intermittent pressure or compression via an electric pump • Used in acute-care settings to prevent DVTs in calves and thighs: operating room, ICU, post ICU, any patient with risk of DVT • The device is worn continuously except during bath, skin assessment, and during ambulation • SCDs are not applied if the patient has an active DVT, because the intermittent compression action can loosen the clot (thrombus) which may travel to the lungs (pulmonary embolus)
DVTs can have serious consequences Who is at risk for DVT? • • • Major surgery, orthopedic or non-orthopedic Recent spinal cord injury or major trauma Immobility: not ambulating outside of room at least BID Injury to vein from fracture or surgery Varicose veins Coagulation problems, venous wall damage, venous stasis Obesity Smoking Oral contraceptives History of DVT Over 50 Chronic diseases: HF, COPD, kidney disease
DVT Prevention, Prophylaxis • Prevention of DVT is one of the core measure established by Joint Commission and The National Quality Form • Hospitals are encouraged to have a Thromboprophylaxis Policy in place which addresses DVT prevention on admission of all adult patients • Early & aggressive mobilization • Walking 4 to 6 times a day • Sitting in the chair for all meals • Position change every 2 hours • Active range of motion every 2 to 4 hours • Anticoagulation for moderate or high risk patients (SQ Heparin, Lovenox) • Mechanical prophylaxis: compression (SCDs alone or in combination with stockings) • Knee length compression does not prevent DVTs in thigh area