Comprehensive Child Development Service CCDS Early Identification and





- Slides: 51
Comprehensive Child Development Service (CCDS) – Early Identification and Timely Intervention 10 March 2017 Department of Health Hospital Authority Social Welfare Department 1
CONTENT (1) CCDS Collaborative Model (2) CCDS in Kowloon East Cluster & pregnant psychotropic substance abusers family supporting scheme (3) Development of Parenting Capacity Assessment Framework 2
(1) CCDS Collaborative Model 3
CCDS: BACKGROUND A 2005 POLICY ADDRESS INITIATIVE l To address the various developmental needs of young children (0 to 5 years) l An integrated community-based child and family service model 4
The Critical early years • The early years of a child’s life are critical in affecting the outcomes through the life course • Genes set the blueprint for brain development early before birth. • The environment experienced by a young child literally sculpts the developing brain and establishes the trajectory for long term cognitive and social-emotional outcomes • If we want to improve outcomes in adult life we have to focus on the early years • Investing in early childhood is a sound economic investment. Centre for Community Child Health, Royal Children Hospital, Melbourne 5
CCDS: Aim l To identify and meet, at an early stage, various health and social needs of children (aged 0 to 5) and their families. l Needy children and families identified will be referred to the appropriate health and/or social services for management. 6
CCDS: Partners l Labour and Welfare Bureau (LWB) l Department of Health (DH) Maternal and Child Health Centres (MCHCs) l Hospital Authority (HA) Obstetrics, Paediatrics and Psychiatric Services l Social Welfare Department (SWD) & Non-governmental organisations (NGOs) Integrated Family Service Centres (IFSCs), Integrated Services Centres (ISCs), and other service units l Education Bureau (EDB) Pre-primary institutions 7
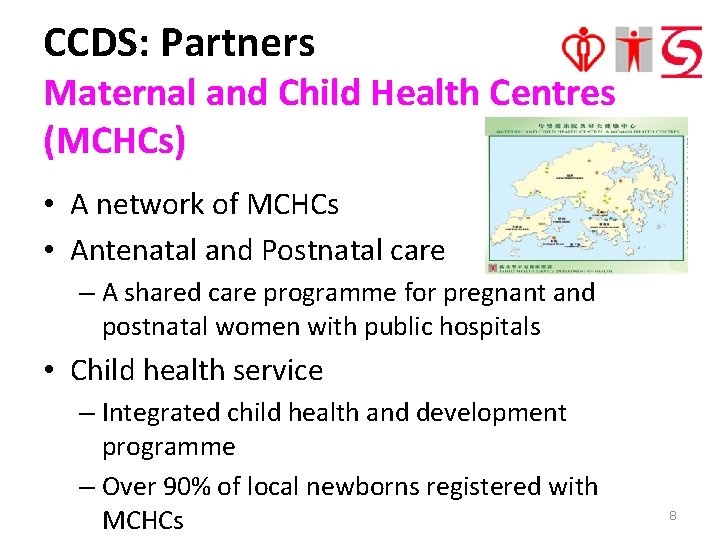
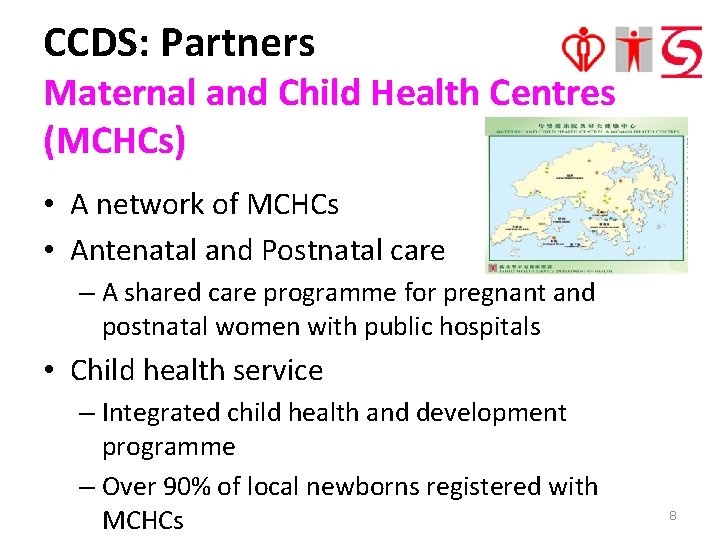
CCDS: Partners Maternal and Child Health Centres (MCHCs) • A network of MCHCs • Antenatal and Postnatal care – A shared care programme for pregnant and postnatal women with public hospitals • Child health service – Integrated child health and development programme – Over 90% of local newborns registered with MCHCs 8
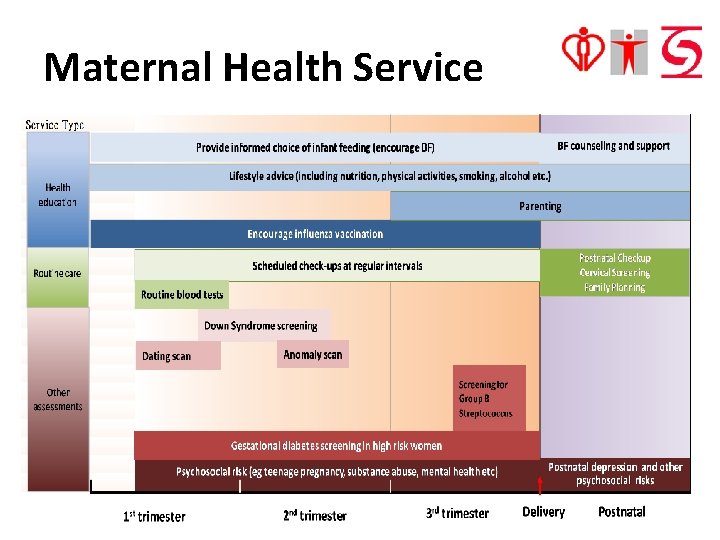
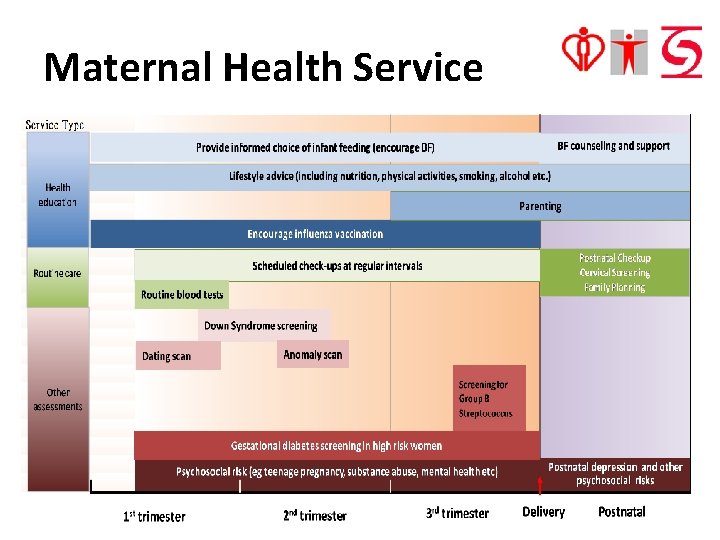
Maternal Health Service 9

10


CCDS: Partners Child Care Centres and Kindergartens Percentage of 3 to 5 -year-olds attending pre-school • 2011 Census: 91. 3% • 2016 By-census: 92. 5% 12
CCDS: Partners Hospital Authority Hospitals & Clinics l Provision of various specialist out-patient and in-patient services l Obstetrics, Paediatrics and Psychiatric Services for CCDS 13
CCDS: Partners Integrated Family Service Centre (IFSC) / Integrated Services Centre (ISC) l Currently, there a total of 65 IFSCs and 2 ISCs covering the whole territory. l Each IFSC serves a well-defined geographical service boundary to facilitate the accessibility of services for service users. 14

CCDS: Partners IFSC / ISC Three major components: Family Counselling Unit Family Support Unit Family Resource Unit Intensive counselling, therapeutic groups & crisis intervention Support services to vulnerable or at-risk individuals & families Developmental & preventive services 15
CCDS: Partners IFSC / ISC A continuum of preventive, supportive and remedial family services: • Enquiry service • Resource corner • Family life education /Parent-child activities • Groups and programmes • Volunteer training and service • Outreaching service • Counselling service • Referral service • Statutory cases including DSW Ward / Care or Protection / Guardianship Order cases (by SWD IFSCs only) 16
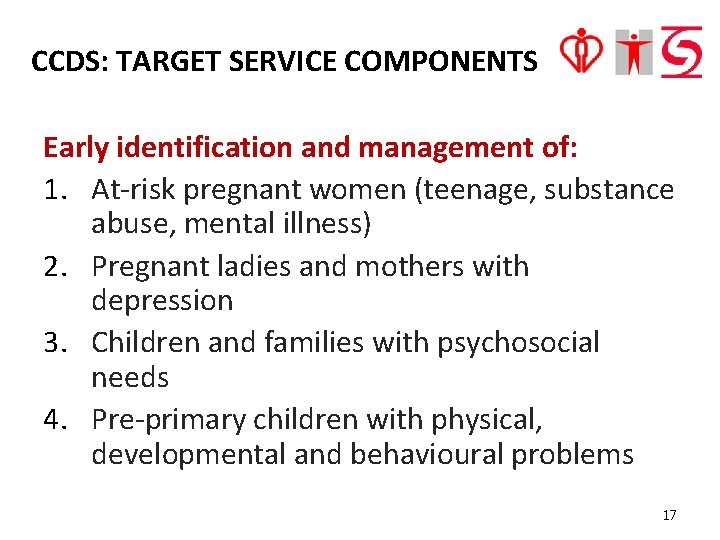
CCDS: TARGET SERVICE COMPONENTS Early identification and management of: 1. At-risk pregnant women (teenage, substance abuse, mental illness) 2. Pregnant ladies and mothers with depression 3. Children and families with psychosocial needs 4. Pre-primary children with physical, developmental and behavioural problems 17
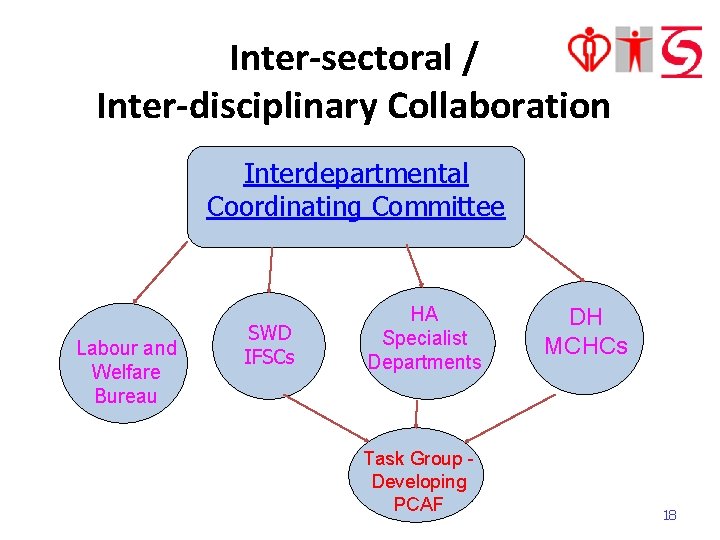
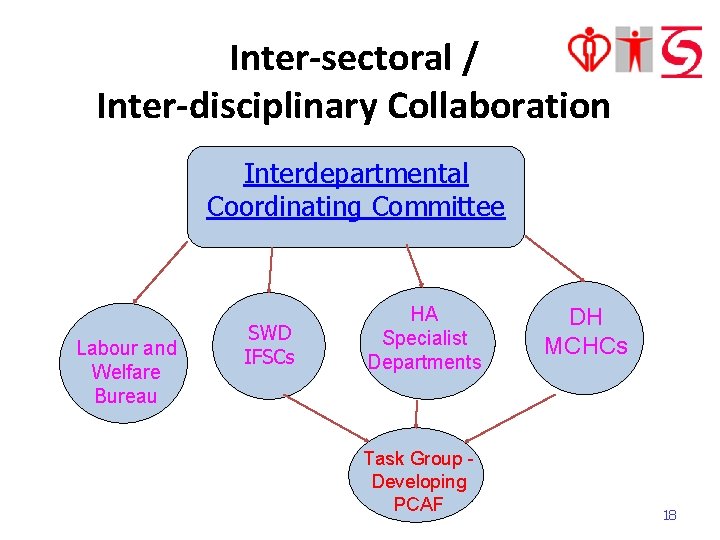
Inter-sectoral / Inter-disciplinary Collaboration Interdepartmental Coordinating Committee Labour and Welfare Bureau SWD IFSCs HA Specialist Departments Task Group Developing PCAF DH MCHCs 18
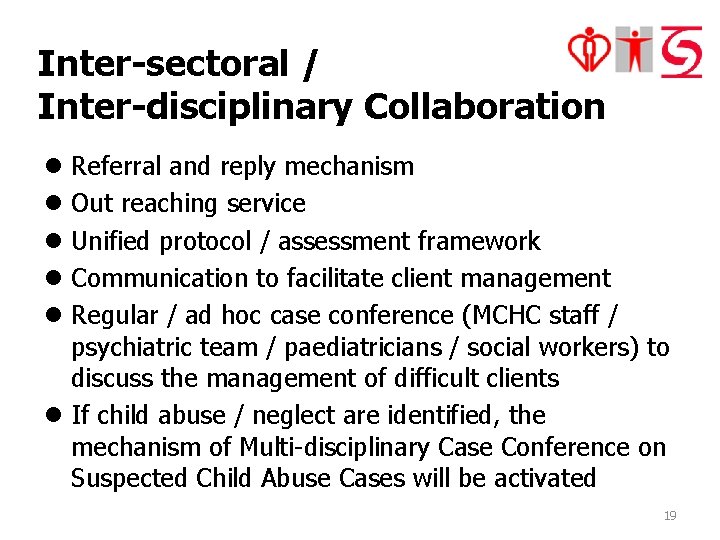
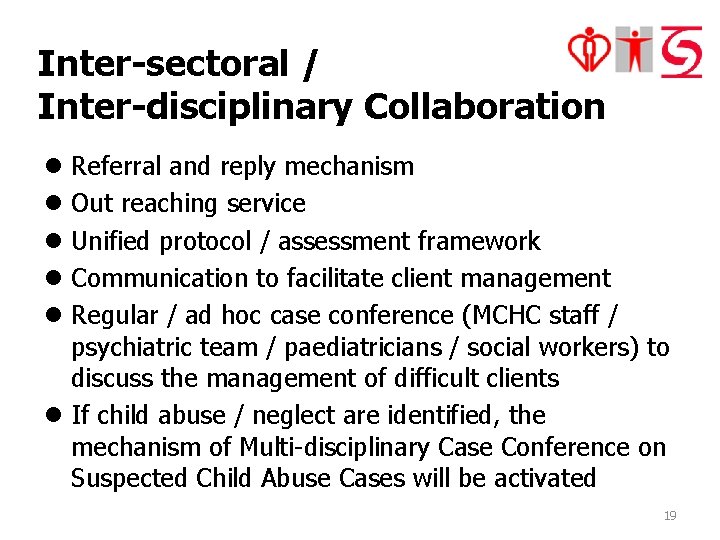
Inter-sectoral / Inter-disciplinary Collaboration l Referral and reply mechanism l Out reaching service l Unified protocol / assessment framework l Communication to facilitate client management l Regular / ad hoc case conference (MCHC staff / psychiatric team / paediatricians / social workers) to discuss the management of difficult clients l If child abuse / neglect are identified, the mechanism of Multi-disciplinary Case Conference on Suspected Child Abuse Cases will be activated 19
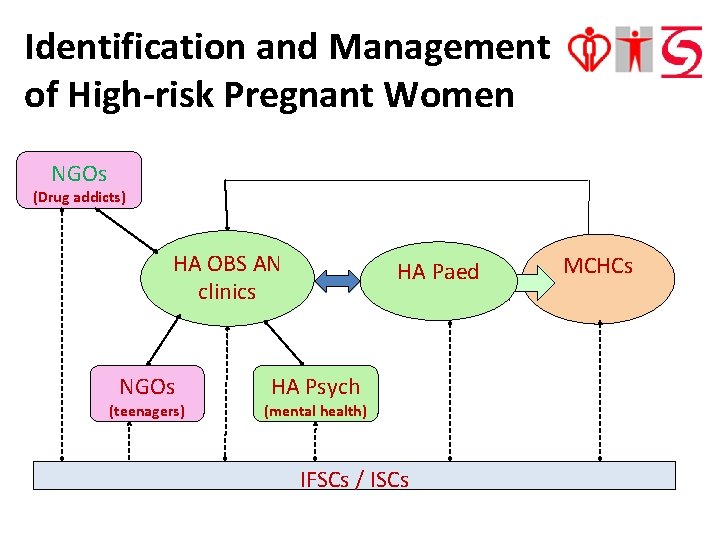
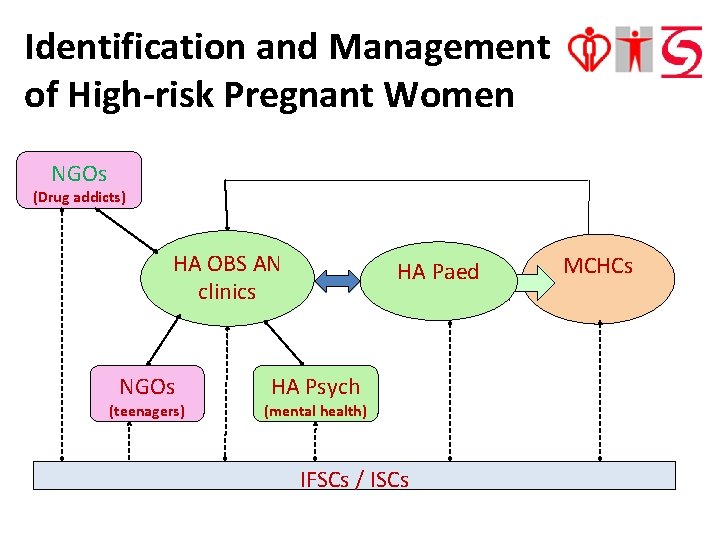
Identification and Management of High-risk Pregnant Women NGOs (Drug addicts) HA OBS AN clinics NGOs (teenagers) HA Paed HA Psych (mental health) IFSCs / ISCs MCHCs
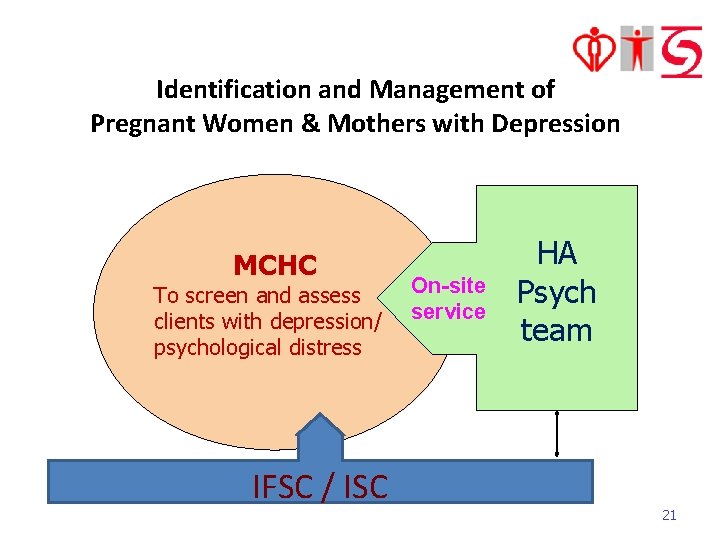
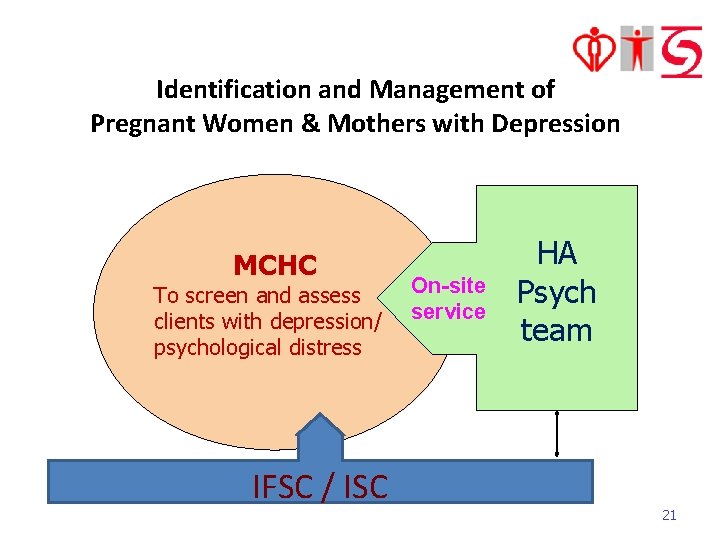
Identification and Management of Pregnant Women & Mothers with Depression MCHC To screen and assess clients with depression/ psychological distress IFSC / ISC On-site service HA Psych team 21
Identification and Management of Pregnant Women & Mothers with Depression Antenatal period: Nurses and Doctors in MCHC • Identify pregnant women with mood problem or past history of psychiatric illness • Offer supportive counselling service • Refer to the CCDS midwives at the obstetric clinics of HA or the visiting psychiatric team for assessment and follow up 22
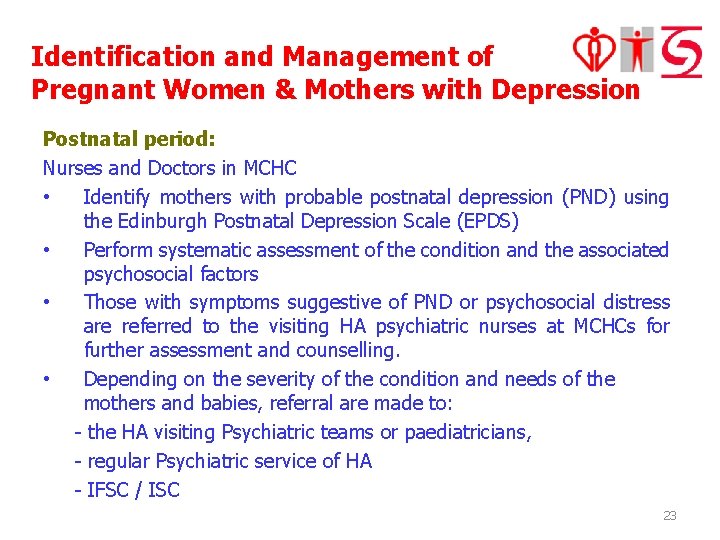
Identification and Management of Pregnant Women & Mothers with Depression Postnatal period: Nurses and Doctors in MCHC • Identify mothers with probable postnatal depression (PND) using the Edinburgh Postnatal Depression Scale (EPDS) • Perform systematic assessment of the condition and the associated psychosocial factors • Those with symptoms suggestive of PND or psychosocial distress are referred to the visiting HA psychiatric nurses at MCHCs for further assessment and counselling. • Depending on the severity of the condition and needs of the mothers and babies, referral are made to: - the HA visiting Psychiatric teams or paediatricians, - regular Psychiatric service of HA - IFSC / ISC 23
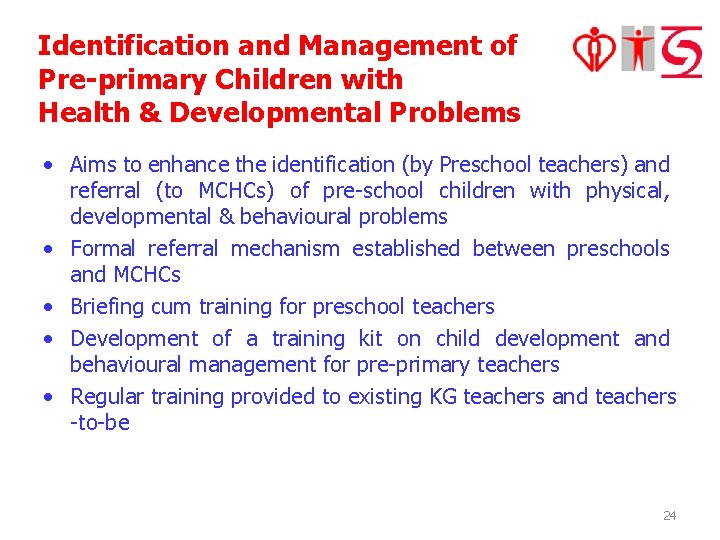
Identification and Management of Pre-primary Children with Health & Developmental Problems • Aims to enhance the identification (by Preschool teachers) and referral (to MCHCs) of pre-school children with physical, developmental & behavioural problems • Formal referral mechanism established between preschools and MCHCs • Briefing cum training for preschool teachers • Development of a training kit on child development and behavioural management for pre-primary teachers • Regular training provided to existing KG teachers and teachers -to-be 24
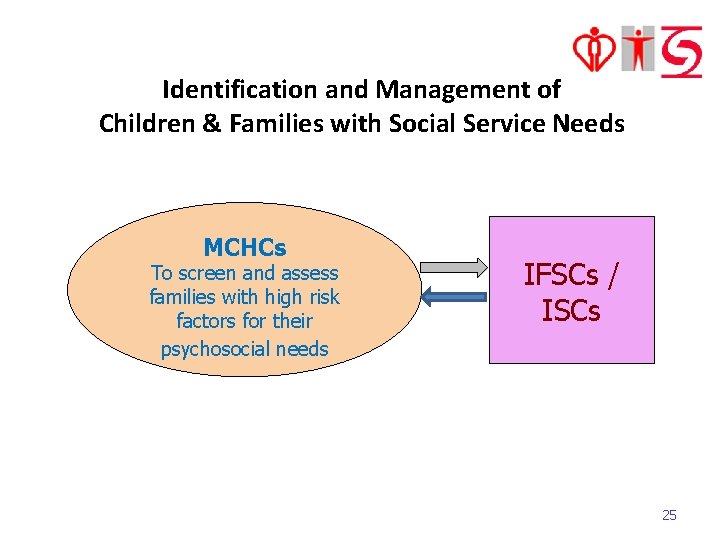
Identification and Management of Children & Families with Social Service Needs MCHCs To screen and assess families with high risk factors for their psychosocial needs IFSCs / ISCs 25
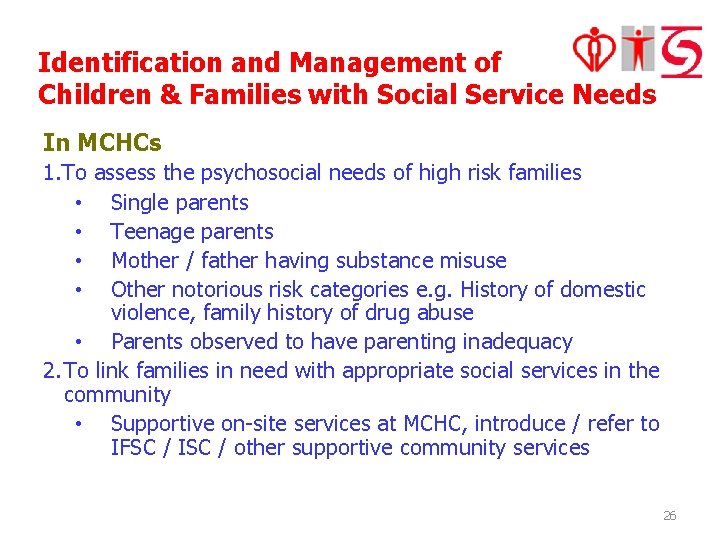
Identification and Management of Children & Families with Social Service Needs In MCHCs 1. To assess the psychosocial needs of high risk families • Single parents • Teenage parents • Mother / father having substance misuse • Other notorious risk categories e. g. History of domestic violence, family history of drug abuse • Parents observed to have parenting inadequacy 2. To link families in need with appropriate social services in the community • Supportive on-site services at MCHC, introduce / refer to IFSC / ISC / other supportive community services 26
Identification and Management of Children & Families with Social Service Needs By IFSCs / ISCs District Support to Needy Cases • Assessment of parenting capacity • Casework and counseling support • Educational / support / mutual-help / therapeutic groups and programmes Support for MCHCs • Briefing on family services and community resources • Setting up information booth to introduce welfare services and deliver service leaflets to service users 27
(3) Development of Parenting Capacity Assessment Framework 28
Suboptimal child care and parenting capacity • It is always one of the main problems found in high risk families. • At times, discrepancy among different professionals on assessment of child care adequacy, and • lack of a common language for sharing their respective assessment and proposed management plans for the at-risk families. 29
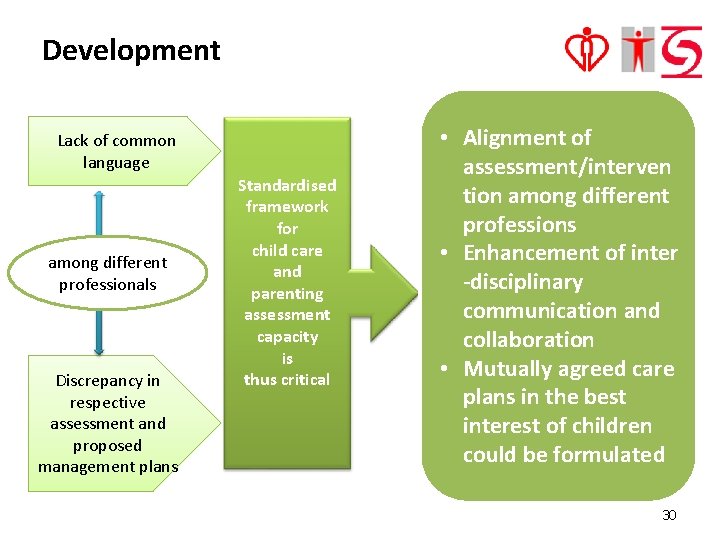
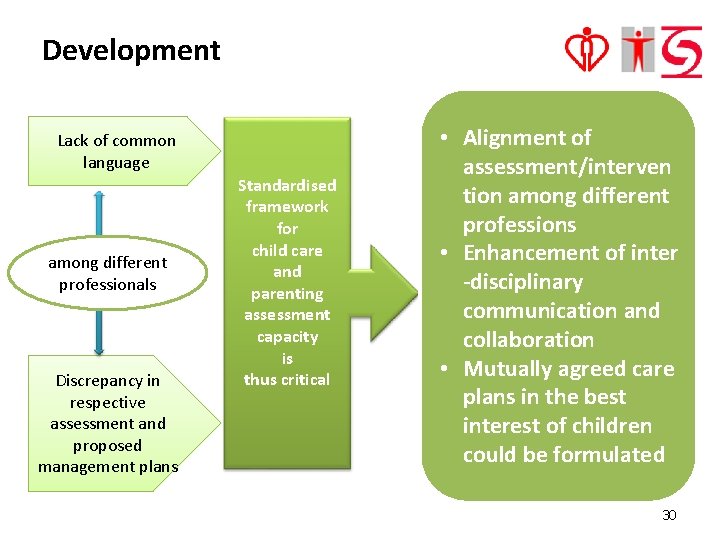
Development Lack of common language among different professionals Discrepancy in respective assessment and proposed management plans Standardised framework for child care and parenting assessment capacity is thus critical • Alignment of assessment/interven tion among different professions • Enhancement of inter -disciplinary communication and collaboration • Mutually agreed care plans in the best interest of children could be formulated 30
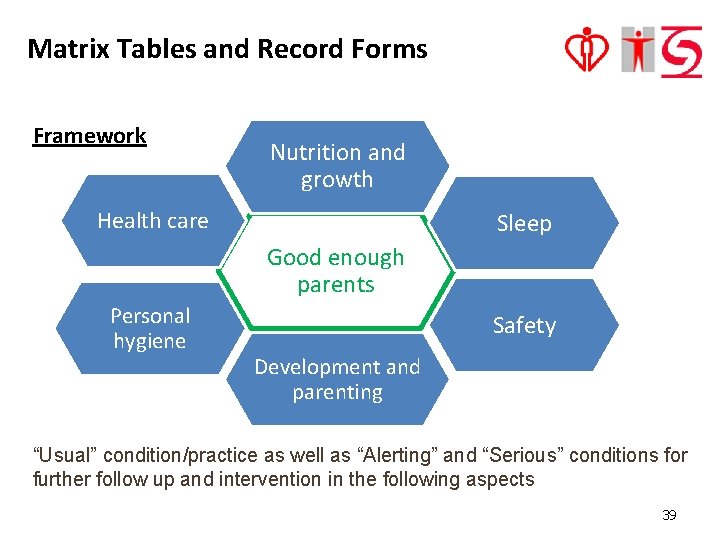
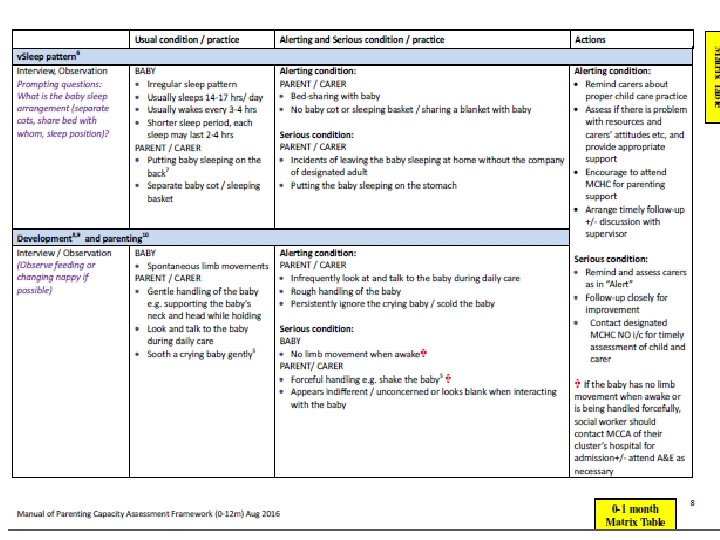
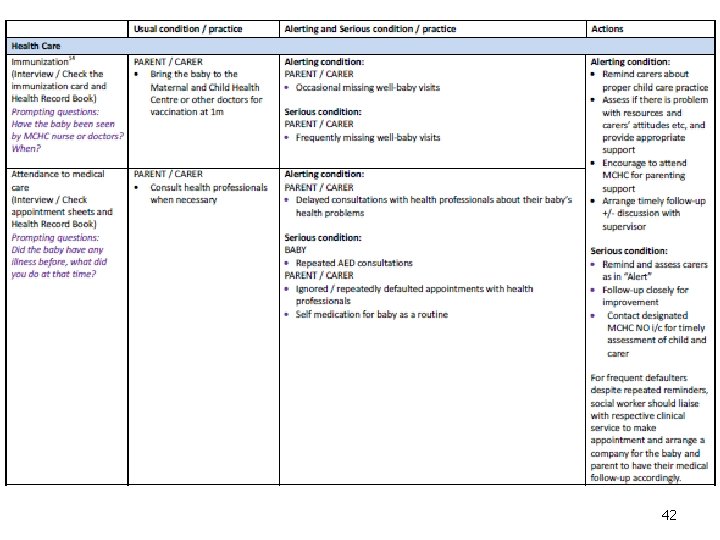
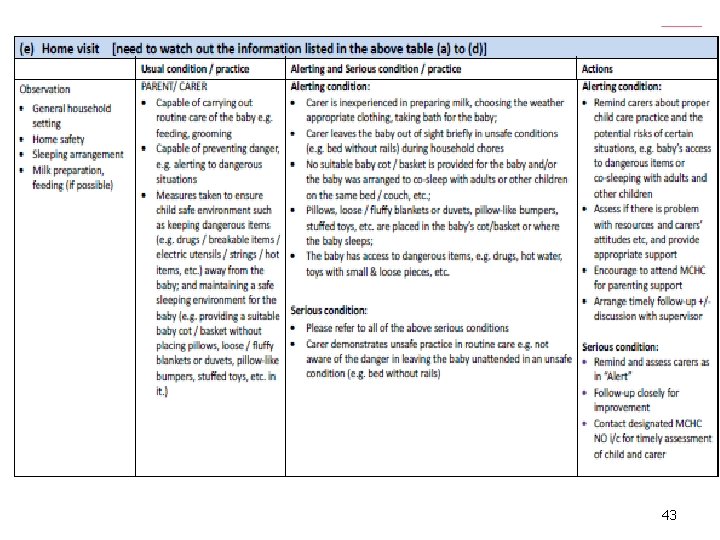
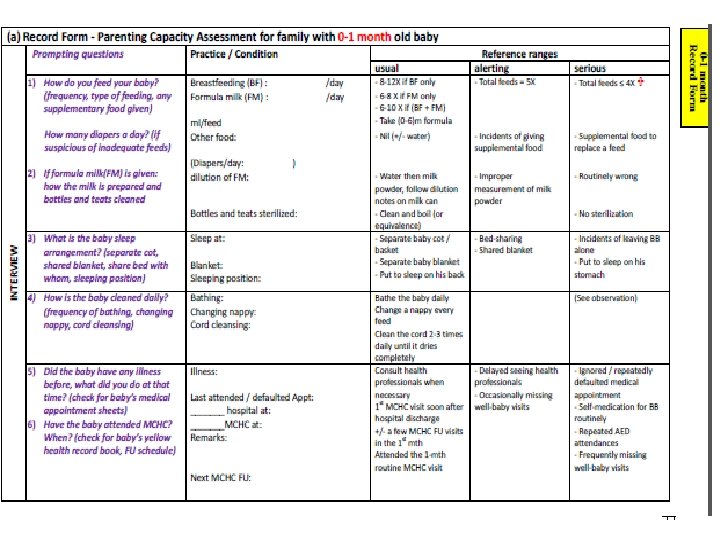
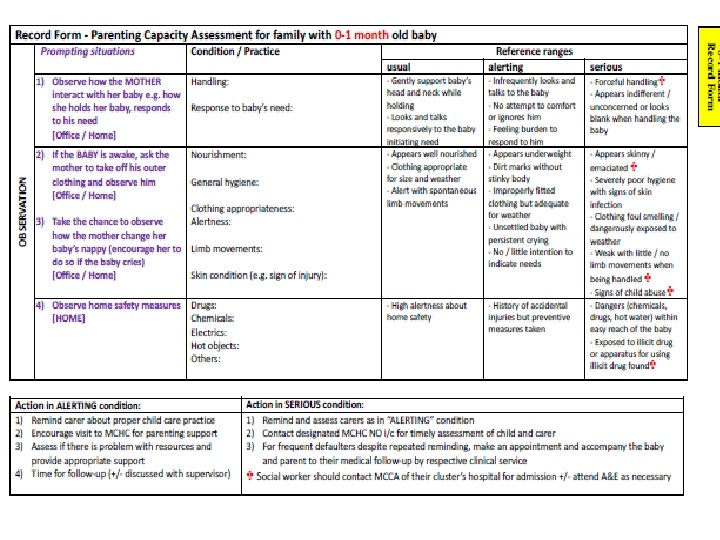
Parenting Capacity Assessment Framework (PCAF) Overview • Designed for the use by various disciplines of social and health sectors • Developed and implemented by phases for children aged between 0 to 3 years • First PCAF is targeted for children aged between 0 to 12 months for use by social workers • 6 domains including nutrition and growth, sleep pattern, development and parenting, personal hygiene, safety and health care Remarks • It is NOT a checklist or a psychometric scoring test pointing to any specific diagnosis. • The PCAF provided reference in assessing the capacity of the parents/carers when social worker conduct the social assessment. 31
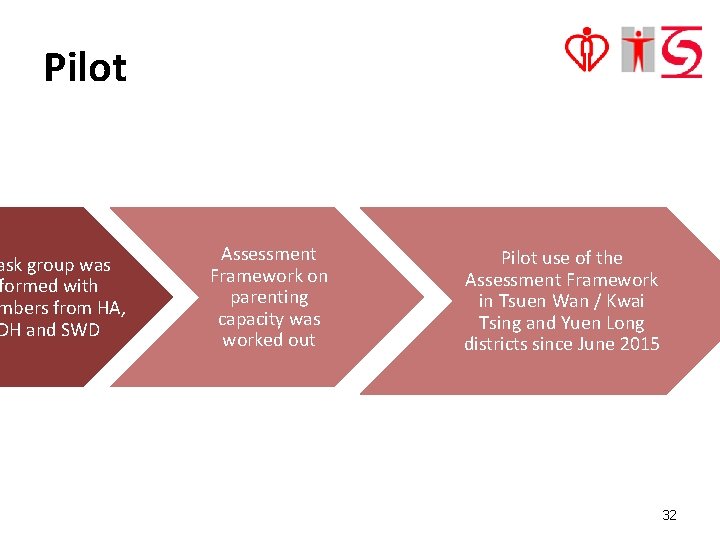
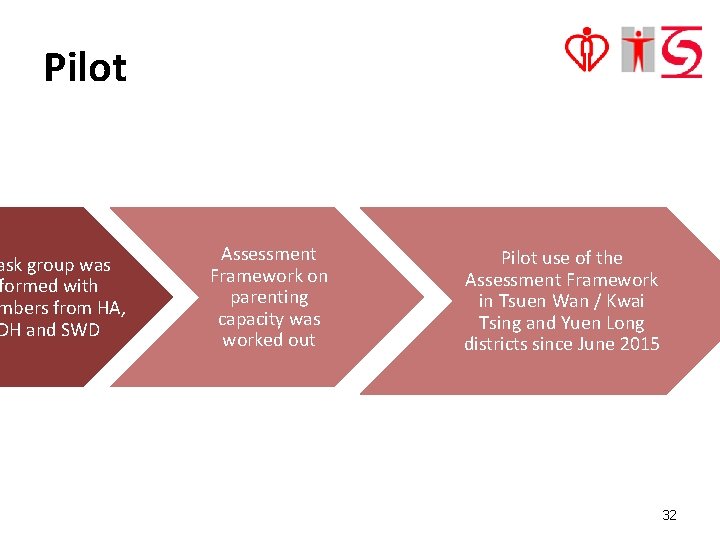
Pilot ask group was formed with mbers from HA, DH and SWD Assessment Framework on parenting capacity was worked out Pilot use of the Assessment Framework in Tsuen Wan / Kwai Tsing and Yuen Long districts since June 2015 32
Training, sharing and focus group • Seminars and Workshops • Case Sharing Sessions • Focus groups 33
Feedbacks Positive feedback • a useful reference tool to facilitate social workers to conduct a comprehensive assessment on parents with new born babies • formulating intervention • for facilitating inter-disciplinary collaboration • for engaging clients 34
Feedbacks (cont’d) Sharing of difficulties • unmotivated parents • clients live in partitioned cubicle / rooms Comments on • training design / needs • Manual and Record Forms • collaboration with other professionals 35
Refinement after pilot - manual • Elaboration on the part related to assessment on parents with drug / substance abuse habit • Matrix table – highlight key words • Record forms – format – adding bullet points 36
Manual 37
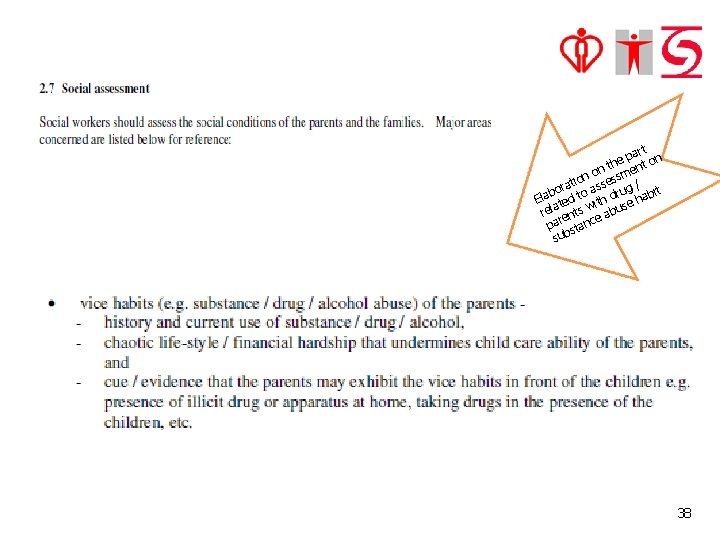
t par on e t th on smen n s e tio ora to ass rug / bit b a d a El ted ith use h a w l e s b r ent ea par stanc sub 38
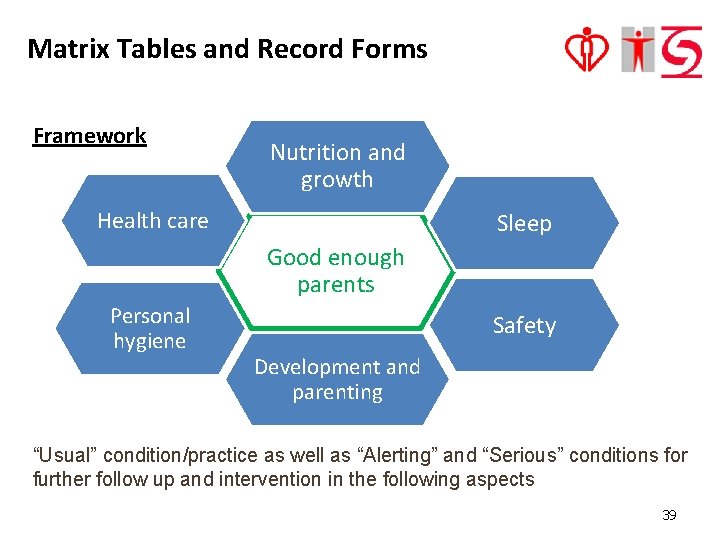
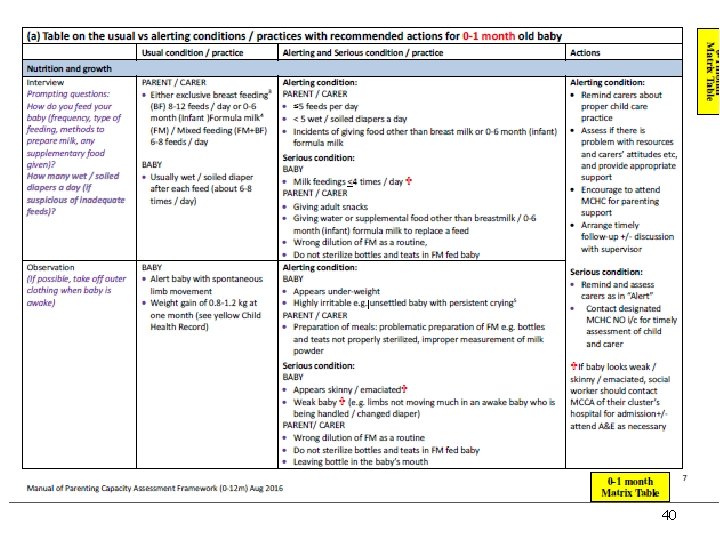
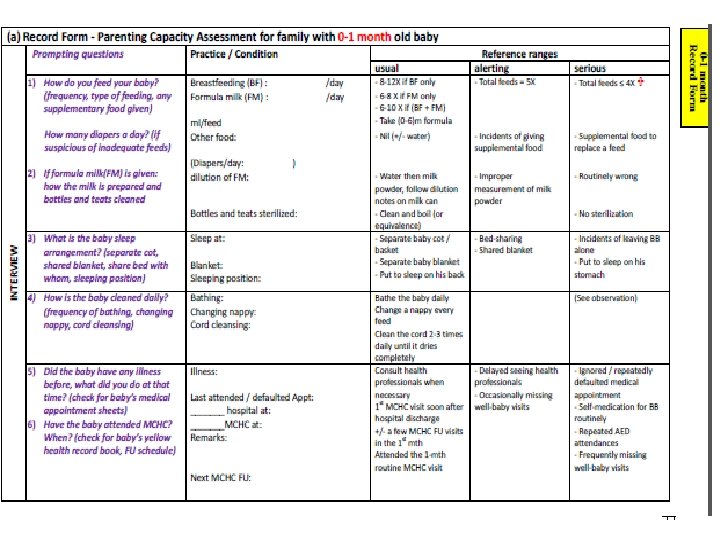
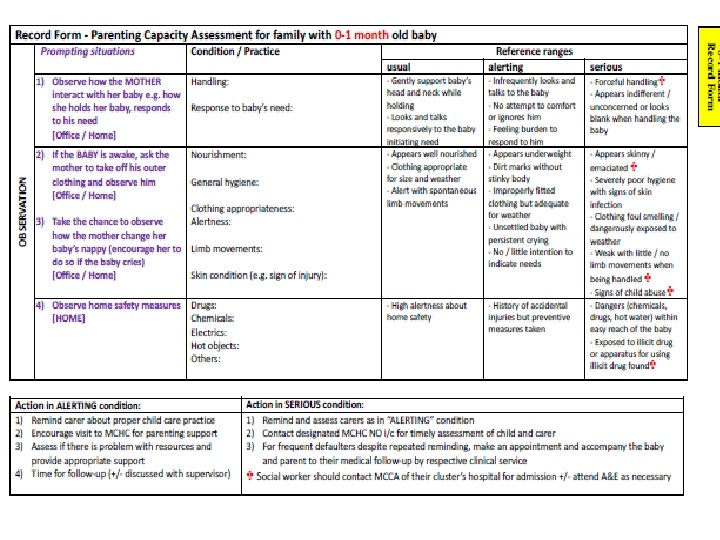
Matrix Tables and Record Forms Framework Nutrition and growth Health care Sleep Good enough parents Personal hygiene Safety Development and parenting “Usual” condition/practice as well as “Alerting” and “Serious” conditions for further follow up and intervention in the following aspects 39
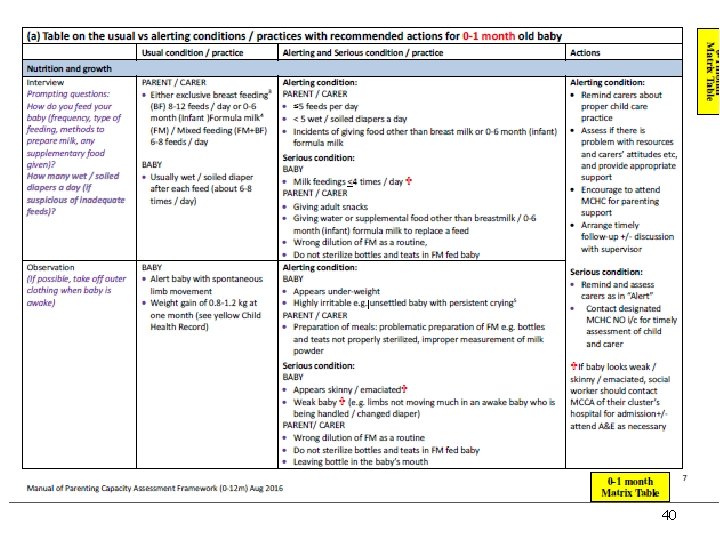
40
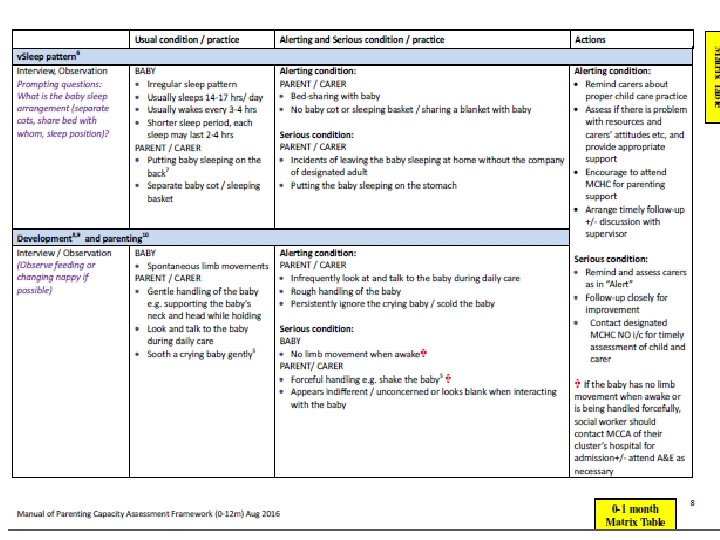
41
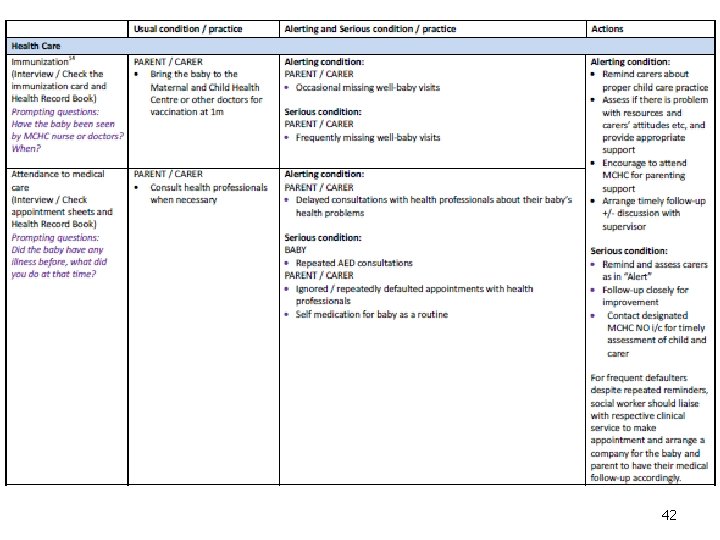
42
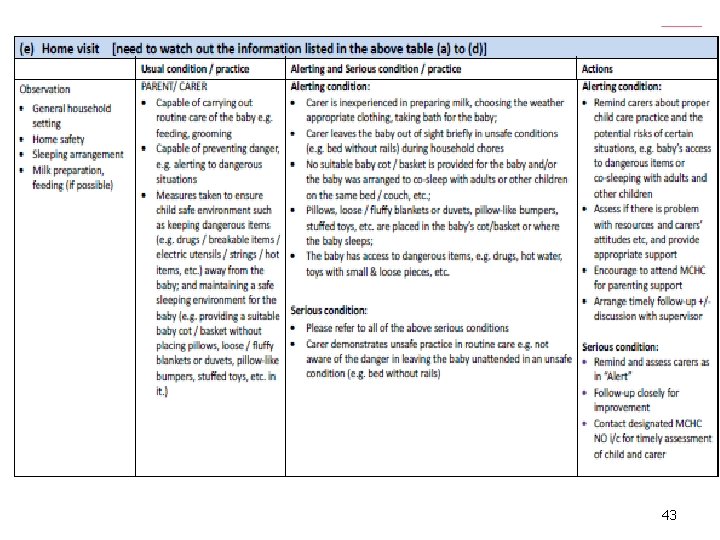
43
44
45
Refinement after pilot - training • videos for illustrating the application • having small group discussion • providing two cases for discussion each group for practice • experienced social worker to share practical tips 46
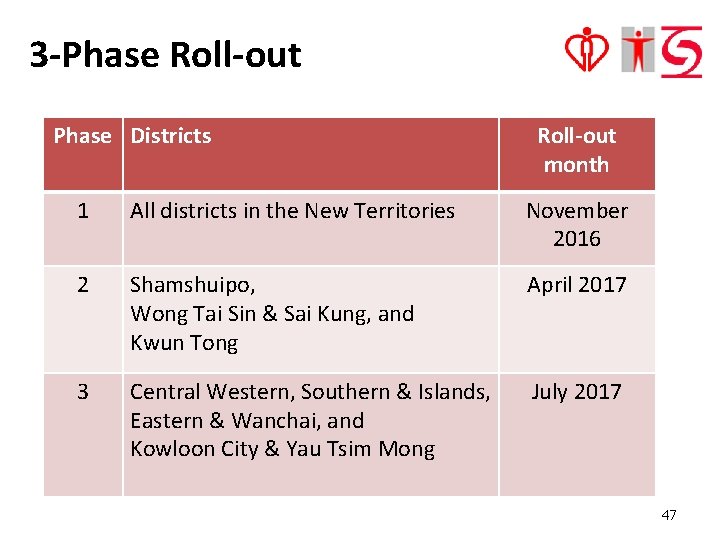
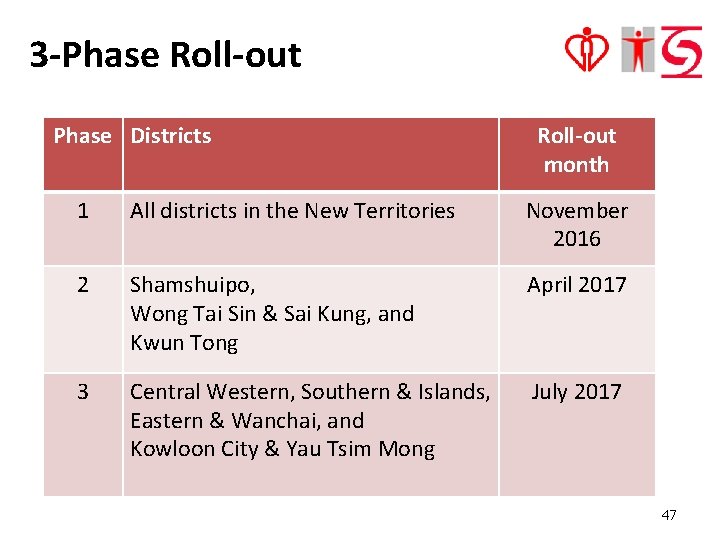
3 -Phase Roll-out Phase Districts Roll-out month 1 All districts in the New Territories November 2016 2 Shamshuipo, Wong Tai Sin & Sai Kung, and Kwun Tong April 2017 3 Central Western, Southern & Islands, Eastern & Wanchai, and Kowloon City & Yau Tsim Mong July 2017 47
Encourage to use Social workers of IFSCs and the related settings are encouraged to use the framework on any at-risk families 48
Way forward l Assessment framework for social worker for children aged 13 to 36 months and another version for health sector. 49
Experience Sharing 50

51