Component of BOO A dynamic physiologic reversible component
Component of BOO • A dynamic (physiologic, reversible) component – related to the tension of prostatic smooth muscle in the prostate, prostate capsule, and bladder neck • A fixed (structural) component – related to the bulk of the enlarged prostate impinging upon the urethra
Current treatment options • • Conservative treatment Alpha blockers 5 -alpha-reductase inhibitors (5 ARIs) Combination therapy Phytotherapy Minimally invasive techniques Surgery

Goal of treatment • • • Relieving LUTS Decreasing BOO Improving bladder emptying Ameliorating overactive bladder activity Reversing renal insufficiency Preventing disease progression
Watchful waiting • Patient selection • Education, • Reassurance, • Periodic monitoring, • Lifestyle advice
Watchful waiting • Patient selection • Education, • Reassurance, • Periodic monitoring, • Lifestyle advice
Life Style Advice • • Reduction in fluid intake Avoidance of moderation of caffeine and alcohol Double voiding technique Urethral stripping Distraction- mind out of bladder n toilet Bladder retraining- Hold on Optimising drugs Treatment of constipation
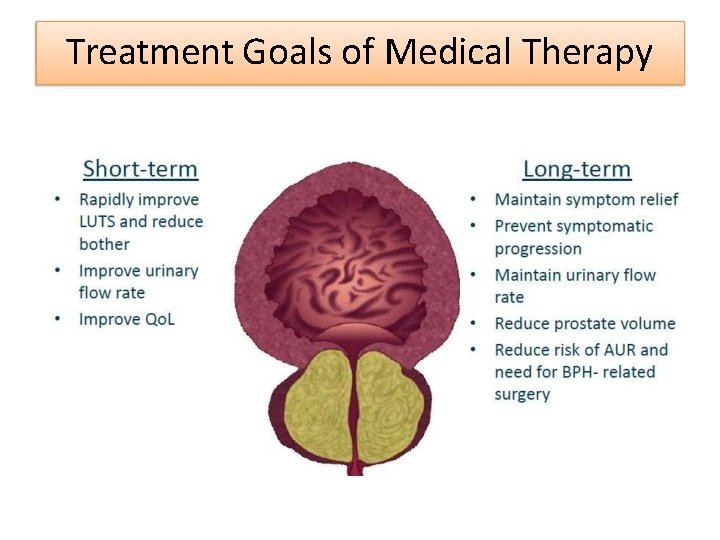
Treatment Goals of Medical Therapy
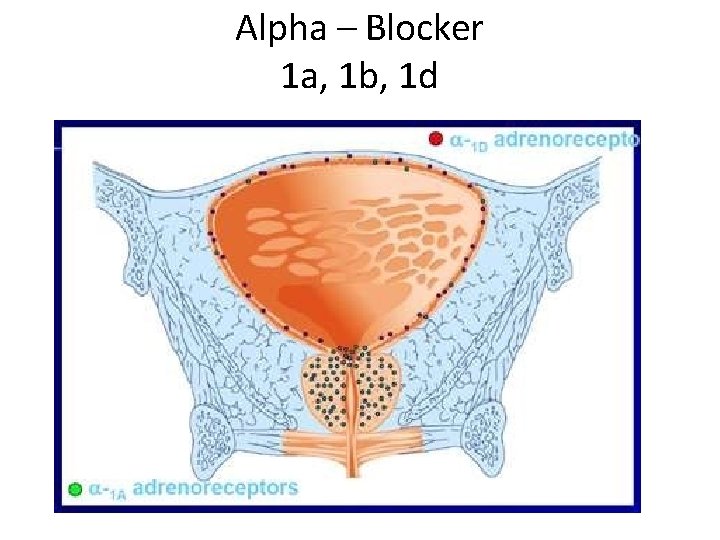
Alpha – Blocker 1 a, 1 b, 1 d
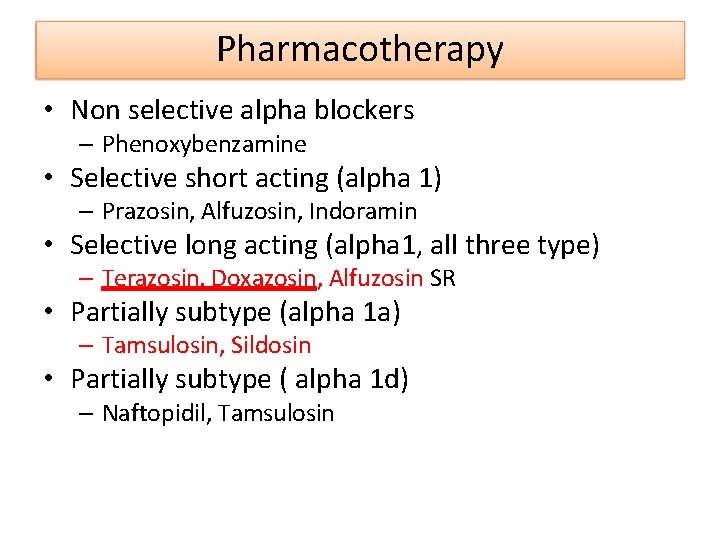
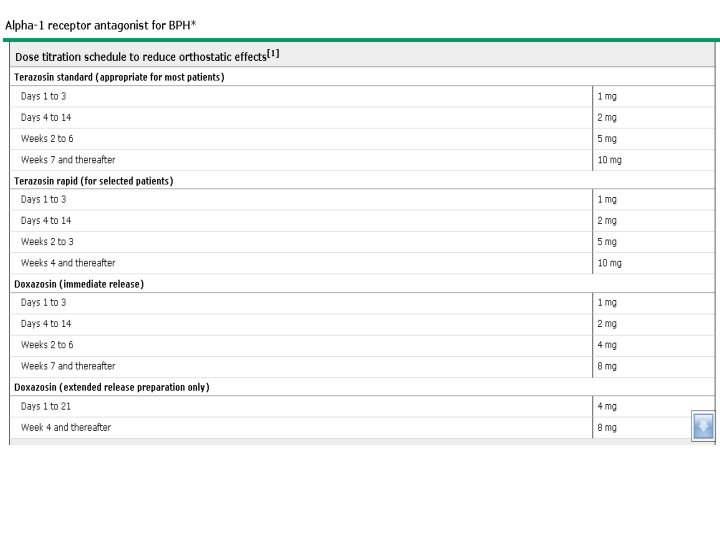
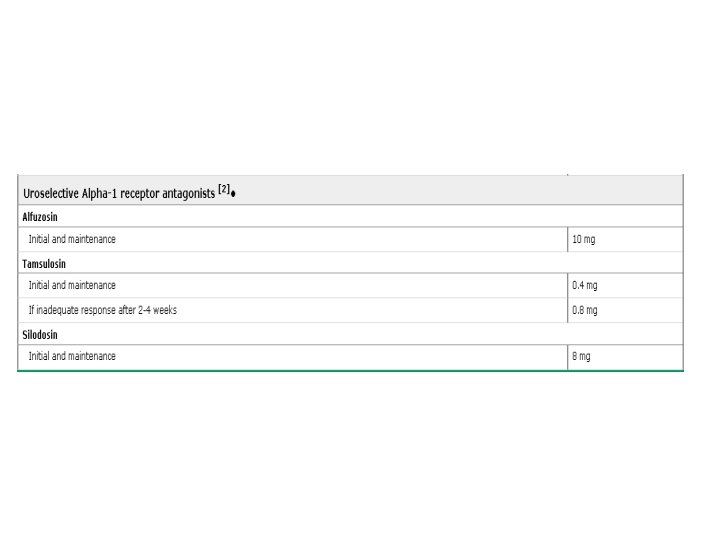
Pharmacotherapy • Non selective alpha blockers – Phenoxybenzamine • Selective short acting (alpha 1) – Prazosin, Alfuzosin, Indoramin • Selective long acting (alpha 1, all three type) – Terazosin, Doxazosin, Alfuzosin SR • Partially subtype (alpha 1 a) – Tamsulosin, Sildosin • Partially subtype ( alpha 1 d) – Naftopidil, Tamsulosin
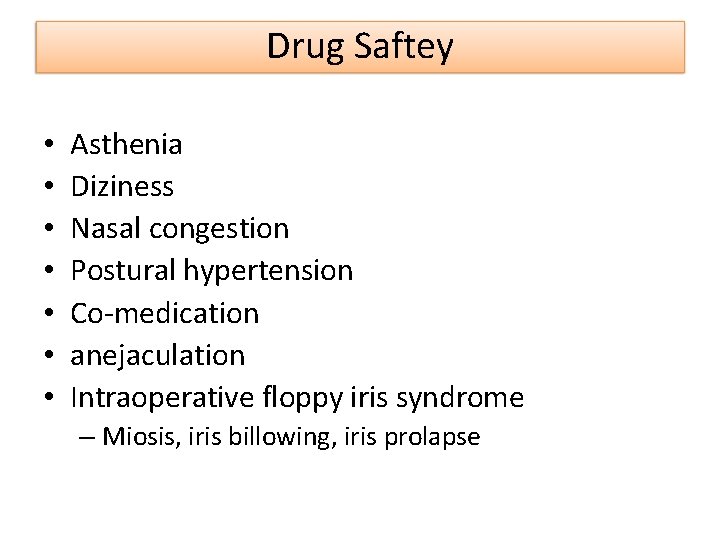
Drug Saftey • • Asthenia Diziness Nasal congestion Postural hypertension Co-medication anejaculation Intraoperative floppy iris syndrome – Miosis, iris billowing, iris prolapse
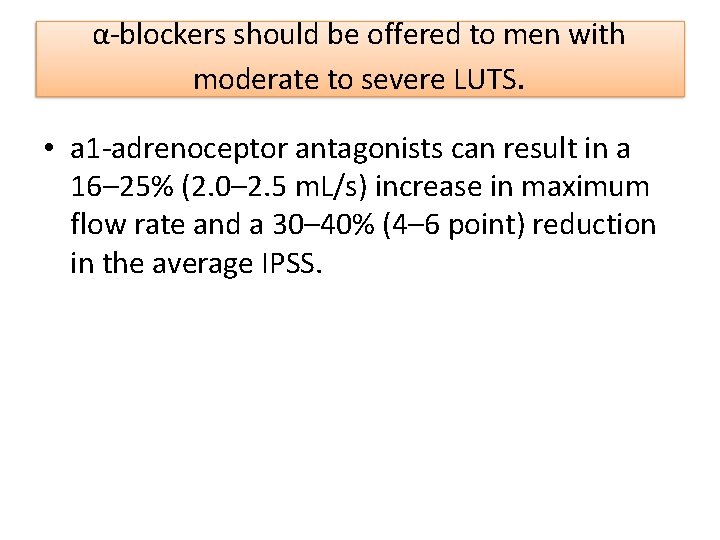
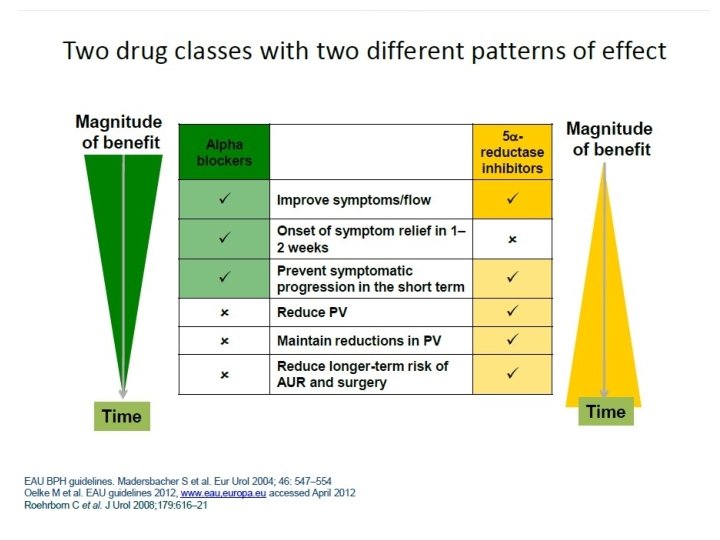
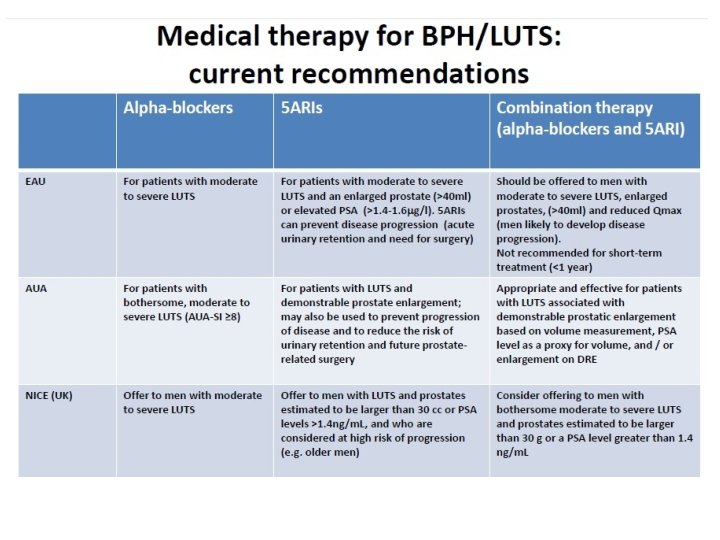
α-blockers should be offered to men with moderate to severe LUTS. • a 1 -adrenoceptor antagonists can result in a 16– 25% (2. 0– 2. 5 m. L/s) increase in maximum flow rate and a 30– 40% (4– 6 point) reduction in the average IPSS.

5 alpha Reductase inhibitor Dutasteride Finasteride Type II 5 AR Testosterone DHT Type I 5 AR Bartsch G et al. Eur Urol. 2000; 37: 367 380. Dutasteride Prostate volume reduced
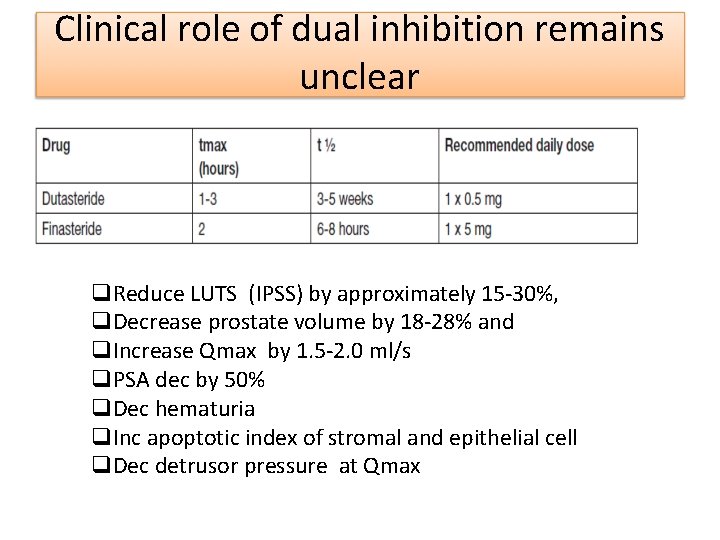
Clinical role of dual inhibition remains unclear Reduce LUTS (IPSS) by approximately 15 -30%, Decrease prostate volume by 18 -28% and Increase Qmax by 1. 5 -2. 0 ml/s PSA dec by 50% Dec hematuria Inc apoptotic index of stromal and epithelial cell Dec detrusor pressure at Qmax
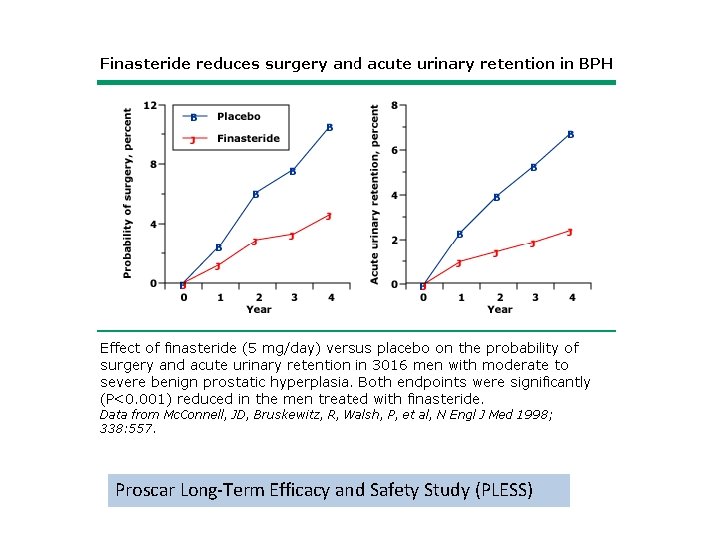
Proscar Long-Term Efficacy and Safety Study (PLESS)
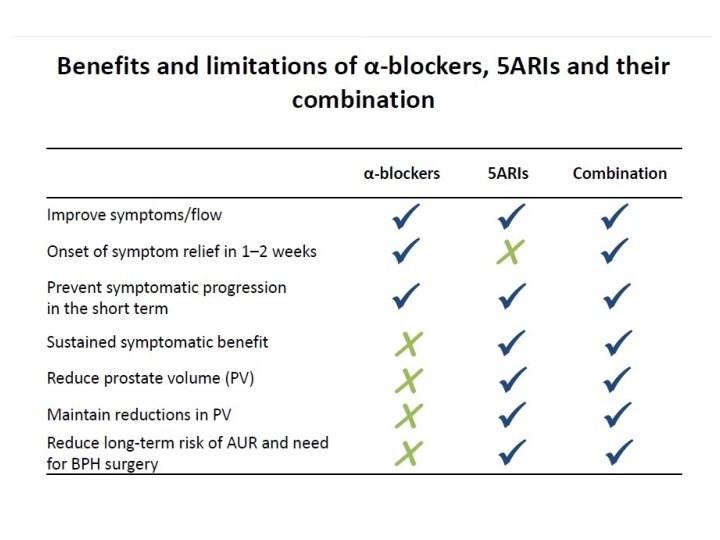
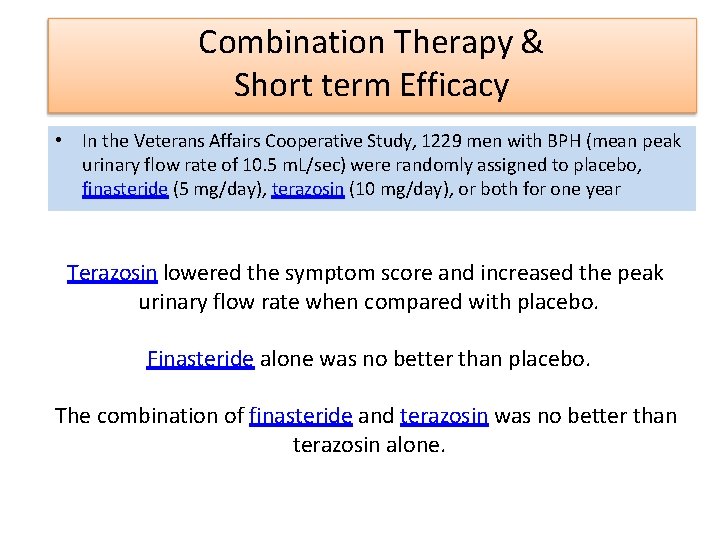
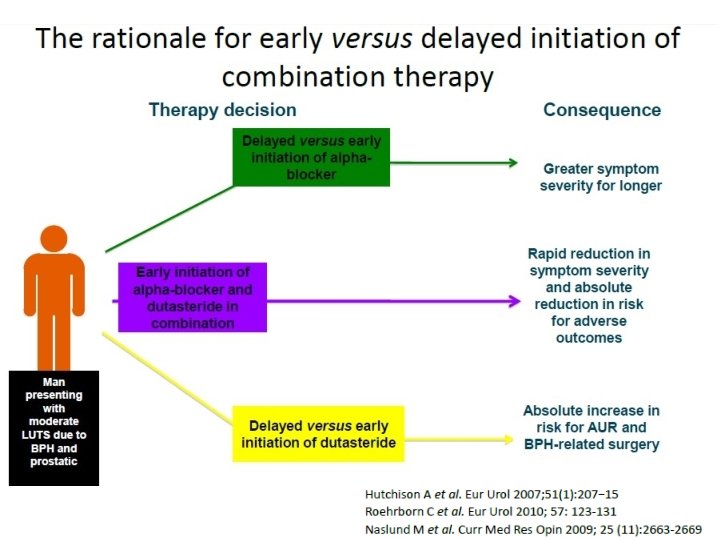
Combination Therapy & Short term Efficacy • In the Veterans Affairs Cooperative Study, 1229 men with BPH (mean peak urinary flow rate of 10. 5 m. L/sec) were randomly assigned to placebo, finasteride (5 mg/day), terazosin (10 mg/day), or both for one year Terazosin lowered the symptom score and increased the peak urinary flow rate when compared with placebo. Finasteride alone was no better than placebo. The combination of finasteride and terazosin was no better than terazosin alone.
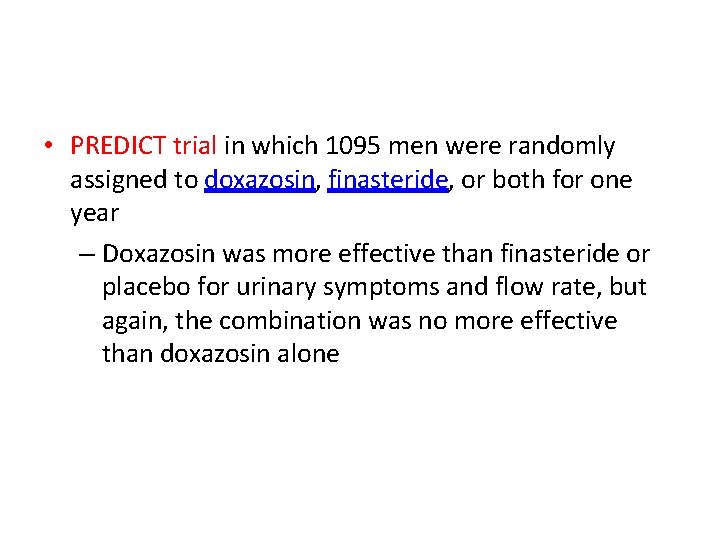
• PREDICT trial in which 1095 men were randomly assigned to doxazosin, finasteride, or both for one year – Doxazosin was more effective than finasteride or placebo for urinary symptoms and flow rate, but again, the combination was no more effective than doxazosin alone
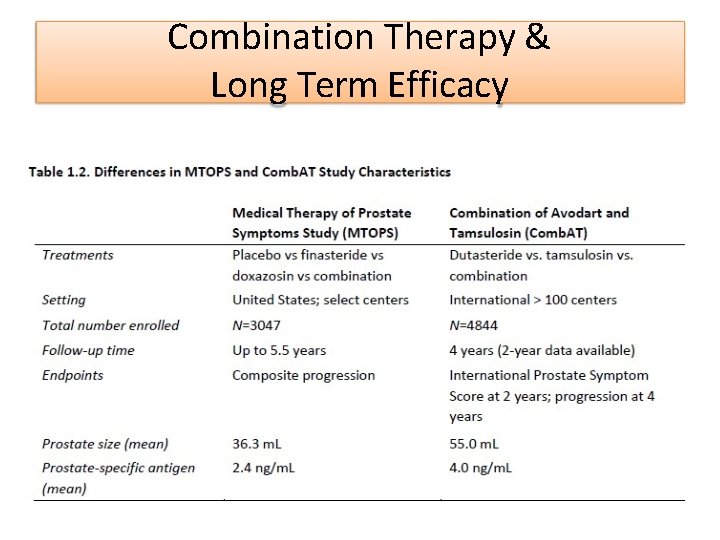
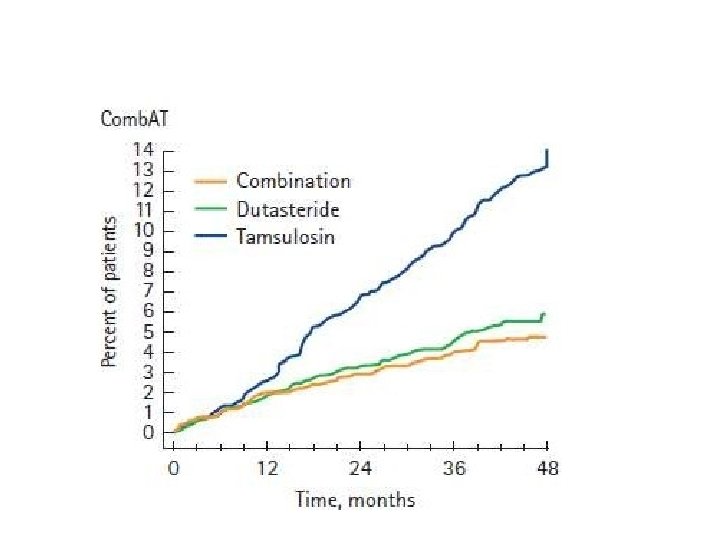
Combination Therapy & Long Term Efficacy
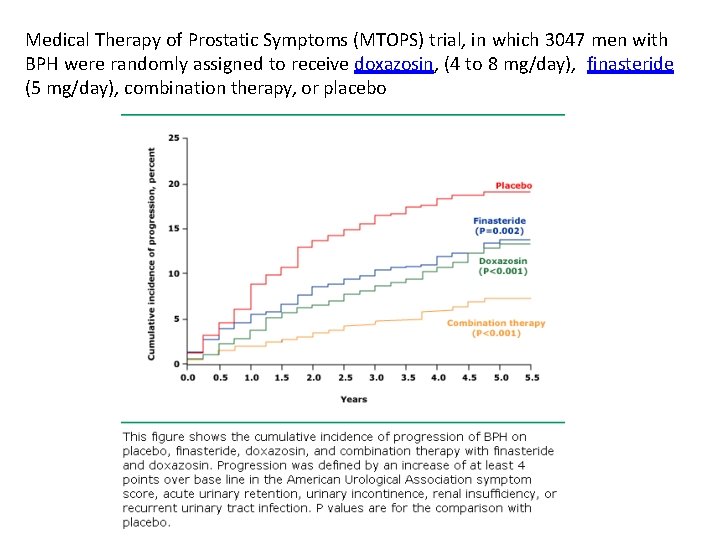
Medical Therapy of Prostatic Symptoms (MTOPS) trial, in which 3047 men with BPH were randomly assigned to receive doxazosin, (4 to 8 mg/day), finasteride (5 mg/day), combination therapy, or placebo
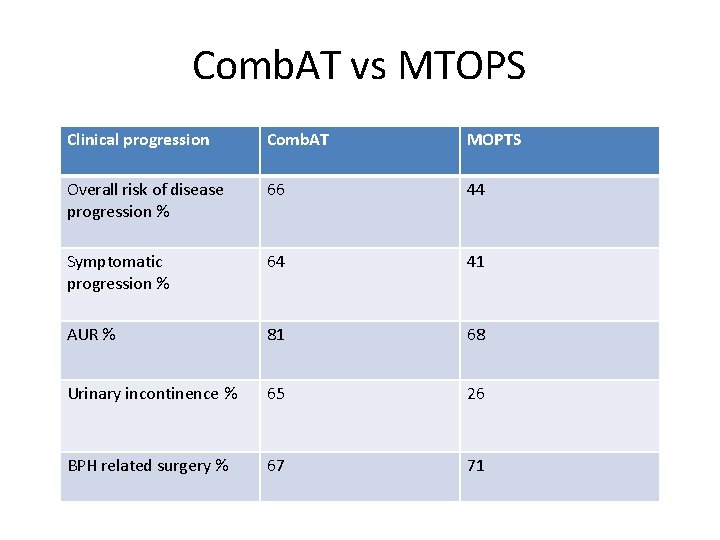
Comb. AT vs MTOPS Clinical progression Comb. AT MOPTS Overall risk of disease progression % 66 44 Symptomatic progression % 64 41 AUR % 81 68 Urinary incontinence % 65 26 BPH related surgery % 67 71
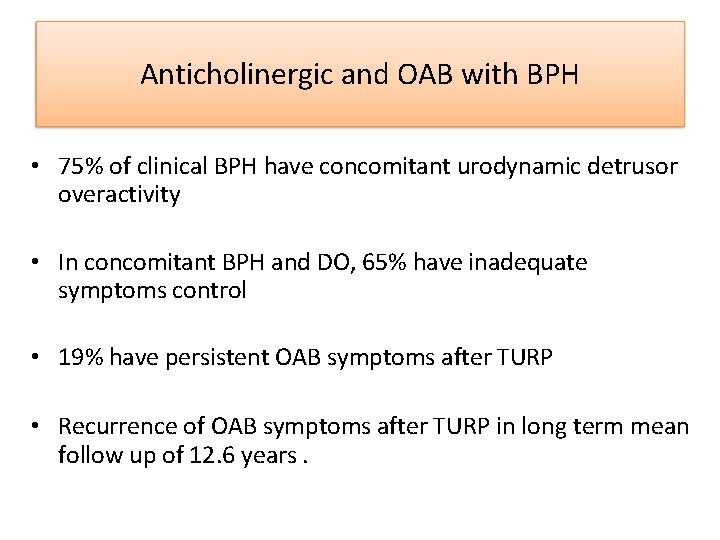
Anticholinergic and OAB with BPH • 75% of clinical BPH have concomitant urodynamic detrusor overactivity • In concomitant BPH and DO, 65% have inadequate symptoms control • 19% have persistent OAB symptoms after TURP • Recurrence of OAB symptoms after TURP in long term mean follow up of 12. 6 years.
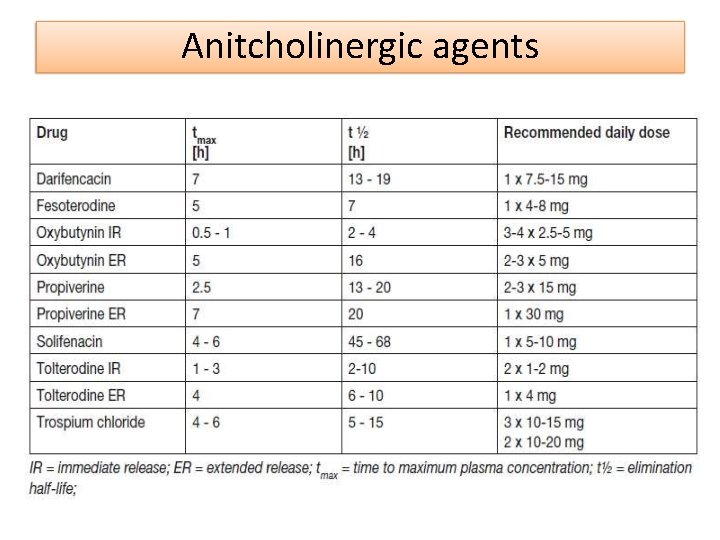
Anitcholinergic agents
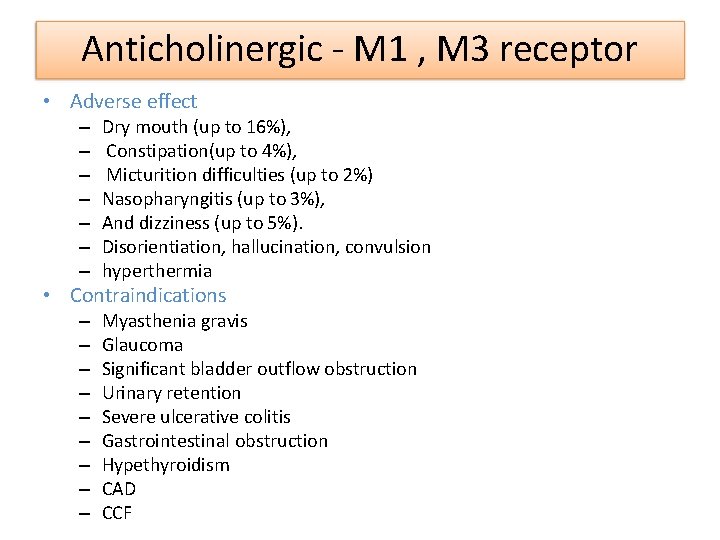
Anticholinergic - M 1 , M 3 receptor • Adverse effect – – – – Dry mouth (up to 16%), Constipation(up to 4%), Micturition difficulties (up to 2%) Nasopharyngitis (up to 3%), And dizziness (up to 5%). Disorientiation, hallucination, convulsion hyperthermia • Contraindications – – – – – Myasthenia gravis Glaucoma Significant bladder outflow obstruction Urinary retention Severe ulcerative colitis Gastrointestinal obstruction Hypethyroidism CAD CCF
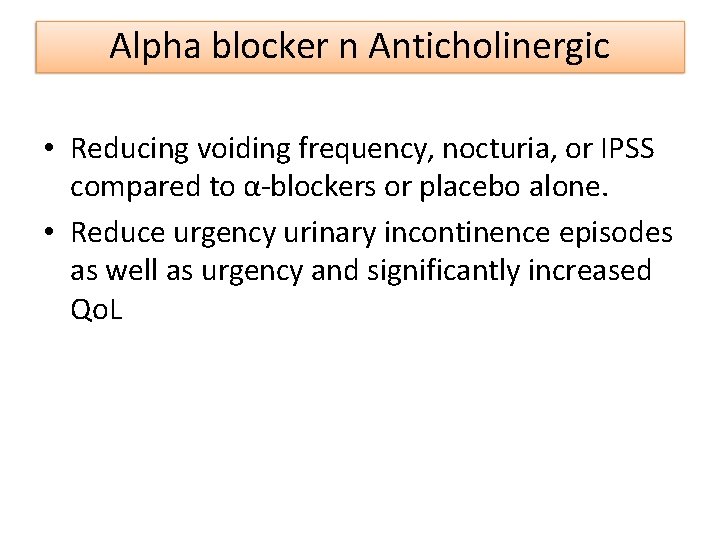
Alpha blocker n Anticholinergic • Reducing voiding frequency, nocturia, or IPSS compared to α-blockers or placebo alone. • Reduce urgency urinary incontinence episodes as well as urgency and significantly increased Qo. L
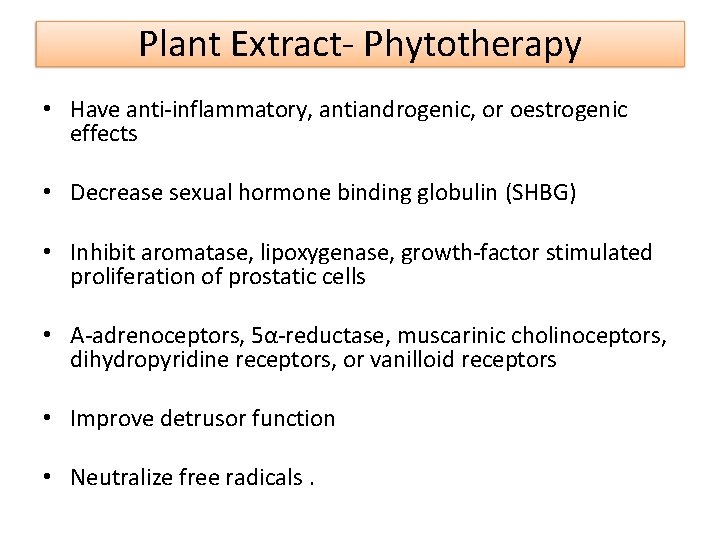
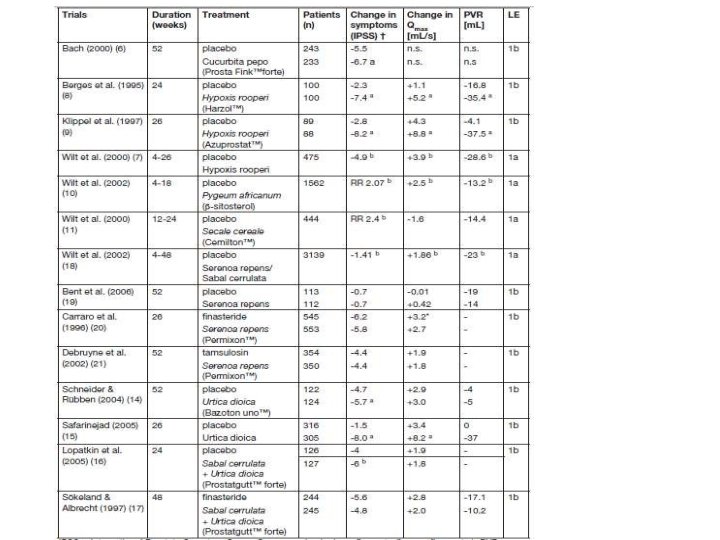
Plant Extract- Phytotherapy • Have anti-inflammatory, antiandrogenic, or oestrogenic effects • Decrease sexual hormone binding globulin (SHBG) • Inhibit aromatase, lipoxygenase, growth-factor stimulated proliferation of prostatic cells • Α-adrenoceptors, 5α-reductase, muscarinic cholinoceptors, dihydropyridine receptors, or vanilloid receptors • Improve detrusor function • Neutralize free radicals.
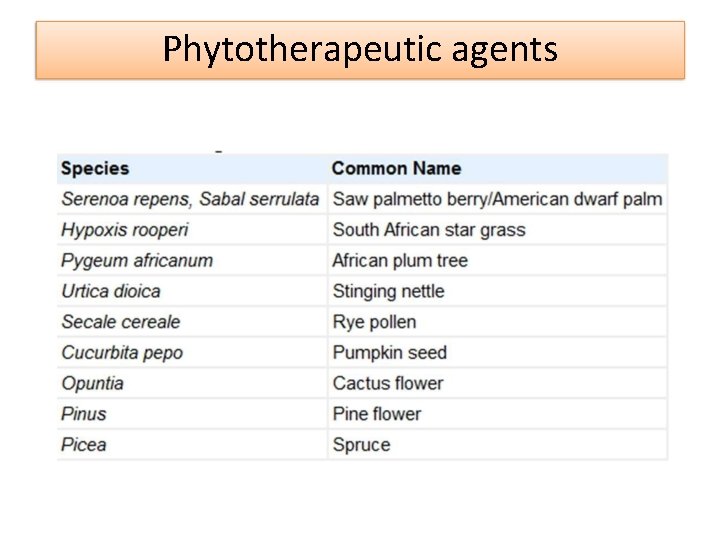
Phytotherapeutic agents
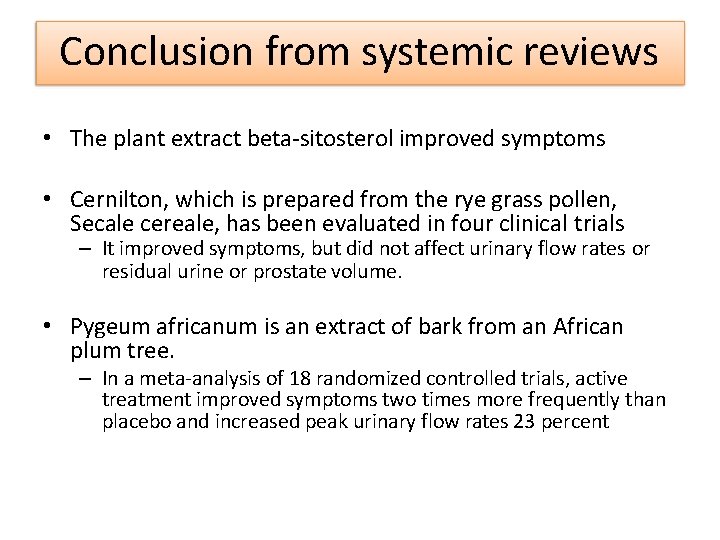
Conclusion from systemic reviews • The plant extract beta-sitosterol improved symptoms • Cernilton, which is prepared from the rye grass pollen, Secale cereale, has been evaluated in four clinical trials – It improved symptoms, but did not affect urinary flow rates or residual urine or prostate volume. • Pygeum africanum is an extract of bark from an African plum tree. – In a meta-analysis of 18 randomized controlled trials, active treatment improved symptoms two times more frequently than placebo and increased peak urinary flow rates 23 percent
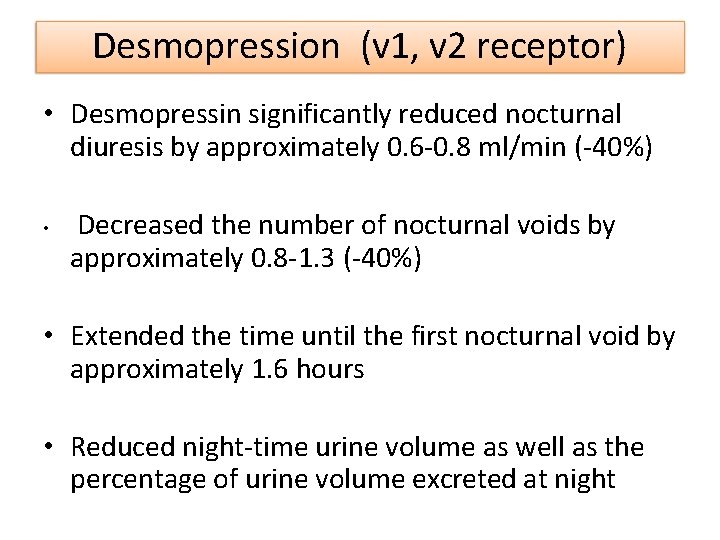
Desmopression (v 1, v 2 receptor) • Desmopressin significantly reduced nocturnal diuresis by approximately 0. 6 -0. 8 ml/min (-40%) • Decreased the number of nocturnal voids by approximately 0. 8 -1. 3 (-40%) • Extended the time until the first nocturnal void by approximately 1. 6 hours • Reduced night-time urine volume as well as the percentage of urine volume excreted at night
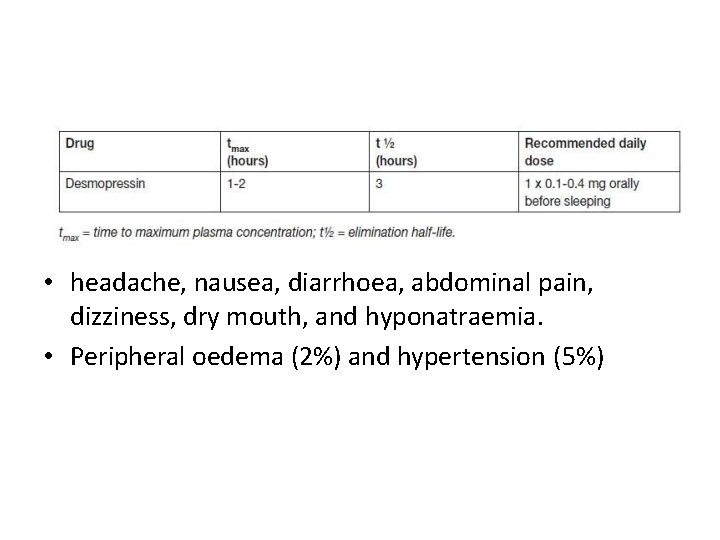
• headache, nausea, diarrhoea, abdominal pain, dizziness, dry mouth, and hyponatraemia. • Peripheral oedema (2%) and hypertension (5%)
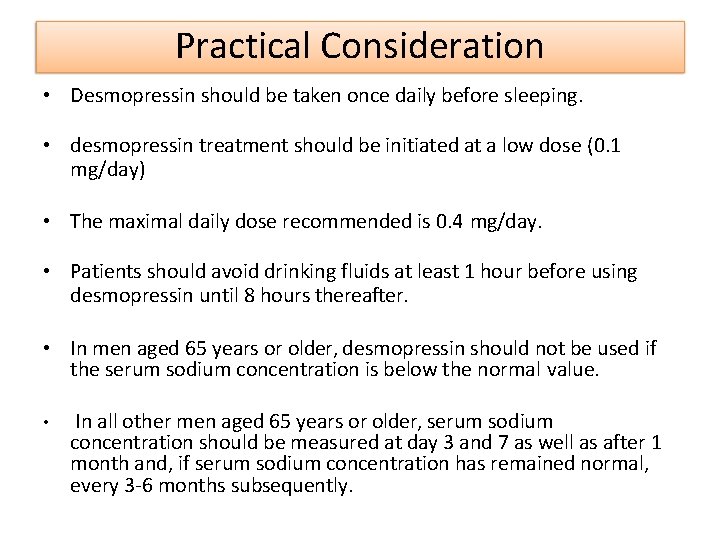
Practical Consideration • Desmopressin should be taken once daily before sleeping. • desmopressin treatment should be initiated at a low dose (0. 1 mg/day) • The maximal daily dose recommended is 0. 4 mg/day. • Patients should avoid drinking fluids at least 1 hour before using desmopressin until 8 hours thereafter. • In men aged 65 years or older, desmopressin should not be used if the serum sodium concentration is below the normal value. • In all other men aged 65 years or older, serum sodium concentration should be measured at day 3 and 7 as well as after 1 month and, if serum sodium concentration has remained normal, every 3 -6 months subsequently.
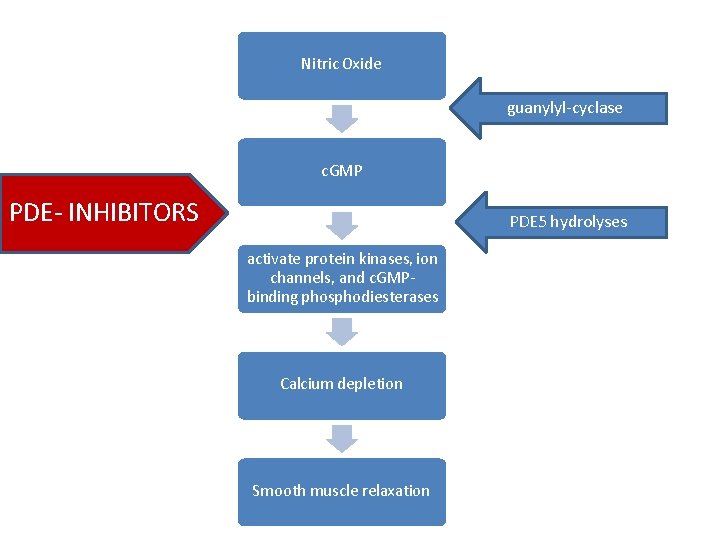
Nitric Oxide guanylyl-cyclase c. GMP PDE- INHIBITORS PDE 5 hydrolyses activate protein kinases, ion channels, and c. GMPbinding phosphodiesterases Calcium depletion Smooth muscle relaxation
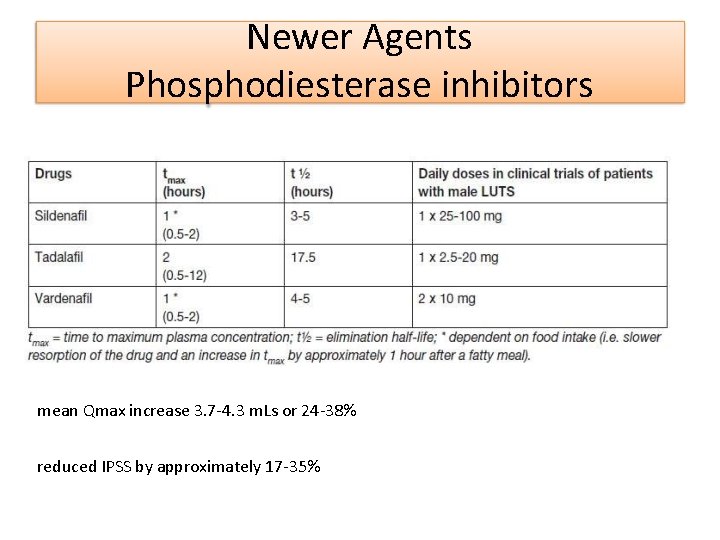
Newer Agents Phosphodiesterase inhibitors mean Qmax increase 3. 7 -4. 3 m. Ls or 24 -38% reduced IPSS by approximately 17 -35%
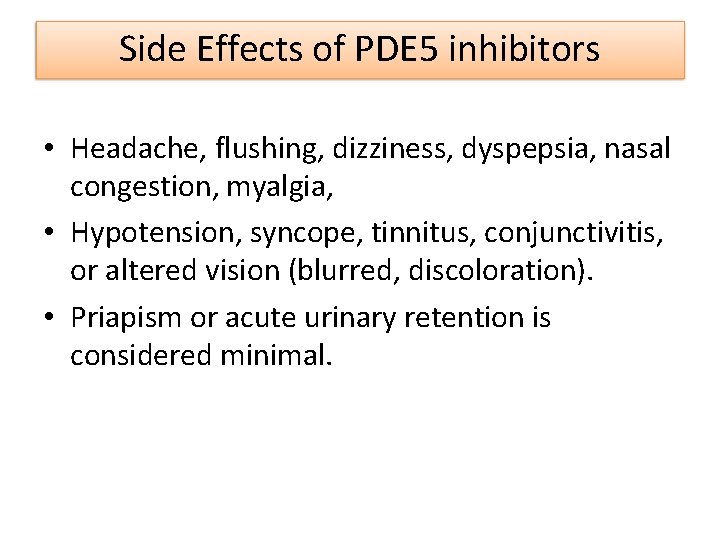
Side Effects of PDE 5 inhibitors • Headache, flushing, dizziness, dyspepsia, nasal congestion, myalgia, • Hypotension, syncope, tinnitus, conjunctivitis, or altered vision (blurred, discoloration). • Priapism or acute urinary retention is considered minimal.
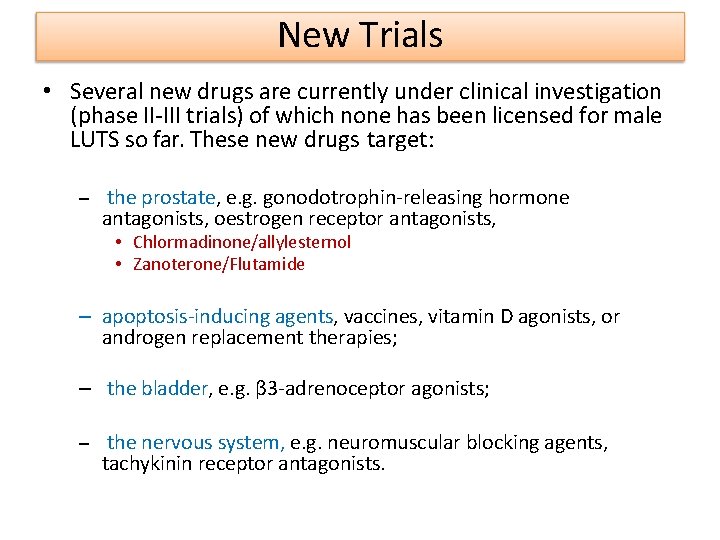
New Trials • Several new drugs are currently under clinical investigation (phase II-III trials) of which none has been licensed for male LUTS so far. These new drugs target: – the prostate, e. g. gonodotrophin-releasing hormone antagonists, oestrogen receptor antagonists, • Chlormadinone/allylesternol • Zanoterone/Flutamide – apoptosis-inducing agents, vaccines, vitamin D agonists, or androgen replacement therapies; – the bladder, e. g. β 3 -adrenoceptor agonists; – the nervous system, e. g. neuromuscular blocking agents, tachykinin receptor antagonists.

Is long-term therapy with a 1 -adrenoceptor antagonists recommended? Approximately 18, 64, and 36– 80% of patients withdrew from the studies after 2, 3, and >4 years, respectively.
What foods and dietary habits are recommended for patients with BPH?

Is a reduced alcohol intake recommended in patients with BPH

What treatments are recommended for urinary retention by BPH?
What therapeutic strategies are recommended to avoid sexual dysfunction as an adverse event?
References • JUA clinical guidelines for benign prostatic hyperplasia • EUA guidelines for LUTS • AUA Guidelines • Campbell Urology- 12 th edn

- Slides: 49