Complications of Extraction of Impacted Teeth Outline I














- Slides: 38
Complications of Extraction of Impacted Teeth
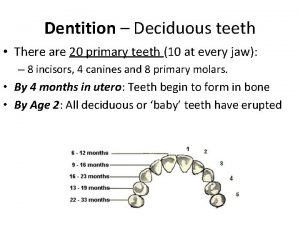
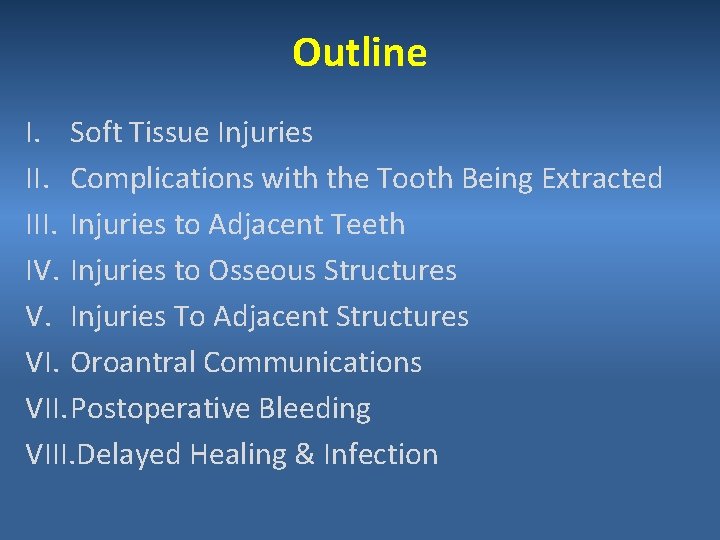
Outline I. Soft Tissue Injuries II. Complications with the Tooth Being Extracted III. Injuries to Adjacent Teeth IV. Injuries to Osseous Structures V. Injuries To Adjacent Structures VI. Oroantral Communications VII. Postoperative Bleeding VIII. Delayed Healing & Infection
I. Soft Tissue Injuries
1. Tearing Mucosal Flap Causes Due to an inadequately sized flap which is retracted beyond the tissue`s ability to stretch. As with a short envelope flap when the area of surgery is at the apex.
Prevention -Adequately sized flaps -Gentle Retraction Management Reposition the flap & suture If the tear is jagged, trim it before suturing
2. Puncture Wound of Soft Tissue Cause Instrument Slippage Prevention Controlled force Management Suturing to prevent infection & allow healing to occur

3. Stretch or Abrasion Injury Cause Bur shank or retractor injury Prevention Care Management Keep it moist ( ointment ) Heals within 5 – 10 days

II. Complications with the tooth Being Extracted
1. Root Fracture Cause Long, curved, divergent roots Excessive force during extraction Prevention Proper exposure & bone removal

2. Root Displacement Into: • Mandibular Canal • Lingual Pouch • Infratemporal Space • Maxillary Sinus




III. Injuries to Adjacent Teeth 1. Luxation of Adjacent Teeth 2. Fracture of Adjacent Restoration Cause Carelesness Prevention Judicious use of elevators
IV. Injuries to Osseous Structures
1. Fracture of Alveolar Process Fracture of the Buccal or Lingual Cortex Cause Inadequate exposure & excessive force Prevention Adequate bone removal & eposure

2. Fracture of Maxillary Tuberosity Cause Excessive force Prevention Proper support and controlled force Management If still attached; dissect and remove the tooth If detached; smooth bone edges & suture

3. Fracture of the Mandible Cause Excessive force Prevention Proper bone removal & controlled force
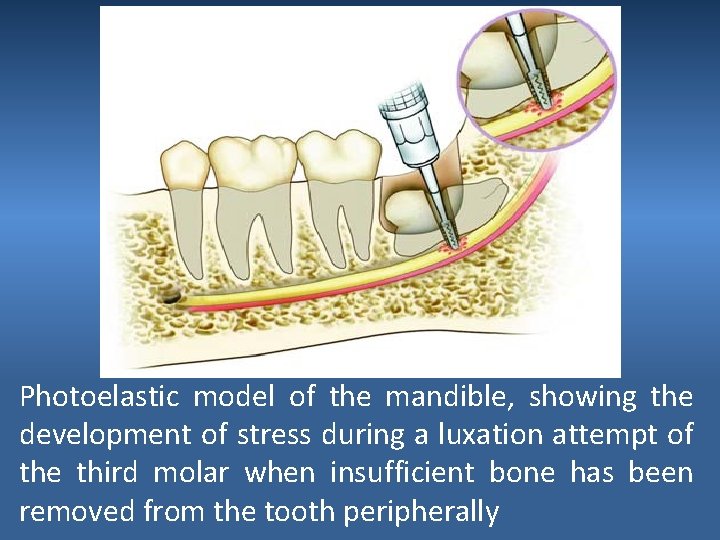
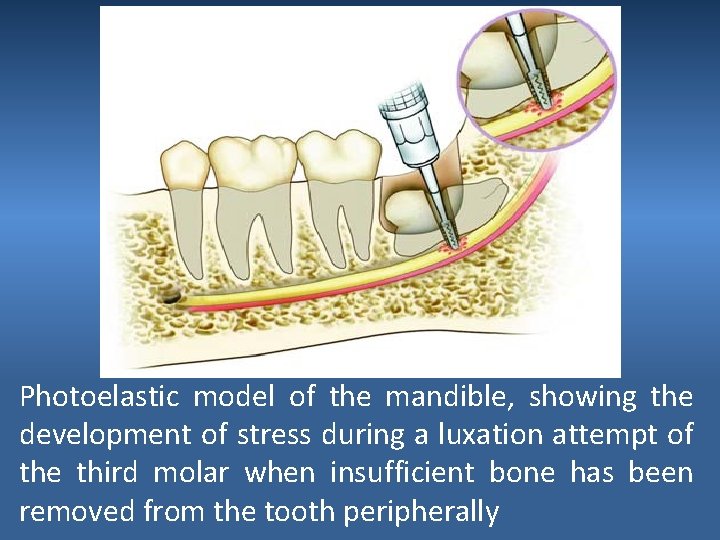
Photoelastic model of the mandible, showing the development of stress during a luxation attempt of the third molar when insufficient bone has been removed from the tooth peripherally
V. Injuries to Adjacent Structures
1. Injury to Inferior Alveolar Nerve Cause -Excessive extraction force in case of curved roots -Sectioning the tooth all the way inferiorly Prevention -Proper exposure & bone removal -Controlled force -Careful setioning, leaving a shell of the tooth

2. Injury to the Lingual Nerve Cause -Placement of the retromolar incision far lingually -Sectioning the tooth all the way to the lingual cortex Prevention -Proper incision -Careful sectioning, leaving a shell of the tooth
3. Injury to the TMJ Cause Inadequate support of the mandible during extraction Prevention Use of bite block Management Reduction


Vi. Oroantral Communication Cause During extraction of an impacted maxillary canine -Excessive bone removal -Failure to locate the tooth Prevention -Proper preoperative radiographic evaluation -Proper bone removal -Controlled force

VII. Postoperative Bleeding Cause -Bleeding at wound margins -Bleeding at a bony foramen within the socket -Medical Problem
Prevention -Good history taking (coagulopathy, medications…etc) -Atrumatic surgical extraction (clean incisions, gentle management of soft tissues, smoothen bony specules, curette granulation tissue) -Obtain good homeostasis at surgery - Postoperative instructions
Management Local Measures • Pressure packs • Suturing • Ligate bleeding vessels • Burnish bone • Apply material to aid in hemostasis (surgicell, collaplug)

VIII. Delayed Healing & Infection
1. Infection Cause Debris left under the flap Prevention Irrigation Management Debridement & Drainage
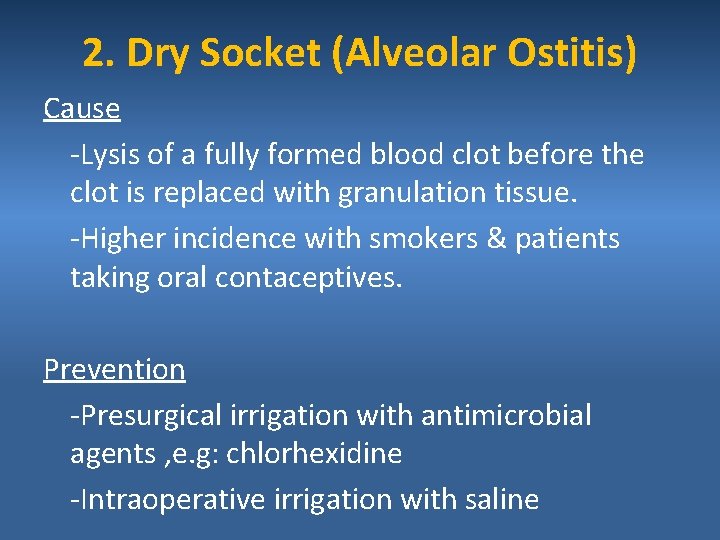
2. Dry Socket (Alveolar Ostitis) Cause -Lysis of a fully formed blood clot before the clot is replaced with granulation tissue. -Higher incidence with smokers & patients taking oral contaceptives. Prevention -Presurgical irrigation with antimicrobial agents , e. g: chlorhexidine -Intraoperative irrigation with saline
Management – Irrigate with warm saline – Remove old clots – Place sedative dressing – Prescribe mild analgesics – Reassess after 24 to 48 hours
 Contraindications for extraction of teeth
Contraindications for extraction of teeth Lingual split technique diagram
Lingual split technique diagram How has the printing press impacted society
How has the printing press impacted society Archer's classification impacted canines
Archer's classification impacted canines Why is canada rarely impacted by natural weather hazards
Why is canada rarely impacted by natural weather hazards Impacted colon pictures
Impacted colon pictures Mcq on higher education
Mcq on higher education Impacted stool symptoms
Impacted stool symptoms Otomycosis icd 10
Otomycosis icd 10 Example of a sentence outline
Example of a sentence outline Sle mnemonic soap brain md
Sle mnemonic soap brain md Lecture title
Lecture title Lower segment caesarean section slideshare
Lower segment caesarean section slideshare Complications of otitis media
Complications of otitis media Gdm presentation
Gdm presentation Complications c section
Complications c section Iliac stent complications
Iliac stent complications Pop cast complications
Pop cast complications Bronchoscopy complications
Bronchoscopy complications Cva complications
Cva complications Brain hemorrhage
Brain hemorrhage What are the complications of blood transfusion
What are the complications of blood transfusion Prefibrotic primary myelofibrosis
Prefibrotic primary myelofibrosis Complications of gestational diabetes
Complications of gestational diabetes Complications of mechanical ventilation
Complications of mechanical ventilation Define homans sign
Define homans sign Complications of myelofibrosis
Complications of myelofibrosis Dr tachere
Dr tachere Diolopia
Diolopia 15yo
15yo Post dated pregnancy complications
Post dated pregnancy complications Septic arthritis complications
Septic arthritis complications Complications of blood transfusion
Complications of blood transfusion Algodystrophy
Algodystrophy Complications c section
Complications c section Vasovagal reaction
Vasovagal reaction Lights criteria
Lights criteria Duodenal switch complications
Duodenal switch complications Heart failure complications
Heart failure complications