Complications after patellar stabilization surgery and how to
Complications after patellar stabilization surgery and how to avoid them.

Objectives Drew E. Warnick M. D. Children’s Orthopaedic and Scoliosis Surgery Associates, LLP. St. Petersburg, Florida • Surgical Director of Pediatric Sports Medicine Johns Hopkins All Children’s Hospital • USF Residency program Surgical Director IMG academy Bradenton
Complications after patellar stabilization surgery and how to avoid them. Overview Complications of MPFLR Preventable/technical complications of MPFLR Complications of distal realignment in children Proposed techniques/considerations to avoid complications Management of complications
Complications after patellar stabilization surgery and how to avoid them Complication Rate after MPFLR -8 -26% 26. 1% Overall complication rate after MPFLR Sys review Shah et al. AJSM 2012 Aug. 8. 3% Overall complication rate MPFLR Double bundle reconstruction may have less complications 7. 7% Complication rate Double Bundle MPFLR 10. 6% Complication rate single Bundle MPFLR Sys Review Kang et al. Knee Surg Sports Traum Arth. 2018 Aug.
Complications after patellar stabilization surgery and how to avoid them Complication Rate after MPFL In Young patients – 16% Complication rate after MPFL reconstruction in young patients 16. 2% Level 4 evidence, Case series of 179 knees Parikh et al. AJSM 2013
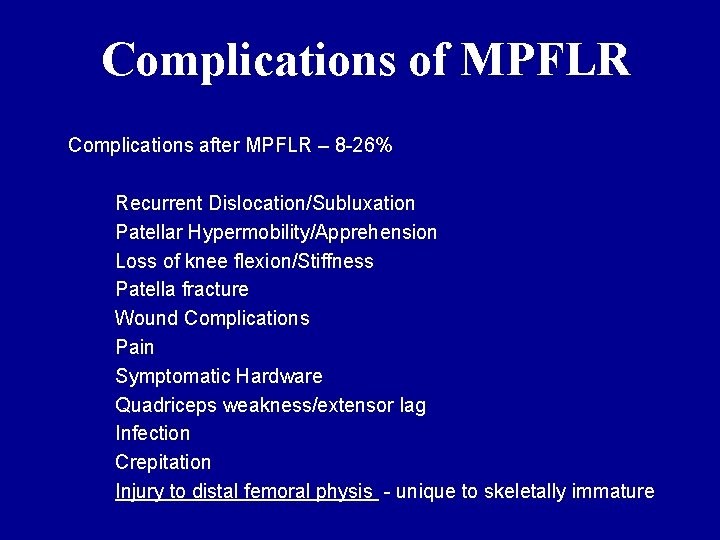
Complications of MPFLR Complications after MPFLR – 8 -26% Recurrent Dislocation/Subluxation Patellar Hypermobility/Apprehension Loss of knee flexion/Stiffness Patella fracture Wound Complications Pain Symptomatic Hardware Quadriceps weakness/extensor lag Infection Crepitation Injury to distal femoral physis - unique to skeletally immature
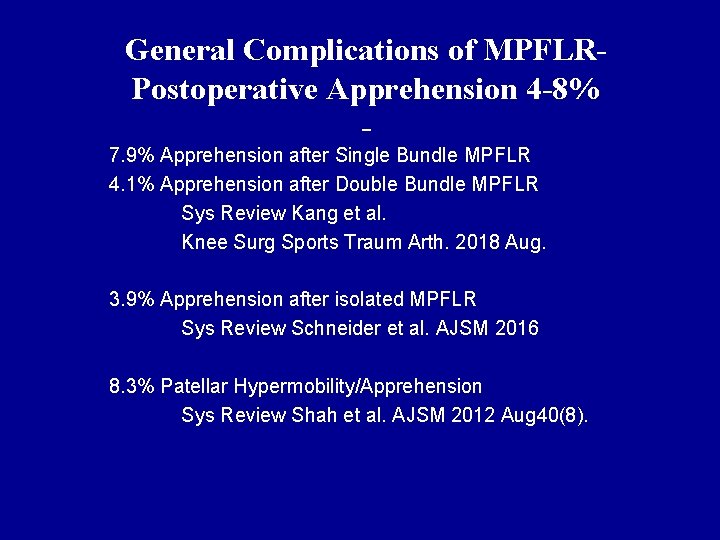
General Complications of MPFLRPostoperative Apprehension 4 -8% 7. 9% Apprehension after Single Bundle MPFLR 4. 1% Apprehension after Double Bundle MPFLR Sys Review Kang et al. Knee Surg Sports Traum Arth. 2018 Aug. 3. 9% Apprehension after isolated MPFLR Sys Review Schneider et al. AJSM 2016 8. 3% Patellar Hypermobility/Apprehension Sys Review Shah et al. AJSM 2012 Aug 40(8).
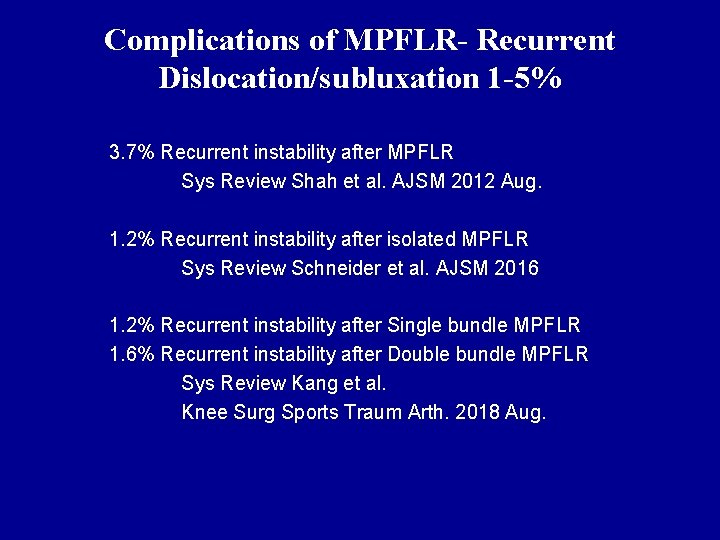
Complications of MPFLR- Recurrent Dislocation/subluxation 1 -5% 3. 7% Recurrent instability after MPFLR Sys Review Shah et al. AJSM 2012 Aug. 1. 2% Recurrent instability after isolated MPFLR Sys Review Schneider et al. AJSM 2016 1. 2% Recurrent instability after Single bundle MPFLR 1. 6% Recurrent instability after Double bundle MPFLR Sys Review Kang et al. Knee Surg Sports Traum Arth. 2018 Aug.
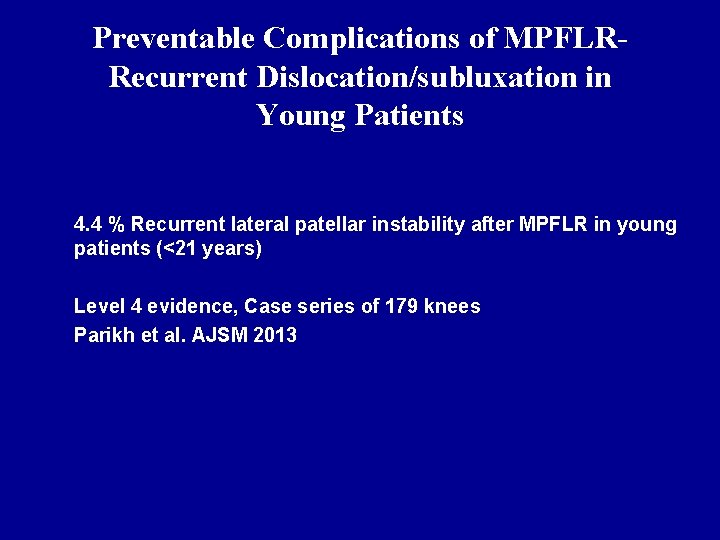
Preventable Complications of MPFLRRecurrent Dislocation/subluxation in Young Patients 4. 4 % Recurrent lateral patellar instability after MPFLR in young patients (<21 years) Level 4 evidence, Case series of 179 knees Parikh et al. AJSM 2013
Proposed techniques/considerations to avoid- Recurrent Dislocation/subluxation in Young Patients Avoid malposition of the femoral tunnel by using anatomic and radiographic landmarks. 8 patients with recurrent lateral instability 7/8 had femoral tunnel malpositioning Level 4 evidence, Case series of 179 knees Parikh et al. AJSM 2013
Proposed techniques/considerations to avoid- Recurrent Dislocation/subluxation after MPFL Appropriate tensioning of graft Lack of appropriate tensioning of the graft intraoperatively can lead to lateral patellar instability. Conversely, over tightening of the graft can cause increased strain on the graft and ultimately result in failure
Preventable technical Complications of MPFLR Loss of knee flexion after MPFL 1. 4% Sys Review Shah et al. AJSM Aug. 40(8) Loss of knee flexion in young patients (<21 years) after MPFL 5% Case series, 179 knees, Parikh et al. AJSM 2013
Management of complications- Loss of knee flexion after MPFL Manipulation under anesthesia 8 patients with restricted flexion of the knee after MPFL 5 pts had anterior placement of femoral tunnel 3 pts had anterior and distal placement of femoral tunnel All underwent Manipulation under anesthesia and continued therapy All regained full ROM Parikh et al. AJSM 2013
Management of complications- Loss of knee flexion after MPFL Percutaneous release of graft § 2 cases of restricted knee motion after over tightening of the graft • 1 resulted in loss of flexion • 1 resulted in loss of extension. • Both were treated successfully with percutaneous release of the medial patellofemoral ligament graft Thaunat M Erasmus PJ. Recurrent patellar dislocation after medial patellofemoral ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2008;
Proposed techniques/considerations to avoid Loss of knee flexion Avoid anterior placement of the femoral tunnel Avoid anterior and distal placement of the femoral tunnel Parikh et al. AJSM 2013
Preventable/Technical Complications of MPFLR- Symptomatic Hardware 1 -57% 1. 1% Patients with Symptomatic Hardware Sys Review, Shah et al. AJSM 2012 Aug 40(8) 57% Pts with symptomatic hardware Nomera et al. Knee. 2000
Preventable/Technical Complications of MPFLR- Symptomatic Hardware 3 of 44 patients required removal of prominent or painful screw at femoral fixation site Steiner TM Torga-Spak R Teitge RA. Medial patellofemoral ligament reconstruction in patients with lateral patellar instability and trochlear dysplasia. Am J Sports Med. 2006
Preventable/Technical Complications of MPFLR- Symptomatic Hardware Pain at the fixation site in 57% of patients treated with staples and in 23% of patients treated with an integrated double-staple system. Nomura E Horiuchi Y Kihara M. A mid-term follow-up of medial patellofemoral ligament reconstruction using an artificial ligament for recurrent patellar dislocation. Knee. 2000
Proposed techniques to avoid complications - Symptomatic Hardware Avoid proud hardware on the medial femoral insertion Don’t use staples

Preventable/technical complications of MPFLR – Patella Fracture 3. 6% rate of patella fracture with 2 transpatellar 4. 5 mm tunnels Schiphouwer et al. Knee Surg Sports Traumatol Arthrosc. 2017 Jan; 25(1): 245 -250.
Preventable/technical complications of MPFLR – Patella Fracture 2012 AJSM Shah et al. Aug 40(8). Systematic review of complications 4 patients with patella fracture had transpatellar tunnels
Preventable/technical complications of MPFLR – Patella Fracture in Young Patients Case Series, 179 knees, Young patients < 21 years Parikh et al. AJSM 2013 6 pts had patella fractures 5 transverse patella fractures 1 avulsion fracture of superior pole
Preventable/technical complications of MPFLR – Patella Fracture in Young Patients 2 patients with an avulsion fracture of the patella at the fixation site Thaunat M Erasmus PJ. Recurrent patellar dislocation after medial patellofemoral ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2008
Proposed techniques/considerations to avoid complications– Patella Fracture Avoid transpatellar tunnels Avoid converging tunnels Use tunnels < 4. 5 mm diameter Use single tunnel
Proposed techniques/considerations to avoid complications- Patella Fracture Don’t Drill into the patella! • MQTFL provides anatomic reconstruction and avoids patella fracture Medial Quadriceps Tendon–Femoral Ligament: Surgical Anatomy and Reconstruction Technique to Prevent Patella Instability Fulkerson et al. Arthrosc Tech. 2013
Proposed techniques/considerations to avoid complications- Patella Fracture Don’t Drill into the patella! Creation of a bony sulcus and suture anchor fixation may avoid risk of patella fracture s Surgical Management of Patellofemoral Instability in the Skeletally Immature Patient s Redler et al. JAAOS Oct. 2018
Proposed techniques/considerations to avoid complications– Patella Fracture in Young Patients In young patients with a less ossified patella and small margin for error. Use techniques that do not require patellar bone tunnels (quadriceps or patellar tendon autograft or suture anchor fixation) to avoid this complication Redler et al. JAAOS Oct. 2018
Management of patella fractures after MPFL Parikh et al. AJSM 2013 – 6 pts whom sustained patella fractures after MPFL Transpatellar fractures ORIF with tension band Avulsion fractures Excision of avulsion fracture and quad tendon repair
Management of patella fractures after MPFL 2 patients with an avulsion fracture of the patella at the fixation site Both patients were treated with open reduction and internal fixation. Thaunat M Erasmus PJ. Recurrent patellar dislocation after medial patellofemoral ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2008
Preventable/technical complications of MPFLR – Patellofemoral arthritis in young patients 5 patients developed patellofemoral arthritis and pain after MFPL Parikh et al. AJSM 2013 Case series , 179 knees.

Proposed techniques/considerations to avoid complications– Patellofemoral arthritis Avoid anterior placement of femoral tunnel Parikh et al. AJSM 2013
Management of complications– Patellofemoral arthritis Revision MPFL reconstruction with anatomic placement of the femoral tunnel. Avoid anterior placement of femoral tunnel Parikh et al. AJSM 2013
Preventable/technical complications of MPFLR – Medial Patellofemoral dislocation § Case report § 1 patient with medial instability after MPFL with over tightening of the graft, lateral release and Elmslie Trillat procedure § Bollier M, Fulkerson J, Cosgarea A, Tanaka M. Technical failure of medial patellofemoral ligament reconstruction. Arthroscopy. 2011; 27: 1153 -1159.

Management of complications– Medial Patellofemoral dislocation after MPFL § 1 patient was treated with medial release, chondroplasty and lateral imbrication with pain relief and resolution of symptoms. § § Bollier M, Fulkerson J, Cosgarea A, Tanaka M. Technical failure of medial patellofemoral ligament reconstruction. Arthroscopy. 2011; 27: 1153 -1159.
Proposed techniques to avoid complications– Medial Patellofemoral dislocation and arthritis Identify anatomic and radiographic markers to avoid malposition of femoral tunnel Proximal malpositioning of the femoral tunnel has been shown to: Increases medial tilt Increases medial patellofemoral contact pressures Anterior malpositioning of the femoral tunnel has been shown to: Overload the medial facet. Elias JJ Cosgarea AJ. Technical errors during medial patellofemoral ligament reconstruction could overload medial patellofemoral cartilage: a computational analysis. Am J Sports Med. 2006
Preventable/technical complications of MPFLR – Growth Arrest Case Report 1 patient developed partial posterior physeal growth arrest and subsequent flexion deformity of the distal femur after MPFL reconstruction in a skeletally immature patient. § Knee. 2017 Jun; 24(3): 680 -685 Acquired femoral flexion deformity due to physeal injury during medial patellofemoral ligament reconstruction.
Management of complications– Growth Arrest causing flexion deformity Patient was successfully treated with distal femoral extension osteotomy and revision patellar stabilization surgery. § Knee. 2017 Jun; 24(3): 680 -685 Acquired femoral flexion deformity due to physeal injury during medial patellofemoral ligament reconstruction.
Proposed techniques to avoid complications – Growth arrest Grafts placed proximal to the physis have the unique complication of proximal migration of the insertion after reconstruction and high tension across the physis. Redler et al. JAAOS Oct. 2018
Proposed techniques to avoid complications – Growth arrest The MPFL attachment was an average of 8. 5 mm distal to the medial aspect of the distal femoral physis. Angle the tunnel distally and anteriorly to avoid injury to the distal femoral physis § L. D. Farrow, V. J. Alentado, Z. Abdulnabi, A. Gilmore, R. W. Liu § The relationship of the medial patellofemoral ligament attachment to the distal femoral physis § Am J Sports Med, 42 (2014),
Proposed techniques to avoid complications – Growth arrest It is also important to consider the perichondrium of the physis because it is sensitive to injury. Caution must be exercised to avoid violation of the perichondrium during both surgical dissection and tunnel placement. Redler et al. JAAOS Oct. 2018
Factors Critical for Successful MPFL Reconstruction – Femoral Tunnel positioning Get a true lateral radiograph and identify schottles point Schottle et al. Radiographic landmarks for femoral tunnel placement in medial patellofemoral ligament reconstruction. Am J Sports Med. 2007; 35(5): 801– 804. Angle the tunnel distally and anteriorly to avoid injury to the distal femoral physis in skeletally immature patients. § L. D. Farrow, V. J. Alentado, Z. Abdulnabi, A. Gilmore, R. W. Liu s The relationship of the medial patellofemoral ligament attachment to the distal femoral physis s Am J Sports Med, 42 (2014),
Factors Critical for Successful MPFL Reconstruction – Femoral Tunnel positioning Identify anatomic markers to avoid malposition of femoral tunnel The femoral tunnel should be placed at the anatomic insertion point of the ligament between the adductor tubercle and the medial femoral epicondyle § Redfern et al. Am J Sports Med. 2010 Feb; 38(2): 293 -7. Anatomical confirmation of the use of radiographic landmarks in medial patellofemoral ligament reconstruction.
Factors Critical for Successful MPFL Reconstruction – Patella Tunnel positioning The patellar tunnel should: Begin at the anatomic insertion of the ligament on the proximal half of the medial border of the patella Extend through the center of the patella in the sagittal plane. The mean width of the patellar attachment is 17 mm at its Insertion on the proximal two-thirds of the medial border of the patella Steensen et al. A simple technique for reconstruction of the medial patellofemoral ligament using a quadriceps tendon graft. Arthroscopy.

Factors Critical for Successful MPFL Reconstruction – Graft Tensioning § Graft tensioning is perhaps the most important factor in a successful medial patellofemoral ligament reconstruction. § The patella should be centered in the trochlear groove during the first 30° of flexion. § Complications of Medial Patellofemoral Ligament Reconstruction: Common Technical Errors and Factors for Success: AAOS Exhibit Selection § Tanaka, Miho J. MD; Bollier, Matthew J. MD; Andrish, Jack T. MD; Fulkerson, John P. MD; Cosgarea, Andrew J. MD
Distal realignment in children • • An elevated tibial tubercle to trochlear groove (TTTG) distance creates contributes to patellar instability. Because of the open apophysis, an osteotomy can not be used to address the elevated TT-TG distance in the skeletally immature patient.

Distal realignment in children • Patella alta cannot be treated with a distalizing osteotomy because of the risk of growth arrest and subsequent deformity.

Distal realignment in children • • Distal realignment procedures that avoid growth plate injury include Modified Roux-Goldthwait, Galeazzi Nietosvaara techniques.
Distal realignment in children • • • The modified Roux-Goldthwait procedure In an early study of 30 knees that underwent the procedure, 26 knees had excellent results based on the Insall criteria. Marsh JS, Daigneault JP, Sethi P, Polzhofer GK: Treatment of recurrent patellar instability with a modification of the Roux. Goldthwait technique. J Pediatr Orthop 2006; 26: 461– 465
• • Complications of distal realignment in children- Recurrent Subluxation or dislocation Galeazzi Semitendinosis Tenodesis A 2012 study of 34 knees treated with the procedure found that 35% required a second surgery and 82% had recurrent subluxation or dislocation It has largely been abandoned for more effective and anatomic reconstruction procedures Grannatt K, Heyworth BE, Ogunwole O, Micheli LJ, Kocher MS: Galeazzi semitendinosus tenodesis for patellofemoral instability in skeletally immature patients. J Pediatr Orthop 2012; 32: 621– 625.

Distal realignment in children Nietosvaara Procedure A more anatomic modification of the Galeazzi distal reconstruction Long-term outcome studies have not yet been performed. Nietosvaara et al: Acute patellar dislocation in children and adolescents: Surgical technique. J Bone Joint Surg Am 2009; 91: 139– 145.

Thank you • Email: dwarnick@chortho. com • Office: 727 -898 -2663 www. chortho. com
- Slides: 51