Complication of Type 2 diabetes Stroke Diabetic retinopathy
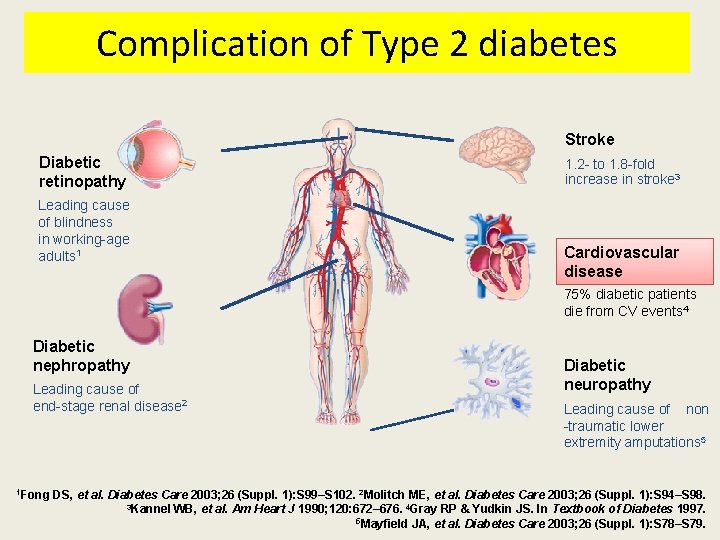
Complication of Type 2 diabetes Stroke Diabetic retinopathy Leading cause of blindness in working-age adults 1 1. 2 - to 1. 8 -fold increase in stroke 3 Cardiovascular disease 75% diabetic patients die from CV events 4 Diabetic nephropathy Leading cause of end-stage renal disease 2 1 Fong Diabetic neuropathy Leading cause of non -traumatic lower extremity amputations 5 DS, et al. Diabetes Care 2003; 26 (Suppl. 1): S 99–S 102. 2 Molitch ME, et al. Diabetes Care 2003; 26 (Suppl. 1): S 94–S 98. 3 Kannel WB, et al. Am Heart J 1990; 120: 672– 676. 4 Gray RP & Yudkin JS. In Textbook of Diabetes 1997. 5 Mayfield JA, et al. Diabetes Care 2003; 26 (Suppl. 1): S 78–S 79.
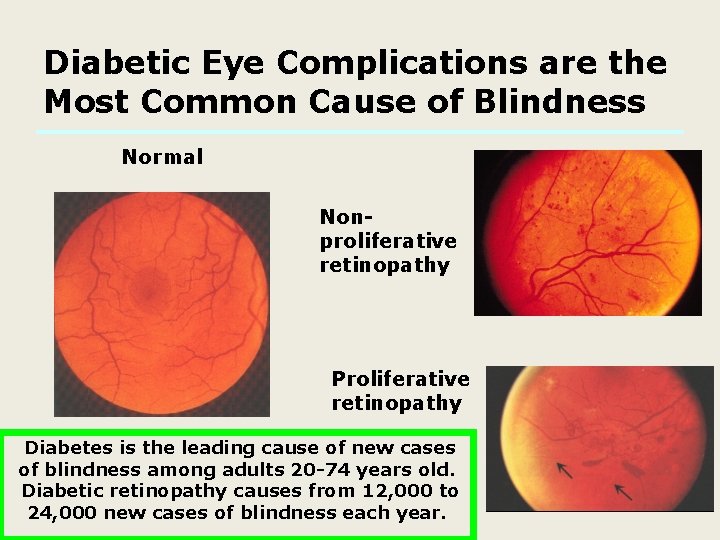
Diabetic Eye Complications are the Most Common Cause of Blindness Normal Nonproliferative retinopathy Proliferative retinopathy Diabetes is the leading cause of new cases of blindness among adults 20 -74 years old. Diabetic retinopathy causes from 12, 000 to 24, 000 new cases of blindness each year.

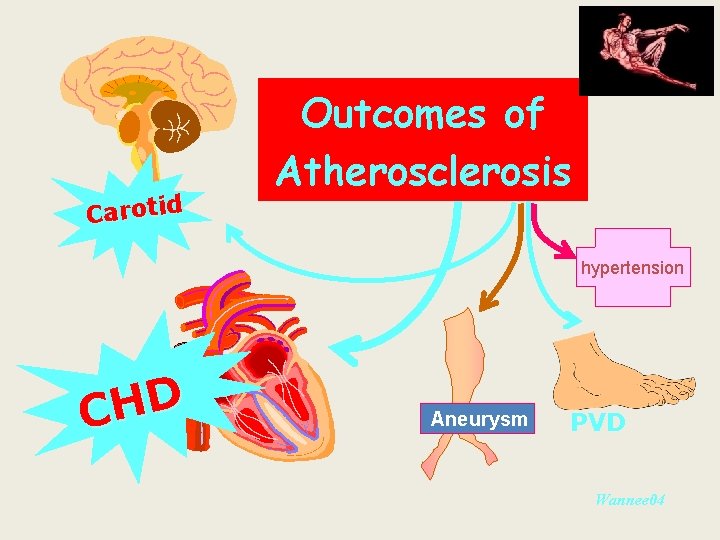
Carotid Outcomes of Atherosclerosis hypertension D H C Aneurysm PVD Wannee 04
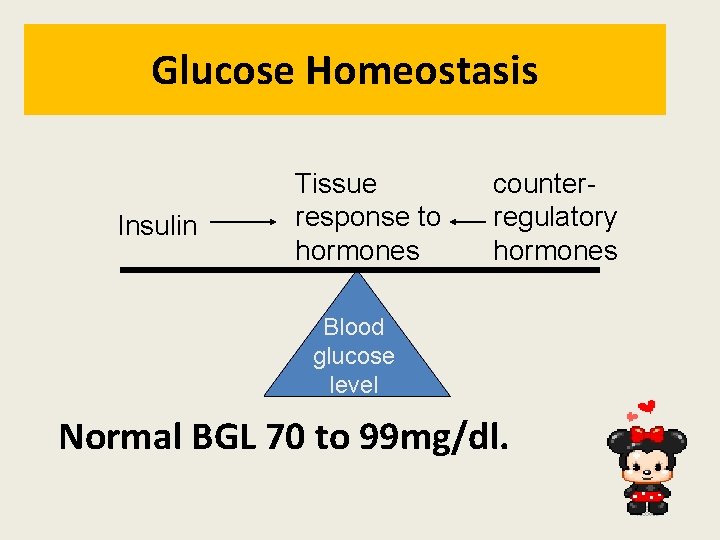
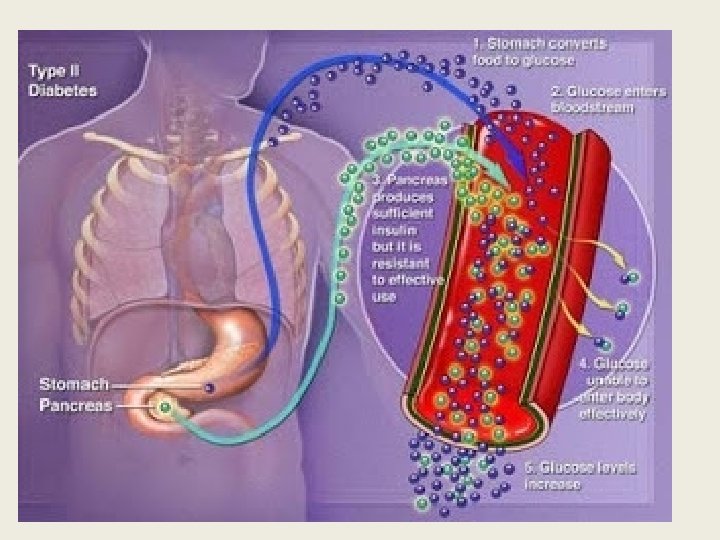
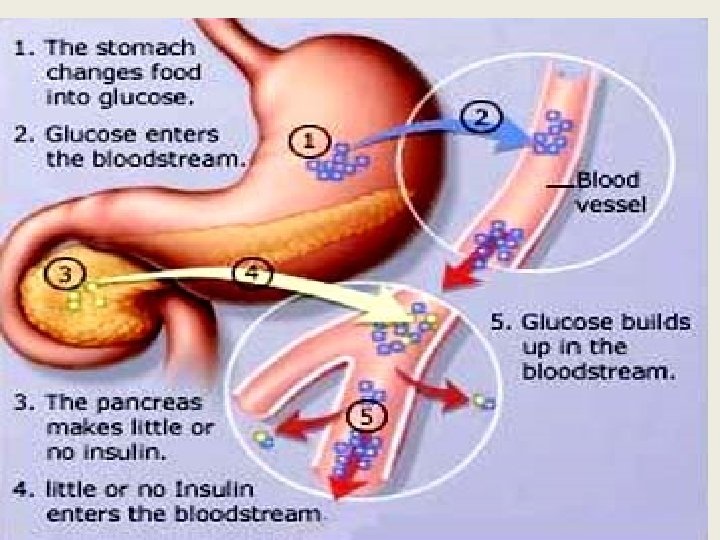
Glucose Homeostasis Insulin Tissue response to hormones counterregulatory hormones Blood glucose level Normal BGL 70 to 99 mg/dl.
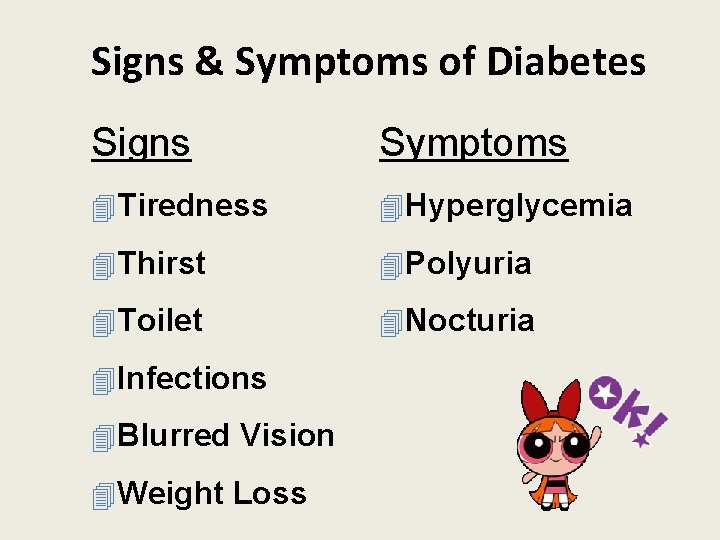
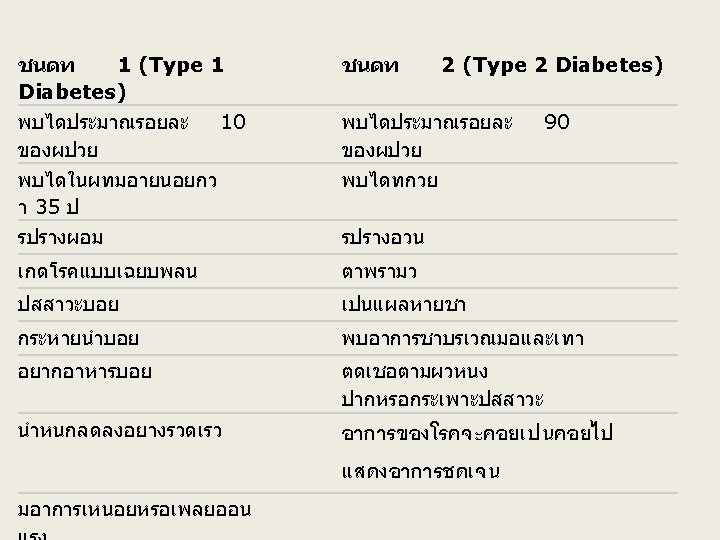
Signs & Symptoms of Diabetes Signs Symptoms 4 Tiredness 4 Hyperglycemia 4 Thirst 4 Polyuria 4 Toilet 4 Nocturia 4 Infections 4 Blurred Vision 4 Weight Loss
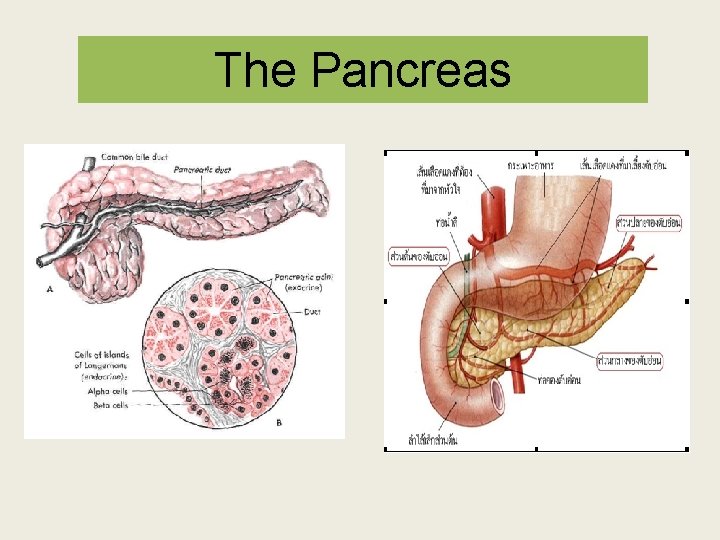
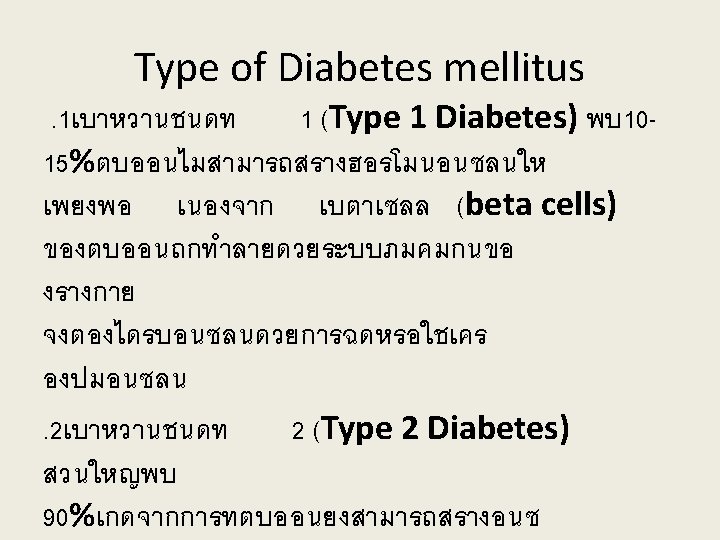
The Pancreas
Insulin Action Insulin secreted by the Beta cell in response to a rise in BGL) Blood glucose level( Glucagon secreted in response to a drop in Blood glucose level) BGL(
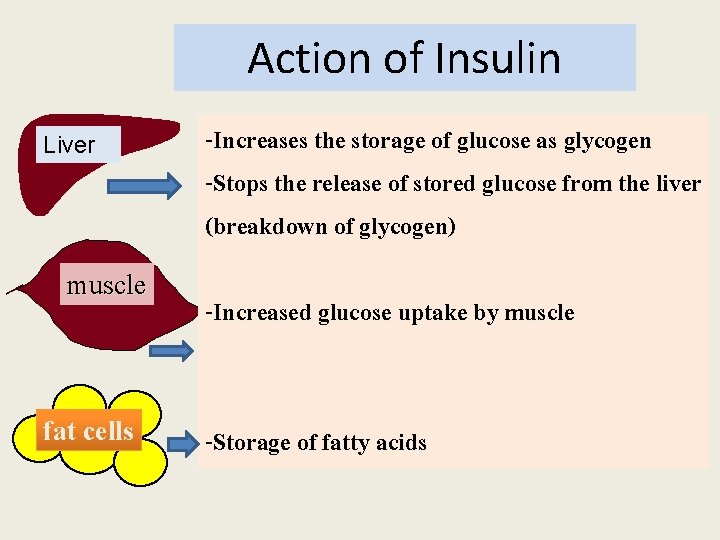
Action of Insulin Liver muscle fat cells -Increases the storage of glucose as glycogen -Stops the release of stored glucose from the liver (breakdown of glycogen) -Increased glucose uptake by muscle -Storage of fatty acids
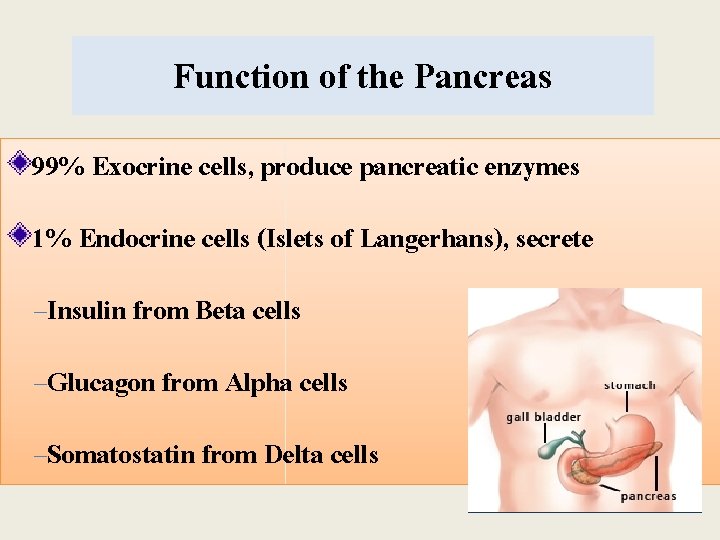
Function of the Pancreas 99% Exocrine cells, produce pancreatic enzymes 1% Endocrine cells (Islets of Langerhans), secrete –Insulin from Beta cells –Glucagon from Alpha cells –Somatostatin from Delta cells
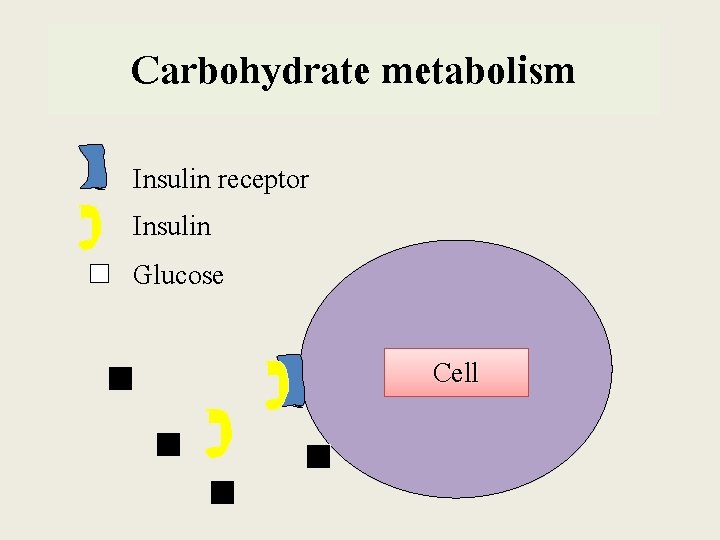
Carbohydrate metabolism Insulin receptor Insulin Glucose Cell
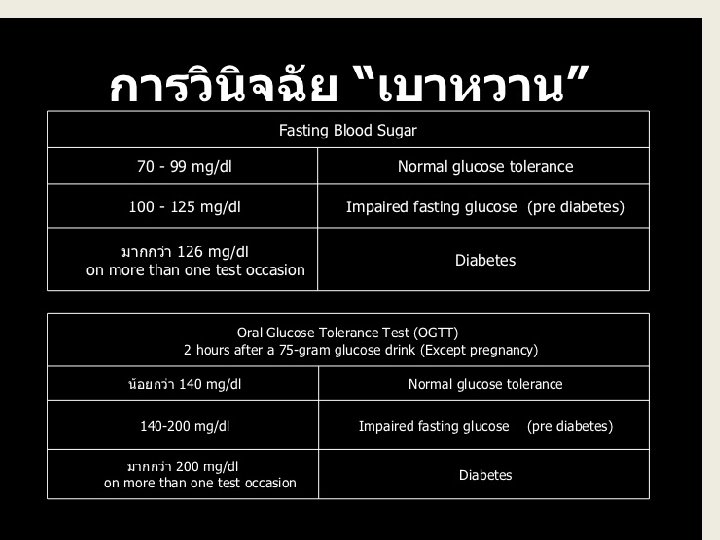
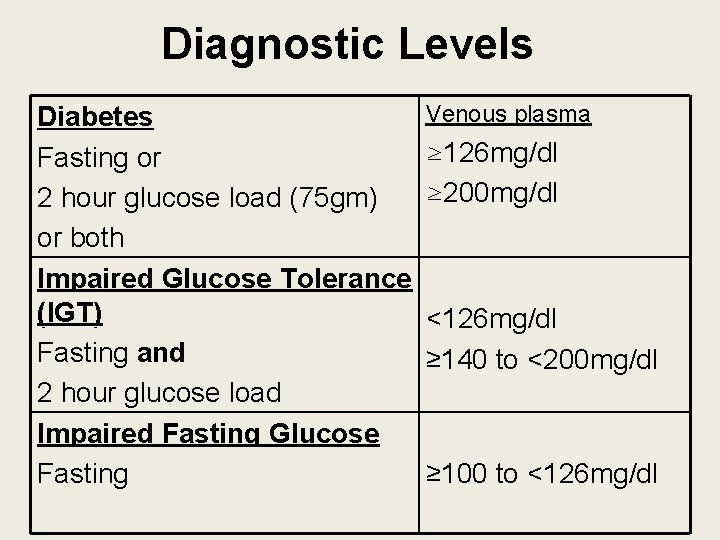
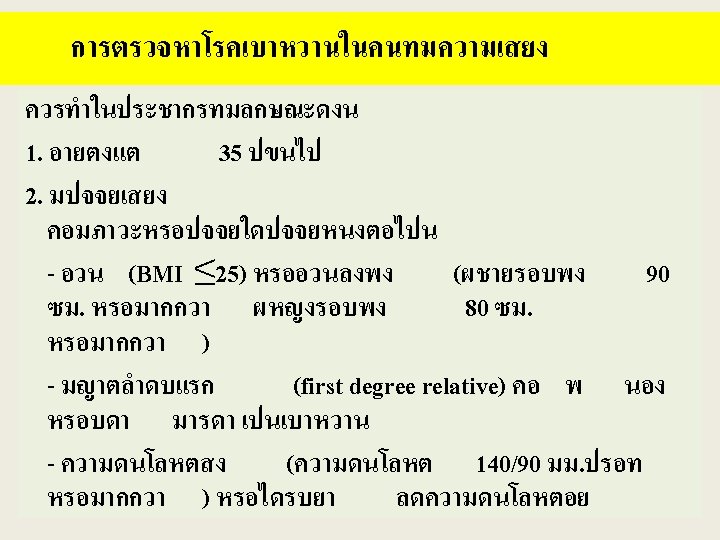
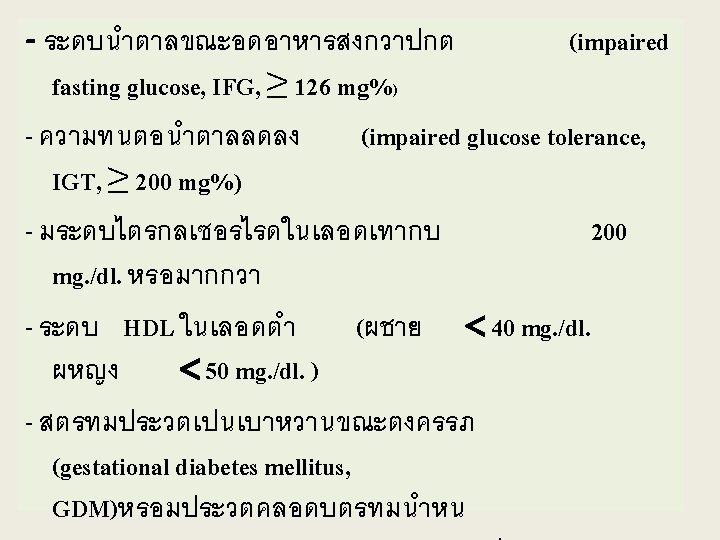
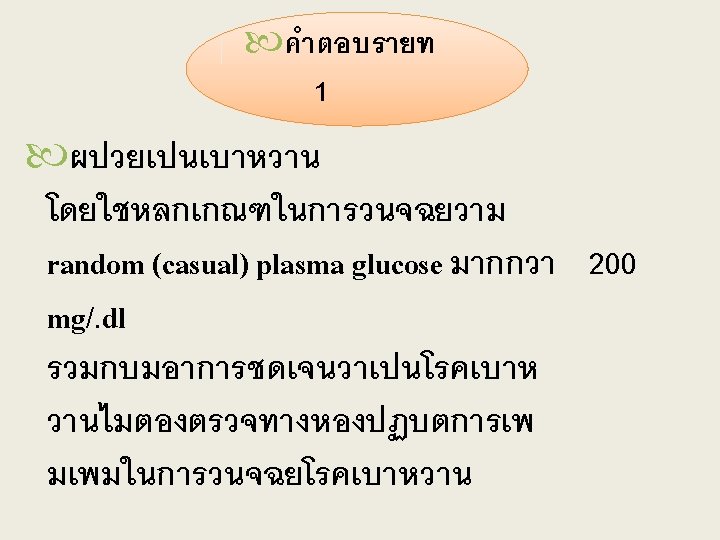
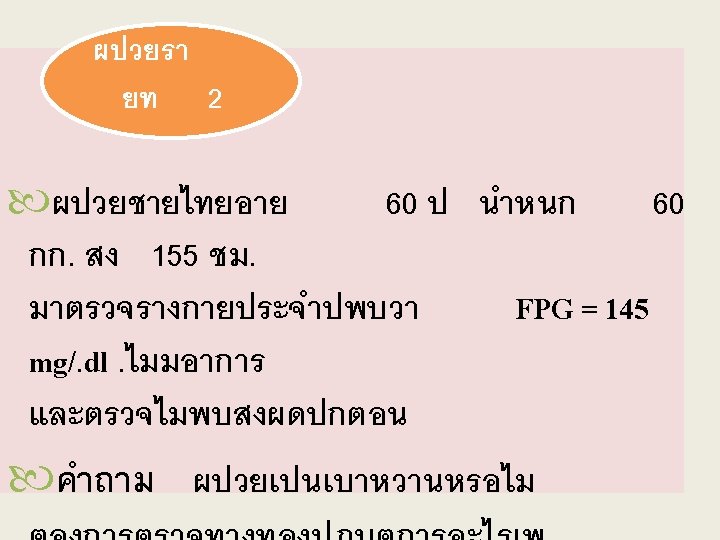
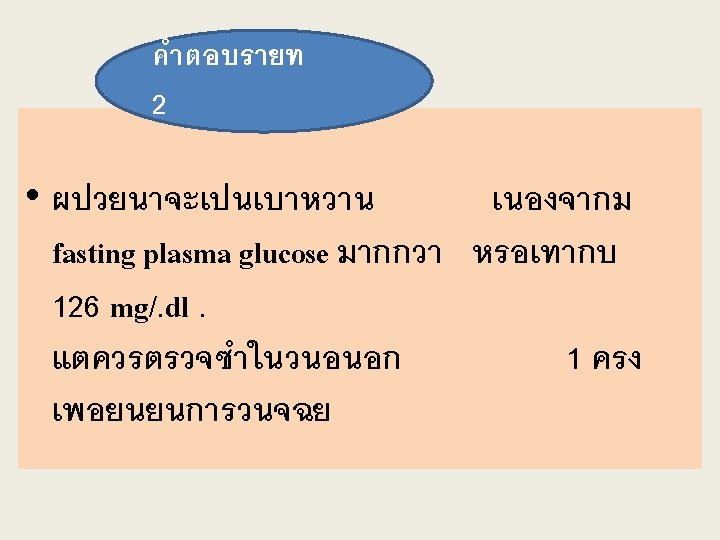
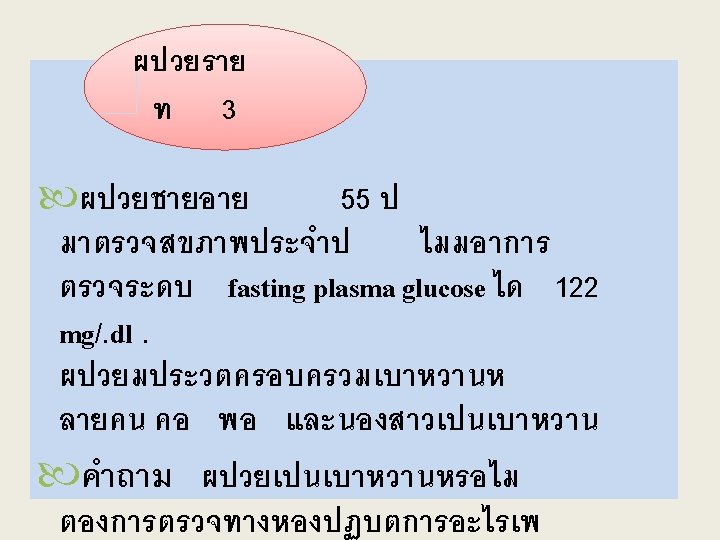
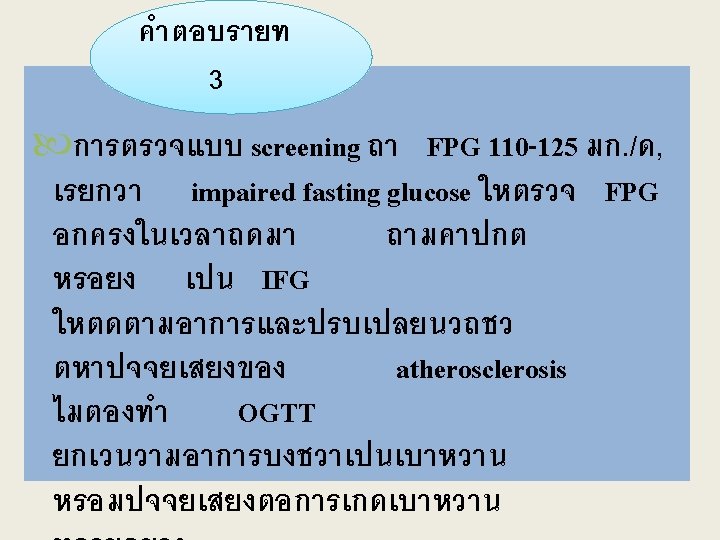
Diagnostic Levels Diabetes Fasting or 2 hour glucose load (75 gm) or both Impaired Glucose Tolerance (IGT) Fasting and 2 hour glucose load Impaired Fasting Glucose Fasting Venous plasma ≥ 126 mg/dl ≥ 200 mg/dl <126 mg/dl ≥ 140 to <200 mg/dl ≥ 100 to <126 mg/dl
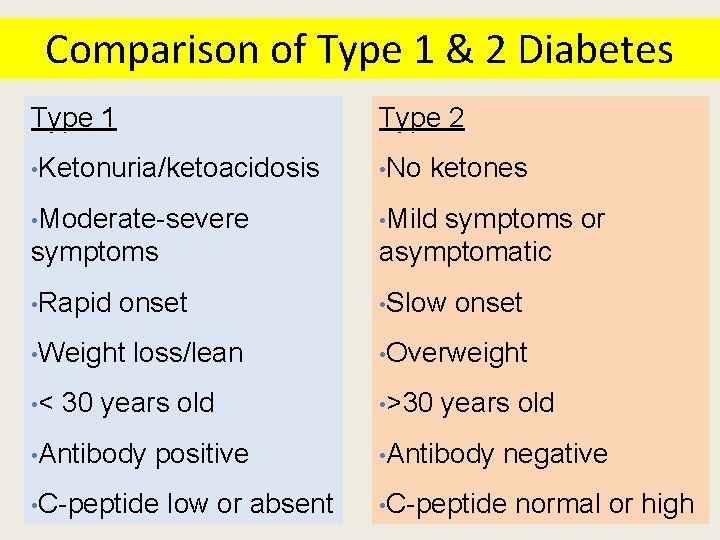
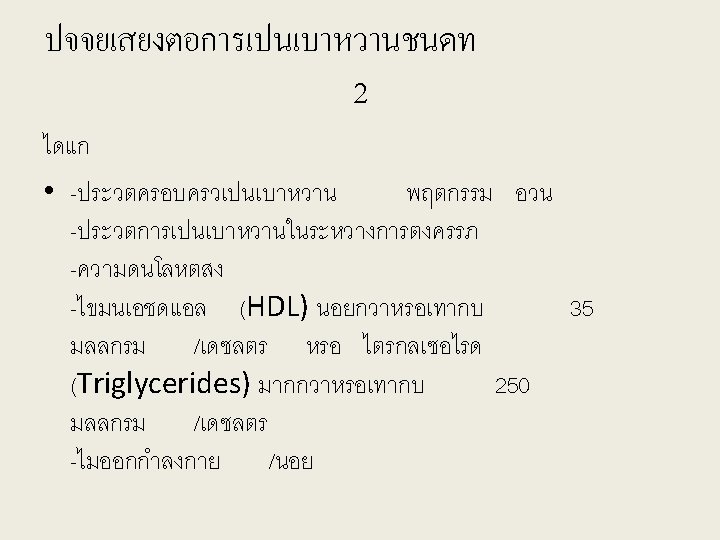
Comparison of Type 1 & 2 Diabetes Type 1 Type 2 • Ketonuria/ketoacidosis • No • Moderate-severe • Mild ketones symptoms or asymptomatic • Rapid • Slow onset • Weight • < loss/lean 30 years old • Antibody positive • C-peptide low or absent onset • Overweight • >30 years old • Antibody negative • C-peptide normal or high
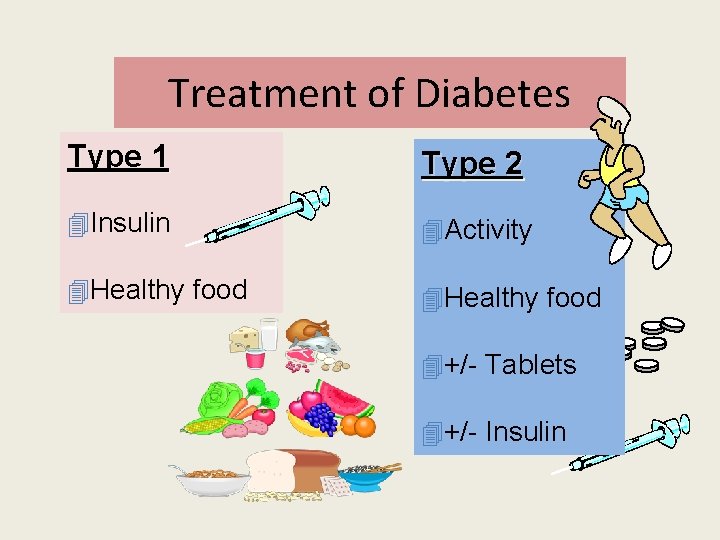
Treatment of Diabetes Type 1 Type 2 4 Insulin 4 Activity 4 Healthy food 4+/- Tablets 4+/- Insulin










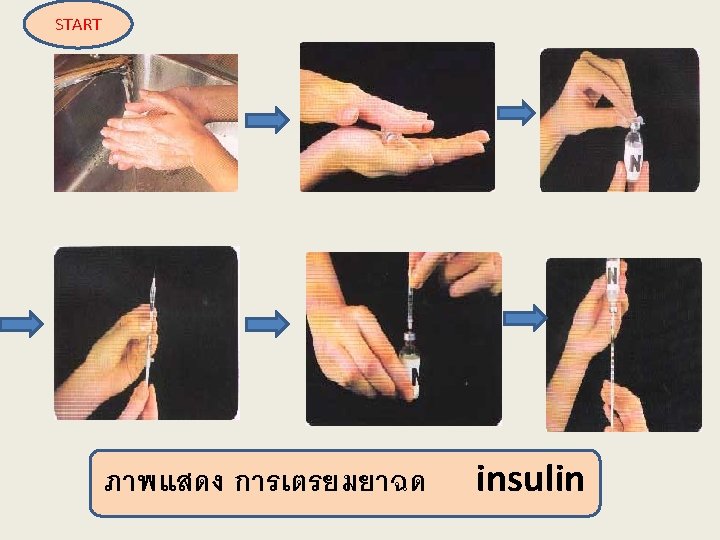
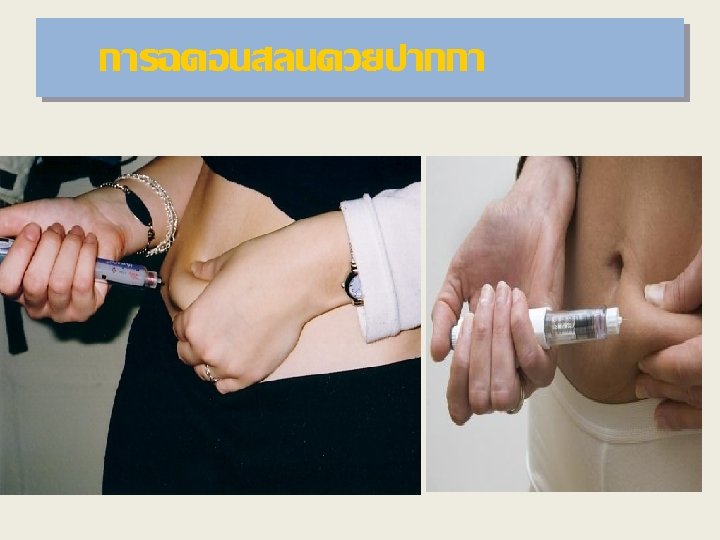
INSULIN INJECTION
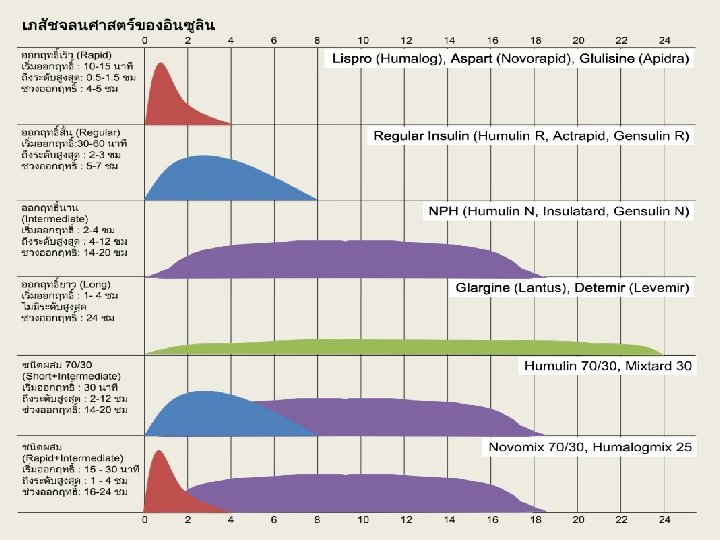
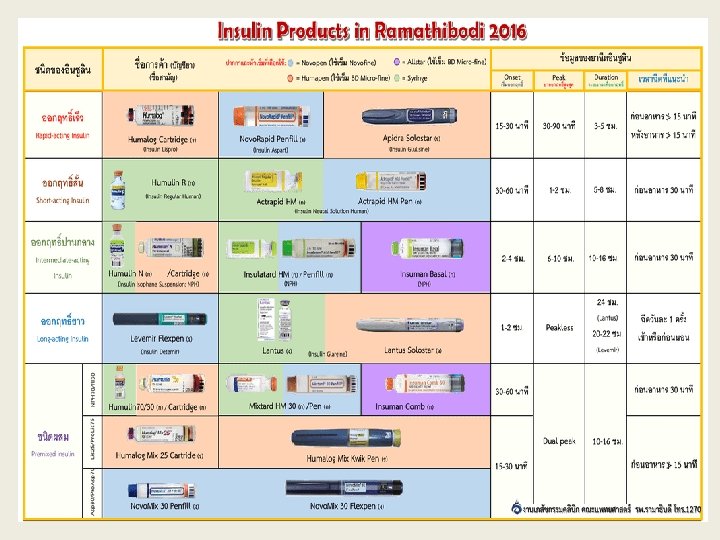

Insulin injection

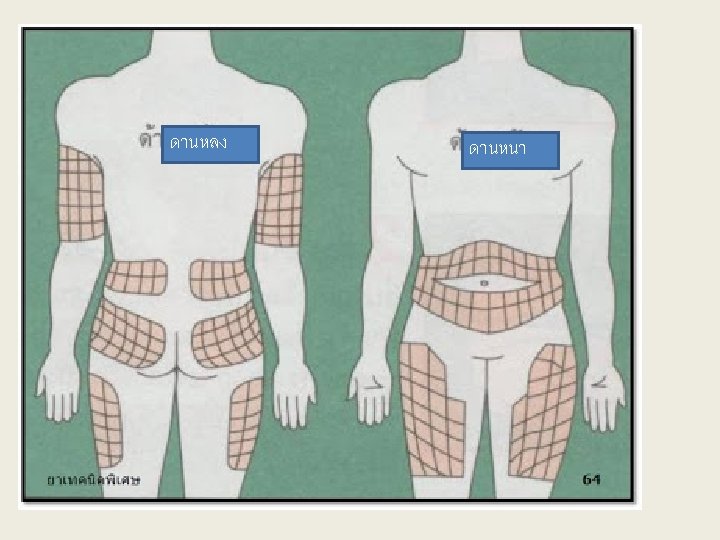
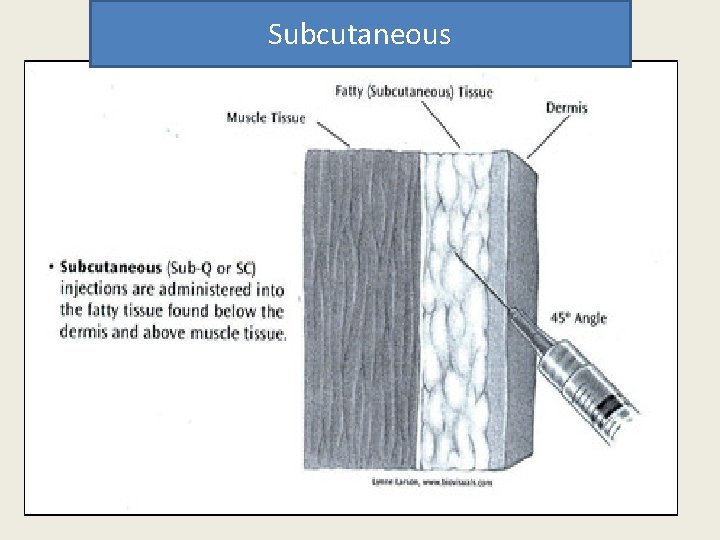
Subcutaneous



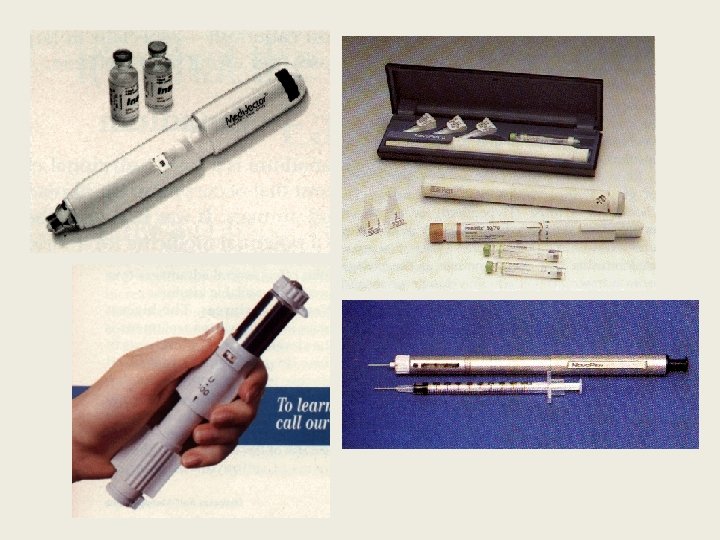
New Technology
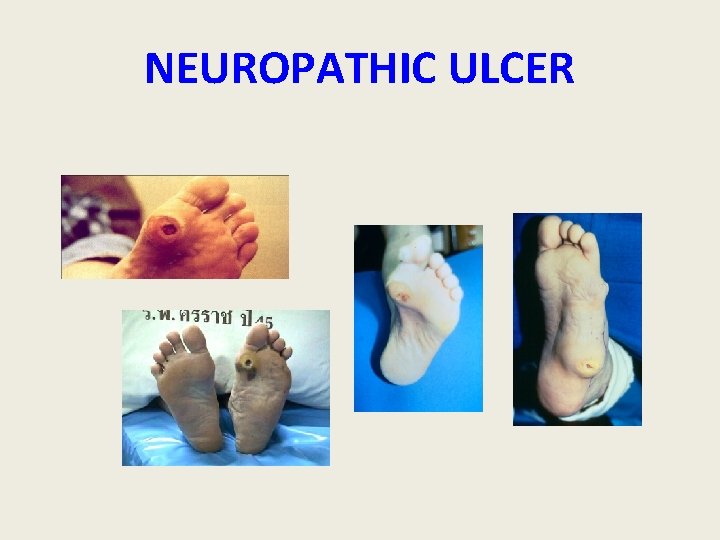
NEUROPATHIC ULCER
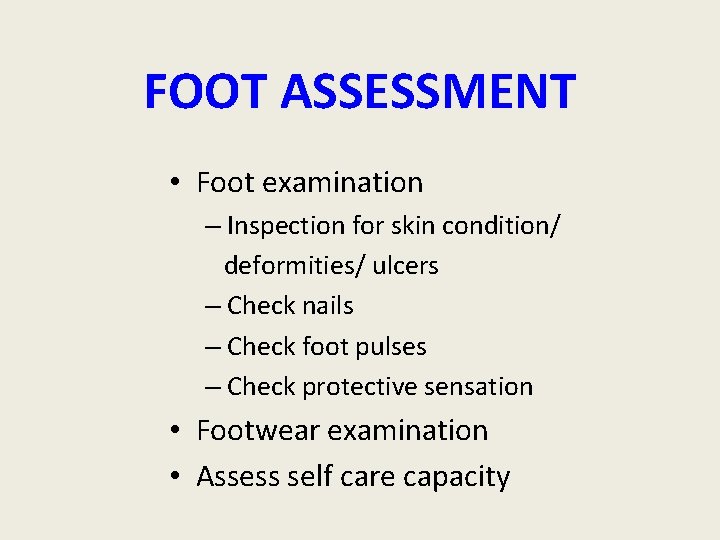
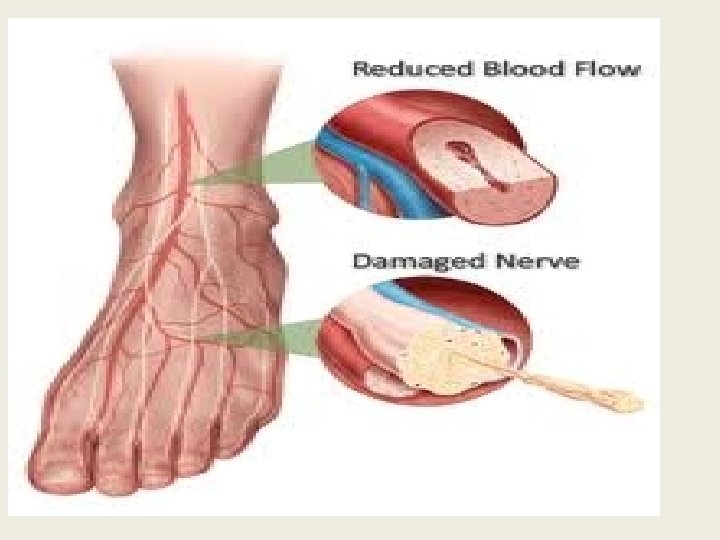
FOOT ASSESSMENT • Foot examination – Inspection for skin condition/ deformities/ ulcers – Check nails – Check foot pulses – Check protective sensation • Footwear examination • Assess self care capacity
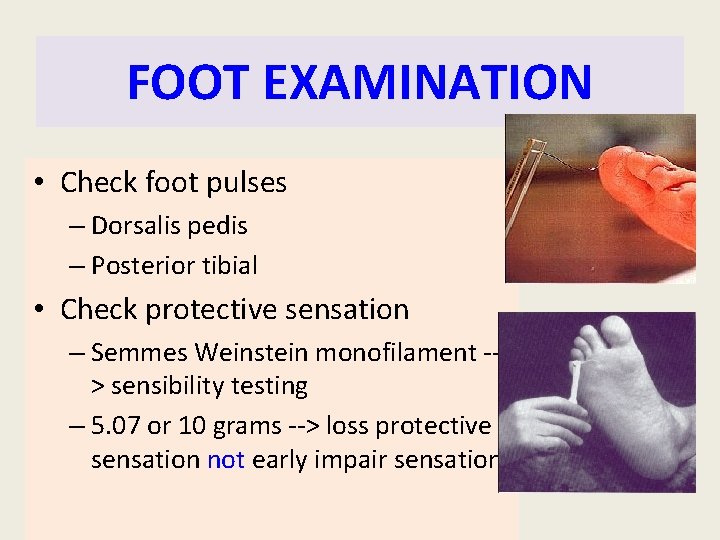
FOOT EXAMINATION • Check foot pulses – Dorsalis pedis – Posterior tibial • Check protective sensation – Semmes Weinstein monofilament -> sensibility testing – 5. 07 or 10 grams --> loss protective sensation not early impair sensation
WOUND CARE • Evaluation • Dressing • Pressure relieve

SHOE MODIFICATION
Hypoglycemia
Hypoglycaemia Definition: • Blood glucose level < 50 mg/dl • Counter- regulatory hormone and symptoms responses to falling glucose levels develop at higher levels, may be detected at blood glucose values between 50 70 mg/dl (3. 5 - 4. 0 mmol/l)
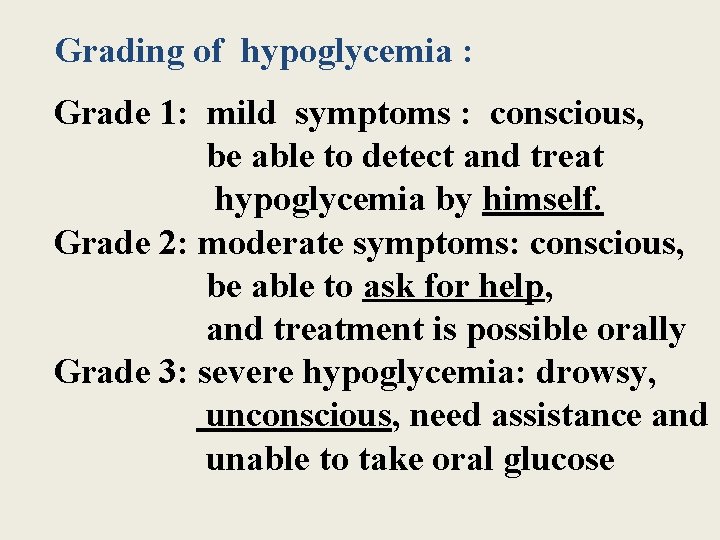
Grading of hypoglycemia : Grade 1: mild symptoms : conscious, be able to detect and treat hypoglycemia by himself. Grade 2: moderate symptoms: conscious, be able to ask for help, and treatment is possible orally Grade 3: severe hypoglycemia: drowsy, unconscious, need assistance and unable to take oral glucose
Causes of Hypoglycemia
Insufficient Food or Delayed Meal or Snack
Too High a Dose of Insulin or Sulphonylurea
Extra Exercise Without Extra Food or Insulin Adjustment
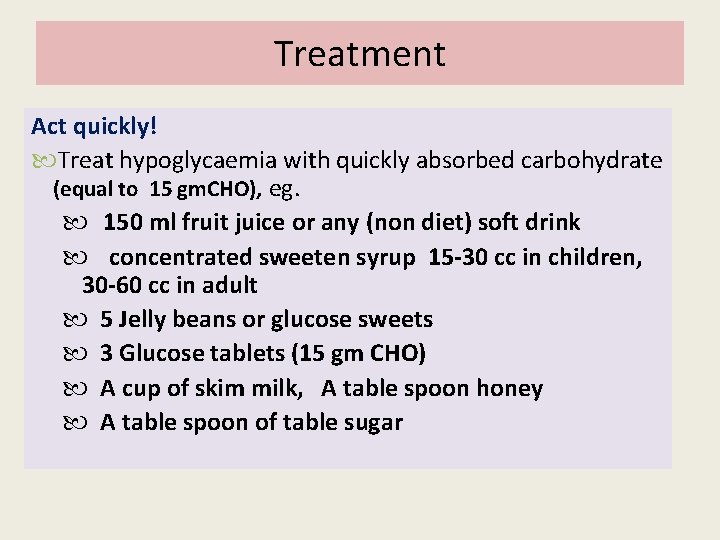
Treatment Act quickly! Treat hypoglycaemia with quickly absorbed carbohydrate (equal to 15 gm. CHO), eg. 150 ml fruit juice or any (non diet) soft drink concentrated sweeten syrup 15 -30 cc in children, 30 -60 cc in adult 5 Jelly beans or glucose sweets 3 Glucose tablets (15 gm CHO) A cup of skim milk, A table spoon honey A table spoon of table sugar
Treatment Check blood glucose level until > 70 mg/dl If symptoms have not resolved in 5 -10 minutes treatment needs to be repeated quickly absorbed C 6 H 12 O 6 . Follow with slowly absorbed carbohydrate eg. A piece of Fruit, rice , bread, noodles ( egual to 1 portion of C 6 H 12 O 6)
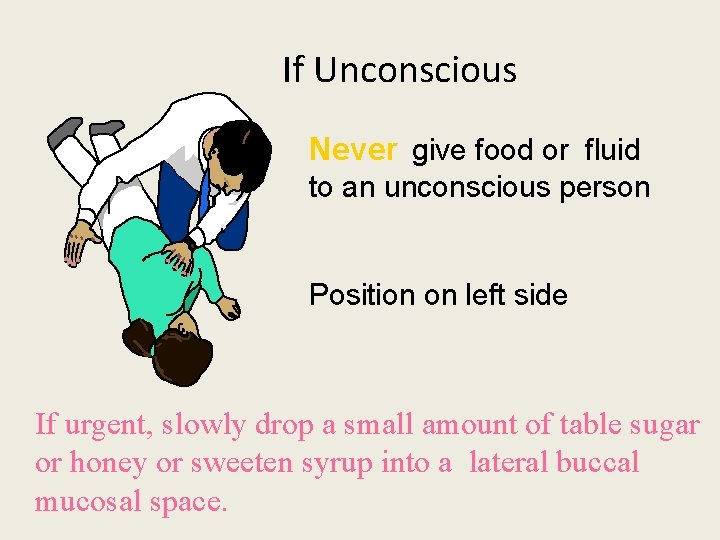
If Unconscious Never give food or fluid to an unconscious person Position on left side If urgent, slowly drop a small amount of table sugar or honey or sweeten syrup into a lateral buccal mucosal space.
Treatment if Unconscious • Intravenous 50% dextrose 50 ml dilute (Doctor) OR • Intramuscular glucagon 0. 5 – 1 mg can be administered subcutaneously, intramuscularly or intravenously OR • • Call an ambulance / take to hospital When conscious give oral carbohydrate Monitor BGL 24 -48 hours Intravenous glucose infusion may be required
Advice to Patients Always carry sweets ( Doraemon bag : contain glucometer, sweets, fruit, crackers, milk, water ) Inform friends, relatives and workmates of symptoms and treatment of hypoglycaemia Carry medical identification If on insulin, eat a bedtime snack Test 2 -3 am if nocturnal hypoglycemia suspected Give patient guidelines to self adjust insulin dose when required
Hyperglycemia
Hyperglycemia • or high blood sugar (also spelled hyperglycaemia is a condition in which an excessive amount of glucose circulates in the blood plasma. • This is generally a blood sugar level higher than 11. 1 mmol/l (200 mg/dl), • but symptoms may not start to become noticeable until even higher values such as 15– 20 mmol/l (~250– 300 mg/dl). • (American Diabetes Association guidelines)
• SIGNS & SYMPTOMS • Polyphagia – frequent hunger, especially pronounced hunger • Polydipsia – frequent thirst, especially excessive thirst • Polyuria – increased volume of urination (not an increased frequency for urination) • Blurred vision • Fatigue • Restlessness Weight loss
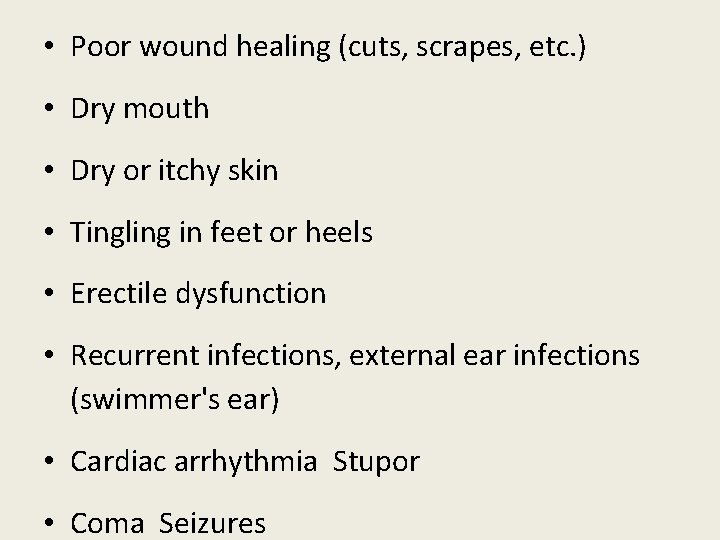
• Poor wound healing (cuts, scrapes, etc. ) • Dry mouth • Dry or itchy skin • Tingling in feet or heels • Erectile dysfunction • Recurrent infections, external ear infections (swimmer's ear) • Cardiac arrhythmia Stupor • Coma Seizures
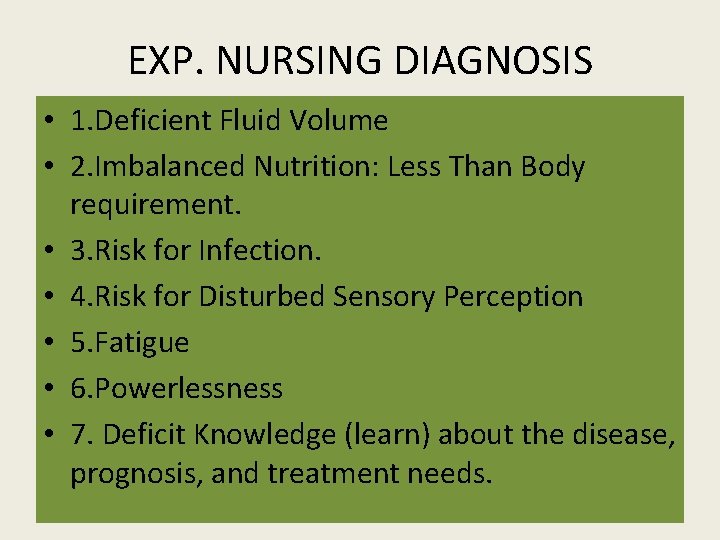
EXP. NURSING DIAGNOSIS • 1. Deficient Fluid Volume • 2. Imbalanced Nutrition: Less Than Body requirement. • 3. Risk for Infection. • 4. Risk for Disturbed Sensory Perception • 5. Fatigue • 6. Powerlessness • 7. Deficit Knowledge (learn) about the disease, prognosis, and treatment needs.
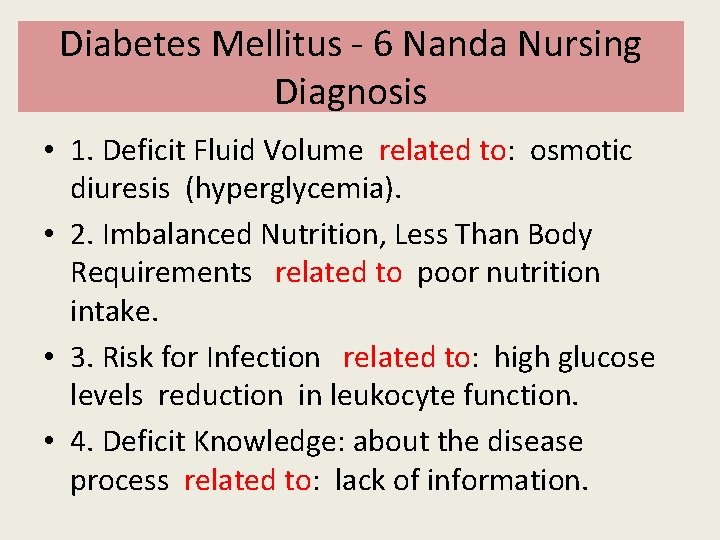
Diabetes Mellitus - 6 Nanda Nursing Diagnosis • 1. Deficit Fluid Volume related to: osmotic diuresis (hyperglycemia). • 2. Imbalanced Nutrition, Less Than Body Requirements related to poor nutrition intake. • 3. Risk for Infection related to: high glucose levels reduction in leukocyte function. • 4. Deficit Knowledge: about the disease process related to: lack of information.
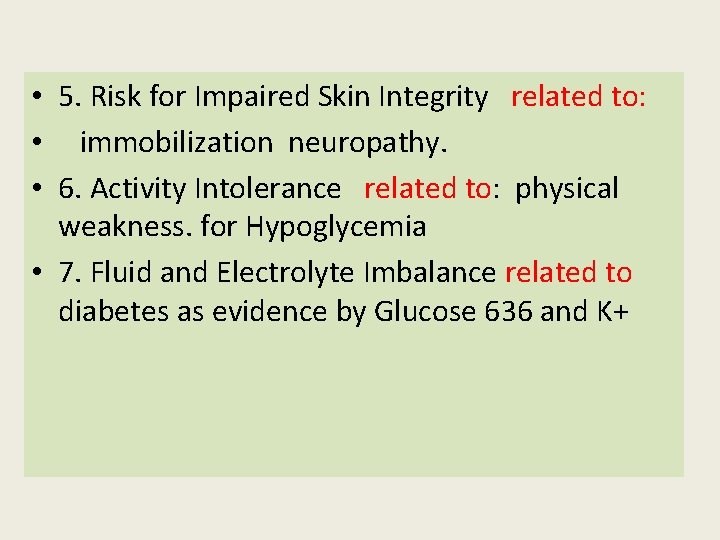
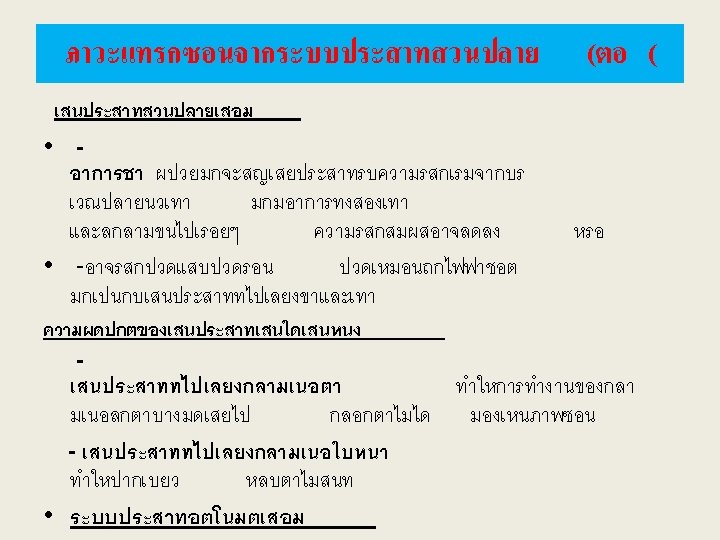
• 5. Risk for Impaired Skin Integrity related to: • immobilization neuropathy. • 6. Activity Intolerance related to: physical weakness. for Hypoglycemia • 7. Fluid and Electrolyte Imbalance related to diabetes as evidence by Glucose 636 and K+
8. Risk for Infection related to: • high glucose levels reduction in leukocyte function. 9. Imbalanced Nutrition, Less Than Body Requirement related to poor nutrition intake. • Check serum glucose before and after meals. • Monitor: glucose, pallor, cold sweat, skin moist. • Monitor vital signs. • Monitor consciousness.
• 1. Risk for complications related to lower plasma glucose levels such as mental disorders, behavioral disorders, autonomic nerve function disorders, hypoglycemic coma Interventions: • Check serum glucose before and after meals. • Monitor: glucose, pallor, cold sweat, skin moist. • Monitor vital signs. • Monitor consciousness. • Monitor sign of nerves, irritability.
• Monitor sign of nerves, irritability. • Perform oral administration of sweet milk 20 cc X 12. • Analysis of environmental conditions that could potentially cause hypoglycemia. • Weight checks every day. • Check for signs of infection. • Avoid the occurrence of hypothermia. • Collaborate provision of oxygenation.
A&Q
- Slides: 109