Complex Wounds By Mark Vance RN WCC 2017
Complex Wounds By Mark Vance RN WCC 2017
Managing Complex Wounds Managing complex wound requires multifaceted approach which includes following: 1. 2. 3. 4. Assessment Building plan Choosing product Meeting patient needs and wants
Assessment Baseline assessment includes: 1. Age 2. Mobility and activity 3. Presence of pain 4. Presence or absence of sensory deficits. 5. Nutrition and hydration status. 6. Circulation and tissue oxygenation status. 7. Signs and symptoms of infection or history of infection. 8. Continence status.
Assessment Continued 9. 10. 11. 12. 13. 14. 15. 16. 17. 18. DME in place Comorbidities Medication Profile History of previous wounds/ulcers Measurements Staging, as appropriate Exudate/Drainage Location Wound bed Peri-wound (color, edema, maceration and induration

Understanding Wound Bed 1. 2. 3. 4. Viable tissues a. Epithelial (pale pink to shiny white) b. Granulation(Beefy red and bumpy; sub optimal may be smooth) Non-viable tissues. a. Eschar ( brown or black and thick leathery) b. Slough (adherent or non-adherent and yellow, gray, brown or green) c. Necrotic (soft black or gray tissue) Foreign bodies: Maggots, sutures, wood or metal, and dressing remnants. Underlying structures: ligaments, tendons, muscle or bone.
Types Of Complex Wounds 1. 2. 3. 4. 5. 6. Stage 3 pressure ulcers. Stage 4 pressure ulcers. Malignant cutaneous wounds. Fistulas. Venous stasis ulcers. Diabetic foot ulcers.
Stage 3 Pressure Ulcer 1. 2. 3. 4. Full thickness tissue loss involving epidermis, dermis and into but not through subcutaneous fat. Slough may be present but does not obscure the depth of tissue loss. May include undermining and tunneling The depth can vary depending on location.
Stage 4 Pressure Ulcer 1. 2. 3. Full thickness tissue loss involving epidermis, subcutaneous fat with exposed bone, tendon or muscle that is visible or directly palpable. Slough or eschar may be present. Often includes undermining and tunneling. Depth can vary depending on location and patient condition.
Malignant Cutaneous Wounds �A cancerous lesion involving the skin, which is open and may be draining. The lesion may be a result of a primary cancer, or a metastasis to the skin from a local tumor in a distant site. It may take the form of a cavity, an open area on the surface of the skin, skin nodules, or a nodular growth extending from the surface of the skin. ”
Fistulas �A fistula is an abnormal connection between two hollow spaces (technically, two epithelized surfaces), such as Blood vessels, intestines , or other hollow organs. Fistulas are usually caused by injury or surgery, but they can also result from an infection or inflammation. Fistulas are generally a disease condition, but they may be surgically created for therapeutic reasons.
Building Plan For Treatment 1. 2. 3. 4. 5. 6. What does patient want? Aggressive vs. simple care. Managing pain Controlling odor Protect peri-wound Control and prevent bleeding Collect and contain exudate
Patient Wants 1. 2. 3. Build trust and report with patient. Understand impact of wound to patient. Negotiate treatment plan.
Managing Pain Nonpharmacologic control 1. 2. 3. 4. 5. Wound cleansing Peri-wound skin care Debridement Support and positioning Wound dressings
Managing Pain Pharmacologic Interventions World Health Organization Analgesic Ladder 1. Step 1: Patients with mild to moderate pain should be treated with a non-opioid analgesic. 2. Step 2 : Patients who have limited opioid exposure and moderate to severe pain or who fail to achieve adequate relief after a trail of a nonopioid analgesic should be treated with an opioid conventionally used for moderate pain.
Managing Pain Continued 3. Step 3: Patients who have severe pain or who fail to achieve adequate relief after appropriate administration of drugs in step 2 of the analgesic ladder should receive an opioid conventionally used for severe pain.
Managing Pain Continued Topical Management: These medications are typically used prior to wound debridement. They can also be used with dressing changes carefully, but need have risk for systemic absorption. Typical options are: 1. Lidocaine 2. EMLA
Controlling Odor 1. 2. 3. 4. Wound cleansing, removing exudate and debris with wound cleansers can be more effective for cleaning and bacterial management Topical deodorizers such has Manuka honey, Dakin's solution and other silver products can be helpful. Room deodorizers , aromatherapy oils, scented candles can help with environment. Debriding slough and eschar will also help.
Protecting Peri-wound 1. 2. 3. Use of skin sealant pads or sprays to periwound can help prevent breakdown from tape shearing and exudate maceration. Use of lotions to surrounding are also helpful. If You have maceration use of stoma powder and skin sealants can help heal macerated tissues.
Control or Prevent Bleeding Erosion of capillaries can lead to bleeding. Atraumatic dressing removal is essential to prevent bleeding. 1. Use of petroleum or silicone dressing can help very fragile wound beds. 2. If bleeding persists during wound care then use of silver nitrate can help to stop and control bleeding.
Collecting and Managing Drainage 1. For highly exudative wounds there are products that can help to collect drainage. a. Examples are; ABD pads, exudry, xtrasorb, calcium alginate, hydrofiber. b. Several types of wound drainage pouches that are available from ostomy supply companies. c. Negative pressure wound therapy should be used sparingly. ( not always reimbursed with palliative patients) 2. Dressing change frequency can help to determine which product to chose. Finding product that can reduce dressing change frequency to daily is preferred.
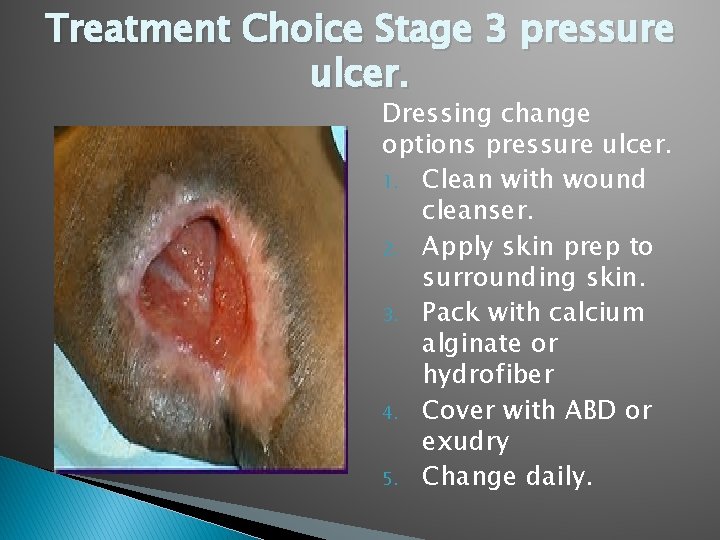
Treatment Choice Stage 3 pressure ulcer. Dressing change options pressure ulcer. 1. Clean with wound cleanser. 2. Apply skin prep to surrounding skin. 3. Pack with calcium alginate or hydrofiber 4. Cover with ABD or exudry 5. Change daily.
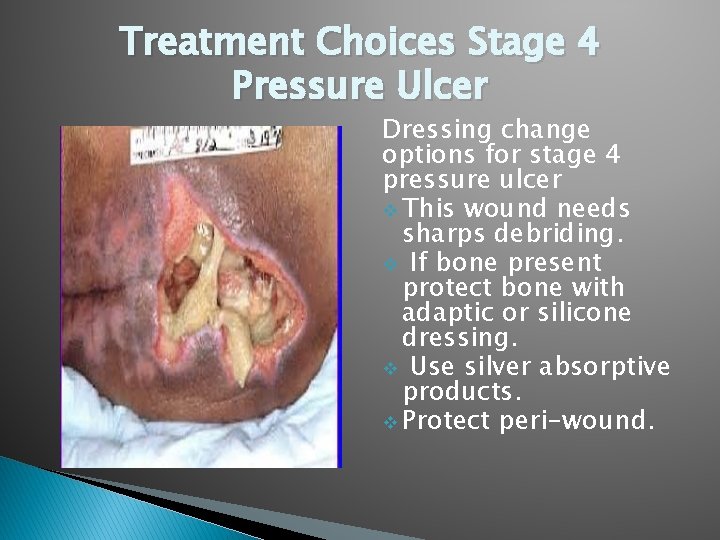
Treatment Choices Stage 4 Pressure Ulcer Dressing change options for stage 4 pressure ulcer v This wound needs sharps debriding. v If bone present protect bone with adaptic or silicone dressing. v Use silver absorptive products. v Protect peri-wound.
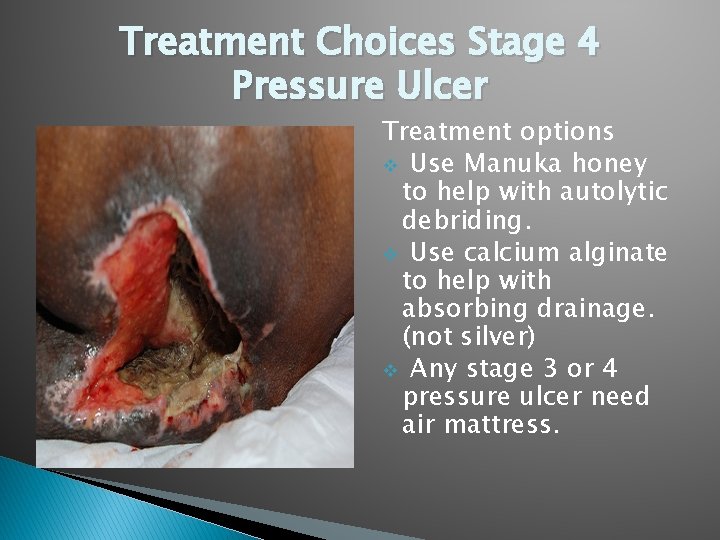
Treatment Choices Stage 4 Pressure Ulcer Treatment options v Use Manuka honey to help with autolytic debriding. v Use calcium alginate to help with absorbing drainage. (not silver) v Any stage 3 or 4 pressure ulcer need air mattress.
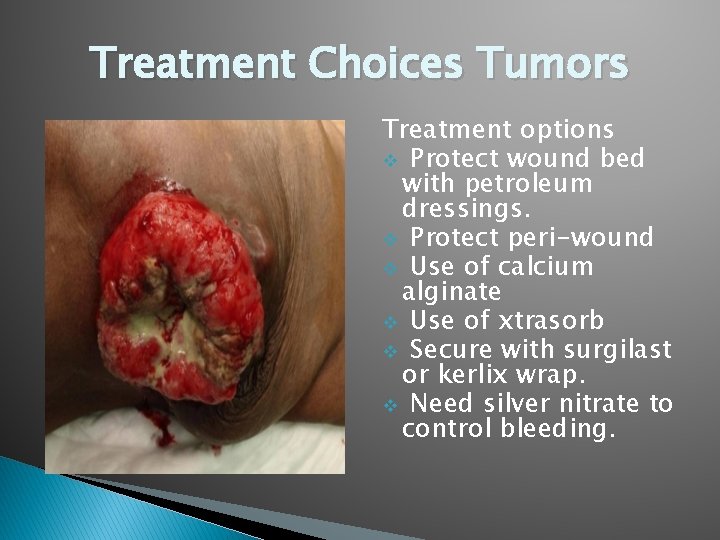
Treatment Choices Tumors Treatment options v Protect wound bed with petroleum dressings. v Protect peri-wound v Use of calcium alginate v Use of xtrasorb v Secure with surgilast or kerlix wrap. v Need silver nitrate to control bleeding.
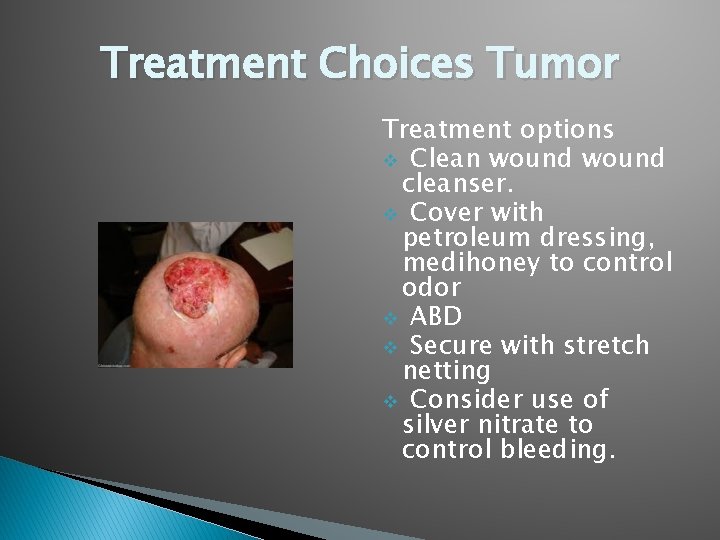
Treatment Choices Tumor Treatment options v Clean wound cleanser. v Cover with petroleum dressing, medihoney to control odor v ABD v Secure with stretch netting v Consider use of silver nitrate to control bleeding.

Treatment Choices Fistulas Keep surrounding skin protected, with skin prep and stoma powder. v Use Wound pouch to cover and contain drainage. v
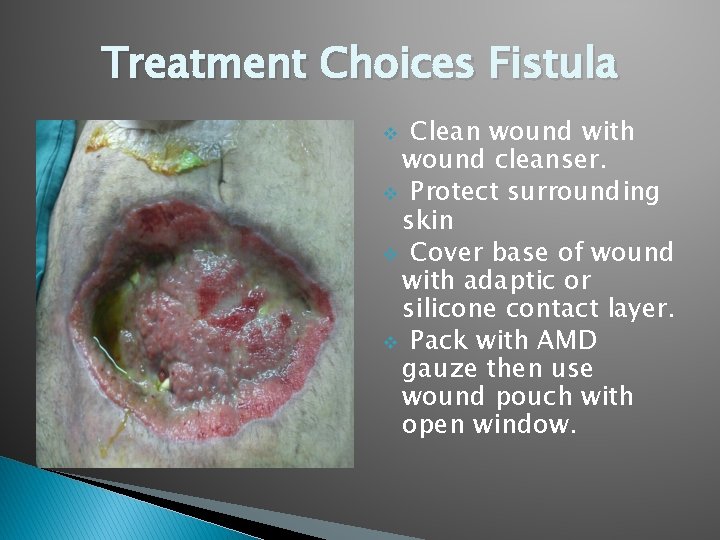
Treatment Choices Fistula Clean wound with wound cleanser. v Protect surrounding skin v Cover base of wound with adaptic or silicone contact layer. v Pack with AMD gauze then use wound pouch with open window. v

Wound Pouches
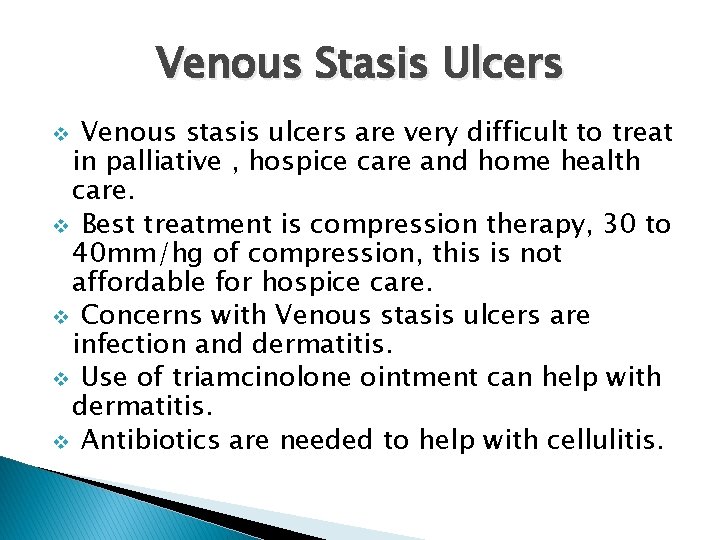
Venous Stasis Ulcers Venous stasis ulcers are very difficult to treat in palliative , hospice care and home health care. v Best treatment is compression therapy, 30 to 40 mm/hg of compression, this is not affordable for hospice care. v Concerns with Venous stasis ulcers are infection and dermatitis. v Use of triamcinolone ointment can help with dermatitis. v Antibiotics are needed to help with cellulitis. v
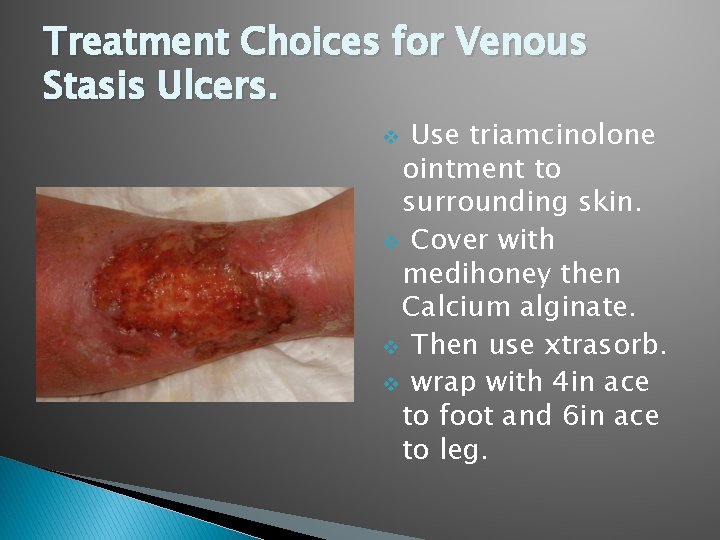
Treatment Choices for Venous Stasis Ulcers. Use triamcinolone ointment to surrounding skin. v Cover with medihoney then Calcium alginate. v Then use xtrasorb. v wrap with 4 in ace to foot and 6 in ace to leg. v
Diabetic Foot Ulcers Best treatment for diabetic foot ulcers is pressure relief. v Treatment choices depend of location of wound, size and depth of wound. v Diabetic foot ulcers are caused by poorly fitting shoes or injury from going shoe less. v Also very difficult and can be costly to treat. v
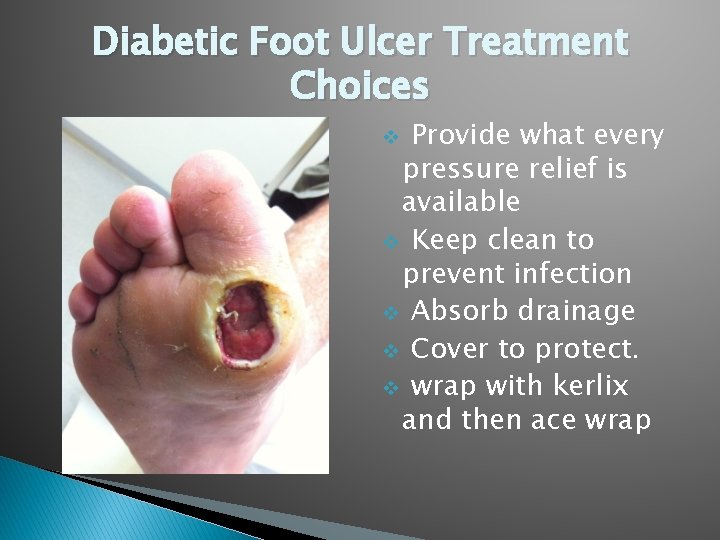
Diabetic Foot Ulcer Treatment Choices Provide what every pressure relief is available v Keep clean to prevent infection v Absorb drainage v Cover to protect. v wrap with kerlix and then ace wrap v
Conclusion These treatment options are only suggestions, other treatments may be just as effective. v If not sure how to use products read you package inserts or look up on line. v Are there any questions? v Thank you for this opprotunity. v
- Slides: 33