Complex PTSD Complex Dissociation and Incest Disorders Associated

- Slides: 31
Complex PTSD, Complex Dissociation, and Incest
Disorders Associated with Traumatic Stress �Attachment Disorders �Acute Stress Disorder �PTSD and Chronic PTSD (not a diagnoses) �Borderline Personality Disorder �Complex PTSD or c. PTSD �Dissociative Disorders �Somatic and Conversion Disorders
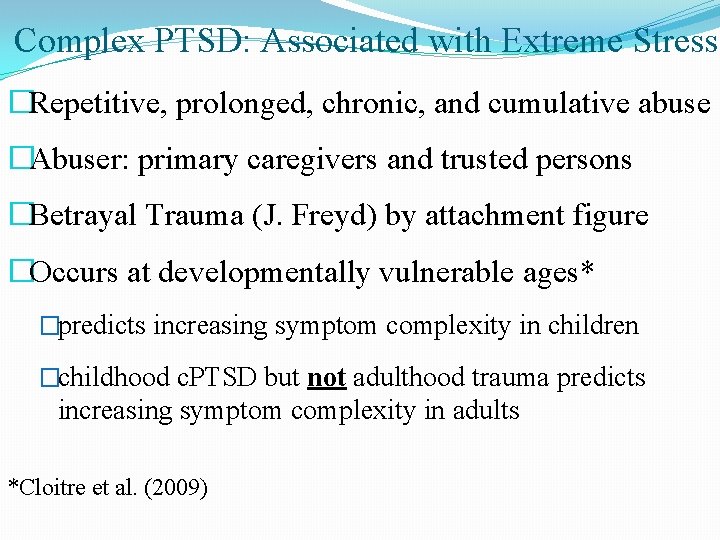
Complex PTSD: Associated with Extreme Stress �Repetitive, prolonged, chronic, and cumulative abuse �Abuser: primary caregivers and trusted persons �Betrayal Trauma (J. Freyd) by attachment figure �Occurs at developmentally vulnerable ages* �predicts increasing symptom complexity in children �childhood c. PTSD but not adulthood trauma predicts increasing symptom complexity in adults *Cloitre et al. (2009)
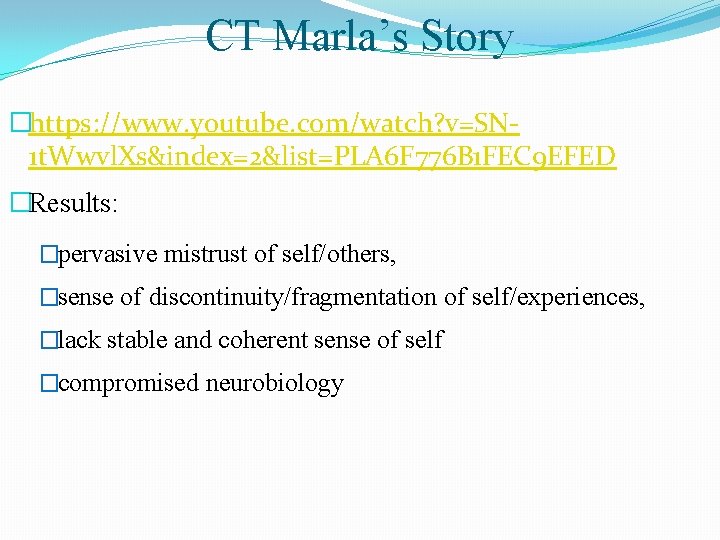
CT Marla’s Story �https: //www. youtube. com/watch? v=SN 1 t. Wwvl. Xs&index=2&list=PLA 6 F 776 B 1 FEC 9 EFED �Results: �pervasive mistrust of self/others, �sense of discontinuity/fragmentation of self/experiences, �lack stable and coherent sense of self �compromised neurobiology
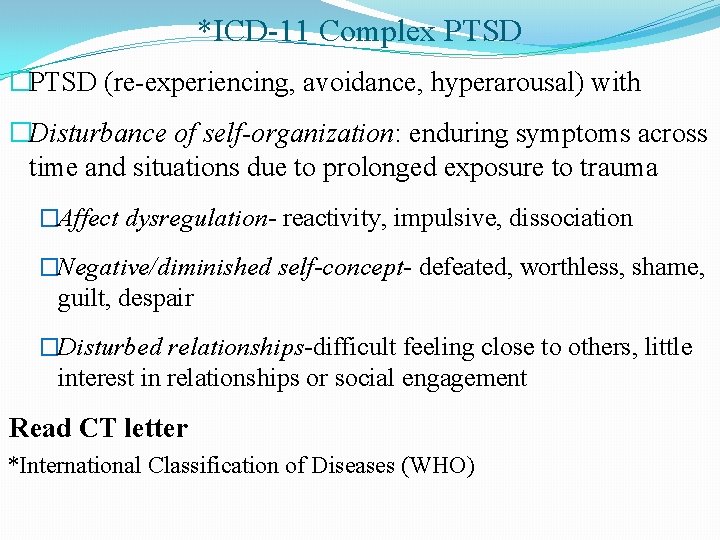
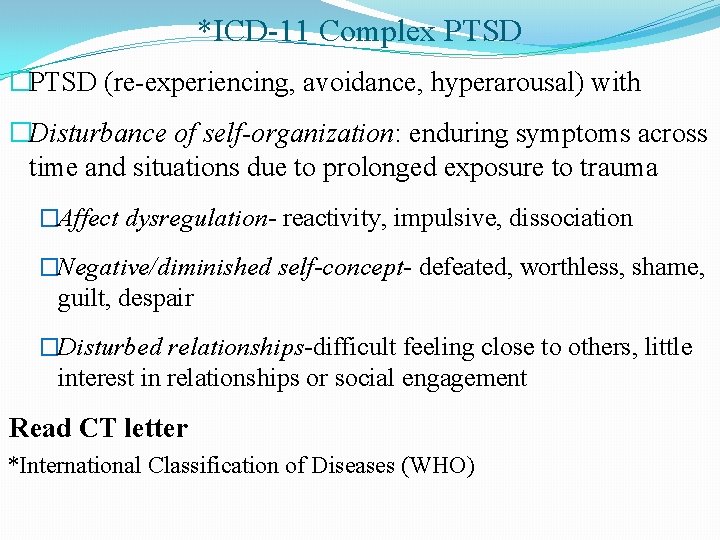
*ICD-11 Complex PTSD �PTSD (re-experiencing, avoidance, hyperarousal) with �Disturbance of self-organization: enduring symptoms across time and situations due to prolonged exposure to trauma �Affect dysregulation- reactivity, impulsive, dissociation �Negative/diminished self-concept- defeated, worthless, shame, guilt, despair �Disturbed relationships-difficult feeling close to others, little interest in relationships or social engagement Read CT letter *International Classification of Diseases (WHO)
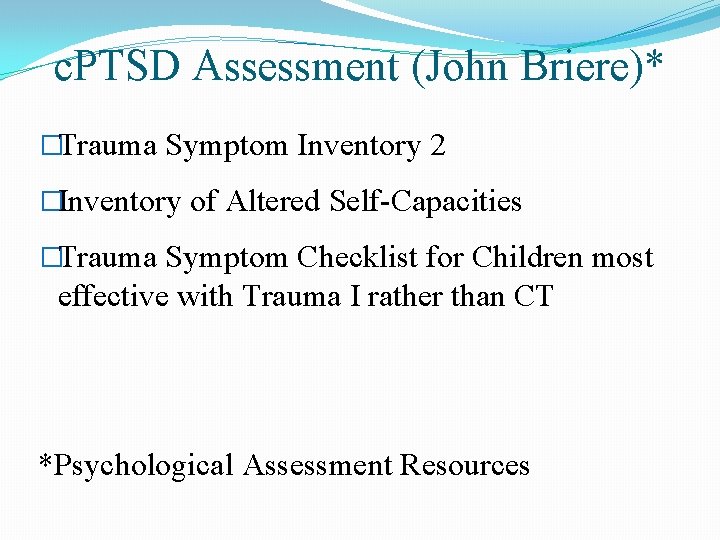
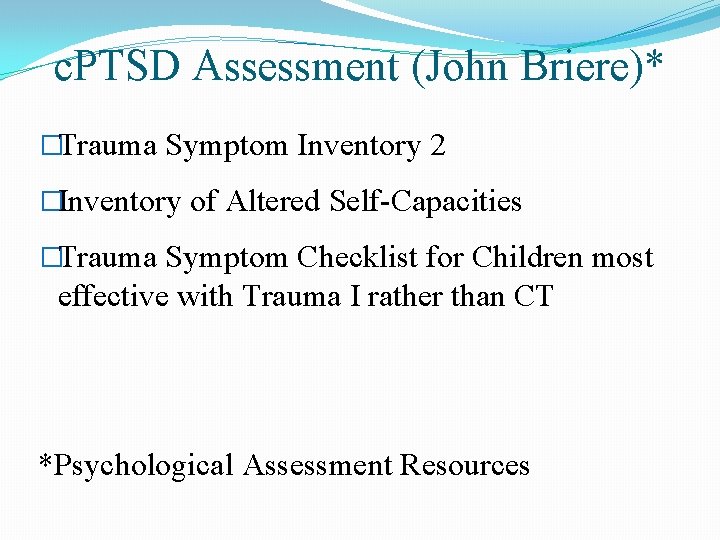
c. PTSD Assessment (John Briere)* �Trauma Symptom Inventory 2 �Inventory of Altered Self-Capacities �Trauma Symptom Checklist for Children most effective with Trauma I rather than CT *Psychological Assessment Resources
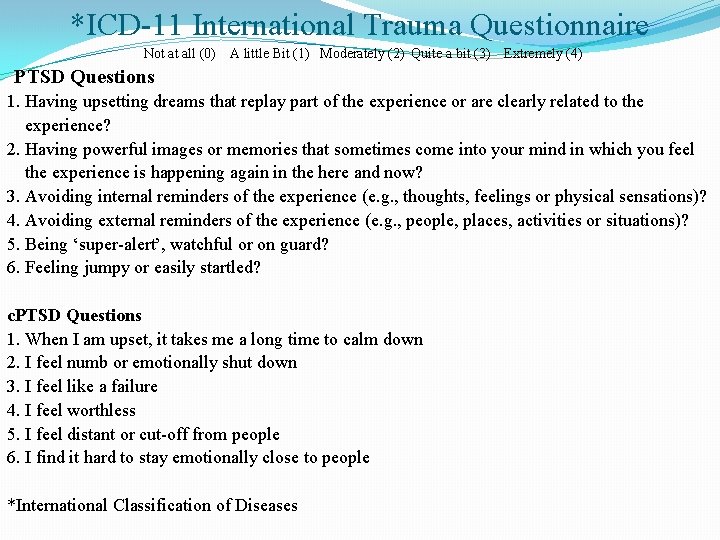
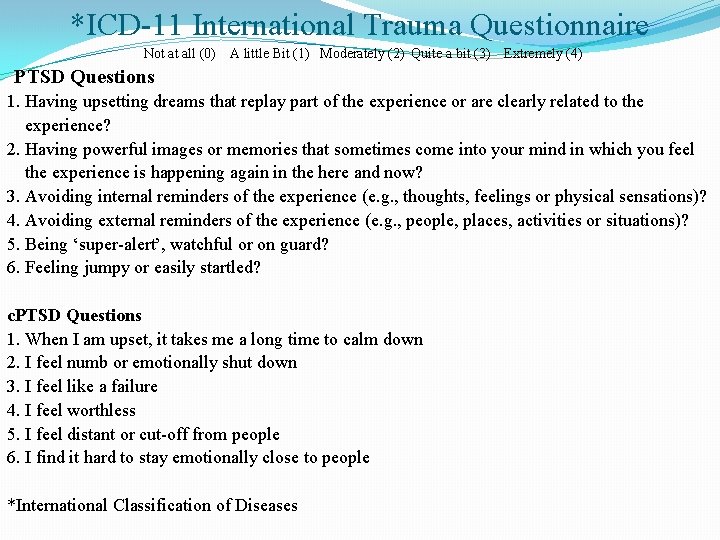
*ICD-11 International Trauma Questionnaire Not at all (0) A little Bit (1) Moderately (2) Quite a bit (3) Extremely (4) PTSD Questions 1. Having upsetting dreams that replay part of the experience or are clearly related to the experience? 2. Having powerful images or memories that sometimes come into your mind in which you feel the experience is happening again in the here and now? 3. Avoiding internal reminders of the experience (e. g. , thoughts, feelings or physical sensations)? 4. Avoiding external reminders of the experience (e. g. , people, places, activities or situations)? 5. Being ‘super-alert’, watchful or on guard? 6. Feeling jumpy or easily startled? c. PTSD Questions 1. When I am upset, it takes me a long time to calm down 2. I feel numb or emotionally shut down 3. I feel like a failure 4. I feel worthless 5. I feel distant or cut-off from people 6. I find it hard to stay emotionally close to people *International Classification of Diseases
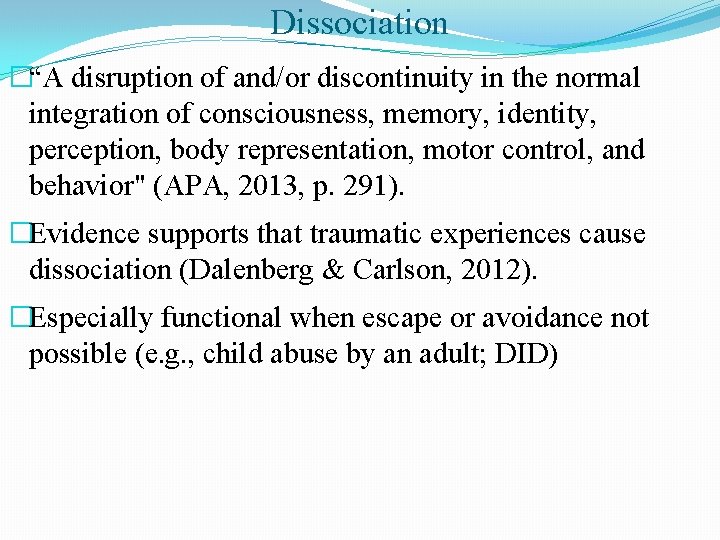
Dissociation �“A disruption of and/or discontinuity in the normal integration of consciousness, memory, identity, perception, body representation, motor control, and behavior" (APA, 2013, p. 291). �Evidence supports that traumatic experiences cause dissociation (Dalenberg & Carlson, 2012). �Especially functional when escape or avoidance not possible (e. g. , child abuse by an adult; DID)
Dissociative Disorders (DD) �Depersonalization/derealization �most prevalent DD (APA, 2013); � 2% lifetime prevalence rate �associated with childhood trauma �often reduced by enhancing emotion regulation skills �Dissociative Amnesia: inability to recall important autobiographical information that is inconsistent with ordinary forgetting (1. 8%, 12 -month prevalence rate).
Dissociative Identity Disorder �“Two or more personality states involving marked discontinuity in sense of self, sense of agency, and alternations in affect, behavior, consciousness, memory, perception, cognition, and sensory-motor functioning” (APA, 2013). �Recurrent gaps in memory and amnesia between parts �Other Specified Dissociative Disorders (OSDD) #1: less marked discontinuities in sense of self and agency, or alterations of identity
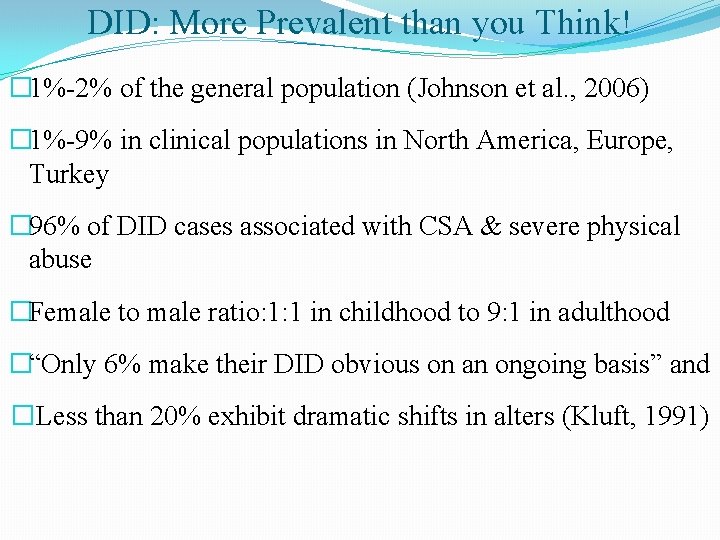
DID: More Prevalent than you Think! � 1%-2% of the general population (Johnson et al. , 2006) � 1%-9% in clinical populations in North America, Europe, Turkey � 96% of DID cases associated with CSA & severe physical abuse �Female to male ratio: 1: 1 in childhood to 9: 1 in adulthood �“Only 6% make their DID obvious on an ongoing basis” and �Less than 20% exhibit dramatic shifts in alters (Kluft, 1991)

DID with Visual Impairment https: //www. bing. com/videos/search? q=richard+kluft+disso ciative+identity+disorder&&view=detail&mid=2594212099 F 335 A 7969 C 2594212099 F 335 A 7969 C&&FORM=VDRVR V Start 1 min 15 sec
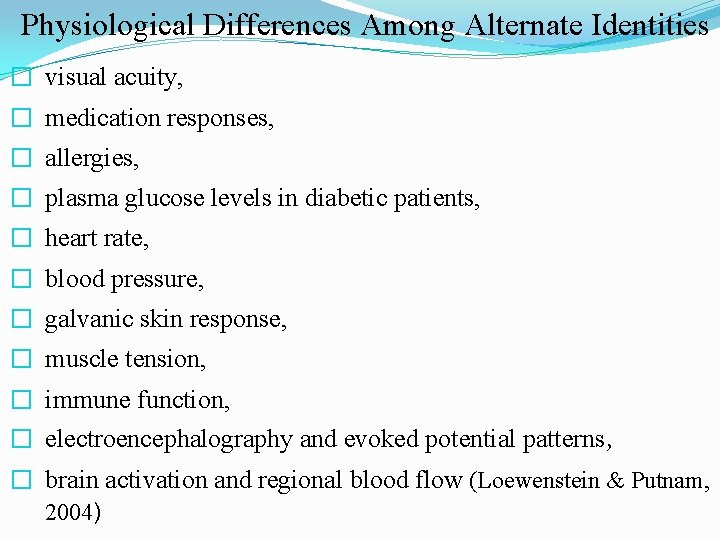
Physiological Differences Among Alternate Identities � visual acuity, � medication responses, � allergies, � plasma glucose levels in diabetic patients, � heart rate, � blood pressure, � galvanic skin response, � muscle tension, � immune function, � electroencephalography and evoked potential patterns, � brain activation and regional blood flow (Loewenstein & Putnam, 2004)
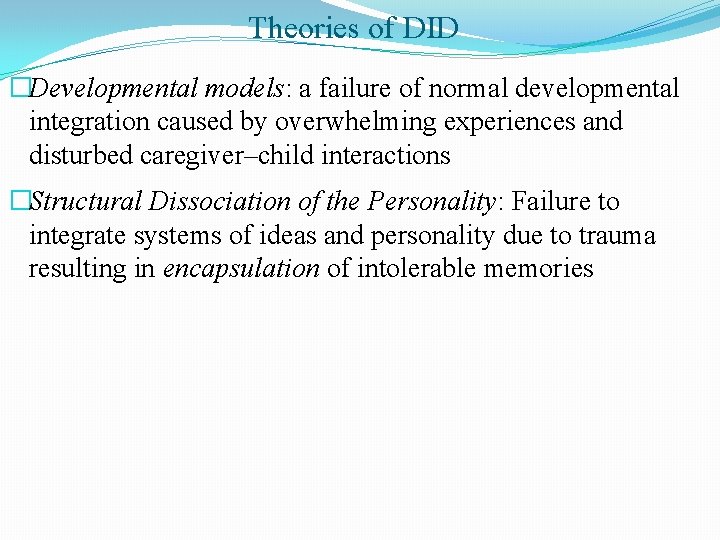
Theories of DID �Developmental models: a failure of normal developmental integration caused by overwhelming experiences and disturbed caregiver–child interactions �Structural Dissociation of the Personality: Failure to integrate systems of ideas and personality due to trauma resulting in encapsulation of intolerable memories
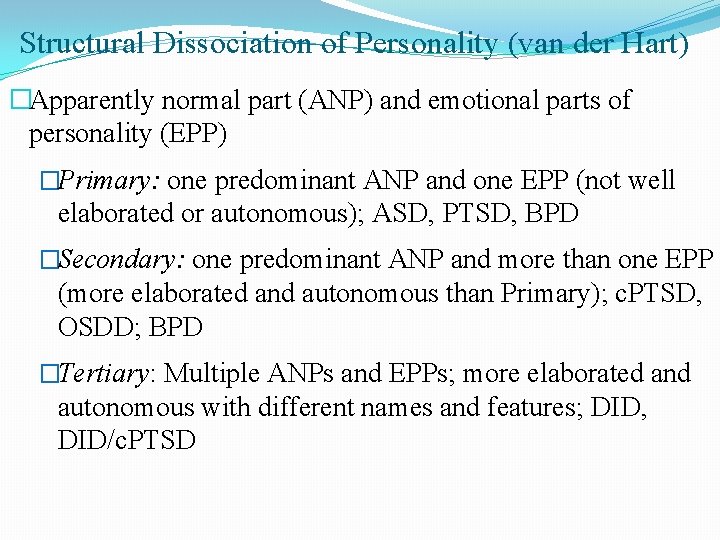
Structural Dissociation of Personality (van der Hart) �Apparently normal part (ANP) and emotional parts of personality (EPP) �Primary: one predominant ANP and one EPP (not well elaborated or autonomous); ASD, PTSD, BPD �Secondary: one predominant ANP and more than one EPP (more elaborated and autonomous than Primary); c. PTSD, OSDD; BPD �Tertiary: Multiple ANPs and EPPs; more elaborated and autonomous with different names and features; DID, DID/c. PTSD
Clinical Impact of DID �Can disrupt or prevent formation of therapeutic alliance �Client’s changing perceptions of therapist and environment �Higher alliance associated with less dissociative symptoms (Cronin et al. ). �Solves a problem, conscious absence during abuse, but creates a long-term problem, fragmented sense of self �Underdiagnosed due to skepticism and lack of training �Often takes years in treatment before getting an accurate diagnoses
Include in Intake Interviews � History of physical/sexual abuse or other maltreatment � Gaps in memory/loosing time/amnesia � Hearing voices � Imaginary companions � Trance states
Differential Diagnosis � DID vs BPD- less volatile emotions; amnesia between emotion states; less identity confusion; BDP recall shifts across emotional states � DID vs Psychotic disorder- DID voices begin in childhood, child and adult voices, parts have a sense of self, passive control. � Bi-polar disorder: lacks memory deficits and distinctive parts � Ego states are normal phenomena without autonomy; maintain a shared sense of belonging
Recognizing Dissociative Parts �Sense of fragmentation, division of self, involuntariness, “not me” �You hear yourself talking, but it seems as though the thoughts or words you hear are not your own and you have no control over it. �Amnesia- Swiss cheese memory, blanks, foggy, time loss �You discover that something has been done that only you could have done, yet you have no memory of it. �Depersonalization/derealization �You experience yourself outside your body and/or your perceptions of the environment looks different, distorted, unreal, surrealistic �You have body sensations/movements that seem to be other controlled (passive influence)
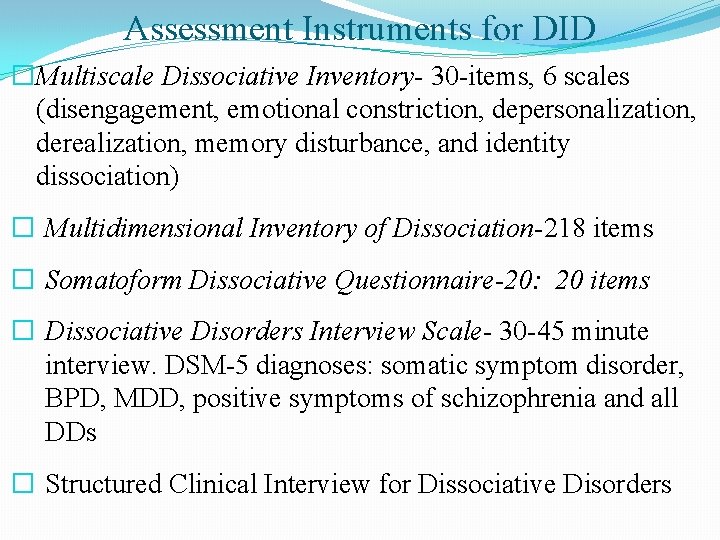
Assessment Instruments for DID �Multiscale Dissociative Inventory- 30 -items, 6 scales (disengagement, emotional constriction, depersonalization, derealization, memory disturbance, and identity dissociation) � Multidimensional Inventory of Dissociation-218 items � Somatoform Dissociative Questionnaire-20: 20 items � Dissociative Disorders Interview Scale- 30 -45 minute interview. DSM-5 diagnoses: somatic symptom disorder, BPD, MDD, positive symptoms of schizophrenia and all DDs � Structured Clinical Interview for Dissociative Disorders
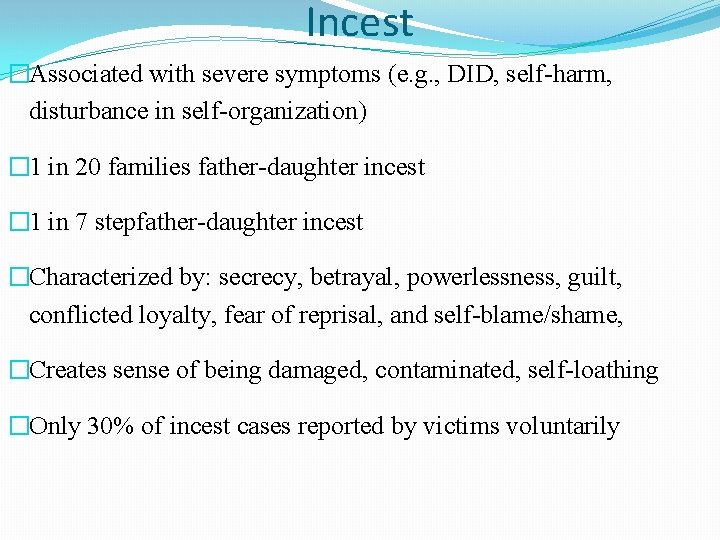
Incest �Associated with severe symptoms (e. g. , DID, self-harm, disturbance in self-organization) � 1 in 20 families father-daughter incest � 1 in 7 stepfather-daughter incest �Characterized by: secrecy, betrayal, powerlessness, guilt, conflicted loyalty, fear of reprisal, and self-blame/shame, �Creates sense of being damaged, contaminated, self-loathing �Only 30% of incest cases reported by victims voluntarily
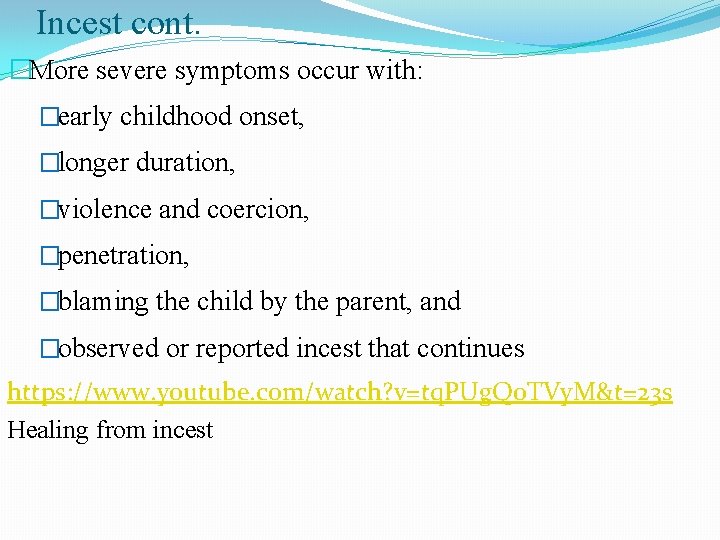
Incest cont. �More severe symptoms occur with: �early childhood onset, �longer duration, �violence and coercion, �penetration, �blaming the child by the parent, and �observed or reported incest that continues https: //www. youtube. com/watch? v=tq. PUg. Qo. TVy. M&t=23 s Healing from incest
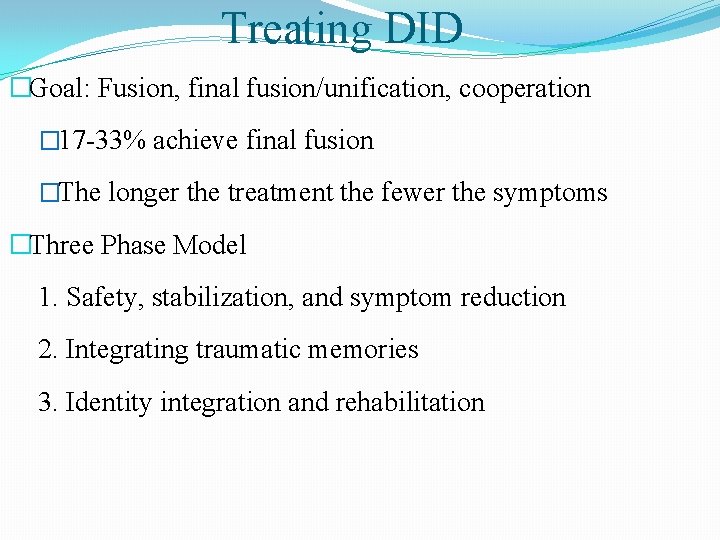
Treating DID �Goal: Fusion, final fusion/unification, cooperation � 17 -33% achieve final fusion �The longer the treatment the fewer the symptoms �Three Phase Model 1. Safety, stabilization, and symptom reduction 2. Integrating traumatic memories 3. Identity integration and rehabilitation
1. Establish Safety, Stabilization, and Symptom Reduction �Safety self-mgmt and agreements (Seeking Safety- Najavits) �Emotion Regulation skill building (TF-CBT, Sk. Trn. Af. Int. Re) �grounding (awareness through senses) �mindfulness breathing and/or �progressive muscle relaxation �mindfulness �cognitive interventions
Phase I cont �present-ness and self-reflective �trust �therapeutic alliance �Polyvagal Theory (Stephen Porges) �But, no improvement without direct work with alters and amnesia
Working with Alters prior to Memory Work �Client must accept, value, and be able to access their alters �Practice- Daily inward focus, awareness, and listening to parts �Denial of parts prolongs symptoms and DID �Practice- Daily talking to parts, writing to parts, inner meetings �Encourage negotiation between the alters to resolve differences �Establish commitments by all identities for safety from self-harm and/or suicidal behaviors. �Practice- Create safe, calm place in client’s mind and �in external world for client
Preparation for Trauma Memory Work �Determine: �Which procedures will be used to contain traumatic memories (e. g. , put some alters to sleep or safe place) �Which memories will be focal, �Which alternate identities will participate, �What steps will be taken to maintain safety �At what level of intensity they will be processed, �Is client stable enough to begin memory work?
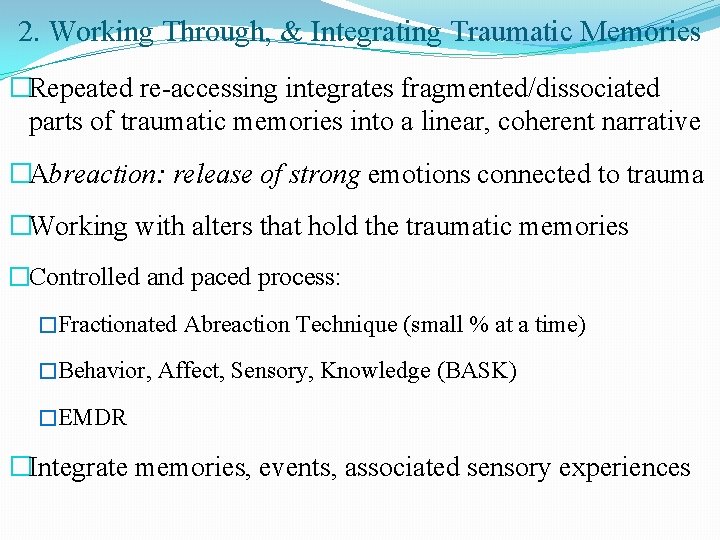
2. Working Through, & Integrating Traumatic Memories �Repeated re-accessing integrates fragmented/dissociated parts of traumatic memories into a linear, coherent narrative �Abreaction: release of strong emotions connected to trauma �Working with alters that hold the traumatic memories �Controlled and paced process: �Fractionated Abreaction Technique (small % at a time) �Behavior, Affect, Sensory, Knowledge (BASK) �EMDR �Integrate memories, events, associated sensory experiences
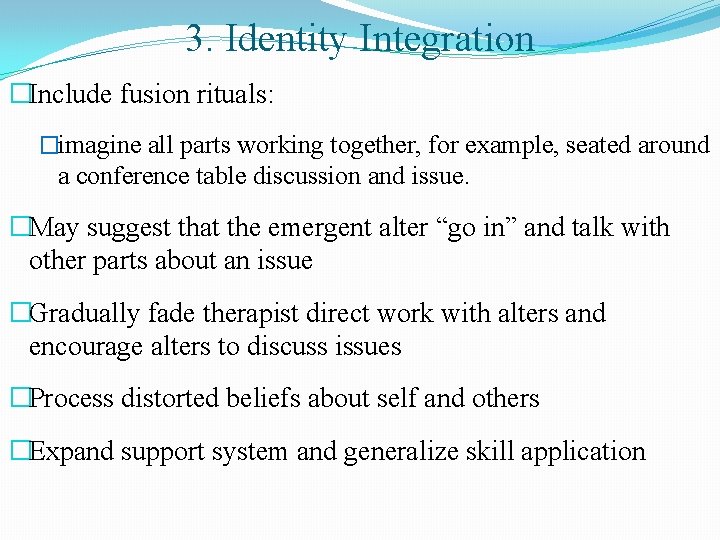
3. Identity Integration �Include fusion rituals: �imagine all parts working together, for example, seated around a conference table discussion and issue. �May suggest that the emergent alter “go in” and talk with other parts about an issue �Gradually fade therapist direct work with alters and encourage alters to discuss issues �Process distorted beliefs about self and others �Expand support system and generalize skill application
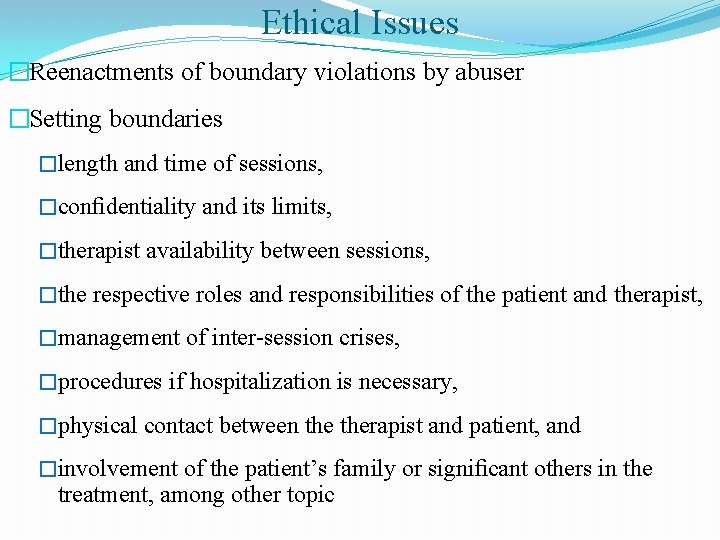
Ethical Issues �Reenactments of boundary violations by abuser �Setting boundaries �length and time of sessions, �confidentiality and its limits, �therapist availability between sessions, �the respective roles and responsibilities of the patient and therapist, �management of inter-session crises, �procedures if hospitalization is necessary, �physical contact between therapist and patient, and �involvement of the patient’s family or significant others in the treatment, among other topic
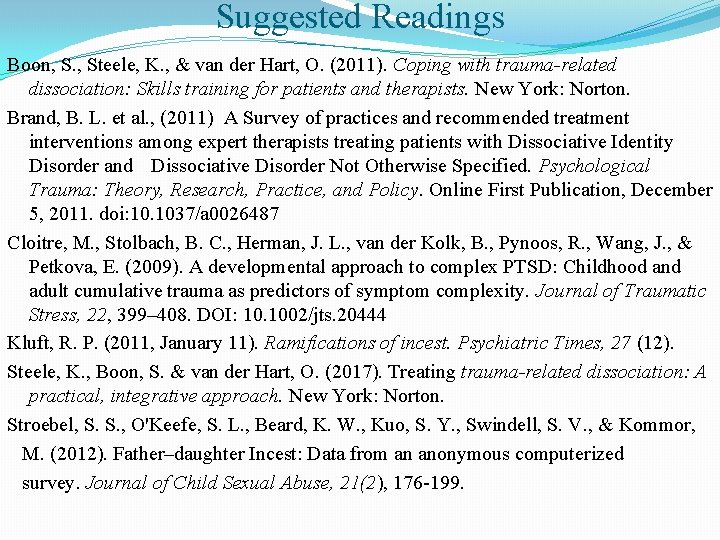
Suggested Readings Boon, S. , Steele, K. , & van der Hart, O. (2011). Coping with trauma-related dissociation: Skills training for patients and therapists. New York: Norton. Brand, B. L. et al. , (2011) A Survey of practices and recommended treatment interventions among expert therapists treating patients with Dissociative Identity Disorder and Dissociative Disorder Not Otherwise Specified. Psychological Trauma: Theory, Research, Practice, and Policy. Online First Publication, December 5, 2011. doi: 10. 1037/a 0026487 Cloitre, M. , Stolbach, B. C. , Herman, J. L. , van der Kolk, B. , Pynoos, R. , Wang, J. , & Petkova, E. (2009). A developmental approach to complex PTSD: Childhood and adult cumulative trauma as predictors of symptom complexity. Journal of Traumatic Stress, 22, 399– 408. DOI: 10. 1002/jts. 20444 Kluft, R. P. (2011, January 11). Ramifications of incest. Psychiatric Times, 27 (12). Steele, K. , Boon, S. & van der Hart, O. (2017). Treating trauma-related dissociation: A practical, integrative approach. New York: Norton. Stroebel, S. S. , O'Keefe, S. L. , Beard, K. W. , Kuo, S. Y. , Swindell, S. V. , & Kommor, M. (2012). Father–daughter Incest: Data from an anonymous computerized survey. Journal of Child Sexual Abuse, 21(2), 176 -199.