Complex ASD Closures John M Lasala MD Ph





















- Slides: 50

Complex ASD Closures John M. Lasala MD Ph. D Director Interventional Cardiology Professor of Medicine Washington University St Louis MO
DISCLOSURES John M. Lasala, MD, Ph. D Honoraria – AGA Medical Corporation
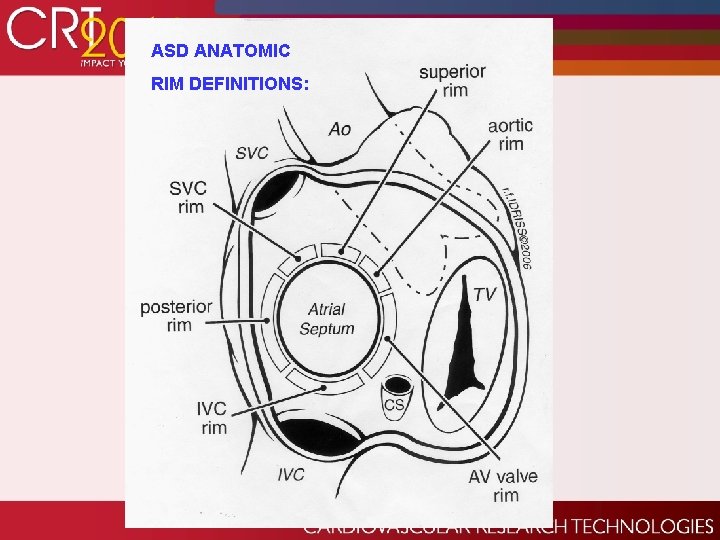
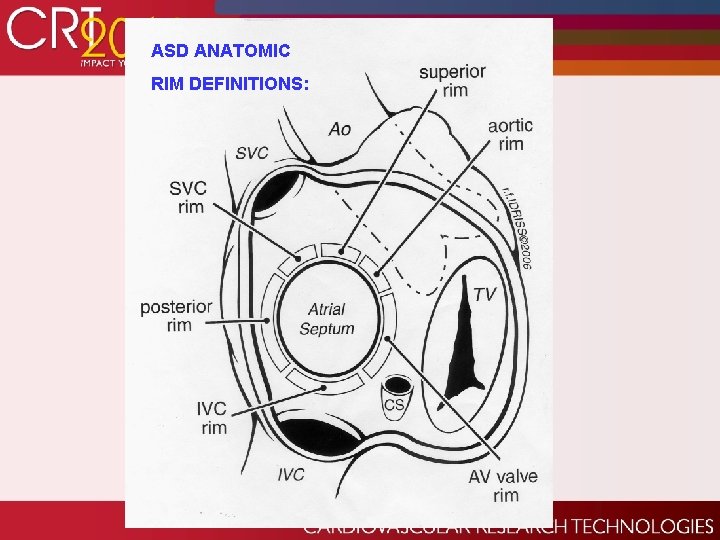
ASD ANATOMIC RIM DEFINITIONS:
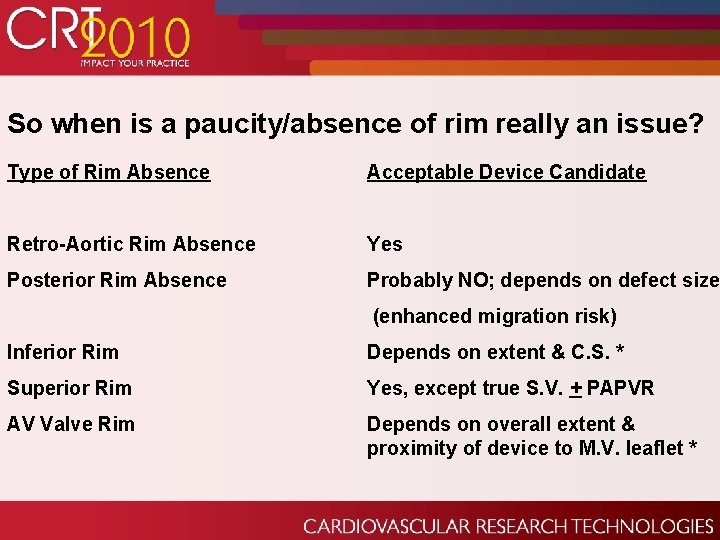
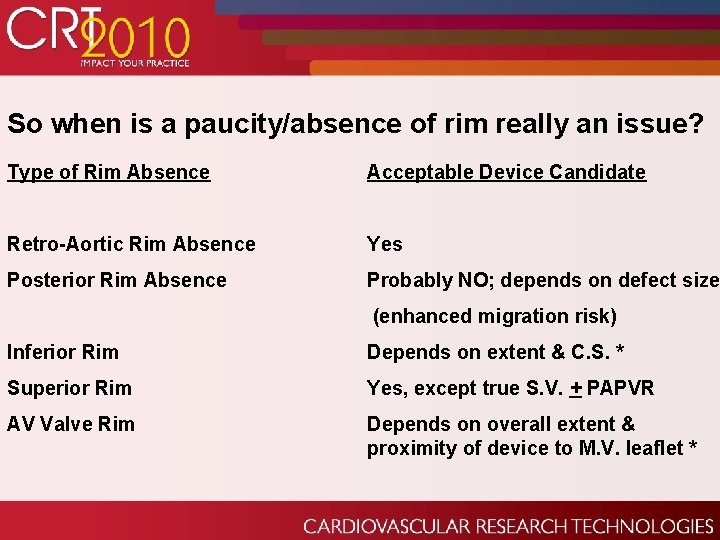
So when is a paucity/absence of rim really an issue? Type of Rim Absence Acceptable Device Candidate Retro-Aortic Rim Absence Yes Posterior Rim Absence Probably NO; depends on defect size (enhanced migration risk) Inferior Rim Depends on extent & C. S. * Superior Rim Yes, except true S. V. + PAPVR AV Valve Rim Depends on overall extent & proximity of device to M. V. leaflet *
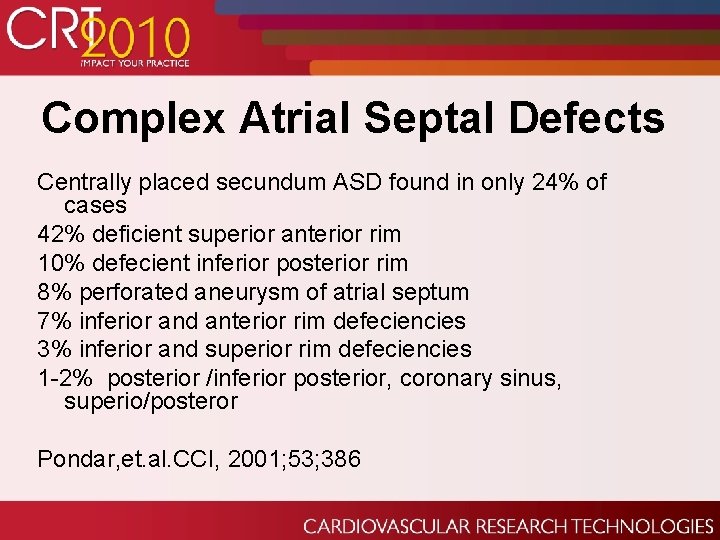
Complex Atrial Septal Defects Centrally placed secundum ASD found in only 24% of cases 42% deficient superior anterior rim 10% defecient inferior posterior rim 8% perforated aneurysm of atrial septum 7% inferior and anterior rim defeciencies 3% inferior and superior rim defeciencies 1 -2% posterior /inferior posterior, coronary sinus, superio/posteror Pondar, et. al. CCI, 2001; 53; 386
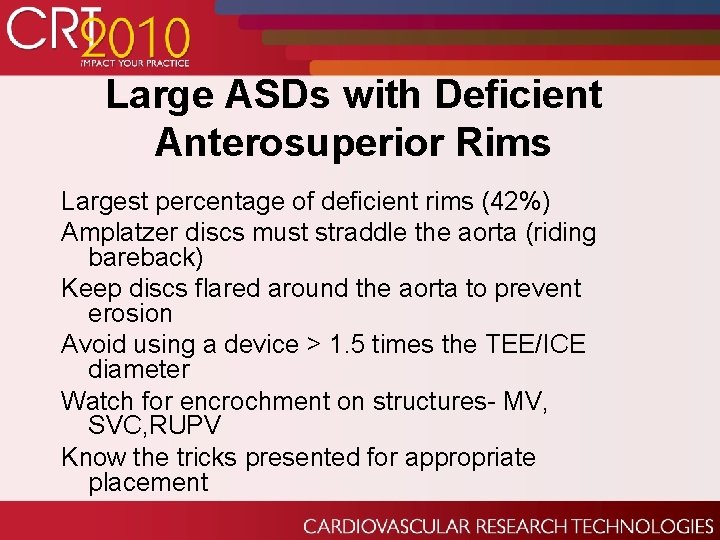
Large ASDs with Deficient Anterosuperior Rims Largest percentage of deficient rims (42%) Amplatzer discs must straddle the aorta (riding bareback) Keep discs flared around the aorta to prevent erosion Avoid using a device > 1. 5 times the TEE/ICE diameter Watch for encrochment on structures- MV, SVC, RUPV Know the tricks presented for appropriate placement
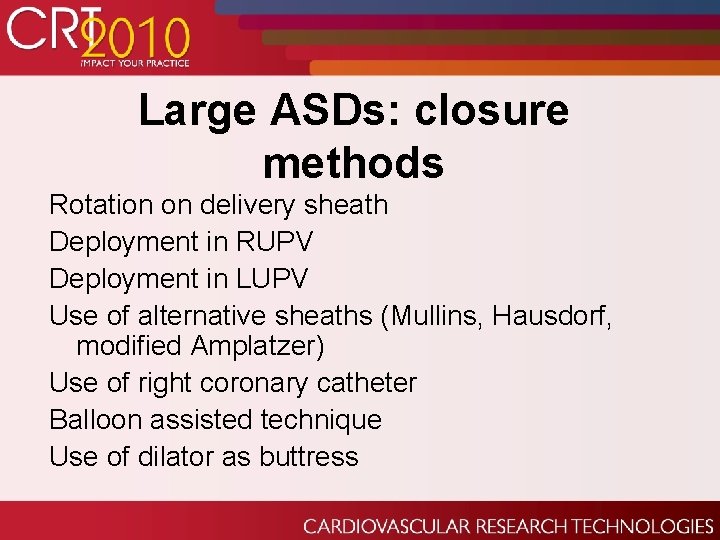
Large ASDs: closure methods Rotation on delivery sheath Deployment in RUPV Deployment in LUPV Use of alternative sheaths (Mullins, Hausdorf, modified Amplatzer) Use of right coronary catheter Balloon assisted technique Use of dilator as buttress
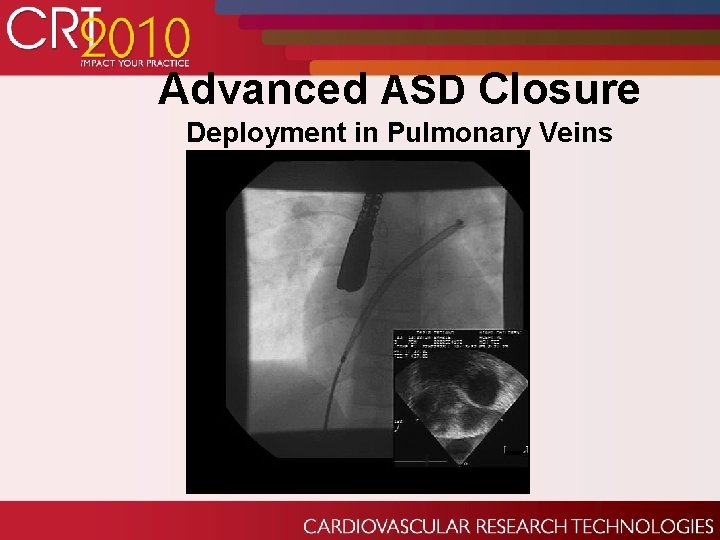
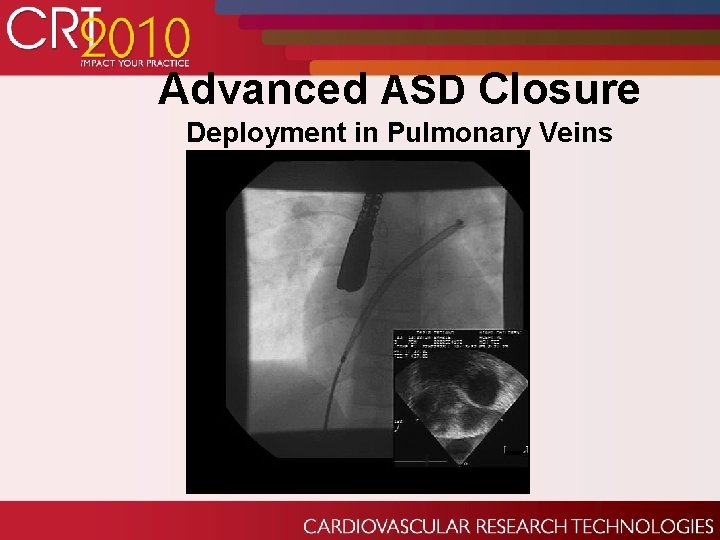
Advanced ASD Closure Deployment in Pulmonary Veins
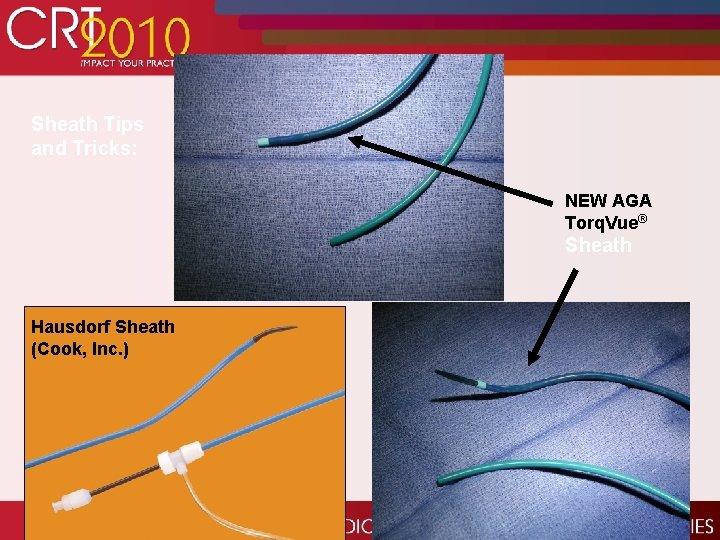
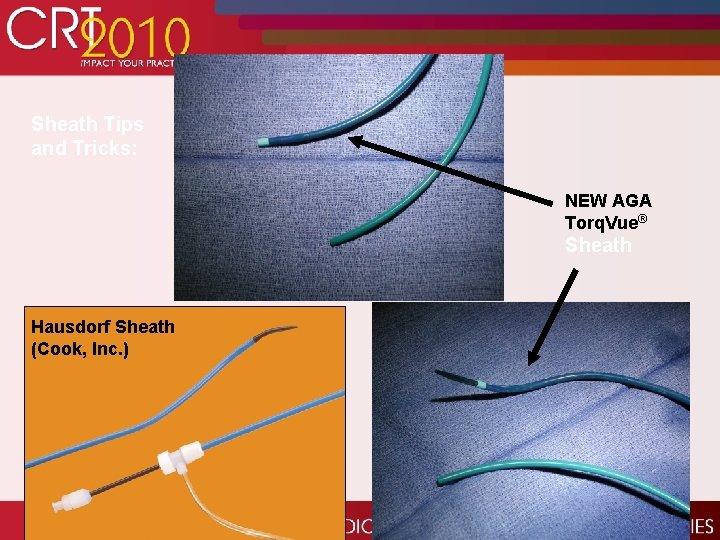
Sheath Tips and Tricks: NEW AGA Torq. Vue® Sheath Hausdorf Sheath (Cook, Inc. )

Balloon Assisted Technique LA disk and sheath pulled toward IAS Waist and RA disk released Balloon gradually deflated During deflation the RA disk was moved toward LA disk by pushing the delivery cable Balloon and guidewire were subsequently removed Catheter Cardiovasc Interv 2005; 64: 102 -107
Challenging Case: Large ASD
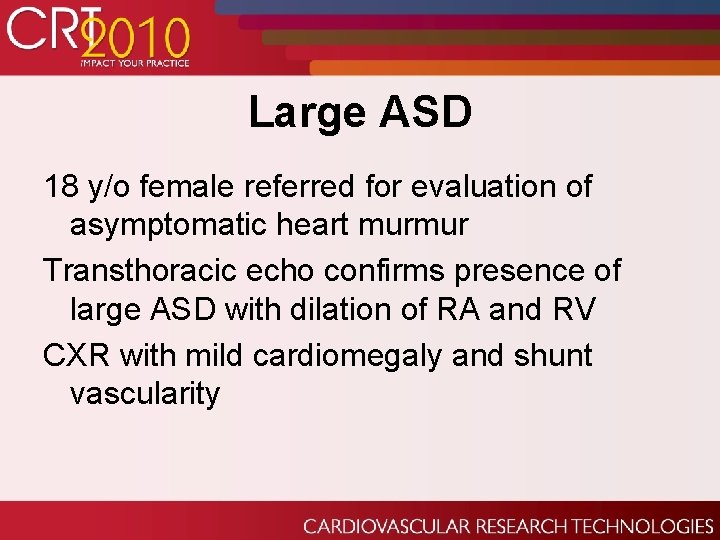
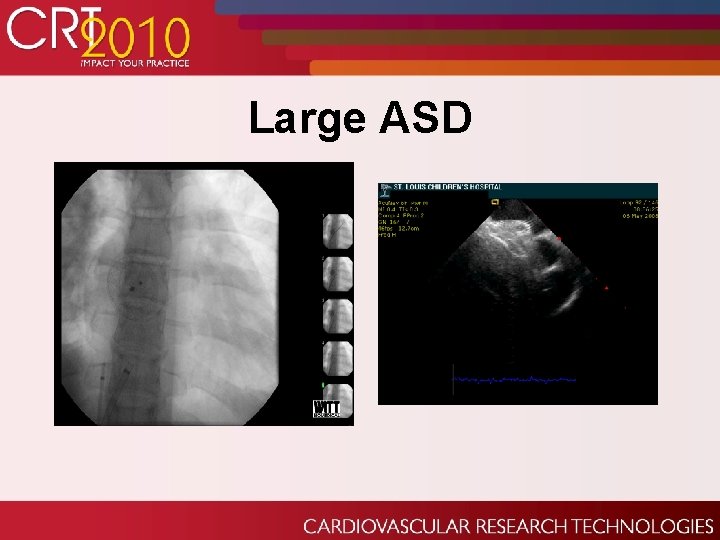
Large ASD 18 y/o female referred for evaluation of asymptomatic heart murmur Transthoracic echo confirms presence of large ASD with dilation of RA and RV CXR with mild cardiomegaly and shunt vascularity

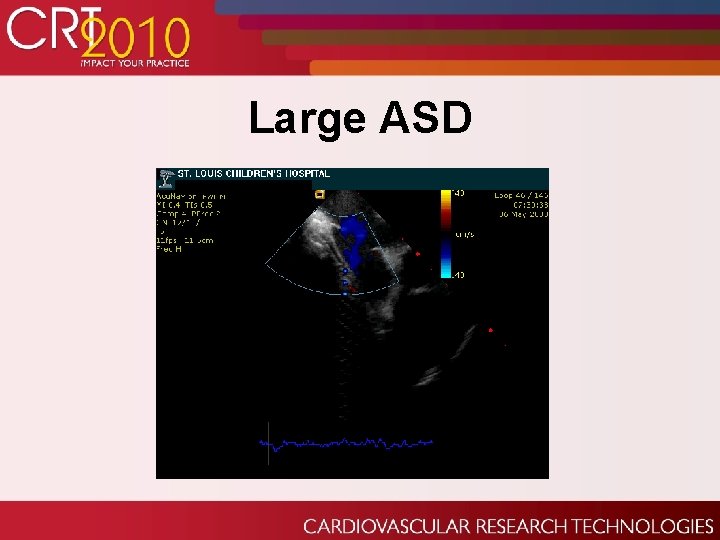
Large ASD Cardiac cath demonstrates normal right heart pressures and Qp: Qs 3: 1 ICE demonstrates large secundum ASD
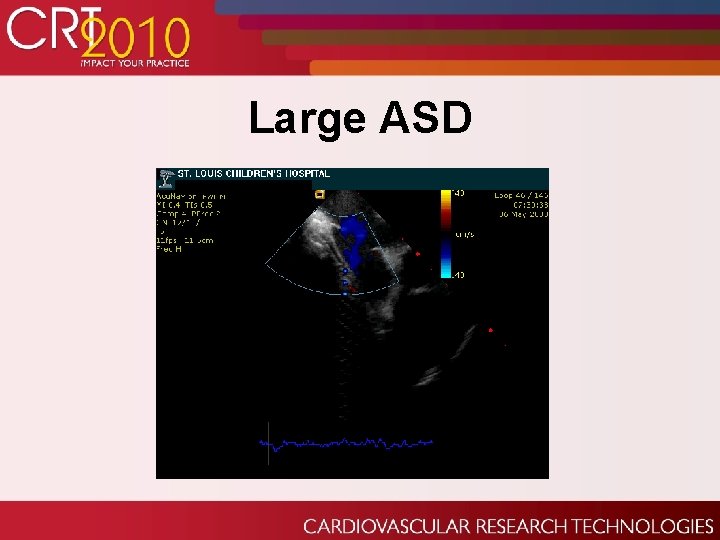
Large ASD

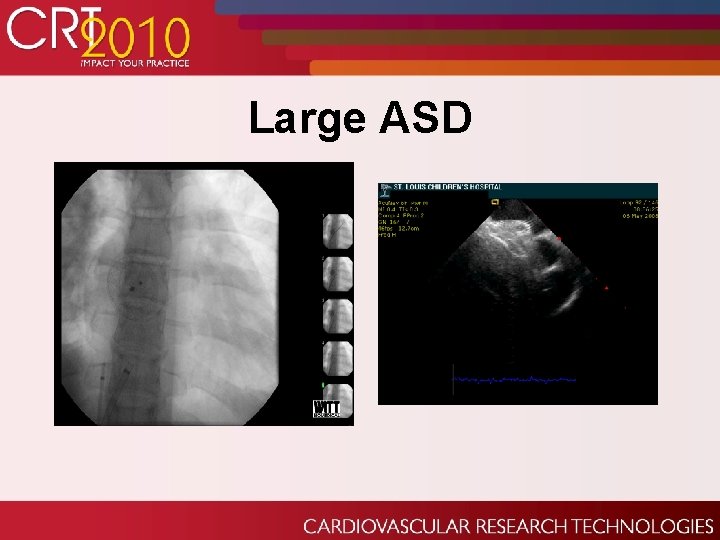
Large ASD Several unsuccessful attempts were made to deploy 28 mm Amplatzer device in conventional manner Attempts at left PV deployment technique or a Hausedorf Sheath were also unsuccessful secondary to prolapse of LA disc through retroaortic rim

Large ASD

Large ASD

Large ASD

Large ASD
Large ASD

Large ASD

Closure of Multiple ASDs
Multiple ASDs Balloon sizing sequentially (single venous access) or simultaneously (2 venous access) If simultaneous delivery of 2 devices: – Need two sheaths – Deliver smaller device first – Larger device “sandwich” smaller device – Deliver both devices before release – Reassess entire septum to make sure there is no impingement of device against atrial wall before release (especially in deficient or absent rims) 23 23

Multiple ASDs Occurs in up to 6. 6% of ASDs May require multiple devices to close the defects if far enough apart Single device may be adequate for closely spaced defects Occasionally balloon sizing will convert multiple defects into a single defect

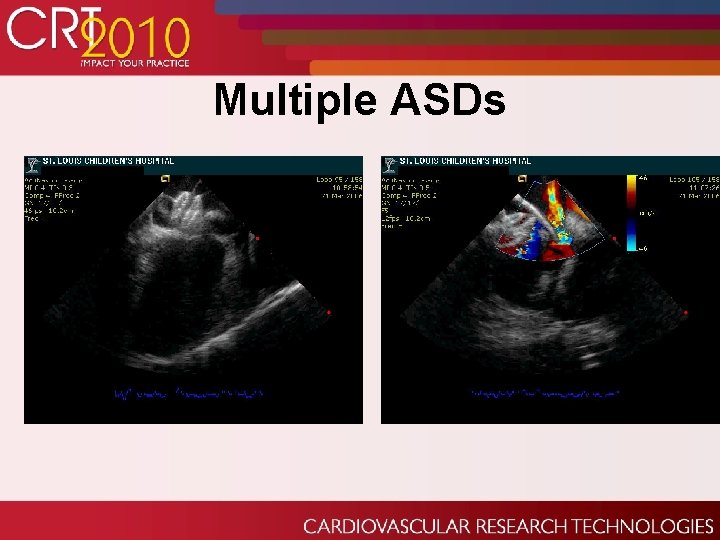
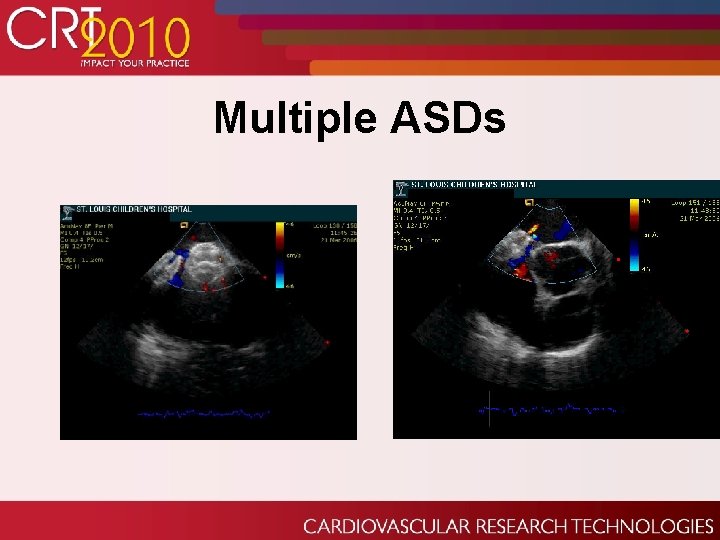
Multiple ASDs
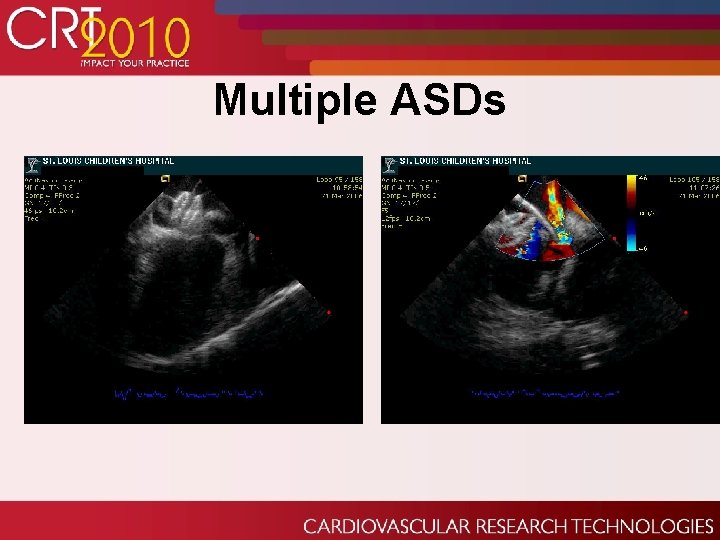
Multiple ASDs
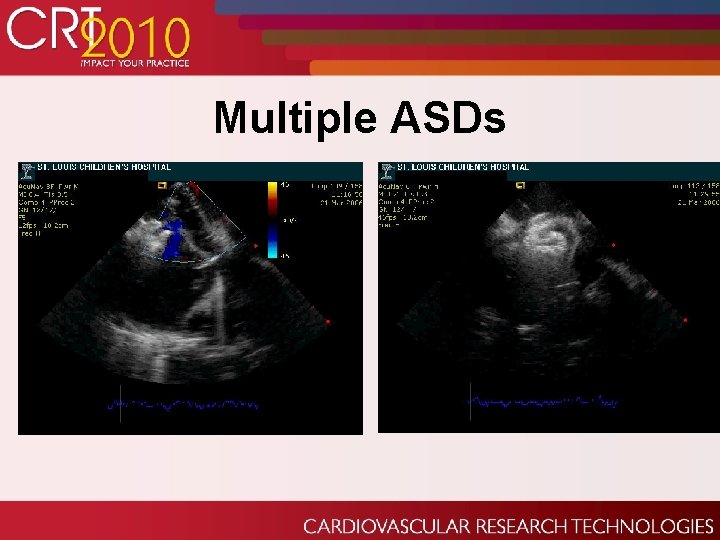
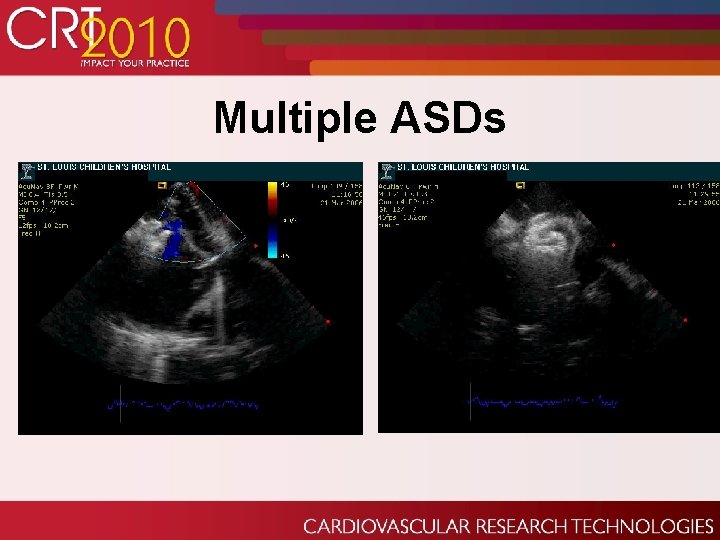
Multiple ASDs
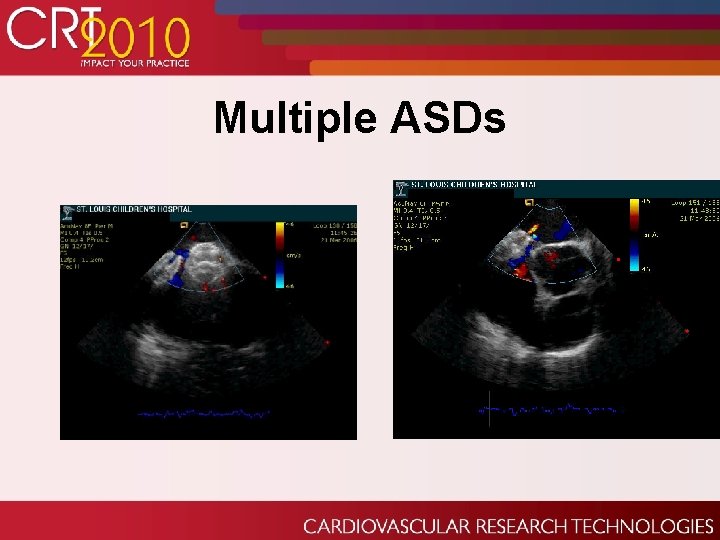
Multiple ASDs
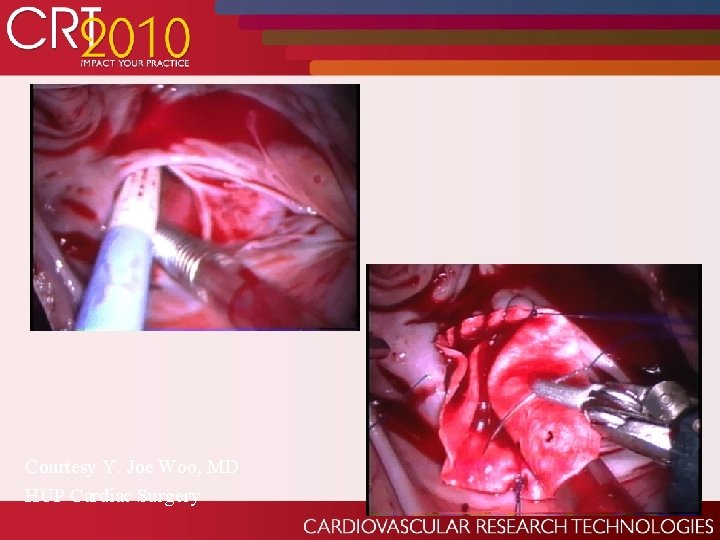
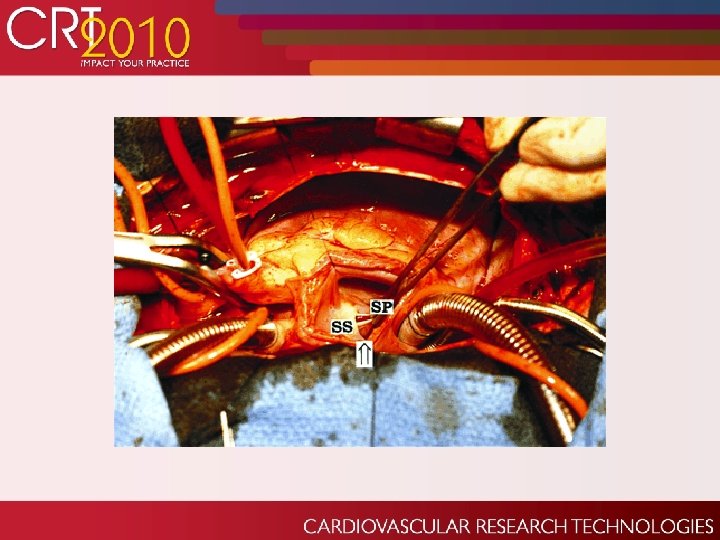
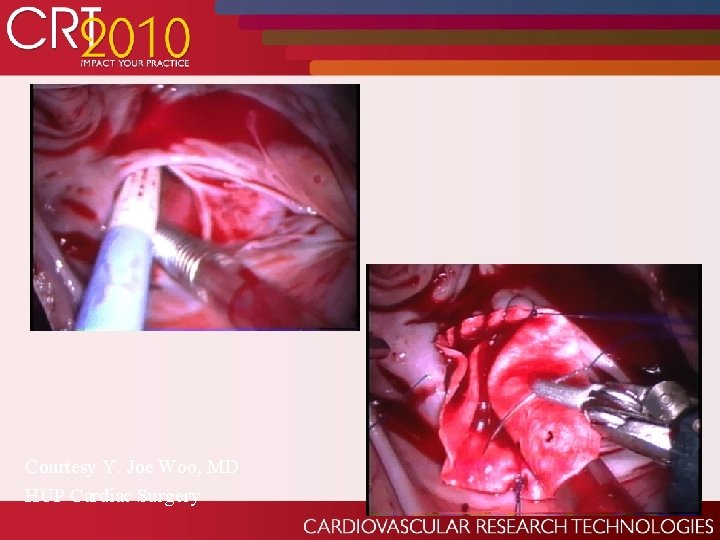
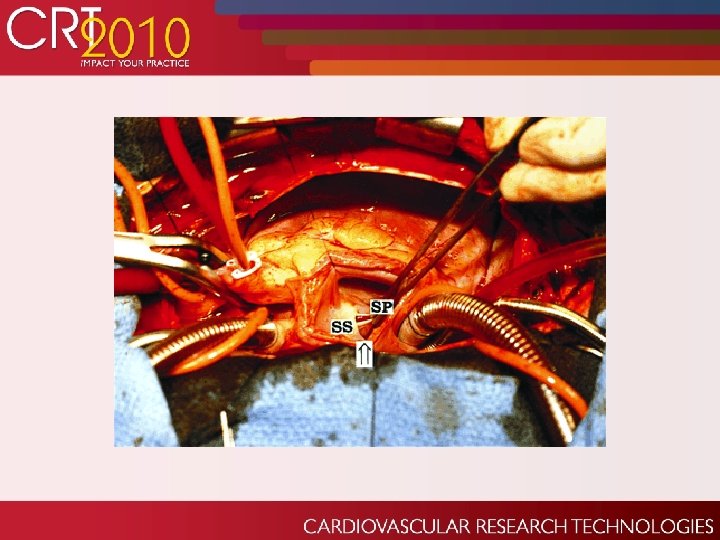
Courtesy Y. Joe Woo, MD HUP Cardiac Surgery

Amplatzer “Cribiform” Multi-Fenestrated Atrial Septal Occluder
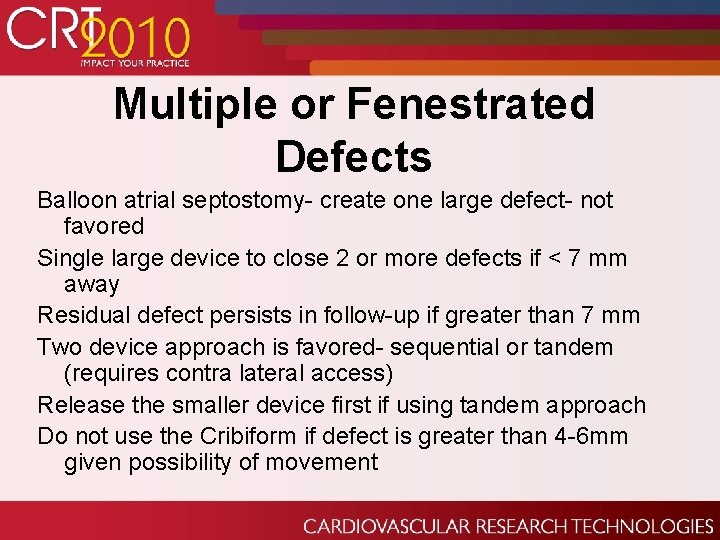
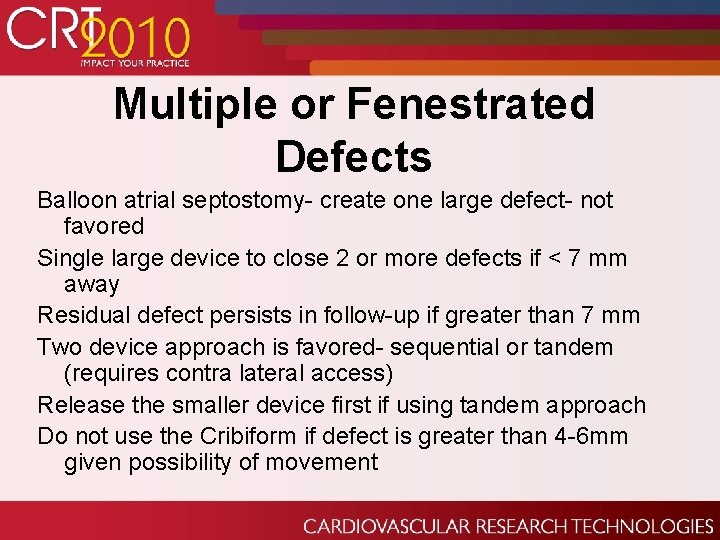
Multiple or Fenestrated Defects Balloon atrial septostomy- create one large defect- not favored Single large device to close 2 or more defects if < 7 mm away Residual defect persists in follow-up if greater than 7 mm Two device approach is favored- sequential or tandem (requires contra lateral access) Release the smaller device first if using tandem approach Do not use the Cribiform if defect is greater than 4 -6 mm given possibility of movement

Closure performed – #25 AGA Cribiform ASO inserted in PFO – #14 AGA Atrial septal occluder for ASD
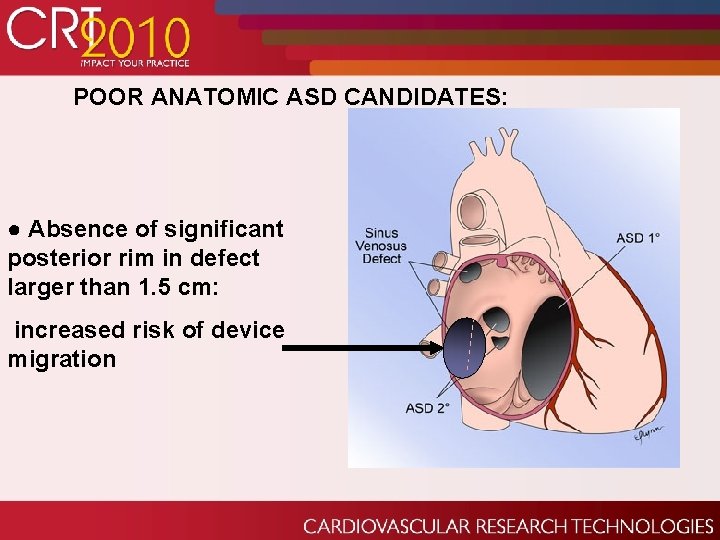
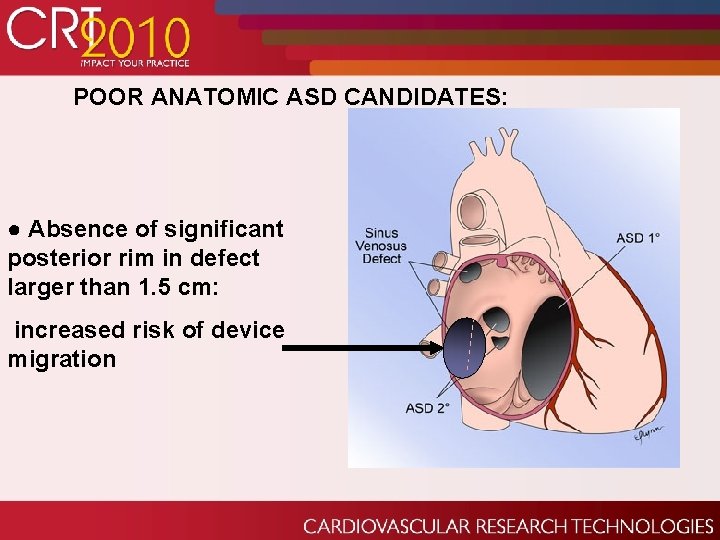
POOR ANATOMIC ASD CANDIDATES: ● Absence of significant posterior rim in defect larger than 1. 5 cm: increased risk of device migration
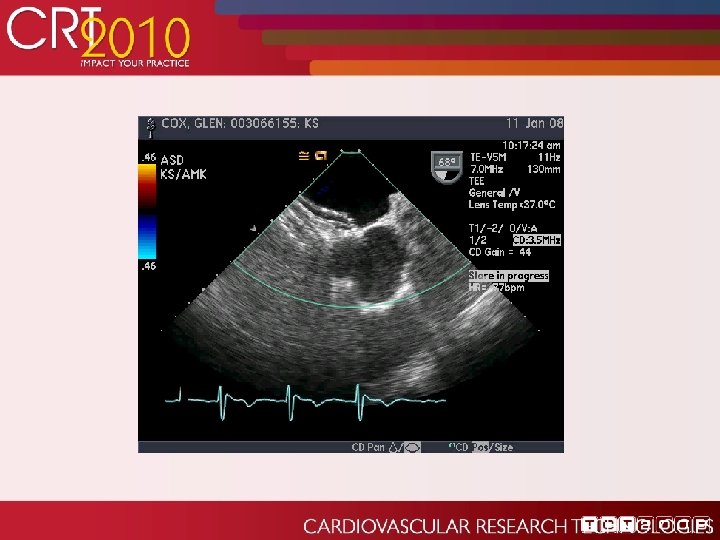
Case Report: History of Present Illness: GC is a 68 yo male with a long hx of A-fib on coumadin. He has had increasing fatigue and worsening DOE over last several months. Past Medical Hx: • HTN • A-fib • Gout
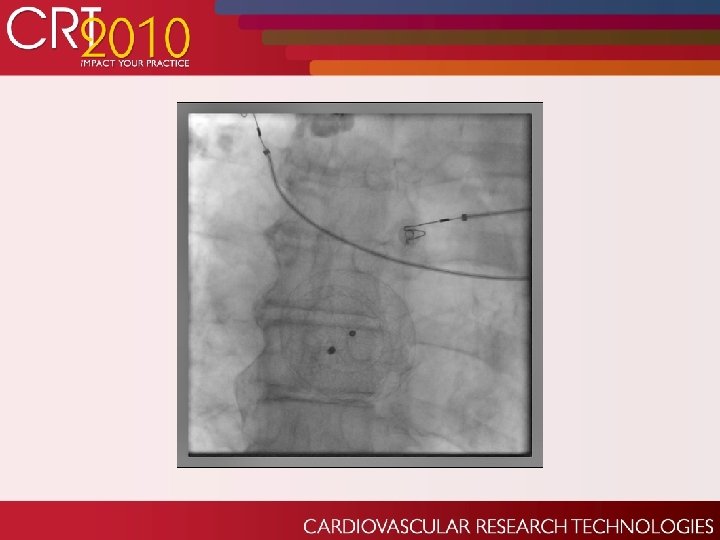
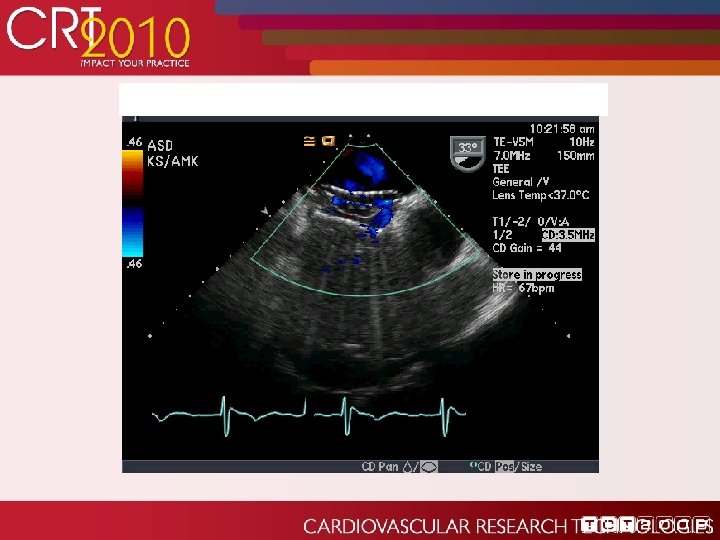
Case Report cont: ASD History: Recent murmur appreciated and echo revealed a large secundum ASD with estimated diameter of 27 and 28 mm. R-sided chambers were enlarged, mod Pulm HTN was present. MRI ruled out sinus venosus defect with any anomalous pulmonary drainage. He underwent initial attempt at percutaneous closure at OSH, but defect unsuccessfully closed. Patient referred to Barnes-Jewish for second attempt at percutaneous closure.



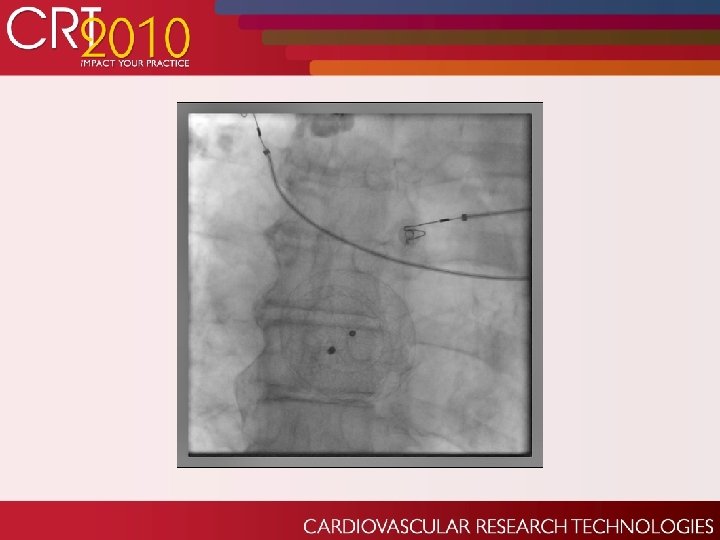

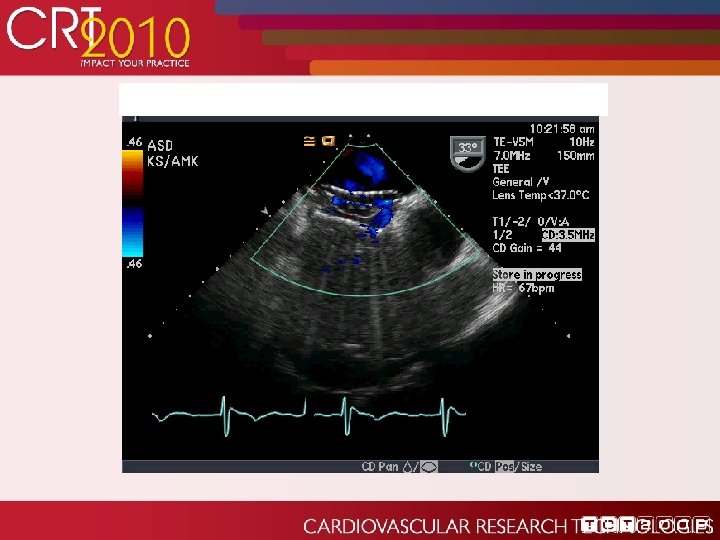
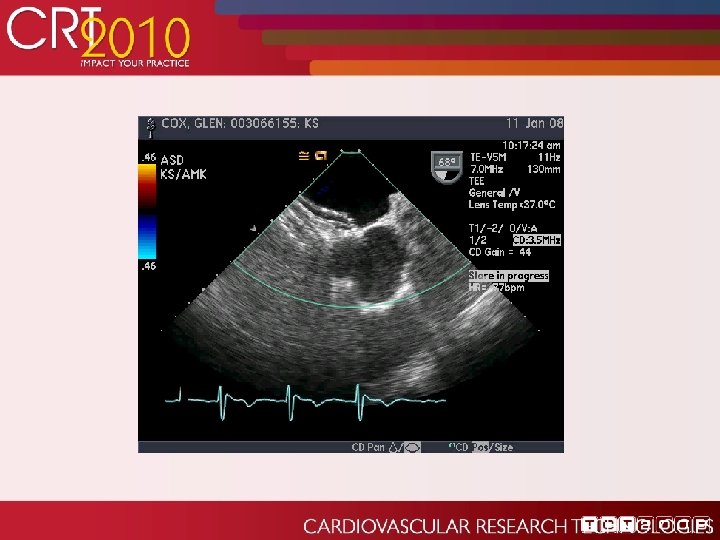
Later the Same Day… Patient was transferred to the floor No complaints Routine TTE obtained that night per protocol 911 page sent
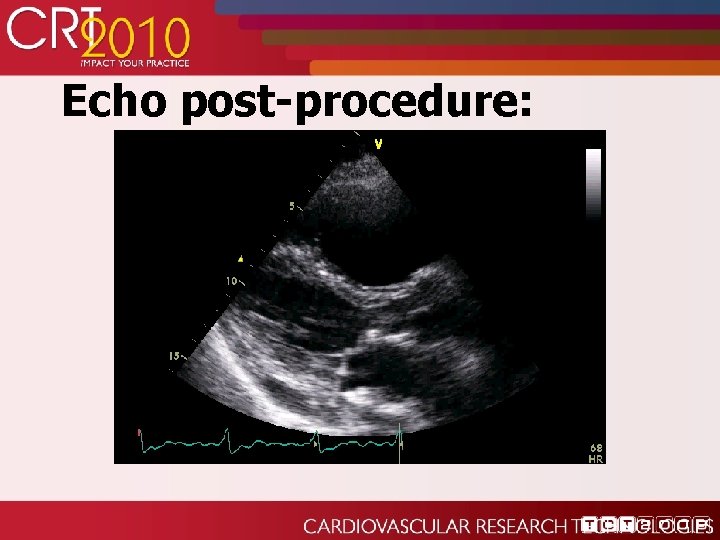
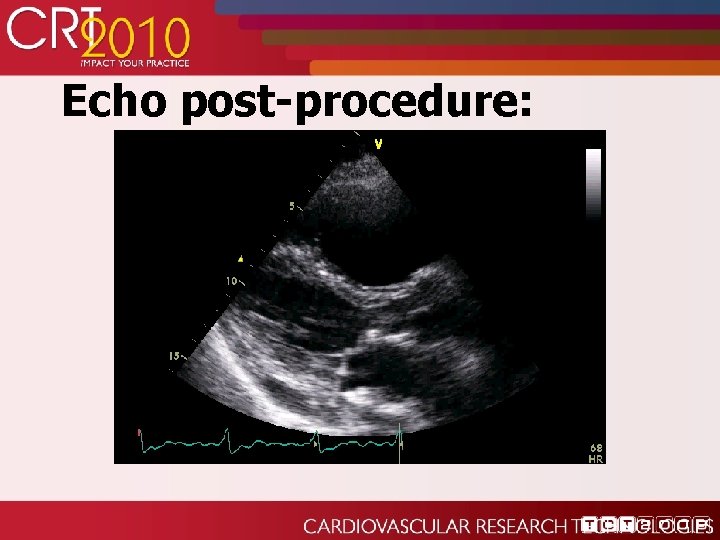
Echo post-procedure:

Echo post-procedure:

Later the Same Day…. Though non-emergent CT surgery took patient to OR the same night. Percutaneous extraction considered but concern over thrombus potentional on device sitting in LA so long. Did well post op until day 3.
Deficient Posteroinferior Rims A real challenge as these tend to be larger ASDs MD beware if rim is < 3 mm. Increased complication rate- IVC or Pulmonary vein obstruction, encroachment on mitral valve, frank embolization
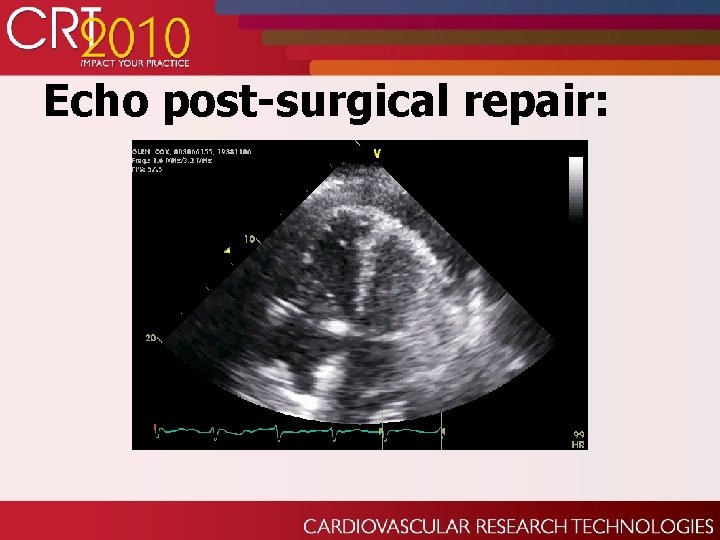
Echo post-surgical repair:

Percutaneous Complications: Device embolization or malposition Residual shunting Atrial arrhythmias, heart block, sudden death Bleeding, groin hematoma Cardiac perforation, pericardial effusion Thrombus formation (overall rate 1. 2%) More common with Cardio. SEAL/STARflex than with Amplatzer device Device erosion (0. 1%)