Complete Recovery of Renal Function After Acute Kidney
- Slides: 1
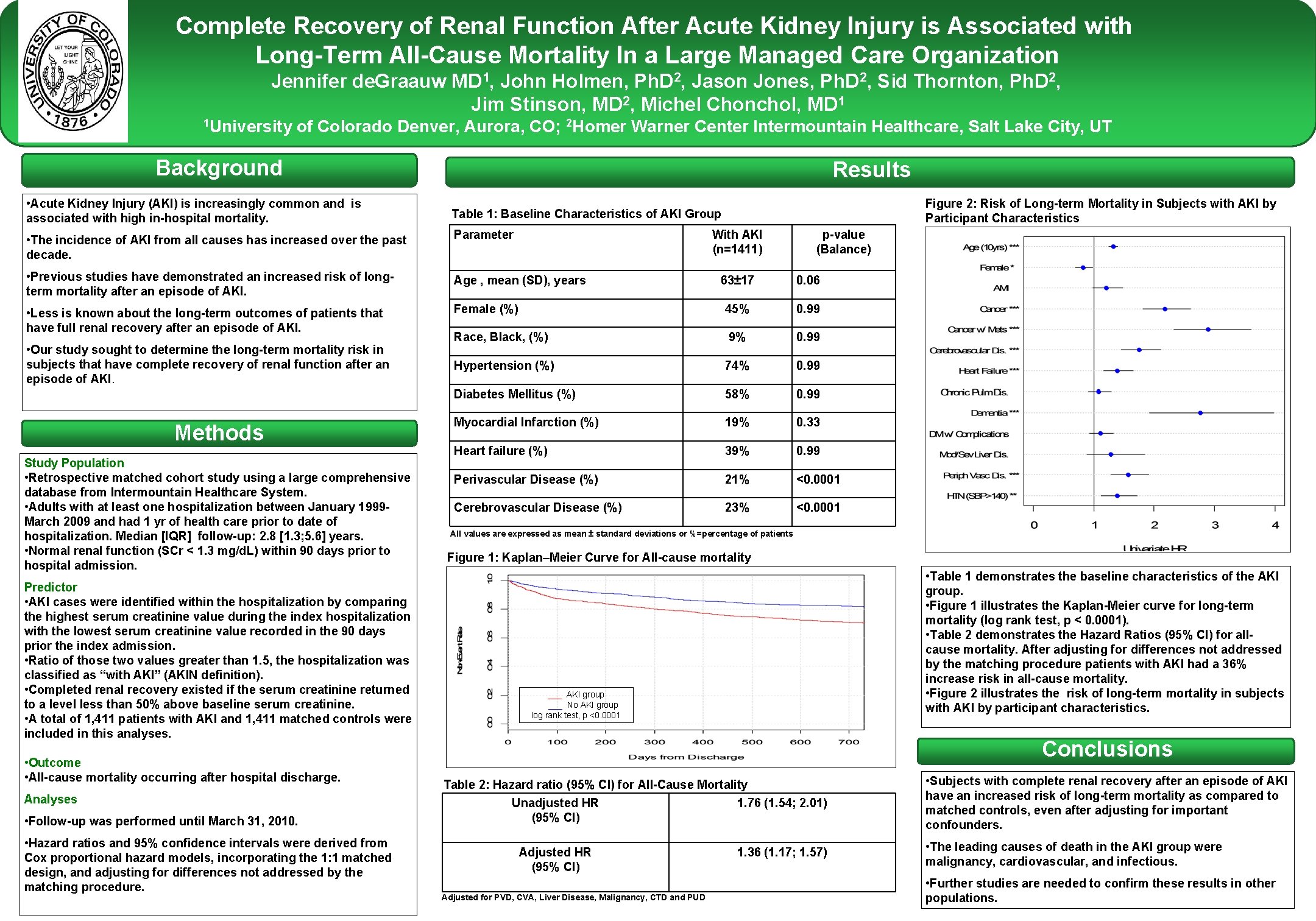
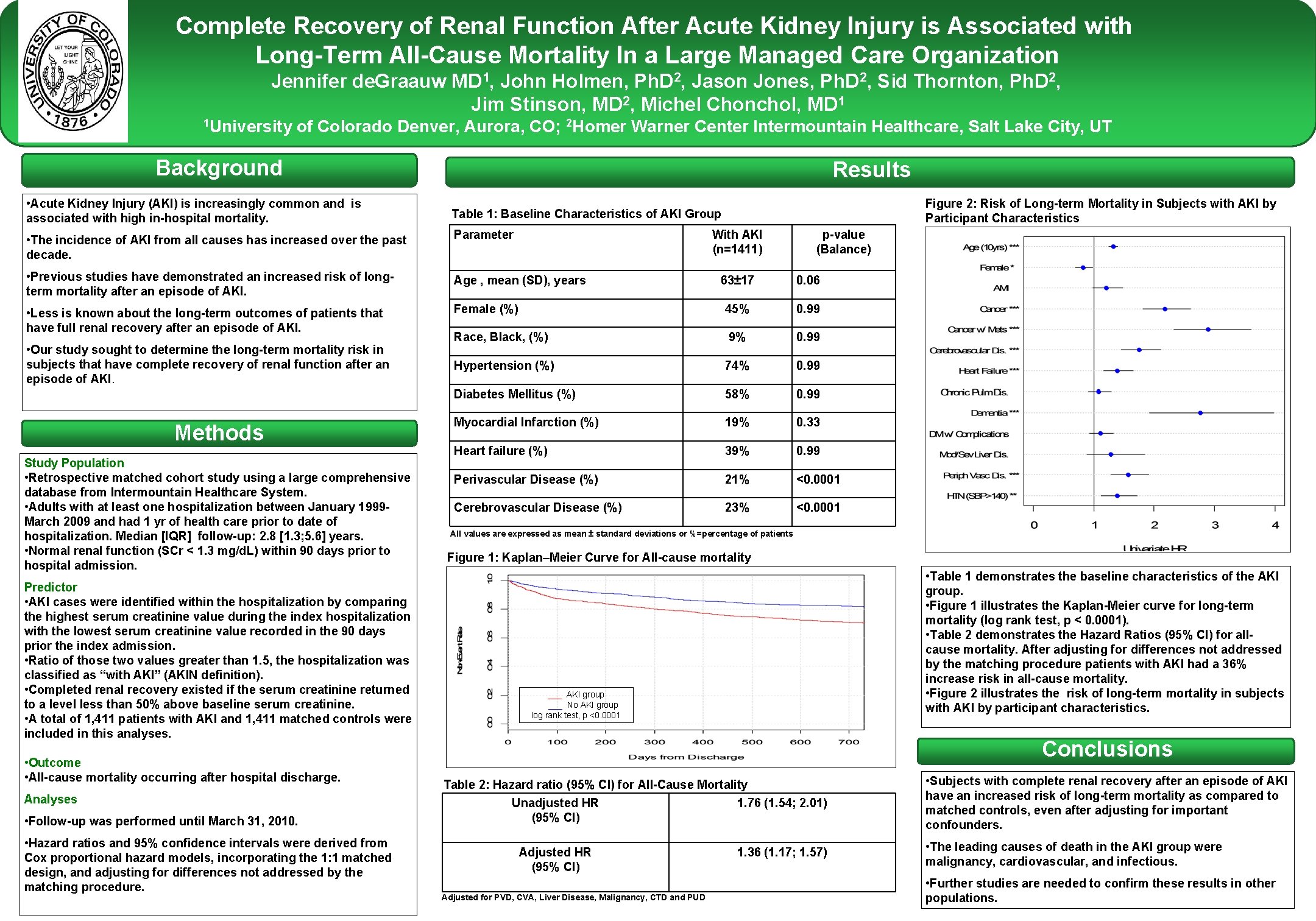
Complete Recovery of Renal Function After Acute Kidney Injury is Associated with Long-Term All-Cause Mortality In a Large Managed Care Organization Jennifer de. Graauw MD 1, John Holmen, Ph. D 2, Jason Jones, Ph. D 2, Sid Thornton, Ph. D 2, Jim Stinson, MD 2, Michel Chonchol, MD 1 1 University of Colorado Denver, Aurora, CO; 2 Homer Warner Center Intermountain Healthcare, Salt Lake City, UT Background • Acute Kidney Injury (AKI) is increasingly common and is associated with high in-hospital mortality. Results Table 1: Baseline Characteristics of AKI Group • The incidence of AKI from all causes has increased over the past decade. Parameter • Previous studies have demonstrated an increased risk of longterm mortality after an episode of AKI. Age , mean (SD), years • Less is known about the long-term outcomes of patients that have full renal recovery after an episode of AKI. • Our study sought to determine the long-term mortality risk in subjects that have complete recovery of renal function after an episode of AKI. Methods Study Population • Retrospective matched cohort study using a large comprehensive database from Intermountain Healthcare System. • Adults with at least one hospitalization between January 1999 March 2009 and had 1 yr of health care prior to date of hospitalization. Median [IQR] follow-up: 2. 8 [1. 3; 5. 6] years. • Normal renal function (SCr < 1. 3 mg/d. L) within 90 days prior to hospital admission. Predictor • AKI cases were identified within the hospitalization by comparing the highest serum creatinine value during the index hospitalization with the lowest serum creatinine value recorded in the 90 days prior the index admission. • Ratio of those two values greater than 1. 5, the hospitalization was classified as “with AKI” (AKIN definition). • Completed renal recovery existed if the serum creatinine returned to a level less than 50% above baseline serum creatinine. • A total of 1, 411 patients with AKI and 1, 411 matched controls were included in this analyses. • Outcome • All-cause mortality occurring after hospital discharge. Analyses • Follow-up was performed until March 31, 2010. • Hazard ratios and 95% confidence intervals were derived from Cox proportional hazard models, incorporating the 1: 1 matched design, and adjusting for differences not addressed by the matching procedure. Figure 2: Risk of Long-term Mortality in Subjects with AKI by Participant Characteristics With AKI (n=1411) p-value (Balance) 63± 17 0. 06 Female (%) 45% 0. 99 Race, Black, (%) 9% 0. 99 Hypertension (%) 74% 0. 99 Diabetes Mellitus (%) 58% 0. 99 Myocardial Infarction (%) 19% 0. 33 Heart failure (%) 39% 0. 99 Perivascular Disease (%) 21% <0. 0001 Cerebrovascular Disease (%) 23% <0. 0001 Conclusions All values are expressed as mean ± standard deviations or %=percentage of patients Figure 1: Kaplan–Meier Curve for All-cause mortality • Table 1 demonstrates the baseline characteristics of the AKI group. • Figure 1 illustrates the Kaplan-Meier curve for long-term mortality (log rank test, p < 0. 0001). • Table 2 demonstrates the Hazard Ratios (95% CI) for allcause mortality. After adjusting for differences not addressed by the matching procedure patients with AKI had a 36% increase risk in all-cause mortality. • Figure 2 illustrates the risk of long-term mortality in subjects with AKI by participant characteristics. ___ AKI group ___ No AKI group log rank test, p <0. 0001 Conclusions Table 2: Hazard ratio (95% CI) for All-Cause Mortality Unadjusted HR 1. 76 (1. 54; 2. 01) (95% CI) Adjusted HR (95% CI) Adjusted for PVD, CVA, Liver Disease, Malignancy, CTD and PUD 1. 36 (1. 17; 1. 57) • Subjects with complete renal recovery after an episode of AKI have an increased risk of long-term mortality as compared to matched controls, even after adjusting for important confounders. • The leading causes of death in the AKI group were malignancy, cardiovascular, and infectious. • Further studies are needed to confirm these results in other Printed by populations.