Complement J Ochotn Complement humoral component of nonspecific


- Slides: 52

Complement J. Ochotná
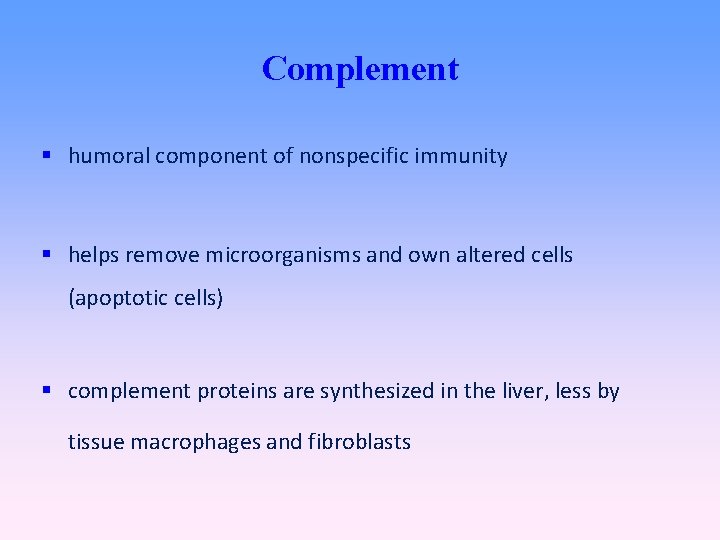
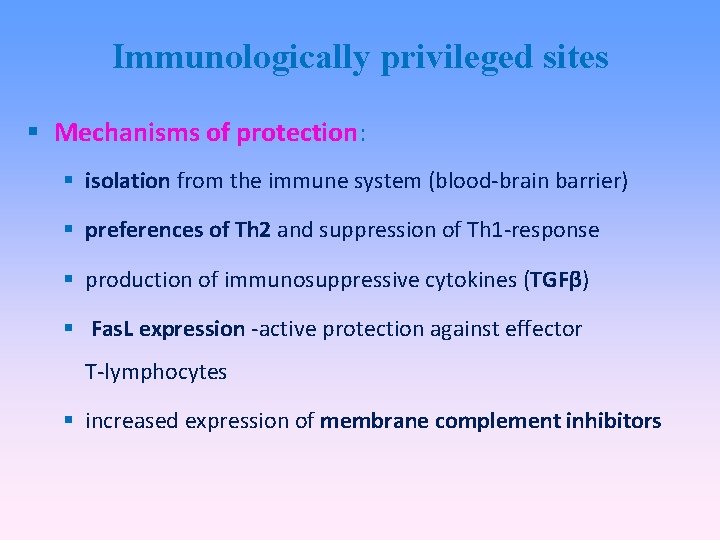
Complement humoral component of nonspecific immunity helps remove microorganisms and own altered cells (apoptotic cells) complement proteins are synthesized in the liver, less by tissue macrophages and fibroblasts
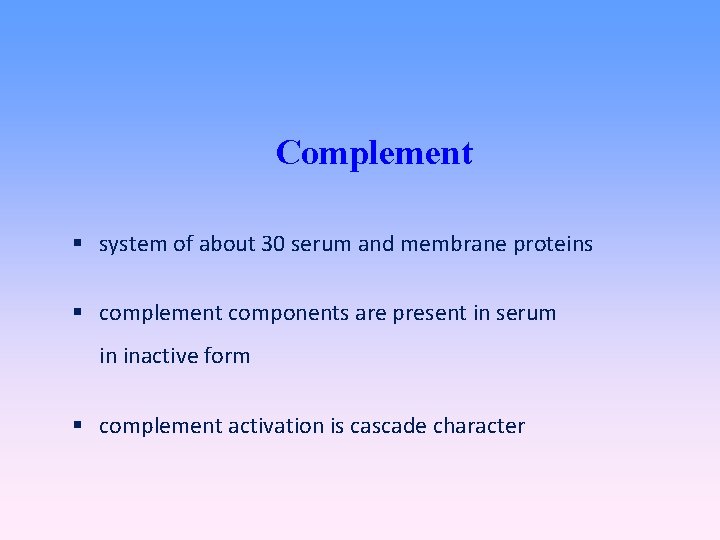
Complement system of about 30 serum and membrane proteins complement components are present in serum in inactive form complement activation is cascade character
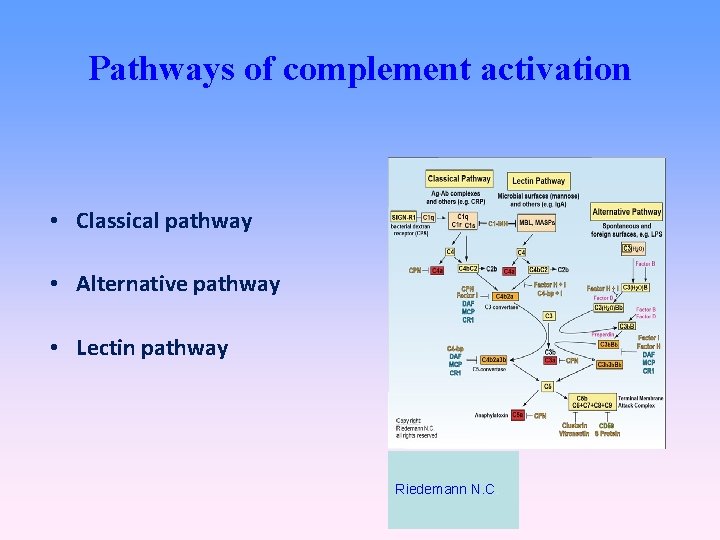
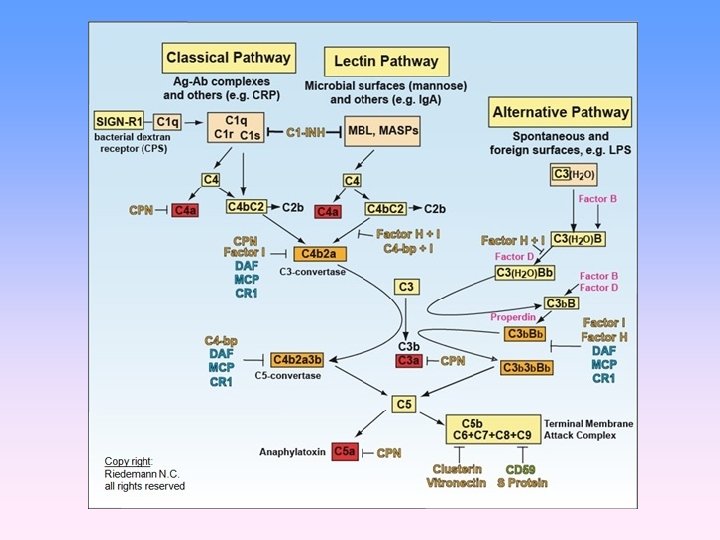
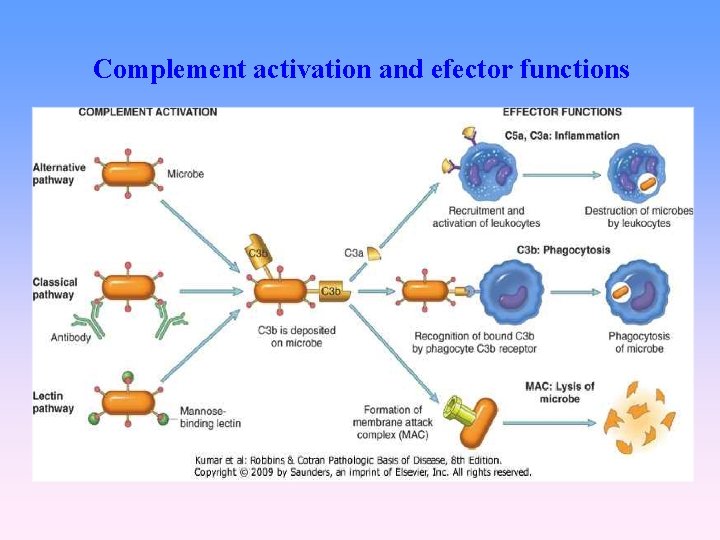
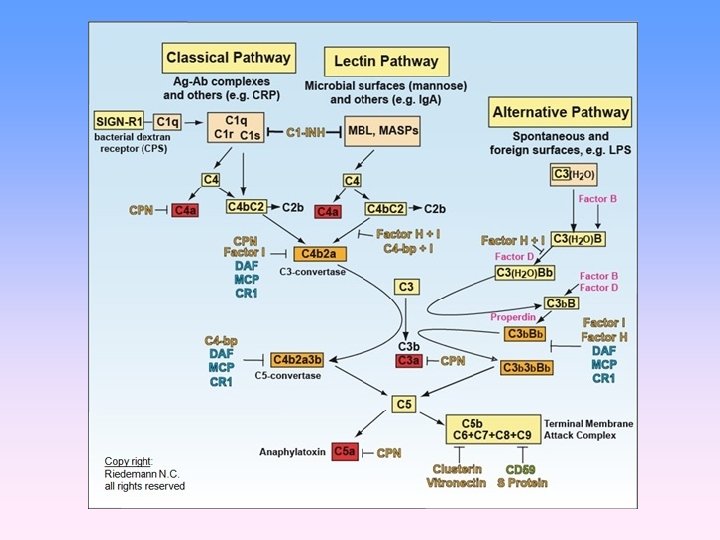
Pathways of complement activation • Classical pathway • Alternative pathway • Lectin pathway Riedemann N. C.
Classical complement pathway can be initiated by antibodies Ig. G ( not by Ig. G 4) and Ig. M or by pentraxins (CRP, SAP - acute phase proteins) after binding of antibodies to the bacteria surface, Ab changes its conformation and than can bind C 1 protein https: //www. youtube. com/watch? v=vb. WYz 9 XDt. Lw
Alternative complement pathway C 3 component of complement rarely spontaneously breaks into C 3 b and C 3 a C 3 b can covalently bind on the surface of a particle (own cell, microorganism) or reacts with water, thereby inactivates https: //www. youtube. com/watch? v=qga 3 Wn 76 d 9 w
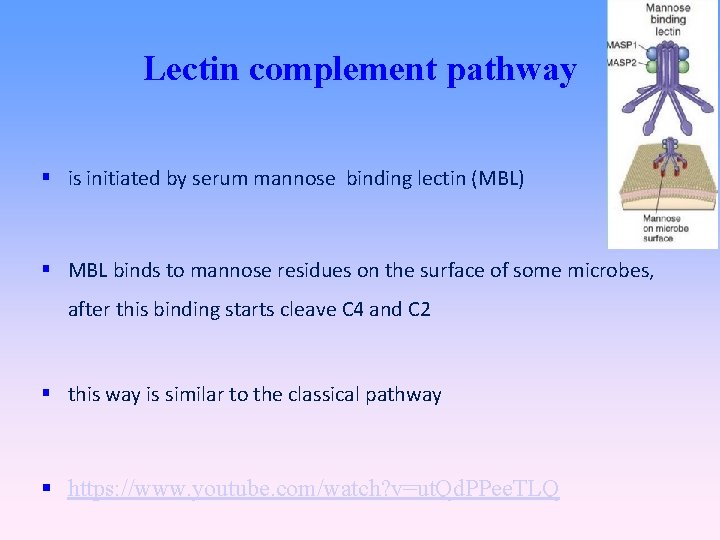
Lectin complement pathway is initiated by serum mannose binding lectin (MBL) MBL binds to mannose residues on the surface of some microbes, after this binding starts cleave C 4 and C 2 this way is similar to the classical pathway https: //www. youtube. com/watch? v=ut. Qd. PPee. TLQ
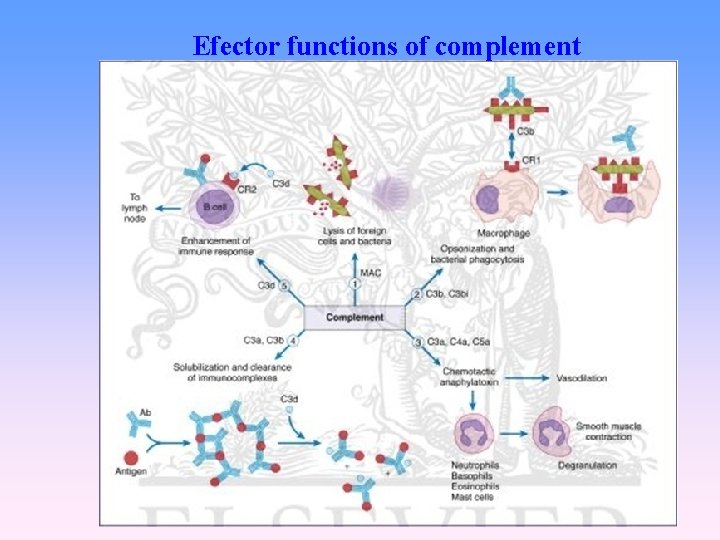
Biological significance of complement Opsonization (C 3 b, C 4 b) Chemotaxis (C 3 a, C 5 a) Osmotic lysis (MAC C 5 b-C 9) Anaphylatoxins (C 3 a, C 4 a, C 5 a)
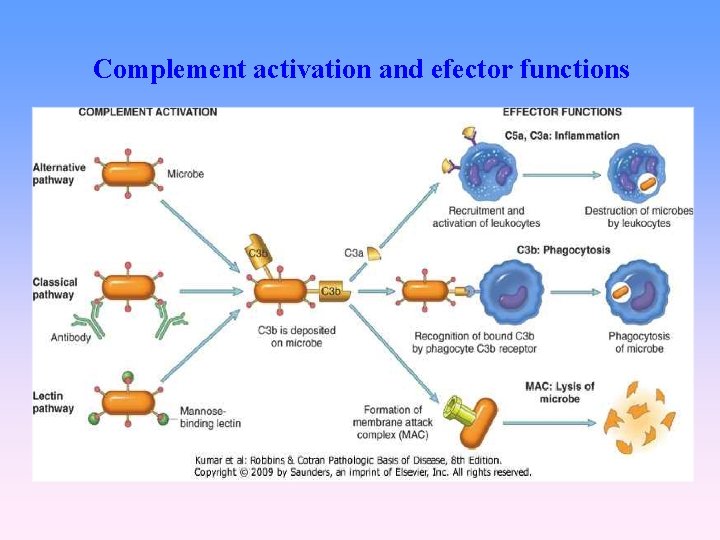
Complement activation and efector functions
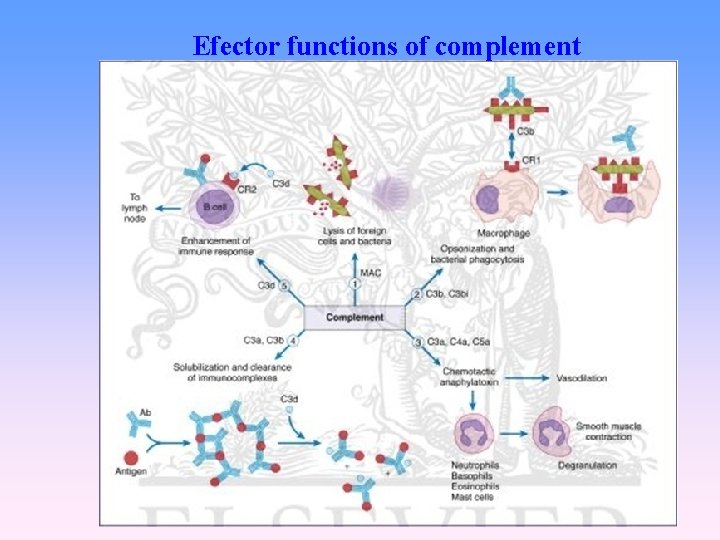
Efector functions of complement
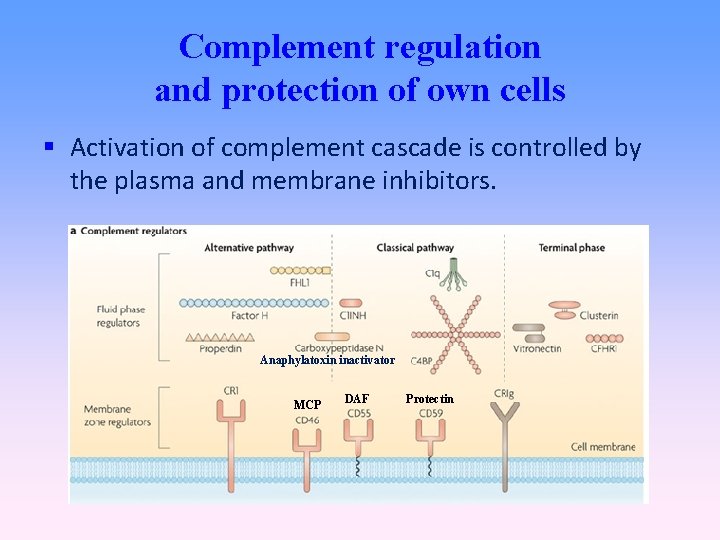
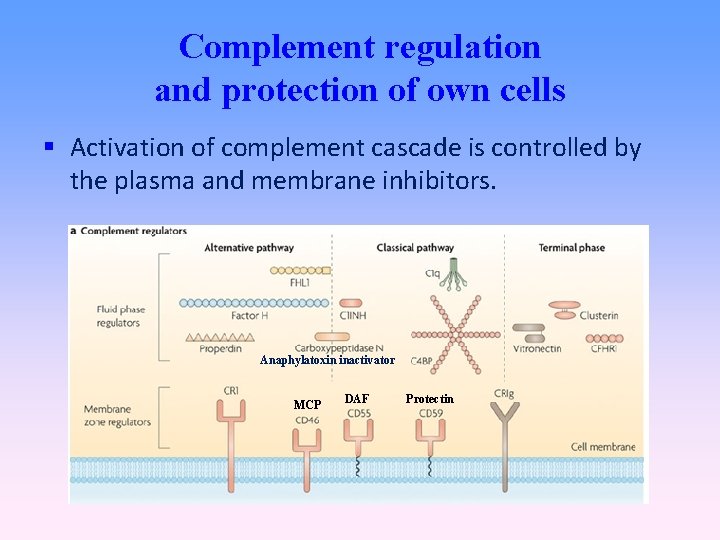
Complement regulation and protection of own cells Activation of complement cascade is controlled by the plasma and membrane inhibitors. Anaphylatoxin inactivator MCP DAF Protectin
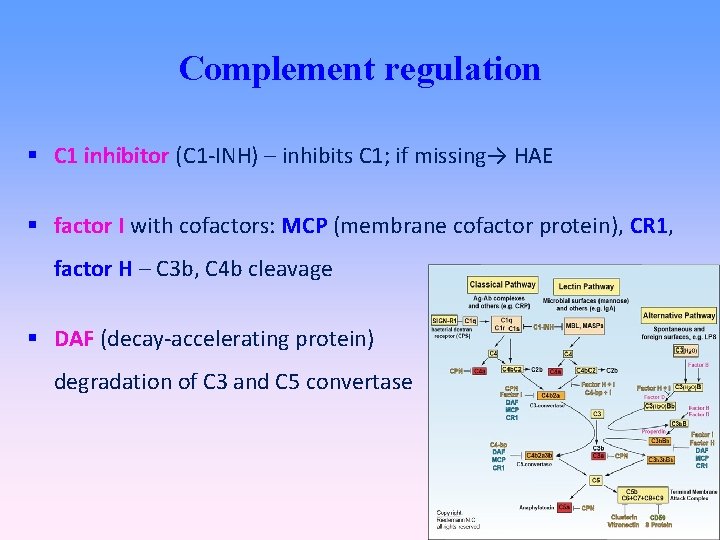
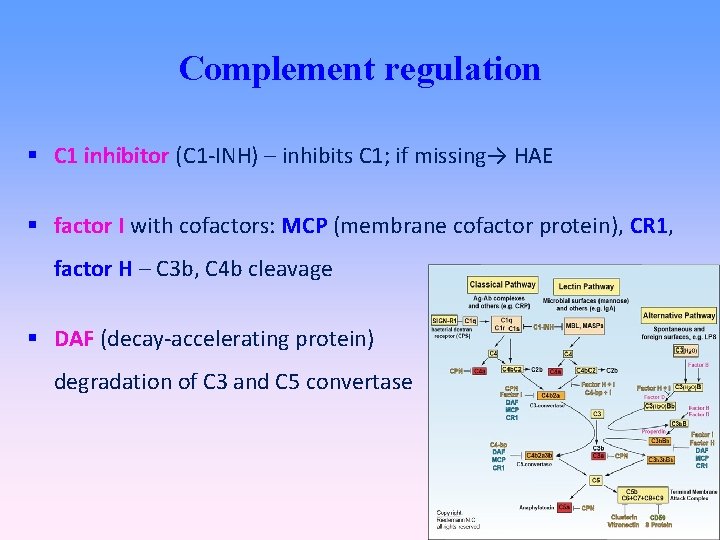
Complement regulation C 1 inhibitor (C 1 -INH) – inhibits C 1; if missing→ HAE factor I with cofactors: MCP (membrane cofactor protein), CR 1, factor H – C 3 b, C 4 b cleavage DAF (decay-accelerating protein) degradation of C 3 and C 5 convertase
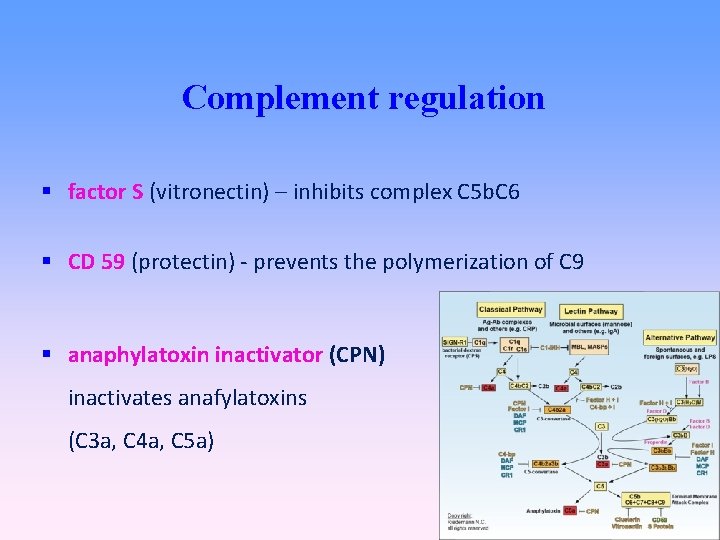
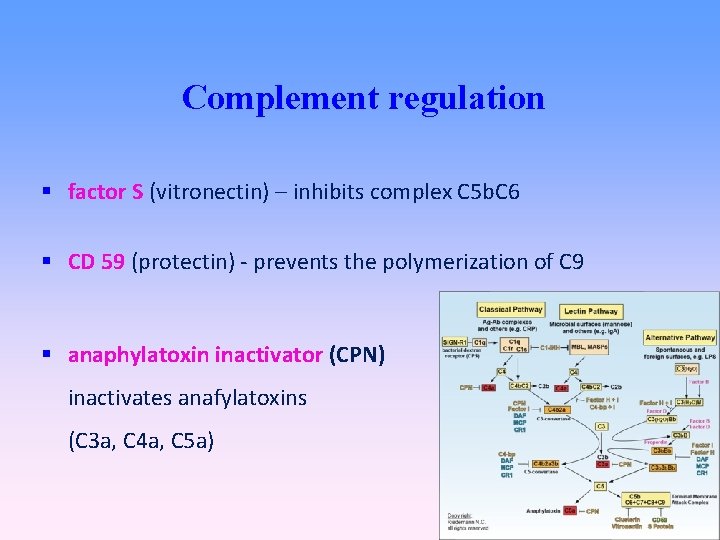
Complement regulation factor S (vitronectin) – inhibits complex C 5 b. C 6 CD 59 (protectin) - prevents the polymerization of C 9 anaphylatoxin inactivator (CPN) inactivates anafylatoxins (C 3 a, C 4 a, C 5 a)
Complement receptors Bind fragments of complement components CR 1 - on various cells - promotes C 3 b, C 4 b decay - stimulate phagocytosis - erythrocyte transport of immunecomplexes CR 2 - on B lymphocytes and FDC - activation of B cells
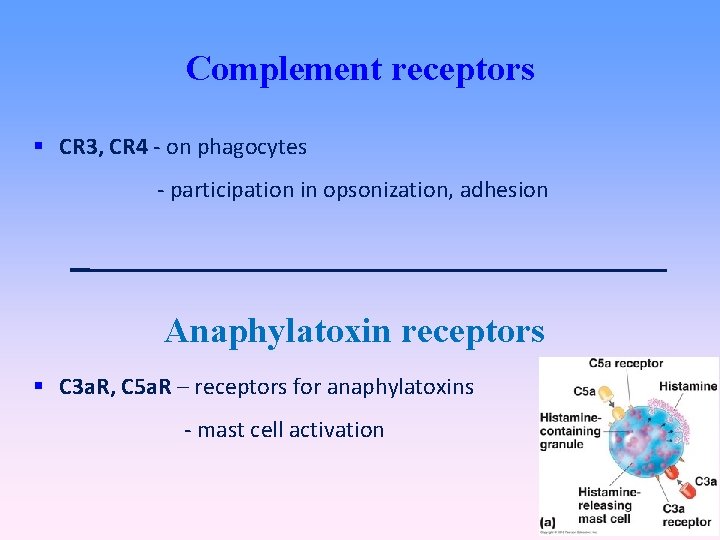
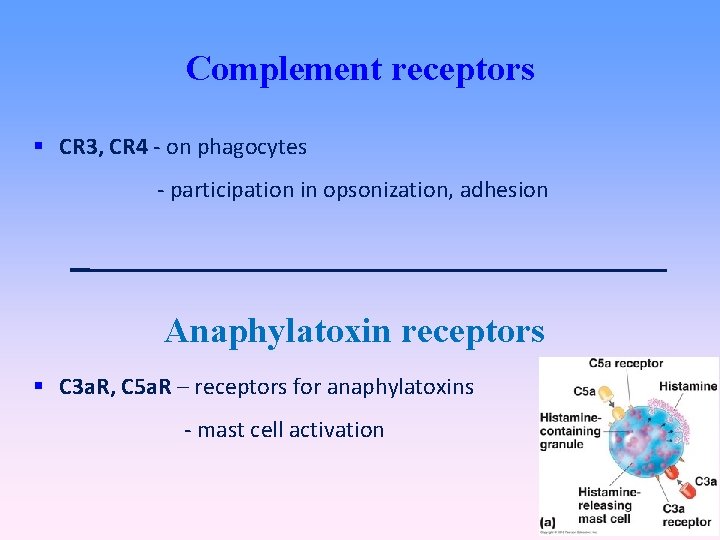
Complement receptors CR 3, CR 4 - on phagocytes - participation in opsonization, adhesion Anaphylatoxin receptors C 3 a. R, C 5 a. R – receptors for anaphylatoxins - mast cell activation
Basophils and mast cells and their importance in immune responses
Mast cells Mucosal mast cells - in the mucous membranes of respiratory and gastrointestinal tract, produce histamine, serotonin, heparin, tryptase, leukotriene C 4. . . , participate in parasitosis and allergy Connective tissue mast cells – in parasitosis and allergy are not participating
Mast cell functions Defense against parasitic infections In pathological circumstances, responsible for the allergic reactions (immunopathological reaction type I) Apply during inflammation, in angiogenesis, in tissue remodeling
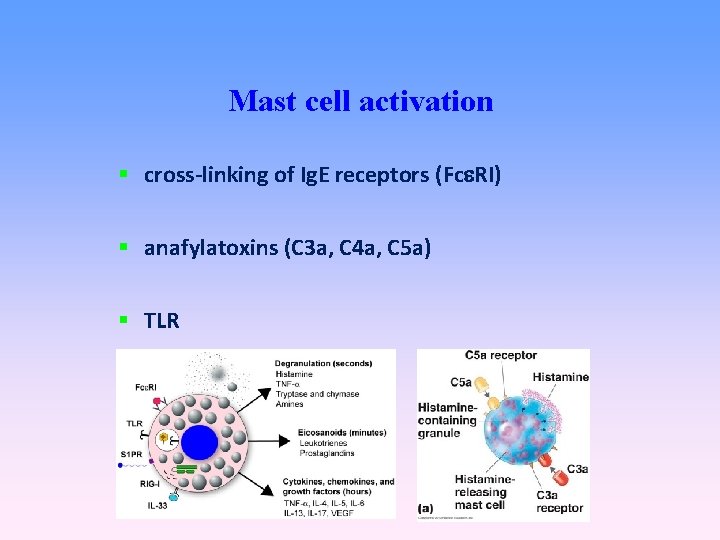
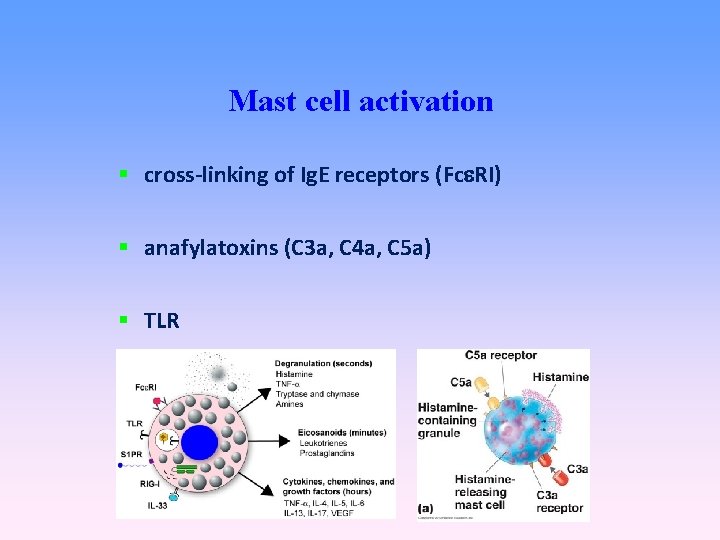
Mast cell activation cross-linking of Ig. E receptors (Fc RI) anafylatoxins (C 3 a, C 4 a, C 5 a) TLR
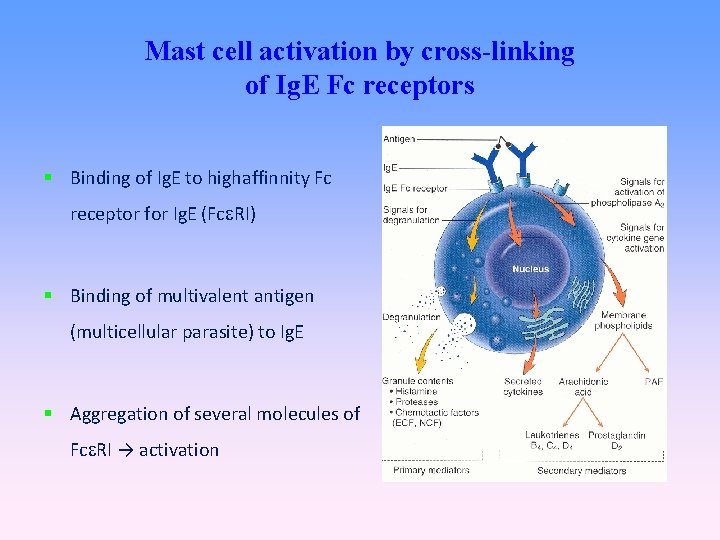
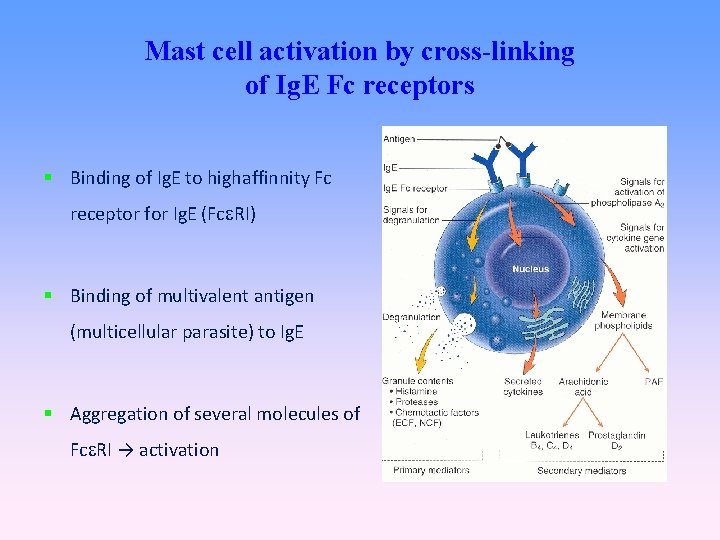
Mast cell activation by cross-linking of Ig. E Fc receptors Binding of Ig. E to highaffinnity Fc receptor for Ig. E (Fc RI) Binding of multivalent antigen (multicellular parasite) to Ig. E Aggregation of several molecules of Fc RI → activation
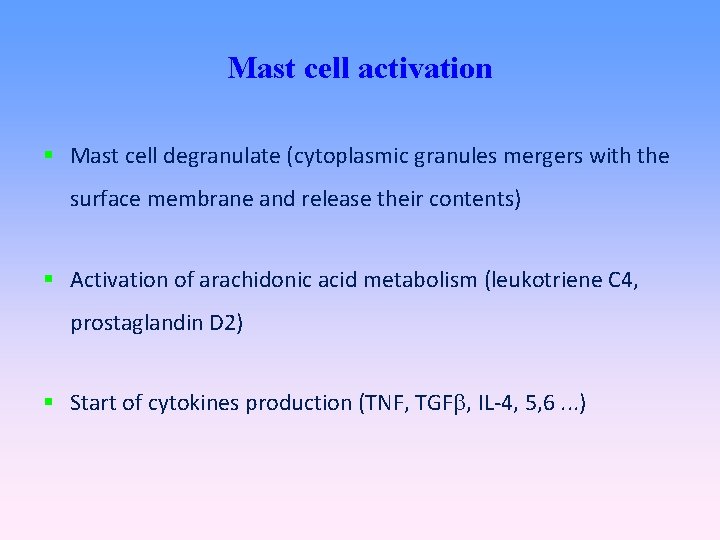
Mast cell activation Mast cell degranulate (cytoplasmic granules mergers with the surface membrane and release their contents) Activation of arachidonic acid metabolism (leukotriene C 4, prostaglandin D 2) Start of cytokines production (TNF, TGF , IL-4, 5, 6. . . )
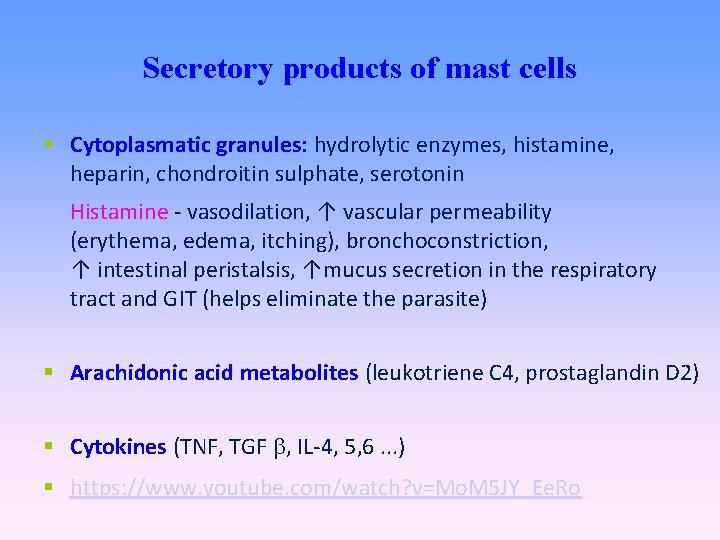
Secretory products of mast cells Cytoplasmatic granules: hydrolytic enzymes, histamine, heparin, chondroitin sulphate, serotonin Histamine - vasodilation, ↑ vascular permeability (erythema, edema, itching), bronchoconstriction, ↑ intestinal peristalsis, ↑mucus secretion in the respiratory tract and GIT (helps eliminate the parasite) Arachidonic acid metabolites (leukotriene C 4, prostaglandin D 2) Cytokines (TNF, TGF , IL-4, 5, 6. . . ) https: //www. youtube. com/watch? v=Mo. M 5 JY_Ee. Ro
Basophils Differentiate from myeloid precursor Receptor equipment, content of granules, the mechanisms of stimulation and functions are very similar to mast cells Play a role in parasitic infections and allergies Basophil activation markers: CD 63, (CD 203)
Immune mechanisms of inflammation (Local and systemic reactions)
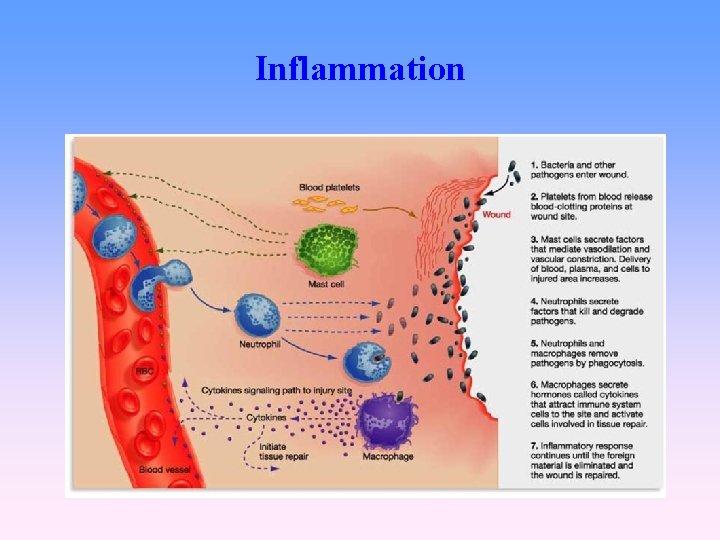
Inflammation Is a protective physiological response leading to protection against infection in damaged sites, localization of damage, elimination of necrotic cells and tissue repair.
Causes of inflammation Physical injury Infection by pathogens Damage caused by chemicals Cancer Alergic disease Autoimmune disease
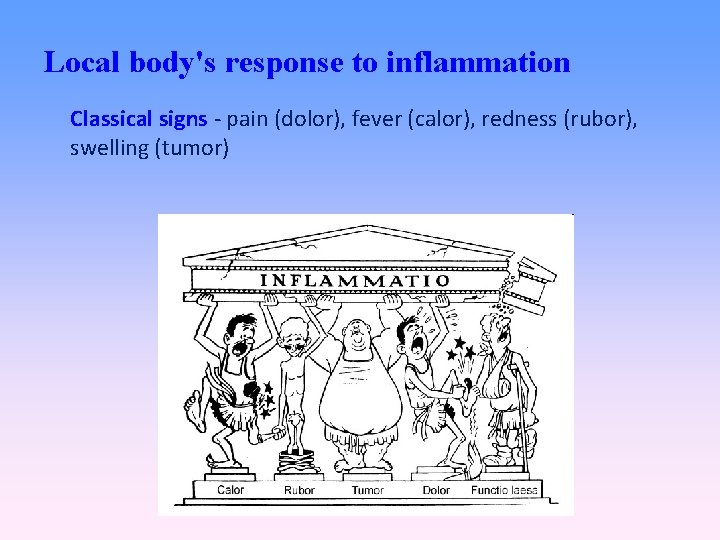
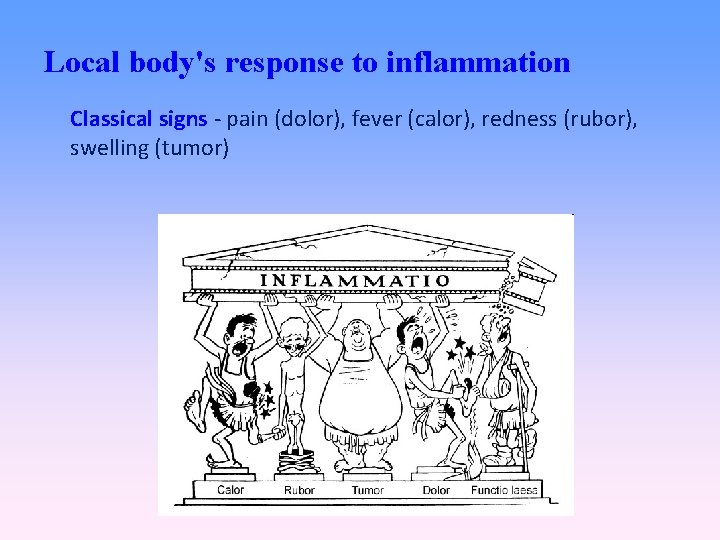
Local body's response to inflammation Classical signs - pain (dolor), fever (calor), redness (rubor), swelling (tumor)
Inflammation • The first signals for the development of inflammatory response come from mast cells, phagocytes, and the substances released from damaged cells and components of extracellular matrix. • An antigen-specific mechanisms (T and B lymphocytes) are activated with longer duration of local inflammation.
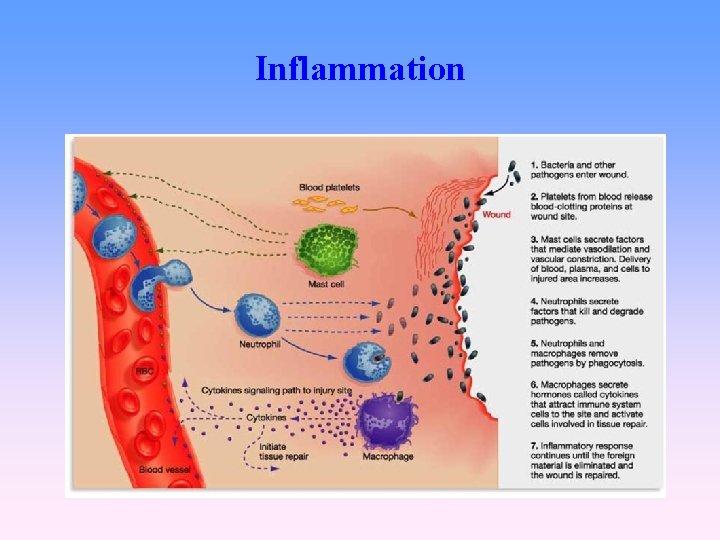
Inflammation
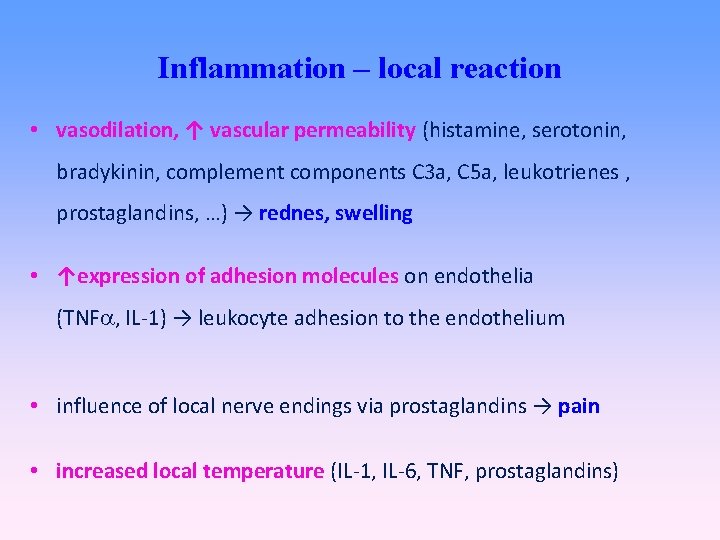
Inflammation – local reaction • vasodilation, ↑ vascular permeability (histamine, serotonin, bradykinin, complement components C 3 a, C 5 a, leukotrienes , prostaglandins, …) → rednes, swelling • ↑expression of adhesion molecules on endothelia (TNF , IL-1) → leukocyte adhesion to the endothelium • influence of local nerve endings via prostaglandins → pain • increased local temperature (IL-1, IL-6, TNF, prostaglandins)
Inflammation - systemic reaction • Leukocytosis • Fever (TNF, IL-1, IL-6, IFN ) ↑ tissue metabolism ↑ mobility of leukocytes ↑ formation of IFN, cytokines, Ig ↑ expression of Hsp • Acute phase proteins (IL-6, TNF , IL-1) CRP, SAP - opsonization and complement activation
Inflammation - systemic reaction • Septic shock - the massive penetration of microorganisms into the bloodstream (TNF) • Anaphylactic shock - basophil and mast cells activation with allergen (histamine)
Tissue repair • elimination of damaged cells with phagocytes • activation of fibroplastic mechanisms • activation of angiogenesis • regeneration and tissue remodeling • TGF
Antigens
Antigen (immunogen) substance which provokes specific immune response usually proteins or polysaccharides (lipids and nucleic acids only in the combination with proteins or polysaccharides) molecules > 5 k. Da (optimal size of the antigen molecules is about 40 k. Da)
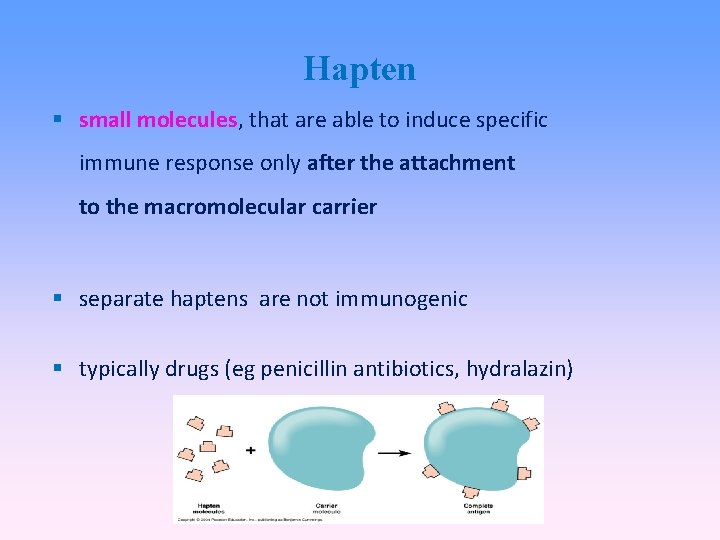
Hapten small molecules, that are able to induce specific immune response only after the attachment to the macromolecular carrier separate haptens are not immunogenic typically drugs (eg penicillin antibiotics, hydralazin)
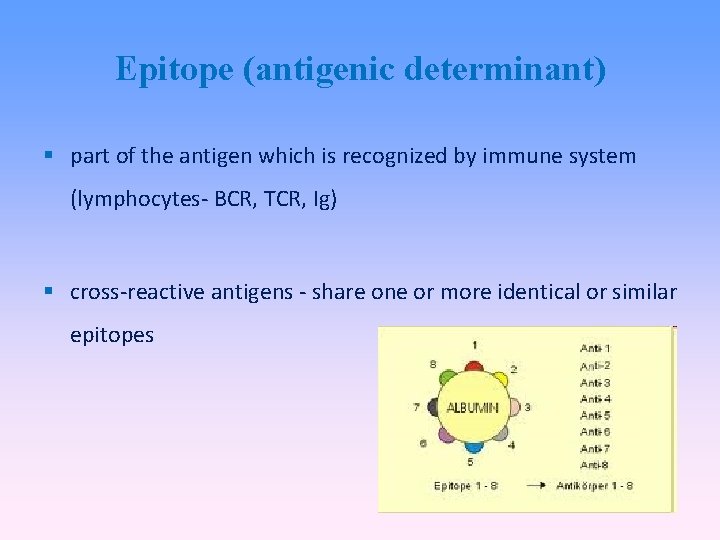
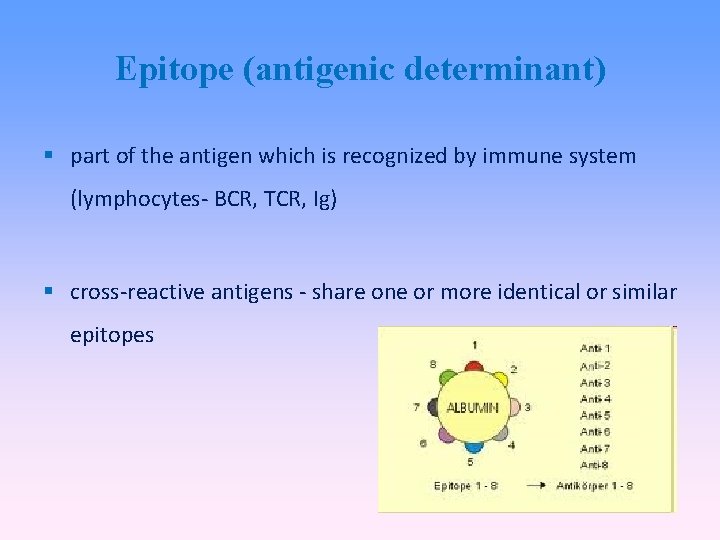
Epitope (antigenic determinant) part of the antigen which is recognized by immune system (lymphocytes- BCR, TCR, Ig) cross-reactive antigens - share one or more identical or similar epitopes
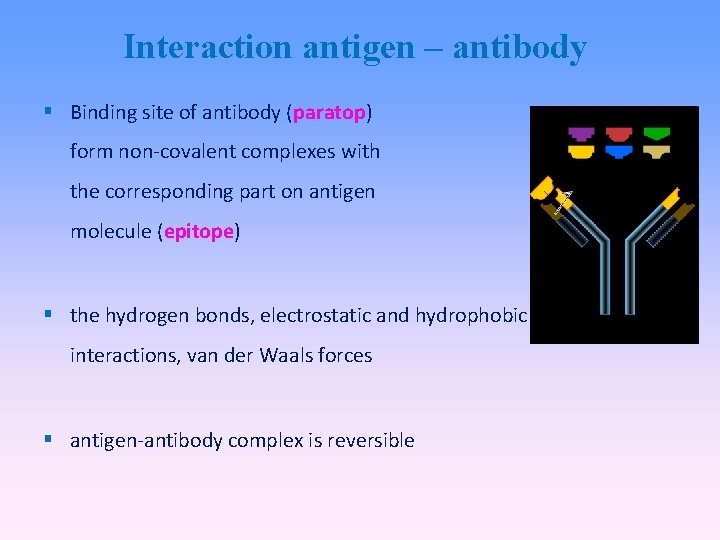
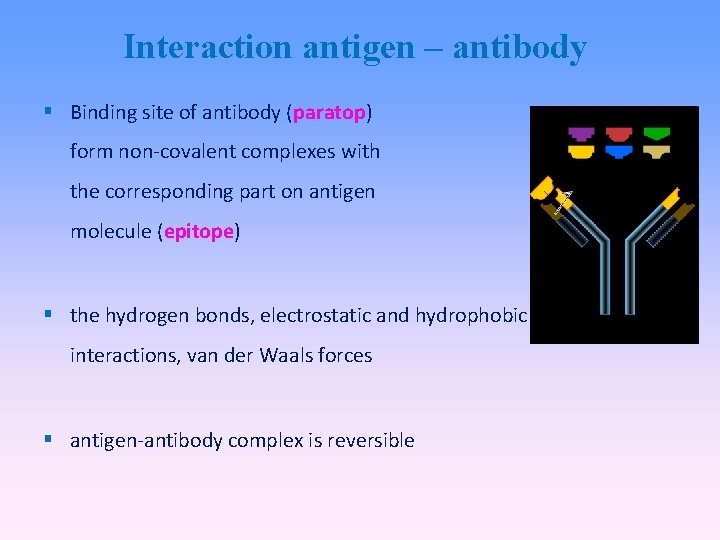
Interaction antigen – antibody Binding site of antibody (paratop) form non-covalent complexes with the corresponding part on antigen molecule (epitope) the hydrogen bonds, electrostatic and hydrophobic interactions, van der Waals forces antigen-antibody complex is reversible
Antigen endogenous antigens - autoantigens (self Ag) exogenous antigens - foreign substances from the environment allergen is exoantigen that in the susceptible individuals can cause pathological (allergic) immune response
Properties of antigen immunogenicity proteins> carbohydrates> macromolecule complexes (glycoproteins, nucleoproteins, and glycolipids)> lipids specificity
Factors affecting immunogenicity Physical: solubility - insoluble Ag more immunogenic molecular weight - ideal 5 -40 k. Da Chemical: structure - the number of determinants degradability - "ease" of uncovering the determinants in antigen presenting cells (APC cell) Biological: biological heterogeneity genetic and physiological disposition of the body
Degree of foreignness Autogeneic - antigens of the same individual Syngeneic - antigens of genetically identical individuals (eg twins) Allogeneic (alloantigens) - antigens genetically different individuals of the same species Xenogeneic (heterologous) - antigens derived from individuals of different species (eg monkey kidney transplant man)

Types of antigens according to antigen presentation T- dependent antigens T- independent antigens
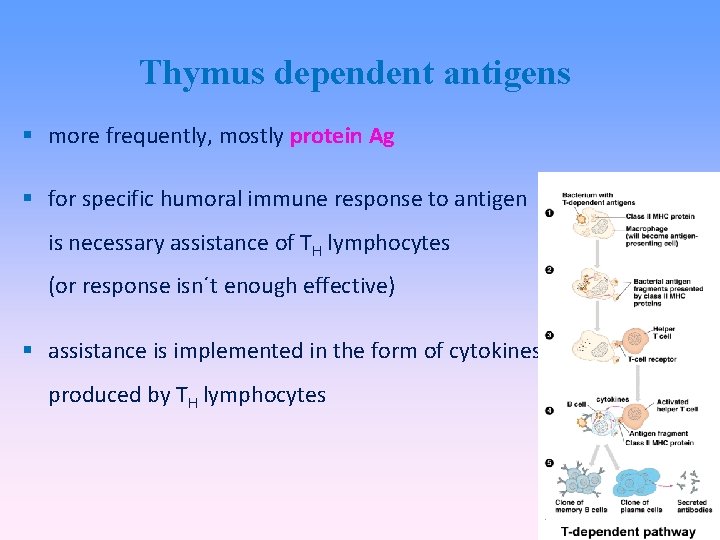
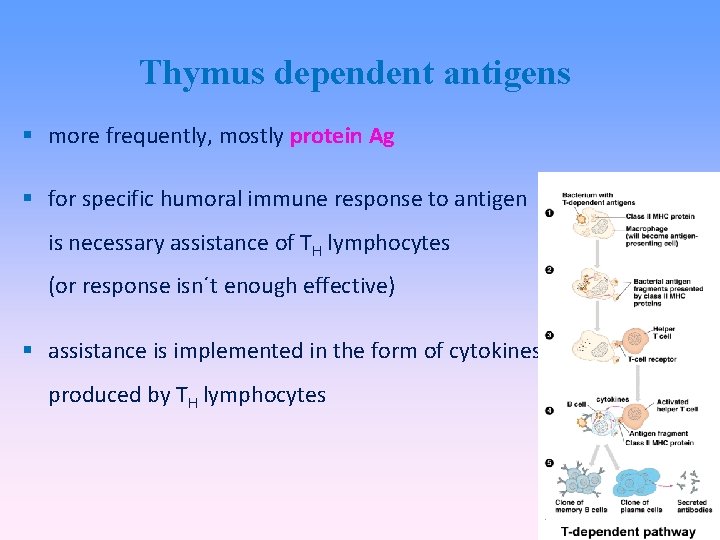
Thymus dependent antigens more frequently, mostly protein Ag for specific humoral immune response to antigen is necessary assistance of TH lymphocytes (or response isn´t enough effective) assistance is implemented in the form of cytokines produced by TH lymphocytes
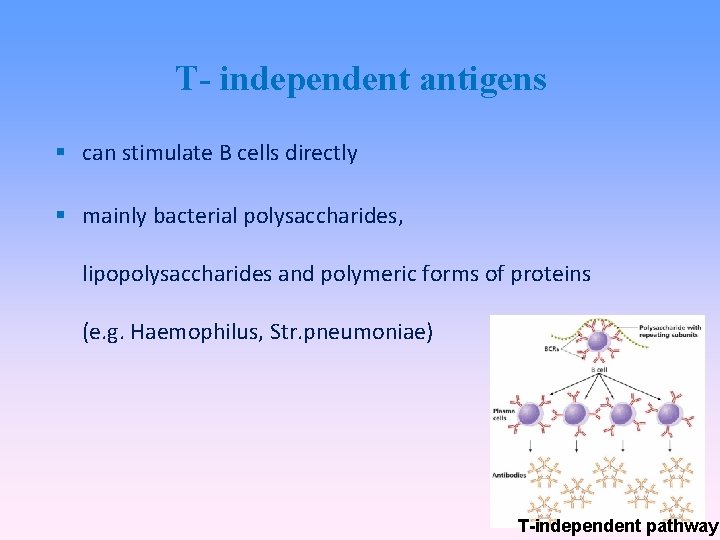
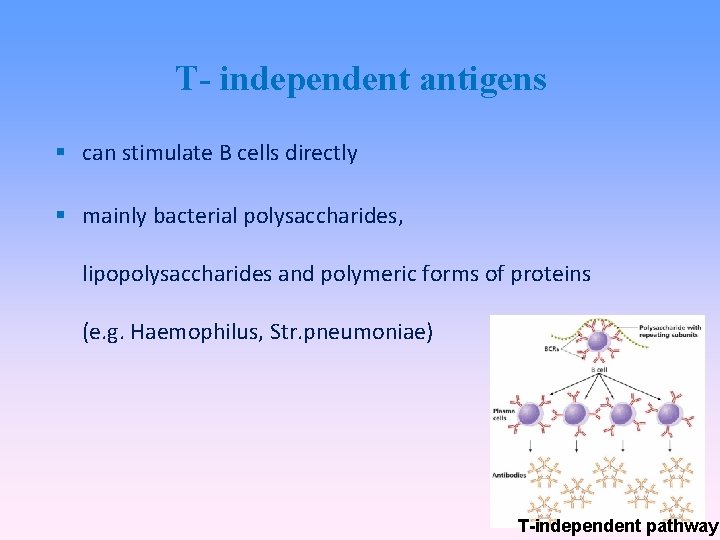
T- independent antigens can stimulate B cells directly mainly bacterial polysaccharides, lipopolysaccharides and polymeric forms of proteins (e. g. Haemophilus, Str. pneumoniae) T-independent pathway
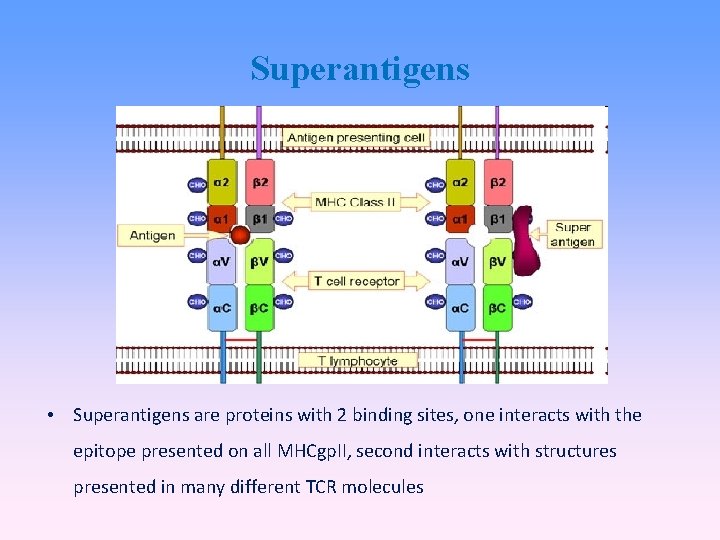
Superantigens stimulate T cells polyclonaly and massively (massive cytokine release) massive activation of T cells can cause shock e. g. bacterial toxins (Staph. aureus, Str. pyogenes, Pseud. aeruginosa)
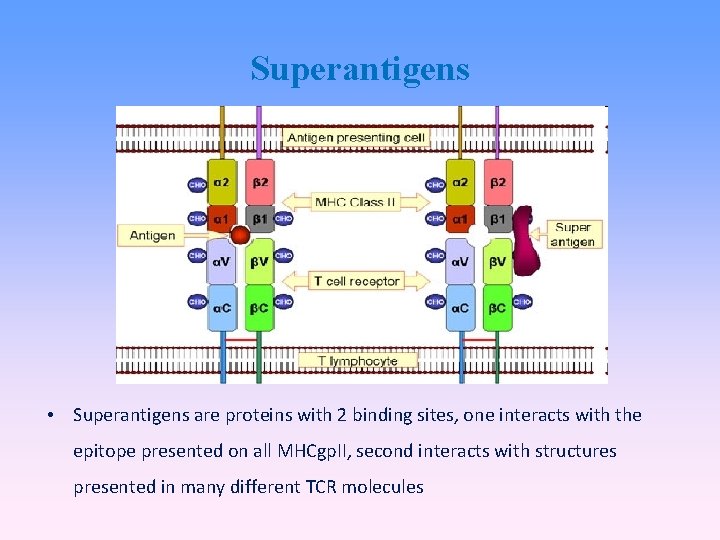
Superantigens • Superantigens are proteins with 2 binding sites, one interacts with the epitope presented on all MHCgp. II, second interacts with structures presented in many different TCR molecules
Sequestered antigens autoantigens, that are normally hidden to immune system and therefore unknow (e. g. brain, the lens of the eye , testes) if they are "uncovered" by demage, exposed to the immune system, are recognized as foreign (one of theories of autoimmune processes)
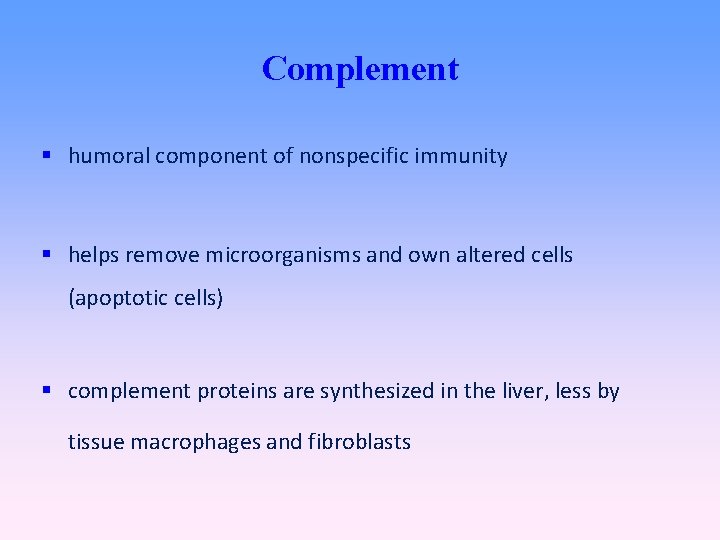
Immunologically privileged sites brain, eye, gonads are protected from potentially damaging inflammatory immune responses this tissues are far less rejected in allogeneic transplant (cornea) this privileged position is not absolute
Immunologically privileged sites Mechanisms of protection: isolation from the immune system (blood-brain barrier) preferences of Th 2 and suppression of Th 1 -response production of immunosuppressive cytokines (TGFβ) Fas. L expression -active protection against effector T-lymphocytes increased expression of membrane complement inhibitors
Thank you for your attention